User login
Are Ayurvedic herbs for diabetes effective?
- Limited randomized control trial data and observational studies show that the herbs Coccinia indica, holy basil, fenugreek, Gymnema sylvestre, and the herbal formulas Ayush-82 and D-400 have glucose-lowering effects. But these herbs are not as well studied as others more familiar to Western medicine. (B)
- Inform patients who ask about Ayurveda that traditional practitioners rely on the interaction of several components, of which herbs are just one, and that no formal studies have looked at Ayurveda as a whole system. (B)
- Objective: To evaluate and synthesize the evidence on the effect of Ayurvedic therapies for diabetes mellitus.
- Design: Systematic review of trials.
- Measurements and main results: We found no study that assessed Ayurvedic as a system of care. Botanical therapy was by far the most commonly studied Ayurvedic treatment. Herbs were studied either singly or as formulas. In all, 993 titles in Western computerized databases and 318 titles identified by hand-searching journals in India were examined, yielding 54 articles reporting the results of 62 studies. The most-studied herbs were G sylvestre, C indica, fenugreek, and Eugenia jambolana. A number of herbal formulas were tested, but Ayush-82 and D-400 were most often studied. Thirty-five of the studies included came from the Western literature, 27 from the Indian. Seven were randomized controlled trials (RCTs) and 10 controlled clinical trials (CCTs) or natural experiments. Twenty-two studies went on to further analysis based on a set of criteria. Of these, 10 were RCTs, CCTs, or natural experiments, 12 were case series or cohort studies. There is evidence to suggest that the herbs C indica, holy basil, fenugreek, and G sylvestre, and the herbal formulas Ayush-82 and D-400 have a glucose-lowering effect and deserve further study. Evidence of effectiveness of several other herbs is less extensive (C tamala, E jambolana, and Momordica charantia).
- Conclusions: There is heterogeneity in the available literature on Ayurvedic treatment for diabetes. Most studies test herbal therapy. Heterogeneity exists in the herbs and formulas tested (more than 44 different interventions identified) and in the method of their preparation. Despite these limitations, there are sufficient data for several herbs or herbal formulas to warrant further studies.
Given the US population’s increasing interest in herbal and alternative therapies, it is just a matter of time before you will be fielding questions from patients about Ayurveda—a comprehensive system of health care that originated in India roughly 3000 years ago, emphasizing the relationships among body, mind, and spirit. Diabetes has been a particular focus of this medical system, and a few Ayurvedic herbs do indeed appear to exert glucose lowering mechanisms.
But how strong is the evidence? Though Ayurveda involves the interaction of many kinds of therapy, this review examines only the literature pertaining to herbal remedies your patients with diabetes are likely to ask about.
Ayurveda more than herbs
Ayurveda (Sanskrit for “knowledge of life” or “knowledge of longevity”) has now spread beyond India’s borders to include the rest of the Indian subcontinent, Sri Lanka, Malaysia, Mauritius, South Africa, Japan, Russia, Europe, and North America. At its root, Ayurveda seeks to restore an individual’s innate harmony. Primary Ayurvedic treatments include diet, exercise, meditation, herbs, massage, exposure to sunlight, controlled breathing, and detoxification treatments.
Dosha imbalance. Ayurveda considers human beings a microcosm of nature. All living and nonliving things are believed to consist of 5 basic elements: ether (space), air, fire, water, and earth. In humans these elements combine and manifest in the human body as 3 humors, or doshas, known as vata, pitta, and kapha.
The doshas govern all biological, psychological, and pathophysiological functions. They are fundamental to human health, and an imbalance of the doshas brings on illness. Consequently, Ayurveda seeks to bring the doshas back into harmony. Balanced doshas, as well as good-quality tissues (dhatus), proper digestion, and elimination of excretions (malas), are considered essential in Ayurveda for maintaining health.
Dosha body type influences treatment. In addition, humans are endowed at birth with 1 of 7 body types, depending on which dosha or combination of the 3 basic doshas dominates. Body types can be dominated by a single humor (vata, pitta, or kapha), or they can be dominated by combinations: vata-kapha (when vata and kapha are present in almost equal amounts); vata-pitta; pitta-kapha; or vata-pitta-kapha. A person’s dosha body type is expressed physically and emotionally; for example, a person with a vata-dominant body type will have a thin frame and an insecure temperament. The Ayurvedic physician takes body type and imbalances among the doshas into consideration when treating a patient.
Application to diabetes. The Indian word for diabetes is madhumeha, from madhu, meaning “sweet/sweetness,” and meha, meaning excessive urination. Classical Ayurvedic therapy for madhumeha (diabetes) begins with an assessment of the dosha imbalance. In all types of pramehas (urinary disorders), kapha is vitiated, but in madhumeha, vata is often aggravated as well. Therefore, therapies will be directed at both vata and kapha simultaneously to restore the balance of the doshas.1,2
Herbs are a commonly used treatment in Ayurveda. Ethnobotanical studies of traditional herbal remedies used for diabetes around the world have identified more than 1200 species of plants with hypoglycemic activity. These plants are broadly distributed throughout 725 different genera. The pharmacopoeia of India is especially rich in herbal treatments for diabetes. Eighty-five percent of the 20 antidiabetes plants most widely used around the world are prescribed in India.3 A few of the herbs commonly used by Ayurveda practitioners to treat diabetes are summarized in the TABLE.
In response to the increasing interest in Ayurveda and herbal treatments for diabetes in this country, the National Center for Complimentary and Alternative Medicine (NCCAM) requested we conduct a systematic review of Ayurvedic therapy for diabetes. This paper reports the results of that review, and is a condensation of an evidence report available at www.ahrq.gov/clinic/epcsums/ayurvsum.htm.
TABLE
Ayurvedic characteristics of herbs commonly used to treat diabetes
| HERB | TASTE (RASA) | INCREASES (AGGRAVATES) | DECREASES (PACIFIES) |
|---|---|---|---|
| Gymnema | Kasaya (astringent) | Kapha, Pitta | |
| Momordica | Tikta (bitter) | Kapha, Pitta | |
| Trigonella (fenugreek) | Tikta (bitter); Madhura (sweet) | Pitta | Kapha, Vata |
| Coccinia indica | Kasaya (astringent); Tikta (bitter) | Vata, Pitta | |
| Pterocarpus | Kasaya (astringent) | Vata | |
| Source: Kapoor, 1990;32 Dash, 198733 Mishra, Singh, and Dagenais, 2001.34 | |||
Methods
Identification of literature
We used the search term “Ayurveda” plus the names of 16 major botanicals characteristically used in Ayurveda for an initial search of the Western literature. The herbal terms were added to the search to increase its sensitivity, making it possible to find studies that used Ayurvedic herbal therapy without necessarily being directly identified as Ayurvedic studies.
We were concerned that a large body of literature existed in India that could not be obtained through the conventional search strategy outlined above. Hence, we decided to conduct a search for Ayurvedic literature from the Indian subcontinent. A physician member of the research team, fluent in English and Hindi and who had trained in India, went to India to identify Ayurvedic literature available there.
We therefore used several sources for our search:
- An initial “waterfront” search, which already had identified 120 articles on diabetes and Ayurveda (which was used by NCCAM to establish the rationale for selecting diabetes as the focus of this review).4 This search is detailed in our Evidence Report (available at www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat1.chapter.95372) and included Medline, HealthSTAR, Allied and Complementary Medicine, MANTIS, CAB HEALTH, BIOSIS Previews, and EMBASE.
- The in-person literature search in India—we obtained 16 volumes of abstracts from various Indian Ayurvedic journals, as compiled by the Central Council for Research in Ayurveda and Siddha (CCRAS) library. This yielded 318 titles.
- An additional online search of the previously mentioned databases for common botanicals used in the treatment of diabetes. This search yielded 773 additional articles.
- A search of the online CINAHL database, which yielded 70 articles.
- The reference lists of important articles in the Ayurveda/diabetes literature. We identified review articles of herbal treatment of diabetes and checked to see if they focused on any of the Ayurvedic herbal therapies we had identified for diabetes. Checking the bibliographies of all the articles we identified from any source, we found an additional 30 titles that were potentially relevant to our search.
- An RCT or a CCT or a natural experiment with a comparison arm that did not receive an herb or Ayurvedic therapy. RCTs of any size were included. For CCTs or natural experiments, the study had to have at least 1 treatment arm that contained at least 10 patients.
- Because of a paucity of studies meeting these design criteria, we also assessed cohort or case series data that used a “pre/post” method of analysis, if their sample included at least 10 subjects.
- The study had to test Ayurveda as a method or herbs used as a single agent, a formula acting as a single agent, or a limited combination of products (no more than 3) acting as a single agent. The agent had to be dispensed more than 1 time to the study patients (in other words, no single-dose studies).
- The study had to report on at least 1 of 3 outcome measures at 30 days minimum following the start of the study: glycosylated hemoglobin (Hb A1c), fasting blood glucose, or postprandial blood glucose at either 2 hours (preferred) or 1 hour (acceptable).
Data extraction
Detailed information from each study was extracted using a specialized form. The physician reviewers, working independently, extracted data in duplicate and resolved disagreements by consensus. A senior physician resolved any remaining disagreements. Information extracted from articles included the diagnostic criteria used to make the diagnosis (Ayurvedic or Western or both); the location in which the study was done; the subject population (age, gender, other demographics); the sample size in each arm of the study; the interventions used (primarily the names of the individual herbs or mineral and the manner of their preparation); the length of the study; and the outcomes. To evaluate the quality of the design and execution of trials, we collected information on the study design, appropriateness of randomization, blinding, description of withdrawals and dropouts, and concealment of allocation.5,6 A quality score was calculated for each trial using a system developed by Jadad.5 Empirical evidence has shown that studies scoring 2 or less on the Jadad scale report exaggerated results compared with studies scoring 3 or more.7 While other elements of the design and execution of controlled trials have been proposed as quality measures, empirical evidence supporting their use as generic quality measures is lacking.8
Data synthesis
The studies we reviewed were judged clinically to be too heterogeneous to support a quantitative synthesis; therefore, our review is narrative. However, to promote the comparison of results across studies we extracted outcome data in a common format and present it in graphs for visual comparison. For studies that reported on both 1-hour and 2-hour postprandial blood glucose levels, we chose the 2-hour measurement for the analysis. For studies that reported more than 1 follow-up time, we selected the follow-up time that was closest to 3 months.
Twenty-two studies were selected for further analysis based on the criteria described above. These studies represented either RCTs (2) or CCTs/natural experiments (5) with a comparison arm that did not receive an herb, or studies that had pre/post comparison data available (8).
We considered 2 subgroups of eligible studies separately: the RCTs and CCTs or natural experiments that had nonherbal/Ayurvedic comparison arm(s) were considered 1 subgroup, and all other eligible (pre/post data available) studies made up the second subgroup. The RCT/CCT/natural experiments subgroup allowed us to do a comparison between herbal and nonherbal arms within a study, providing a stronger level of evidence than pre/post comparisons. For these studies, we were able to compare the effects of different treatments after the placebo or nonherbal arm results were taken into account by estimating a difference of differences statistic and its 95% confidence interval. This statistic is equal to the difference between the pre- and post-treatment means in the Ayurvedic arm minus the analogous difference in the nonherbal/Ayurvedic arm. The pre/post studies subgroup did not allow a concurrent comparison, but the difference between pre- and post-treatment means could be estimated along with a 95% confidence interval.4 Further details are given in our Evidence Report (available online at www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat1.chapter.95372).
For each study subgroup, we assessed the possibility of publication bias graphically by evaluating a funnel plot of the study summary statistics for asymmetry, which would result from the nonpublication of small trials with negative outcomes. Because graphical evaluation can be subjective, we also conducted an adjusted rank-correlation test9 and a regression asymmetry test10 as formal statistical tests for publication bias.
