User login
Quick Diagnosis Units
Inpatient admissions are a major component of healthcare costs in the United States,[1] where the number of annual inpatient hospital admissions has increased by 15% from 34.3 million in 1993 to 39.5 million in 2006.2 Studies performed predominantly in Europe have shown that inappropriate use of hospital beds exceeds 20% across various specialties.[3] A study by Campbell et al. showed that if given the choice, 60% of physicians would consider an alternative to admission for such patients, if such an option were available, and 70% of patients would prefer not to be admitted for workup.[4] Based on similar findings, various hospitals across the world have tried to make organizational changes to allocate healthcare resources more efficiently. The concept of quick and early diagnosis was first introduced in 1996 by Kendall et al., and it included a hospital unit in the United Kingdom managed by consultants receiving referrals from primary care doctors and led to early diagnostic workup without hospitalization.[5] A more refined version of this concept, a potentially cost‐saving and efficient alternative to inpatient hospitalization for diagnostic purposes, was described by Bosch et al., and named the quick diagnosis unit (QDU).[1]
The basic objectives of QDUs include early diagnosis of potentially severe diseases such as cancer, avoiding unnecessary hospitalization, minimizing hospital morbidity, reducing costs, and improving patient satisfaction. The first described QDU was managed by internists, where patients with specific symptoms such as undiagnosed lumps or masses, anemia, hematuria, or gastrointestinal symptoms could be referred for a diagnostic evaluation. Patients were required to be well enough to travel to the QDU on an outpatient basis, and patients unable to do so were thought to be better suited for hospitalization.[1]
In the present study, we conduct a systematic review, the first one on this subject to our knowledge, of studies that tested established QDUs or similar units in hospital settings. The majority of established units were tested and exist in Europe.[1, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14] They have been studied in Spain, from where much of these data have been obtained.[1]
METHODS
Study Selection
We searched MEDLINE (January 1946 to November 2012) via OVID and EMBASE (January 1974 to November 2012) via SCOPUS using keywords and Medical Subject Heading terms for quick diagnosis units and rapid diagnosis units. The detailed search strategy can be found in Table 1. A screening of titles and abstracts was done by 2 independent reviewers and followed by full‐text screening. We screened for additional articles by reviewing the bibliography of the articles selected for full‐text screening. We included in our review all studies that (1) were published in any language, (2) focused on the design and implementation of a quick diagnosis unit or a rapid diagnosis unit in a hospital setting, and (3) included at least 2 of the primary outcomes, as described below.
| No. | Searches |
|---|---|
| 1 | Quick diagnosis units.mp. |
| 2 | Quick diagnosis unit.mp. |
| 3 | (Quick adj diagnosis adj units).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 4 | (Quick adj diagnosis adj unit).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 5 | (Quick adj diagnosis).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 6 | (Diagnosis adj unit).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 7 | (Diagnosis adj units).mp [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 8 | Rapid diagnosis units.mp. |
| 9 | Rapid diagnosis unit.mp. |
| 10 | (Rapid adj diagnosis adj units).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 11 | (Rapid adj diagnosis adj unit).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 12 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 |
Outcome Measures
Our primary outcome measures were categories of final diagnosis, mean time to final diagnosis in an outpatient setting, inpatient bed‐days per patient saved, and costs saved per patient for QDUs versus in‐hospital stay. Secondary outcomes included disposition of patients after completion of this initial evaluation (whether admitted to the hospital or discharged to clinics) and the patients' care preferences, if available. For cost outcomes, currency exchange rates used for conversion were provided by Citibank National Bank Association, powered by Google online currency converter service (accessed June 16, 2013).
Data Extraction
We extracted data on the specifics of the early diagnostic unit setup including staffing and hours of operation, hospital setting, sources of referral, referring diagnosis, patient population, and the role of the diagnostic units in expediting workup and duration of study. For multiple studies done in the same institution by the same principal author, we used the study with the largest patient population to avoid duplication of data. The primary outcome measures for comparing costs were calculated by different methods and in different currencies by different investigators, which we have attempted to reconcile by using current currency conversion rates. We also evaluated patient preferences (if available) via patient surveys. The data were extracted by 2 independent reviewers, and disagreements were resolved by consensus.
