User login
Reality of Night Shifts: How to Stay Sharp and Healthy
Laura Vater remembers sneaking into her home after 12-hour night shifts during medical training while her husband distracted their toddler. The stealthy tag-teaming effort helped her get enough undisturbed sleep before returning to an Indiana University hospital the following night to repeat the pattern.
“He would pretend to take out the trash when I pulled in,” said Vater, MD, now a gastrointestinal oncologist and assistant professor of medicine at IU Health Simon Cancer Center in Indianapolis. “I would sneak in so she [their daughter] wouldn’t see me, and then he would go back in.”
For Vater, prioritizing sleep during the day to combat sleep deprivation common among doctors-in-training on night shifts required enlisting a supportive spouse. It’s just one of the tips she and a few chief residents shared with this news organization for staying sharp and healthy during overnight rotations.
While the pace of patient rounds may slow from the frenetic daytime rush, training as a doctor after the sun goes down can be quite challenging for residents, they told this news organization. From sleep deprivation working while the rest of us slumbers to the after-effects of late-night caffeine, learning to manage night rotations requires a balance of preparation and attention to personal health while caring for others, the residents and adviser said.
Compromised sleep is one of the biggest hurdles residents have to overcome. Sleep loss comes with risks to cardiovascular disease and type 2 diabetes, among other heath conditions, according to Medscape Medical News reports. And night shift workers who sleep 6 or fewer hours a night have at least one sleep disorder.
Sleep deprivation associated with overnight call schedules also can worsen a resident’s mood and motivation while impairing their judgment, leading to medical errors, according to a new study published in JAMA Open Network. The study proposed shorter consecutive night shifts and naps as ways to offset the results of sleep loss, especially for interns or first-year residents.
Residency programs recently have been experimenting with shorter call schedules.
Catching Zzs
Working the night shift demands a disciplined sleep schedule, said Nat deQuillfeldt, MD, a Denver Health chief resident in the University of Colorado’s internal medicine residency program.
“When I was on night admissions, I was very strict about going to sleep at 8 AM and waking at 3 PM every single day. It can be very tempting to try to stay up and spend time with loved ones, but my husband and I both prioritized my physical well-being for those weeks,” said deQuillfeldt, a PGY-4 resident. “It was especially challenging for me because I had to commute about 50 minutes each way and without such a rigid schedule I would have struggled to be on time.”
deQuillfeldt doesn’t have young children at home, a noisy community, or other distractions to interrupt sleep during the day. But it was still difficult for her to sleep while the sun was out. “I used an eye mask and ear plugs but definitely woke up more often than I would at night.”
Blackout curtains may have helped, she added.
“Without adequate sleep, your clinical thinking is not as sharp. When emergencies happen overnight, you’re often the first person to arrive and need to be able to make rapid, accurate assessments and decisions.”
As a chief resident, she chooses never to sleep during night shifts.
“I personally didn’t want to leave my interns alone or make them feel like they were waking me up or bothering me if they needed help, and I also didn’t want to be groggy in case of a rapid response or code blue.”
But napping on night shift is definitely possible, deQuillfeldt said. Between following up on overnight lab results, answering nurses’ questions, and responding to emergencies, she found downtime on night shift to eat and hydrate. She believes others can catch an hour or 2 of shut eye, even if they work in the intensive care unit, or 3-4 hours on rare quiet nights.
Vater suggests residents transitioning from daytime work to night shift prepare by trying to catch an afternoon nap, staying up later the night before the change, and banking sleep hours in advance.
When he knows he’s starting night shifts, Apurva Popat, MD, said he tries to go to sleep an hour or so later nights before to avoid becoming sleep deprived. The chief resident of internal medicine at Marshfield Clinic Health System in Marshfield, Wisconsin, doesn’t recommend sleeping during the night shift.
“I typically try not to sleep, even if I have time, so I can go home and sleep later in the morning,” said Popat, a PGY-3 resident.
To help him snooze, he uses blackout curtains and a fan to block out noise. His wife, a first-year internal medicine intern, often works a different shift, so she helps set up his sleeping environment and he reciprocates when it’s her turn for night shifts.
Some interns may need to catch a 20- to 30-minute nap on the first night shift, he said.
Popat also seeks out brighter areas of the hospital, such as the emergency department, where there are more people and colleagues to keep him alert.
Bypass Vending Machines
Lack of sleep makes it even more difficult to eat healthy on night shift, said Vater, who advises residents about wellness issues at IU and on social media.
“When you are sleep deprived, when you do not get enough sleep, you eat but you don’t feel full,” she said. “It’s hard to eat well on night shift. It’s harder if you go to the break room and there’s candy and junk food.”
Vater said that, as a resident, she brought a lunch bag to the hospital during night shifts. “I never had time to prep food, so I’d bring a whole apple, a whole orange, a whole avocado or nuts. It allowed me to eat more fruits and vegetables than I normally would.”
She advises caution when considering coffee to stay awake, especially after about 9 PM, which could interfere with sleep residents need later when they finish their shifts. Caffeine may help in the moment, but it prevents deep sleep, Vater said. So when residents finally get sleep after their shifts, they may wake up feeling tired, she said.
To avoid sleepiness, Popat brings protein shakes with him to night shifts. They stave off sugar spikes and keep his energy level high, he said. He might have a protein shake and fruit before he leaves home and carry his vegetarian dinner with him to eat in the early morning hours when the hospital is calm.
Eating small and frequent meals also helps ward off sleepiness, deQuillfeldt said.
Take the Stairs
Trying to stay healthy on night shifts, Vater also checked on patients by taking the stairs. “I’d set the timer on my phone for 30 minutes and if I got paged at 15, I’d pause the timer and reset it if I had a moment later. I’d get at least 30 minutes in, although not always continuous. I think some activity is better than none.”
Vater said her hospital had a gym, but it wasn’t practical for her because it was further away from where she worked. “Sometimes my coresidents would be more creative, and we would do squats.”
Popat tries to lift weights 2 hours before his night shift, but he also takes short walks between patients’ rooms in the early morning hours when it’s quietest. He also promotes deep breathing to stay alert.
Ask for a Ride
Vater urges those coming off night shifts, especially those transitioning for the first time from daytime rotations, not to drive if they’re exhausted. “Get an Uber. ... Make sure you get a ride home.”
The CU residency program covers the cost of a ridesharing service when doctors-in-training are too tired to drive home, deQuillfeldt said. “We really try to encourage people to use this to reduce the risk of car accidents.”
Promoting Mental Health
The residency program also links residents with primary care and mental health services. People who really struggle with shift work sleep disorder may qualify for medications to help them stay awake overnight, in addition to sleep hygiene apps and sleep aides.
“Night shifts can put a strain on mental health, especially when you’re only working, eating, and sleeping and not spending any time with family and friends,” deQuillfeldt said. “My husband works late afternoons, so we often would go weeks seeing each other for 15-20 minutes a day.”
“Sleeping when the sun is out often leads to a lack of light exposure which can compound the problem. Seeking mental health support early is really important to avoiding burnout,” she said.
She also recommended planning a fun weekend activity, trip, or celebration with friends or family after night shifts end “so you have something to look forward to…It’s so important to have a light at the end of the tunnel, which will allow you to enjoy the sense of accomplishment even more.”
For more advice on the subject, consider the American Medical Association guide to managing sleep deprivation in residency or Laura Vater’s tips for night shifts.
A version of this article first appeared on Medscape.com.
Laura Vater remembers sneaking into her home after 12-hour night shifts during medical training while her husband distracted their toddler. The stealthy tag-teaming effort helped her get enough undisturbed sleep before returning to an Indiana University hospital the following night to repeat the pattern.
“He would pretend to take out the trash when I pulled in,” said Vater, MD, now a gastrointestinal oncologist and assistant professor of medicine at IU Health Simon Cancer Center in Indianapolis. “I would sneak in so she [their daughter] wouldn’t see me, and then he would go back in.”
For Vater, prioritizing sleep during the day to combat sleep deprivation common among doctors-in-training on night shifts required enlisting a supportive spouse. It’s just one of the tips she and a few chief residents shared with this news organization for staying sharp and healthy during overnight rotations.
While the pace of patient rounds may slow from the frenetic daytime rush, training as a doctor after the sun goes down can be quite challenging for residents, they told this news organization. From sleep deprivation working while the rest of us slumbers to the after-effects of late-night caffeine, learning to manage night rotations requires a balance of preparation and attention to personal health while caring for others, the residents and adviser said.
Compromised sleep is one of the biggest hurdles residents have to overcome. Sleep loss comes with risks to cardiovascular disease and type 2 diabetes, among other heath conditions, according to Medscape Medical News reports. And night shift workers who sleep 6 or fewer hours a night have at least one sleep disorder.
Sleep deprivation associated with overnight call schedules also can worsen a resident’s mood and motivation while impairing their judgment, leading to medical errors, according to a new study published in JAMA Open Network. The study proposed shorter consecutive night shifts and naps as ways to offset the results of sleep loss, especially for interns or first-year residents.
Residency programs recently have been experimenting with shorter call schedules.
Catching Zzs
Working the night shift demands a disciplined sleep schedule, said Nat deQuillfeldt, MD, a Denver Health chief resident in the University of Colorado’s internal medicine residency program.
“When I was on night admissions, I was very strict about going to sleep at 8 AM and waking at 3 PM every single day. It can be very tempting to try to stay up and spend time with loved ones, but my husband and I both prioritized my physical well-being for those weeks,” said deQuillfeldt, a PGY-4 resident. “It was especially challenging for me because I had to commute about 50 minutes each way and without such a rigid schedule I would have struggled to be on time.”
deQuillfeldt doesn’t have young children at home, a noisy community, or other distractions to interrupt sleep during the day. But it was still difficult for her to sleep while the sun was out. “I used an eye mask and ear plugs but definitely woke up more often than I would at night.”
Blackout curtains may have helped, she added.
“Without adequate sleep, your clinical thinking is not as sharp. When emergencies happen overnight, you’re often the first person to arrive and need to be able to make rapid, accurate assessments and decisions.”
As a chief resident, she chooses never to sleep during night shifts.
“I personally didn’t want to leave my interns alone or make them feel like they were waking me up or bothering me if they needed help, and I also didn’t want to be groggy in case of a rapid response or code blue.”
But napping on night shift is definitely possible, deQuillfeldt said. Between following up on overnight lab results, answering nurses’ questions, and responding to emergencies, she found downtime on night shift to eat and hydrate. She believes others can catch an hour or 2 of shut eye, even if they work in the intensive care unit, or 3-4 hours on rare quiet nights.
Vater suggests residents transitioning from daytime work to night shift prepare by trying to catch an afternoon nap, staying up later the night before the change, and banking sleep hours in advance.
When he knows he’s starting night shifts, Apurva Popat, MD, said he tries to go to sleep an hour or so later nights before to avoid becoming sleep deprived. The chief resident of internal medicine at Marshfield Clinic Health System in Marshfield, Wisconsin, doesn’t recommend sleeping during the night shift.
“I typically try not to sleep, even if I have time, so I can go home and sleep later in the morning,” said Popat, a PGY-3 resident.
To help him snooze, he uses blackout curtains and a fan to block out noise. His wife, a first-year internal medicine intern, often works a different shift, so she helps set up his sleeping environment and he reciprocates when it’s her turn for night shifts.
Some interns may need to catch a 20- to 30-minute nap on the first night shift, he said.
Popat also seeks out brighter areas of the hospital, such as the emergency department, where there are more people and colleagues to keep him alert.
Bypass Vending Machines
Lack of sleep makes it even more difficult to eat healthy on night shift, said Vater, who advises residents about wellness issues at IU and on social media.
“When you are sleep deprived, when you do not get enough sleep, you eat but you don’t feel full,” she said. “It’s hard to eat well on night shift. It’s harder if you go to the break room and there’s candy and junk food.”
Vater said that, as a resident, she brought a lunch bag to the hospital during night shifts. “I never had time to prep food, so I’d bring a whole apple, a whole orange, a whole avocado or nuts. It allowed me to eat more fruits and vegetables than I normally would.”
She advises caution when considering coffee to stay awake, especially after about 9 PM, which could interfere with sleep residents need later when they finish their shifts. Caffeine may help in the moment, but it prevents deep sleep, Vater said. So when residents finally get sleep after their shifts, they may wake up feeling tired, she said.
To avoid sleepiness, Popat brings protein shakes with him to night shifts. They stave off sugar spikes and keep his energy level high, he said. He might have a protein shake and fruit before he leaves home and carry his vegetarian dinner with him to eat in the early morning hours when the hospital is calm.
Eating small and frequent meals also helps ward off sleepiness, deQuillfeldt said.
Take the Stairs
Trying to stay healthy on night shifts, Vater also checked on patients by taking the stairs. “I’d set the timer on my phone for 30 minutes and if I got paged at 15, I’d pause the timer and reset it if I had a moment later. I’d get at least 30 minutes in, although not always continuous. I think some activity is better than none.”
Vater said her hospital had a gym, but it wasn’t practical for her because it was further away from where she worked. “Sometimes my coresidents would be more creative, and we would do squats.”
Popat tries to lift weights 2 hours before his night shift, but he also takes short walks between patients’ rooms in the early morning hours when it’s quietest. He also promotes deep breathing to stay alert.
Ask for a Ride
Vater urges those coming off night shifts, especially those transitioning for the first time from daytime rotations, not to drive if they’re exhausted. “Get an Uber. ... Make sure you get a ride home.”
The CU residency program covers the cost of a ridesharing service when doctors-in-training are too tired to drive home, deQuillfeldt said. “We really try to encourage people to use this to reduce the risk of car accidents.”
Promoting Mental Health
The residency program also links residents with primary care and mental health services. People who really struggle with shift work sleep disorder may qualify for medications to help them stay awake overnight, in addition to sleep hygiene apps and sleep aides.
“Night shifts can put a strain on mental health, especially when you’re only working, eating, and sleeping and not spending any time with family and friends,” deQuillfeldt said. “My husband works late afternoons, so we often would go weeks seeing each other for 15-20 minutes a day.”
“Sleeping when the sun is out often leads to a lack of light exposure which can compound the problem. Seeking mental health support early is really important to avoiding burnout,” she said.
She also recommended planning a fun weekend activity, trip, or celebration with friends or family after night shifts end “so you have something to look forward to…It’s so important to have a light at the end of the tunnel, which will allow you to enjoy the sense of accomplishment even more.”
For more advice on the subject, consider the American Medical Association guide to managing sleep deprivation in residency or Laura Vater’s tips for night shifts.
A version of this article first appeared on Medscape.com.
Laura Vater remembers sneaking into her home after 12-hour night shifts during medical training while her husband distracted their toddler. The stealthy tag-teaming effort helped her get enough undisturbed sleep before returning to an Indiana University hospital the following night to repeat the pattern.
“He would pretend to take out the trash when I pulled in,” said Vater, MD, now a gastrointestinal oncologist and assistant professor of medicine at IU Health Simon Cancer Center in Indianapolis. “I would sneak in so she [their daughter] wouldn’t see me, and then he would go back in.”
For Vater, prioritizing sleep during the day to combat sleep deprivation common among doctors-in-training on night shifts required enlisting a supportive spouse. It’s just one of the tips she and a few chief residents shared with this news organization for staying sharp and healthy during overnight rotations.
While the pace of patient rounds may slow from the frenetic daytime rush, training as a doctor after the sun goes down can be quite challenging for residents, they told this news organization. From sleep deprivation working while the rest of us slumbers to the after-effects of late-night caffeine, learning to manage night rotations requires a balance of preparation and attention to personal health while caring for others, the residents and adviser said.
Compromised sleep is one of the biggest hurdles residents have to overcome. Sleep loss comes with risks to cardiovascular disease and type 2 diabetes, among other heath conditions, according to Medscape Medical News reports. And night shift workers who sleep 6 or fewer hours a night have at least one sleep disorder.
Sleep deprivation associated with overnight call schedules also can worsen a resident’s mood and motivation while impairing their judgment, leading to medical errors, according to a new study published in JAMA Open Network. The study proposed shorter consecutive night shifts and naps as ways to offset the results of sleep loss, especially for interns or first-year residents.
Residency programs recently have been experimenting with shorter call schedules.
Catching Zzs
Working the night shift demands a disciplined sleep schedule, said Nat deQuillfeldt, MD, a Denver Health chief resident in the University of Colorado’s internal medicine residency program.
“When I was on night admissions, I was very strict about going to sleep at 8 AM and waking at 3 PM every single day. It can be very tempting to try to stay up and spend time with loved ones, but my husband and I both prioritized my physical well-being for those weeks,” said deQuillfeldt, a PGY-4 resident. “It was especially challenging for me because I had to commute about 50 minutes each way and without such a rigid schedule I would have struggled to be on time.”
deQuillfeldt doesn’t have young children at home, a noisy community, or other distractions to interrupt sleep during the day. But it was still difficult for her to sleep while the sun was out. “I used an eye mask and ear plugs but definitely woke up more often than I would at night.”
Blackout curtains may have helped, she added.
“Without adequate sleep, your clinical thinking is not as sharp. When emergencies happen overnight, you’re often the first person to arrive and need to be able to make rapid, accurate assessments and decisions.”
As a chief resident, she chooses never to sleep during night shifts.
“I personally didn’t want to leave my interns alone or make them feel like they were waking me up or bothering me if they needed help, and I also didn’t want to be groggy in case of a rapid response or code blue.”
But napping on night shift is definitely possible, deQuillfeldt said. Between following up on overnight lab results, answering nurses’ questions, and responding to emergencies, she found downtime on night shift to eat and hydrate. She believes others can catch an hour or 2 of shut eye, even if they work in the intensive care unit, or 3-4 hours on rare quiet nights.
Vater suggests residents transitioning from daytime work to night shift prepare by trying to catch an afternoon nap, staying up later the night before the change, and banking sleep hours in advance.
When he knows he’s starting night shifts, Apurva Popat, MD, said he tries to go to sleep an hour or so later nights before to avoid becoming sleep deprived. The chief resident of internal medicine at Marshfield Clinic Health System in Marshfield, Wisconsin, doesn’t recommend sleeping during the night shift.
“I typically try not to sleep, even if I have time, so I can go home and sleep later in the morning,” said Popat, a PGY-3 resident.
To help him snooze, he uses blackout curtains and a fan to block out noise. His wife, a first-year internal medicine intern, often works a different shift, so she helps set up his sleeping environment and he reciprocates when it’s her turn for night shifts.
Some interns may need to catch a 20- to 30-minute nap on the first night shift, he said.
Popat also seeks out brighter areas of the hospital, such as the emergency department, where there are more people and colleagues to keep him alert.
Bypass Vending Machines
Lack of sleep makes it even more difficult to eat healthy on night shift, said Vater, who advises residents about wellness issues at IU and on social media.
“When you are sleep deprived, when you do not get enough sleep, you eat but you don’t feel full,” she said. “It’s hard to eat well on night shift. It’s harder if you go to the break room and there’s candy and junk food.”
Vater said that, as a resident, she brought a lunch bag to the hospital during night shifts. “I never had time to prep food, so I’d bring a whole apple, a whole orange, a whole avocado or nuts. It allowed me to eat more fruits and vegetables than I normally would.”
She advises caution when considering coffee to stay awake, especially after about 9 PM, which could interfere with sleep residents need later when they finish their shifts. Caffeine may help in the moment, but it prevents deep sleep, Vater said. So when residents finally get sleep after their shifts, they may wake up feeling tired, she said.
To avoid sleepiness, Popat brings protein shakes with him to night shifts. They stave off sugar spikes and keep his energy level high, he said. He might have a protein shake and fruit before he leaves home and carry his vegetarian dinner with him to eat in the early morning hours when the hospital is calm.
Eating small and frequent meals also helps ward off sleepiness, deQuillfeldt said.
Take the Stairs
Trying to stay healthy on night shifts, Vater also checked on patients by taking the stairs. “I’d set the timer on my phone for 30 minutes and if I got paged at 15, I’d pause the timer and reset it if I had a moment later. I’d get at least 30 minutes in, although not always continuous. I think some activity is better than none.”
Vater said her hospital had a gym, but it wasn’t practical for her because it was further away from where she worked. “Sometimes my coresidents would be more creative, and we would do squats.”
Popat tries to lift weights 2 hours before his night shift, but he also takes short walks between patients’ rooms in the early morning hours when it’s quietest. He also promotes deep breathing to stay alert.
Ask for a Ride
Vater urges those coming off night shifts, especially those transitioning for the first time from daytime rotations, not to drive if they’re exhausted. “Get an Uber. ... Make sure you get a ride home.”
The CU residency program covers the cost of a ridesharing service when doctors-in-training are too tired to drive home, deQuillfeldt said. “We really try to encourage people to use this to reduce the risk of car accidents.”
Promoting Mental Health
The residency program also links residents with primary care and mental health services. People who really struggle with shift work sleep disorder may qualify for medications to help them stay awake overnight, in addition to sleep hygiene apps and sleep aides.
“Night shifts can put a strain on mental health, especially when you’re only working, eating, and sleeping and not spending any time with family and friends,” deQuillfeldt said. “My husband works late afternoons, so we often would go weeks seeing each other for 15-20 minutes a day.”
“Sleeping when the sun is out often leads to a lack of light exposure which can compound the problem. Seeking mental health support early is really important to avoiding burnout,” she said.
She also recommended planning a fun weekend activity, trip, or celebration with friends or family after night shifts end “so you have something to look forward to…It’s so important to have a light at the end of the tunnel, which will allow you to enjoy the sense of accomplishment even more.”
For more advice on the subject, consider the American Medical Association guide to managing sleep deprivation in residency or Laura Vater’s tips for night shifts.
A version of this article first appeared on Medscape.com.
Residency to Reality: The Job Outlook for New Docs
Roshan Bransden didn’t count how many job offers she received during her recently completed training in family medicine. “It was pretty nonstop throughout all of my PGY-3 year,” she said.
Most of the job opportunities were different from the type of position she sought or where she wanted to work. Bransden graduated from residency at Montefiore Hospital in New York and accepted a position as a primary care doctor in Miami, close to where she grew up and where her family lives.
More than half (56%) of all residents in AMN Healthcare’s 2023 Survey of Final-Year Medical Residents received 100 or more job solicitations during their training, the highest figure since the survey began more than 30 years ago, the staffing agency reported.
Employers are recruiting residents earlier, offering residency stipends of $1500 to $2500 up to 18 months before they finish their training if they commit to an employment contract, said Leah Grant, president of AMN Healthcare’s Physician Permanent Solutions division, specializing in doctor recruitment. She said that the company’s clients are already eyeing residents completing their training in 2026.
“The key for residents is not about finding a position but choosing the right one out of many.” Grant added that residents typically aren’t taught negotiation skills or how to evaluate job offers. They tend to choose a position based on location, but they should also consider work–life balance issues such as call schedules and whether incentives such as signing bonuses, relocation allowances, and student loan reimbursement offset the job’s time commitment.
“If you are a physician and you are willing to go anywhere, you will have hundreds of opportunities,” said Tibor Nagy, DO, an emergency medicine fellow who recently searched for jobs. “It depends on what they want out of their careers.”
Location Is a Key Consideration
Nagy said he had fewer options because he was limited by location, staying close to where his wife is finishing her internal medicine residency. He is completing his fellowship at Atrium Health Carolinas Medical Center in Charlotte, North Carolina, and preparing to return to Prisma Health in Greenville, South Carolina, where he did his residency.
He said that the job search was easier than he anticipated considering the tight market following a job report from the American College of Emergency Physicians in 2021 that predicted an oversupply of 8000 emergency medicine physicians by 2030.
Halfway through Nagy’s residency, he sought a fellowship in emergency medical services (EMS) to be more competitive in the job market. After that, “Every door I knocked on was open to hiring. Maybe it’s a regional thing. They were happy to interview me.”
In addition to location, Nagy’s top priorities when choosing a job were stability and being able to use his EMS fellowship to become a medical director of an EMS system, agency, or fire department. He wanted to work for a hospital system with an academic focus without much employee turnover.
Salary vs Benefits
AMN Healthcare received the most physician searches for family medicine doctors, followed by OB/GYNs. The staffing agency reported that close to two thirds (63%) of its search engagements during the 2023-2024 review period were for specialists, reflecting the needs of an aging population.
The highest average starting salaries were for surgical and internal medicine subspecialties, according to AMN Healthcare’s 2024 Physician and Advanced Practitioner Recruiting Incentives. Orthopedic surgery averaged $633,000; urology, $540,000; gastroenterology, $506,000; and pulmonary medicine, $418,000. For comparison, the average starting salaries for primary care doctors were family medicine, $255,000; internal medicine, $255,000; and pediatrics, $233,000.