Results
Description of the evidence
As a result of our search, we considered a total of 1311 articles (FIGURE 1). We reviewed in depth 62 studies, of which 22 were analyzed statistically. Ten studies came from the Western literature, and 12 came from the Indian literature. There were 7 randomized controlled trials, controlled clinical trials, or natural experiments with a treatment/no treatment comparison. There were 15 case series or cohort studies using a “pre/post” analysis. TABLE W2 (available online at www.jfponline.com) summarizes the characteristics of studies.
In terms of interventions, there was no study that tested Ayurveda as a system of care; all tested herbs. Of the 22 studies described narratively in this article, the 2 most commonly tested single herbs were Coccinia indica and fenugreek. The Ayurvedic formula Ayush-82 was the most commonly tested herbal formula. Diet was used as an intervention or co-intervention in 15 of the 22 studies.
FIGURE 1
Ayurveda literature review strategy of focused search for human diabetes articles
Quality of the evidence
Only the RCTs, CCTs, and natural experiments were given a Jadad score, which rates studies on a 0 to 5 scale.5 Of the 7 such studies, 3 received a Jadad score of zero, 3 studies scored a 1, and only 1 study received a 4 on this scale. This is the only high quality study in our analysis.
Controlled trials/natural experiments with nonherbal comparison arm(s)
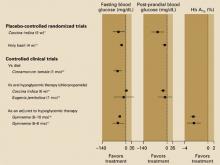
There were 7 RCTs, CCTs or natural experiments that met the inclusion criteria. The data for these 7 studies are reported in FIGURE 2.
Coccinia indica. Azad Khan, Akhtar, and Mahtab (1979) performed a randomized controlled trial to assess the hypoglycemic properties of a preparation of the herb C indica on uncontrolled and untreated type 2 diabetes patients.11 Thirty-eight patients with type 2 diabetes who were attending the outpatient department of the Bangladesh Institute of Research and Rehabilitation in Diabetes in Dhaka, Bangladesh, were recruited for the study. Only uncontrolled or newly diagnosed patients were enlisted. The intervention consisted of a freeze-dried powder of crushed leaves of C indica, given in a dose of 900 mg twice a day for 6 weeks. Control patients received placebo twice a day for the same period. Of the 16 patients receiving C indica, 10 patients showed a marked improvement in the glucose tolerance tests to values closer to normal, while none in the placebo arm showed marked improvement. The Jadad score for the trial was 4. This study was identified from the Eastern literature search.
Holy basil. Agrawal, Rai, and Singh (1996) reported the results of a randomized, placebo controlled crossover trial of the effects of a leaf extract of holy basil (Ocimum sanctum) on patients with type 2 diabetes.12 Forty patients were recruited from community advertisements in Kanpur, India, and through visits to the offices of local dieticians. All subjects had a 5-day run-in period during which they all consumed a tea made from holy basil leaves. This was followed by an 8-week experimental period. The patients were randomly assigned to drink the holy basil leaf tea for 4 weeks followed by placebo leaves for 4 weeks, or the reverse (the placebo leaves first, followed by the holy basil leaf tea). The authors concluded that holy basil leaf powder caused significant reduction in the level of fasting blood sugar and postprandial blood sugar, and a moderate reduction in cholesterol. The Jadad score for this trial is 1. This study was identified from the Western literature search.
Cinnamonum tamala. Chandola, Tripathi, and Udupa (1980) assessed the hypoglycemic effects of C tamala in type 2 diabetes patients.13 Thirty-two patients were recruited from the outpatient departments of the Institute of Medical Sciences, Varanasi, India, and received the intervention and 8 patients with type 2 diabetes served as controls. The socioeconomic characteristics of the patients were not noted, and the authors did not report if the 2 arms of patients were statistically equivalent on important prognostic variables at the start of the trial. The intervention consisted of leaves of C tamala (tejpatra) that were dried, pulverized, and filtered through a fine mesh, and given as 2 heaped teaspoons 4 times a day before meals and tea for a total of 1 month. All patients were advised to follow a 1800-calorie diet with restriction of sugar, potato, and rice. The control patients were only instructed to follow the above diet with no other medications. Fasting blood sugars were assessed in both arms of patients before the trial and at the end of 1 month. The authors reported the mean fasting blood sugar improved from 153 mg/dL to 113 mg/dL (P<.001) at the end of 1 month in patients treated with C tamala, while there was no improvement in control patients. The Jadad score for this study was 0. This study was identified from the Eastern literature search.
Coccina indica. Kamble, Jyotishi, Kamalakar, et al (1996) studied the effect of fresh leaves of C indica on blood sugar levels and on hyperlipidemia in noninsulin-dependent diabetes mellitus (NIDDM, type 2) patients at an Ayurvedic clinic in Nagpur, India.14 Patients were classified into 4 arms: a healthy comparison arm (arm I, 15 patients); a NIDDM comparison arm (arm II, 30 patients); NIDDM patients treated with Coccinia (arm III, 25 patients); and a NIDDM arm treated with chlorpropamide (arm IV, 15 patients). Patients were given the Coccinia (decocted from fresh leaves, dried into a paste, and made into a 3-g tablet) twice a day for 12 weeks, although control group data only exist at 6 weeks. For patients in arm III, the study showed a statistically significant reduction in mean fasting blood sugar, from 160 to 118 mg/dL (P<.001) at 12 weeks, and a significant decrease in blood sugar levels after glucose tolerance tests: the 2-hour level dropped from 308 mg/dL to 142 mg/dL (P<.001). These results were roughly equivalent to those found in the chlorpropamide arm at 6 weeks, with any differences being not statistically significant. Additionally, after 12 weeks of treatment, the Coccinia treated patients showed significant within group reductions in levels of cholesterol (P<.001), phospholipid (P<.05), triglyceride (P<.001), and free fatty acid (P<.001) compared with untreated patients with diabetes. The Jadad score for this study was 0. This study was identified from the Eastern literature search.
Jamun beej. Kohli and Singh (1993) studied the effects of Jamun beej (Eugenia jambolana) on fasting blood sugar, glucose tolerance test, and symptomatic relief of symptoms associated with diabetes.15 Thirty patients identified from the outpatient unit of the Sunderlal Hospital in Varanasi, India, who had NIDDM confirmed by glucose tolerance test, were given E jambolana crushed into a fine powder at a dose of 4 g 3 times a day for 3 months. No dietary restrictions were included in the study. A second arm of 6 patients with confirmed NIDDM was given chlorpropamide (250 mg/d). No demographic information was provided on these patients. The authors reported a statistically significant reduction in mean fasting blood sugar of 51.86 mg/dL at 2 months (P<.001) but not at 3 months. The study also demonstrated a significant reduction in the response to the glucose tolerance test at both 2 months (P<.001) and at 3 months (P<.01), but comparisons with the patients receiving chlorpropamide were not statistically significant. The Jadad score total is 1. This study was identified from the Eastern literature search.
Gymnema sylvestre. Baskaran, Ahamath, Shanmugasundaram, et al (1990) studied the effects of GS4, a specific isolate of G sylvestre, on the blood sugar of 47 type 2 diabetes patients.16 The intervention group consisted of 22 patients with diabetes on oral hypoglycemic therapy (continued during the trial), plus herbal therapy with Gymnema at a dose of 400 mg/d. The control group consisted of 25 patients with type 2 diabetes on conventional medications alone. Although the arms were reasonably matched for age and Broca index (percent of ideal body weight) based on our analysis of individual patient data in the study, the 2 arms were statistically different at baseline with respect to fasting blood sugar. The authors reported that in the intervention group at 12 months of follow-up, mean fasting blood sugar improved from 174 mg/dL to 124 mg/dL (P<.001) and Hb A1c improved from 11.9% to 8.48% (P<.001). Changes in the control group over this time were not significant. Virtually all patients in arm I developed hypoglycemic symptoms, and the dose of their normal oral hypoglycemic agent needed to be changed or stopped. The Jadad score is 0. This study was identified from the Western literature search.
GS4. Shanmugasundaram, Rajeswari, Baskaran, et al (1990b) reported the effect of an herbal compound GS4 on blood glucose, insulin requirements, and cholesterol in patients with type 1 and type 2 diabetes.17 The intervention group consisted of 23 type 1 patients and 4 type 2 patients (ages 44–50 years, 25% female) who continued their insulin in addition to taking the herbal intervention, and the control group consisted of 37 type 1 patients who were on insulin therapy. The clinical equivalence of the 2 arms at baseline was not mentioned. The intervention drug was GS4, a recrystallized precipitate of the alcoholic extract of the acidic fraction of G sylvestre; at dose of 400 mg/d. At 6 to 8 months of follow-up, all patients in the intervention group developed hypoglycemic episodes, and their insulin doses were reduced by 10 units at a time; differences compared to controls were statistically significant. The Jadad score was 1. This study was identified from the Western literature search.
Summary. In summary, comparisons of the studied herbs with either placebo, diet, or as an adjunct to medical hypoglycemic therapy consistently reported statistically significant benefits in glucose control. Studies comparing herbs to the oral hypoglycemic chlorpropamide did not report differences between groups.
FIGURE 2
Glucose-lowering effects of Ayurvedic herbs compared with nonherbal treatments
Case series or cohort studies without a concurrent comparison group
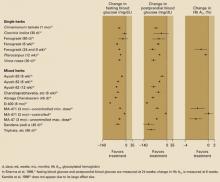
Fifteen studies had treatment arms that reported blood glucose or Hb A1c values before and after herbal interventions—ie, that made available pre/post data.13,18-31 Herbs were tested singly (7 studies), in combination (7 studies), or both singly and in combination (1 study). All of these studies are limited by the lack of randomization. Many are also limited by small sample size and short study duration.
The data are presented in FIGURE 3 in the following order: studies or arms of studies using a single herbal preparation first, followed by studies that use a formula or a group of herbs and minerals. Some studies with multiple arms will have listings in more than one place. As FIGURE 3 shows, most pre/post comparison studies using single herbs and formulas favor treatment. Hb A1c is measured in only 5 of the studies. Two of those studies seem to strongly favor treatment; 2 are almost equivocal; and 1 does not favor treatment.
The small number of RCTs/CCTs/natural experiments measuring postprandial blood glucose and Hb A1c, and the small number of case series and cohorts measuring Hb A1c, make the assessment of publication bias for these outcomes problematic. For the remaining outcomes, only slight evidence of publication bias was evident among the case series and cohort studies for the fasting blood glucose outcome (adjusted rank correlation test P=.97; regression asymmetry test P=.06). For this outcome, we have trial data available, a setting in which no evidence of publication bias is seen.
FIGURE 3
Effect of Ayurvedic herbs on blood glucose and Hb A1c
Discussion
No controlled trials have assessed Ayurveda as a system of care. Furthermore, among studies of herbal preparations, controlled trials are rare and mostly of poor quality. Still, we found evidence suggesting that some Ayurvedic herbs have clinically important hypoglycemic effects.
The best-quality RCT reported beneficial results for C indica. Other studies have generally reported benefits of C indica; however, results have been inconsistent.
A single trial of holy basil reported a benefit in controlling fasting blood glucose only. G sylvestre was used in a number of studies, again with generally beneficial results. Gymnema was also a constituent in 2 of the formulas that reported beneficial results: D-400 and Ayush-82.
Methodological shortcomings. The evidence we found falls short of proof. As noted, the individual studies we assessed had significant methodological shortcomings. Few used a randomized, placebo-controlled design, despite the feasibility of such methods. Studies generally were underpowered to determine even large effect sizes. Many studies involved an extremely small number of subjects (fewer than 10). A number of studies failed to use appropriate statistical methods in reporting the results. Furthermore, the duration of most studies was short, and only intermediate outcomes (measure of blood sugar control) were reported. Longer term studies that assess clinical outcomes are required. Lastly, there is great heterogeneity in the available literature on Ayurvedic treatment for diabetes, despite the fact that the overwhelming majority of studies test herbal therapy. Heterogeneity exists in the herbs and formulas tested and in the method of their preparation.