RESULTS
Study Selection
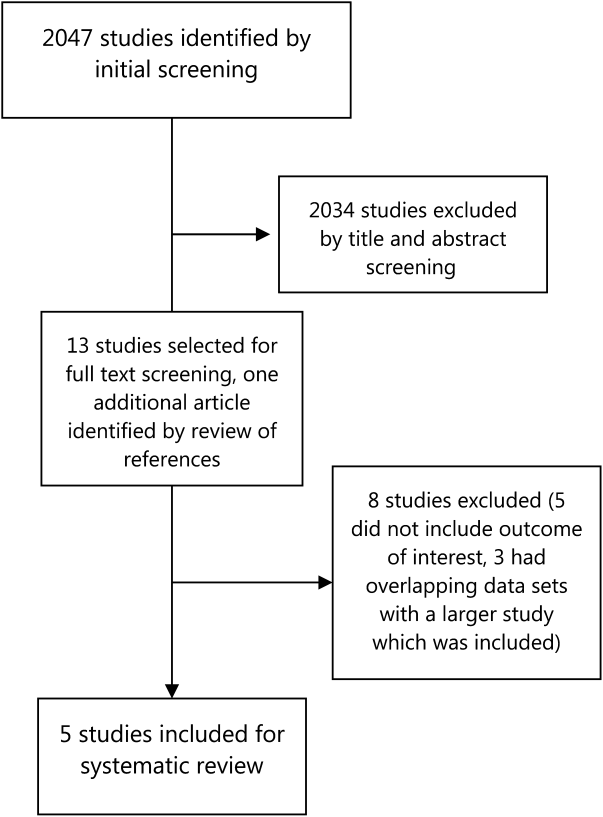
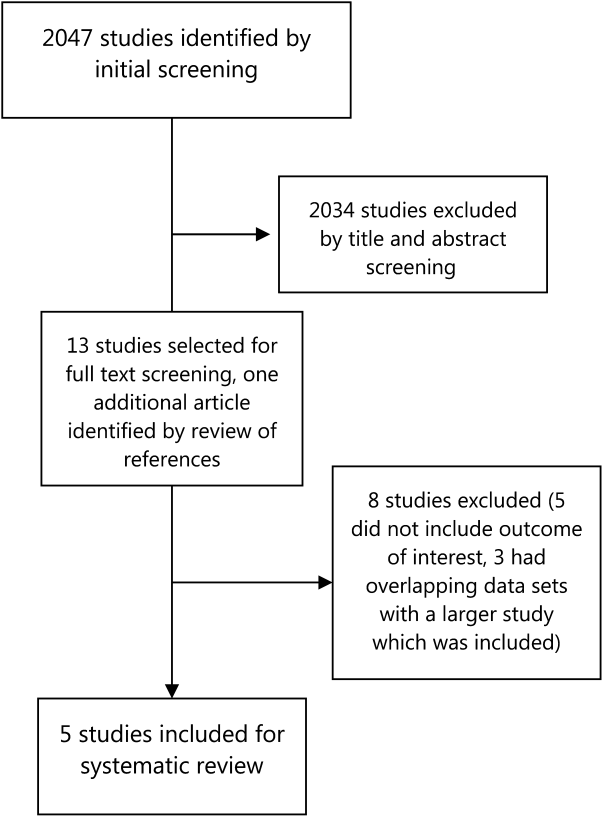
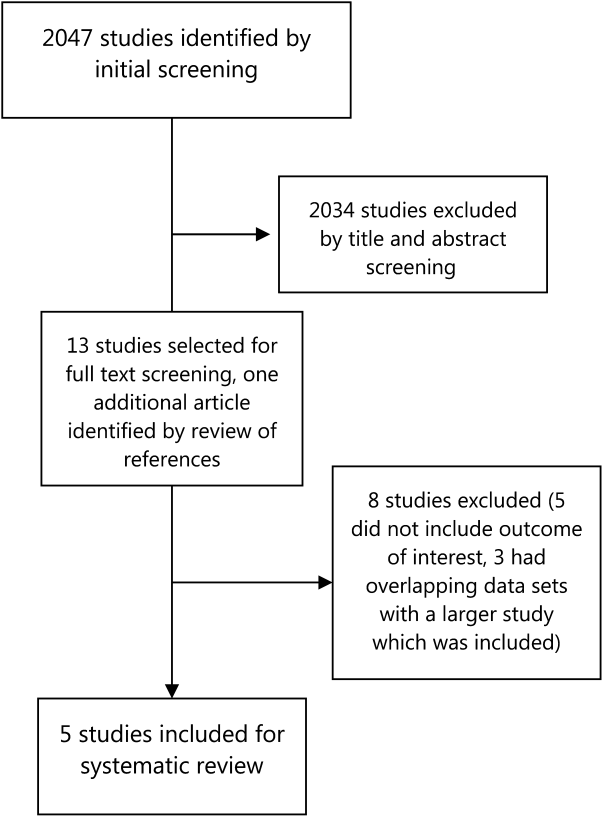
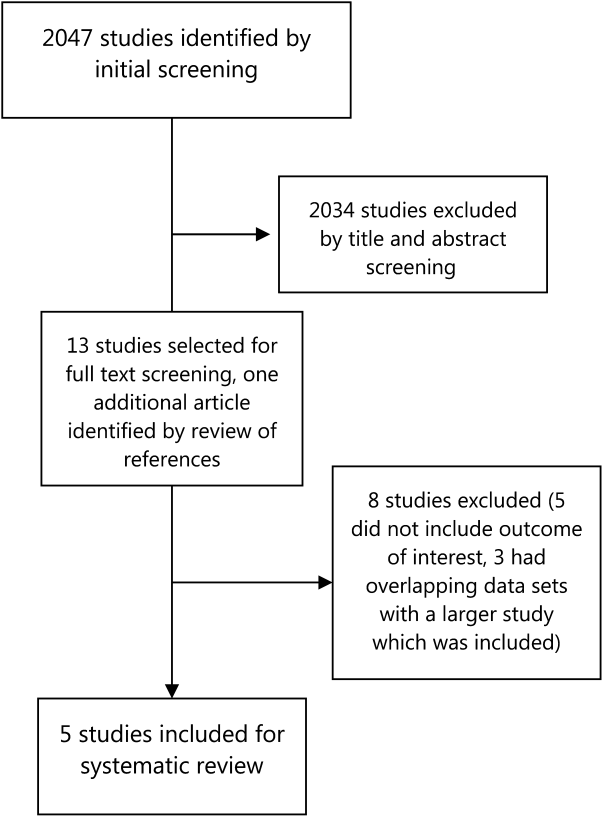
Our literature search initially yielded 2047 publications, out of which 2034 were excluded after title and abstract screening. Thirteen studies were selected for full‐text review, out of which 5 were selected for detailed review based on our inclusion criteria (Figure 1). Three of the studies were in Spanish, and the results were analyzed with the help of a Spanish translator. The other 2 studies were in English.
