User login
Esophageal Perforation, Complication of EGD
Esophagogastroduodenoscopy (EGD) carries a small but serious risk of esophageal perforation.13 With its potential for sepsis and fatal mediastinitis, prompt recognition and treatment are essential for favorable outcomes. The risk of perforation with diagnostic flexible EGD is 0.03%, which is an improvement from the 0.1%0.4% risk associated with rigid endoscopy.4 However, the risk of perforation can dramatically increase to 17% depending on the methods of therapeutic intervention and underlying risk factors (Table 1).1, 57
| Level of operator experience |
| Underlying esophageal disease |
| Zenker's diverticulum |
| Eosinophilic esophagitis |
| Esophageal or mediastinal irradiation |
| Esophageal malignancy |
| Esophageal strictures |
| Systemic disease |
| Anterior cervical osteophytes |
| Advanced liver cirrhosis |
| Diabetes mellitus |
| Scleroderma |
| Complexity of intervention |
| Esophageal stent placement |
| Pneumatic dilation |
| Other |
| Heavy sedation |
| Advanced age |
It is estimated that 33%75% of all esophageal perforations are iatrogenic.8 Of those caused by EGD, therapeutic interventions portend an increased risk compared with the risk of diagnostic endoscopy alone (Table 2).4 With the expanding role of flexible EGD and the increasing number of procedures performed, this modest risk per procedure still translates into a sizable number of perforations with their ensuing complications.4, 7 Mortality rates following esophageal perforation may approach 25%.9
| Endoscopic procedure | Esophageal perforation risk |
|---|---|
| Diagnostic | 0.03% |
| Dilation | 0.25% (normal esophagus)4%7% (achalasia)*7% (gastric outlet obstruction)*17% (strictures due to caustic agent) |
| Thermal method (treatment of malignancy) | 10% |
| Endoprosthesis | 3% |
| Variceal sclerotherapy | 1%5% (acute perforation)2%5% (delayed perforation) |
| Band ligation | 0.7% (perforation) |
| Nonvariceal hemostasis (use of sclerosant or cautery) | 0%2% (first hemostasis)4% (hemostasis repeated within 2448 hours) |
ANATOMY AND PATHOPHYSIOLOGY
The most common site of perforation is at the level of the cricopharyngeus, as it is a narrow introitus leading to the esophagus. The risk of perforation at this location is further increased with the presence of a Zenker's diverticulum or cervical osteophytes. The second most common site is proximal to the lower esophageal sphincter because of the angulation of the hiatus and the high frequency of esophageal webs, rings, reflux strictures, and hiatal hernias. The relatively straight middle esophagus is an uncommon site for perforations.
Cervical perforations are less commonly caused by organic lesions of the esophagus. Often, they are the result of technique and manipulation of the endoscope, or of certain conditions associated with the jaw, neck, or spinal column that are unfavorable for endoscopy. The risk of cervical perforation increases with the presence of bony spurs, as the upper esophagus is compressed over the underlying spinal column. Thoracic perforations, however, are more commonly seen with organic esophageal obstruction. These obstructions may be caused by an underlying inflammatory process, benign stricture, or neoplasm. In these cases, the risk of thoracic perforation is increased with blind procedures. Thoracic perforations carry a worse prognosis if diagnosis is delayed, or if the underlying obstruction cannot be removed.10
Esophageal perforation leads to periesophageal tissues being contaminated by food, secretions, air, or gastric contents and may be followed by chemical tissue injury and infection. The nature and extent of infection depend on the site of esophageal perforation. Cervical esophageal perforation can cause retropharyngeal space infection, which has the potential to extend directly into the posterior mediastinum via the danger space, which is between the retropharyngeal and prevertebral spaces and extends from the base of the skull descending freely throughout the entire length of the posterior mediastinum. With thoracic perforations, esophageal contents can enter the pleural space by negative intrathoracic pressure with subsequent pleural contamination and empyema.8, 1113