No true studies of Ayurveda. None of the identified studies assessed Ayurveda as a system of diagnosis and care. The literature reported mainly studies of single herbs; however, in clinical Ayurvedic practice, herbs are usually given in combination. Formulas can include minerals and metals in addition to multiple plants.
Ayurvedic practitioners assert that the sum of a formula is more potent than the constituents taken individually and, further, that the mineral and metal components boost the formula’s potency. Additional Ayurvedic therapies such as diet, yoga, or special purification routines, should be controlled for when recruiting and assessing patients. It is unclear, perhaps doubtful, that taking a single component of Ayurvedic is sufficient to represent the holistic effect of Ayurvedic interventions.
Limitations of our review. Our searches showed that herbal therapies were emphasized in published studies of Ayurveda. However, no conclusions can be drawn about the use of Ayurveda as a whole system for the treatment of diabetes. Although extensive efforts were made to obtain the relevant literature from India, studies not published in English were excluded, as were MD thesis reports. A handful of studies could not be obtained. Therefore we may not have included in this review all clinical trials. By specifically hand searching documents published in India, we identified that an important body of Ayurvedic literature is not identifiable using traditional systematic review methods.
In summary, we found preliminary evidence suggesting that some herbs and herbal formulas used in Ayurvedic therapy can have clinically important glucose-lowering effects. C indica, holy basil, and Gymnema are particularly worthy of additional study.
Acknowledgments
This research was performed by the Southern California Evidence-Based Practice Center based at RAND, Santa Monica, CA under contract with the Agency for Healthcare Research and Quality (Contract No. 290-97-0001) with support from the National Center for Complementary and Alternative Medicine. The authors of this article are responsible for its contents. No statement in this article should be construed as an official position of the Agency for Healthcare Research and Quality, the National Center for Complementary and Alternative Medicine, National Institutes of Health, or the US Department of Health and Human Services.
CORRESPONDING AUTHOR
Paul G. Shekelle, MD, PhD, West Los Angeles VA Medical Center, 111G, 11301 Wilshire Blvd, Los Angeles, CA 90073. E-mail: [email protected]. At the time of this study, Dr. Shekelle was a Senior Research Associate of the Veterans Affairs Health Services Research and Development Service.
1. Lad V. An introduction to Ayurveda. Altern Ther Health Med 1995;1:57-63.
2. Chopra A, Doiphode VV. Ayurvedic medicine. Core concept, therapeutic principles and current relevance. Med Clin North Am 2002;86:75-89.
3. Marles RJ, Farnsworth NR. Antidiabetic plants and their active constituents. Phytomedicine 1995;2:137-189.
4. Hardy M, Coulter I, Venuturupalli S, et al. Ayurvedic interventions for diabetes mellitus: a systematic review. Evidence Report/Technology Assessment No. 41. AHRQ Publication No. 01-E040; 2001.
5. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1-12.
6. Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408-412.
7. Moher D, Pham B, Jones A, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 1998;352:609-613.
8. Balk EM, Bonis PA, Moskowitz H, et al. Correlation of quality measures with estimates of treatment effect in meta-analyses of randomized controlled trials. JAMA 2002;287:2973-2982.
9. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088-1101.
10. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-634.
11. Azad Khan A, Akhtar S, Mahtab H. Coccinia indica in the treatment of patients with diabetes mellitus. Bangladesh Med Res Counc Bull 1979;5:60-66.
12. Agrawal P, Rai V, Singh RB. Randomized placebo-controlled single-blind trial of holy basil leaves in patients with non-insulin-dependent diabetes mellitus. Int J Clin Pharmacol Ther 1996;34:406-409.
13. Chandola HM, Tripathi SN, Udupa KH. Hypoglycaemic response of c. tamala in patients of maturity onset (insulin independent) diabetes. J Res Ayurveda Sidda 1980;1:275-290.
14. Kamble SM, Jyotishi GS, Kamalakar PL, Vaidya SM. Efficacy of coccinia indica w. & a. in diabetes mellitus. J Res Ayurveda and Sidda 1996;17(1–2):77-84.
15. Kohli KR, Singh RH. A clinical trial of jambu (eugenia jambolana) in non-insulin dependant diabetes mellitus. J Res Ayurveda Sidda 1993;14(3–4):89-97.
16. Baskaran K, Kizar Ahamath B, Radha Shanmugasundaram K, Shanmugasundaram ER. Antidiabetic effect of a leaf extract from gymnema sylvestre in non-insulin-dependent diabetes mellitus patients. J Ethnopharmacol 1990;30:295-300.
17. Shanmugasundaram E, Rajeswari G, Baskaran K, Rajesh Kumar BR, Radha Shanmugasundaram K, Kizar Ahmath B. Use of gymnema sylvestre leaf extract in the control of blood glucose in insulin-dependent diabetes mellitus. J Ethnopharmacol 1990;30:281-294.
18. Kuppurajan K, Seshadri C, Revathi R. Hypoglycaemic effect of coccinia indica in diabetes mellitus. Nagarjun 1986;29:1-4.
19. Kuppurajan K, Srivatsa A, Krishnaswami CV. Hypoglycemic and hypotriglyceridemic effects of methika churna (fenugreek). Antiseptic 1998;95:78-79.
20. Kumar N, Kumar A, Sharma ML. Clinical evaluation of single and herbo-mineral compound drugs in the management of madhumeha. J Res Ayurveda Sidda 1999;20(1–2):1-9.
21. Sharma RD, et al. Use of fenugreek seed powder in the management of non-insulin dependent diabetes mellitus. Nutr Res 1996;16:1331-1339.
22. Flexible dose open trial of Vijayasar in cases of newly-diagnosed non-insulin-dependent diabetes mellitus. Indian Council of Medical Research (ICMR), Collaborating Centres, New Delhi. Indian J Med Res 1998;108:24-29.
23. Goyal DK, Tiwari SK. Study on sadabahar (vinca rosea linn.) In madhumeha (diabetes mellitus). J Res Ayurveda Sidda 1999;20(1–2):93-100.
24. Chowdhary DP, Dua M, Bharti, Kishore P. Hypoglycaemic effect of a coded formulation: aysuh-82. J Res Ayurveda Sidda 1998;19(3–4):107-115.
25. Pandey VN, Rajagopalan SS, Chowdhary DP. An effective ayurvedic hypoglycemic formulation. J Res Ayurveda Sidda 1995;16(1–2):1-14.
26. Shankar R, Singhal R. Clinical studies of the effect of abraga (mica) chendooram in the treatment of diabetes mellitus (neerazhivu). J Res Ayurveda Sidda 1995;16(3–4):108-117.
27. Maji D, Singh AK. Clinical trial of D-400, a herbomineral preparation in diabetes mellitus. J Diabetic Assoc India 1995;35:1-4.
28. Sircar AR, Ahuja RC, Natu SM, Roy B, Sharma HM. Hypoglycemic, hypolipidemic and general beneficial effects of an herbal mixture MA-471. Alternat Ther Clin Pract 1996;3:26-31.
29. Shankar R, Sighal R. Clinical assessment of the effects of sandana (sandal) podi-a in the treatment of diabetes mellitus (neerazhiv). J Res Ayurveda Sidda 1994;15(3–4):89-97.
30. Sivaprakasam K, Rao KK, Yasodha R, Veluchamy G. Siddha remedy for diabetes mellitus. J Res Ayurveda Sidda 1984;5(1–4):25-32.
31. Kamble SM, Kamlakar PL, Vaidya S, Bambole VD. Influence of coccinia indica on certain enzymes in glycolytic and lipolytic pathway in human diabetes. Indian J Med Sci 1998;52:143-146.
32. Kapoor LD. CRC Handbook of Ayurvedic Medicinal Plants. Boca Raton, Fla: CRC Press; 1990.
33. Dash VB. Materia Medica of Indo-Tibetan Medicine. Delhi, India: MDIA Classics India; 1987;10-11.
34. Mishra L, Singh B, Dagenais S. Ayurveda: a historical perspective and principles of the traditional healthcare system in India. Altern Ther Health Med 2001;7:36-42.
- Limited randomized control trial data and observational studies show that the herbs Coccinia indica, holy basil, fenugreek, Gymnema sylvestre, and the herbal formulas Ayush-82 and D-400 have glucose-lowering effects. But these herbs are not as well studied as others more familiar to Western medicine. (B)
- Inform patients who ask about Ayurveda that traditional practitioners rely on the interaction of several components, of which herbs are just one, and that no formal studies have looked at Ayurveda as a whole system. (B)
- Objective: To evaluate and synthesize the evidence on the effect of Ayurvedic therapies for diabetes mellitus.
- Design: Systematic review of trials.
- Measurements and main results: We found no study that assessed Ayurvedic as a system of care. Botanical therapy was by far the most commonly studied Ayurvedic treatment. Herbs were studied either singly or as formulas. In all, 993 titles in Western computerized databases and 318 titles identified by hand-searching journals in India were examined, yielding 54 articles reporting the results of 62 studies. The most-studied herbs were G sylvestre, C indica, fenugreek, and Eugenia jambolana. A number of herbal formulas were tested, but Ayush-82 and D-400 were most often studied. Thirty-five of the studies included came from the Western literature, 27 from the Indian. Seven were randomized controlled trials (RCTs) and 10 controlled clinical trials (CCTs) or natural experiments. Twenty-two studies went on to further analysis based on a set of criteria. Of these, 10 were RCTs, CCTs, or natural experiments, 12 were case series or cohort studies. There is evidence to suggest that the herbs C indica, holy basil, fenugreek, and G sylvestre, and the herbal formulas Ayush-82 and D-400 have a glucose-lowering effect and deserve further study. Evidence of effectiveness of several other herbs is less extensive (C tamala, E jambolana, and Momordica charantia).
- Conclusions: There is heterogeneity in the available literature on Ayurvedic treatment for diabetes. Most studies test herbal therapy. Heterogeneity exists in the herbs and formulas tested (more than 44 different interventions identified) and in the method of their preparation. Despite these limitations, there are sufficient data for several herbs or herbal formulas to warrant further studies.
Given the US population’s increasing interest in herbal and alternative therapies, it is just a matter of time before you will be fielding questions from patients about Ayurveda—a comprehensive system of health care that originated in India roughly 3000 years ago, emphasizing the relationships among body, mind, and spirit. Diabetes has been a particular focus of this medical system, and a few Ayurvedic herbs do indeed appear to exert glucose lowering mechanisms.
But how strong is the evidence? Though Ayurveda involves the interaction of many kinds of therapy, this review examines only the literature pertaining to herbal remedies your patients with diabetes are likely to ask about.
Ayurveda more than herbs
Ayurveda (Sanskrit for “knowledge of life” or “knowledge of longevity”) has now spread beyond India’s borders to include the rest of the Indian subcontinent, Sri Lanka, Malaysia, Mauritius, South Africa, Japan, Russia, Europe, and North America. At its root, Ayurveda seeks to restore an individual’s innate harmony. Primary Ayurvedic treatments include diet, exercise, meditation, herbs, massage, exposure to sunlight, controlled breathing, and detoxification treatments.
Dosha imbalance. Ayurveda considers human beings a microcosm of nature. All living and nonliving things are believed to consist of 5 basic elements: ether (space), air, fire, water, and earth. In humans these elements combine and manifest in the human body as 3 humors, or doshas, known as vata, pitta, and kapha.
The doshas govern all biological, psychological, and pathophysiological functions. They are fundamental to human health, and an imbalance of the doshas brings on illness. Consequently, Ayurveda seeks to bring the doshas back into harmony. Balanced doshas, as well as good-quality tissues (dhatus), proper digestion, and elimination of excretions (malas), are considered essential in Ayurveda for maintaining health.