Study Characteristics
Four studies that were included were descriptive longitudinal studies,[6, 7, 9, 10] and 1 was a retrospective study[8] (Table 2). There were a total of 8895 patients included in all of the studies. All of the studies except 1 described a similar organizational arrangement for the QDU, with 1 internist and 1 registered nurse, administrative support, and the ability to expedite the scheduling of diagnostic tests. The exception was a dedicated lung cancer rapid diagnostic unit (RDU) set up by Sanz‐Santos et al.[9] The study durations ranged from 6 months to 5 years. Patients were referred from local emergency rooms, primary care clinics, and specialty care clinics. The most common reasons for referral were anemia, adenopathy, visceromegaly, febrile syndromes, and incidentally detected masses or nodules on imaging. Two studies included some form of cost analysis,[6, 7] and 3 included patient surveys on satisfaction with patient care.[6, 7, 10]
| Author | Methods | Setup of Rapid Diagnosis Units | Sources of Referrals to the Unit | Reasons for Referrals to the Unit | Cases | Duration | Intervention |
|---|---|---|---|---|---|---|---|
| |||||||
| Bosch et al., 2012 | Prospective descriptive study in 4,170 patients evaluated by a dedicated QDU in a university hospital in Barcelona, Spain, between December 2007 to December 2009 and January 2010 to January 2012. QDU costs compared with costs for randomly selected, retrospectively reviewed hospital admissions for similar diagnosis. Care preferences studied with random surveys. | Quick diagnostic unit consisting of an internist, and a registered nurse. Single consulting room with a family waiting room. Assisted by specialists from other specialties. | Local primary health center (40%), emergency room (56%), other sources (4%). | Anemia, anorexia‐cachexia syndrome, febrile syndrome, adenopathies, abdominal pain, chronic diarrhea, lung abnormalities. | 4,170 | 4 years | Outpatient workup with urgent first visit, preferential scheduling of diagnostic tests and follow‐up until diagnosis is made. |
| Capell et al., 2004 | Prospective descriptive study with retrospective controls in 2,748 patients evaluated by a QEDU in a university hospital in Barcelona, Spain, between September 1996 and 2001. QEDU costs compared with costs for randomly selected, retrospectively reviewed hospital admissions for similar diagnosis. Care preferences studied with random surveys. | UDR made up of an internist and a nurse, a consultation and waiting room. | Referrals from emergency rooms (64%), primary care (28.6%), specialty clinics (6.4%). | Abdominal pain (12%), focal neurological symptoms (11.5%), constitutional symptoms (11%), anemia (6%), abnormal chest radiology (5.8%), palpable tumors (5.3%), adenopathies (4.7%), rectal bleeding (4.6%), febrile syndrome (4.6%), hemoptysis (3.5%), others (30%). | 2,748 | 5 years | Preferential scheduling and urgent workup. |
| Rubio‐Rivas et al., 2008 | Retrospective, descriptive study for 1,132 patients evaluated by a dedicated RDU in a university hospital in Barcelona, Spain from October 2005 to March 2007. | RDU consisted of an internist, a radiologist, and a nurse. | Local primary health centers (71%), emergency rooms (26%), and others (3%). | FUO, adenopathies, visceromegalies, chronic diarrhea, rectal bleeding, dysphagia, jaundice, hypercalcemia. | 1,132 | 11.5 years | Prioritized scheduling and urgent workup. |
| Sanz‐Santos et al., 2010 | Prospective observational study in 678 patients referred to an LC RDU, at a tertiary care center in Barcelona, Spain from October 2005 to September 2009. | An LC‐RDU, with nursing staff, 3 pulmonologists, bronchoscopy suites with EBUS‐TBNA, facilities for mediastinoscopy, CT‐guided FNAC, thoracoscopy, and surgery. | Referrals from specialty clinics (59.4%), primary care (20.2%), and local emergency rooms (20.4%). | Cough, dyspnea, hemoptysis, weight loss, imaging evidence of lung masses. | 678 | 4 years | Specialized outpatient noninvasive and invasive workup. |
| Franco‐Hidalgo et al., 2012 | Prospective descriptive study on 167 patients, evaluated by an RDU in a tertiary care hospital in Palencia, Spain between November 2008 and April 2009. Care preferences studied with random surveys. | An RDU run by an internist and nursing staff with administrative support. Has a consulting room and a waiting room. | Referrals from primary care (70.7%), emergency room (21.6%), specialty clinics (7.8%). | Abdominal masses and visceromegalies, chronic diarrhea, dysphagia, ascites, icterus, transaminitis, heart failure, abnormal chest imaging, suspicion of pulmonary TB, or neoplasia, | 167 | 6 months | Early scheduling and urgent specialized workup. |
Outcomes
The most common final diagnosis was malignancy in 18% to 30% of the cases[6, 7, 8, 10] and in 55% of the lung cancer RDU cases[9] (Table 3). The time from initial contact to final diagnosis ranged from 6 to 11 days. Only 3% to 10% of the patients were admitted to the hospital from the QDUs; most patients were discharged to specialty‐care clinics or to primary care centers. Capell et al.[7] estimated that such a unit could save 7 inpatient bed‐days per patient, whereas Rubio‐Rivas et al.[8] estimated that value to be 4.5 bed‐days per patient. Bosch et al.[6] calculated that they saved 8.76 bed‐days per patient.