Pathogens responsible for infections after esophageal perforation vary based on several factors including site of perforation, clinical status of patient when perforation occurs (hospitalized versus not hospitalized, critically ill versus healthy), receipt of enteral nutrition, gastric acid suppression with H2‐receptor antagonists or proton‐pump inhibitors, immunosuppression, and recent (or current) receipt of antimicrobials. In nonintubated, healthy adults not on antimicrobial therapy, organisms in the upper esophagus are essentially identical to those in the oropharynx and include viridans streptococci, Haemophilus species, and anaerobes. During critical illness and following antibiotic therapy, the normal oral flora is rapidly replaced by aerobic Gram‐negative bacilli, Staphylococcus aureus, and yeast.14 The stomach, which is normally devoid of bacteria, can likewise be colonized with pathogenic organisms in the setting of gastric acid suppression and enteral nutrition.15, 16
SIGNS AND SYMPTOMS
Esophageal perforation should be considered after EGD, dilation, sclerotherapy, variceal banding, and esophageal stenting. However, perforation can also result from other invasive procedures such as insertion of feeding and nasogastric tubes, rapid sequence intubation, and transesophageal echocardiography.
The clinical triad of esophageal perforation includes pain, fever, and subcutaneous air.17 In a study by Wychulis et al., among 33 patients with esophageal perforation, 75% demonstrated all 3 findings.10 Pain is the most sensitive finding and occurs in nearly all patients identified with esophageal perforation. Crepitation, which results from air dissecting along soft tissue planes of the mediastinum and into the neck, occurs in up to 70% with cervical perforation and 30% with thoracic perforation.8, 10, 18
Clinical presentation and outcomes vary depending on the location of the perforation (Table 3).8 Cervical perforation is usually associated with anterior neck pain, located at the anterior border of the sternocleidomastoid muscle. Movement of the neck and palpation typically aggravate the pain. Thoracic perforation typically presents as substernal chest pain, often with a component of pleurisy. Pleural effusions are present in 50% of thoracic perforations, and mediastinitis is more likely to occur.19 Hamman's sign, a finding characterized by an audible crunch with chest auscultation, is suggestive of mediastinal emphysema. Perforation of the intra‐abdominal esophagus can result in epigastric pain and signs of acute abdomen.10, 17 Subcutaneous emphysema occurs more frequently with cervical perforation but can be present regardless of location.10 Secondary infections following esophageal perforation can manifest with an accelerated clinical course leading to sepsis and shock.
| Location of perforation | Symptom | Sign* |
|---|---|---|
| ||
| Cervical esophagus | Muscle spasm Dysphonia Hoarseness Dysphagia | Anterior neck tendernessTenderness on cervical motionSubcutaneous emphysema |
| Thoracic esophagus | Substernal chest pain Dysphagia Odynophagia | Cyanosis, Dyspnea Hamman's sign Pleural effusion Subcutaneous emphysema |
| Intraabdominal esophagus | Epigastric pain | Acute abdomenSubcutaneous emphysema |
DIAGNOSIS
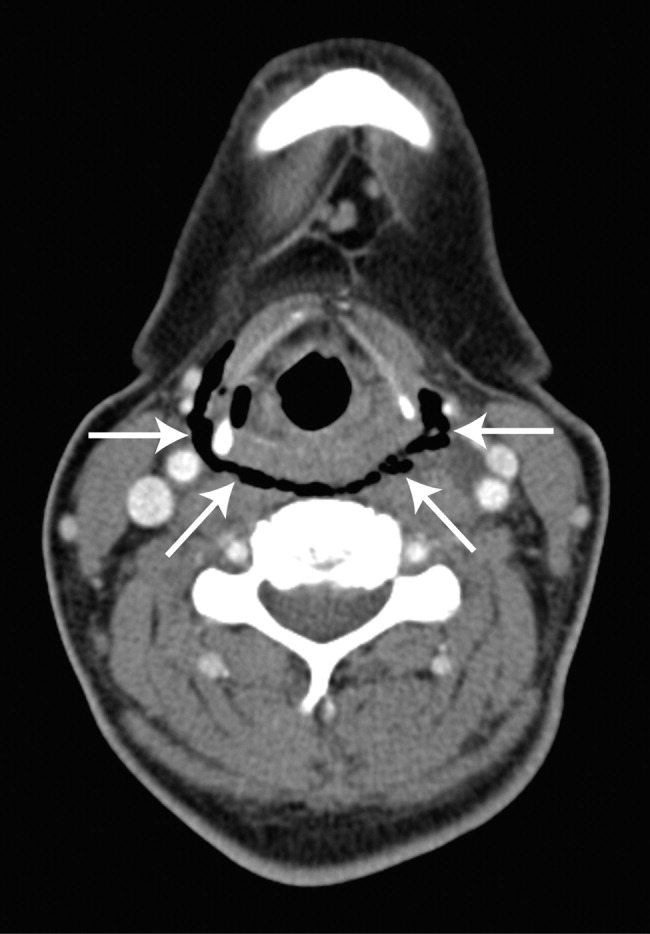
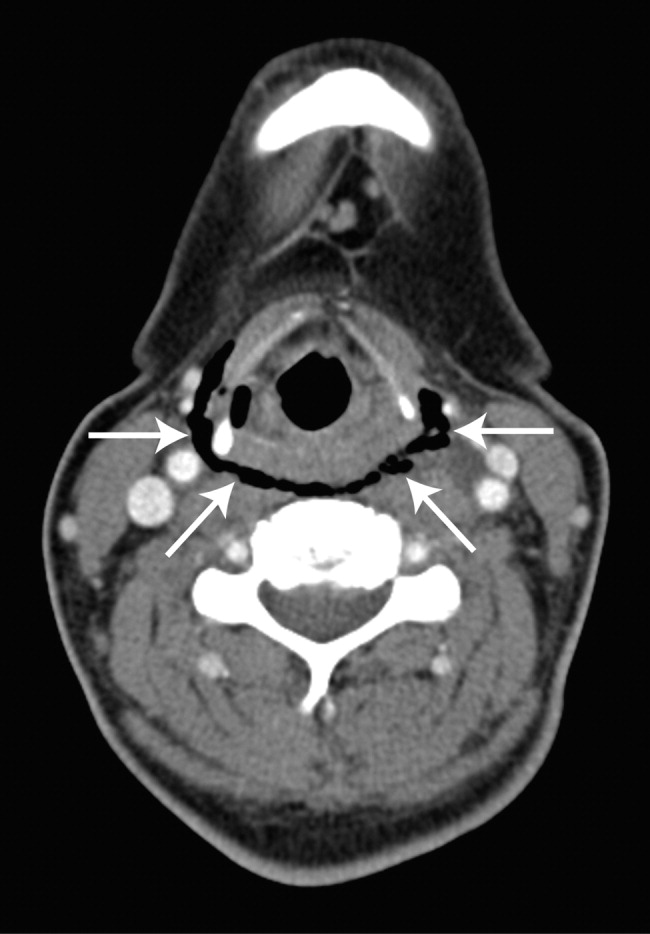
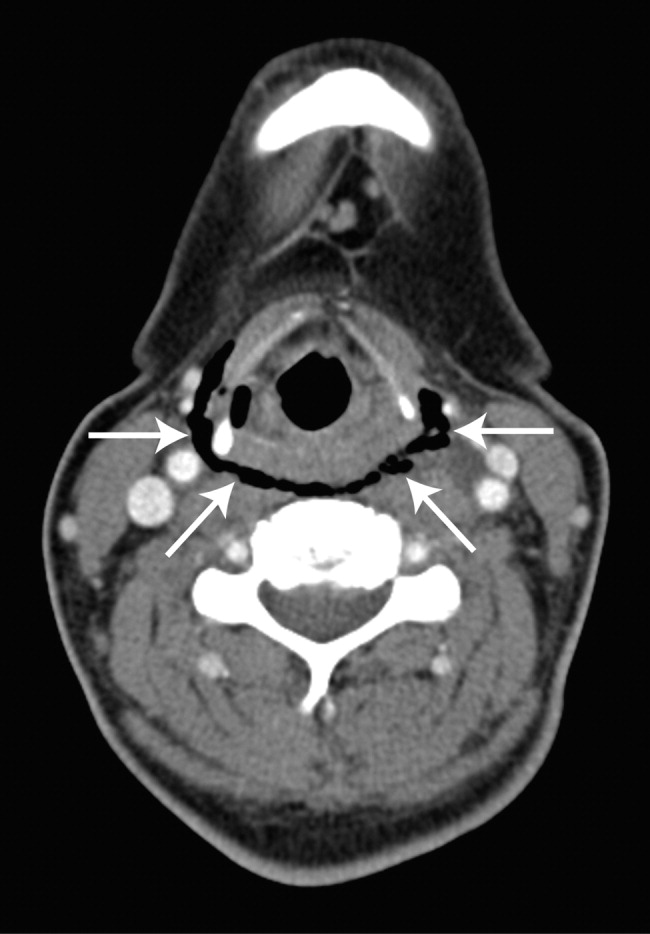
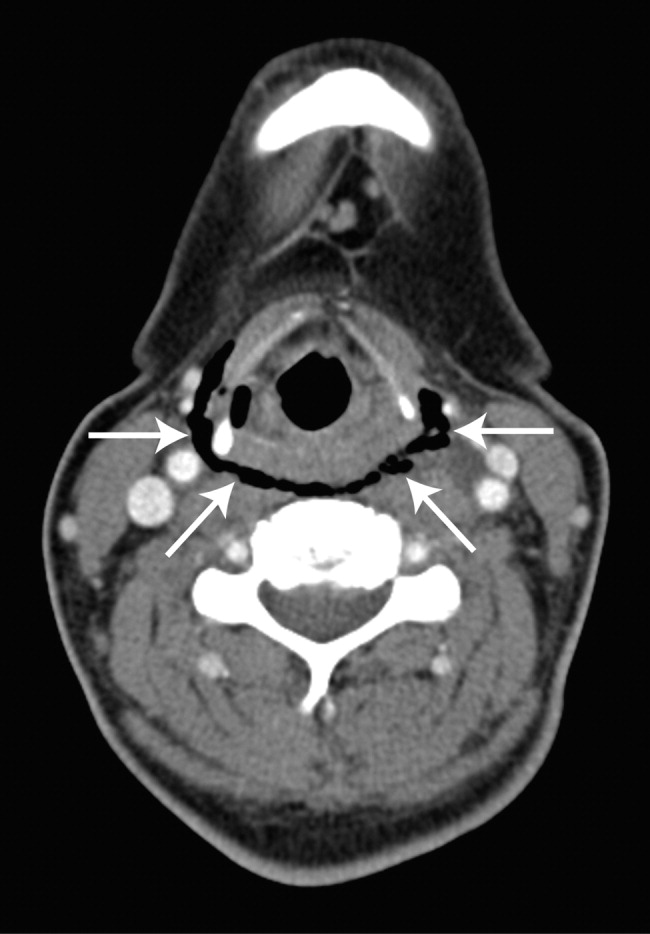
Clinical suspicion of esophageal perforation should prompt necessary radiographic studies to establish the diagnosis.18, 20 Contrast‐enhanced computed tomography (CT) scans of the neck and chest are preferable because of their increased sensitivity in localizing the site and showing the extent of perforation and abscess. CT scans may reveal subcutaneous or mediastinal air, abscess cavities adjacent to the esophagus, and fistulas between the esophagus and mediastinum (Figs. 1 and 2).2022 Results of contrast studies may be negative and warrant repeating within several hours.19