Dosha body type influences treatment. In addition, humans are endowed at birth with 1 of 7 body types, depending on which dosha or combination of the 3 basic doshas dominates. Body types can be dominated by a single humor (vata, pitta, or kapha), or they can be dominated by combinations: vata-kapha (when vata and kapha are present in almost equal amounts); vata-pitta; pitta-kapha; or vata-pitta-kapha. A person’s dosha body type is expressed physically and emotionally; for example, a person with a vata-dominant body type will have a thin frame and an insecure temperament. The Ayurvedic physician takes body type and imbalances among the doshas into consideration when treating a patient.
Application to diabetes. The Indian word for diabetes is madhumeha, from madhu, meaning “sweet/sweetness,” and meha, meaning excessive urination. Classical Ayurvedic therapy for madhumeha (diabetes) begins with an assessment of the dosha imbalance. In all types of pramehas (urinary disorders), kapha is vitiated, but in madhumeha, vata is often aggravated as well. Therefore, therapies will be directed at both vata and kapha simultaneously to restore the balance of the doshas.1,2
Herbs are a commonly used treatment in Ayurveda. Ethnobotanical studies of traditional herbal remedies used for diabetes around the world have identified more than 1200 species of plants with hypoglycemic activity. These plants are broadly distributed throughout 725 different genera. The pharmacopoeia of India is especially rich in herbal treatments for diabetes. Eighty-five percent of the 20 antidiabetes plants most widely used around the world are prescribed in India.3 A few of the herbs commonly used by Ayurveda practitioners to treat diabetes are summarized in the TABLE.
In response to the increasing interest in Ayurveda and herbal treatments for diabetes in this country, the National Center for Complimentary and Alternative Medicine (NCCAM) requested we conduct a systematic review of Ayurvedic therapy for diabetes. This paper reports the results of that review, and is a condensation of an evidence report available at www.ahrq.gov/clinic/epcsums/ayurvsum.htm.
TABLE
Ayurvedic characteristics of herbs commonly used to treat diabetes
| HERB | TASTE (RASA) | INCREASES (AGGRAVATES) | DECREASES (PACIFIES) |
|---|---|---|---|
| Gymnema | Kasaya (astringent) | Kapha, Pitta | |
| Momordica | Tikta (bitter) | Kapha, Pitta | |
| Trigonella (fenugreek) | Tikta (bitter); Madhura (sweet) | Pitta | Kapha, Vata |
| Coccinia indica | Kasaya (astringent); Tikta (bitter) | Vata, Pitta | |
| Pterocarpus | Kasaya (astringent) | Vata | |
| Source: Kapoor, 1990;32 Dash, 198733 Mishra, Singh, and Dagenais, 2001.34 | |||
Methods
Identification of literature
We used the search term “Ayurveda” plus the names of 16 major botanicals characteristically used in Ayurveda for an initial search of the Western literature. The herbal terms were added to the search to increase its sensitivity, making it possible to find studies that used Ayurvedic herbal therapy without necessarily being directly identified as Ayurvedic studies.
We were concerned that a large body of literature existed in India that could not be obtained through the conventional search strategy outlined above. Hence, we decided to conduct a search for Ayurvedic literature from the Indian subcontinent. A physician member of the research team, fluent in English and Hindi and who had trained in India, went to India to identify Ayurvedic literature available there.
We therefore used several sources for our search:
- An initial “waterfront” search, which already had identified 120 articles on diabetes and Ayurveda (which was used by NCCAM to establish the rationale for selecting diabetes as the focus of this review).4 This search is detailed in our Evidence Report (available at www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat1.chapter.95372) and included Medline, HealthSTAR, Allied and Complementary Medicine, MANTIS, CAB HEALTH, BIOSIS Previews, and EMBASE.
- The in-person literature search in India—we obtained 16 volumes of abstracts from various Indian Ayurvedic journals, as compiled by the Central Council for Research in Ayurveda and Siddha (CCRAS) library. This yielded 318 titles.
- An additional online search of the previously mentioned databases for common botanicals used in the treatment of diabetes. This search yielded 773 additional articles.
- A search of the online CINAHL database, which yielded 70 articles.
- The reference lists of important articles in the Ayurveda/diabetes literature. We identified review articles of herbal treatment of diabetes and checked to see if they focused on any of the Ayurvedic herbal therapies we had identified for diabetes. Checking the bibliographies of all the articles we identified from any source, we found an additional 30 titles that were potentially relevant to our search.
- An RCT or a CCT or a natural experiment with a comparison arm that did not receive an herb or Ayurvedic therapy. RCTs of any size were included. For CCTs or natural experiments, the study had to have at least 1 treatment arm that contained at least 10 patients.
- Because of a paucity of studies meeting these design criteria, we also assessed cohort or case series data that used a “pre/post” method of analysis, if their sample included at least 10 subjects.
- The study had to test Ayurveda as a method or herbs used as a single agent, a formula acting as a single agent, or a limited combination of products (no more than 3) acting as a single agent. The agent had to be dispensed more than 1 time to the study patients (in other words, no single-dose studies).
- The study had to report on at least 1 of 3 outcome measures at 30 days minimum following the start of the study: glycosylated hemoglobin (Hb A1c), fasting blood glucose, or postprandial blood glucose at either 2 hours (preferred) or 1 hour (acceptable).
Data extraction
Detailed information from each study was extracted using a specialized form. The physician reviewers, working independently, extracted data in duplicate and resolved disagreements by consensus. A senior physician resolved any remaining disagreements. Information extracted from articles included the diagnostic criteria used to make the diagnosis (Ayurvedic or Western or both); the location in which the study was done; the subject population (age, gender, other demographics); the sample size in each arm of the study; the interventions used (primarily the names of the individual herbs or mineral and the manner of their preparation); the length of the study; and the outcomes. To evaluate the quality of the design and execution of trials, we collected information on the study design, appropriateness of randomization, blinding, description of withdrawals and dropouts, and concealment of allocation.5,6 A quality score was calculated for each trial using a system developed by Jadad.5 Empirical evidence has shown that studies scoring 2 or less on the Jadad scale report exaggerated results compared with studies scoring 3 or more.7 While other elements of the design and execution of controlled trials have been proposed as quality measures, empirical evidence supporting their use as generic quality measures is lacking.8
Data synthesis
The studies we reviewed were judged clinically to be too heterogeneous to support a quantitative synthesis; therefore, our review is narrative. However, to promote the comparison of results across studies we extracted outcome data in a common format and present it in graphs for visual comparison. For studies that reported on both 1-hour and 2-hour postprandial blood glucose levels, we chose the 2-hour measurement for the analysis. For studies that reported more than 1 follow-up time, we selected the follow-up time that was closest to 3 months.
Twenty-two studies were selected for further analysis based on the criteria described above. These studies represented either RCTs (2) or CCTs/natural experiments (5) with a comparison arm that did not receive an herb, or studies that had pre/post comparison data available (8).
We considered 2 subgroups of eligible studies separately: the RCTs and CCTs or natural experiments that had nonherbal/Ayurvedic comparison arm(s) were considered 1 subgroup, and all other eligible (pre/post data available) studies made up the second subgroup. The RCT/CCT/natural experiments subgroup allowed us to do a comparison between herbal and nonherbal arms within a study, providing a stronger level of evidence than pre/post comparisons. For these studies, we were able to compare the effects of different treatments after the placebo or nonherbal arm results were taken into account by estimating a difference of differences statistic and its 95% confidence interval. This statistic is equal to the difference between the pre- and post-treatment means in the Ayurvedic arm minus the analogous difference in the nonherbal/Ayurvedic arm. The pre/post studies subgroup did not allow a concurrent comparison, but the difference between pre- and post-treatment means could be estimated along with a 95% confidence interval.4 Further details are given in our Evidence Report (available online at www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat1.chapter.95372).
For each study subgroup, we assessed the possibility of publication bias graphically by evaluating a funnel plot of the study summary statistics for asymmetry, which would result from the nonpublication of small trials with negative outcomes. Because graphical evaluation can be subjective, we also conducted an adjusted rank-correlation test9 and a regression asymmetry test10 as formal statistical tests for publication bias.
Results
Description of the evidence
As a result of our search, we considered a total of 1311 articles (FIGURE 1). We reviewed in depth 62 studies, of which 22 were analyzed statistically. Ten studies came from the Western literature, and 12 came from the Indian literature. There were 7 randomized controlled trials, controlled clinical trials, or natural experiments with a treatment/no treatment comparison. There were 15 case series or cohort studies using a “pre/post” analysis. TABLE W2 (available online at www.jfponline.com) summarizes the characteristics of studies.
In terms of interventions, there was no study that tested Ayurveda as a system of care; all tested herbs. Of the 22 studies described narratively in this article, the 2 most commonly tested single herbs were Coccinia indica and fenugreek. The Ayurvedic formula Ayush-82 was the most commonly tested herbal formula. Diet was used as an intervention or co-intervention in 15 of the 22 studies.
FIGURE 1
Ayurveda literature review strategy of focused search for human diabetes articles
Quality of the evidence
Only the RCTs, CCTs, and natural experiments were given a Jadad score, which rates studies on a 0 to 5 scale.5 Of the 7 such studies, 3 received a Jadad score of zero, 3 studies scored a 1, and only 1 study received a 4 on this scale. This is the only high quality study in our analysis.
Controlled trials/natural experiments with nonherbal comparison arm(s)
There were 7 RCTs, CCTs or natural experiments that met the inclusion criteria. The data for these 7 studies are reported in FIGURE 2.
Coccinia indica. Azad Khan, Akhtar, and Mahtab (1979) performed a randomized controlled trial to assess the hypoglycemic properties of a preparation of the herb C indica on uncontrolled and untreated type 2 diabetes patients.11 Thirty-eight patients with type 2 diabetes who were attending the outpatient department of the Bangladesh Institute of Research and Rehabilitation in Diabetes in Dhaka, Bangladesh, were recruited for the study. Only uncontrolled or newly diagnosed patients were enlisted. The intervention consisted of a freeze-dried powder of crushed leaves of C indica, given in a dose of 900 mg twice a day for 6 weeks. Control patients received placebo twice a day for the same period. Of the 16 patients receiving C indica, 10 patients showed a marked improvement in the glucose tolerance tests to values closer to normal, while none in the placebo arm showed marked improvement. The Jadad score for the trial was 4. This study was identified from the Eastern literature search.
Holy basil. Agrawal, Rai, and Singh (1996) reported the results of a randomized, placebo controlled crossover trial of the effects of a leaf extract of holy basil (Ocimum sanctum) on patients with type 2 diabetes.12 Forty patients were recruited from community advertisements in Kanpur, India, and through visits to the offices of local dieticians. All subjects had a 5-day run-in period during which they all consumed a tea made from holy basil leaves. This was followed by an 8-week experimental period. The patients were randomly assigned to drink the holy basil leaf tea for 4 weeks followed by placebo leaves for 4 weeks, or the reverse (the placebo leaves first, followed by the holy basil leaf tea). The authors concluded that holy basil leaf powder caused significant reduction in the level of fasting blood sugar and postprandial blood sugar, and a moderate reduction in cholesterol. The Jadad score for this trial is 1. This study was identified from the Western literature search.
Cinnamonum tamala. Chandola, Tripathi, and Udupa (1980) assessed the hypoglycemic effects of C tamala in type 2 diabetes patients.13 Thirty-two patients were recruited from the outpatient departments of the Institute of Medical Sciences, Varanasi, India, and received the intervention and 8 patients with type 2 diabetes served as controls. The socioeconomic characteristics of the patients were not noted, and the authors did not report if the 2 arms of patients were statistically equivalent on important prognostic variables at the start of the trial. The intervention consisted of leaves of C tamala (tejpatra) that were dried, pulverized, and filtered through a fine mesh, and given as 2 heaped teaspoons 4 times a day before meals and tea for a total of 1 month. All patients were advised to follow a 1800-calorie diet with restriction of sugar, potato, and rice. The control patients were only instructed to follow the above diet with no other medications. Fasting blood sugars were assessed in both arms of patients before the trial and at the end of 1 month. The authors reported the mean fasting blood sugar improved from 153 mg/dL to 113 mg/dL (P<.001) at the end of 1 month in patients treated with C tamala, while there was no improvement in control patients. The Jadad score for this study was 0. This study was identified from the Eastern literature search.