| Author | Final Diagnosis | Time to Diagnosis | Final Disposition | Benefit Analysis | Care Preference Survey | Duration | Intervention |
|---|---|---|---|---|---|---|---|
| |||||||
| Bosch et al., 2012 | Malignancy (30%), IDA (19%), other benign GI disorders (12%), others (39%). | Mean=8.9 days (cases) (3.13 QDU visits) | Hospital for admission: 3%, primary health centers: 62%, outpatient follow‐up: 35%. | Estimated hospital days saved: mean length of stay 8.76 days. Average cost saved per process (admission to discharge): 2,514.64. | 88% preferred QDU care model over hospital stay. | 4 years | Outpatient workup with urgent first visit, preferential scheduling of diagnostic tests, and follow‐up until diagnosis is made. |
| Capell et al., 2004 | Malignancy (15%), GI disorders (24%), neurological disorders (14%). | Mean=5.7 days | Hospital for admission: 7%, primary care: 51%, outpatient hospital follow‐up: 38%,specialty clinics: 4%. | Estimated 7 inpatient bed/days per year during the period of study. Cost saved per encounter: 1,764. | 95% reported high satisfaction with QEDU. | 5 years | Prioritized scheduling and urgent workup. |
| Rubio‐Rivas et al., 2008 | Malignancy (18%). | Mean=9 days | Hospital for admission: 10%, outpatient follow‐up: 56%, discharged from follow‐up: 38%. | Hospitalizations avoided: 4.5 bed/days over the study period. Cost analysis not available. | None | 11.5 years | Prioritized scheduling and urgent workup. |
| Sanz‐Santos et al., 2010 | Lung cancer (55%). | Mean=11 days | Not available. | No available data on cost analysis or hospitalizations avoided. | None | 4 years | Specialized outpatient noninvasive and invasive workup. |
| Franco‐Hidalgo et al., 2012 | Neoplastic (19%), nonmalignant digestive diseases (23%,), infection 13%, and rheumatic (11%). | Mean=8 days | Not available. | No available data on cost analysis or hospitalizations avoided. | 97% reported high/very high satisfaction with the UDR. | 6 months | Early scheduling and urgent specialized workup. |
Two studies included a cost comparison between a conventional inpatient evaluation and a QDU evaluation. Bosch et al.[6] and Capell et al.[7] found an average saving of $3304 (2514) and $2353 (1764) per patient, respectively. Bosch et al.[6] calculated these savings by comparing QDU patients to randomly selected control patients with similar referring complaints, who had reached their final diagnosis during a conventional inpatient evaluation. Capell et al.[7] compared their QDU patient costs to estimated in‐hospital costs for similar diagnoses.
Safety data were reported in detail only by Bosch et al.[6] who showed that 125 (3%) patients who initially were stable for QDU evaluation were referred to the emergency department. A total of 15 patients required admission and 12 died, with an overall mortality for the QDU cohort of 0.3%. Causes of death in this group included sudden unexplained death in 8 patients, pulmonary embolism in 2, aspiration pneumonia in 1, and shock of unknown origin in 1. Capell et al.[7] described a 7% admission rate, and Rubio‐Rivas et al.[8] noted that number to be 10%. No mortality was reported in these 2 studies.
In terms of preference for care, an overwhelming majority (88%) of patients in 1 study[6] preferred the QDU care model over hospitalization, and 95% to 97% of patients in 2 other studies[7, 10] reported very high satisfaction rates.
DISCUSSION
Our systematic review evaluated the effectiveness of QDUs for the diagnostic evaluation of patients with potentially severe disease and showed that such units, where established, are cost‐effective, prevent unnecessary hospitalizations, and diagnose potentially severe diseases, particularly malignant conditions, in a timely manner.
QDUs can evaluate medically stable patients with a variety of complaints such as anemia, lymphadenopathy, undiagnosed lumps and masses, and gastrointestinal symptoms and accelerate the diagnostic evaluation without requiring inpatient hospitalization. Many times patients are admitted to the hospital for a diagnostic evaluation without actual treatment.[12] These patients may not be sick enough to warrant hospitalization and may be able to return to the clinic for an outpatient workup. The QDU approach can complete the evaluation in such patients with the added advantages of saving money and higher patient satisfaction, due to diminished disruption of the patient's daily life.[1, 12] As most primary care physicians are unlikely to provide regular and frequent access for unscheduled care and EDs are more likely to admit patients for diagnostic workup,[2] a QDU approach seems a reasonable alternative for making a quick diagnosis and at the same time avoiding unnecessary hospitalization. Bosch et al. have also evaluated the impact of the QDUs in the diagnosis of specific diseases such as cancer in 169 patients diagnosed at the QDU, and compared them to 53 patients who were diagnosed with cancer during an inpatient evaluation.[11] They found that although QDU patients were significantly younger than hospitalized patients, there was no difference in diagnoses established and the time to diagnosis at the QDU and length of stay in the hospital.