If CT scans cannot be performed, neck (soft‐tissue) and chest x‐rays may be useful. Although plain films have limited value in evaluating the retropharyngeal space, they can reveal soft‐tissue emphysema, a widened mediastinum, pulmonary infiltrates or effusions, neck abscess, and mediastinal air‐fluid levels. In cervical perforation, a lateral film of the neck can show air in deep cervical tissue before clinical signs are apparent.
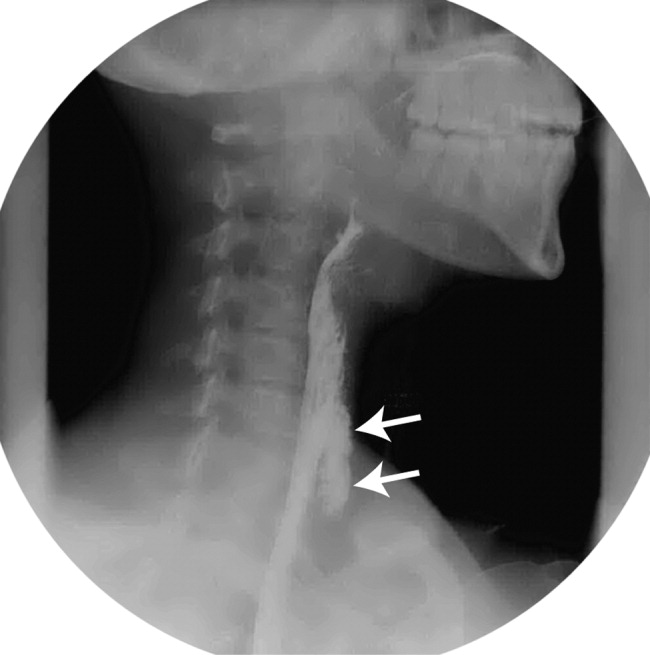
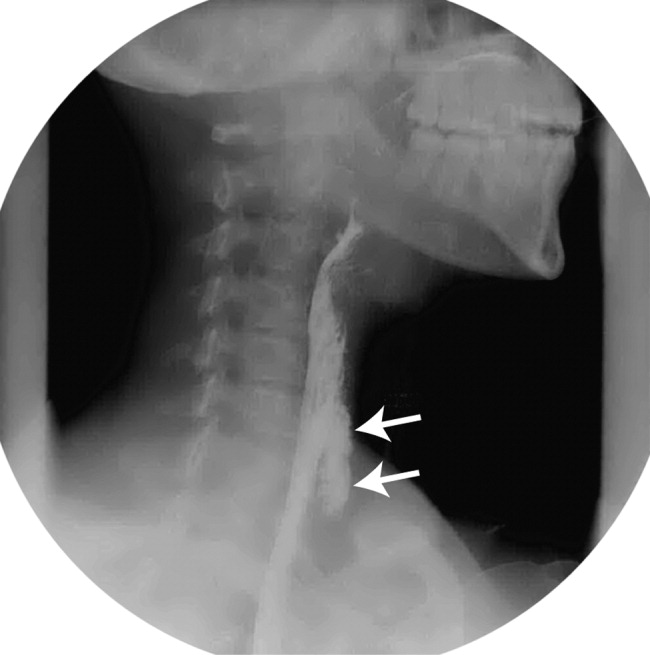
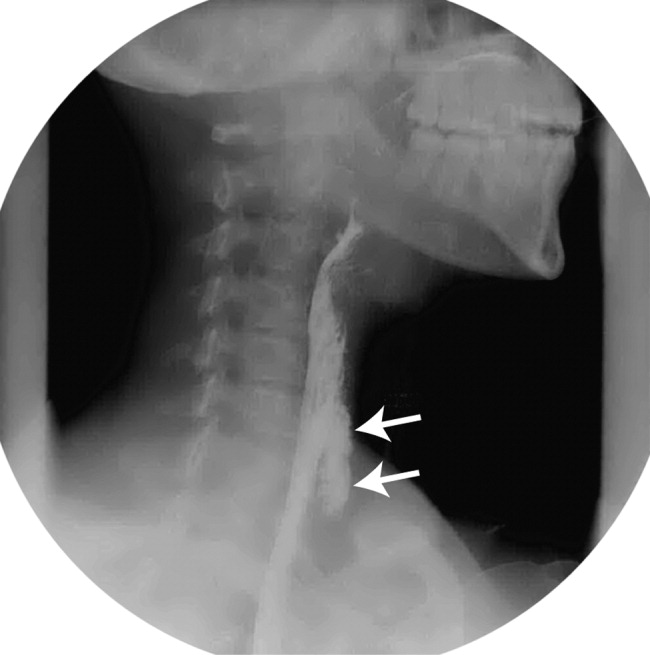
Swallow studies with Gastrografin (meglumine diatrizoate) are useful in defining the exact location of the perforation (Fig. 3). However, the false‐negative rate of swallow studies can exceed 10%, especially if the patient is upright during the study. When the contrast propagates past the site of perforation too quickly, it may not extravasate.23 Although barium may provide slightly greater contrast, it may add to the problem of foreign body reaction in the area of perforation.18 An additional complication of barium is that once it has extravasated, it is not readily absorbed. The persistence of extravasated barium makes it difficult to assess the resolution of an esophageal tear on subsequent fluoroscopic or CT exams. Hence, our institution avoids using barium to evaluate esophageal perforation, unless Gastrografin swallow has excluded any major esophageal perforation. Barium swallow may then be used to exclude small mural tears. Some medical centers elect to routinely screen their high‐risk patients with swallow evaluations after an EGD, although this is not common practice.8, 24
If the above workup is negative, the use of EGD may be considered for establishing the diagnosis if a high index of suspicion remains. However, the risks of EGD in this situation include extension of the perforation, further extravasation of esophageal contents, and difficulty with subsequent radiographic studies to visualize the perforation.19
MANAGEMENT
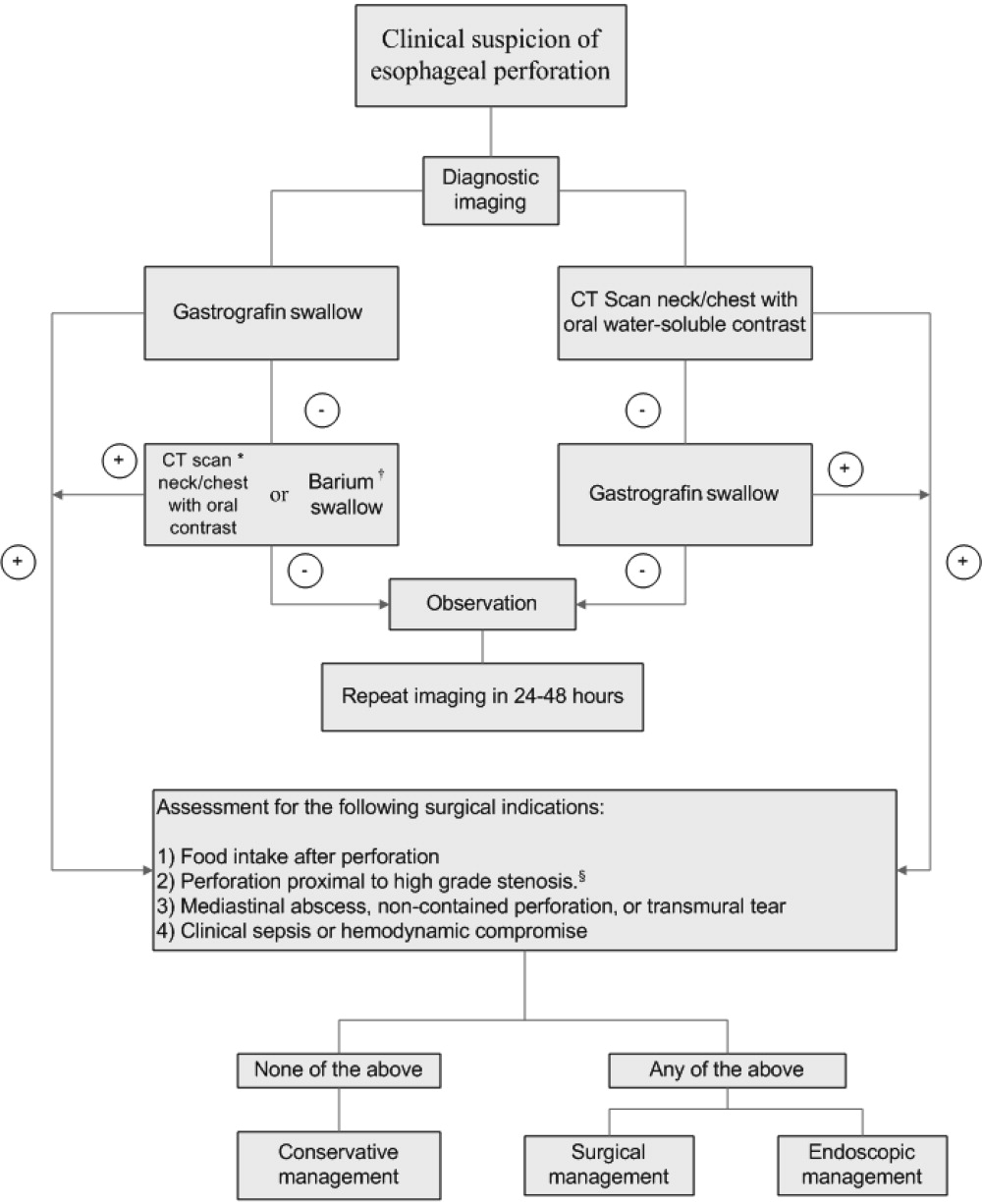
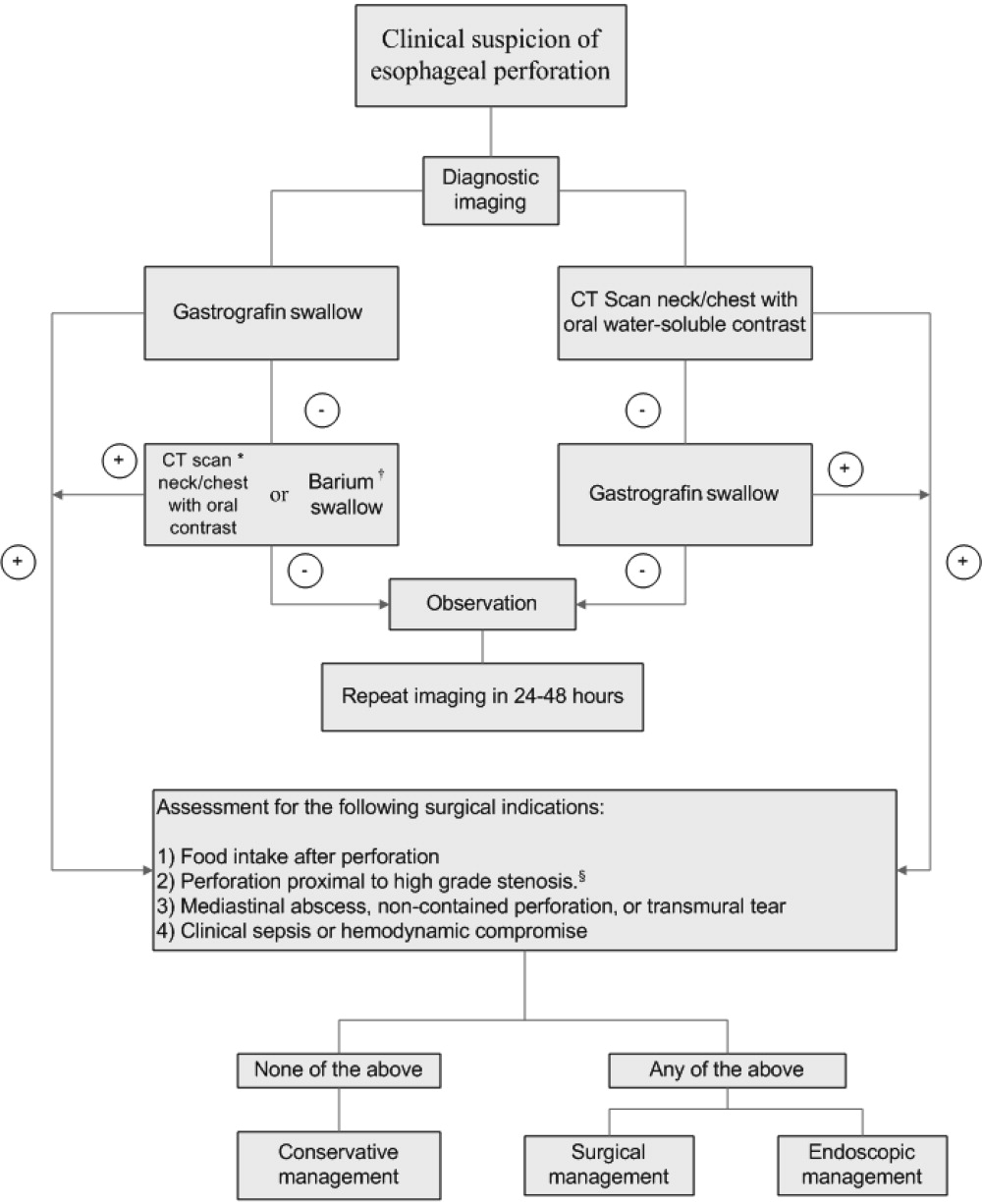
Once the diagnosis of esophageal perforation has been established, treatment options are individualized based on the clinical scenario. Currently, there are no established guidelines, and large randomized clinical trials comparing outcomes of operative versus nonoperative management have not been conducted (Fig. 4).25, 26 Outcomes associated with esophageal perforations depend on preoperative clinical condition, comorbidities, location and size of the perforation, nature of underlying esophageal disease (if any), and time to establish the diagnosis and initiate therapy.10 Delay in patient presentation or diagnosis beyond 24 hours following esophageal perforation has been associated with adverse outcomes.18, 27, 28
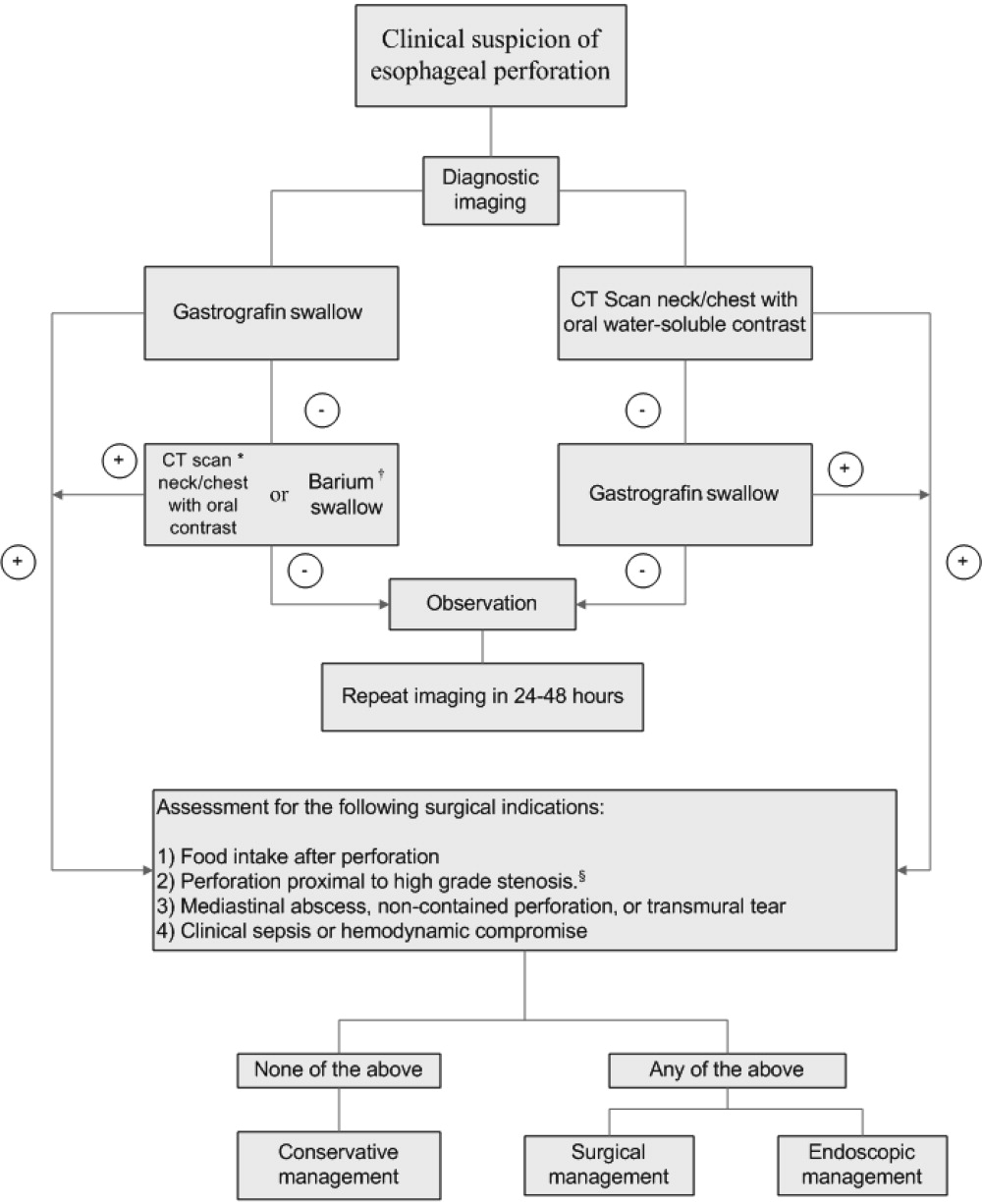
A conservative approach is appropriate when clinically stable patients with minimal symptoms have well‐contained, nontransmural tears. Management entails broad‐spectrum antibiotics, nothing by mouth, nasogastric suction, and parenteral nutrition.24 Early surgical consultation is recommended in all cases. Serial CT scanning is useful for following the resolution of fistulas and tears. An oral diet can be resumed when contrast or swallow studies show no extravasation of dye. Cervical perforations typically fare well with this approach.26, 29
Surgical therapy is recommended for patients with large or uncontained esophageal perforations, mediastinal abscesses, and/or sepsis.25, 27 Surgical options include esophageal diversion, esophagectomy, or drainage with or without primary repair. Drainage with primary repair is considered the treatment of choice, regardless of time to presentation. Esophagectomy is considered in cases of delayed or neglected perforations, extensive transmural necrosis or underlying cancer.30 Operative mortality is 0%30% when treated within 24 hours. This rate increases to 26%64% when treatment is delayed beyond 24 hours, reaffirming the importance of making a prompt diagnosis.8