Coccina indica. Kamble, Jyotishi, Kamalakar, et al (1996) studied the effect of fresh leaves of C indica on blood sugar levels and on hyperlipidemia in noninsulin-dependent diabetes mellitus (NIDDM, type 2) patients at an Ayurvedic clinic in Nagpur, India.14 Patients were classified into 4 arms: a healthy comparison arm (arm I, 15 patients); a NIDDM comparison arm (arm II, 30 patients); NIDDM patients treated with Coccinia (arm III, 25 patients); and a NIDDM arm treated with chlorpropamide (arm IV, 15 patients). Patients were given the Coccinia (decocted from fresh leaves, dried into a paste, and made into a 3-g tablet) twice a day for 12 weeks, although control group data only exist at 6 weeks. For patients in arm III, the study showed a statistically significant reduction in mean fasting blood sugar, from 160 to 118 mg/dL (P<.001) at 12 weeks, and a significant decrease in blood sugar levels after glucose tolerance tests: the 2-hour level dropped from 308 mg/dL to 142 mg/dL (P<.001). These results were roughly equivalent to those found in the chlorpropamide arm at 6 weeks, with any differences being not statistically significant. Additionally, after 12 weeks of treatment, the Coccinia treated patients showed significant within group reductions in levels of cholesterol (P<.001), phospholipid (P<.05), triglyceride (P<.001), and free fatty acid (P<.001) compared with untreated patients with diabetes. The Jadad score for this study was 0. This study was identified from the Eastern literature search.
Jamun beej. Kohli and Singh (1993) studied the effects of Jamun beej (Eugenia jambolana) on fasting blood sugar, glucose tolerance test, and symptomatic relief of symptoms associated with diabetes.15 Thirty patients identified from the outpatient unit of the Sunderlal Hospital in Varanasi, India, who had NIDDM confirmed by glucose tolerance test, were given E jambolana crushed into a fine powder at a dose of 4 g 3 times a day for 3 months. No dietary restrictions were included in the study. A second arm of 6 patients with confirmed NIDDM was given chlorpropamide (250 mg/d). No demographic information was provided on these patients. The authors reported a statistically significant reduction in mean fasting blood sugar of 51.86 mg/dL at 2 months (P<.001) but not at 3 months. The study also demonstrated a significant reduction in the response to the glucose tolerance test at both 2 months (P<.001) and at 3 months (P<.01), but comparisons with the patients receiving chlorpropamide were not statistically significant. The Jadad score total is 1. This study was identified from the Eastern literature search.
Gymnema sylvestre. Baskaran, Ahamath, Shanmugasundaram, et al (1990) studied the effects of GS4, a specific isolate of G sylvestre, on the blood sugar of 47 type 2 diabetes patients.16 The intervention group consisted of 22 patients with diabetes on oral hypoglycemic therapy (continued during the trial), plus herbal therapy with Gymnema at a dose of 400 mg/d. The control group consisted of 25 patients with type 2 diabetes on conventional medications alone. Although the arms were reasonably matched for age and Broca index (percent of ideal body weight) based on our analysis of individual patient data in the study, the 2 arms were statistically different at baseline with respect to fasting blood sugar. The authors reported that in the intervention group at 12 months of follow-up, mean fasting blood sugar improved from 174 mg/dL to 124 mg/dL (P<.001) and Hb A1c improved from 11.9% to 8.48% (P<.001). Changes in the control group over this time were not significant. Virtually all patients in arm I developed hypoglycemic symptoms, and the dose of their normal oral hypoglycemic agent needed to be changed or stopped. The Jadad score is 0. This study was identified from the Western literature search.
GS4. Shanmugasundaram, Rajeswari, Baskaran, et al (1990b) reported the effect of an herbal compound GS4 on blood glucose, insulin requirements, and cholesterol in patients with type 1 and type 2 diabetes.17 The intervention group consisted of 23 type 1 patients and 4 type 2 patients (ages 44–50 years, 25% female) who continued their insulin in addition to taking the herbal intervention, and the control group consisted of 37 type 1 patients who were on insulin therapy. The clinical equivalence of the 2 arms at baseline was not mentioned. The intervention drug was GS4, a recrystallized precipitate of the alcoholic extract of the acidic fraction of G sylvestre; at dose of 400 mg/d. At 6 to 8 months of follow-up, all patients in the intervention group developed hypoglycemic episodes, and their insulin doses were reduced by 10 units at a time; differences compared to controls were statistically significant. The Jadad score was 1. This study was identified from the Western literature search.
Summary. In summary, comparisons of the studied herbs with either placebo, diet, or as an adjunct to medical hypoglycemic therapy consistently reported statistically significant benefits in glucose control. Studies comparing herbs to the oral hypoglycemic chlorpropamide did not report differences between groups.
FIGURE 2
Glucose-lowering effects of Ayurvedic herbs compared with nonherbal treatments
Case series or cohort studies without a concurrent comparison group
Fifteen studies had treatment arms that reported blood glucose or Hb A1c values before and after herbal interventions—ie, that made available pre/post data.13,18-31 Herbs were tested singly (7 studies), in combination (7 studies), or both singly and in combination (1 study). All of these studies are limited by the lack of randomization. Many are also limited by small sample size and short study duration.
The data are presented in FIGURE 3 in the following order: studies or arms of studies using a single herbal preparation first, followed by studies that use a formula or a group of herbs and minerals. Some studies with multiple arms will have listings in more than one place. As FIGURE 3 shows, most pre/post comparison studies using single herbs and formulas favor treatment. Hb A1c is measured in only 5 of the studies. Two of those studies seem to strongly favor treatment; 2 are almost equivocal; and 1 does not favor treatment.
The small number of RCTs/CCTs/natural experiments measuring postprandial blood glucose and Hb A1c, and the small number of case series and cohorts measuring Hb A1c, make the assessment of publication bias for these outcomes problematic. For the remaining outcomes, only slight evidence of publication bias was evident among the case series and cohort studies for the fasting blood glucose outcome (adjusted rank correlation test P=.97; regression asymmetry test P=.06). For this outcome, we have trial data available, a setting in which no evidence of publication bias is seen.
FIGURE 3
Effect of Ayurvedic herbs on blood glucose and Hb A1c
Discussion
No controlled trials have assessed Ayurveda as a system of care. Furthermore, among studies of herbal preparations, controlled trials are rare and mostly of poor quality. Still, we found evidence suggesting that some Ayurvedic herbs have clinically important hypoglycemic effects.
The best-quality RCT reported beneficial results for C indica. Other studies have generally reported benefits of C indica; however, results have been inconsistent.
A single trial of holy basil reported a benefit in controlling fasting blood glucose only. G sylvestre was used in a number of studies, again with generally beneficial results. Gymnema was also a constituent in 2 of the formulas that reported beneficial results: D-400 and Ayush-82.
Methodological shortcomings. The evidence we found falls short of proof. As noted, the individual studies we assessed had significant methodological shortcomings. Few used a randomized, placebo-controlled design, despite the feasibility of such methods. Studies generally were underpowered to determine even large effect sizes. Many studies involved an extremely small number of subjects (fewer than 10). A number of studies failed to use appropriate statistical methods in reporting the results. Furthermore, the duration of most studies was short, and only intermediate outcomes (measure of blood sugar control) were reported. Longer term studies that assess clinical outcomes are required. Lastly, there is great heterogeneity in the available literature on Ayurvedic treatment for diabetes, despite the fact that the overwhelming majority of studies test herbal therapy. Heterogeneity exists in the herbs and formulas tested and in the method of their preparation.
No true studies of Ayurveda. None of the identified studies assessed Ayurveda as a system of diagnosis and care. The literature reported mainly studies of single herbs; however, in clinical Ayurvedic practice, herbs are usually given in combination. Formulas can include minerals and metals in addition to multiple plants.
Ayurvedic practitioners assert that the sum of a formula is more potent than the constituents taken individually and, further, that the mineral and metal components boost the formula’s potency. Additional Ayurvedic therapies such as diet, yoga, or special purification routines, should be controlled for when recruiting and assessing patients. It is unclear, perhaps doubtful, that taking a single component of Ayurvedic is sufficient to represent the holistic effect of Ayurvedic interventions.
Limitations of our review. Our searches showed that herbal therapies were emphasized in published studies of Ayurveda. However, no conclusions can be drawn about the use of Ayurveda as a whole system for the treatment of diabetes. Although extensive efforts were made to obtain the relevant literature from India, studies not published in English were excluded, as were MD thesis reports. A handful of studies could not be obtained. Therefore we may not have included in this review all clinical trials. By specifically hand searching documents published in India, we identified that an important body of Ayurvedic literature is not identifiable using traditional systematic review methods.
In summary, we found preliminary evidence suggesting that some herbs and herbal formulas used in Ayurvedic therapy can have clinically important glucose-lowering effects. C indica, holy basil, and Gymnema are particularly worthy of additional study.
Acknowledgments
This research was performed by the Southern California Evidence-Based Practice Center based at RAND, Santa Monica, CA under contract with the Agency for Healthcare Research and Quality (Contract No. 290-97-0001) with support from the National Center for Complementary and Alternative Medicine. The authors of this article are responsible for its contents. No statement in this article should be construed as an official position of the Agency for Healthcare Research and Quality, the National Center for Complementary and Alternative Medicine, National Institutes of Health, or the US Department of Health and Human Services.
CORRESPONDING AUTHOR
Paul G. Shekelle, MD, PhD, West Los Angeles VA Medical Center, 111G, 11301 Wilshire Blvd, Los Angeles, CA 90073. E-mail: [email protected]. At the time of this study, Dr. Shekelle was a Senior Research Associate of the Veterans Affairs Health Services Research and Development Service.
- Limited randomized control trial data and observational studies show that the herbs Coccinia indica, holy basil, fenugreek, Gymnema sylvestre, and the herbal formulas Ayush-82 and D-400 have glucose-lowering effects. But these herbs are not as well studied as others more familiar to Western medicine. (B)
- Inform patients who ask about Ayurveda that traditional practitioners rely on the interaction of several components, of which herbs are just one, and that no formal studies have looked at Ayurveda as a whole system. (B)
- Objective: To evaluate and synthesize the evidence on the effect of Ayurvedic therapies for diabetes mellitus.
- Design: Systematic review of trials.
- Measurements and main results: We found no study that assessed Ayurvedic as a system of care. Botanical therapy was by far the most commonly studied Ayurvedic treatment. Herbs were studied either singly or as formulas. In all, 993 titles in Western computerized databases and 318 titles identified by hand-searching journals in India were examined, yielding 54 articles reporting the results of 62 studies. The most-studied herbs were G sylvestre, C indica, fenugreek, and Eugenia jambolana. A number of herbal formulas were tested, but Ayush-82 and D-400 were most often studied. Thirty-five of the studies included came from the Western literature, 27 from the Indian. Seven were randomized controlled trials (RCTs) and 10 controlled clinical trials (CCTs) or natural experiments. Twenty-two studies went on to further analysis based on a set of criteria. Of these, 10 were RCTs, CCTs, or natural experiments, 12 were case series or cohort studies. There is evidence to suggest that the herbs C indica, holy basil, fenugreek, and G sylvestre, and the herbal formulas Ayush-82 and D-400 have a glucose-lowering effect and deserve further study. Evidence of effectiveness of several other herbs is less extensive (C tamala, E jambolana, and Momordica charantia).