There is a significant cost saving associated with QDUs. The cost savings calculated by Bosch et al. and Capell et al. were for each patient enrolled in this protocol from index encounter to final diagnosis.[6, 7] These 2 studies describe primarily fixed costs saved per patient treated in the QDU versus an inpatient admission. Fixed costs in hospital care include personnel cost, buildings, and equipment, whereas variable costs include medication, test reagents, and disposable supplies.[15] In comparison with the US healthcare system, fixed costs in Europe are considerably lower, and certain variable costs (like medications and procedures) are significantly higher in the United States.[16] This suggests a greater opportunity for healthcare savings for carefully selected patients in the United States, where costs related to inpatient admissions are significantly higher.[16]
Another limitation of our analysis is the paucity of studies on this topic. Many of the publications are from Bosch et al.,[1, 6, 11, 12, 13, 14] a single group in Spain, and these show considerable cost savings, patient satisfaction, and patient safety. However, most of their data are either retrospective or from nonrandomized, prospective cohort studies. The only report describing a similar approach in the United States was by Paschal in the city of New Orleans.[17] After Charity Hospital and the Veterans Affairs Hospital in New Orleans were lost to hurricane Katrina, an urgent care clinic was set up where potentially severe diseases such as cancer, leukemia, and autoimmune and endocrine disorders were diagnosed efficiently, although safety data were not reported.
The reported studies used different study designs and evaluated different primary outcomes. These limitations can be overcome with a well‐designed prospective trial, which could also evaluate the actual impact on patient care, safety, and healthcare savings in the United States.
Safety data were reported in detail only in 1 study,[6] and the rates of admissions were reported by 2 other studies.[7, 8] These suggest that QDUs may be safe for a selected group of patients. Patients evaluated in these units preferred this approach as shown by the overwhelming majority of the patients who chose QDU care over inpatient admissions when patient surveys were performed.
CONCLUSION
In this era of healthcare reform and emphasis on value‐based care, we must optimize the efficiency of our care delivery systems and challenge our preexisting resource‐intensive healthcare models. One source of potential savings is avoiding hospitalizations for purely diagnostic purposes, utilizing quick diagnostic units for patients who are able to return for outpatient evaluations. Such units are established, have been studied in Europe, and our systematic review shows that they are cost‐effective, time‐ and resource‐efficient, and preferred by patients. In our healthcare system, with the high cost of inpatient care, the QDU can yield large savings of healthcare dollars while expediting diagnostic workup, increasing patient satisfaction, and preventing lost productivity from hospital stays. Further exploration and study of alternative care delivery models, such as quick diagnostic units, is required to achieve the goal of cost‐effective high‐quality care for all.
Disclosure: Nothing to report.
- , , , , . Quick diagnosis units: a potentially useful alternative to conventional hospitalization. Med J Aust. 2009;191:496–498.
- , . The growing role of emergency departments in hospital admissions. N Engl J Med. 2012;5:391–393.
- , , . Measuring appropriate use of acute beds. A Systematic review of methods and results. Health Policy. 2000;3:157–184.
- . Inappropriate admissions: thoughts of patients and referring doctors. J R Soc Med. 2001;12:628–631.
- , , . QED: quick and early diagnosis. Lancet. 1996;348:528–529.
- , , . Quick diagnosis units: avoiding referrals from primary care to the ED and hospitalizations. Am J Emerg Med. 2013;31(1):114–123.
- , , , et al. Quick and early diagnostic outpatient unit: an effective and efficient assistential model. Five years experience. Med Clin (Barc). 2004;123(7):247–250.
- , , , . Rapid diagnosis unit in a third level hospital. Descriptive study of the first year and a half. Rev Clin Esp. 2008;208(11):561–563.
- , , , et al. Usefulness of a lung cancer rapid diagnosis specialist clinic. Contribution of ultrasound bronchoscopy. Arch Bronconeumol. 2010;46(12):640–645.
- , , , . Rapid diagnosis units or immediate health care clinics in internal medicine. Analysis of the first six months of operation in Palencia (Spain). Semergen. 2012;38(2):126–130.
- , , , , . Comparison of quick diagnosis units and conventional hospitalization for the diagnosis of cancer in Spain: a descriptive cohort study. Oncology (Switzerland). 2012;83(5):283–291.
- , , , . Quick diagnosis units versus hospitalization for the diagnosis of potentially severe diseases in Spain. J Hosp Med. 2012;7(1):41–47.
- , , , , . Outpatient quick diagnosis units for the evaluation of suspected severe diseases: an observational study. Clinics. 2011;66(5):737–741.
- , , , et al. Quick diagnosis units or conventional hospitalization for the diagnostic evaluation of severe anemia: a paradigm shift in public health systems? Eur J Int Med. 2012;23(2):159–164.
- , , , et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999;281(7):644–649.
- . Explaining high healthcare spending in the united states: an international comparison of supply, utilization, prices and quality. Issue Brief (Commonw Fund). 2012;10:1–14.