In addition to starting salaries, many physicians receive signing bonuses, relocation allowances, and continuing medical education (CME) allowances. According to the report, the average signing bonus for physicians was $31,473. The average relocation allowance for physicians was $11,284 and the average CME allowance was $3969.
Salary wasn’t Nagy’s top priority when choosing a job, though he admits that the ability to pay back thousands of dollars in medical school loans will be helpful. Instead of focusing on higher pay to offset student loans, Nagy said he sought nonprofit positions to help him qualify for public service loan forgiveness.
The federal program forgives loan balances after the recipient makes monthly payments for 10 years while working for a government or nonprofit organization. He also racked up 3 years of residency and his fellowship year at nonprofit hospitals toward that commitment.
He said jobs that pay more may require doctors to see more patients. “The hustle may be different. There are definitely tradeoffs,” he said.
Bransden said the position she begins in January will allow her to work part-time with full benefits, among other perks. “My employer is a membership-based practice, so I’ll be able to gift a few memberships to family and friends.”
Going Solo
Mohammad Ibrahim, DO, is among a minority of new physicians who have chosen to set up their own practice.
Only 6% of residents in AMN Healthcare’s 2024 report indicated that a solo practice was among their top two choices, while 20% listed partnering with another physician.
Ibrahim is a sports medicine fellow at the University of Michigan Health-West in Wyoming, after finishing his family medicine residency at Trinity Health Livingston Hospital in Howell, Michigan.
After his fellowship ends, he said he plans to stay in Michigan, where his family lives.
Ibrahim said he began his medical education knowing he wanted to become a solo clinician in private practice. He sees it as a way to have more control over his decisions about patient care and business practices.
Working in a hospital often requires doctors to gain approval from several levels of authority for decisions such as ordering new equipment or forgiving part of a service payment. He also wanted to set his schedule to take Friday afternoons off for Muslim prayer.
Although he realizes the challenges of starting a private practice, Ibrahim said those who go through graduate medical education can figure out how to adapt and overcome any obstacles. “I think it’s more doable than we are led to believe.”
He said that if more residents were exposed to private practice, they might pursue that path. During his training, Ibrahim did a rotation with a private practice physician. “It’s nice to see people proud of what they built, what they contributed.”
Most residents don’t choose private practice. In the AMN Healthcare survey, 68% of residents said that employment by a hospital was among their top two choices for a practice setting, 42% said employment by a single-specialty group, and 32%, employment by a multispecialty group.
Of the majority of job searches AMN Healthcare conducted, 28% were to fill positions in hospital settings, followed by 26% for medical groups, 22% for academic medical centers, 13% for urgent care centers and retail clinics, 6% for solo practices, partnerships, or concierge practice settings, and 5% for Federally Qualified Health Centers/Community Health Centers or Indian Health facilities.
Still, the report noted an increase in recruiting for independent medical practice ownership, which dwindled in recent years, with the majority of doctors today employed likely due to financial obstacles of starting a practice.
The increase in recruiting indicates possible renewed interest in these practice settings, particularly concierge medicine, which allows doctors to avoid the challenges of third-party payments, the report stated.
Grant said that despite the flexibility and financial autonomy of starting their own practice, new providers who choose this path face obstacles, such as competing with urgent care centers and retail health clinics, which have been on the rise in the past year.
Saddled with debt from medical training, most graduating residents will choose to work toward financial stability and then consider their own practice later in their career, she said.
Flexible Schedules
Work schedule/call hours or work-life balance was the biggest factor (36%) guiding residents’ choice of first post-residency positions compared with starting salary (19%), according to the Medscape Resident Salary & Debt Report 2024.
Grant said that larger practices and those closer to rural communities tend to offer more innovative work schedules, especially for certain specialists. Some solo practices that form partnerships could potentially allow flexible schedules such as 4-day work weeks or week-on-week-off arrangements, she added.
Physicians are also opting for the flexibility of temporary, locum tenens work to improve job conditions and address feelings of burnout. Dr. Kaydo, DO, as she’s known on Instagram, posts about her experiences as locum tenens. “I found that I could have more flexibility as a locum. I want to be able to take time off when I want and as long as I wanted,” said the full-time family medicine doctor who practices at an outpatient clinic in Philadelphia.
“Basically, I’m contract-working, and they pay me as much as I work, and I can also take more time off.” Her employer for the past year also allowed her to work 10 hours a day, 4 days a week instead of the more traditional 8-hour, 5-day schedule.
Dr. Kaydo said she believes many young doctors think contract employees don’t have a permanent job, are not guaranteed a certain salary, and could easily lose their jobs. “I’ve found that most places really need doctors and are willing to negotiate.”
She said primary care locum doctors are particularly in demand in rural clinics and urban underserved areas.
Nagy said he is considering being a nocturnist, an emergency medicine doctor who works nights, to have more control over his schedule, higher pay, and more flexible shifts. “I switch days and nights and that can be tiring.”
Bransden said job flexibility was her primary job criterion. “I have a young child, so I wanted to work part-time with the potential for even more flexibility down the line. I am working 3 days a week, 8-hour days with a 1-hour break. A 3-day work week came with a pay cut, but for me, it works and is what I need right now.”
A version of this article appeared on Medscape.com.
Roshan Bransden didn’t count how many job offers she received during her recently completed training in family medicine. “It was pretty nonstop throughout all of my PGY-3 year,” she said.
Most of the job opportunities were different from the type of position she sought or where she wanted to work. Bransden graduated from residency at Montefiore Hospital in New York and accepted a position as a primary care doctor in Miami, close to where she grew up and where her family lives.
More than half (56%) of all residents in AMN Healthcare’s 2023 Survey of Final-Year Medical Residents received 100 or more job solicitations during their training, the highest figure since the survey began more than 30 years ago, the staffing agency reported.
Employers are recruiting residents earlier, offering residency stipends of $1500 to $2500 up to 18 months before they finish their training if they commit to an employment contract, said Leah Grant, president of AMN Healthcare’s Physician Permanent Solutions division, specializing in doctor recruitment. She said that the company’s clients are already eyeing residents completing their training in 2026.
“The key for residents is not about finding a position but choosing the right one out of many.” Grant added that residents typically aren’t taught negotiation skills or how to evaluate job offers. They tend to choose a position based on location, but they should also consider work–life balance issues such as call schedules and whether incentives such as signing bonuses, relocation allowances, and student loan reimbursement offset the job’s time commitment.
“If you are a physician and you are willing to go anywhere, you will have hundreds of opportunities,” said Tibor Nagy, DO, an emergency medicine fellow who recently searched for jobs. “It depends on what they want out of their careers.”
Location Is a Key Consideration
Nagy said he had fewer options because he was limited by location, staying close to where his wife is finishing her internal medicine residency. He is completing his fellowship at Atrium Health Carolinas Medical Center in Charlotte, North Carolina, and preparing to return to Prisma Health in Greenville, South Carolina, where he did his residency.
He said that the job search was easier than he anticipated considering the tight market following a job report from the American College of Emergency Physicians in 2021 that predicted an oversupply of 8000 emergency medicine physicians by 2030.
Halfway through Nagy’s residency, he sought a fellowship in emergency medical services (EMS) to be more competitive in the job market. After that, “Every door I knocked on was open to hiring. Maybe it’s a regional thing. They were happy to interview me.”
In addition to location, Nagy’s top priorities when choosing a job were stability and being able to use his EMS fellowship to become a medical director of an EMS system, agency, or fire department. He wanted to work for a hospital system with an academic focus without much employee turnover.
Salary vs Benefits
AMN Healthcare received the most physician searches for family medicine doctors, followed by OB/GYNs. The staffing agency reported that close to two thirds (63%) of its search engagements during the 2023-2024 review period were for specialists, reflecting the needs of an aging population.
The highest average starting salaries were for surgical and internal medicine subspecialties, according to AMN Healthcare’s 2024 Physician and Advanced Practitioner Recruiting Incentives. Orthopedic surgery averaged $633,000; urology, $540,000; gastroenterology, $506,000; and pulmonary medicine, $418,000. For comparison, the average starting salaries for primary care doctors were family medicine, $255,000; internal medicine, $255,000; and pediatrics, $233,000.
In addition to starting salaries, many physicians receive signing bonuses, relocation allowances, and continuing medical education (CME) allowances. According to the report, the average signing bonus for physicians was $31,473. The average relocation allowance for physicians was $11,284 and the average CME allowance was $3969.
Salary wasn’t Nagy’s top priority when choosing a job, though he admits that the ability to pay back thousands of dollars in medical school loans will be helpful. Instead of focusing on higher pay to offset student loans, Nagy said he sought nonprofit positions to help him qualify for public service loan forgiveness.
The federal program forgives loan balances after the recipient makes monthly payments for 10 years while working for a government or nonprofit organization. He also racked up 3 years of residency and his fellowship year at nonprofit hospitals toward that commitment.
He said jobs that pay more may require doctors to see more patients. “The hustle may be different. There are definitely tradeoffs,” he said.
Bransden said the position she begins in January will allow her to work part-time with full benefits, among other perks. “My employer is a membership-based practice, so I’ll be able to gift a few memberships to family and friends.”
Going Solo
Mohammad Ibrahim, DO, is among a minority of new physicians who have chosen to set up their own practice.
Only 6% of residents in AMN Healthcare’s 2024 report indicated that a solo practice was among their top two choices, while 20% listed partnering with another physician.
Ibrahim is a sports medicine fellow at the University of Michigan Health-West in Wyoming, after finishing his family medicine residency at Trinity Health Livingston Hospital in Howell, Michigan.
After his fellowship ends, he said he plans to stay in Michigan, where his family lives.
Ibrahim said he began his medical education knowing he wanted to become a solo clinician in private practice. He sees it as a way to have more control over his decisions about patient care and business practices.
Working in a hospital often requires doctors to gain approval from several levels of authority for decisions such as ordering new equipment or forgiving part of a service payment. He also wanted to set his schedule to take Friday afternoons off for Muslim prayer.
Although he realizes the challenges of starting a private practice, Ibrahim said those who go through graduate medical education can figure out how to adapt and overcome any obstacles. “I think it’s more doable than we are led to believe.”
He said that if more residents were exposed to private practice, they might pursue that path. During his training, Ibrahim did a rotation with a private practice physician. “It’s nice to see people proud of what they built, what they contributed.”
Most residents don’t choose private practice. In the AMN Healthcare survey, 68% of residents said that employment by a hospital was among their top two choices for a practice setting, 42% said employment by a single-specialty group, and 32%, employment by a multispecialty group.
Of the majority of job searches AMN Healthcare conducted, 28% were to fill positions in hospital settings, followed by 26% for medical groups, 22% for academic medical centers, 13% for urgent care centers and retail clinics, 6% for solo practices, partnerships, or concierge practice settings, and 5% for Federally Qualified Health Centers/Community Health Centers or Indian Health facilities.
Still, the report noted an increase in recruiting for independent medical practice ownership, which dwindled in recent years, with the majority of doctors today employed likely due to financial obstacles of starting a practice.
The increase in recruiting indicates possible renewed interest in these practice settings, particularly concierge medicine, which allows doctors to avoid the challenges of third-party payments, the report stated.
Grant said that despite the flexibility and financial autonomy of starting their own practice, new providers who choose this path face obstacles, such as competing with urgent care centers and retail health clinics, which have been on the rise in the past year.
Saddled with debt from medical training, most graduating residents will choose to work toward financial stability and then consider their own practice later in their career, she said.
Flexible Schedules
Work schedule/call hours or work-life balance was the biggest factor (36%) guiding residents’ choice of first post-residency positions compared with starting salary (19%), according to the Medscape Resident Salary & Debt Report 2024.
Grant said that larger practices and those closer to rural communities tend to offer more innovative work schedules, especially for certain specialists. Some solo practices that form partnerships could potentially allow flexible schedules such as 4-day work weeks or week-on-week-off arrangements, she added.
Physicians are also opting for the flexibility of temporary, locum tenens work to improve job conditions and address feelings of burnout. Dr. Kaydo, DO, as she’s known on Instagram, posts about her experiences as locum tenens. “I found that I could have more flexibility as a locum. I want to be able to take time off when I want and as long as I wanted,” said the full-time family medicine doctor who practices at an outpatient clinic in Philadelphia.
“Basically, I’m contract-working, and they pay me as much as I work, and I can also take more time off.” Her employer for the past year also allowed her to work 10 hours a day, 4 days a week instead of the more traditional 8-hour, 5-day schedule.
Dr. Kaydo said she believes many young doctors think contract employees don’t have a permanent job, are not guaranteed a certain salary, and could easily lose their jobs. “I’ve found that most places really need doctors and are willing to negotiate.”
She said primary care locum doctors are particularly in demand in rural clinics and urban underserved areas.
Nagy said he is considering being a nocturnist, an emergency medicine doctor who works nights, to have more control over his schedule, higher pay, and more flexible shifts. “I switch days and nights and that can be tiring.”
Bransden said job flexibility was her primary job criterion. “I have a young child, so I wanted to work part-time with the potential for even more flexibility down the line. I am working 3 days a week, 8-hour days with a 1-hour break. A 3-day work week came with a pay cut, but for me, it works and is what I need right now.”
A version of this article appeared on Medscape.com.
Roshan Bransden didn’t count how many job offers she received during her recently completed training in family medicine. “It was pretty nonstop throughout all of my PGY-3 year,” she said.
Most of the job opportunities were different from the type of position she sought or where she wanted to work. Bransden graduated from residency at Montefiore Hospital in New York and accepted a position as a primary care doctor in Miami, close to where she grew up and where her family lives.
More than half (56%) of all residents in AMN Healthcare’s 2023 Survey of Final-Year Medical Residents received 100 or more job solicitations during their training, the highest figure since the survey began more than 30 years ago, the staffing agency reported.
Employers are recruiting residents earlier, offering residency stipends of $1500 to $2500 up to 18 months before they finish their training if they commit to an employment contract, said Leah Grant, president of AMN Healthcare’s Physician Permanent Solutions division, specializing in doctor recruitment. She said that the company’s clients are already eyeing residents completing their training in 2026.
“The key for residents is not about finding a position but choosing the right one out of many.” Grant added that residents typically aren’t taught negotiation skills or how to evaluate job offers. They tend to choose a position based on location, but they should also consider work–life balance issues such as call schedules and whether incentives such as signing bonuses, relocation allowances, and student loan reimbursement offset the job’s time commitment.
“If you are a physician and you are willing to go anywhere, you will have hundreds of opportunities,” said Tibor Nagy, DO, an emergency medicine fellow who recently searched for jobs. “It depends on what they want out of their careers.”
Location Is a Key Consideration
Nagy said he had fewer options because he was limited by location, staying close to where his wife is finishing her internal medicine residency. He is completing his fellowship at Atrium Health Carolinas Medical Center in Charlotte, North Carolina, and preparing to return to Prisma Health in Greenville, South Carolina, where he did his residency.
He said that the job search was easier than he anticipated considering the tight market following a job report from the American College of Emergency Physicians in 2021 that predicted an oversupply of 8000 emergency medicine physicians by 2030.
Halfway through Nagy’s residency, he sought a fellowship in emergency medical services (EMS) to be more competitive in the job market. After that, “Every door I knocked on was open to hiring. Maybe it’s a regional thing. They were happy to interview me.”
In addition to location, Nagy’s top priorities when choosing a job were stability and being able to use his EMS fellowship to become a medical director of an EMS system, agency, or fire department. He wanted to work for a hospital system with an academic focus without much employee turnover.
Salary vs Benefits
AMN Healthcare received the most physician searches for family medicine doctors, followed by OB/GYNs. The staffing agency reported that close to two thirds (63%) of its search engagements during the 2023-2024 review period were for specialists, reflecting the needs of an aging population.
The highest average starting salaries were for surgical and internal medicine subspecialties, according to AMN Healthcare’s 2024 Physician and Advanced Practitioner Recruiting Incentives. Orthopedic surgery averaged $633,000; urology, $540,000; gastroenterology, $506,000; and pulmonary medicine, $418,000. For comparison, the average starting salaries for primary care doctors were family medicine, $255,000; internal medicine, $255,000; and pediatrics, $233,000.
In addition to starting salaries, many physicians receive signing bonuses, relocation allowances, and continuing medical education (CME) allowances. According to the report, the average signing bonus for physicians was $31,473. The average relocation allowance for physicians was $11,284 and the average CME allowance was $3969.
Salary wasn’t Nagy’s top priority when choosing a job, though he admits that the ability to pay back thousands of dollars in medical school loans will be helpful. Instead of focusing on higher pay to offset student loans, Nagy said he sought nonprofit positions to help him qualify for public service loan forgiveness.
The federal program forgives loan balances after the recipient makes monthly payments for 10 years while working for a government or nonprofit organization. He also racked up 3 years of residency and his fellowship year at nonprofit hospitals toward that commitment.
He said jobs that pay more may require doctors to see more patients. “The hustle may be different. There are definitely tradeoffs,” he said.
Bransden said the position she begins in January will allow her to work part-time with full benefits, among other perks. “My employer is a membership-based practice, so I’ll be able to gift a few memberships to family and friends.”
Going Solo
Mohammad Ibrahim, DO, is among a minority of new physicians who have chosen to set up their own practice.
Only 6% of residents in AMN Healthcare’s 2024 report indicated that a solo practice was among their top two choices, while 20% listed partnering with another physician.
Ibrahim is a sports medicine fellow at the University of Michigan Health-West in Wyoming, after finishing his family medicine residency at Trinity Health Livingston Hospital in Howell, Michigan.
After his fellowship ends, he said he plans to stay in Michigan, where his family lives.
Ibrahim said he began his medical education knowing he wanted to become a solo clinician in private practice. He sees it as a way to have more control over his decisions about patient care and business practices.
Working in a hospital often requires doctors to gain approval from several levels of authority for decisions such as ordering new equipment or forgiving part of a service payment. He also wanted to set his schedule to take Friday afternoons off for Muslim prayer.
Although he realizes the challenges of starting a private practice, Ibrahim said those who go through graduate medical education can figure out how to adapt and overcome any obstacles. “I think it’s more doable than we are led to believe.”
He said that if more residents were exposed to private practice, they might pursue that path. During his training, Ibrahim did a rotation with a private practice physician. “It’s nice to see people proud of what they built, what they contributed.”
Most residents don’t choose private practice. In the AMN Healthcare survey, 68% of residents said that employment by a hospital was among their top two choices for a practice setting, 42% said employment by a single-specialty group, and 32%, employment by a multispecialty group.
Of the majority of job searches AMN Healthcare conducted, 28% were to fill positions in hospital settings, followed by 26% for medical groups, 22% for academic medical centers, 13% for urgent care centers and retail clinics, 6% for solo practices, partnerships, or concierge practice settings, and 5% for Federally Qualified Health Centers/Community Health Centers or Indian Health facilities.
Still, the report noted an increase in recruiting for independent medical practice ownership, which dwindled in recent years, with the majority of doctors today employed likely due to financial obstacles of starting a practice.
The increase in recruiting indicates possible renewed interest in these practice settings, particularly concierge medicine, which allows doctors to avoid the challenges of third-party payments, the report stated.
Grant said that despite the flexibility and financial autonomy of starting their own practice, new providers who choose this path face obstacles, such as competing with urgent care centers and retail health clinics, which have been on the rise in the past year.
Saddled with debt from medical training, most graduating residents will choose to work toward financial stability and then consider their own practice later in their career, she said.
Flexible Schedules
Work schedule/call hours or work-life balance was the biggest factor (36%) guiding residents’ choice of first post-residency positions compared with starting salary (19%), according to the Medscape Resident Salary & Debt Report 2024.
Grant said that larger practices and those closer to rural communities tend to offer more innovative work schedules, especially for certain specialists. Some solo practices that form partnerships could potentially allow flexible schedules such as 4-day work weeks or week-on-week-off arrangements, she added.
Physicians are also opting for the flexibility of temporary, locum tenens work to improve job conditions and address feelings of burnout. Dr. Kaydo, DO, as she’s known on Instagram, posts about her experiences as locum tenens. “I found that I could have more flexibility as a locum. I want to be able to take time off when I want and as long as I wanted,” said the full-time family medicine doctor who practices at an outpatient clinic in Philadelphia.
“Basically, I’m contract-working, and they pay me as much as I work, and I can also take more time off.” Her employer for the past year also allowed her to work 10 hours a day, 4 days a week instead of the more traditional 8-hour, 5-day schedule.
Dr. Kaydo said she believes many young doctors think contract employees don’t have a permanent job, are not guaranteed a certain salary, and could easily lose their jobs. “I’ve found that most places really need doctors and are willing to negotiate.”
She said primary care locum doctors are particularly in demand in rural clinics and urban underserved areas.
Nagy said he is considering being a nocturnist, an emergency medicine doctor who works nights, to have more control over his schedule, higher pay, and more flexible shifts. “I switch days and nights and that can be tiring.”
Bransden said job flexibility was her primary job criterion. “I have a young child, so I wanted to work part-time with the potential for even more flexibility down the line. I am working 3 days a week, 8-hour days with a 1-hour break. A 3-day work week came with a pay cut, but for me, it works and is what I need right now.”
A version of this article appeared on Medscape.com.
First Hike of Medicare Funding for Residencies in 25 Years Aims to Help Shortages
Residency programs across the country may have a few more slots for incoming residents due to a recent bump in Medicare funding.
Case in point: The University of Alabama at Birmingham (UAB). The state has one of the top stroke rates in the country, and yet UAB has the only hospital in the state training future doctors to help stroke patients recover. “Our hospital cares for Alabama’s sickest patients, many who need rehabilitation services,” said Craig Hoesley, MD, senior associate dean for medical education, who oversees graduate medical education (GME) or residency programs.
After decades of stagnant support, a recent bump in Medicare funding will allow UAB to add two more physical medicine and rehabilitation residents to the four residencies already receiving such funding.
Medicare also awarded UAB more funding last year to add an addiction medicine fellowship, one of two such training programs in the state for the specialty that helps treat patients fighting addiction.
UAB is among healthcare systems and hospitals nationwide benefiting from a recent hike in Medicare funding for residency programs after some 25 years at the same level of federal support. Medicare is the largest funder of training positions. Otherwise, hospitals finance training through means such as state support.
The latest round of funding, which went into effect in July, adds 200 positions to the doctor pipeline, creating more openings for residents seeking positions after medical school.
In the next few months, the Centers for Medicare & Medicaid Services (CMS) will notify teaching hospitals whether they’ll receive the next round of Medicare funding for more residency positions. At that time, CMS will have awarded nearly half of the 1200 residency training slots Congress approved in the past few years. In 2020 — for the first time since 1996 — Congress approved adding 1000 residency slots at teaching hospitals nationwide. CMS awards the money for 200 slots each year for 5 years.
More than half of the initial round of funding focused on training primary care specialists, with other slots designated for mental health specialists. Last year, Congress also approved a separate allocation of 200 more Medicare-funded residency positions, with at least half designated for psychiatry and related subspecialty residencies to help meet the growing need for more mental health specialists. On August 1, CMS announced it would distribute the funds next year, effective in 2026.
The additional Medicare funding attempts to address the shortage of healthcare providers and ensure future access to care, including in rural and underserved communities. The Association of American Medical Colleges (AAMC) estimates the nation will face a shortage of up to 86,000 physicians by 2036, including primary care doctors and specialists.
In addition, more than 100 million Americans, nearly a third of the nation, don’t have access to primary care due to the physician shortages in their communities, according to the National Association of Community Health Centers.
Major medical organizations, medical schools, and hospital groups have been pushing for years for increased Medicare funding to train new doctors to keep up with the demand for healthcare services and offset the physician shortage. As a cost-saving measure, Medicare set its cap in 1996 for how much it will reimburse each hospital offering GME training. However, according to the medical groups that continue to advocate to Congress for more funding, the funding hasn’t kept pace with the growing healthcare needs or rising medical school enrollment.
Adding Residency Spots
In April, Dr. Hoesley of UAB spoke at a Congressional briefing among health systems and hospitals that benefited from the additional funding. He told Congressional leaders how the increased number of GME positions affects UAB Medicine and its ability to care for rural areas.
“We have entire counties in Alabama that don’t have physicians. One way to address the physician shortage is to grow the GME programs. The funding we received will help us grow these programs and care for residents in our state.”
Still, the Medicare funding is only a drop in the bucket, Dr. Hoesley said. “We rely on Medicare funding alongside other funding partners to train residents and expand our care across the state.” He said many UAB residency programs are over their Medicare funding cap and would like to grow, but they can’t without more funding.