- Conclusions: There is heterogeneity in the available literature on Ayurvedic treatment for diabetes. Most studies test herbal therapy. Heterogeneity exists in the herbs and formulas tested (more than 44 different interventions identified) and in the method of their preparation. Despite these limitations, there are sufficient data for several herbs or herbal formulas to warrant further studies.
Given the US population’s increasing interest in herbal and alternative therapies, it is just a matter of time before you will be fielding questions from patients about Ayurveda—a comprehensive system of health care that originated in India roughly 3000 years ago, emphasizing the relationships among body, mind, and spirit. Diabetes has been a particular focus of this medical system, and a few Ayurvedic herbs do indeed appear to exert glucose lowering mechanisms.
But how strong is the evidence? Though Ayurveda involves the interaction of many kinds of therapy, this review examines only the literature pertaining to herbal remedies your patients with diabetes are likely to ask about.
Ayurveda more than herbs
Ayurveda (Sanskrit for “knowledge of life” or “knowledge of longevity”) has now spread beyond India’s borders to include the rest of the Indian subcontinent, Sri Lanka, Malaysia, Mauritius, South Africa, Japan, Russia, Europe, and North America. At its root, Ayurveda seeks to restore an individual’s innate harmony. Primary Ayurvedic treatments include diet, exercise, meditation, herbs, massage, exposure to sunlight, controlled breathing, and detoxification treatments.
Dosha imbalance. Ayurveda considers human beings a microcosm of nature. All living and nonliving things are believed to consist of 5 basic elements: ether (space), air, fire, water, and earth. In humans these elements combine and manifest in the human body as 3 humors, or doshas, known as vata, pitta, and kapha.
The doshas govern all biological, psychological, and pathophysiological functions. They are fundamental to human health, and an imbalance of the doshas brings on illness. Consequently, Ayurveda seeks to bring the doshas back into harmony. Balanced doshas, as well as good-quality tissues (dhatus), proper digestion, and elimination of excretions (malas), are considered essential in Ayurveda for maintaining health.
Dosha body type influences treatment. In addition, humans are endowed at birth with 1 of 7 body types, depending on which dosha or combination of the 3 basic doshas dominates. Body types can be dominated by a single humor (vata, pitta, or kapha), or they can be dominated by combinations: vata-kapha (when vata and kapha are present in almost equal amounts); vata-pitta; pitta-kapha; or vata-pitta-kapha. A person’s dosha body type is expressed physically and emotionally; for example, a person with a vata-dominant body type will have a thin frame and an insecure temperament. The Ayurvedic physician takes body type and imbalances among the doshas into consideration when treating a patient.
Application to diabetes. The Indian word for diabetes is madhumeha, from madhu, meaning “sweet/sweetness,” and meha, meaning excessive urination. Classical Ayurvedic therapy for madhumeha (diabetes) begins with an assessment of the dosha imbalance. In all types of pramehas (urinary disorders), kapha is vitiated, but in madhumeha, vata is often aggravated as well. Therefore, therapies will be directed at both vata and kapha simultaneously to restore the balance of the doshas.1,2
Herbs are a commonly used treatment in Ayurveda. Ethnobotanical studies of traditional herbal remedies used for diabetes around the world have identified more than 1200 species of plants with hypoglycemic activity. These plants are broadly distributed throughout 725 different genera. The pharmacopoeia of India is especially rich in herbal treatments for diabetes. Eighty-five percent of the 20 antidiabetes plants most widely used around the world are prescribed in India.3 A few of the herbs commonly used by Ayurveda practitioners to treat diabetes are summarized in the TABLE.
In response to the increasing interest in Ayurveda and herbal treatments for diabetes in this country, the National Center for Complimentary and Alternative Medicine (NCCAM) requested we conduct a systematic review of Ayurvedic therapy for diabetes. This paper reports the results of that review, and is a condensation of an evidence report available at www.ahrq.gov/clinic/epcsums/ayurvsum.htm.
TABLE
Ayurvedic characteristics of herbs commonly used to treat diabetes
| HERB | TASTE (RASA) | INCREASES (AGGRAVATES) | DECREASES (PACIFIES) |
|---|---|---|---|
| Gymnema | Kasaya (astringent) | Kapha, Pitta | |
| Momordica | Tikta (bitter) | Kapha, Pitta | |
| Trigonella (fenugreek) | Tikta (bitter); Madhura (sweet) | Pitta | Kapha, Vata |
| Coccinia indica | Kasaya (astringent); Tikta (bitter) | Vata, Pitta | |
| Pterocarpus | Kasaya (astringent) | Vata | |
| Source: Kapoor, 1990;32 Dash, 198733 Mishra, Singh, and Dagenais, 2001.34 | |||
Methods
Identification of literature
We used the search term “Ayurveda” plus the names of 16 major botanicals characteristically used in Ayurveda for an initial search of the Western literature. The herbal terms were added to the search to increase its sensitivity, making it possible to find studies that used Ayurvedic herbal therapy without necessarily being directly identified as Ayurvedic studies.
We were concerned that a large body of literature existed in India that could not be obtained through the conventional search strategy outlined above. Hence, we decided to conduct a search for Ayurvedic literature from the Indian subcontinent. A physician member of the research team, fluent in English and Hindi and who had trained in India, went to India to identify Ayurvedic literature available there.
We therefore used several sources for our search:
- An initial “waterfront” search, which already had identified 120 articles on diabetes and Ayurveda (which was used by NCCAM to establish the rationale for selecting diabetes as the focus of this review).4 This search is detailed in our Evidence Report (available at www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat1.chapter.95372) and included Medline, HealthSTAR, Allied and Complementary Medicine, MANTIS, CAB HEALTH, BIOSIS Previews, and EMBASE.
- The in-person literature search in India—we obtained 16 volumes of abstracts from various Indian Ayurvedic journals, as compiled by the Central Council for Research in Ayurveda and Siddha (CCRAS) library. This yielded 318 titles.
- An additional online search of the previously mentioned databases for common botanicals used in the treatment of diabetes. This search yielded 773 additional articles.
- A search of the online CINAHL database, which yielded 70 articles.
- The reference lists of important articles in the Ayurveda/diabetes literature. We identified review articles of herbal treatment of diabetes and checked to see if they focused on any of the Ayurvedic herbal therapies we had identified for diabetes. Checking the bibliographies of all the articles we identified from any source, we found an additional 30 titles that were potentially relevant to our search.
- An RCT or a CCT or a natural experiment with a comparison arm that did not receive an herb or Ayurvedic therapy. RCTs of any size were included. For CCTs or natural experiments, the study had to have at least 1 treatment arm that contained at least 10 patients.
- Because of a paucity of studies meeting these design criteria, we also assessed cohort or case series data that used a “pre/post” method of analysis, if their sample included at least 10 subjects.
- The study had to test Ayurveda as a method or herbs used as a single agent, a formula acting as a single agent, or a limited combination of products (no more than 3) acting as a single agent. The agent had to be dispensed more than 1 time to the study patients (in other words, no single-dose studies).
- The study had to report on at least 1 of 3 outcome measures at 30 days minimum following the start of the study: glycosylated hemoglobin (Hb A1c), fasting blood glucose, or postprandial blood glucose at either 2 hours (preferred) or 1 hour (acceptable).
Data extraction
Detailed information from each study was extracted using a specialized form. The physician reviewers, working independently, extracted data in duplicate and resolved disagreements by consensus. A senior physician resolved any remaining disagreements. Information extracted from articles included the diagnostic criteria used to make the diagnosis (Ayurvedic or Western or both); the location in which the study was done; the subject population (age, gender, other demographics); the sample size in each arm of the study; the interventions used (primarily the names of the individual herbs or mineral and the manner of their preparation); the length of the study; and the outcomes. To evaluate the quality of the design and execution of trials, we collected information on the study design, appropriateness of randomization, blinding, description of withdrawals and dropouts, and concealment of allocation.5,6 A quality score was calculated for each trial using a system developed by Jadad.5 Empirical evidence has shown that studies scoring 2 or less on the Jadad scale report exaggerated results compared with studies scoring 3 or more.7 While other elements of the design and execution of controlled trials have been proposed as quality measures, empirical evidence supporting their use as generic quality measures is lacking.8
Data synthesis
The studies we reviewed were judged clinically to be too heterogeneous to support a quantitative synthesis; therefore, our review is narrative. However, to promote the comparison of results across studies we extracted outcome data in a common format and present it in graphs for visual comparison. For studies that reported on both 1-hour and 2-hour postprandial blood glucose levels, we chose the 2-hour measurement for the analysis. For studies that reported more than 1 follow-up time, we selected the follow-up time that was closest to 3 months.
Twenty-two studies were selected for further analysis based on the criteria described above. These studies represented either RCTs (2) or CCTs/natural experiments (5) with a comparison arm that did not receive an herb, or studies that had pre/post comparison data available (8).
We considered 2 subgroups of eligible studies separately: the RCTs and CCTs or natural experiments that had nonherbal/Ayurvedic comparison arm(s) were considered 1 subgroup, and all other eligible (pre/post data available) studies made up the second subgroup. The RCT/CCT/natural experiments subgroup allowed us to do a comparison between herbal and nonherbal arms within a study, providing a stronger level of evidence than pre/post comparisons. For these studies, we were able to compare the effects of different treatments after the placebo or nonherbal arm results were taken into account by estimating a difference of differences statistic and its 95% confidence interval. This statistic is equal to the difference between the pre- and post-treatment means in the Ayurvedic arm minus the analogous difference in the nonherbal/Ayurvedic arm. The pre/post studies subgroup did not allow a concurrent comparison, but the difference between pre- and post-treatment means could be estimated along with a 95% confidence interval.4 Further details are given in our Evidence Report (available online at www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat1.chapter.95372).
For each study subgroup, we assessed the possibility of publication bias graphically by evaluating a funnel plot of the study summary statistics for asymmetry, which would result from the nonpublication of small trials with negative outcomes. Because graphical evaluation can be subjective, we also conducted an adjusted rank-correlation test9 and a regression asymmetry test10 as formal statistical tests for publication bias.
Results
Description of the evidence
As a result of our search, we considered a total of 1311 articles (FIGURE 1). We reviewed in depth 62 studies, of which 22 were analyzed statistically. Ten studies came from the Western literature, and 12 came from the Indian literature. There were 7 randomized controlled trials, controlled clinical trials, or natural experiments with a treatment/no treatment comparison. There were 15 case series or cohort studies using a “pre/post” analysis. TABLE W2 (available online at www.jfponline.com) summarizes the characteristics of studies.
In terms of interventions, there was no study that tested Ayurveda as a system of care; all tested herbs. Of the 22 studies described narratively in this article, the 2 most commonly tested single herbs were Coccinia indica and fenugreek. The Ayurvedic formula Ayush-82 was the most commonly tested herbal formula. Diet was used as an intervention or co-intervention in 15 of the 22 studies.
FIGURE 1
Ayurveda literature review strategy of focused search for human diabetes articles
Quality of the evidence
Only the RCTs, CCTs, and natural experiments were given a Jadad score, which rates studies on a 0 to 5 scale.5 Of the 7 such studies, 3 received a Jadad score of zero, 3 studies scored a 1, and only 1 study received a 4 on this scale. This is the only high quality study in our analysis.
Controlled trials/natural experiments with nonherbal comparison arm(s)
There were 7 RCTs, CCTs or natural experiments that met the inclusion criteria. The data for these 7 studies are reported in FIGURE 2.
Coccinia indica. Azad Khan, Akhtar, and Mahtab (1979) performed a randomized controlled trial to assess the hypoglycemic properties of a preparation of the herb C indica on uncontrolled and untreated type 2 diabetes patients.11 Thirty-eight patients with type 2 diabetes who were attending the outpatient department of the Bangladesh Institute of Research and Rehabilitation in Diabetes in Dhaka, Bangladesh, were recruited for the study. Only uncontrolled or newly diagnosed patients were enlisted. The intervention consisted of a freeze-dried powder of crushed leaves of C indica, given in a dose of 900 mg twice a day for 6 weeks. Control patients received placebo twice a day for the same period. Of the 16 patients receiving C indica, 10 patients showed a marked improvement in the glucose tolerance tests to values closer to normal, while none in the placebo arm showed marked improvement. The Jadad score for the trial was 4. This study was identified from the Eastern literature search.