- . Launching complex medical workups from an urgent care platform. Ann Int Med. 2012;156:232–233.
Inpatient admissions are a major component of healthcare costs in the United States,[1] where the number of annual inpatient hospital admissions has increased by 15% from 34.3 million in 1993 to 39.5 million in 2006.2 Studies performed predominantly in Europe have shown that inappropriate use of hospital beds exceeds 20% across various specialties.[3] A study by Campbell et al. showed that if given the choice, 60% of physicians would consider an alternative to admission for such patients, if such an option were available, and 70% of patients would prefer not to be admitted for workup.[4] Based on similar findings, various hospitals across the world have tried to make organizational changes to allocate healthcare resources more efficiently. The concept of quick and early diagnosis was first introduced in 1996 by Kendall et al., and it included a hospital unit in the United Kingdom managed by consultants receiving referrals from primary care doctors and led to early diagnostic workup without hospitalization.[5] A more refined version of this concept, a potentially cost‐saving and efficient alternative to inpatient hospitalization for diagnostic purposes, was described by Bosch et al., and named the quick diagnosis unit (QDU).[1]
The basic objectives of QDUs include early diagnosis of potentially severe diseases such as cancer, avoiding unnecessary hospitalization, minimizing hospital morbidity, reducing costs, and improving patient satisfaction. The first described QDU was managed by internists, where patients with specific symptoms such as undiagnosed lumps or masses, anemia, hematuria, or gastrointestinal symptoms could be referred for a diagnostic evaluation. Patients were required to be well enough to travel to the QDU on an outpatient basis, and patients unable to do so were thought to be better suited for hospitalization.[1]
In the present study, we conduct a systematic review, the first one on this subject to our knowledge, of studies that tested established QDUs or similar units in hospital settings. The majority of established units were tested and exist in Europe.[1, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14] They have been studied in Spain, from where much of these data have been obtained.[1]
METHODS
Study Selection
We searched MEDLINE (January 1946 to November 2012) via OVID and EMBASE (January 1974 to November 2012) via SCOPUS using keywords and Medical Subject Heading terms for quick diagnosis units and rapid diagnosis units. The detailed search strategy can be found in Table 1. A screening of titles and abstracts was done by 2 independent reviewers and followed by full‐text screening. We screened for additional articles by reviewing the bibliography of the articles selected for full‐text screening. We included in our review all studies that (1) were published in any language, (2) focused on the design and implementation of a quick diagnosis unit or a rapid diagnosis unit in a hospital setting, and (3) included at least 2 of the primary outcomes, as described below.
| No. | Searches |
|---|---|
| 1 | Quick diagnosis units.mp. |
| 2 | Quick diagnosis unit.mp. |
| 3 | (Quick adj diagnosis adj units).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 4 | (Quick adj diagnosis adj unit).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 5 | (Quick adj diagnosis).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 6 | (Diagnosis adj unit).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 7 | (Diagnosis adj units).mp [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 8 | Rapid diagnosis units.mp. |
| 9 | Rapid diagnosis unit.mp. |
| 10 | (Rapid adj diagnosis adj units).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 11 | (Rapid adj diagnosis adj unit).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 12 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 |
Outcome Measures
Our primary outcome measures were categories of final diagnosis, mean time to final diagnosis in an outpatient setting, inpatient bed‐days per patient saved, and costs saved per patient for QDUs versus in‐hospital stay. Secondary outcomes included disposition of patients after completion of this initial evaluation (whether admitted to the hospital or discharged to clinics) and the patients' care preferences, if available. For cost outcomes, currency exchange rates used for conversion were provided by Citibank National Bank Association, powered by Google online currency converter service (accessed June 16, 2013).
Data Extraction
We extracted data on the specifics of the early diagnostic unit setup including staffing and hours of operation, hospital setting, sources of referral, referring diagnosis, patient population, and the role of the diagnostic units in expediting workup and duration of study. For multiple studies done in the same institution by the same principal author, we used the study with the largest patient population to avoid duplication of data. The primary outcome measures for comparing costs were calculated by different methods and in different currencies by different investigators, which we have attempted to reconcile by using current currency conversion rates. We also evaluated patient preferences (if available) via patient surveys. The data were extracted by 2 independent reviewers, and disagreements were resolved by consensus.
RESULTS
Study Selection
Our literature search initially yielded 2047 publications, out of which 2034 were excluded after title and abstract screening. Thirteen studies were selected for full‐text review, out of which 5 were selected for detailed review based on our inclusion criteria (Figure 1). Three of the studies were in Spanish, and the results were analyzed with the help of a Spanish translator. The other 2 studies were in English.