Mount Sinai Health System in New York City also will be able to expand its residency program after receiving Medicare support in the latest round of funding. The health system will use the federal funds to train an additional vascular surgeon. Mount Sinai currently receives CMS funding to train three residents in the specialty.
Over a 5-year program, that means CMS funding will help train 20 residents in the specialty that treats blood vessel blockages and diseases of the veins and arteries generally associated with aging.
“The funding is amazing,” said Peter L. Faries, MD, a surgery professor and system chief of vascular surgery at the Icahn School of Medicine at Mount Sinai, New York City, who directs the residency program.
“We don’t have the capacity to provide an individual training program without the funding. It’s not economically feasible.”
The need for more vascular surgeons increases as the population continues to age, he said. Mount Sinai treats patients throughout New York, including underserved areas in Harlem, the Bronx, Washington Heights, Brooklyn, and Queens. “These individuals might not receive an appropriate level of vascular care if we don’t have clinicians to treat them.”
Of the recent funding, Dr. Faries said it’s taken the residency program 15 years of advocacy to increase by two slots. “It’s a long process to get funding.” Vascular training programs can remain very selective with Medicare funding, typically receiving two applicants for every position,” said Dr. Faries.
Pushing for More Funds
Nearly 98,000 students enrolled in medical school this year, according to the National Resident Matching Program. A total of 44,853 applicants vied for the 38,494 first-year residency positions and 3009 second-year slots, leaving 3350 medical school graduates without a match.
“There are not enough spots to meet the growing demand,” said Jesse M. Ehrenfeld, MD, MPH, immediate past president of the American Medical Association. “Graduate medical education funding has not kept up.”
Despite the increase in medical school graduates over the past two decades, Medicare-supported training opportunities remained frozen at the 1996 level. A limited number of training positions meant residency programs couldn’t expand the physician pipeline to offset an aging workforce, contributing to the shortage. “The way to solve this is to expand GME,” Dr. Ehrenfeld said. “We continue to advocate to remove the cap.”
Dr. Ehrenfeld also told this news organization that he doesn’t mind that Congress recently designated GME funding to certain specialties, such as psychiatry, because he believes the need is great for residency spots across the board. “The good news is people recognize it’s challenging to get much through Congress.” He’s optimistic, though, about recent legislative efforts to increase funding.
AAMC, representing about a third of the nation’s 1100 teaching hospitals and health systems, feels the same. Congress “acknowledges and continues to recognize that the shortage is not getting better, and one way to address it is to increase Medicare-supported GME positions,” said Leonard Marquez, senior director of government relations and legislative advocacy.
Still, he said that the Medicare funding bump is only making a small dent in the need. AAMC estimates the average cost to train residents is $23 billion annually, and Medicare only funds 20% of that, or $5 billion. “Our members are at the point where they say: We already can’t add new training positions,” Mr. Marquez said. He added that without increasing residency slots, patient care will suffer. “We have to do anything possible we can to increase access to care.”
Mr. Marquez also believes Medicare funding should increase residency positions across the specialty spectrum, not just for psychiatry and primary care. He said that the targeted funding may prevent some teaching hospitals from applying for residency positions if they need other types of specialists based on their community’s needs.
Among the current proposals before Congress, the Resident Physician Shortage Reduction Act of 2023 would add 14,000 Medicare-supported residency slots over 7 years. Mr. Marquez said it may be more realistic to expect fewer new slots. A decision on potential legislation is expected at the end of the year. He said that if the medical groups aren’t pleased with the decision, they’ll advocate again in 2025.
A version of this article first appeared on Medscape.com.
Residency programs across the country may have a few more slots for incoming residents due to a recent bump in Medicare funding.
Case in point: The University of Alabama at Birmingham (UAB). The state has one of the top stroke rates in the country, and yet UAB has the only hospital in the state training future doctors to help stroke patients recover. “Our hospital cares for Alabama’s sickest patients, many who need rehabilitation services,” said Craig Hoesley, MD, senior associate dean for medical education, who oversees graduate medical education (GME) or residency programs.
After decades of stagnant support, a recent bump in Medicare funding will allow UAB to add two more physical medicine and rehabilitation residents to the four residencies already receiving such funding.
Medicare also awarded UAB more funding last year to add an addiction medicine fellowship, one of two such training programs in the state for the specialty that helps treat patients fighting addiction.
UAB is among healthcare systems and hospitals nationwide benefiting from a recent hike in Medicare funding for residency programs after some 25 years at the same level of federal support. Medicare is the largest funder of training positions. Otherwise, hospitals finance training through means such as state support.
The latest round of funding, which went into effect in July, adds 200 positions to the doctor pipeline, creating more openings for residents seeking positions after medical school.
In the next few months, the Centers for Medicare & Medicaid Services (CMS) will notify teaching hospitals whether they’ll receive the next round of Medicare funding for more residency positions. At that time, CMS will have awarded nearly half of the 1200 residency training slots Congress approved in the past few years. In 2020 — for the first time since 1996 — Congress approved adding 1000 residency slots at teaching hospitals nationwide. CMS awards the money for 200 slots each year for 5 years.
More than half of the initial round of funding focused on training primary care specialists, with other slots designated for mental health specialists. Last year, Congress also approved a separate allocation of 200 more Medicare-funded residency positions, with at least half designated for psychiatry and related subspecialty residencies to help meet the growing need for more mental health specialists. On August 1, CMS announced it would distribute the funds next year, effective in 2026.
The additional Medicare funding attempts to address the shortage of healthcare providers and ensure future access to care, including in rural and underserved communities. The Association of American Medical Colleges (AAMC) estimates the nation will face a shortage of up to 86,000 physicians by 2036, including primary care doctors and specialists.
In addition, more than 100 million Americans, nearly a third of the nation, don’t have access to primary care due to the physician shortages in their communities, according to the National Association of Community Health Centers.
Major medical organizations, medical schools, and hospital groups have been pushing for years for increased Medicare funding to train new doctors to keep up with the demand for healthcare services and offset the physician shortage. As a cost-saving measure, Medicare set its cap in 1996 for how much it will reimburse each hospital offering GME training. However, according to the medical groups that continue to advocate to Congress for more funding, the funding hasn’t kept pace with the growing healthcare needs or rising medical school enrollment.
Adding Residency Spots
In April, Dr. Hoesley of UAB spoke at a Congressional briefing among health systems and hospitals that benefited from the additional funding. He told Congressional leaders how the increased number of GME positions affects UAB Medicine and its ability to care for rural areas.
“We have entire counties in Alabama that don’t have physicians. One way to address the physician shortage is to grow the GME programs. The funding we received will help us grow these programs and care for residents in our state.”
Still, the Medicare funding is only a drop in the bucket, Dr. Hoesley said. “We rely on Medicare funding alongside other funding partners to train residents and expand our care across the state.” He said many UAB residency programs are over their Medicare funding cap and would like to grow, but they can’t without more funding.
Mount Sinai Health System in New York City also will be able to expand its residency program after receiving Medicare support in the latest round of funding. The health system will use the federal funds to train an additional vascular surgeon. Mount Sinai currently receives CMS funding to train three residents in the specialty.
Over a 5-year program, that means CMS funding will help train 20 residents in the specialty that treats blood vessel blockages and diseases of the veins and arteries generally associated with aging.
“The funding is amazing,” said Peter L. Faries, MD, a surgery professor and system chief of vascular surgery at the Icahn School of Medicine at Mount Sinai, New York City, who directs the residency program.
“We don’t have the capacity to provide an individual training program without the funding. It’s not economically feasible.”
The need for more vascular surgeons increases as the population continues to age, he said. Mount Sinai treats patients throughout New York, including underserved areas in Harlem, the Bronx, Washington Heights, Brooklyn, and Queens. “These individuals might not receive an appropriate level of vascular care if we don’t have clinicians to treat them.”
Of the recent funding, Dr. Faries said it’s taken the residency program 15 years of advocacy to increase by two slots. “It’s a long process to get funding.” Vascular training programs can remain very selective with Medicare funding, typically receiving two applicants for every position,” said Dr. Faries.
Pushing for More Funds
Nearly 98,000 students enrolled in medical school this year, according to the National Resident Matching Program. A total of 44,853 applicants vied for the 38,494 first-year residency positions and 3009 second-year slots, leaving 3350 medical school graduates without a match.
“There are not enough spots to meet the growing demand,” said Jesse M. Ehrenfeld, MD, MPH, immediate past president of the American Medical Association. “Graduate medical education funding has not kept up.”
Despite the increase in medical school graduates over the past two decades, Medicare-supported training opportunities remained frozen at the 1996 level. A limited number of training positions meant residency programs couldn’t expand the physician pipeline to offset an aging workforce, contributing to the shortage. “The way to solve this is to expand GME,” Dr. Ehrenfeld said. “We continue to advocate to remove the cap.”
Dr. Ehrenfeld also told this news organization that he doesn’t mind that Congress recently designated GME funding to certain specialties, such as psychiatry, because he believes the need is great for residency spots across the board. “The good news is people recognize it’s challenging to get much through Congress.” He’s optimistic, though, about recent legislative efforts to increase funding.
AAMC, representing about a third of the nation’s 1100 teaching hospitals and health systems, feels the same. Congress “acknowledges and continues to recognize that the shortage is not getting better, and one way to address it is to increase Medicare-supported GME positions,” said Leonard Marquez, senior director of government relations and legislative advocacy.
Still, he said that the Medicare funding bump is only making a small dent in the need. AAMC estimates the average cost to train residents is $23 billion annually, and Medicare only funds 20% of that, or $5 billion. “Our members are at the point where they say: We already can’t add new training positions,” Mr. Marquez said. He added that without increasing residency slots, patient care will suffer. “We have to do anything possible we can to increase access to care.”
Mr. Marquez also believes Medicare funding should increase residency positions across the specialty spectrum, not just for psychiatry and primary care. He said that the targeted funding may prevent some teaching hospitals from applying for residency positions if they need other types of specialists based on their community’s needs.
Among the current proposals before Congress, the Resident Physician Shortage Reduction Act of 2023 would add 14,000 Medicare-supported residency slots over 7 years. Mr. Marquez said it may be more realistic to expect fewer new slots. A decision on potential legislation is expected at the end of the year. He said that if the medical groups aren’t pleased with the decision, they’ll advocate again in 2025.
A version of this article first appeared on Medscape.com.
Residency programs across the country may have a few more slots for incoming residents due to a recent bump in Medicare funding.
Case in point: The University of Alabama at Birmingham (UAB). The state has one of the top stroke rates in the country, and yet UAB has the only hospital in the state training future doctors to help stroke patients recover. “Our hospital cares for Alabama’s sickest patients, many who need rehabilitation services,” said Craig Hoesley, MD, senior associate dean for medical education, who oversees graduate medical education (GME) or residency programs.
After decades of stagnant support, a recent bump in Medicare funding will allow UAB to add two more physical medicine and rehabilitation residents to the four residencies already receiving such funding.
Medicare also awarded UAB more funding last year to add an addiction medicine fellowship, one of two such training programs in the state for the specialty that helps treat patients fighting addiction.
UAB is among healthcare systems and hospitals nationwide benefiting from a recent hike in Medicare funding for residency programs after some 25 years at the same level of federal support. Medicare is the largest funder of training positions. Otherwise, hospitals finance training through means such as state support.
The latest round of funding, which went into effect in July, adds 200 positions to the doctor pipeline, creating more openings for residents seeking positions after medical school.
In the next few months, the Centers for Medicare & Medicaid Services (CMS) will notify teaching hospitals whether they’ll receive the next round of Medicare funding for more residency positions. At that time, CMS will have awarded nearly half of the 1200 residency training slots Congress approved in the past few years. In 2020 — for the first time since 1996 — Congress approved adding 1000 residency slots at teaching hospitals nationwide. CMS awards the money for 200 slots each year for 5 years.
More than half of the initial round of funding focused on training primary care specialists, with other slots designated for mental health specialists. Last year, Congress also approved a separate allocation of 200 more Medicare-funded residency positions, with at least half designated for psychiatry and related subspecialty residencies to help meet the growing need for more mental health specialists. On August 1, CMS announced it would distribute the funds next year, effective in 2026.
The additional Medicare funding attempts to address the shortage of healthcare providers and ensure future access to care, including in rural and underserved communities. The Association of American Medical Colleges (AAMC) estimates the nation will face a shortage of up to 86,000 physicians by 2036, including primary care doctors and specialists.
In addition, more than 100 million Americans, nearly a third of the nation, don’t have access to primary care due to the physician shortages in their communities, according to the National Association of Community Health Centers.
Major medical organizations, medical schools, and hospital groups have been pushing for years for increased Medicare funding to train new doctors to keep up with the demand for healthcare services and offset the physician shortage. As a cost-saving measure, Medicare set its cap in 1996 for how much it will reimburse each hospital offering GME training. However, according to the medical groups that continue to advocate to Congress for more funding, the funding hasn’t kept pace with the growing healthcare needs or rising medical school enrollment.
Adding Residency Spots
In April, Dr. Hoesley of UAB spoke at a Congressional briefing among health systems and hospitals that benefited from the additional funding. He told Congressional leaders how the increased number of GME positions affects UAB Medicine and its ability to care for rural areas.
“We have entire counties in Alabama that don’t have physicians. One way to address the physician shortage is to grow the GME programs. The funding we received will help us grow these programs and care for residents in our state.”
Still, the Medicare funding is only a drop in the bucket, Dr. Hoesley said. “We rely on Medicare funding alongside other funding partners to train residents and expand our care across the state.” He said many UAB residency programs are over their Medicare funding cap and would like to grow, but they can’t without more funding.
Mount Sinai Health System in New York City also will be able to expand its residency program after receiving Medicare support in the latest round of funding. The health system will use the federal funds to train an additional vascular surgeon. Mount Sinai currently receives CMS funding to train three residents in the specialty.
Over a 5-year program, that means CMS funding will help train 20 residents in the specialty that treats blood vessel blockages and diseases of the veins and arteries generally associated with aging.
“The funding is amazing,” said Peter L. Faries, MD, a surgery professor and system chief of vascular surgery at the Icahn School of Medicine at Mount Sinai, New York City, who directs the residency program.
“We don’t have the capacity to provide an individual training program without the funding. It’s not economically feasible.”
The need for more vascular surgeons increases as the population continues to age, he said. Mount Sinai treats patients throughout New York, including underserved areas in Harlem, the Bronx, Washington Heights, Brooklyn, and Queens. “These individuals might not receive an appropriate level of vascular care if we don’t have clinicians to treat them.”
Of the recent funding, Dr. Faries said it’s taken the residency program 15 years of advocacy to increase by two slots. “It’s a long process to get funding.” Vascular training programs can remain very selective with Medicare funding, typically receiving two applicants for every position,” said Dr. Faries.
Pushing for More Funds
Nearly 98,000 students enrolled in medical school this year, according to the National Resident Matching Program. A total of 44,853 applicants vied for the 38,494 first-year residency positions and 3009 second-year slots, leaving 3350 medical school graduates without a match.
“There are not enough spots to meet the growing demand,” said Jesse M. Ehrenfeld, MD, MPH, immediate past president of the American Medical Association. “Graduate medical education funding has not kept up.”
Despite the increase in medical school graduates over the past two decades, Medicare-supported training opportunities remained frozen at the 1996 level. A limited number of training positions meant residency programs couldn’t expand the physician pipeline to offset an aging workforce, contributing to the shortage. “The way to solve this is to expand GME,” Dr. Ehrenfeld said. “We continue to advocate to remove the cap.”
Dr. Ehrenfeld also told this news organization that he doesn’t mind that Congress recently designated GME funding to certain specialties, such as psychiatry, because he believes the need is great for residency spots across the board. “The good news is people recognize it’s challenging to get much through Congress.” He’s optimistic, though, about recent legislative efforts to increase funding.
AAMC, representing about a third of the nation’s 1100 teaching hospitals and health systems, feels the same. Congress “acknowledges and continues to recognize that the shortage is not getting better, and one way to address it is to increase Medicare-supported GME positions,” said Leonard Marquez, senior director of government relations and legislative advocacy.
Still, he said that the Medicare funding bump is only making a small dent in the need. AAMC estimates the average cost to train residents is $23 billion annually, and Medicare only funds 20% of that, or $5 billion. “Our members are at the point where they say: We already can’t add new training positions,” Mr. Marquez said. He added that without increasing residency slots, patient care will suffer. “We have to do anything possible we can to increase access to care.”
Mr. Marquez also believes Medicare funding should increase residency positions across the specialty spectrum, not just for psychiatry and primary care. He said that the targeted funding may prevent some teaching hospitals from applying for residency positions if they need other types of specialists based on their community’s needs.
Among the current proposals before Congress, the Resident Physician Shortage Reduction Act of 2023 would add 14,000 Medicare-supported residency slots over 7 years. Mr. Marquez said it may be more realistic to expect fewer new slots. A decision on potential legislation is expected at the end of the year. He said that if the medical groups aren’t pleased with the decision, they’ll advocate again in 2025.
A version of this article first appeared on Medscape.com.
From Scrubs to Social Media: How Some Med Students Become Influencers
A medical student’s life is an endless cycle of classes, exams, clinical rotations, and residency preparation. On TikTok and Instagram, among other sites, they share medical school experiences and lessons learned in the classroom and advocate for causes such as increased diversity and gender rights in the medical field.
This news organization caught up with a few social media influencers with a large online following to learn how medical students can effectively use social media to build a professional brand and network. Most of the students interviewed said that their social media platforms offered an opportunity to educate others about significant medical developments, feel part of a community with a like-minded audience, and network with doctors who may lead them to a future residency or career path.
Many med students said that they built their large audiences by creating a platform for people of their ethnic background, nationality, race, gender, or simply what others weren’t already talking about. They said they saw a niche in social media that was missing or others hadn’t tackled in the same way.
When Joel Bervell began med school in 2020, he questioned some of the lessons he learned about how race is used in medical practice, which didn’t make sense to him. So, he began his own research. He had about 2000 followers on Instagram at the time.
Mr. Bervell read a new study about pulse oximeters and how they often produce misleading readings on patients with dark skin.
He wondered why he hadn’t learned this in medical school, so he posted it on TikTok. Within 24 hours, about 500,000 people viewed it. Most of the comments were from doctors, nurses, and physician assistants who said they weren’t aware of the disparity.
While his initial posts detailed his journey to medical school and a day-in-the-life of a medical student, he transitioned to posts primarily about race, health equity, and what he perceives as racial bias in medicine.
Now, the fourth-year Ghanaian-American student at the Elson S. Floyd College of Medicine at Washington State University Spokane has close to 1.2 million followers on Instagram and TikTok combined. He frequently visits the White House to advise on social media’s influence on healthcare and has appeared on the Kelly Clarkson Show, Good Morning America, CNN, and ABC, among others.
He said he also uses social media to translate complex medical information for a general audience, many of whom access health information online so they can manage their own healthcare. He sees his social media work as an extension of his medical education, allowing him to delve deeper into subjects and report on them as if he were publishing research in a medical journal.
“When I came to medical school, yes, I wanted to be a doctor. But I also wanted to impact people.” Social media allows him to educate many more people than individual patients, the 29-year-old told this news organization.
Inspiring Minorities
Tabhata Paulet, 27, started her TikTok presence as a premed student in 2021. She aimed to provide free resources to help low-income, first-generation Latinx students like herself study for standardized exams.
“I always looked online for guidance and resources, and the medical influencers did not share a similar background. So, I shared my story and what I had to do as a first-generation and first person in my family to become a physician. I did not have access to the same resources as my peers,” said Ms. Paulet, who was born in Peru and came to New Jersey as a child.
Students who are Hispanic, Latinx, or of Spanish origin made up 6.8% of total medical school enrollment in 2023-2024, up slightly from 6.7% in 2022-2023, according to the Association of American Medical Colleges (AAMC).
Ms. Paulet’s online presence grew when she began documenting her experiences as a first-year medical student, bridging the language barrier for Spanish-speaking patients so they could understand their diagnosis and treatment. She often posts about health disparity and barriers to care for underserved communities.
Most of her nearly 22,000 followers are Hispanic, said the now fourth-year student at Rutgers New Jersey Medical School in Newark, New Jersey. “I talk a lot about my interesting Spanish-speaking patients ... and how sometimes speaking their native language truly makes a difference in their care.”
She believes that she serves an important role in social media. “It can be very inspirational for those who come after you [in med school] to see someone from a similar culture and upbringing.”
Creating a Community
It was during a therapy session 4 years ago that Jeremy “JP” Scott decided to share Instagram posts about his experiences as a nontraditional medical student. The 37-year-old was studying at Ross University School of Medicine in Barbados and was feeling lonely as an international medical student training to be a doctor as a second career.
Before starting med school, Mr. Scott was an adjunct professor and lab supervisor at the University of Hartford Biology Department, West Hartford, Connecticut, and then a research assistant and lab manager at the Wistar Institute in Philadelphia.
Although he wanted to follow his mother’s path to becoming a doctor, it was more difficult than he envisioned, said the fourth-year student who completed clinical rotations in the United States and is now applying for residencies.
“I talked about how medical school is not what it appears to be ... There are a lot of challenges we are going through,” especially as people of color, he said.
Mr. Scott believes social media helps people feel included and less alone. He said many of his followers are med students and physicians.
His posts often focus on LGBTQIA+ pride and being a minority as a Black man in medicine.
“The pandemic spurred a lot of us. We had a racial reckoning in our country at the time. It inspired us to talk as Black creators and Black medical students.”
Black or African American medical students made up 8.5% of total med school enrollment in 2023-2024, a slight increase from 2022 to 2023, according to AAMC figures. Black men represented 7% of total enrollment in 2023-2024, while Black women represented 9.8%.
After only a handful of online posts in which Mr. Scott candidly discussed his mental health struggles and relationships, he attracted the attention of several medical apparel companies, including the popular FIGS scrubs. He’s now an ambassador for the company, which supports him and his content.
“My association with FIGS has helped attract a wider online audience, increasing my presence.” Today, he has 14,000 Instagram followers. “It opened up so many opportunities,” Mr. Scott said. One example is working with the national LGBTQIA+ community.
“The goal was never to be a social media influencer, to gain sponsorships or photo opportunities,” he said.
“My job, first, is as a medical student. Everything else is second. I am not trying to be a professional social media personality. I’m trying to be an actual physician.” He also tries to separate JP “social media” from Jeremy, the medical student.
“On Instagram, anyone can pull it up and see what you’re doing. The last thing I want is for them to think that I’m not serious about what I’m doing, that I’m not here to learn and become a doctor.”
Benefits and Drawbacks
Ms. Paulet said her social media following helped her connect with leaders in the Latinx medical community, including an obstetrics anesthesiologist, her intended specialty. “I don’t think I’d be able to do that without a social media platform.”
Her online activity also propelled her from regional to national leadership in the Latino Medical Student Association (LMSA). She now also runs their Instagram page, which has 14,000 followers.
Mr. Bervell believes social media is a great way to network. He’s connected with people he wouldn’t have met otherwise, including physicians. “I think it will help me get into a residency,” he said. “It allows people to know who you are ... They will be able to tell in a few videos the type of doctor I want to be.”
On the other hand, Mr. Bervell is aware of the negative impacts of social media on mental health. “You can get lost in social media.” For that reason, he often tries to disconnect. “I can go days without my phone.”
Posting on social media can be time-consuming, Mr. Bervell admitted. He said he spent about 2 hours a day researching, editing, and posting on TikTok when he first started building his following. Now, he spends about 2-3 hours a week creating videos. “I don’t post every day anymore. I don’t have the time.”
When she started building her TikTok presence, Ms. Paulet said she devoted 15 hours a week to the endeavor, but now she spends 10-12 hours a week posting online, including on LMSA’s Instagram page. “Whenever you are done with an exam or have a study break, this is something fun to do.” She also says you never know who you’re going to inspire when you put yourself out there.
“Talk about your journey, rotations, or your experience in your first or second year of medical school. Talk about milestones like board exams.”
Word to the Wise
Some students may be concerned that their posts might affect a potential residency program. But the medical students interviewed say they want to find programs that align with their values and accept them for who they are.
Mr. Scott said he’s not worried about someone not liking him because of who he is. “I am Black and openly gay. If it’s a problem, I don’t need to work with you or your institution.”
Mr. Bervell stressed that medical students should stay professional online. “I reach 5-10 million people a month, and I have to think: Would I want them to see this? You have to know at all times that someone is watching. I’m very careful about how I post. I script out every video.”
Mr. Scott agreed. He advises those interested in becoming medical influencers to know what they can’t post online. For example, to ensure safety and privacy, Mr. Scott doesn’t take photos in the hospital, show his medical badge, or post patient information. “You want to be respectful of your future medical profession,” he said.
“If it’s something my mother would be ashamed of, I don’t need to post about it.”