Holy basil. Agrawal, Rai, and Singh (1996) reported the results of a randomized, placebo controlled crossover trial of the effects of a leaf extract of holy basil (Ocimum sanctum) on patients with type 2 diabetes.12 Forty patients were recruited from community advertisements in Kanpur, India, and through visits to the offices of local dieticians. All subjects had a 5-day run-in period during which they all consumed a tea made from holy basil leaves. This was followed by an 8-week experimental period. The patients were randomly assigned to drink the holy basil leaf tea for 4 weeks followed by placebo leaves for 4 weeks, or the reverse (the placebo leaves first, followed by the holy basil leaf tea). The authors concluded that holy basil leaf powder caused significant reduction in the level of fasting blood sugar and postprandial blood sugar, and a moderate reduction in cholesterol. The Jadad score for this trial is 1. This study was identified from the Western literature search.
Cinnamonum tamala. Chandola, Tripathi, and Udupa (1980) assessed the hypoglycemic effects of C tamala in type 2 diabetes patients.13 Thirty-two patients were recruited from the outpatient departments of the Institute of Medical Sciences, Varanasi, India, and received the intervention and 8 patients with type 2 diabetes served as controls. The socioeconomic characteristics of the patients were not noted, and the authors did not report if the 2 arms of patients were statistically equivalent on important prognostic variables at the start of the trial. The intervention consisted of leaves of C tamala (tejpatra) that were dried, pulverized, and filtered through a fine mesh, and given as 2 heaped teaspoons 4 times a day before meals and tea for a total of 1 month. All patients were advised to follow a 1800-calorie diet with restriction of sugar, potato, and rice. The control patients were only instructed to follow the above diet with no other medications. Fasting blood sugars were assessed in both arms of patients before the trial and at the end of 1 month. The authors reported the mean fasting blood sugar improved from 153 mg/dL to 113 mg/dL (P<.001) at the end of 1 month in patients treated with C tamala, while there was no improvement in control patients. The Jadad score for this study was 0. This study was identified from the Eastern literature search.
Coccina indica. Kamble, Jyotishi, Kamalakar, et al (1996) studied the effect of fresh leaves of C indica on blood sugar levels and on hyperlipidemia in noninsulin-dependent diabetes mellitus (NIDDM, type 2) patients at an Ayurvedic clinic in Nagpur, India.14 Patients were classified into 4 arms: a healthy comparison arm (arm I, 15 patients); a NIDDM comparison arm (arm II, 30 patients); NIDDM patients treated with Coccinia (arm III, 25 patients); and a NIDDM arm treated with chlorpropamide (arm IV, 15 patients). Patients were given the Coccinia (decocted from fresh leaves, dried into a paste, and made into a 3-g tablet) twice a day for 12 weeks, although control group data only exist at 6 weeks. For patients in arm III, the study showed a statistically significant reduction in mean fasting blood sugar, from 160 to 118 mg/dL (P<.001) at 12 weeks, and a significant decrease in blood sugar levels after glucose tolerance tests: the 2-hour level dropped from 308 mg/dL to 142 mg/dL (P<.001). These results were roughly equivalent to those found in the chlorpropamide arm at 6 weeks, with any differences being not statistically significant. Additionally, after 12 weeks of treatment, the Coccinia treated patients showed significant within group reductions in levels of cholesterol (P<.001), phospholipid (P<.05), triglyceride (P<.001), and free fatty acid (P<.001) compared with untreated patients with diabetes. The Jadad score for this study was 0. This study was identified from the Eastern literature search.
Jamun beej. Kohli and Singh (1993) studied the effects of Jamun beej (Eugenia jambolana) on fasting blood sugar, glucose tolerance test, and symptomatic relief of symptoms associated with diabetes.15 Thirty patients identified from the outpatient unit of the Sunderlal Hospital in Varanasi, India, who had NIDDM confirmed by glucose tolerance test, were given E jambolana crushed into a fine powder at a dose of 4 g 3 times a day for 3 months. No dietary restrictions were included in the study. A second arm of 6 patients with confirmed NIDDM was given chlorpropamide (250 mg/d). No demographic information was provided on these patients. The authors reported a statistically significant reduction in mean fasting blood sugar of 51.86 mg/dL at 2 months (P<.001) but not at 3 months. The study also demonstrated a significant reduction in the response to the glucose tolerance test at both 2 months (P<.001) and at 3 months (P<.01), but comparisons with the patients receiving chlorpropamide were not statistically significant. The Jadad score total is 1. This study was identified from the Eastern literature search.
Gymnema sylvestre. Baskaran, Ahamath, Shanmugasundaram, et al (1990) studied the effects of GS4, a specific isolate of G sylvestre, on the blood sugar of 47 type 2 diabetes patients.16 The intervention group consisted of 22 patients with diabetes on oral hypoglycemic therapy (continued during the trial), plus herbal therapy with Gymnema at a dose of 400 mg/d. The control group consisted of 25 patients with type 2 diabetes on conventional medications alone. Although the arms were reasonably matched for age and Broca index (percent of ideal body weight) based on our analysis of individual patient data in the study, the 2 arms were statistically different at baseline with respect to fasting blood sugar. The authors reported that in the intervention group at 12 months of follow-up, mean fasting blood sugar improved from 174 mg/dL to 124 mg/dL (P<.001) and Hb A1c improved from 11.9% to 8.48% (P<.001). Changes in the control group over this time were not significant. Virtually all patients in arm I developed hypoglycemic symptoms, and the dose of their normal oral hypoglycemic agent needed to be changed or stopped. The Jadad score is 0. This study was identified from the Western literature search.
GS4. Shanmugasundaram, Rajeswari, Baskaran, et al (1990b) reported the effect of an herbal compound GS4 on blood glucose, insulin requirements, and cholesterol in patients with type 1 and type 2 diabetes.17 The intervention group consisted of 23 type 1 patients and 4 type 2 patients (ages 44–50 years, 25% female) who continued their insulin in addition to taking the herbal intervention, and the control group consisted of 37 type 1 patients who were on insulin therapy. The clinical equivalence of the 2 arms at baseline was not mentioned. The intervention drug was GS4, a recrystallized precipitate of the alcoholic extract of the acidic fraction of G sylvestre; at dose of 400 mg/d. At 6 to 8 months of follow-up, all patients in the intervention group developed hypoglycemic episodes, and their insulin doses were reduced by 10 units at a time; differences compared to controls were statistically significant. The Jadad score was 1. This study was identified from the Western literature search.
Summary. In summary, comparisons of the studied herbs with either placebo, diet, or as an adjunct to medical hypoglycemic therapy consistently reported statistically significant benefits in glucose control. Studies comparing herbs to the oral hypoglycemic chlorpropamide did not report differences between groups.
FIGURE 2
Glucose-lowering effects of Ayurvedic herbs compared with nonherbal treatments
Case series or cohort studies without a concurrent comparison group
Fifteen studies had treatment arms that reported blood glucose or Hb A1c values before and after herbal interventions—ie, that made available pre/post data.13,18-31 Herbs were tested singly (7 studies), in combination (7 studies), or both singly and in combination (1 study). All of these studies are limited by the lack of randomization. Many are also limited by small sample size and short study duration.
The data are presented in FIGURE 3 in the following order: studies or arms of studies using a single herbal preparation first, followed by studies that use a formula or a group of herbs and minerals. Some studies with multiple arms will have listings in more than one place. As FIGURE 3 shows, most pre/post comparison studies using single herbs and formulas favor treatment. Hb A1c is measured in only 5 of the studies. Two of those studies seem to strongly favor treatment; 2 are almost equivocal; and 1 does not favor treatment.
The small number of RCTs/CCTs/natural experiments measuring postprandial blood glucose and Hb A1c, and the small number of case series and cohorts measuring Hb A1c, make the assessment of publication bias for these outcomes problematic. For the remaining outcomes, only slight evidence of publication bias was evident among the case series and cohort studies for the fasting blood glucose outcome (adjusted rank correlation test P=.97; regression asymmetry test P=.06). For this outcome, we have trial data available, a setting in which no evidence of publication bias is seen.
FIGURE 3
Effect of Ayurvedic herbs on blood glucose and Hb A1c
Discussion
No controlled trials have assessed Ayurveda as a system of care. Furthermore, among studies of herbal preparations, controlled trials are rare and mostly of poor quality. Still, we found evidence suggesting that some Ayurvedic herbs have clinically important hypoglycemic effects.
The best-quality RCT reported beneficial results for C indica. Other studies have generally reported benefits of C indica; however, results have been inconsistent.
A single trial of holy basil reported a benefit in controlling fasting blood glucose only. G sylvestre was used in a number of studies, again with generally beneficial results. Gymnema was also a constituent in 2 of the formulas that reported beneficial results: D-400 and Ayush-82.
Methodological shortcomings. The evidence we found falls short of proof. As noted, the individual studies we assessed had significant methodological shortcomings. Few used a randomized, placebo-controlled design, despite the feasibility of such methods. Studies generally were underpowered to determine even large effect sizes. Many studies involved an extremely small number of subjects (fewer than 10). A number of studies failed to use appropriate statistical methods in reporting the results. Furthermore, the duration of most studies was short, and only intermediate outcomes (measure of blood sugar control) were reported. Longer term studies that assess clinical outcomes are required. Lastly, there is great heterogeneity in the available literature on Ayurvedic treatment for diabetes, despite the fact that the overwhelming majority of studies test herbal therapy. Heterogeneity exists in the herbs and formulas tested and in the method of their preparation.
No true studies of Ayurveda. None of the identified studies assessed Ayurveda as a system of diagnosis and care. The literature reported mainly studies of single herbs; however, in clinical Ayurvedic practice, herbs are usually given in combination. Formulas can include minerals and metals in addition to multiple plants.
Ayurvedic practitioners assert that the sum of a formula is more potent than the constituents taken individually and, further, that the mineral and metal components boost the formula’s potency. Additional Ayurvedic therapies such as diet, yoga, or special purification routines, should be controlled for when recruiting and assessing patients. It is unclear, perhaps doubtful, that taking a single component of Ayurvedic is sufficient to represent the holistic effect of Ayurvedic interventions.
Limitations of our review. Our searches showed that herbal therapies were emphasized in published studies of Ayurveda. However, no conclusions can be drawn about the use of Ayurveda as a whole system for the treatment of diabetes. Although extensive efforts were made to obtain the relevant literature from India, studies not published in English were excluded, as were MD thesis reports. A handful of studies could not be obtained. Therefore we may not have included in this review all clinical trials. By specifically hand searching documents published in India, we identified that an important body of Ayurvedic literature is not identifiable using traditional systematic review methods.
In summary, we found preliminary evidence suggesting that some herbs and herbal formulas used in Ayurvedic therapy can have clinically important glucose-lowering effects. C indica, holy basil, and Gymnema are particularly worthy of additional study.
Acknowledgments
This research was performed by the Southern California Evidence-Based Practice Center based at RAND, Santa Monica, CA under contract with the Agency for Healthcare Research and Quality (Contract No. 290-97-0001) with support from the National Center for Complementary and Alternative Medicine. The authors of this article are responsible for its contents. No statement in this article should be construed as an official position of the Agency for Healthcare Research and Quality, the National Center for Complementary and Alternative Medicine, National Institutes of Health, or the US Department of Health and Human Services.