Study Characteristics
Four studies that were included were descriptive longitudinal studies,[6, 7, 9, 10] and 1 was a retrospective study[8] (Table 2). There were a total of 8895 patients included in all of the studies. All of the studies except 1 described a similar organizational arrangement for the QDU, with 1 internist and 1 registered nurse, administrative support, and the ability to expedite the scheduling of diagnostic tests. The exception was a dedicated lung cancer rapid diagnostic unit (RDU) set up by Sanz‐Santos et al.[9] The study durations ranged from 6 months to 5 years. Patients were referred from local emergency rooms, primary care clinics, and specialty care clinics. The most common reasons for referral were anemia, adenopathy, visceromegaly, febrile syndromes, and incidentally detected masses or nodules on imaging. Two studies included some form of cost analysis,[6, 7] and 3 included patient surveys on satisfaction with patient care.[6, 7, 10]
| Author | Methods | Setup of Rapid Diagnosis Units | Sources of Referrals to the Unit | Reasons for Referrals to the Unit | Cases | Duration | Intervention |
|---|---|---|---|---|---|---|---|
| |||||||
| Bosch et al., 2012 | Prospective descriptive study in 4,170 patients evaluated by a dedicated QDU in a university hospital in Barcelona, Spain, between December 2007 to December 2009 and January 2010 to January 2012. QDU costs compared with costs for randomly selected, retrospectively reviewed hospital admissions for similar diagnosis. Care preferences studied with random surveys. | Quick diagnostic unit consisting of an internist, and a registered nurse. Single consulting room with a family waiting room. Assisted by specialists from other specialties. | Local primary health center (40%), emergency room (56%), other sources (4%). | Anemia, anorexia‐cachexia syndrome, febrile syndrome, adenopathies, abdominal pain, chronic diarrhea, lung abnormalities. | 4,170 | 4 years | Outpatient workup with urgent first visit, preferential scheduling of diagnostic tests and follow‐up until diagnosis is made. |
| Capell et al., 2004 | Prospective descriptive study with retrospective controls in 2,748 patients evaluated by a QEDU in a university hospital in Barcelona, Spain, between September 1996 and 2001. QEDU costs compared with costs for randomly selected, retrospectively reviewed hospital admissions for similar diagnosis. Care preferences studied with random surveys. | UDR made up of an internist and a nurse, a consultation and waiting room. | Referrals from emergency rooms (64%), primary care (28.6%), specialty clinics (6.4%). | Abdominal pain (12%), focal neurological symptoms (11.5%), constitutional symptoms (11%), anemia (6%), abnormal chest radiology (5.8%), palpable tumors (5.3%), adenopathies (4.7%), rectal bleeding (4.6%), febrile syndrome (4.6%), hemoptysis (3.5%), others (30%). | 2,748 | 5 years | Preferential scheduling and urgent workup. |
| Rubio‐Rivas et al., 2008 | Retrospective, descriptive study for 1,132 patients evaluated by a dedicated RDU in a university hospital in Barcelona, Spain from October 2005 to March 2007. | RDU consisted of an internist, a radiologist, and a nurse. | Local primary health centers (71%), emergency rooms (26%), and others (3%). | FUO, adenopathies, visceromegalies, chronic diarrhea, rectal bleeding, dysphagia, jaundice, hypercalcemia. | 1,132 | 11.5 years | Prioritized scheduling and urgent workup. |
| Sanz‐Santos et al., 2010 | Prospective observational study in 678 patients referred to an LC RDU, at a tertiary care center in Barcelona, Spain from October 2005 to September 2009. | An LC‐RDU, with nursing staff, 3 pulmonologists, bronchoscopy suites with EBUS‐TBNA, facilities for mediastinoscopy, CT‐guided FNAC, thoracoscopy, and surgery. | Referrals from specialty clinics (59.4%), primary care (20.2%), and local emergency rooms (20.4%). | Cough, dyspnea, hemoptysis, weight loss, imaging evidence of lung masses. | 678 | 4 years | Specialized outpatient noninvasive and invasive workup. |
| Franco‐Hidalgo et al., 2012 | Prospective descriptive study on 167 patients, evaluated by an RDU in a tertiary care hospital in Palencia, Spain between November 2008 and April 2009. Care preferences studied with random surveys. | An RDU run by an internist and nursing staff with administrative support. Has a consulting room and a waiting room. | Referrals from primary care (70.7%), emergency room (21.6%), specialty clinics (7.8%). | Abdominal masses and visceromegalies, chronic diarrhea, dysphagia, ascites, icterus, transaminitis, heart failure, abnormal chest imaging, suspicion of pulmonary TB, or neoplasia, | 167 | 6 months | Early scheduling and urgent specialized workup. |
Outcomes
The most common final diagnosis was malignancy in 18% to 30% of the cases[6, 7, 8, 10] and in 55% of the lung cancer RDU cases[9] (Table 3). The time from initial contact to final diagnosis ranged from 6 to 11 days. Only 3% to 10% of the patients were admitted to the hospital from the QDUs; most patients were discharged to specialty‐care clinics or to primary care centers. Capell et al.[7] estimated that such a unit could save 7 inpatient bed‐days per patient, whereas Rubio‐Rivas et al.[8] estimated that value to be 4.5 bed‐days per patient. Bosch et al.[6] calculated that they saved 8.76 bed‐days per patient.