A version of this article first appeared on Medscape.com.
A medical student’s life is an endless cycle of classes, exams, clinical rotations, and residency preparation. On TikTok and Instagram, among other sites, they share medical school experiences and lessons learned in the classroom and advocate for causes such as increased diversity and gender rights in the medical field.
This news organization caught up with a few social media influencers with a large online following to learn how medical students can effectively use social media to build a professional brand and network. Most of the students interviewed said that their social media platforms offered an opportunity to educate others about significant medical developments, feel part of a community with a like-minded audience, and network with doctors who may lead them to a future residency or career path.
Many med students said that they built their large audiences by creating a platform for people of their ethnic background, nationality, race, gender, or simply what others weren’t already talking about. They said they saw a niche in social media that was missing or others hadn’t tackled in the same way.
When Joel Bervell began med school in 2020, he questioned some of the lessons he learned about how race is used in medical practice, which didn’t make sense to him. So, he began his own research. He had about 2000 followers on Instagram at the time.
Mr. Bervell read a new study about pulse oximeters and how they often produce misleading readings on patients with dark skin.
He wondered why he hadn’t learned this in medical school, so he posted it on TikTok. Within 24 hours, about 500,000 people viewed it. Most of the comments were from doctors, nurses, and physician assistants who said they weren’t aware of the disparity.
While his initial posts detailed his journey to medical school and a day-in-the-life of a medical student, he transitioned to posts primarily about race, health equity, and what he perceives as racial bias in medicine.
Now, the fourth-year Ghanaian-American student at the Elson S. Floyd College of Medicine at Washington State University Spokane has close to 1.2 million followers on Instagram and TikTok combined. He frequently visits the White House to advise on social media’s influence on healthcare and has appeared on the Kelly Clarkson Show, Good Morning America, CNN, and ABC, among others.
He said he also uses social media to translate complex medical information for a general audience, many of whom access health information online so they can manage their own healthcare. He sees his social media work as an extension of his medical education, allowing him to delve deeper into subjects and report on them as if he were publishing research in a medical journal.
“When I came to medical school, yes, I wanted to be a doctor. But I also wanted to impact people.” Social media allows him to educate many more people than individual patients, the 29-year-old told this news organization.
Inspiring Minorities
Tabhata Paulet, 27, started her TikTok presence as a premed student in 2021. She aimed to provide free resources to help low-income, first-generation Latinx students like herself study for standardized exams.
“I always looked online for guidance and resources, and the medical influencers did not share a similar background. So, I shared my story and what I had to do as a first-generation and first person in my family to become a physician. I did not have access to the same resources as my peers,” said Ms. Paulet, who was born in Peru and came to New Jersey as a child.
Students who are Hispanic, Latinx, or of Spanish origin made up 6.8% of total medical school enrollment in 2023-2024, up slightly from 6.7% in 2022-2023, according to the Association of American Medical Colleges (AAMC).
Ms. Paulet’s online presence grew when she began documenting her experiences as a first-year medical student, bridging the language barrier for Spanish-speaking patients so they could understand their diagnosis and treatment. She often posts about health disparity and barriers to care for underserved communities.
Most of her nearly 22,000 followers are Hispanic, said the now fourth-year student at Rutgers New Jersey Medical School in Newark, New Jersey. “I talk a lot about my interesting Spanish-speaking patients ... and how sometimes speaking their native language truly makes a difference in their care.”
She believes that she serves an important role in social media. “It can be very inspirational for those who come after you [in med school] to see someone from a similar culture and upbringing.”
Creating a Community
It was during a therapy session 4 years ago that Jeremy “JP” Scott decided to share Instagram posts about his experiences as a nontraditional medical student. The 37-year-old was studying at Ross University School of Medicine in Barbados and was feeling lonely as an international medical student training to be a doctor as a second career.
Before starting med school, Mr. Scott was an adjunct professor and lab supervisor at the University of Hartford Biology Department, West Hartford, Connecticut, and then a research assistant and lab manager at the Wistar Institute in Philadelphia.
Although he wanted to follow his mother’s path to becoming a doctor, it was more difficult than he envisioned, said the fourth-year student who completed clinical rotations in the United States and is now applying for residencies.
“I talked about how medical school is not what it appears to be ... There are a lot of challenges we are going through,” especially as people of color, he said.
Mr. Scott believes social media helps people feel included and less alone. He said many of his followers are med students and physicians.
His posts often focus on LGBTQIA+ pride and being a minority as a Black man in medicine.
“The pandemic spurred a lot of us. We had a racial reckoning in our country at the time. It inspired us to talk as Black creators and Black medical students.”
Black or African American medical students made up 8.5% of total med school enrollment in 2023-2024, a slight increase from 2022 to 2023, according to AAMC figures. Black men represented 7% of total enrollment in 2023-2024, while Black women represented 9.8%.
After only a handful of online posts in which Mr. Scott candidly discussed his mental health struggles and relationships, he attracted the attention of several medical apparel companies, including the popular FIGS scrubs. He’s now an ambassador for the company, which supports him and his content.
“My association with FIGS has helped attract a wider online audience, increasing my presence.” Today, he has 14,000 Instagram followers. “It opened up so many opportunities,” Mr. Scott said. One example is working with the national LGBTQIA+ community.
“The goal was never to be a social media influencer, to gain sponsorships or photo opportunities,” he said.
“My job, first, is as a medical student. Everything else is second. I am not trying to be a professional social media personality. I’m trying to be an actual physician.” He also tries to separate JP “social media” from Jeremy, the medical student.
“On Instagram, anyone can pull it up and see what you’re doing. The last thing I want is for them to think that I’m not serious about what I’m doing, that I’m not here to learn and become a doctor.”
Benefits and Drawbacks
Ms. Paulet said her social media following helped her connect with leaders in the Latinx medical community, including an obstetrics anesthesiologist, her intended specialty. “I don’t think I’d be able to do that without a social media platform.”
Her online activity also propelled her from regional to national leadership in the Latino Medical Student Association (LMSA). She now also runs their Instagram page, which has 14,000 followers.
Mr. Bervell believes social media is a great way to network. He’s connected with people he wouldn’t have met otherwise, including physicians. “I think it will help me get into a residency,” he said. “It allows people to know who you are ... They will be able to tell in a few videos the type of doctor I want to be.”
On the other hand, Mr. Bervell is aware of the negative impacts of social media on mental health. “You can get lost in social media.” For that reason, he often tries to disconnect. “I can go days without my phone.”
Posting on social media can be time-consuming, Mr. Bervell admitted. He said he spent about 2 hours a day researching, editing, and posting on TikTok when he first started building his following. Now, he spends about 2-3 hours a week creating videos. “I don’t post every day anymore. I don’t have the time.”
When she started building her TikTok presence, Ms. Paulet said she devoted 15 hours a week to the endeavor, but now she spends 10-12 hours a week posting online, including on LMSA’s Instagram page. “Whenever you are done with an exam or have a study break, this is something fun to do.” She also says you never know who you’re going to inspire when you put yourself out there.
“Talk about your journey, rotations, or your experience in your first or second year of medical school. Talk about milestones like board exams.”
Word to the Wise
Some students may be concerned that their posts might affect a potential residency program. But the medical students interviewed say they want to find programs that align with their values and accept them for who they are.
Mr. Scott said he’s not worried about someone not liking him because of who he is. “I am Black and openly gay. If it’s a problem, I don’t need to work with you or your institution.”
Mr. Bervell stressed that medical students should stay professional online. “I reach 5-10 million people a month, and I have to think: Would I want them to see this? You have to know at all times that someone is watching. I’m very careful about how I post. I script out every video.”
Mr. Scott agreed. He advises those interested in becoming medical influencers to know what they can’t post online. For example, to ensure safety and privacy, Mr. Scott doesn’t take photos in the hospital, show his medical badge, or post patient information. “You want to be respectful of your future medical profession,” he said.
“If it’s something my mother would be ashamed of, I don’t need to post about it.”
A version of this article first appeared on Medscape.com.
A medical student’s life is an endless cycle of classes, exams, clinical rotations, and residency preparation. On TikTok and Instagram, among other sites, they share medical school experiences and lessons learned in the classroom and advocate for causes such as increased diversity and gender rights in the medical field.
This news organization caught up with a few social media influencers with a large online following to learn how medical students can effectively use social media to build a professional brand and network. Most of the students interviewed said that their social media platforms offered an opportunity to educate others about significant medical developments, feel part of a community with a like-minded audience, and network with doctors who may lead them to a future residency or career path.
Many med students said that they built their large audiences by creating a platform for people of their ethnic background, nationality, race, gender, or simply what others weren’t already talking about. They said they saw a niche in social media that was missing or others hadn’t tackled in the same way.
When Joel Bervell began med school in 2020, he questioned some of the lessons he learned about how race is used in medical practice, which didn’t make sense to him. So, he began his own research. He had about 2000 followers on Instagram at the time.
Mr. Bervell read a new study about pulse oximeters and how they often produce misleading readings on patients with dark skin.
He wondered why he hadn’t learned this in medical school, so he posted it on TikTok. Within 24 hours, about 500,000 people viewed it. Most of the comments were from doctors, nurses, and physician assistants who said they weren’t aware of the disparity.
While his initial posts detailed his journey to medical school and a day-in-the-life of a medical student, he transitioned to posts primarily about race, health equity, and what he perceives as racial bias in medicine.
Now, the fourth-year Ghanaian-American student at the Elson S. Floyd College of Medicine at Washington State University Spokane has close to 1.2 million followers on Instagram and TikTok combined. He frequently visits the White House to advise on social media’s influence on healthcare and has appeared on the Kelly Clarkson Show, Good Morning America, CNN, and ABC, among others.
He said he also uses social media to translate complex medical information for a general audience, many of whom access health information online so they can manage their own healthcare. He sees his social media work as an extension of his medical education, allowing him to delve deeper into subjects and report on them as if he were publishing research in a medical journal.
“When I came to medical school, yes, I wanted to be a doctor. But I also wanted to impact people.” Social media allows him to educate many more people than individual patients, the 29-year-old told this news organization.
Inspiring Minorities
Tabhata Paulet, 27, started her TikTok presence as a premed student in 2021. She aimed to provide free resources to help low-income, first-generation Latinx students like herself study for standardized exams.
“I always looked online for guidance and resources, and the medical influencers did not share a similar background. So, I shared my story and what I had to do as a first-generation and first person in my family to become a physician. I did not have access to the same resources as my peers,” said Ms. Paulet, who was born in Peru and came to New Jersey as a child.
Students who are Hispanic, Latinx, or of Spanish origin made up 6.8% of total medical school enrollment in 2023-2024, up slightly from 6.7% in 2022-2023, according to the Association of American Medical Colleges (AAMC).
Ms. Paulet’s online presence grew when she began documenting her experiences as a first-year medical student, bridging the language barrier for Spanish-speaking patients so they could understand their diagnosis and treatment. She often posts about health disparity and barriers to care for underserved communities.
Most of her nearly 22,000 followers are Hispanic, said the now fourth-year student at Rutgers New Jersey Medical School in Newark, New Jersey. “I talk a lot about my interesting Spanish-speaking patients ... and how sometimes speaking their native language truly makes a difference in their care.”
She believes that she serves an important role in social media. “It can be very inspirational for those who come after you [in med school] to see someone from a similar culture and upbringing.”
Creating a Community
It was during a therapy session 4 years ago that Jeremy “JP” Scott decided to share Instagram posts about his experiences as a nontraditional medical student. The 37-year-old was studying at Ross University School of Medicine in Barbados and was feeling lonely as an international medical student training to be a doctor as a second career.
Before starting med school, Mr. Scott was an adjunct professor and lab supervisor at the University of Hartford Biology Department, West Hartford, Connecticut, and then a research assistant and lab manager at the Wistar Institute in Philadelphia.
Although he wanted to follow his mother’s path to becoming a doctor, it was more difficult than he envisioned, said the fourth-year student who completed clinical rotations in the United States and is now applying for residencies.
“I talked about how medical school is not what it appears to be ... There are a lot of challenges we are going through,” especially as people of color, he said.
Mr. Scott believes social media helps people feel included and less alone. He said many of his followers are med students and physicians.
His posts often focus on LGBTQIA+ pride and being a minority as a Black man in medicine.
“The pandemic spurred a lot of us. We had a racial reckoning in our country at the time. It inspired us to talk as Black creators and Black medical students.”
Black or African American medical students made up 8.5% of total med school enrollment in 2023-2024, a slight increase from 2022 to 2023, according to AAMC figures. Black men represented 7% of total enrollment in 2023-2024, while Black women represented 9.8%.
After only a handful of online posts in which Mr. Scott candidly discussed his mental health struggles and relationships, he attracted the attention of several medical apparel companies, including the popular FIGS scrubs. He’s now an ambassador for the company, which supports him and his content.
“My association with FIGS has helped attract a wider online audience, increasing my presence.” Today, he has 14,000 Instagram followers. “It opened up so many opportunities,” Mr. Scott said. One example is working with the national LGBTQIA+ community.
“The goal was never to be a social media influencer, to gain sponsorships or photo opportunities,” he said.
“My job, first, is as a medical student. Everything else is second. I am not trying to be a professional social media personality. I’m trying to be an actual physician.” He also tries to separate JP “social media” from Jeremy, the medical student.
“On Instagram, anyone can pull it up and see what you’re doing. The last thing I want is for them to think that I’m not serious about what I’m doing, that I’m not here to learn and become a doctor.”
Benefits and Drawbacks
Ms. Paulet said her social media following helped her connect with leaders in the Latinx medical community, including an obstetrics anesthesiologist, her intended specialty. “I don’t think I’d be able to do that without a social media platform.”
Her online activity also propelled her from regional to national leadership in the Latino Medical Student Association (LMSA). She now also runs their Instagram page, which has 14,000 followers.
Mr. Bervell believes social media is a great way to network. He’s connected with people he wouldn’t have met otherwise, including physicians. “I think it will help me get into a residency,” he said. “It allows people to know who you are ... They will be able to tell in a few videos the type of doctor I want to be.”
On the other hand, Mr. Bervell is aware of the negative impacts of social media on mental health. “You can get lost in social media.” For that reason, he often tries to disconnect. “I can go days without my phone.”
Posting on social media can be time-consuming, Mr. Bervell admitted. He said he spent about 2 hours a day researching, editing, and posting on TikTok when he first started building his following. Now, he spends about 2-3 hours a week creating videos. “I don’t post every day anymore. I don’t have the time.”
When she started building her TikTok presence, Ms. Paulet said she devoted 15 hours a week to the endeavor, but now she spends 10-12 hours a week posting online, including on LMSA’s Instagram page. “Whenever you are done with an exam or have a study break, this is something fun to do.” She also says you never know who you’re going to inspire when you put yourself out there.
“Talk about your journey, rotations, or your experience in your first or second year of medical school. Talk about milestones like board exams.”
Word to the Wise
Some students may be concerned that their posts might affect a potential residency program. But the medical students interviewed say they want to find programs that align with their values and accept them for who they are.
Mr. Scott said he’s not worried about someone not liking him because of who he is. “I am Black and openly gay. If it’s a problem, I don’t need to work with you or your institution.”
Mr. Bervell stressed that medical students should stay professional online. “I reach 5-10 million people a month, and I have to think: Would I want them to see this? You have to know at all times that someone is watching. I’m very careful about how I post. I script out every video.”
Mr. Scott agreed. He advises those interested in becoming medical influencers to know what they can’t post online. For example, to ensure safety and privacy, Mr. Scott doesn’t take photos in the hospital, show his medical badge, or post patient information. “You want to be respectful of your future medical profession,” he said.
“If it’s something my mother would be ashamed of, I don’t need to post about it.”
A version of this article first appeared on Medscape.com.
Revamping Resident Schedules to Reduce Burnout
It’s the difference between running a marathon and taking a leisurely stroll. That’s how recent pediatrics resident Joey Whelihan, MD, compared an 11-hour inpatient hospital day with an 8-hour outpatient shift where residents see patients in a clinic.
With inpatient training, “you are lucky if you have time to cook dinner, go to bed, and get ready for the next day,” said Dr. Whelihan, who recently started his adolescent medicine fellowship at Children’s Hospital of Philadelphia after 3 years of residency there. Some residents have call every fourth day during inpatient rotations, working 24-28 hours at a time. They come in one morning and go home the next, he told this news organization.
“Outpatient blocks give you more time to catch your breath and feel somewhat refreshed and ready to take care of patients.”
Longer stretches of inpatient rotations are not sustainable, Dr. Whelihan added, and residents are likely to become exhausted. Fatigue is a leading cause of burnout, a mental, physical, and emotional challenge that residency programs and national medical organizations have been struggling to address.
In recent years, there has been a movement to reduce the maximum consecutive duration of resident duty hours in residency programs across the country. Fueled by resident health and patient safety concerns, the movement is a shift from the previous 24- to 36-hour call duty schedules.
Improved Call Systems = Better Residents
The connection between burnout, well-being, and work schedules appears regularly in national program standards. “Residents and faculty members are at risk for burnout and depression,” according to the current Accreditation Council for Graduate Medical Education’s standard residency program requirements.
“Programs, in partnership with their sponsoring institutions, have the same responsibility to address well-being as other aspects of resident competence,” the guidelines state. That charge includes “attention to scheduling, work intensity, and work compression that impacts resident well-being.”
In Medscape’s Residents Lifestyle & Happiness Report 2023, a third of residents surveyed rarely or never paid attention to their well-being, which closely mirrors the 31% who rarely or never had time for a social life. Slightly more residents (37%) said their work-life balance was “somewhat worse” or “much worse” than they expected.
“I think everyone has burnout as a resident, regardless of the type of program they are in,” Dr. Whelihan said. He described the experience as when you lack fulfillment and empathy and feel exhausted, callous, and removed from interactions with colleagues and patients.
The American Medical Association’s recently released report on the state of residency well-being in 2023 also found that about 43% of residents and fellows had at least one symptom of burnout, about a 2% increase from 2022.
Efforts to Combat Burnout
One residency program found a way to reduce burnout by changing its block scheduling from 4 inpatient weeks followed by 1 outpatient week (4 + 1) to 4 inpatient call-based weeks and 4 outpatient ambulatory, non-call weeks (4 + 4), according to a survey study published recently in JAMA Network Open. The initiative drew praise from some residents and a med school professor who studies wellness issues.
In the survey of postgraduate year (PGY) 1 and PGY-2 hospitalist and primary care residents from the University of Colorado’s Internal Medicine Residency Program, Aurora, between June 2019 and June 2021, the schedule change resulted in improved burnout scores and self-reported professional, educational, and health benefits.
As part of the survey, residents rated symptoms on a 7-point scale on the basis of how frequently they experienced emotional exhaustion, depersonalization, and personal accomplishment.
Investigators also used a questionnaire to evaluate how participants perceived the rotation structure with various outcomes, including the ability to acquire clinical skills, access educational and scholarly opportunities, job satisfaction, and health.
The study concluded that the schedule change improved burnout, health, wellness, and professional development without weakening residents perceived clinical skills or standardized exam scores.
Still, the study authors acknowledged that several factors, including the pandemic, may have limited the findings. During that time, the study transitioned from in-person to electronic submissions, resulting in reduced response rates because of changes in staffing needs and fewer research and scholarly activities.
“One of the things we worried about was that the pandemic would make [burnout findings] look worse,” said lead author Dan Heppe, MD, a hospitalist and associate director of the CU Internal Medicine Residency Program. “Anecdotally, residents may have had more support in our program than perhaps some other programs. Though they had long hours with very sick patients, we tried to keep going in a positive direction.”
Dr. Heppe said in an interview that the purpose of the schedule change was to space out more intense rotations and build in more time for research, leadership, teaching, and professional development. He suggested the new schedule could help with other aspects of residents’ careers, exposing them to alternate avenues earlier in their training and in a more structured way.
Like most of the study authors, Dr. Heppe is a graduate of the residency program. He recalled how the program changed from multiple inpatient months in a row with clinic half days during those rotations to a 4 + 1 schedule. But the 1 week between inpatient rotations wasn’t enough time to recover or catch up on clinical work, said Dr. Heppe, who is also an associate professor of medicine at CU.
“It was too erratic,” he said of his former residency schedule. “There was a month of research here or there and clinic and then right back to the ICU for a couple of months without a break, and it was less predictable.”
Dr. Heppe said other residency programs have expressed interest in duplicating CU’s schedule change. He admits it may be difficult because of intensive schedule coordination, and some hospitals may not want to reduce clinical services.
The Yale Internal Medicine Traditional Residency Program also recently ended its 28-hour call, during which residents worked 24 hours with an additional 4 hours to transfer the patient to the incoming team. The move was made in response to residents’ requests, saying that the grueling call rotation’s time had come. The reaction has been overwhelmingly positive.
Proponents of alternate scheduling blocks [4 + 4 or 6 + 2] say that they improve residents’ educational experience, patient care, and continuity of care, reduce burnout, and guarantee residents time off.
Advancing Resident Well-Being
“The premise of looking at scheduling in a more intentional way is a sound one in the process of trying to support and advance resident well-being,” said Mark Greenawald, MD, vice chair of academic affairs, well-being, and professional development for the Virginia Tech Carilion School of Medicine’s Department of Family and Community Medicine in Roanoke.
He said it’s up to residency program directors or graduate medical education departments within a specialty to determine whether such scheduling changes fit their requirements for inpatient and outpatient care and training electives. Requirements may limit some scheduling changes, but within the specialty, there’s some flexibility to be creative with rotations. The CU study considered how to create a residency rhythm without stacking inpatient rotations so there’s recovery time.
“Human beings need a break. If residents work 80 hours continually, they will start to experience greater distress, which for many leads to burnout,” he said
Still, the study includes design flaws because it doesn’t explain how call times and hours differ between inpatient and outpatient rotations. “My own [family medicine] program also does outpatient clinics when we have inpatient service. We have half days in the clinic, which ensures better continuity care with the patient.”
Dr. Greenawald has yet to see much research published about the impact of resident schedule changes. By taking an experimental approach, the CU study showed that their particular change positively affected burnout. If the study leads to improvements in rotation schedules or encourages other programs to experiment with their schedules, it will be a step in the right direction.
How Residents Respond
Haidn Foster, MD, a third-year internal medicine resident at Penn State Health Milton S. Hershey Medical Center, Hershey, remembered experiencing burnout as an intern. At that time, he occasionally dealt with poor patient outcomes and sick patients while working long hours with only 1 day off each week. During a particularly challenging rotation, he felt overwhelmed and numb, which was exacerbated if a patient’s condition worsened or they passed away, he said.
His program follows a schedule of 6 weeks of inpatient training and 2 weeks of outpatient rotations (6 + 2). He said that restructuring residents’ schedules may be more effective than commonly used individual wellness modules, referring to the CU study. “The authors tried out a novel systematic way to tackle the epidemic of physician burnout overwhelming people in the medical community.”
Although the study found that schedule changes don’t affect standardized exam scores, Dr. Foster wondered about preceptor ratings, another marker for clinical competency.
He said future studies should attempt to change the structure of medical training delivery by evaluating models that best reduce burnout, are consistent with residents’ career goals, and produce competent physicians. “Burnout plagues our medical system and leads to too many physicians and physicians-in-training leaving the field or taking their lives. I’m not sure this particular mechanism gets us there, but it’s a step, and so that’s very important.”
Like Dr. Foster, Dr. Whelihan follows a 6 + 2 schedule. He said he would have welcomed a schedule that included more outpatient and less inpatient training and can see how changes in scheduling could reduce burnout. “More outpatient time gives you an opportunity to breathe. You get a little more time off working in clinic with less sick people at a slower pace.”
Ally Fuher, MD, said she chose CU’s Internal Medicine Residency Program 4 years ago largely because of its innovative schedule. Now the program’s chief medical resident, she knew the structure would give her more time to pursue other nonclinical interests including research and medical education, meet regularly with mentors, visit family in another state, and attend important life events.
She acknowledged that the alternative would have meant a more irregular schedule with the possibility of working as many as 80 hours a week on back-to-back inpatient rotations with only 1 day off a week, leaving minimal time to plan other activities, let alone rest and recover.
Dr. Fuher said a balanced schedule made her a more well-rounded person excited to engage in her profession. While she hasn’t personally experienced burnout, she realizes a schedule change may not completely solve the issue for others. However, it shows what progress programs can make when they create systemic structural change.
A version of this article first appeared on Medscape.com.
It’s the difference between running a marathon and taking a leisurely stroll. That’s how recent pediatrics resident Joey Whelihan, MD, compared an 11-hour inpatient hospital day with an 8-hour outpatient shift where residents see patients in a clinic.