Endoscopic intervention is gaining recognition for its role in the management of esophageal perforations, especially when the risks make surgery prohibitive. Therapeutic options include stenting and clipping a perforation, as well as debriding and draining an abscess. Endoscopists can successfully treat traumatic nonmalignant esophageal perforations smaller than 50% to 70% of the circumference with self‐expanding plastic stents.26 Another option is to use metallic clipping devices to treat small esophageal perforations (1 cm).3133 Combined with medical management and appropriate patient selection, the benefits of an endoscopic approach may potentially outweigh the risks of surgery.26, 29, 33, 34
Regardless of treatment approach, the appropriate and timely selection of empiric antibiotic therapy improves outcomes. Empiric antimicrobial therapy for esophageal perforation will depend on several host factors as well as the site of perforation. In healthy nonhospitalized adults, ampicillin‐sulbactam, clindamycin, and penicillin G plus metronidazole are good choices because of their excellent activity against oral microflora. In patients who are critically ill, are hospitalized, are immunosuppressed, or have gastric acid suppression, initial broad‐spectrum antimicrobials such as piperacillin‐tazobactam, imipenem, meropenem, or a third‐generation cephalosporin plus metronidazole (or clindamycin) should be initiated. Additional therapy against methicillin‐resistant Staphylococcus aureus or Candida sp. should be considered if the patient is critically ill or is known to be colonized with these organisms. Initial empiric therapy should be modified as necessary based on culture results. Total duration of therapy will vary based on location and magnitude of the infection, adjunctive surgical debridement, and pathogens involved.
SUMMARY
Despite being an extremely safe procedure, EGD carries a known serious risk of esophageal perforation. Mortality after esophageal perforation can approach 25%. Although diagnostic endoscopy has a perforation rate of less than 0.03%, the risk can approach 17% with therapeutic interventions such as stent placement and esophageal dilation. Factors influencing the risks of perforation include procedural complexity, operator experience, and underlying esophageal and systemic diseases. Furthermore, perforations complicated by infection can lead to fatal mediastinitis and sepsis. The clinical triad of esophageal perforation is fever, neck pain, and crepitus. The optimal diagnostic study is CT scan of the neck and thorax with water‐soluble oral contrast. Treatment options range from conservative management with broad‐spectrum antibiotics to surgery. Diagnosis of esophageal perforation within 24 hours is essential for favorable outcomes.
- .Complications of endoscopic gastrointestinal dilation techniques.Gastrointest Endosc Clin N Am.1996;6:323–341.
- .Complications of upper gastrointestinal endoscopy.Gastrointest Endosc Clin N Am.1996;6:287–303.
- ,.Complications of upper gastrointestinal endoscopy and their management.Gastrointest Endosc Clin N Am.1994;4:551–570.
- ,,,,.Treatment of endoscopic esophageal perforation.Surg Endosc.1999;13:962–966.
- ,,,.Unsedated small‐caliber esophagogastroduodenoscopy (EGD) versus conventional EGD: a comparative study [see comment].Gastroenterology.1999;117:1301–1307.
- ,,,,.Complications associated with esophagogastroduodenoscopy and with esophageal dilation.Gastrointest Endosc.1976;23(1):16–19.
- ,,.Comparison among the perforation rates of Maloney, balloon, and savary dilation of esophageal strictures.Gastrointest Endosc.2000;51(4 Pt 1):460–462.
- ,.Esophageal emergencies: things that will wake you from a sound sleep.Gastroenterol Clin N Am.2003;32:1035–1052.
- ,,, et al.Complications of upper GI endoscopy.Gastrointest Endosc.2002;55:784–793.
- ,,.Instrumental perforations of the esophagus.Dis Chest.1969;55(3):184–189.