CORRESPONDING AUTHOR
Paul G. Shekelle, MD, PhD, West Los Angeles VA Medical Center, 111G, 11301 Wilshire Blvd, Los Angeles, CA 90073. E-mail: [email protected]. At the time of this study, Dr. Shekelle was a Senior Research Associate of the Veterans Affairs Health Services Research and Development Service.
1. Lad V. An introduction to Ayurveda. Altern Ther Health Med 1995;1:57-63.
2. Chopra A, Doiphode VV. Ayurvedic medicine. Core concept, therapeutic principles and current relevance. Med Clin North Am 2002;86:75-89.
3. Marles RJ, Farnsworth NR. Antidiabetic plants and their active constituents. Phytomedicine 1995;2:137-189.
4. Hardy M, Coulter I, Venuturupalli S, et al. Ayurvedic interventions for diabetes mellitus: a systematic review. Evidence Report/Technology Assessment No. 41. AHRQ Publication No. 01-E040; 2001.
5. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1-12.
6. Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408-412.
7. Moher D, Pham B, Jones A, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 1998;352:609-613.
8. Balk EM, Bonis PA, Moskowitz H, et al. Correlation of quality measures with estimates of treatment effect in meta-analyses of randomized controlled trials. JAMA 2002;287:2973-2982.
9. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088-1101.
10. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-634.
11. Azad Khan A, Akhtar S, Mahtab H. Coccinia indica in the treatment of patients with diabetes mellitus. Bangladesh Med Res Counc Bull 1979;5:60-66.
12. Agrawal P, Rai V, Singh RB. Randomized placebo-controlled single-blind trial of holy basil leaves in patients with non-insulin-dependent diabetes mellitus. Int J Clin Pharmacol Ther 1996;34:406-409.
13. Chandola HM, Tripathi SN, Udupa KH. Hypoglycaemic response of c. tamala in patients of maturity onset (insulin independent) diabetes. J Res Ayurveda Sidda 1980;1:275-290.
14. Kamble SM, Jyotishi GS, Kamalakar PL, Vaidya SM. Efficacy of coccinia indica w. & a. in diabetes mellitus. J Res Ayurveda and Sidda 1996;17(1–2):77-84.
15. Kohli KR, Singh RH. A clinical trial of jambu (eugenia jambolana) in non-insulin dependant diabetes mellitus. J Res Ayurveda Sidda 1993;14(3–4):89-97.
16. Baskaran K, Kizar Ahamath B, Radha Shanmugasundaram K, Shanmugasundaram ER. Antidiabetic effect of a leaf extract from gymnema sylvestre in non-insulin-dependent diabetes mellitus patients. J Ethnopharmacol 1990;30:295-300.
17. Shanmugasundaram E, Rajeswari G, Baskaran K, Rajesh Kumar BR, Radha Shanmugasundaram K, Kizar Ahmath B. Use of gymnema sylvestre leaf extract in the control of blood glucose in insulin-dependent diabetes mellitus. J Ethnopharmacol 1990;30:281-294.
18. Kuppurajan K, Seshadri C, Revathi R. Hypoglycaemic effect of coccinia indica in diabetes mellitus. Nagarjun 1986;29:1-4.
19. Kuppurajan K, Srivatsa A, Krishnaswami CV. Hypoglycemic and hypotriglyceridemic effects of methika churna (fenugreek). Antiseptic 1998;95:78-79.
20. Kumar N, Kumar A, Sharma ML. Clinical evaluation of single and herbo-mineral compound drugs in the management of madhumeha. J Res Ayurveda Sidda 1999;20(1–2):1-9.
21. Sharma RD, et al. Use of fenugreek seed powder in the management of non-insulin dependent diabetes mellitus. Nutr Res 1996;16:1331-1339.
22. Flexible dose open trial of Vijayasar in cases of newly-diagnosed non-insulin-dependent diabetes mellitus. Indian Council of Medical Research (ICMR), Collaborating Centres, New Delhi. Indian J Med Res 1998;108:24-29.
23. Goyal DK, Tiwari SK. Study on sadabahar (vinca rosea linn.) In madhumeha (diabetes mellitus). J Res Ayurveda Sidda 1999;20(1–2):93-100.
24. Chowdhary DP, Dua M, Bharti, Kishore P. Hypoglycaemic effect of a coded formulation: aysuh-82. J Res Ayurveda Sidda 1998;19(3–4):107-115.
25. Pandey VN, Rajagopalan SS, Chowdhary DP. An effective ayurvedic hypoglycemic formulation. J Res Ayurveda Sidda 1995;16(1–2):1-14.
26. Shankar R, Singhal R. Clinical studies of the effect of abraga (mica) chendooram in the treatment of diabetes mellitus (neerazhivu). J Res Ayurveda Sidda 1995;16(3–4):108-117.
27. Maji D, Singh AK. Clinical trial of D-400, a herbomineral preparation in diabetes mellitus. J Diabetic Assoc India 1995;35:1-4.
28. Sircar AR, Ahuja RC, Natu SM, Roy B, Sharma HM. Hypoglycemic, hypolipidemic and general beneficial effects of an herbal mixture MA-471. Alternat Ther Clin Pract 1996;3:26-31.
29. Shankar R, Sighal R. Clinical assessment of the effects of sandana (sandal) podi-a in the treatment of diabetes mellitus (neerazhiv). J Res Ayurveda Sidda 1994;15(3–4):89-97.
30. Sivaprakasam K, Rao KK, Yasodha R, Veluchamy G. Siddha remedy for diabetes mellitus. J Res Ayurveda Sidda 1984;5(1–4):25-32.
31. Kamble SM, Kamlakar PL, Vaidya S, Bambole VD. Influence of coccinia indica on certain enzymes in glycolytic and lipolytic pathway in human diabetes. Indian J Med Sci 1998;52:143-146.
32. Kapoor LD. CRC Handbook of Ayurvedic Medicinal Plants. Boca Raton, Fla: CRC Press; 1990.
33. Dash VB. Materia Medica of Indo-Tibetan Medicine. Delhi, India: MDIA Classics India; 1987;10-11.
34. Mishra L, Singh B, Dagenais S. Ayurveda: a historical perspective and principles of the traditional healthcare system in India. Altern Ther Health Med 2001;7:36-42.
1. Lad V. An introduction to Ayurveda. Altern Ther Health Med 1995;1:57-63.
2. Chopra A, Doiphode VV. Ayurvedic medicine. Core concept, therapeutic principles and current relevance. Med Clin North Am 2002;86:75-89.
3. Marles RJ, Farnsworth NR. Antidiabetic plants and their active constituents. Phytomedicine 1995;2:137-189.
4. Hardy M, Coulter I, Venuturupalli S, et al. Ayurvedic interventions for diabetes mellitus: a systematic review. Evidence Report/Technology Assessment No. 41. AHRQ Publication No. 01-E040; 2001.
5. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1-12.
6. Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408-412.
7. Moher D, Pham B, Jones A, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 1998;352:609-613.
8. Balk EM, Bonis PA, Moskowitz H, et al. Correlation of quality measures with estimates of treatment effect in meta-analyses of randomized controlled trials. JAMA 2002;287:2973-2982.
9. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088-1101.
10. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-634.
11. Azad Khan A, Akhtar S, Mahtab H. Coccinia indica in the treatment of patients with diabetes mellitus. Bangladesh Med Res Counc Bull 1979;5:60-66.
12. Agrawal P, Rai V, Singh RB. Randomized placebo-controlled single-blind trial of holy basil leaves in patients with non-insulin-dependent diabetes mellitus. Int J Clin Pharmacol Ther 1996;34:406-409.
13. Chandola HM, Tripathi SN, Udupa KH. Hypoglycaemic response of c. tamala in patients of maturity onset (insulin independent) diabetes. J Res Ayurveda Sidda 1980;1:275-290.
14. Kamble SM, Jyotishi GS, Kamalakar PL, Vaidya SM. Efficacy of coccinia indica w. & a. in diabetes mellitus. J Res Ayurveda and Sidda 1996;17(1–2):77-84.
15. Kohli KR, Singh RH. A clinical trial of jambu (eugenia jambolana) in non-insulin dependant diabetes mellitus. J Res Ayurveda Sidda 1993;14(3–4):89-97.
16. Baskaran K, Kizar Ahamath B, Radha Shanmugasundaram K, Shanmugasundaram ER. Antidiabetic effect of a leaf extract from gymnema sylvestre in non-insulin-dependent diabetes mellitus patients. J Ethnopharmacol 1990;30:295-300.
17. Shanmugasundaram E, Rajeswari G, Baskaran K, Rajesh Kumar BR, Radha Shanmugasundaram K, Kizar Ahmath B. Use of gymnema sylvestre leaf extract in the control of blood glucose in insulin-dependent diabetes mellitus. J Ethnopharmacol 1990;30:281-294.
18. Kuppurajan K, Seshadri C, Revathi R. Hypoglycaemic effect of coccinia indica in diabetes mellitus. Nagarjun 1986;29:1-4.
19. Kuppurajan K, Srivatsa A, Krishnaswami CV. Hypoglycemic and hypotriglyceridemic effects of methika churna (fenugreek). Antiseptic 1998;95:78-79.
20. Kumar N, Kumar A, Sharma ML. Clinical evaluation of single and herbo-mineral compound drugs in the management of madhumeha. J Res Ayurveda Sidda 1999;20(1–2):1-9.
21. Sharma RD, et al. Use of fenugreek seed powder in the management of non-insulin dependent diabetes mellitus. Nutr Res 1996;16:1331-1339.
22. Flexible dose open trial of Vijayasar in cases of newly-diagnosed non-insulin-dependent diabetes mellitus. Indian Council of Medical Research (ICMR), Collaborating Centres, New Delhi. Indian J Med Res 1998;108:24-29.
23. Goyal DK, Tiwari SK. Study on sadabahar (vinca rosea linn.) In madhumeha (diabetes mellitus). J Res Ayurveda Sidda 1999;20(1–2):93-100.
24. Chowdhary DP, Dua M, Bharti, Kishore P. Hypoglycaemic effect of a coded formulation: aysuh-82. J Res Ayurveda Sidda 1998;19(3–4):107-115.
25. Pandey VN, Rajagopalan SS, Chowdhary DP. An effective ayurvedic hypoglycemic formulation. J Res Ayurveda Sidda 1995;16(1–2):1-14.
26. Shankar R, Singhal R. Clinical studies of the effect of abraga (mica) chendooram in the treatment of diabetes mellitus (neerazhivu). J Res Ayurveda Sidda 1995;16(3–4):108-117.
27. Maji D, Singh AK. Clinical trial of D-400, a herbomineral preparation in diabetes mellitus. J Diabetic Assoc India 1995;35:1-4.
28. Sircar AR, Ahuja RC, Natu SM, Roy B, Sharma HM. Hypoglycemic, hypolipidemic and general beneficial effects of an herbal mixture MA-471. Alternat Ther Clin Pract 1996;3:26-31.
29. Shankar R, Sighal R. Clinical assessment of the effects of sandana (sandal) podi-a in the treatment of diabetes mellitus (neerazhiv). J Res Ayurveda Sidda 1994;15(3–4):89-97.
30. Sivaprakasam K, Rao KK, Yasodha R, Veluchamy G. Siddha remedy for diabetes mellitus. J Res Ayurveda Sidda 1984;5(1–4):25-32.
31. Kamble SM, Kamlakar PL, Vaidya S, Bambole VD. Influence of coccinia indica on certain enzymes in glycolytic and lipolytic pathway in human diabetes. Indian J Med Sci 1998;52:143-146.
32. Kapoor LD. CRC Handbook of Ayurvedic Medicinal Plants. Boca Raton, Fla: CRC Press; 1990.
33. Dash VB. Materia Medica of Indo-Tibetan Medicine. Delhi, India: MDIA Classics India; 1987;10-11.
34. Mishra L, Singh B, Dagenais S. Ayurveda: a historical perspective and principles of the traditional healthcare system in India. Altern Ther Health Med 2001;7:36-42.