With inpatient training, “you are lucky if you have time to cook dinner, go to bed, and get ready for the next day,” said Dr. Whelihan, who recently started his adolescent medicine fellowship at Children’s Hospital of Philadelphia after 3 years of residency there. Some residents have call every fourth day during inpatient rotations, working 24-28 hours at a time. They come in one morning and go home the next, he told this news organization.
“Outpatient blocks give you more time to catch your breath and feel somewhat refreshed and ready to take care of patients.”
Longer stretches of inpatient rotations are not sustainable, Dr. Whelihan added, and residents are likely to become exhausted. Fatigue is a leading cause of burnout, a mental, physical, and emotional challenge that residency programs and national medical organizations have been struggling to address.
In recent years, there has been a movement to reduce the maximum consecutive duration of resident duty hours in residency programs across the country. Fueled by resident health and patient safety concerns, the movement is a shift from the previous 24- to 36-hour call duty schedules.
Improved Call Systems = Better Residents
The connection between burnout, well-being, and work schedules appears regularly in national program standards. “Residents and faculty members are at risk for burnout and depression,” according to the current Accreditation Council for Graduate Medical Education’s standard residency program requirements.
“Programs, in partnership with their sponsoring institutions, have the same responsibility to address well-being as other aspects of resident competence,” the guidelines state. That charge includes “attention to scheduling, work intensity, and work compression that impacts resident well-being.”
In Medscape’s Residents Lifestyle & Happiness Report 2023, a third of residents surveyed rarely or never paid attention to their well-being, which closely mirrors the 31% who rarely or never had time for a social life. Slightly more residents (37%) said their work-life balance was “somewhat worse” or “much worse” than they expected.
“I think everyone has burnout as a resident, regardless of the type of program they are in,” Dr. Whelihan said. He described the experience as when you lack fulfillment and empathy and feel exhausted, callous, and removed from interactions with colleagues and patients.
The American Medical Association’s recently released report on the state of residency well-being in 2023 also found that about 43% of residents and fellows had at least one symptom of burnout, about a 2% increase from 2022.
Efforts to Combat Burnout
One residency program found a way to reduce burnout by changing its block scheduling from 4 inpatient weeks followed by 1 outpatient week (4 + 1) to 4 inpatient call-based weeks and 4 outpatient ambulatory, non-call weeks (4 + 4), according to a survey study published recently in JAMA Network Open. The initiative drew praise from some residents and a med school professor who studies wellness issues.
In the survey of postgraduate year (PGY) 1 and PGY-2 hospitalist and primary care residents from the University of Colorado’s Internal Medicine Residency Program, Aurora, between June 2019 and June 2021, the schedule change resulted in improved burnout scores and self-reported professional, educational, and health benefits.
As part of the survey, residents rated symptoms on a 7-point scale on the basis of how frequently they experienced emotional exhaustion, depersonalization, and personal accomplishment.
Investigators also used a questionnaire to evaluate how participants perceived the rotation structure with various outcomes, including the ability to acquire clinical skills, access educational and scholarly opportunities, job satisfaction, and health.
The study concluded that the schedule change improved burnout, health, wellness, and professional development without weakening residents perceived clinical skills or standardized exam scores.
Still, the study authors acknowledged that several factors, including the pandemic, may have limited the findings. During that time, the study transitioned from in-person to electronic submissions, resulting in reduced response rates because of changes in staffing needs and fewer research and scholarly activities.
“One of the things we worried about was that the pandemic would make [burnout findings] look worse,” said lead author Dan Heppe, MD, a hospitalist and associate director of the CU Internal Medicine Residency Program. “Anecdotally, residents may have had more support in our program than perhaps some other programs. Though they had long hours with very sick patients, we tried to keep going in a positive direction.”
Dr. Heppe said in an interview that the purpose of the schedule change was to space out more intense rotations and build in more time for research, leadership, teaching, and professional development. He suggested the new schedule could help with other aspects of residents’ careers, exposing them to alternate avenues earlier in their training and in a more structured way.
Like most of the study authors, Dr. Heppe is a graduate of the residency program. He recalled how the program changed from multiple inpatient months in a row with clinic half days during those rotations to a 4 + 1 schedule. But the 1 week between inpatient rotations wasn’t enough time to recover or catch up on clinical work, said Dr. Heppe, who is also an associate professor of medicine at CU.
“It was too erratic,” he said of his former residency schedule. “There was a month of research here or there and clinic and then right back to the ICU for a couple of months without a break, and it was less predictable.”
Dr. Heppe said other residency programs have expressed interest in duplicating CU’s schedule change. He admits it may be difficult because of intensive schedule coordination, and some hospitals may not want to reduce clinical services.
The Yale Internal Medicine Traditional Residency Program also recently ended its 28-hour call, during which residents worked 24 hours with an additional 4 hours to transfer the patient to the incoming team. The move was made in response to residents’ requests, saying that the grueling call rotation’s time had come. The reaction has been overwhelmingly positive.
Proponents of alternate scheduling blocks [4 + 4 or 6 + 2] say that they improve residents’ educational experience, patient care, and continuity of care, reduce burnout, and guarantee residents time off.
Advancing Resident Well-Being
“The premise of looking at scheduling in a more intentional way is a sound one in the process of trying to support and advance resident well-being,” said Mark Greenawald, MD, vice chair of academic affairs, well-being, and professional development for the Virginia Tech Carilion School of Medicine’s Department of Family and Community Medicine in Roanoke.
He said it’s up to residency program directors or graduate medical education departments within a specialty to determine whether such scheduling changes fit their requirements for inpatient and outpatient care and training electives. Requirements may limit some scheduling changes, but within the specialty, there’s some flexibility to be creative with rotations. The CU study considered how to create a residency rhythm without stacking inpatient rotations so there’s recovery time.
“Human beings need a break. If residents work 80 hours continually, they will start to experience greater distress, which for many leads to burnout,” he said
Still, the study includes design flaws because it doesn’t explain how call times and hours differ between inpatient and outpatient rotations. “My own [family medicine] program also does outpatient clinics when we have inpatient service. We have half days in the clinic, which ensures better continuity care with the patient.”
Dr. Greenawald has yet to see much research published about the impact of resident schedule changes. By taking an experimental approach, the CU study showed that their particular change positively affected burnout. If the study leads to improvements in rotation schedules or encourages other programs to experiment with their schedules, it will be a step in the right direction.
How Residents Respond
Haidn Foster, MD, a third-year internal medicine resident at Penn State Health Milton S. Hershey Medical Center, Hershey, remembered experiencing burnout as an intern. At that time, he occasionally dealt with poor patient outcomes and sick patients while working long hours with only 1 day off each week. During a particularly challenging rotation, he felt overwhelmed and numb, which was exacerbated if a patient’s condition worsened or they passed away, he said.
His program follows a schedule of 6 weeks of inpatient training and 2 weeks of outpatient rotations (6 + 2). He said that restructuring residents’ schedules may be more effective than commonly used individual wellness modules, referring to the CU study. “The authors tried out a novel systematic way to tackle the epidemic of physician burnout overwhelming people in the medical community.”
Although the study found that schedule changes don’t affect standardized exam scores, Dr. Foster wondered about preceptor ratings, another marker for clinical competency.
He said future studies should attempt to change the structure of medical training delivery by evaluating models that best reduce burnout, are consistent with residents’ career goals, and produce competent physicians. “Burnout plagues our medical system and leads to too many physicians and physicians-in-training leaving the field or taking their lives. I’m not sure this particular mechanism gets us there, but it’s a step, and so that’s very important.”
Like Dr. Foster, Dr. Whelihan follows a 6 + 2 schedule. He said he would have welcomed a schedule that included more outpatient and less inpatient training and can see how changes in scheduling could reduce burnout. “More outpatient time gives you an opportunity to breathe. You get a little more time off working in clinic with less sick people at a slower pace.”
Ally Fuher, MD, said she chose CU’s Internal Medicine Residency Program 4 years ago largely because of its innovative schedule. Now the program’s chief medical resident, she knew the structure would give her more time to pursue other nonclinical interests including research and medical education, meet regularly with mentors, visit family in another state, and attend important life events.
She acknowledged that the alternative would have meant a more irregular schedule with the possibility of working as many as 80 hours a week on back-to-back inpatient rotations with only 1 day off a week, leaving minimal time to plan other activities, let alone rest and recover.
Dr. Fuher said a balanced schedule made her a more well-rounded person excited to engage in her profession. While she hasn’t personally experienced burnout, she realizes a schedule change may not completely solve the issue for others. However, it shows what progress programs can make when they create systemic structural change.
A version of this article first appeared on Medscape.com.
It’s the difference between running a marathon and taking a leisurely stroll. That’s how recent pediatrics resident Joey Whelihan, MD, compared an 11-hour inpatient hospital day with an 8-hour outpatient shift where residents see patients in a clinic.
With inpatient training, “you are lucky if you have time to cook dinner, go to bed, and get ready for the next day,” said Dr. Whelihan, who recently started his adolescent medicine fellowship at Children’s Hospital of Philadelphia after 3 years of residency there. Some residents have call every fourth day during inpatient rotations, working 24-28 hours at a time. They come in one morning and go home the next, he told this news organization.
“Outpatient blocks give you more time to catch your breath and feel somewhat refreshed and ready to take care of patients.”
Longer stretches of inpatient rotations are not sustainable, Dr. Whelihan added, and residents are likely to become exhausted. Fatigue is a leading cause of burnout, a mental, physical, and emotional challenge that residency programs and national medical organizations have been struggling to address.
In recent years, there has been a movement to reduce the maximum consecutive duration of resident duty hours in residency programs across the country. Fueled by resident health and patient safety concerns, the movement is a shift from the previous 24- to 36-hour call duty schedules.
Improved Call Systems = Better Residents
The connection between burnout, well-being, and work schedules appears regularly in national program standards. “Residents and faculty members are at risk for burnout and depression,” according to the current Accreditation Council for Graduate Medical Education’s standard residency program requirements.
“Programs, in partnership with their sponsoring institutions, have the same responsibility to address well-being as other aspects of resident competence,” the guidelines state. That charge includes “attention to scheduling, work intensity, and work compression that impacts resident well-being.”
In Medscape’s Residents Lifestyle & Happiness Report 2023, a third of residents surveyed rarely or never paid attention to their well-being, which closely mirrors the 31% who rarely or never had time for a social life. Slightly more residents (37%) said their work-life balance was “somewhat worse” or “much worse” than they expected.
“I think everyone has burnout as a resident, regardless of the type of program they are in,” Dr. Whelihan said. He described the experience as when you lack fulfillment and empathy and feel exhausted, callous, and removed from interactions with colleagues and patients.
The American Medical Association’s recently released report on the state of residency well-being in 2023 also found that about 43% of residents and fellows had at least one symptom of burnout, about a 2% increase from 2022.
Efforts to Combat Burnout
One residency program found a way to reduce burnout by changing its block scheduling from 4 inpatient weeks followed by 1 outpatient week (4 + 1) to 4 inpatient call-based weeks and 4 outpatient ambulatory, non-call weeks (4 + 4), according to a survey study published recently in JAMA Network Open. The initiative drew praise from some residents and a med school professor who studies wellness issues.
In the survey of postgraduate year (PGY) 1 and PGY-2 hospitalist and primary care residents from the University of Colorado’s Internal Medicine Residency Program, Aurora, between June 2019 and June 2021, the schedule change resulted in improved burnout scores and self-reported professional, educational, and health benefits.
As part of the survey, residents rated symptoms on a 7-point scale on the basis of how frequently they experienced emotional exhaustion, depersonalization, and personal accomplishment.
Investigators also used a questionnaire to evaluate how participants perceived the rotation structure with various outcomes, including the ability to acquire clinical skills, access educational and scholarly opportunities, job satisfaction, and health.
The study concluded that the schedule change improved burnout, health, wellness, and professional development without weakening residents perceived clinical skills or standardized exam scores.
Still, the study authors acknowledged that several factors, including the pandemic, may have limited the findings. During that time, the study transitioned from in-person to electronic submissions, resulting in reduced response rates because of changes in staffing needs and fewer research and scholarly activities.
“One of the things we worried about was that the pandemic would make [burnout findings] look worse,” said lead author Dan Heppe, MD, a hospitalist and associate director of the CU Internal Medicine Residency Program. “Anecdotally, residents may have had more support in our program than perhaps some other programs. Though they had long hours with very sick patients, we tried to keep going in a positive direction.”
Dr. Heppe said in an interview that the purpose of the schedule change was to space out more intense rotations and build in more time for research, leadership, teaching, and professional development. He suggested the new schedule could help with other aspects of residents’ careers, exposing them to alternate avenues earlier in their training and in a more structured way.
Like most of the study authors, Dr. Heppe is a graduate of the residency program. He recalled how the program changed from multiple inpatient months in a row with clinic half days during those rotations to a 4 + 1 schedule. But the 1 week between inpatient rotations wasn’t enough time to recover or catch up on clinical work, said Dr. Heppe, who is also an associate professor of medicine at CU.
“It was too erratic,” he said of his former residency schedule. “There was a month of research here or there and clinic and then right back to the ICU for a couple of months without a break, and it was less predictable.”
Dr. Heppe said other residency programs have expressed interest in duplicating CU’s schedule change. He admits it may be difficult because of intensive schedule coordination, and some hospitals may not want to reduce clinical services.
The Yale Internal Medicine Traditional Residency Program also recently ended its 28-hour call, during which residents worked 24 hours with an additional 4 hours to transfer the patient to the incoming team. The move was made in response to residents’ requests, saying that the grueling call rotation’s time had come. The reaction has been overwhelmingly positive.
Proponents of alternate scheduling blocks [4 + 4 or 6 + 2] say that they improve residents’ educational experience, patient care, and continuity of care, reduce burnout, and guarantee residents time off.
Advancing Resident Well-Being
“The premise of looking at scheduling in a more intentional way is a sound one in the process of trying to support and advance resident well-being,” said Mark Greenawald, MD, vice chair of academic affairs, well-being, and professional development for the Virginia Tech Carilion School of Medicine’s Department of Family and Community Medicine in Roanoke.
He said it’s up to residency program directors or graduate medical education departments within a specialty to determine whether such scheduling changes fit their requirements for inpatient and outpatient care and training electives. Requirements may limit some scheduling changes, but within the specialty, there’s some flexibility to be creative with rotations. The CU study considered how to create a residency rhythm without stacking inpatient rotations so there’s recovery time.
“Human beings need a break. If residents work 80 hours continually, they will start to experience greater distress, which for many leads to burnout,” he said
Still, the study includes design flaws because it doesn’t explain how call times and hours differ between inpatient and outpatient rotations. “My own [family medicine] program also does outpatient clinics when we have inpatient service. We have half days in the clinic, which ensures better continuity care with the patient.”
Dr. Greenawald has yet to see much research published about the impact of resident schedule changes. By taking an experimental approach, the CU study showed that their particular change positively affected burnout. If the study leads to improvements in rotation schedules or encourages other programs to experiment with their schedules, it will be a step in the right direction.
How Residents Respond
Haidn Foster, MD, a third-year internal medicine resident at Penn State Health Milton S. Hershey Medical Center, Hershey, remembered experiencing burnout as an intern. At that time, he occasionally dealt with poor patient outcomes and sick patients while working long hours with only 1 day off each week. During a particularly challenging rotation, he felt overwhelmed and numb, which was exacerbated if a patient’s condition worsened or they passed away, he said.
His program follows a schedule of 6 weeks of inpatient training and 2 weeks of outpatient rotations (6 + 2). He said that restructuring residents’ schedules may be more effective than commonly used individual wellness modules, referring to the CU study. “The authors tried out a novel systematic way to tackle the epidemic of physician burnout overwhelming people in the medical community.”
Although the study found that schedule changes don’t affect standardized exam scores, Dr. Foster wondered about preceptor ratings, another marker for clinical competency.
He said future studies should attempt to change the structure of medical training delivery by evaluating models that best reduce burnout, are consistent with residents’ career goals, and produce competent physicians. “Burnout plagues our medical system and leads to too many physicians and physicians-in-training leaving the field or taking their lives. I’m not sure this particular mechanism gets us there, but it’s a step, and so that’s very important.”
Like Dr. Foster, Dr. Whelihan follows a 6 + 2 schedule. He said he would have welcomed a schedule that included more outpatient and less inpatient training and can see how changes in scheduling could reduce burnout. “More outpatient time gives you an opportunity to breathe. You get a little more time off working in clinic with less sick people at a slower pace.”
Ally Fuher, MD, said she chose CU’s Internal Medicine Residency Program 4 years ago largely because of its innovative schedule. Now the program’s chief medical resident, she knew the structure would give her more time to pursue other nonclinical interests including research and medical education, meet regularly with mentors, visit family in another state, and attend important life events.
She acknowledged that the alternative would have meant a more irregular schedule with the possibility of working as many as 80 hours a week on back-to-back inpatient rotations with only 1 day off a week, leaving minimal time to plan other activities, let alone rest and recover.
Dr. Fuher said a balanced schedule made her a more well-rounded person excited to engage in her profession. While she hasn’t personally experienced burnout, she realizes a schedule change may not completely solve the issue for others. However, it shows what progress programs can make when they create systemic structural change.
A version of this article first appeared on Medscape.com.
After the Match: Next steps for new residents, unmatched
Medical school graduates around the US took to social media after last week's Match Day to share their joy ― or explore their options if they did not match.
Take this post March 19 on Twitter: “I went unmatched this year; looking for research position at any institute for internal medicine.”
including an international medical graduate who matched into his chosen specialty after multiple disappointments.
“I’ve waited for this email for 8 years,” Sahil Bawa, MD, posted on Twitter on March 13. A few days later, when he learned about his residency position, he posted: “I’m beyond grateful. Will be moving to Alabama soon #familymedicine.”
Dr. Bawa, who matched into UAB Medicine Selma (Ala.), graduated from medical school in India in 2014. He said in an interview that he has visited the United States periodically since then to pass medical tests, obtain letters of recommendation, and participate in research.
Over the years he watched his Indian colleagues give up on becoming American doctors, find alternative careers, or resolve to practice in their native country. But he held onto the few success stories he saw on social media. “There were always one to two every year. It kept me going. If they can do it, I can do it.”
International medical graduates (IMGs) like Dr. Bawa applied in record numbers to Match2023, according to the National Resident Matching Program (NRMP), which announced the results on March 13 of its main residency match and the Supplemental Offer and Acceptance Program (SOAP) for unfilled positions or unmatched applicants.
Overall, 48,156 total applicants registered for the match, which was driven by the increase of non-U.S. IMG applicants and U.S. DO seniors over the past year, NRMP stated in its release. U.S. MD seniors had a match rate of nearly 94%, and U.S. DO seniors, nearly 92%. U.S. IMGs had a match rate of nearly 68%, an “all-time high,” and non-U.S. IMGs, nearly 60%, NRMP stated.
Three specialties that filled all of their 30 or more available positions were orthopedic surgery, plastic surgery (integrated), radiology – diagnostic, and thoracic surgery. Specialties with 30 or more positions that filled with the highest percentage of U.S. MD and DO seniors were plastic surgery (integrated), internal medicine-pediatrics, ob.gyn., and orthopedic surgery.
The number of available primary care positions increased slightly, NRMP reported. Considering “a serious and growing shortage of primary care physicians across the U.S.,” there were 571 more primary care positions than 2022. That’s an increase of about 3% over last year and 17% over the past 5 years. Primary care positions filled at a rate of 94%, which remained steady from 2022.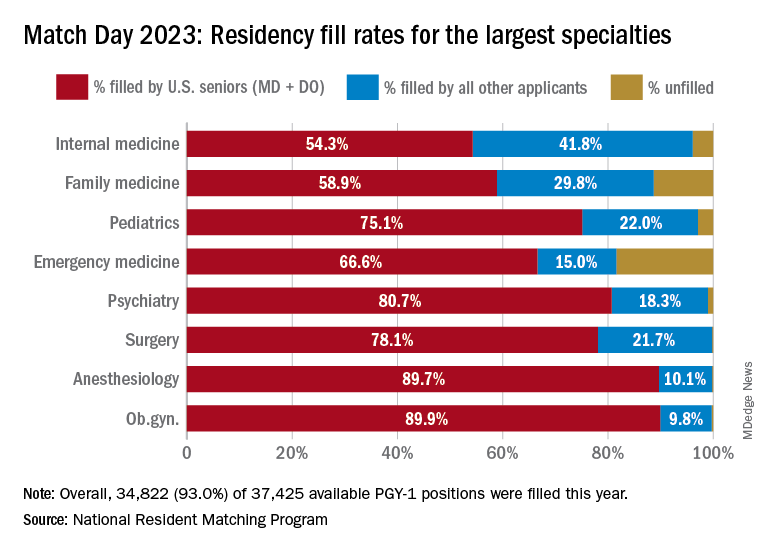
NRMP also pointed out specialties with increases in the number of positions filled by U.S. MD seniors of more than 10% and 10 positions in the past 5 years: anesthesiology, child neurology, interventional radiology, neurology, pathology, physical medicine and rehabilitation, plastic surgery (integrated), psychiatry, radiology-diagnostic, transitional year, and vascular surgery.
Bryan Carmody, MD, MPH, a pediatric nephrologist known for his medical school commentaries, said in an interview that the most competitive specialties he noted in 2023 were radiology, pathology, and neurology.
“The surgical specialties are always competitive, so it wasn’t a surprise that orthopedics, plastic surgery, and thoracic surgery filled all of their positions. But I was surprised to see diagnostic radiology fill every single one of their positions in the match. And although pathology and neurology aren’t typically considered extremely competitive specialties, they filled over 99% of their positions in the Match this year.”
On Dr. Carmody’s blog about the winners and losers of Match Day, he said that despite the record number of primary care positions offered, family medicine programs suffered. “Only 89% of family medicine programs filled in the Match, and graduating U.S. MD and DO students only filled a little more than half of all the available positions,” he wrote.
For a record number of applicants that match each year, and “the most favorable ratio in the past 2 decades” of applicants-to-positions in 2023, there are still a lot unmatched, Dr. Carmody said. “It’s a tough thing to talk about. The reality is the number of residency positions should be determined by the number of physicians needed.”
One student, Asim Ansari, didn’t match into a traditional residency or through SOAP. It was his fifth attempt. He was serving a transitional-year residency at Merit Health Wesley in Hattiesburg, Miss., and when he didn’t match, he accepted a child and adolescent psychiatry fellowship at the University of Kansas Medical Center, Kansas City.
He said he was “relieved and excited” to have found a program in his chosen specialty. Still, in 2 years, Mr. Ansari must again try to match into a traditional psychiatry residency.
Meanwhile, Dr. Bawa will prepare for his 3-year residency in Alabama after completing his interim research year in the surgery department at Wayne State University, Detroit, in May.
Despite his years in limbo, Dr. Bawa said, “I have no regrets, no complaints. I am still very happy.”
A version of this article originally appeared on Medscape.com.
Medical school graduates around the US took to social media after last week's Match Day to share their joy ― or explore their options if they did not match.
Take this post March 19 on Twitter: “I went unmatched this year; looking for research position at any institute for internal medicine.”
including an international medical graduate who matched into his chosen specialty after multiple disappointments.
“I’ve waited for this email for 8 years,” Sahil Bawa, MD, posted on Twitter on March 13. A few days later, when he learned about his residency position, he posted: “I’m beyond grateful. Will be moving to Alabama soon #familymedicine.”
Dr. Bawa, who matched into UAB Medicine Selma (Ala.), graduated from medical school in India in 2014. He said in an interview that he has visited the United States periodically since then to pass medical tests, obtain letters of recommendation, and participate in research.
Over the years he watched his Indian colleagues give up on becoming American doctors, find alternative careers, or resolve to practice in their native country. But he held onto the few success stories he saw on social media. “There were always one to two every year. It kept me going. If they can do it, I can do it.”
International medical graduates (IMGs) like Dr. Bawa applied in record numbers to Match2023, according to the National Resident Matching Program (NRMP), which announced the results on March 13 of its main residency match and the Supplemental Offer and Acceptance Program (SOAP) for unfilled positions or unmatched applicants.
Overall, 48,156 total applicants registered for the match, which was driven by the increase of non-U.S. IMG applicants and U.S. DO seniors over the past year, NRMP stated in its release. U.S. MD seniors had a match rate of nearly 94%, and U.S. DO seniors, nearly 92%. U.S. IMGs had a match rate of nearly 68%, an “all-time high,” and non-U.S. IMGs, nearly 60%, NRMP stated.