- ,Complications of esophageal dilation and guidelines for their prevention.Gastrointest Endosc.1981;27:229–234.
- .Infectious complications associated with gastrointestinal endoscopy.Gastrointest Endosc Clin N Am.2000;10:215–232.
- ,,,The occurrence of bacteremia after esophageal dilation.Gastrointestinal Endoscopy1975;22(2):86–87.
- ,,,,,.The pathogenesis of ventilator‐associated pneumonia: its relevance to developing effective strategies for prevention.Respir Care.2005;50:725–739; discussion39–41.
- ,,, et al.Stomach as a source of colonization of the respiratory tract during mechanical ventilation: association with ventilator‐associated pneumonia.Eur Respir J.1996;9:1729–1735.
- ,,, et al.Gastric microbiota in elderly patients fed via nasogastric tubes for prolonged periods.J Hosp Infect.2006;63(1):79–83.
- ,.Retroesophageal abscess twenty‐five days after esophagoscopy. An unusual complication of endoscopy.Gastrointest Endosc.1972;18:167–168.
- ,,.The radiologist in prevention and diagnosis of instrumental perforation of the esophagus.South Med J.1974;67:830–836.
- ,,.Short‐ and long‐term outcome of esophageal perforation.Gastrointest Endosc.1995;41(2):130–134.
- ,,,.The diagnosis and treatment of esophageal perforations resulting from nonmalignant causes.Surg Today.1997;27:793–800.
- ,.Radiology of the retropharyngeal space.Clin Radiol.2000;55:740–748.
- ,,.Diagnosis and management decisions in infections of the deep fascial spaces of the head and neck utilizing computerized tomography.Laryngoscope.1982;92(6, Pt. 1):630–633.
- .Perforation of the esophagus.Ann Thorac Surg.1986;42:231–232.
- ,,, et al.Successfully treated case of cervical abscess and mediastinitis due to esophageal perforation after gastrointestinal endoscopy.Dis Esophagus.2002;15:250–252.
- ,.The spectrum of spontaneous and iatrogenic esophageal injury: perforations, Mallory‐Weiss tears, and hematomas.J Clin Gastroenterol.1999;29:306–317.
- .Treatment of esophageal perforations and anastomotic leaks: the endoscopist is stepping into the arena.Gastrointest Endosc.2005;61:897–900.
- ,,.Operative and nonoperative management of esophageal perforations.Ann Surg.1981;194(1):57–63.
- ,,.Current results of therapy for esophageal perforation.Am J Surg.1995;169:615–617.
- ,,.Successful endoscopic management of a cervical pharyngeal perforation and mediastinal abscess.Gastrointest Endosc.2005;61(1):158–160.
- ,,,,.Thoracic esophageal perforations: a decade of experience.[see comment].Ann Thorac Surg.2003;75:1071–1074.
- ,.Perforation: part and parcel of endoscopic resection? [comment].Gastrointest Endosc.2006;63:602–605.
- ,,,.Endoscopic clip application as an adjunct to closure of mature esophageal perforation with fistulae.Clin Gastroenterol Hepatol.2003;1(1):44–50.
- ,,.Endoscopic clipping of esophageal perforation after pneumatic dilation for achalasia.Endoscopy.1995;27:608–611.
- ,,, et al.Esophageal dilation.Gastrointest Endosc.2006;63:755–760.
Esophagogastroduodenoscopy (EGD) carries a small but serious risk of esophageal perforation.13 With its potential for sepsis and fatal mediastinitis, prompt recognition and treatment are essential for favorable outcomes. The risk of perforation with diagnostic flexible EGD is 0.03%, which is an improvement from the 0.1%0.4% risk associated with rigid endoscopy.4 However, the risk of perforation can dramatically increase to 17% depending on the methods of therapeutic intervention and underlying risk factors (Table 1).1, 57
| Level of operator experience |
| Underlying esophageal disease |
| Zenker's diverticulum |
| Eosinophilic esophagitis |
| Esophageal or mediastinal irradiation |
| Esophageal malignancy |
| Esophageal strictures |
| Systemic disease |
| Anterior cervical osteophytes |
| Advanced liver cirrhosis |
| Diabetes mellitus |
| Scleroderma |
| Complexity of intervention |
| Esophageal stent placement |
| Pneumatic dilation |
| Other |
| Heavy sedation |
| Advanced age |
It is estimated that 33%75% of all esophageal perforations are iatrogenic.8 Of those caused by EGD, therapeutic interventions portend an increased risk compared with the risk of diagnostic endoscopy alone (Table 2).4 With the expanding role of flexible EGD and the increasing number of procedures performed, this modest risk per procedure still translates into a sizable number of perforations with their ensuing complications.4, 7 Mortality rates following esophageal perforation may approach 25%.9
| Endoscopic procedure | Esophageal perforation risk |
|---|---|
| Diagnostic | 0.03% |
| Dilation | 0.25% (normal esophagus)4%7% (achalasia)*7% (gastric outlet obstruction)*17% (strictures due to caustic agent) |
| Thermal method (treatment of malignancy) | 10% |
| Endoprosthesis | 3% |
| Variceal sclerotherapy | 1%5% (acute perforation)2%5% (delayed perforation) |
| Band ligation | 0.7% (perforation) |
| Nonvariceal hemostasis (use of sclerosant or cautery) | 0%2% (first hemostasis)4% (hemostasis repeated within 2448 hours) |
ANATOMY AND PATHOPHYSIOLOGY
The most common site of perforation is at the level of the cricopharyngeus, as it is a narrow introitus leading to the esophagus. The risk of perforation at this location is further increased with the presence of a Zenker's diverticulum or cervical osteophytes. The second most common site is proximal to the lower esophageal sphincter because of the angulation of the hiatus and the high frequency of esophageal webs, rings, reflux strictures, and hiatal hernias. The relatively straight middle esophagus is an uncommon site for perforations.
Cervical perforations are less commonly caused by organic lesions of the esophagus. Often, they are the result of technique and manipulation of the endoscope, or of certain conditions associated with the jaw, neck, or spinal column that are unfavorable for endoscopy. The risk of cervical perforation increases with the presence of bony spurs, as the upper esophagus is compressed over the underlying spinal column. Thoracic perforations, however, are more commonly seen with organic esophageal obstruction. These obstructions may be caused by an underlying inflammatory process, benign stricture, or neoplasm. In these cases, the risk of thoracic perforation is increased with blind procedures. Thoracic perforations carry a worse prognosis if diagnosis is delayed, or if the underlying obstruction cannot be removed.10
Esophageal perforation leads to periesophageal tissues being contaminated by food, secretions, air, or gastric contents and may be followed by chemical tissue injury and infection. The nature and extent of infection depend on the site of esophageal perforation. Cervical esophageal perforation can cause retropharyngeal space infection, which has the potential to extend directly into the posterior mediastinum via the danger space, which is between the retropharyngeal and prevertebral spaces and extends from the base of the skull descending freely throughout the entire length of the posterior mediastinum. With thoracic perforations, esophageal contents can enter the pleural space by negative intrathoracic pressure with subsequent pleural contamination and empyema.8, 1113
Pathogens responsible for infections after esophageal perforation vary based on several factors including site of perforation, clinical status of patient when perforation occurs (hospitalized versus not hospitalized, critically ill versus healthy), receipt of enteral nutrition, gastric acid suppression with H2‐receptor antagonists or proton‐pump inhibitors, immunosuppression, and recent (or current) receipt of antimicrobials. In nonintubated, healthy adults not on antimicrobial therapy, organisms in the upper esophagus are essentially identical to those in the oropharynx and include viridans streptococci, Haemophilus species, and anaerobes. During critical illness and following antibiotic therapy, the normal oral flora is rapidly replaced by aerobic Gram‐negative bacilli, Staphylococcus aureus, and yeast.14 The stomach, which is normally devoid of bacteria, can likewise be colonized with pathogenic organisms in the setting of gastric acid suppression and enteral nutrition.15, 16
SIGNS AND SYMPTOMS
Esophageal perforation should be considered after EGD, dilation, sclerotherapy, variceal banding, and esophageal stenting. However, perforation can also result from other invasive procedures such as insertion of feeding and nasogastric tubes, rapid sequence intubation, and transesophageal echocardiography.
The clinical triad of esophageal perforation includes pain, fever, and subcutaneous air.17 In a study by Wychulis et al., among 33 patients with esophageal perforation, 75% demonstrated all 3 findings.10 Pain is the most sensitive finding and occurs in nearly all patients identified with esophageal perforation. Crepitation, which results from air dissecting along soft tissue planes of the mediastinum and into the neck, occurs in up to 70% with cervical perforation and 30% with thoracic perforation.8, 10, 18
Clinical presentation and outcomes vary depending on the location of the perforation (Table 3).8 Cervical perforation is usually associated with anterior neck pain, located at the anterior border of the sternocleidomastoid muscle. Movement of the neck and palpation typically aggravate the pain. Thoracic perforation typically presents as substernal chest pain, often with a component of pleurisy. Pleural effusions are present in 50% of thoracic perforations, and mediastinitis is more likely to occur.19 Hamman's sign, a finding characterized by an audible crunch with chest auscultation, is suggestive of mediastinal emphysema. Perforation of the intra‐abdominal esophagus can result in epigastric pain and signs of acute abdomen.10, 17 Subcutaneous emphysema occurs more frequently with cervical perforation but can be present regardless of location.10 Secondary infections following esophageal perforation can manifest with an accelerated clinical course leading to sepsis and shock.
| Location of perforation | Symptom | Sign* |
|---|---|---|
| ||
| Cervical esophagus | Muscle spasm Dysphonia Hoarseness Dysphagia | Anterior neck tendernessTenderness on cervical motionSubcutaneous emphysema |
| Thoracic esophagus | Substernal chest pain Dysphagia Odynophagia | Cyanosis, Dyspnea Hamman's sign Pleural effusion Subcutaneous emphysema |
| Intraabdominal esophagus | Epigastric pain | Acute abdomenSubcutaneous emphysema |
DIAGNOSIS
Clinical suspicion of esophageal perforation should prompt necessary radiographic studies to establish the diagnosis.18, 20 Contrast‐enhanced computed tomography (CT) scans of the neck and chest are preferable because of their increased sensitivity in localizing the site and showing the extent of perforation and abscess. CT scans may reveal subcutaneous or mediastinal air, abscess cavities adjacent to the esophagus, and fistulas between the esophagus and mediastinum (Figs. 1 and 2).2022 Results of contrast studies may be negative and warrant repeating within several hours.19

If CT scans cannot be performed, neck (soft‐tissue) and chest x‐rays may be useful. Although plain films have limited value in evaluating the retropharyngeal space, they can reveal soft‐tissue emphysema, a widened mediastinum, pulmonary infiltrates or effusions, neck abscess, and mediastinal air‐fluid levels. In cervical perforation, a lateral film of the neck can show air in deep cervical tissue before clinical signs are apparent.
Swallow studies with Gastrografin (meglumine diatrizoate) are useful in defining the exact location of the perforation (Fig. 3). However, the false‐negative rate of swallow studies can exceed 10%, especially if the patient is upright during the study. When the contrast propagates past the site of perforation too quickly, it may not extravasate.23 Although barium may provide slightly greater contrast, it may add to the problem of foreign body reaction in the area of perforation.18 An additional complication of barium is that once it has extravasated, it is not readily absorbed. The persistence of extravasated barium makes it difficult to assess the resolution of an esophageal tear on subsequent fluoroscopic or CT exams. Hence, our institution avoids using barium to evaluate esophageal perforation, unless Gastrografin swallow has excluded any major esophageal perforation. Barium swallow may then be used to exclude small mural tears. Some medical centers elect to routinely screen their high‐risk patients with swallow evaluations after an EGD, although this is not common practice.8, 24
If the above workup is negative, the use of EGD may be considered for establishing the diagnosis if a high index of suspicion remains. However, the risks of EGD in this situation include extension of the perforation, further extravasation of esophageal contents, and difficulty with subsequent radiographic studies to visualize the perforation.19
MANAGEMENT
Once the diagnosis of esophageal perforation has been established, treatment options are individualized based on the clinical scenario. Currently, there are no established guidelines, and large randomized clinical trials comparing outcomes of operative versus nonoperative management have not been conducted (Fig. 4).25, 26 Outcomes associated with esophageal perforations depend on preoperative clinical condition, comorbidities, location and size of the perforation, nature of underlying esophageal disease (if any), and time to establish the diagnosis and initiate therapy.10 Delay in patient presentation or diagnosis beyond 24 hours following esophageal perforation has been associated with adverse outcomes.18, 27, 28
A conservative approach is appropriate when clinically stable patients with minimal symptoms have well‐contained, nontransmural tears. Management entails broad‐spectrum antibiotics, nothing by mouth, nasogastric suction, and parenteral nutrition.24 Early surgical consultation is recommended in all cases. Serial CT scanning is useful for following the resolution of fistulas and tears. An oral diet can be resumed when contrast or swallow studies show no extravasation of dye. Cervical perforations typically fare well with this approach.26, 29
Surgical therapy is recommended for patients with large or uncontained esophageal perforations, mediastinal abscesses, and/or sepsis.25, 27 Surgical options include esophageal diversion, esophagectomy, or drainage with or without primary repair. Drainage with primary repair is considered the treatment of choice, regardless of time to presentation. Esophagectomy is considered in cases of delayed or neglected perforations, extensive transmural necrosis or underlying cancer.30 Operative mortality is 0%30% when treated within 24 hours. This rate increases to 26%64% when treatment is delayed beyond 24 hours, reaffirming the importance of making a prompt diagnosis.8
Endoscopic intervention is gaining recognition for its role in the management of esophageal perforations, especially when the risks make surgery prohibitive. Therapeutic options include stenting and clipping a perforation, as well as debriding and draining an abscess. Endoscopists can successfully treat traumatic nonmalignant esophageal perforations smaller than 50% to 70% of the circumference with self‐expanding plastic stents.26 Another option is to use metallic clipping devices to treat small esophageal perforations (1 cm).3133 Combined with medical management and appropriate patient selection, the benefits of an endoscopic approach may potentially outweigh the risks of surgery.26, 29, 33, 34
Regardless of treatment approach, the appropriate and timely selection of empiric antibiotic therapy improves outcomes. Empiric antimicrobial therapy for esophageal perforation will depend on several host factors as well as the site of perforation. In healthy nonhospitalized adults, ampicillin‐sulbactam, clindamycin, and penicillin G plus metronidazole are good choices because of their excellent activity against oral microflora. In patients who are critically ill, are hospitalized, are immunosuppressed, or have gastric acid suppression, initial broad‐spectrum antimicrobials such as piperacillin‐tazobactam, imipenem, meropenem, or a third‐generation cephalosporin plus metronidazole (or clindamycin) should be initiated. Additional therapy against methicillin‐resistant Staphylococcus aureus or Candida sp. should be considered if the patient is critically ill or is known to be colonized with these organisms. Initial empiric therapy should be modified as necessary based on culture results. Total duration of therapy will vary based on location and magnitude of the infection, adjunctive surgical debridement, and pathogens involved.
SUMMARY
Despite being an extremely safe procedure, EGD carries a known serious risk of esophageal perforation. Mortality after esophageal perforation can approach 25%. Although diagnostic endoscopy has a perforation rate of less than 0.03%, the risk can approach 17% with therapeutic interventions such as stent placement and esophageal dilation. Factors influencing the risks of perforation include procedural complexity, operator experience, and underlying esophageal and systemic diseases. Furthermore, perforations complicated by infection can lead to fatal mediastinitis and sepsis. The clinical triad of esophageal perforation is fever, neck pain, and crepitus. The optimal diagnostic study is CT scan of the neck and thorax with water‐soluble oral contrast. Treatment options range from conservative management with broad‐spectrum antibiotics to surgery. Diagnosis of esophageal perforation within 24 hours is essential for favorable outcomes.
Esophagogastroduodenoscopy (EGD) carries a small but serious risk of esophageal perforation.13 With its potential for sepsis and fatal mediastinitis, prompt recognition and treatment are essential for favorable outcomes. The risk of perforation with diagnostic flexible EGD is 0.03%, which is an improvement from the 0.1%0.4% risk associated with rigid endoscopy.4 However, the risk of perforation can dramatically increase to 17% depending on the methods of therapeutic intervention and underlying risk factors (Table 1).1, 57
| Level of operator experience |
| Underlying esophageal disease |
| Zenker's diverticulum |
| Eosinophilic esophagitis |
| Esophageal or mediastinal irradiation |
| Esophageal malignancy |
| Esophageal strictures |
| Systemic disease |
| Anterior cervical osteophytes |
| Advanced liver cirrhosis |
| Diabetes mellitus |
| Scleroderma |
| Complexity of intervention |
| Esophageal stent placement |
| Pneumatic dilation |
| Other |
| Heavy sedation |
| Advanced age |
It is estimated that 33%75% of all esophageal perforations are iatrogenic.8 Of those caused by EGD, therapeutic interventions portend an increased risk compared with the risk of diagnostic endoscopy alone (Table 2).4 With the expanding role of flexible EGD and the increasing number of procedures performed, this modest risk per procedure still translates into a sizable number of perforations with their ensuing complications.4, 7 Mortality rates following esophageal perforation may approach 25%.9
| Endoscopic procedure | Esophageal perforation risk |
|---|---|
| Diagnostic | 0.03% |
| Dilation | 0.25% (normal esophagus)4%7% (achalasia)*7% (gastric outlet obstruction)*17% (strictures due to caustic agent) |
| Thermal method (treatment of malignancy) | 10% |
| Endoprosthesis | 3% |
| Variceal sclerotherapy | 1%5% (acute perforation)2%5% (delayed perforation) |
| Band ligation | 0.7% (perforation) |
| Nonvariceal hemostasis (use of sclerosant or cautery) | 0%2% (first hemostasis)4% (hemostasis repeated within 2448 hours) |
ANATOMY AND PATHOPHYSIOLOGY
The most common site of perforation is at the level of the cricopharyngeus, as it is a narrow introitus leading to the esophagus. The risk of perforation at this location is further increased with the presence of a Zenker's diverticulum or cervical osteophytes. The second most common site is proximal to the lower esophageal sphincter because of the angulation of the hiatus and the high frequency of esophageal webs, rings, reflux strictures, and hiatal hernias. The relatively straight middle esophagus is an uncommon site for perforations.