Three specialties that filled all of their 30 or more available positions were orthopedic surgery, plastic surgery (integrated), radiology – diagnostic, and thoracic surgery. Specialties with 30 or more positions that filled with the highest percentage of U.S. MD and DO seniors were plastic surgery (integrated), internal medicine-pediatrics, ob.gyn., and orthopedic surgery.
The number of available primary care positions increased slightly, NRMP reported. Considering “a serious and growing shortage of primary care physicians across the U.S.,” there were 571 more primary care positions than 2022. That’s an increase of about 3% over last year and 17% over the past 5 years. Primary care positions filled at a rate of 94%, which remained steady from 2022.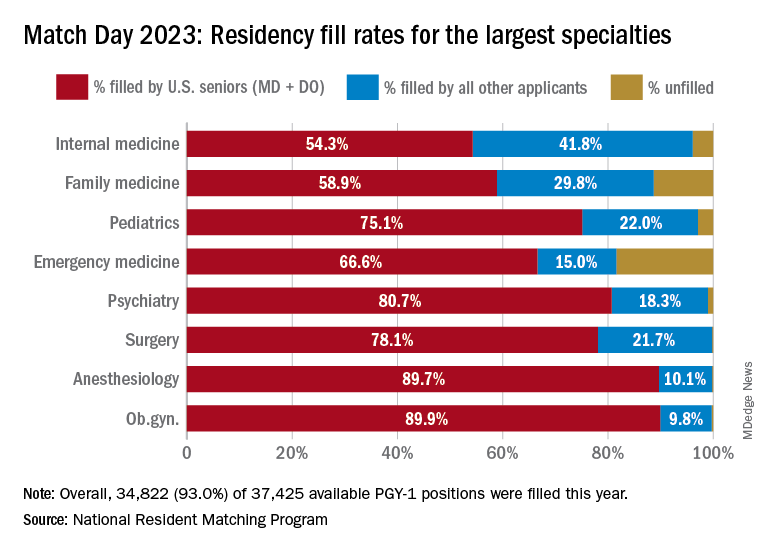
NRMP also pointed out specialties with increases in the number of positions filled by U.S. MD seniors of more than 10% and 10 positions in the past 5 years: anesthesiology, child neurology, interventional radiology, neurology, pathology, physical medicine and rehabilitation, plastic surgery (integrated), psychiatry, radiology-diagnostic, transitional year, and vascular surgery.
Bryan Carmody, MD, MPH, a pediatric nephrologist known for his medical school commentaries, said in an interview that the most competitive specialties he noted in 2023 were radiology, pathology, and neurology.
“The surgical specialties are always competitive, so it wasn’t a surprise that orthopedics, plastic surgery, and thoracic surgery filled all of their positions. But I was surprised to see diagnostic radiology fill every single one of their positions in the match. And although pathology and neurology aren’t typically considered extremely competitive specialties, they filled over 99% of their positions in the Match this year.”
On Dr. Carmody’s blog about the winners and losers of Match Day, he said that despite the record number of primary care positions offered, family medicine programs suffered. “Only 89% of family medicine programs filled in the Match, and graduating U.S. MD and DO students only filled a little more than half of all the available positions,” he wrote.
For a record number of applicants that match each year, and “the most favorable ratio in the past 2 decades” of applicants-to-positions in 2023, there are still a lot unmatched, Dr. Carmody said. “It’s a tough thing to talk about. The reality is the number of residency positions should be determined by the number of physicians needed.”
One student, Asim Ansari, didn’t match into a traditional residency or through SOAP. It was his fifth attempt. He was serving a transitional-year residency at Merit Health Wesley in Hattiesburg, Miss., and when he didn’t match, he accepted a child and adolescent psychiatry fellowship at the University of Kansas Medical Center, Kansas City.
He said he was “relieved and excited” to have found a program in his chosen specialty. Still, in 2 years, Mr. Ansari must again try to match into a traditional psychiatry residency.
Meanwhile, Dr. Bawa will prepare for his 3-year residency in Alabama after completing his interim research year in the surgery department at Wayne State University, Detroit, in May.
Despite his years in limbo, Dr. Bawa said, “I have no regrets, no complaints. I am still very happy.”
A version of this article originally appeared on Medscape.com.
Medical school graduates around the US took to social media after last week's Match Day to share their joy ― or explore their options if they did not match.
Take this post March 19 on Twitter: “I went unmatched this year; looking for research position at any institute for internal medicine.”
including an international medical graduate who matched into his chosen specialty after multiple disappointments.
“I’ve waited for this email for 8 years,” Sahil Bawa, MD, posted on Twitter on March 13. A few days later, when he learned about his residency position, he posted: “I’m beyond grateful. Will be moving to Alabama soon #familymedicine.”
Dr. Bawa, who matched into UAB Medicine Selma (Ala.), graduated from medical school in India in 2014. He said in an interview that he has visited the United States periodically since then to pass medical tests, obtain letters of recommendation, and participate in research.
Over the years he watched his Indian colleagues give up on becoming American doctors, find alternative careers, or resolve to practice in their native country. But he held onto the few success stories he saw on social media. “There were always one to two every year. It kept me going. If they can do it, I can do it.”
International medical graduates (IMGs) like Dr. Bawa applied in record numbers to Match2023, according to the National Resident Matching Program (NRMP), which announced the results on March 13 of its main residency match and the Supplemental Offer and Acceptance Program (SOAP) for unfilled positions or unmatched applicants.
Overall, 48,156 total applicants registered for the match, which was driven by the increase of non-U.S. IMG applicants and U.S. DO seniors over the past year, NRMP stated in its release. U.S. MD seniors had a match rate of nearly 94%, and U.S. DO seniors, nearly 92%. U.S. IMGs had a match rate of nearly 68%, an “all-time high,” and non-U.S. IMGs, nearly 60%, NRMP stated.
Three specialties that filled all of their 30 or more available positions were orthopedic surgery, plastic surgery (integrated), radiology – diagnostic, and thoracic surgery. Specialties with 30 or more positions that filled with the highest percentage of U.S. MD and DO seniors were plastic surgery (integrated), internal medicine-pediatrics, ob.gyn., and orthopedic surgery.
The number of available primary care positions increased slightly, NRMP reported. Considering “a serious and growing shortage of primary care physicians across the U.S.,” there were 571 more primary care positions than 2022. That’s an increase of about 3% over last year and 17% over the past 5 years. Primary care positions filled at a rate of 94%, which remained steady from 2022.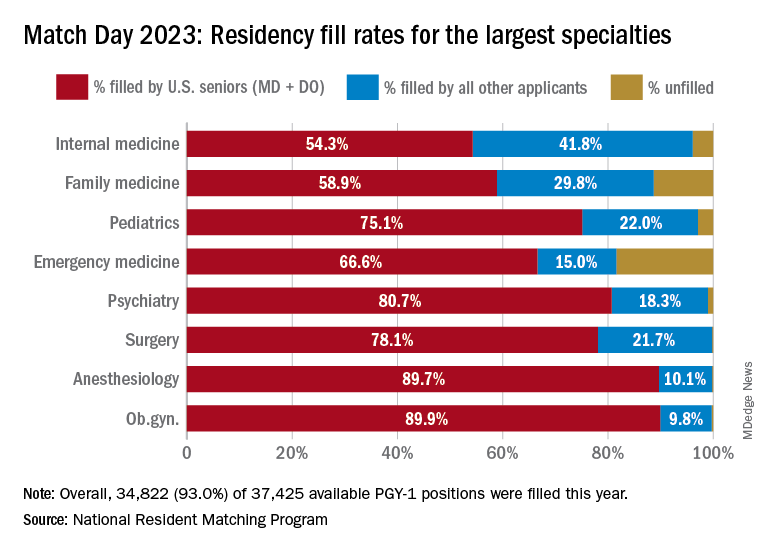
NRMP also pointed out specialties with increases in the number of positions filled by U.S. MD seniors of more than 10% and 10 positions in the past 5 years: anesthesiology, child neurology, interventional radiology, neurology, pathology, physical medicine and rehabilitation, plastic surgery (integrated), psychiatry, radiology-diagnostic, transitional year, and vascular surgery.
Bryan Carmody, MD, MPH, a pediatric nephrologist known for his medical school commentaries, said in an interview that the most competitive specialties he noted in 2023 were radiology, pathology, and neurology.
“The surgical specialties are always competitive, so it wasn’t a surprise that orthopedics, plastic surgery, and thoracic surgery filled all of their positions. But I was surprised to see diagnostic radiology fill every single one of their positions in the match. And although pathology and neurology aren’t typically considered extremely competitive specialties, they filled over 99% of their positions in the Match this year.”
On Dr. Carmody’s blog about the winners and losers of Match Day, he said that despite the record number of primary care positions offered, family medicine programs suffered. “Only 89% of family medicine programs filled in the Match, and graduating U.S. MD and DO students only filled a little more than half of all the available positions,” he wrote.
For a record number of applicants that match each year, and “the most favorable ratio in the past 2 decades” of applicants-to-positions in 2023, there are still a lot unmatched, Dr. Carmody said. “It’s a tough thing to talk about. The reality is the number of residency positions should be determined by the number of physicians needed.”
One student, Asim Ansari, didn’t match into a traditional residency or through SOAP. It was his fifth attempt. He was serving a transitional-year residency at Merit Health Wesley in Hattiesburg, Miss., and when he didn’t match, he accepted a child and adolescent psychiatry fellowship at the University of Kansas Medical Center, Kansas City.
He said he was “relieved and excited” to have found a program in his chosen specialty. Still, in 2 years, Mr. Ansari must again try to match into a traditional psychiatry residency.
Meanwhile, Dr. Bawa will prepare for his 3-year residency in Alabama after completing his interim research year in the surgery department at Wayne State University, Detroit, in May.
Despite his years in limbo, Dr. Bawa said, “I have no regrets, no complaints. I am still very happy.”
A version of this article originally appeared on Medscape.com.
Match Day: Record number of residencies offered
Baily Nagle, vice president of her graduating class at Harvard Medical School, Boston, celebrated “the luck of the Irish” on St. Patrick’s Day that allowed her to match into her chosen specialty and top choice of residency programs: anesthesia at Brigham and Women’s Hospital.
“I am feeling very excited and relieved – I matched,” she said in an interview upon hearing her good fortune on Match Monday, March 13. She had a similar reaction on Match Day, March 17. “After a lot of long nights and hard work, happy to have it pay off.”
Ms. Nagle was so determined to match into her specialty that she didn’t have any other specialties in mind as a backup.
The annual process of matching medical school graduates with compatible residency programs is an emotional roller coaster for all applicants, their personal March Madness, so to speak. But Ms. Nagle was one of the more fortunate applicants. She didn’t have to confront the heartbreak other applicants felt when the National Resident Matching Program (NRMP) announced results of the main residency match and the Supplemental Offer and Acceptance Program (SOAP), which offers alternate programs for unfilled positions or unmatched applicants.
During the 2023 Match process, this news organization has been following a handful of students, checking in with them periodically for updates on their progress. Most of them matched successfully, but at least one international medical graduate (IMG) did not. What the others have in common is that their hearts were set on a chosen specialty. Like Ms. Nagle, another student banked on landing his chosen specialty without a backup plan, whereas another said that she’d continue through the SOAP if she didn’t match successfully.
Overall, Match Day resulted in a record number of residency positions offered, most notably in primary care, which “hit an all-time high,” according to NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN. The number of positions has “consistently increased over the past 5 years, and most importantly the fill rate for primary care has remained steady,” Dr.. Lamb noted in the NRMP release of Match Day results. The release coincided with students learning through emails at noon Eastern Time to which residency or supplemental programs they were matched.
Though more applicants registered for the Match in 2023 than in 2022 – driven primarily by non-U.S. IMGs – the NRMP stated that it was surprised by the decrease in U.S. MD senior applicants.
U.S. MD seniors had a nearly 94% Match rate, a small increase over 2022. U.S. citizen IMGs saw a nearly 68% Match rate, which NRMP reported as an “all-time high” and about six percentage points over in 2022, whereas non-U.S. IMGs had a nearly 60% Match rate, a 1.3 percentage point increase over 2022.
Among the specialties that filled all available positions in 2023 were orthopedic surgery, plastic surgery (integrated), and radiology – diagnostic and thoracic surgery.
Not everyone matches
On March 13, the American College of Emergency Physicians issued a joint statement with other emergency medicine (EM) organizations about a high rate of unfilled EM positions expected in 2023.
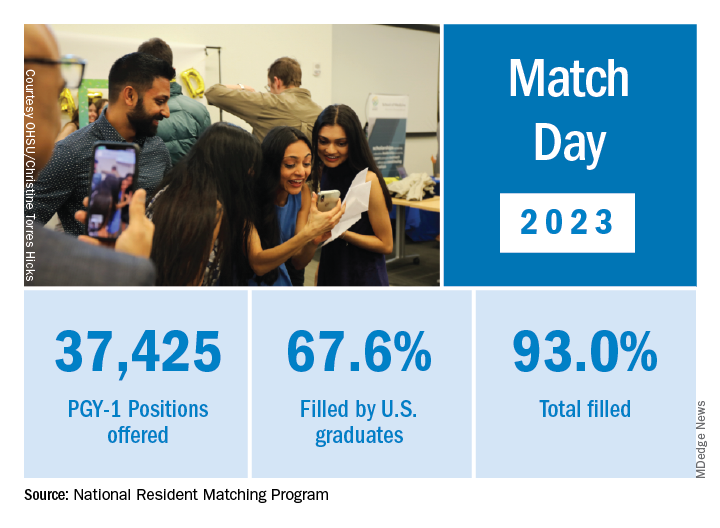
NRMP acknowledged March 17 that 554 positions remained unfilled, an increase of 335 more unfilled positions than 2022. NRMP attributed the increase in unfilled positions in part to a decrease in the number of U.S. MD and U.S. DO seniors who submitted ranks for the specialty, which “could reflect changing applicant interests or projections about workforce opportunities post residency.”
Applicants who didn’t match usually try to obtain an unfilled position through SOAP. In 2023, 2,685 positions were unfilled after the matching algorithm was processed, an increase of nearly 19% over 2022. The vast majority of those positions were placed in SOAP, an increase of 17.5% over 2022.
Asim Ansari was one of the unlucky ones. Mr. Ansari was trying to match for the fifth time. He was unsuccessful in doing so again in 2023 in the Match and SOAP. Still, he was offered and accepted a child and adolescent psychiatry fellowship at Kansas University Medical Center in Kansas City. Psychiatry was his chosen specialty, so he was “feeling good. It’s a nice place to go to do the next 2 years.”
Mr. Ansari, who started the #MatchMadness support group for unmatched doctors on Twitter Spaces, was quick to cheer on his fellow matching peers on March 13 while revealing his own fate: “Congratulations to everyone who matched!!! Y’all are amazing. So proud of each one of you!!! I didn’t.”
Soon after the results, #MatchMadness held a #Soap2023 support session, and Mr. Ansari sought advice for those willing to review SOAP applications. Elsewhere on Twitter Match Day threads, a few doctors offered their support to those who planned to SOAP, students announced their matches, and others either congratulated or encouraged those still trying to match.
Couples match
Not everyone who matched considered the alternative. Before March 13, William Boyer said that he hadn’t given much thought to what would happen if he didn’t match because he was “optimistically confident” he would match into his chosen EM specialty. But he did and got his top choice of programs: Yale New Haven (Conn.) Hospital.
“I feel great,” he said in an interview. “I was definitely nervous opening the envelope” that revealed his residency program, “but there was a rush of relief” when he saw he landed Yale.
Earlier in the match cycle, he said in an interview that he “interviewed at a few ‘reach’ programs, so I hope I don’t match lower than expected on my rank list.”
Mr. Boyer considers himself “a mature applicant,” entering the University of South Carolina, Columbia, after 4 years as an insurance broker.
“I am celebrating today by playing pickleball with a few close medical friends who also matched this morning,” Mr. Boyer said on March 13. “I definitely had periods of nervousness leading up to this morning though that quickly turned into joy and relief” after learning he matched.
Mr. Boyer believes that his professional experience in the insurance industry and health care lobbying efforts with the National Association of Health Underwriters set him apart from other applicants.
“I changed careers to pursue this aspiration, which demonstrates my full dedication to the medical profession.”
He applied to 48 programs and was offered interviews to nearly half. Mr. Boyer visited the majority of those virtually. He said he targeted programs close to where his and his partner’s families are located: Massachusetts, North Carolina, and Texas. “My partner, who I met in medical school, matched into ortho as well so the whole household is very happy,” Mr. Boyer said.
She matched into her top choice as well on March 17, though a distance away at UT Health in San Antonio, he said. “We are both ecstatic. We both got our no. 1 choice. That was the plan going into it. We will make it work. I have 4 weeks of vacation.”
In his program choices, Mr. Boyer prioritized access to nature, minimal leadership turnover, a mix of clinical training sites, and adequate elective rotations and fellowship opportunities, such as in wilderness medicine and health policy.
NRMP reported that there were 1,239 couples participating in the Match; 1,095 had both partners match, and 114 had one partner match to residency training programs for a match rate of 93%.
Like Mr. Boyer, Hannah Hedriana matched into EM, one of the more popular despite the reported unfilled positions. In the past few years, it has consistently been one of the fastest-growing specialties, according to the NRMP.
Still Ms. Hedriana had a fall-back plan. “If I don’t match, then I do plan on going through SOAP. With the number of EM spots that were unfilled in 2022, there’s a chance I could still be an EM physician, but if not, then that’s okay with me.”
Her reaction on March 13, after learning she matched? “Super excited, celebrating with my friends right now.” On Match Day, she said she was “ecstatic” to be matched into Lakeland (Fla.) Regional Health. “This was my first choice so now I can stay close to family and friends,” she said in an interview soon after the results were released.
A first-generation, Filipino American student from the University of South Florida, Tampa, Ms. Hedriana comes from a family of health care professionals. Her father is a respiratory therapist turned physical therapist; her mother a registered nurse. Her sister is a patient care technician applying to nursing school.
Ms. Hedriana applied to 70 programs and interviewed mostly online with 24. Her goal was to stay on the East Coast.
“My partner is a licensed dentist in the state of Florida, and so for his career it would be more practical to stay in state, rather than get relicensed in another state, which could take months,” she said earlier in the matching cycle. “However, when we discussed choosing a residency program, he ultimately left it up to me and wanted me to pick where I thought I’d flourish best,” Ms. Hedriana said, adding that her family lives in Florida, too.
She said she sought a residency program that values family and teamwork.
“A program gets more points in my book if they have sites at nonprofit hospitals or has residents that regularly volunteer throughout their communities or participate in DEI [diversity, equity, and inclusion] initiatives.”
Ms. Hedriana noted that some specialties exclusively offered virtual interviews in 2023, whereas other specialties favored in-person interviews. “This year, many of my classmates were able to do multiple away rotations, which they saw as a positive regarding their chances of matching.” During COVID, in-person visits were limited.
“However, I’ve noticed that many of my classmates are not fond of the signaling aspect that was present for this year’s cycle,” she said. Signaling is a relatively new process that allows applicants to indicate interest in a limited number of residency programs. Not all residencies participate, but it’s growing in popularity among specialties, according to the American Medical Association.
‘Extremely competitive’
Ms. Nagle, a second lieutenant in the U.S. Air Force, applied to 12 programs and interviewed with half of them online. She said that she wasn’t targeting any specific type of program through the match.
“I believe you can get phenomenal training anywhere where you mesh with the residents and leadership. My ultimate priority is to (1) be near good people, (2) be near good food (Indian and Thai are a must), and (3) be near an international airport so I can flee the country during breaks.”
Meanwhile, she said that she found the application process, in which students have to articulate their entire medical school experience, extremely competitive. “I think this process is so easy to get wound up in and the anxiety can be palpable,” Ms. Nagle said. “People around you match your energy. So if you are a ball of anxiety then so are your attendings and residents – and that doesn’t bode well for passing the ‘do I want to be on call with them’ test.”
Looking back at medical school, Ms. Nagle recalled having a baby named after her during her first anesthesia rotation and being featured on The Kelly Clarkson Show. Ms. Nagle said that she had walked into the delivery room where new parents had been debating names of babies beginning with the letter B. “And when I introduced myself, they looked at each other and said, ‘Yep, that’s the one.’”
Mr. Boyer recounted how the majority of his medical school experience involved online education. “Roughly two-thirds of my first year was in-person prior to the pandemic. However, from spring break first year to in-person clinical rotations at the beginning of third year, we were all virtual. While I missed interacting with my classmates, I benefited from the virtual learning environment as I learn more efficiently from reading and visual aids than auditory lectures.”
Ms. Hedriana cited the friends and memories she made while learning to be a doctor. “Medical school was hard, but I wouldn’t have changed a thing.”
A version of this article first appeared on Medscape.com.
Baily Nagle, vice president of her graduating class at Harvard Medical School, Boston, celebrated “the luck of the Irish” on St. Patrick’s Day that allowed her to match into her chosen specialty and top choice of residency programs: anesthesia at Brigham and Women’s Hospital.
“I am feeling very excited and relieved – I matched,” she said in an interview upon hearing her good fortune on Match Monday, March 13. She had a similar reaction on Match Day, March 17. “After a lot of long nights and hard work, happy to have it pay off.”
Ms. Nagle was so determined to match into her specialty that she didn’t have any other specialties in mind as a backup.
The annual process of matching medical school graduates with compatible residency programs is an emotional roller coaster for all applicants, their personal March Madness, so to speak. But Ms. Nagle was one of the more fortunate applicants. She didn’t have to confront the heartbreak other applicants felt when the National Resident Matching Program (NRMP) announced results of the main residency match and the Supplemental Offer and Acceptance Program (SOAP), which offers alternate programs for unfilled positions or unmatched applicants.
During the 2023 Match process, this news organization has been following a handful of students, checking in with them periodically for updates on their progress. Most of them matched successfully, but at least one international medical graduate (IMG) did not. What the others have in common is that their hearts were set on a chosen specialty. Like Ms. Nagle, another student banked on landing his chosen specialty without a backup plan, whereas another said that she’d continue through the SOAP if she didn’t match successfully.
Overall, Match Day resulted in a record number of residency positions offered, most notably in primary care, which “hit an all-time high,” according to NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN. The number of positions has “consistently increased over the past 5 years, and most importantly the fill rate for primary care has remained steady,” Dr.. Lamb noted in the NRMP release of Match Day results. The release coincided with students learning through emails at noon Eastern Time to which residency or supplemental programs they were matched.
Though more applicants registered for the Match in 2023 than in 2022 – driven primarily by non-U.S. IMGs – the NRMP stated that it was surprised by the decrease in U.S. MD senior applicants.
U.S. MD seniors had a nearly 94% Match rate, a small increase over 2022. U.S. citizen IMGs saw a nearly 68% Match rate, which NRMP reported as an “all-time high” and about six percentage points over in 2022, whereas non-U.S. IMGs had a nearly 60% Match rate, a 1.3 percentage point increase over 2022.
Among the specialties that filled all available positions in 2023 were orthopedic surgery, plastic surgery (integrated), and radiology – diagnostic and thoracic surgery.
Not everyone matches
On March 13, the American College of Emergency Physicians issued a joint statement with other emergency medicine (EM) organizations about a high rate of unfilled EM positions expected in 2023.
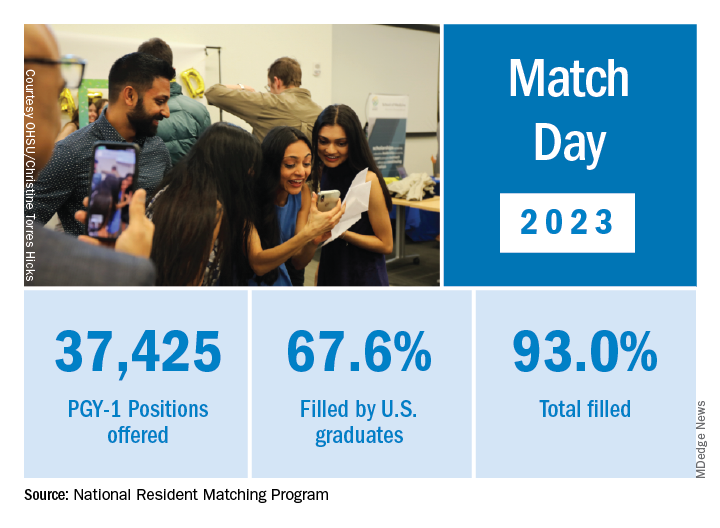
NRMP acknowledged March 17 that 554 positions remained unfilled, an increase of 335 more unfilled positions than 2022. NRMP attributed the increase in unfilled positions in part to a decrease in the number of U.S. MD and U.S. DO seniors who submitted ranks for the specialty, which “could reflect changing applicant interests or projections about workforce opportunities post residency.”
Applicants who didn’t match usually try to obtain an unfilled position through SOAP. In 2023, 2,685 positions were unfilled after the matching algorithm was processed, an increase of nearly 19% over 2022. The vast majority of those positions were placed in SOAP, an increase of 17.5% over 2022.
Asim Ansari was one of the unlucky ones. Mr. Ansari was trying to match for the fifth time. He was unsuccessful in doing so again in 2023 in the Match and SOAP. Still, he was offered and accepted a child and adolescent psychiatry fellowship at Kansas University Medical Center in Kansas City. Psychiatry was his chosen specialty, so he was “feeling good. It’s a nice place to go to do the next 2 years.”
Mr. Ansari, who started the #MatchMadness support group for unmatched doctors on Twitter Spaces, was quick to cheer on his fellow matching peers on March 13 while revealing his own fate: “Congratulations to everyone who matched!!! Y’all are amazing. So proud of each one of you!!! I didn’t.”
Soon after the results, #MatchMadness held a #Soap2023 support session, and Mr. Ansari sought advice for those willing to review SOAP applications. Elsewhere on Twitter Match Day threads, a few doctors offered their support to those who planned to SOAP, students announced their matches, and others either congratulated or encouraged those still trying to match.
Couples match
Not everyone who matched considered the alternative. Before March 13, William Boyer said that he hadn’t given much thought to what would happen if he didn’t match because he was “optimistically confident” he would match into his chosen EM specialty. But he did and got his top choice of programs: Yale New Haven (Conn.) Hospital.
“I feel great,” he said in an interview. “I was definitely nervous opening the envelope” that revealed his residency program, “but there was a rush of relief” when he saw he landed Yale.
Earlier in the match cycle, he said in an interview that he “interviewed at a few ‘reach’ programs, so I hope I don’t match lower than expected on my rank list.”
Mr. Boyer considers himself “a mature applicant,” entering the University of South Carolina, Columbia, after 4 years as an insurance broker.
“I am celebrating today by playing pickleball with a few close medical friends who also matched this morning,” Mr. Boyer said on March 13. “I definitely had periods of nervousness leading up to this morning though that quickly turned into joy and relief” after learning he matched.
Mr. Boyer believes that his professional experience in the insurance industry and health care lobbying efforts with the National Association of Health Underwriters set him apart from other applicants.
“I changed careers to pursue this aspiration, which demonstrates my full dedication to the medical profession.”
He applied to 48 programs and was offered interviews to nearly half. Mr. Boyer visited the majority of those virtually. He said he targeted programs close to where his and his partner’s families are located: Massachusetts, North Carolina, and Texas. “My partner, who I met in medical school, matched into ortho as well so the whole household is very happy,” Mr. Boyer said.
She matched into her top choice as well on March 17, though a distance away at UT Health in San Antonio, he said. “We are both ecstatic. We both got our no. 1 choice. That was the plan going into it. We will make it work. I have 4 weeks of vacation.”
In his program choices, Mr. Boyer prioritized access to nature, minimal leadership turnover, a mix of clinical training sites, and adequate elective rotations and fellowship opportunities, such as in wilderness medicine and health policy.
NRMP reported that there were 1,239 couples participating in the Match; 1,095 had both partners match, and 114 had one partner match to residency training programs for a match rate of 93%.
Like Mr. Boyer, Hannah Hedriana matched into EM, one of the more popular despite the reported unfilled positions. In the past few years, it has consistently been one of the fastest-growing specialties, according to the NRMP.
Still Ms. Hedriana had a fall-back plan. “If I don’t match, then I do plan on going through SOAP. With the number of EM spots that were unfilled in 2022, there’s a chance I could still be an EM physician, but if not, then that’s okay with me.”
Her reaction on March 13, after learning she matched? “Super excited, celebrating with my friends right now.” On Match Day, she said she was “ecstatic” to be matched into Lakeland (Fla.) Regional Health. “This was my first choice so now I can stay close to family and friends,” she said in an interview soon after the results were released.
A first-generation, Filipino American student from the University of South Florida, Tampa, Ms. Hedriana comes from a family of health care professionals. Her father is a respiratory therapist turned physical therapist; her mother a registered nurse. Her sister is a patient care technician applying to nursing school.
Ms. Hedriana applied to 70 programs and interviewed mostly online with 24. Her goal was to stay on the East Coast.
“My partner is a licensed dentist in the state of Florida, and so for his career it would be more practical to stay in state, rather than get relicensed in another state, which could take months,” she said earlier in the matching cycle. “However, when we discussed choosing a residency program, he ultimately left it up to me and wanted me to pick where I thought I’d flourish best,” Ms. Hedriana said, adding that her family lives in Florida, too.
She said she sought a residency program that values family and teamwork.
“A program gets more points in my book if they have sites at nonprofit hospitals or has residents that regularly volunteer throughout their communities or participate in DEI [diversity, equity, and inclusion] initiatives.”
Ms. Hedriana noted that some specialties exclusively offered virtual interviews in 2023, whereas other specialties favored in-person interviews. “This year, many of my classmates were able to do multiple away rotations, which they saw as a positive regarding their chances of matching.” During COVID, in-person visits were limited.
“However, I’ve noticed that many of my classmates are not fond of the signaling aspect that was present for this year’s cycle,” she said. Signaling is a relatively new process that allows applicants to indicate interest in a limited number of residency programs. Not all residencies participate, but it’s growing in popularity among specialties, according to the American Medical Association.
‘Extremely competitive’
Ms. Nagle, a second lieutenant in the U.S. Air Force, applied to 12 programs and interviewed with half of them online. She said that she wasn’t targeting any specific type of program through the match.
“I believe you can get phenomenal training anywhere where you mesh with the residents and leadership. My ultimate priority is to (1) be near good people, (2) be near good food (Indian and Thai are a must), and (3) be near an international airport so I can flee the country during breaks.”
Meanwhile, she said that she found the application process, in which students have to articulate their entire medical school experience, extremely competitive. “I think this process is so easy to get wound up in and the anxiety can be palpable,” Ms. Nagle said. “People around you match your energy. So if you are a ball of anxiety then so are your attendings and residents – and that doesn’t bode well for passing the ‘do I want to be on call with them’ test.”
Looking back at medical school, Ms. Nagle recalled having a baby named after her during her first anesthesia rotation and being featured on The Kelly Clarkson Show. Ms. Nagle said that she had walked into the delivery room where new parents had been debating names of babies beginning with the letter B. “And when I introduced myself, they looked at each other and said, ‘Yep, that’s the one.’”
Mr. Boyer recounted how the majority of his medical school experience involved online education. “Roughly two-thirds of my first year was in-person prior to the pandemic. However, from spring break first year to in-person clinical rotations at the beginning of third year, we were all virtual. While I missed interacting with my classmates, I benefited from the virtual learning environment as I learn more efficiently from reading and visual aids than auditory lectures.”
Ms. Hedriana cited the friends and memories she made while learning to be a doctor. “Medical school was hard, but I wouldn’t have changed a thing.”
A version of this article first appeared on Medscape.com.
Baily Nagle, vice president of her graduating class at Harvard Medical School, Boston, celebrated “the luck of the Irish” on St. Patrick’s Day that allowed her to match into her chosen specialty and top choice of residency programs: anesthesia at Brigham and Women’s Hospital.
“I am feeling very excited and relieved – I matched,” she said in an interview upon hearing her good fortune on Match Monday, March 13. She had a similar reaction on Match Day, March 17. “After a lot of long nights and hard work, happy to have it pay off.”
Ms. Nagle was so determined to match into her specialty that she didn’t have any other specialties in mind as a backup.
The annual process of matching medical school graduates with compatible residency programs is an emotional roller coaster for all applicants, their personal March Madness, so to speak. But Ms. Nagle was one of the more fortunate applicants. She didn’t have to confront the heartbreak other applicants felt when the National Resident Matching Program (NRMP) announced results of the main residency match and the Supplemental Offer and Acceptance Program (SOAP), which offers alternate programs for unfilled positions or unmatched applicants.
During the 2023 Match process, this news organization has been following a handful of students, checking in with them periodically for updates on their progress. Most of them matched successfully, but at least one international medical graduate (IMG) did not. What the others have in common is that their hearts were set on a chosen specialty. Like Ms. Nagle, another student banked on landing his chosen specialty without a backup plan, whereas another said that she’d continue through the SOAP if she didn’t match successfully.
Overall, Match Day resulted in a record number of residency positions offered, most notably in primary care, which “hit an all-time high,” according to NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN. The number of positions has “consistently increased over the past 5 years, and most importantly the fill rate for primary care has remained steady,” Dr.. Lamb noted in the NRMP release of Match Day results. The release coincided with students learning through emails at noon Eastern Time to which residency or supplemental programs they were matched.
Though more applicants registered for the Match in 2023 than in 2022 – driven primarily by non-U.S. IMGs – the NRMP stated that it was surprised by the decrease in U.S. MD senior applicants.
U.S. MD seniors had a nearly 94% Match rate, a small increase over 2022. U.S. citizen IMGs saw a nearly 68% Match rate, which NRMP reported as an “all-time high” and about six percentage points over in 2022, whereas non-U.S. IMGs had a nearly 60% Match rate, a 1.3 percentage point increase over 2022.
Among the specialties that filled all available positions in 2023 were orthopedic surgery, plastic surgery (integrated), and radiology – diagnostic and thoracic surgery.
Not everyone matches
On March 13, the American College of Emergency Physicians issued a joint statement with other emergency medicine (EM) organizations about a high rate of unfilled EM positions expected in 2023.
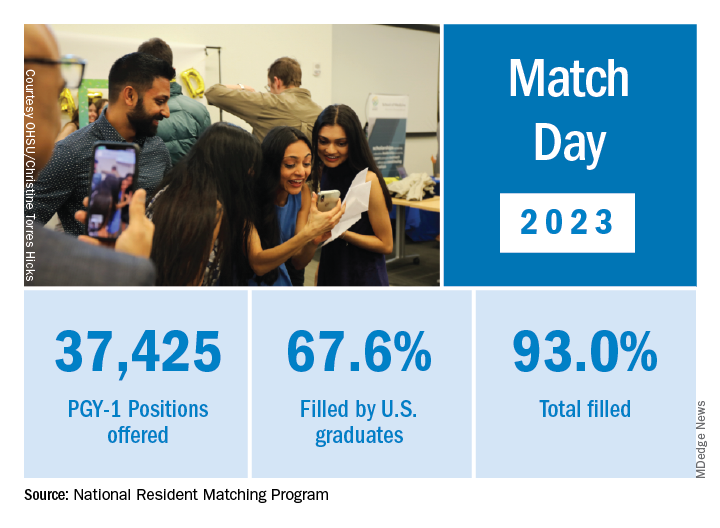
NRMP acknowledged March 17 that 554 positions remained unfilled, an increase of 335 more unfilled positions than 2022. NRMP attributed the increase in unfilled positions in part to a decrease in the number of U.S. MD and U.S. DO seniors who submitted ranks for the specialty, which “could reflect changing applicant interests or projections about workforce opportunities post residency.”
Applicants who didn’t match usually try to obtain an unfilled position through SOAP. In 2023, 2,685 positions were unfilled after the matching algorithm was processed, an increase of nearly 19% over 2022. The vast majority of those positions were placed in SOAP, an increase of 17.5% over 2022.
Asim Ansari was one of the unlucky ones. Mr. Ansari was trying to match for the fifth time. He was unsuccessful in doing so again in 2023 in the Match and SOAP. Still, he was offered and accepted a child and adolescent psychiatry fellowship at Kansas University Medical Center in Kansas City. Psychiatry was his chosen specialty, so he was “feeling good. It’s a nice place to go to do the next 2 years.”
Mr. Ansari, who started the #MatchMadness support group for unmatched doctors on Twitter Spaces, was quick to cheer on his fellow matching peers on March 13 while revealing his own fate: “Congratulations to everyone who matched!!! Y’all are amazing. So proud of each one of you!!! I didn’t.”
Soon after the results, #MatchMadness held a #Soap2023 support session, and Mr. Ansari sought advice for those willing to review SOAP applications. Elsewhere on Twitter Match Day threads, a few doctors offered their support to those who planned to SOAP, students announced their matches, and others either congratulated or encouraged those still trying to match.
Couples match
Not everyone who matched considered the alternative. Before March 13, William Boyer said that he hadn’t given much thought to what would happen if he didn’t match because he was “optimistically confident” he would match into his chosen EM specialty. But he did and got his top choice of programs: Yale New Haven (Conn.) Hospital.
“I feel great,” he said in an interview. “I was definitely nervous opening the envelope” that revealed his residency program, “but there was a rush of relief” when he saw he landed Yale.
Earlier in the match cycle, he said in an interview that he “interviewed at a few ‘reach’ programs, so I hope I don’t match lower than expected on my rank list.”
Mr. Boyer considers himself “a mature applicant,” entering the University of South Carolina, Columbia, after 4 years as an insurance broker.
“I am celebrating today by playing pickleball with a few close medical friends who also matched this morning,” Mr. Boyer said on March 13. “I definitely had periods of nervousness leading up to this morning though that quickly turned into joy and relief” after learning he matched.
Mr. Boyer believes that his professional experience in the insurance industry and health care lobbying efforts with the National Association of Health Underwriters set him apart from other applicants.
“I changed careers to pursue this aspiration, which demonstrates my full dedication to the medical profession.”
He applied to 48 programs and was offered interviews to nearly half. Mr. Boyer visited the majority of those virtually. He said he targeted programs close to where his and his partner’s families are located: Massachusetts, North Carolina, and Texas. “My partner, who I met in medical school, matched into ortho as well so the whole household is very happy,” Mr. Boyer said.
She matched into her top choice as well on March 17, though a distance away at UT Health in San Antonio, he said. “We are both ecstatic. We both got our no. 1 choice. That was the plan going into it. We will make it work. I have 4 weeks of vacation.”
In his program choices, Mr. Boyer prioritized access to nature, minimal leadership turnover, a mix of clinical training sites, and adequate elective rotations and fellowship opportunities, such as in wilderness medicine and health policy.
NRMP reported that there were 1,239 couples participating in the Match; 1,095 had both partners match, and 114 had one partner match to residency training programs for a match rate of 93%.
Like Mr. Boyer, Hannah Hedriana matched into EM, one of the more popular despite the reported unfilled positions. In the past few years, it has consistently been one of the fastest-growing specialties, according to the NRMP.
Still Ms. Hedriana had a fall-back plan. “If I don’t match, then I do plan on going through SOAP. With the number of EM spots that were unfilled in 2022, there’s a chance I could still be an EM physician, but if not, then that’s okay with me.”
Her reaction on March 13, after learning she matched? “Super excited, celebrating with my friends right now.” On Match Day, she said she was “ecstatic” to be matched into Lakeland (Fla.) Regional Health. “This was my first choice so now I can stay close to family and friends,” she said in an interview soon after the results were released.
A first-generation, Filipino American student from the University of South Florida, Tampa, Ms. Hedriana comes from a family of health care professionals. Her father is a respiratory therapist turned physical therapist; her mother a registered nurse. Her sister is a patient care technician applying to nursing school.
Ms. Hedriana applied to 70 programs and interviewed mostly online with 24. Her goal was to stay on the East Coast.
“My partner is a licensed dentist in the state of Florida, and so for his career it would be more practical to stay in state, rather than get relicensed in another state, which could take months,” she said earlier in the matching cycle. “However, when we discussed choosing a residency program, he ultimately left it up to me and wanted me to pick where I thought I’d flourish best,” Ms. Hedriana said, adding that her family lives in Florida, too.
She said she sought a residency program that values family and teamwork.
“A program gets more points in my book if they have sites at nonprofit hospitals or has residents that regularly volunteer throughout their communities or participate in DEI [diversity, equity, and inclusion] initiatives.”
Ms. Hedriana noted that some specialties exclusively offered virtual interviews in 2023, whereas other specialties favored in-person interviews. “This year, many of my classmates were able to do multiple away rotations, which they saw as a positive regarding their chances of matching.” During COVID, in-person visits were limited.
“However, I’ve noticed that many of my classmates are not fond of the signaling aspect that was present for this year’s cycle,” she said. Signaling is a relatively new process that allows applicants to indicate interest in a limited number of residency programs. Not all residencies participate, but it’s growing in popularity among specialties, according to the American Medical Association.
‘Extremely competitive’
Ms. Nagle, a second lieutenant in the U.S. Air Force, applied to 12 programs and interviewed with half of them online. She said that she wasn’t targeting any specific type of program through the match.
“I believe you can get phenomenal training anywhere where you mesh with the residents and leadership. My ultimate priority is to (1) be near good people, (2) be near good food (Indian and Thai are a must), and (3) be near an international airport so I can flee the country during breaks.”
Meanwhile, she said that she found the application process, in which students have to articulate their entire medical school experience, extremely competitive. “I think this process is so easy to get wound up in and the anxiety can be palpable,” Ms. Nagle said. “People around you match your energy. So if you are a ball of anxiety then so are your attendings and residents – and that doesn’t bode well for passing the ‘do I want to be on call with them’ test.”
Looking back at medical school, Ms. Nagle recalled having a baby named after her during her first anesthesia rotation and being featured on The Kelly Clarkson Show. Ms. Nagle said that she had walked into the delivery room where new parents had been debating names of babies beginning with the letter B. “And when I introduced myself, they looked at each other and said, ‘Yep, that’s the one.’”
Mr. Boyer recounted how the majority of his medical school experience involved online education. “Roughly two-thirds of my first year was in-person prior to the pandemic. However, from spring break first year to in-person clinical rotations at the beginning of third year, we were all virtual. While I missed interacting with my classmates, I benefited from the virtual learning environment as I learn more efficiently from reading and visual aids than auditory lectures.”
Ms. Hedriana cited the friends and memories she made while learning to be a doctor. “Medical school was hard, but I wouldn’t have changed a thing.”
A version of this article first appeared on Medscape.com.
Nursing exam failure rates spark review of test results
Nursing oversight groups in the United States and Canada are holding the line on testing standards as more would-be nurses fail entry exams. As a result, pressure is growing to make tests easier to pass given widespread nursing shortages, and some critics wonder whether the exams accurately assess students’ true abilities.
When it comes to training more nurses to keep up with growing demand, the U.S. organization that oversees the main licensing exams for nurses decided earlier this month not to change the passing standards for entry-level tests. Meanwhile,
A similar scenario also is unfolding in Quebec, where the agency overseeing nurse licensing exams announced last month it is holding the line on its passing rates despite an outcry from nurses after more than half of those taking the exam in September failed. Quebec’s commissioner for professional admissions is investigating dozens of complaints from nurses about the failure rate. Nurses who failed the test can sign up to retake it in March.
Joseph Oujeil, DESS, DEF, has been teaching in Canada for 4 years, now at two Quebec nursing schools. “This is surprising and very shocking to our students as well as nurses from outside Quebec who were [completing] an integration program to adjust their practice to Quebec guidelines,” Mr. Oujeil told this news organization. Students from outside the province failed the licensing exam at a higher rate than their Quebec-native peers, he explained.
Quebec’s professional Order of Nurses of Quebec (OIIQ) responded to the nurses’ outcry in a press release last month, saying that the pandemic may be partly to blame for the lower passing rate because it made it more difficult to access internships, labs, and face-to-face teaching. Some students weren’t able to demonstrate their ability to practice during the exam as in previous years, OIIQ reported.
Mr. Oujeil agreed. “I’m sure the pandemic has an impact on the situation as well as some students did less training in hospitals” because of restrictions caused by the pandemic, he said. But students also told Mr. Oujeil some questions seemed ambiguous.
OIIQ stated in its release that it doesn’t want to lower the standard. The goal is to protect the public “by and with nurses,” to “ensure the competence and integrity of nurses in Quebec,” and “promote quality nursing practice,” the release noted.
Similarly in the United States, the National Council of State Boards of Nursing (NCSBN) announced Dec. 8 that it would uphold the current passing standards for its entry-level NCLEX tests for registered nurses and practical nurses. NCSBN analyzes the passing standard every 3 years “to keep the test plan and passing standard current,” a press release explains.
NCLEX pass rates have dropped from about 73% for all candidates and 88% for first-time U.S.-educated candidates to 69% and 82% respectively in 2021, the last full year for which results are available, NCSBN spokesperson Dawn Kappel told this news organization.
Over the past 3 years, including during the pandemic, the board decided “that the current passing standard is appropriate as a measure of safe and effective entry-level nurse practice,” after reviewing national nurse surveys and the findings of panels of nurses representing NCSBN’s geographic areas in the United States and Canada, board president Jay Douglas, MSM, RN, CSAC, said in a press release.
Still, NCSBN is not blind to the larger issues facing nursing, Ms. Kappel told this news organization. “There is a huge nursing shortage in the U.S. and Canada. We want as many nurses in the workforce as possible, but we want to ensure safe practice,” she said.
“Everyone has access to the same test, regardless of which state, province, or country they take it in,” she said. Some international students may not perform as well as U.S.-educated students because of their command of English and the nursing education standards in their home countries, Ms. Kappel added.
“Obviously COVID and the challenge of education in general” affected the results, she said.
Mr. Oujeil, the nursing school professor, said he is frustrated by the test results because the majority of students who failed maintained good grades and passed all of their trainings. Yet they scored just below the passing rate of 55%. He said students are proposing the passing rate be lowered to 50%. The current test doesn’t reflect what students are learning in the classroom or during clinical trainings, Mr. Oujeil added. “I don’t know of any students who scored more than 60%.”
He said he understands that the mission of the OIIQ is protecting the population, but he doesn’t believe lowering the passing rate to 50% will put the population at risk – and it will help offset the staffing shortage.
“I’m especially frustrated by those who were doing integration programs – mothers and fathers with children with family lives and financial responsibilities. Many of them are good, hard workers and were shocked they should have to pass the exam another time.”
Since 2018, the pass rate on the first attempt at the Quebec test has generally been between 71% and 96%, compared with 51.4% during the exam in September, according to the OIIQ press release. Meanwhile, graduates from 30 of the 55 schools and universities in Quebec teaching nurses performed above the average on the recent professional exam, OIIQ reported.
The professional licensing organization pointed out that nursing candidates have three attempts to pass their exam. “In order to better prepare for their next attempt, all those who failed received an individual response detailing the difficulties encountered. The OIIQ offers all the tools necessary to pass the exam; a detailed guide and preparatory workshops are available online.
“In the run up to the next exams, we will continue to support students by working with educational institutions to provide the optimal conditions for passing the exam. This exam is usually successful and we are convinced that the return to face-to-face teaching, as well as support for students, will be factors of success,” OIIQ President Luc Mathieu said in a press release.
Nursing candidates “who have not passed the exam will be put to work in the network, with the possibility of practicing under the supervision of a nurse. ... In addition, we will contact health establishments in order to support them in their supervision activities” of the candidates, he said.
A version of this article first appeared on Medscape.com.
Nursing oversight groups in the United States and Canada are holding the line on testing standards as more would-be nurses fail entry exams. As a result, pressure is growing to make tests easier to pass given widespread nursing shortages, and some critics wonder whether the exams accurately assess students’ true abilities.
When it comes to training more nurses to keep up with growing demand, the U.S. organization that oversees the main licensing exams for nurses decided earlier this month not to change the passing standards for entry-level tests. Meanwhile,
A similar scenario also is unfolding in Quebec, where the agency overseeing nurse licensing exams announced last month it is holding the line on its passing rates despite an outcry from nurses after more than half of those taking the exam in September failed. Quebec’s commissioner for professional admissions is investigating dozens of complaints from nurses about the failure rate. Nurses who failed the test can sign up to retake it in March.
Joseph Oujeil, DESS, DEF, has been teaching in Canada for 4 years, now at two Quebec nursing schools. “This is surprising and very shocking to our students as well as nurses from outside Quebec who were [completing] an integration program to adjust their practice to Quebec guidelines,” Mr. Oujeil told this news organization. Students from outside the province failed the licensing exam at a higher rate than their Quebec-native peers, he explained.
Quebec’s professional Order of Nurses of Quebec (OIIQ) responded to the nurses’ outcry in a press release last month, saying that the pandemic may be partly to blame for the lower passing rate because it made it more difficult to access internships, labs, and face-to-face teaching. Some students weren’t able to demonstrate their ability to practice during the exam as in previous years, OIIQ reported.
Mr. Oujeil agreed. “I’m sure the pandemic has an impact on the situation as well as some students did less training in hospitals” because of restrictions caused by the pandemic, he said. But students also told Mr. Oujeil some questions seemed ambiguous.