Cervical perforations are less commonly caused by organic lesions of the esophagus. Often, they are the result of technique and manipulation of the endoscope, or of certain conditions associated with the jaw, neck, or spinal column that are unfavorable for endoscopy. The risk of cervical perforation increases with the presence of bony spurs, as the upper esophagus is compressed over the underlying spinal column. Thoracic perforations, however, are more commonly seen with organic esophageal obstruction. These obstructions may be caused by an underlying inflammatory process, benign stricture, or neoplasm. In these cases, the risk of thoracic perforation is increased with blind procedures. Thoracic perforations carry a worse prognosis if diagnosis is delayed, or if the underlying obstruction cannot be removed.10
Esophageal perforation leads to periesophageal tissues being contaminated by food, secretions, air, or gastric contents and may be followed by chemical tissue injury and infection. The nature and extent of infection depend on the site of esophageal perforation. Cervical esophageal perforation can cause retropharyngeal space infection, which has the potential to extend directly into the posterior mediastinum via the danger space, which is between the retropharyngeal and prevertebral spaces and extends from the base of the skull descending freely throughout the entire length of the posterior mediastinum. With thoracic perforations, esophageal contents can enter the pleural space by negative intrathoracic pressure with subsequent pleural contamination and empyema.8, 1113
Pathogens responsible for infections after esophageal perforation vary based on several factors including site of perforation, clinical status of patient when perforation occurs (hospitalized versus not hospitalized, critically ill versus healthy), receipt of enteral nutrition, gastric acid suppression with H2‐receptor antagonists or proton‐pump inhibitors, immunosuppression, and recent (or current) receipt of antimicrobials. In nonintubated, healthy adults not on antimicrobial therapy, organisms in the upper esophagus are essentially identical to those in the oropharynx and include viridans streptococci, Haemophilus species, and anaerobes. During critical illness and following antibiotic therapy, the normal oral flora is rapidly replaced by aerobic Gram‐negative bacilli, Staphylococcus aureus, and yeast.14 The stomach, which is normally devoid of bacteria, can likewise be colonized with pathogenic organisms in the setting of gastric acid suppression and enteral nutrition.15, 16
SIGNS AND SYMPTOMS
Esophageal perforation should be considered after EGD, dilation, sclerotherapy, variceal banding, and esophageal stenting. However, perforation can also result from other invasive procedures such as insertion of feeding and nasogastric tubes, rapid sequence intubation, and transesophageal echocardiography.
The clinical triad of esophageal perforation includes pain, fever, and subcutaneous air.17 In a study by Wychulis et al., among 33 patients with esophageal perforation, 75% demonstrated all 3 findings.10 Pain is the most sensitive finding and occurs in nearly all patients identified with esophageal perforation. Crepitation, which results from air dissecting along soft tissue planes of the mediastinum and into the neck, occurs in up to 70% with cervical perforation and 30% with thoracic perforation.8, 10, 18
Clinical presentation and outcomes vary depending on the location of the perforation (Table 3).8 Cervical perforation is usually associated with anterior neck pain, located at the anterior border of the sternocleidomastoid muscle. Movement of the neck and palpation typically aggravate the pain. Thoracic perforation typically presents as substernal chest pain, often with a component of pleurisy. Pleural effusions are present in 50% of thoracic perforations, and mediastinitis is more likely to occur.19 Hamman's sign, a finding characterized by an audible crunch with chest auscultation, is suggestive of mediastinal emphysema. Perforation of the intra‐abdominal esophagus can result in epigastric pain and signs of acute abdomen.10, 17 Subcutaneous emphysema occurs more frequently with cervical perforation but can be present regardless of location.10 Secondary infections following esophageal perforation can manifest with an accelerated clinical course leading to sepsis and shock.
| Location of perforation | Symptom | Sign* |
|---|---|---|
| ||
| Cervical esophagus | Muscle spasm Dysphonia Hoarseness Dysphagia | Anterior neck tendernessTenderness on cervical motionSubcutaneous emphysema |
| Thoracic esophagus | Substernal chest pain Dysphagia Odynophagia | Cyanosis, Dyspnea Hamman's sign Pleural effusion Subcutaneous emphysema |
| Intraabdominal esophagus | Epigastric pain | Acute abdomenSubcutaneous emphysema |
DIAGNOSIS
Clinical suspicion of esophageal perforation should prompt necessary radiographic studies to establish the diagnosis.18, 20 Contrast‐enhanced computed tomography (CT) scans of the neck and chest are preferable because of their increased sensitivity in localizing the site and showing the extent of perforation and abscess. CT scans may reveal subcutaneous or mediastinal air, abscess cavities adjacent to the esophagus, and fistulas between the esophagus and mediastinum (Figs. 1 and 2).2022 Results of contrast studies may be negative and warrant repeating within several hours.19

If CT scans cannot be performed, neck (soft‐tissue) and chest x‐rays may be useful. Although plain films have limited value in evaluating the retropharyngeal space, they can reveal soft‐tissue emphysema, a widened mediastinum, pulmonary infiltrates or effusions, neck abscess, and mediastinal air‐fluid levels. In cervical perforation, a lateral film of the neck can show air in deep cervical tissue before clinical signs are apparent.
Swallow studies with Gastrografin (meglumine diatrizoate) are useful in defining the exact location of the perforation (Fig. 3). However, the false‐negative rate of swallow studies can exceed 10%, especially if the patient is upright during the study. When the contrast propagates past the site of perforation too quickly, it may not extravasate.23 Although barium may provide slightly greater contrast, it may add to the problem of foreign body reaction in the area of perforation.18 An additional complication of barium is that once it has extravasated, it is not readily absorbed. The persistence of extravasated barium makes it difficult to assess the resolution of an esophageal tear on subsequent fluoroscopic or CT exams. Hence, our institution avoids using barium to evaluate esophageal perforation, unless Gastrografin swallow has excluded any major esophageal perforation. Barium swallow may then be used to exclude small mural tears. Some medical centers elect to routinely screen their high‐risk patients with swallow evaluations after an EGD, although this is not common practice.8, 24
If the above workup is negative, the use of EGD may be considered for establishing the diagnosis if a high index of suspicion remains. However, the risks of EGD in this situation include extension of the perforation, further extravasation of esophageal contents, and difficulty with subsequent radiographic studies to visualize the perforation.19
MANAGEMENT
Once the diagnosis of esophageal perforation has been established, treatment options are individualized based on the clinical scenario. Currently, there are no established guidelines, and large randomized clinical trials comparing outcomes of operative versus nonoperative management have not been conducted (Fig. 4).25, 26 Outcomes associated with esophageal perforations depend on preoperative clinical condition, comorbidities, location and size of the perforation, nature of underlying esophageal disease (if any), and time to establish the diagnosis and initiate therapy.10 Delay in patient presentation or diagnosis beyond 24 hours following esophageal perforation has been associated with adverse outcomes.18, 27, 28
A conservative approach is appropriate when clinically stable patients with minimal symptoms have well‐contained, nontransmural tears. Management entails broad‐spectrum antibiotics, nothing by mouth, nasogastric suction, and parenteral nutrition.24 Early surgical consultation is recommended in all cases. Serial CT scanning is useful for following the resolution of fistulas and tears. An oral diet can be resumed when contrast or swallow studies show no extravasation of dye. Cervical perforations typically fare well with this approach.26, 29
Surgical therapy is recommended for patients with large or uncontained esophageal perforations, mediastinal abscesses, and/or sepsis.25, 27 Surgical options include esophageal diversion, esophagectomy, or drainage with or without primary repair. Drainage with primary repair is considered the treatment of choice, regardless of time to presentation. Esophagectomy is considered in cases of delayed or neglected perforations, extensive transmural necrosis or underlying cancer.30 Operative mortality is 0%30% when treated within 24 hours. This rate increases to 26%64% when treatment is delayed beyond 24 hours, reaffirming the importance of making a prompt diagnosis.8
Endoscopic intervention is gaining recognition for its role in the management of esophageal perforations, especially when the risks make surgery prohibitive. Therapeutic options include stenting and clipping a perforation, as well as debriding and draining an abscess. Endoscopists can successfully treat traumatic nonmalignant esophageal perforations smaller than 50% to 70% of the circumference with self‐expanding plastic stents.26 Another option is to use metallic clipping devices to treat small esophageal perforations (1 cm).3133 Combined with medical management and appropriate patient selection, the benefits of an endoscopic approach may potentially outweigh the risks of surgery.26, 29, 33, 34
Regardless of treatment approach, the appropriate and timely selection of empiric antibiotic therapy improves outcomes. Empiric antimicrobial therapy for esophageal perforation will depend on several host factors as well as the site of perforation. In healthy nonhospitalized adults, ampicillin‐sulbactam, clindamycin, and penicillin G plus metronidazole are good choices because of their excellent activity against oral microflora. In patients who are critically ill, are hospitalized, are immunosuppressed, or have gastric acid suppression, initial broad‐spectrum antimicrobials such as piperacillin‐tazobactam, imipenem, meropenem, or a third‐generation cephalosporin plus metronidazole (or clindamycin) should be initiated. Additional therapy against methicillin‐resistant Staphylococcus aureus or Candida sp. should be considered if the patient is critically ill or is known to be colonized with these organisms. Initial empiric therapy should be modified as necessary based on culture results. Total duration of therapy will vary based on location and magnitude of the infection, adjunctive surgical debridement, and pathogens involved.
SUMMARY
Despite being an extremely safe procedure, EGD carries a known serious risk of esophageal perforation. Mortality after esophageal perforation can approach 25%. Although diagnostic endoscopy has a perforation rate of less than 0.03%, the risk can approach 17% with therapeutic interventions such as stent placement and esophageal dilation. Factors influencing the risks of perforation include procedural complexity, operator experience, and underlying esophageal and systemic diseases. Furthermore, perforations complicated by infection can lead to fatal mediastinitis and sepsis. The clinical triad of esophageal perforation is fever, neck pain, and crepitus. The optimal diagnostic study is CT scan of the neck and thorax with water‐soluble oral contrast. Treatment options range from conservative management with broad‐spectrum antibiotics to surgery. Diagnosis of esophageal perforation within 24 hours is essential for favorable outcomes.
- .Complications of endoscopic gastrointestinal dilation techniques.Gastrointest Endosc Clin N Am.1996;6:323–341.
- .Complications of upper gastrointestinal endoscopy.Gastrointest Endosc Clin N Am.1996;6:287–303.
- ,.Complications of upper gastrointestinal endoscopy and their management.Gastrointest Endosc Clin N Am.1994;4:551–570.
- ,,,,.Treatment of endoscopic esophageal perforation.Surg Endosc.1999;13:962–966.
- ,,,.Unsedated small‐caliber esophagogastroduodenoscopy (EGD) versus conventional EGD: a comparative study [see comment].Gastroenterology.1999;117:1301–1307.
- ,,,,.Complications associated with esophagogastroduodenoscopy and with esophageal dilation.Gastrointest Endosc.1976;23(1):16–19.
- ,,.Comparison among the perforation rates of Maloney, balloon, and savary dilation of esophageal strictures.Gastrointest Endosc.2000;51(4 Pt 1):460–462.
- ,.Esophageal emergencies: things that will wake you from a sound sleep.Gastroenterol Clin N Am.2003;32:1035–1052.
- ,,, et al.Complications of upper GI endoscopy.Gastrointest Endosc.2002;55:784–793.
- ,,.Instrumental perforations of the esophagus.Dis Chest.1969;55(3):184–189.
- ,Complications of esophageal dilation and guidelines for their prevention.Gastrointest Endosc.1981;27:229–234.
- .Infectious complications associated with gastrointestinal endoscopy.Gastrointest Endosc Clin N Am.2000;10:215–232.
- ,,,The occurrence of bacteremia after esophageal dilation.Gastrointestinal Endoscopy1975;22(2):86–87.
- ,,,,,.The pathogenesis of ventilator‐associated pneumonia: its relevance to developing effective strategies for prevention.Respir Care.2005;50:725–739; discussion39–41.
- ,,, et al.Stomach as a source of colonization of the respiratory tract during mechanical ventilation: association with ventilator‐associated pneumonia.Eur Respir J.1996;9:1729–1735.
- ,,, et al.Gastric microbiota in elderly patients fed via nasogastric tubes for prolonged periods.J Hosp Infect.2006;63(1):79–83.
- ,.Retroesophageal abscess twenty‐five days after esophagoscopy. An unusual complication of endoscopy.Gastrointest Endosc.1972;18:167–168.
- ,,.The radiologist in prevention and diagnosis of instrumental perforation of the esophagus.South Med J.1974;67:830–836.
- ,,.Short‐ and long‐term outcome of esophageal perforation.Gastrointest Endosc.1995;41(2):130–134.
- ,,,.The diagnosis and treatment of esophageal perforations resulting from nonmalignant causes.Surg Today.1997;27:793–800.
- ,.Radiology of the retropharyngeal space.Clin Radiol.2000;55:740–748.
- ,,.Diagnosis and management decisions in infections of the deep fascial spaces of the head and neck utilizing computerized tomography.Laryngoscope.1982;92(6, Pt. 1):630–633.
- .Perforation of the esophagus.Ann Thorac Surg.1986;42:231–232.
- ,,, et al.Successfully treated case of cervical abscess and mediastinitis due to esophageal perforation after gastrointestinal endoscopy.Dis Esophagus.2002;15:250–252.
- ,.The spectrum of spontaneous and iatrogenic esophageal injury: perforations, Mallory‐Weiss tears, and hematomas.J Clin Gastroenterol.1999;29:306–317.
- .Treatment of esophageal perforations and anastomotic leaks: the endoscopist is stepping into the arena.Gastrointest Endosc.2005;61:897–900.
- ,,.Operative and nonoperative management of esophageal perforations.Ann Surg.1981;194(1):57–63.
- ,,.Current results of therapy for esophageal perforation.Am J Surg.1995;169:615–617.
- ,,.Successful endoscopic management of a cervical pharyngeal perforation and mediastinal abscess.Gastrointest Endosc.2005;61(1):158–160.
- ,,,,.Thoracic esophageal perforations: a decade of experience.[see comment].Ann Thorac Surg.2003;75:1071–1074.
- ,.Perforation: part and parcel of endoscopic resection? [comment].Gastrointest Endosc.2006;63:602–605.
- ,,,.Endoscopic clip application as an adjunct to closure of mature esophageal perforation with fistulae.Clin Gastroenterol Hepatol.2003;1(1):44–50.
- ,,.Endoscopic clipping of esophageal perforation after pneumatic dilation for achalasia.Endoscopy.1995;27:608–611.
- ,,, et al.Esophageal dilation.Gastrointest Endosc.2006;63:755–760.
- .Complications of endoscopic gastrointestinal dilation techniques.Gastrointest Endosc Clin N Am.1996;6:323–341.
- .Complications of upper gastrointestinal endoscopy.Gastrointest Endosc Clin N Am.1996;6:287–303.
- ,.Complications of upper gastrointestinal endoscopy and their management.Gastrointest Endosc Clin N Am.1994;4:551–570.
- ,,,,.Treatment of endoscopic esophageal perforation.Surg Endosc.1999;13:962–966.
- ,,,.Unsedated small‐caliber esophagogastroduodenoscopy (EGD) versus conventional EGD: a comparative study [see comment].Gastroenterology.1999;117:1301–1307.
- ,,,,.Complications associated with esophagogastroduodenoscopy and with esophageal dilation.Gastrointest Endosc.1976;23(1):16–19.
- ,,.Comparison among the perforation rates of Maloney, balloon, and savary dilation of esophageal strictures.Gastrointest Endosc.2000;51(4 Pt 1):460–462.
- ,.Esophageal emergencies: things that will wake you from a sound sleep.Gastroenterol Clin N Am.2003;32:1035–1052.
- ,,, et al.Complications of upper GI endoscopy.Gastrointest Endosc.2002;55:784–793.
- ,,.Instrumental perforations of the esophagus.Dis Chest.1969;55(3):184–189.
- ,Complications of esophageal dilation and guidelines for their prevention.Gastrointest Endosc.1981;27:229–234.
- .Infectious complications associated with gastrointestinal endoscopy.Gastrointest Endosc Clin N Am.2000;10:215–232.
- ,,,The occurrence of bacteremia after esophageal dilation.Gastrointestinal Endoscopy1975;22(2):86–87.
- ,,,,,.The pathogenesis of ventilator‐associated pneumonia: its relevance to developing effective strategies for prevention.Respir Care.2005;50:725–739; discussion39–41.
- ,,, et al.Stomach as a source of colonization of the respiratory tract during mechanical ventilation: association with ventilator‐associated pneumonia.Eur Respir J.1996;9:1729–1735.
- ,,, et al.Gastric microbiota in elderly patients fed via nasogastric tubes for prolonged periods.J Hosp Infect.2006;63(1):79–83.
- ,.Retroesophageal abscess twenty‐five days after esophagoscopy. An unusual complication of endoscopy.Gastrointest Endosc.1972;18:167–168.
- ,,.The radiologist in prevention and diagnosis of instrumental perforation of the esophagus.South Med J.1974;67:830–836.
- ,,.Short‐ and long‐term outcome of esophageal perforation.Gastrointest Endosc.1995;41(2):130–134.
- ,,,.The diagnosis and treatment of esophageal perforations resulting from nonmalignant causes.Surg Today.1997;27:793–800.
- ,.Radiology of the retropharyngeal space.Clin Radiol.2000;55:740–748.
- ,,.Diagnosis and management decisions in infections of the deep fascial spaces of the head and neck utilizing computerized tomography.Laryngoscope.1982;92(6, Pt. 1):630–633.
- .Perforation of the esophagus.Ann Thorac Surg.1986;42:231–232.
- ,,, et al.Successfully treated case of cervical abscess and mediastinitis due to esophageal perforation after gastrointestinal endoscopy.Dis Esophagus.2002;15:250–252.
- ,.The spectrum of spontaneous and iatrogenic esophageal injury: perforations, Mallory‐Weiss tears, and hematomas.J Clin Gastroenterol.1999;29:306–317.
- .Treatment of esophageal perforations and anastomotic leaks: the endoscopist is stepping into the arena.Gastrointest Endosc.2005;61:897–900.
- ,,.Operative and nonoperative management of esophageal perforations.Ann Surg.1981;194(1):57–63.
- ,,.Current results of therapy for esophageal perforation.Am J Surg.1995;169:615–617.
- ,,.Successful endoscopic management of a cervical pharyngeal perforation and mediastinal abscess.Gastrointest Endosc.2005;61(1):158–160.
- ,,,,.Thoracic esophageal perforations: a decade of experience.[see comment].Ann Thorac Surg.2003;75:1071–1074.
- ,.Perforation: part and parcel of endoscopic resection? [comment].Gastrointest Endosc.2006;63:602–605.
- ,,,.Endoscopic clip application as an adjunct to closure of mature esophageal perforation with fistulae.Clin Gastroenterol Hepatol.2003;1(1):44–50.
- ,,.Endoscopic clipping of esophageal perforation after pneumatic dilation for achalasia.Endoscopy.1995;27:608–611.
- ,,, et al.Esophageal dilation.Gastrointest Endosc.2006;63:755–760.