OIIQ stated in its release that it doesn’t want to lower the standard. The goal is to protect the public “by and with nurses,” to “ensure the competence and integrity of nurses in Quebec,” and “promote quality nursing practice,” the release noted.
Similarly in the United States, the National Council of State Boards of Nursing (NCSBN) announced Dec. 8 that it would uphold the current passing standards for its entry-level NCLEX tests for registered nurses and practical nurses. NCSBN analyzes the passing standard every 3 years “to keep the test plan and passing standard current,” a press release explains.
NCLEX pass rates have dropped from about 73% for all candidates and 88% for first-time U.S.-educated candidates to 69% and 82% respectively in 2021, the last full year for which results are available, NCSBN spokesperson Dawn Kappel told this news organization.
Over the past 3 years, including during the pandemic, the board decided “that the current passing standard is appropriate as a measure of safe and effective entry-level nurse practice,” after reviewing national nurse surveys and the findings of panels of nurses representing NCSBN’s geographic areas in the United States and Canada, board president Jay Douglas, MSM, RN, CSAC, said in a press release.
Still, NCSBN is not blind to the larger issues facing nursing, Ms. Kappel told this news organization. “There is a huge nursing shortage in the U.S. and Canada. We want as many nurses in the workforce as possible, but we want to ensure safe practice,” she said.
“Everyone has access to the same test, regardless of which state, province, or country they take it in,” she said. Some international students may not perform as well as U.S.-educated students because of their command of English and the nursing education standards in their home countries, Ms. Kappel added.
“Obviously COVID and the challenge of education in general” affected the results, she said.
Mr. Oujeil, the nursing school professor, said he is frustrated by the test results because the majority of students who failed maintained good grades and passed all of their trainings. Yet they scored just below the passing rate of 55%. He said students are proposing the passing rate be lowered to 50%. The current test doesn’t reflect what students are learning in the classroom or during clinical trainings, Mr. Oujeil added. “I don’t know of any students who scored more than 60%.”
He said he understands that the mission of the OIIQ is protecting the population, but he doesn’t believe lowering the passing rate to 50% will put the population at risk – and it will help offset the staffing shortage.
“I’m especially frustrated by those who were doing integration programs – mothers and fathers with children with family lives and financial responsibilities. Many of them are good, hard workers and were shocked they should have to pass the exam another time.”
Since 2018, the pass rate on the first attempt at the Quebec test has generally been between 71% and 96%, compared with 51.4% during the exam in September, according to the OIIQ press release. Meanwhile, graduates from 30 of the 55 schools and universities in Quebec teaching nurses performed above the average on the recent professional exam, OIIQ reported.
The professional licensing organization pointed out that nursing candidates have three attempts to pass their exam. “In order to better prepare for their next attempt, all those who failed received an individual response detailing the difficulties encountered. The OIIQ offers all the tools necessary to pass the exam; a detailed guide and preparatory workshops are available online.
“In the run up to the next exams, we will continue to support students by working with educational institutions to provide the optimal conditions for passing the exam. This exam is usually successful and we are convinced that the return to face-to-face teaching, as well as support for students, will be factors of success,” OIIQ President Luc Mathieu said in a press release.
Nursing candidates “who have not passed the exam will be put to work in the network, with the possibility of practicing under the supervision of a nurse. ... In addition, we will contact health establishments in order to support them in their supervision activities” of the candidates, he said.
A version of this article first appeared on Medscape.com.
Nursing oversight groups in the United States and Canada are holding the line on testing standards as more would-be nurses fail entry exams. As a result, pressure is growing to make tests easier to pass given widespread nursing shortages, and some critics wonder whether the exams accurately assess students’ true abilities.
When it comes to training more nurses to keep up with growing demand, the U.S. organization that oversees the main licensing exams for nurses decided earlier this month not to change the passing standards for entry-level tests. Meanwhile,
A similar scenario also is unfolding in Quebec, where the agency overseeing nurse licensing exams announced last month it is holding the line on its passing rates despite an outcry from nurses after more than half of those taking the exam in September failed. Quebec’s commissioner for professional admissions is investigating dozens of complaints from nurses about the failure rate. Nurses who failed the test can sign up to retake it in March.
Joseph Oujeil, DESS, DEF, has been teaching in Canada for 4 years, now at two Quebec nursing schools. “This is surprising and very shocking to our students as well as nurses from outside Quebec who were [completing] an integration program to adjust their practice to Quebec guidelines,” Mr. Oujeil told this news organization. Students from outside the province failed the licensing exam at a higher rate than their Quebec-native peers, he explained.
Quebec’s professional Order of Nurses of Quebec (OIIQ) responded to the nurses’ outcry in a press release last month, saying that the pandemic may be partly to blame for the lower passing rate because it made it more difficult to access internships, labs, and face-to-face teaching. Some students weren’t able to demonstrate their ability to practice during the exam as in previous years, OIIQ reported.
Mr. Oujeil agreed. “I’m sure the pandemic has an impact on the situation as well as some students did less training in hospitals” because of restrictions caused by the pandemic, he said. But students also told Mr. Oujeil some questions seemed ambiguous.
OIIQ stated in its release that it doesn’t want to lower the standard. The goal is to protect the public “by and with nurses,” to “ensure the competence and integrity of nurses in Quebec,” and “promote quality nursing practice,” the release noted.
Similarly in the United States, the National Council of State Boards of Nursing (NCSBN) announced Dec. 8 that it would uphold the current passing standards for its entry-level NCLEX tests for registered nurses and practical nurses. NCSBN analyzes the passing standard every 3 years “to keep the test plan and passing standard current,” a press release explains.
NCLEX pass rates have dropped from about 73% for all candidates and 88% for first-time U.S.-educated candidates to 69% and 82% respectively in 2021, the last full year for which results are available, NCSBN spokesperson Dawn Kappel told this news organization.
Over the past 3 years, including during the pandemic, the board decided “that the current passing standard is appropriate as a measure of safe and effective entry-level nurse practice,” after reviewing national nurse surveys and the findings of panels of nurses representing NCSBN’s geographic areas in the United States and Canada, board president Jay Douglas, MSM, RN, CSAC, said in a press release.
Still, NCSBN is not blind to the larger issues facing nursing, Ms. Kappel told this news organization. “There is a huge nursing shortage in the U.S. and Canada. We want as many nurses in the workforce as possible, but we want to ensure safe practice,” she said.
“Everyone has access to the same test, regardless of which state, province, or country they take it in,” she said. Some international students may not perform as well as U.S.-educated students because of their command of English and the nursing education standards in their home countries, Ms. Kappel added.
“Obviously COVID and the challenge of education in general” affected the results, she said.
Mr. Oujeil, the nursing school professor, said he is frustrated by the test results because the majority of students who failed maintained good grades and passed all of their trainings. Yet they scored just below the passing rate of 55%. He said students are proposing the passing rate be lowered to 50%. The current test doesn’t reflect what students are learning in the classroom or during clinical trainings, Mr. Oujeil added. “I don’t know of any students who scored more than 60%.”
He said he understands that the mission of the OIIQ is protecting the population, but he doesn’t believe lowering the passing rate to 50% will put the population at risk – and it will help offset the staffing shortage.
“I’m especially frustrated by those who were doing integration programs – mothers and fathers with children with family lives and financial responsibilities. Many of them are good, hard workers and were shocked they should have to pass the exam another time.”
Since 2018, the pass rate on the first attempt at the Quebec test has generally been between 71% and 96%, compared with 51.4% during the exam in September, according to the OIIQ press release. Meanwhile, graduates from 30 of the 55 schools and universities in Quebec teaching nurses performed above the average on the recent professional exam, OIIQ reported.
The professional licensing organization pointed out that nursing candidates have three attempts to pass their exam. “In order to better prepare for their next attempt, all those who failed received an individual response detailing the difficulties encountered. The OIIQ offers all the tools necessary to pass the exam; a detailed guide and preparatory workshops are available online.
“In the run up to the next exams, we will continue to support students by working with educational institutions to provide the optimal conditions for passing the exam. This exam is usually successful and we are convinced that the return to face-to-face teaching, as well as support for students, will be factors of success,” OIIQ President Luc Mathieu said in a press release.
Nursing candidates “who have not passed the exam will be put to work in the network, with the possibility of practicing under the supervision of a nurse. ... In addition, we will contact health establishments in order to support them in their supervision activities” of the candidates, he said.
A version of this article first appeared on Medscape.com.
Med students dismayed that residency match process won’t change
– mostly medical students, residents, and fellows – who supported the change.
The program’s decision comes after nearly 3 months of feedback from the public, medical students, and education community. Although about 60% of public respondents believed the change could reduce stress and allow students more time for momentous career decisions, the program’s board of directors decided the disadvantages were “of greater consequence,” according to a Oct. 28 statement.
Those disadvantages included introducing application or interview behaviors that could increase students’ stress; potentially identifying partially matched or unmatched applicants, which could lead to bias; and extending the match process time for those applicants.
In addition, members of 12 medical education and student organizations raised other concerns, such as the proposed change not addressing high application numbers, according to the statement. NRMP has reported record numbers of applicants over the past few years, typically with more applicants than available program slots.
“While the testimony gave nod to the positive aspects of the proposal ... there was substantially more concern voiced about the potential negative consequences identified in the public comments,” NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN, told this news organization. Some of those issues could not be addressed without further study, so the board decided not to proceed with the proposal, she explained.
The proposal would have separated the Main Residency Match into two phases and replaced the Supplemental Offer and Acceptance Program (SOAP), in which unmatched or partially matched applicants apply for unfilled residency positions. Under the proposed change, each phase would have operated the same way, from rank order lists and using a matching algorithm to a pair of Match Days instead of a single day.
The two-phase process would have given students who didn’t match more time to carefully weigh residency programs – they can apply to up to 45 placements as part of SOAP – that will guide their career path for the next few years, PGY-1 intern Asim A., who asked not to be identified further, told this news organization. The alternative is a hasty decision once students learn which residency spots are available, he added. “Applicants would have breathing room to make a more informed decision.”
Asim, who is Canadian, said he is participating in a transitional year in internal medicine in the hopes of being matched into internal medicine or psychiatry. He said Canada’s two-phase match is a “lot less stressful” than the U.S. system.
Meanwhile, students on Reddit’s medical school community also questioned NRMP’s decision.
“A significant majority of those surveyed thought it would be beneficial. But NRMP decides to not go through with it,” one Reddit user wrote. Another posted, “The one thing that could have improved the match and they chose not to do it.”
Others supported the decision to retain a 1-day match.
“I think this was the right call,” Bryan Carmody, MD, an outspoken medical education blogger, tweeted after learning of NRMP’s decision. Dr. Carmody, a pediatric nephrologist, previously expressed to this news organization misgivings about whether the two-phase match would make it difficult for programs to thoroughly review candidates and vice versa. He was concerned that it would compress the interview season and pressure programs to rapidly review applicants and conduct interviews.
More than 8,000 people responded to the public survey that began in August and ran for a month. Nearly two-thirds of the respondents (60%) were students, residents, or fellows. About 25% included faculty, program directors, and staff. Among the survey findings, respondents were equally divided between whether the two-phase match would be modestly advantageous (30%) or significantly advantageous (30%) compared to 20% who viewed it as modestly or significantly disadvantageous.
The NRMP said it would continue engaging with the community through focus groups and other means to improve the match experience and transition to residency.
“It is important to remember that a proposal is just that,” Dr. Lamb told this news orgnization, “an opportunity to discuss the pros and cons of an idea or framework ... and to mitigate unwanted consequences determined to be detrimental to learners and programs.”
The NRMP will involve the community in future discussions “to continue to give learners a voice,” she said.
A version of this article first appeared on Medscape.com.
– mostly medical students, residents, and fellows – who supported the change.
The program’s decision comes after nearly 3 months of feedback from the public, medical students, and education community. Although about 60% of public respondents believed the change could reduce stress and allow students more time for momentous career decisions, the program’s board of directors decided the disadvantages were “of greater consequence,” according to a Oct. 28 statement.
Those disadvantages included introducing application or interview behaviors that could increase students’ stress; potentially identifying partially matched or unmatched applicants, which could lead to bias; and extending the match process time for those applicants.
In addition, members of 12 medical education and student organizations raised other concerns, such as the proposed change not addressing high application numbers, according to the statement. NRMP has reported record numbers of applicants over the past few years, typically with more applicants than available program slots.
“While the testimony gave nod to the positive aspects of the proposal ... there was substantially more concern voiced about the potential negative consequences identified in the public comments,” NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN, told this news organization. Some of those issues could not be addressed without further study, so the board decided not to proceed with the proposal, she explained.
The proposal would have separated the Main Residency Match into two phases and replaced the Supplemental Offer and Acceptance Program (SOAP), in which unmatched or partially matched applicants apply for unfilled residency positions. Under the proposed change, each phase would have operated the same way, from rank order lists and using a matching algorithm to a pair of Match Days instead of a single day.
The two-phase process would have given students who didn’t match more time to carefully weigh residency programs – they can apply to up to 45 placements as part of SOAP – that will guide their career path for the next few years, PGY-1 intern Asim A., who asked not to be identified further, told this news organization. The alternative is a hasty decision once students learn which residency spots are available, he added. “Applicants would have breathing room to make a more informed decision.”
Asim, who is Canadian, said he is participating in a transitional year in internal medicine in the hopes of being matched into internal medicine or psychiatry. He said Canada’s two-phase match is a “lot less stressful” than the U.S. system.
Meanwhile, students on Reddit’s medical school community also questioned NRMP’s decision.
“A significant majority of those surveyed thought it would be beneficial. But NRMP decides to not go through with it,” one Reddit user wrote. Another posted, “The one thing that could have improved the match and they chose not to do it.”
Others supported the decision to retain a 1-day match.
“I think this was the right call,” Bryan Carmody, MD, an outspoken medical education blogger, tweeted after learning of NRMP’s decision. Dr. Carmody, a pediatric nephrologist, previously expressed to this news organization misgivings about whether the two-phase match would make it difficult for programs to thoroughly review candidates and vice versa. He was concerned that it would compress the interview season and pressure programs to rapidly review applicants and conduct interviews.
More than 8,000 people responded to the public survey that began in August and ran for a month. Nearly two-thirds of the respondents (60%) were students, residents, or fellows. About 25% included faculty, program directors, and staff. Among the survey findings, respondents were equally divided between whether the two-phase match would be modestly advantageous (30%) or significantly advantageous (30%) compared to 20% who viewed it as modestly or significantly disadvantageous.
The NRMP said it would continue engaging with the community through focus groups and other means to improve the match experience and transition to residency.
“It is important to remember that a proposal is just that,” Dr. Lamb told this news orgnization, “an opportunity to discuss the pros and cons of an idea or framework ... and to mitigate unwanted consequences determined to be detrimental to learners and programs.”
The NRMP will involve the community in future discussions “to continue to give learners a voice,” she said.
A version of this article first appeared on Medscape.com.
– mostly medical students, residents, and fellows – who supported the change.
The program’s decision comes after nearly 3 months of feedback from the public, medical students, and education community. Although about 60% of public respondents believed the change could reduce stress and allow students more time for momentous career decisions, the program’s board of directors decided the disadvantages were “of greater consequence,” according to a Oct. 28 statement.
Those disadvantages included introducing application or interview behaviors that could increase students’ stress; potentially identifying partially matched or unmatched applicants, which could lead to bias; and extending the match process time for those applicants.
In addition, members of 12 medical education and student organizations raised other concerns, such as the proposed change not addressing high application numbers, according to the statement. NRMP has reported record numbers of applicants over the past few years, typically with more applicants than available program slots.
“While the testimony gave nod to the positive aspects of the proposal ... there was substantially more concern voiced about the potential negative consequences identified in the public comments,” NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN, told this news organization. Some of those issues could not be addressed without further study, so the board decided not to proceed with the proposal, she explained.
The proposal would have separated the Main Residency Match into two phases and replaced the Supplemental Offer and Acceptance Program (SOAP), in which unmatched or partially matched applicants apply for unfilled residency positions. Under the proposed change, each phase would have operated the same way, from rank order lists and using a matching algorithm to a pair of Match Days instead of a single day.
The two-phase process would have given students who didn’t match more time to carefully weigh residency programs – they can apply to up to 45 placements as part of SOAP – that will guide their career path for the next few years, PGY-1 intern Asim A., who asked not to be identified further, told this news organization. The alternative is a hasty decision once students learn which residency spots are available, he added. “Applicants would have breathing room to make a more informed decision.”
Asim, who is Canadian, said he is participating in a transitional year in internal medicine in the hopes of being matched into internal medicine or psychiatry. He said Canada’s two-phase match is a “lot less stressful” than the U.S. system.
Meanwhile, students on Reddit’s medical school community also questioned NRMP’s decision.
“A significant majority of those surveyed thought it would be beneficial. But NRMP decides to not go through with it,” one Reddit user wrote. Another posted, “The one thing that could have improved the match and they chose not to do it.”
Others supported the decision to retain a 1-day match.
“I think this was the right call,” Bryan Carmody, MD, an outspoken medical education blogger, tweeted after learning of NRMP’s decision. Dr. Carmody, a pediatric nephrologist, previously expressed to this news organization misgivings about whether the two-phase match would make it difficult for programs to thoroughly review candidates and vice versa. He was concerned that it would compress the interview season and pressure programs to rapidly review applicants and conduct interviews.
More than 8,000 people responded to the public survey that began in August and ran for a month. Nearly two-thirds of the respondents (60%) were students, residents, or fellows. About 25% included faculty, program directors, and staff. Among the survey findings, respondents were equally divided between whether the two-phase match would be modestly advantageous (30%) or significantly advantageous (30%) compared to 20% who viewed it as modestly or significantly disadvantageous.
The NRMP said it would continue engaging with the community through focus groups and other means to improve the match experience and transition to residency.
“It is important to remember that a proposal is just that,” Dr. Lamb told this news orgnization, “an opportunity to discuss the pros and cons of an idea or framework ... and to mitigate unwanted consequences determined to be detrimental to learners and programs.”
The NRMP will involve the community in future discussions “to continue to give learners a voice,” she said.
A version of this article first appeared on Medscape.com.
Former nurse charged with murder in death of 97-year-old war veteran
A former Kentucky nurse was charged with murder stemming from an incident in which she gave “something special” to a 97-year-old patient who died 5 days later, according to multiple sources, including police and nursing records.
Ms. Hunter allegedly gave lorazepam, typically used for anxiety, to Mr. Morris on April 30. He subsequently developed pneumonia and died on May 5.
Ms. Hunter “intentionally performed actions of medical maltreatment,” according to the Lexington Police Department’s report.
A Baptist Health Lexington spokeswoman told this news organization that the nurse who was charged hasn’t worked at the hospital since the April incident. “We have learned that a former nurse at our hospital has been arrested yesterday on criminal charges,” spokeswoman Ruth Ann Childers stated. “The hospital has fully cooperated with the police investigation. Patient care and safety are always our top priorities. Out of respect for the patient’s family and because this is criminal matter, we are not able to talk about the investigation.”
According to the Kentucky Board of Nursing, which suspended Ms. Hunter’s RN license on a temporary basis on Aug. 22, she allegedly asked the on-duty physician and a nurse practitioner separately for a medication order to calm Mr. Morris, who had become agitated and aggressive. They denied Ms. Hunter’s request, so she withdrew lorazepam intended for another patient and administered it to Mr. Morris, the nursing board suspension order states. “When asked what was administered, she replied ‘something special,’ “ the order states.
Another RN found the patient with labored breathing and “it was determined that respondent had disarmed/lowered the oxygen monitoring system several times as to not set off an alarm at the bedside,” the order continued. “The RN discussed with charge nurse that the patient had been given something intravenously that was causing his decline.”
When the charge nurse entered the room later, she found the patient in “respiratory distress with labored breathing and poor oxygen saturation. ... X-rays would show that the aspiration from the substances ingested by the patient while in his condition caused the patient to develop aspirational pneumonia,” the order continues.
“Despite the rapidly declining condition of the patient, respondent never called for rapid response nor acted with any sense of urgency. Respondent did however edit documentation of administration of Ativan on ‘patient B’ to state ‘not given.’ ”
Mr. Morris’ condition never improved. He was taken to hospice care on May 3 and died 2 days later, the order states.
Ms. Hunter was being held in the Lexington Jail on $100,000 bond, according to jail records.
A version of this article first appeared on Medscape.com.
A former Kentucky nurse was charged with murder stemming from an incident in which she gave “something special” to a 97-year-old patient who died 5 days later, according to multiple sources, including police and nursing records.
Ms. Hunter allegedly gave lorazepam, typically used for anxiety, to Mr. Morris on April 30. He subsequently developed pneumonia and died on May 5.
Ms. Hunter “intentionally performed actions of medical maltreatment,” according to the Lexington Police Department’s report.
A Baptist Health Lexington spokeswoman told this news organization that the nurse who was charged hasn’t worked at the hospital since the April incident. “We have learned that a former nurse at our hospital has been arrested yesterday on criminal charges,” spokeswoman Ruth Ann Childers stated. “The hospital has fully cooperated with the police investigation. Patient care and safety are always our top priorities. Out of respect for the patient’s family and because this is criminal matter, we are not able to talk about the investigation.”
According to the Kentucky Board of Nursing, which suspended Ms. Hunter’s RN license on a temporary basis on Aug. 22, she allegedly asked the on-duty physician and a nurse practitioner separately for a medication order to calm Mr. Morris, who had become agitated and aggressive. They denied Ms. Hunter’s request, so she withdrew lorazepam intended for another patient and administered it to Mr. Morris, the nursing board suspension order states. “When asked what was administered, she replied ‘something special,’ “ the order states.
Another RN found the patient with labored breathing and “it was determined that respondent had disarmed/lowered the oxygen monitoring system several times as to not set off an alarm at the bedside,” the order continued. “The RN discussed with charge nurse that the patient had been given something intravenously that was causing his decline.”
When the charge nurse entered the room later, she found the patient in “respiratory distress with labored breathing and poor oxygen saturation. ... X-rays would show that the aspiration from the substances ingested by the patient while in his condition caused the patient to develop aspirational pneumonia,” the order continues.
“Despite the rapidly declining condition of the patient, respondent never called for rapid response nor acted with any sense of urgency. Respondent did however edit documentation of administration of Ativan on ‘patient B’ to state ‘not given.’ ”
Mr. Morris’ condition never improved. He was taken to hospice care on May 3 and died 2 days later, the order states.
Ms. Hunter was being held in the Lexington Jail on $100,000 bond, according to jail records.
A version of this article first appeared on Medscape.com.
A former Kentucky nurse was charged with murder stemming from an incident in which she gave “something special” to a 97-year-old patient who died 5 days later, according to multiple sources, including police and nursing records.
Ms. Hunter allegedly gave lorazepam, typically used for anxiety, to Mr. Morris on April 30. He subsequently developed pneumonia and died on May 5.
Ms. Hunter “intentionally performed actions of medical maltreatment,” according to the Lexington Police Department’s report.
A Baptist Health Lexington spokeswoman told this news organization that the nurse who was charged hasn’t worked at the hospital since the April incident. “We have learned that a former nurse at our hospital has been arrested yesterday on criminal charges,” spokeswoman Ruth Ann Childers stated. “The hospital has fully cooperated with the police investigation. Patient care and safety are always our top priorities. Out of respect for the patient’s family and because this is criminal matter, we are not able to talk about the investigation.”
According to the Kentucky Board of Nursing, which suspended Ms. Hunter’s RN license on a temporary basis on Aug. 22, she allegedly asked the on-duty physician and a nurse practitioner separately for a medication order to calm Mr. Morris, who had become agitated and aggressive. They denied Ms. Hunter’s request, so she withdrew lorazepam intended for another patient and administered it to Mr. Morris, the nursing board suspension order states. “When asked what was administered, she replied ‘something special,’ “ the order states.
Another RN found the patient with labored breathing and “it was determined that respondent had disarmed/lowered the oxygen monitoring system several times as to not set off an alarm at the bedside,” the order continued. “The RN discussed with charge nurse that the patient had been given something intravenously that was causing his decline.”
When the charge nurse entered the room later, she found the patient in “respiratory distress with labored breathing and poor oxygen saturation. ... X-rays would show that the aspiration from the substances ingested by the patient while in his condition caused the patient to develop aspirational pneumonia,” the order continues.
“Despite the rapidly declining condition of the patient, respondent never called for rapid response nor acted with any sense of urgency. Respondent did however edit documentation of administration of Ativan on ‘patient B’ to state ‘not given.’ ”
Mr. Morris’ condition never improved. He was taken to hospice care on May 3 and died 2 days later, the order states.
Ms. Hunter was being held in the Lexington Jail on $100,000 bond, according to jail records.
A version of this article first appeared on Medscape.com.