| Author | Final Diagnosis | Time to Diagnosis | Final Disposition | Benefit Analysis | Care Preference Survey | Duration | Intervention |
|---|---|---|---|---|---|---|---|
| |||||||
| Bosch et al., 2012 | Malignancy (30%), IDA (19%), other benign GI disorders (12%), others (39%). | Mean=8.9 days (cases) (3.13 QDU visits) | Hospital for admission: 3%, primary health centers: 62%, outpatient follow‐up: 35%. | Estimated hospital days saved: mean length of stay 8.76 days. Average cost saved per process (admission to discharge): 2,514.64. | 88% preferred QDU care model over hospital stay. | 4 years | Outpatient workup with urgent first visit, preferential scheduling of diagnostic tests, and follow‐up until diagnosis is made. |
| Capell et al., 2004 | Malignancy (15%), GI disorders (24%), neurological disorders (14%). | Mean=5.7 days | Hospital for admission: 7%, primary care: 51%, outpatient hospital follow‐up: 38%,specialty clinics: 4%. | Estimated 7 inpatient bed/days per year during the period of study. Cost saved per encounter: 1,764. | 95% reported high satisfaction with QEDU. | 5 years | Prioritized scheduling and urgent workup. |
| Rubio‐Rivas et al., 2008 | Malignancy (18%). | Mean=9 days | Hospital for admission: 10%, outpatient follow‐up: 56%, discharged from follow‐up: 38%. | Hospitalizations avoided: 4.5 bed/days over the study period. Cost analysis not available. | None | 11.5 years | Prioritized scheduling and urgent workup. |
| Sanz‐Santos et al., 2010 | Lung cancer (55%). | Mean=11 days | Not available. | No available data on cost analysis or hospitalizations avoided. | None | 4 years | Specialized outpatient noninvasive and invasive workup. |
| Franco‐Hidalgo et al., 2012 | Neoplastic (19%), nonmalignant digestive diseases (23%,), infection 13%, and rheumatic (11%). | Mean=8 days | Not available. | No available data on cost analysis or hospitalizations avoided. | 97% reported high/very high satisfaction with the UDR. | 6 months | Early scheduling and urgent specialized workup. |
Two studies included a cost comparison between a conventional inpatient evaluation and a QDU evaluation. Bosch et al.[6] and Capell et al.[7] found an average saving of $3304 (2514) and $2353 (1764) per patient, respectively. Bosch et al.[6] calculated these savings by comparing QDU patients to randomly selected control patients with similar referring complaints, who had reached their final diagnosis during a conventional inpatient evaluation. Capell et al.[7] compared their QDU patient costs to estimated in‐hospital costs for similar diagnoses.
Safety data were reported in detail only by Bosch et al.[6] who showed that 125 (3%) patients who initially were stable for QDU evaluation were referred to the emergency department. A total of 15 patients required admission and 12 died, with an overall mortality for the QDU cohort of 0.3%. Causes of death in this group included sudden unexplained death in 8 patients, pulmonary embolism in 2, aspiration pneumonia in 1, and shock of unknown origin in 1. Capell et al.[7] described a 7% admission rate, and Rubio‐Rivas et al.[8] noted that number to be 10%. No mortality was reported in these 2 studies.
In terms of preference for care, an overwhelming majority (88%) of patients in 1 study[6] preferred the QDU care model over hospitalization, and 95% to 97% of patients in 2 other studies[7, 10] reported very high satisfaction rates.
DISCUSSION
Our systematic review evaluated the effectiveness of QDUs for the diagnostic evaluation of patients with potentially severe disease and showed that such units, where established, are cost‐effective, prevent unnecessary hospitalizations, and diagnose potentially severe diseases, particularly malignant conditions, in a timely manner.
QDUs can evaluate medically stable patients with a variety of complaints such as anemia, lymphadenopathy, undiagnosed lumps and masses, and gastrointestinal symptoms and accelerate the diagnostic evaluation without requiring inpatient hospitalization. Many times patients are admitted to the hospital for a diagnostic evaluation without actual treatment.[12] These patients may not be sick enough to warrant hospitalization and may be able to return to the clinic for an outpatient workup. The QDU approach can complete the evaluation in such patients with the added advantages of saving money and higher patient satisfaction, due to diminished disruption of the patient's daily life.[1, 12] As most primary care physicians are unlikely to provide regular and frequent access for unscheduled care and EDs are more likely to admit patients for diagnostic workup,[2] a QDU approach seems a reasonable alternative for making a quick diagnosis and at the same time avoiding unnecessary hospitalization. Bosch et al. have also evaluated the impact of the QDUs in the diagnosis of specific diseases such as cancer in 169 patients diagnosed at the QDU, and compared them to 53 patients who were diagnosed with cancer during an inpatient evaluation.[11] They found that although QDU patients were significantly younger than hospitalized patients, there was no difference in diagnoses established and the time to diagnosis at the QDU and length of stay in the hospital.
There is a significant cost saving associated with QDUs. The cost savings calculated by Bosch et al. and Capell et al. were for each patient enrolled in this protocol from index encounter to final diagnosis.[6, 7] These 2 studies describe primarily fixed costs saved per patient treated in the QDU versus an inpatient admission. Fixed costs in hospital care include personnel cost, buildings, and equipment, whereas variable costs include medication, test reagents, and disposable supplies.[15] In comparison with the US healthcare system, fixed costs in Europe are considerably lower, and certain variable costs (like medications and procedures) are significantly higher in the United States.[16] This suggests a greater opportunity for healthcare savings for carefully selected patients in the United States, where costs related to inpatient admissions are significantly higher.[16]
Another limitation of our analysis is the paucity of studies on this topic. Many of the publications are from Bosch et al.,[1, 6, 11, 12, 13, 14] a single group in Spain, and these show considerable cost savings, patient satisfaction, and patient safety. However, most of their data are either retrospective or from nonrandomized, prospective cohort studies. The only report describing a similar approach in the United States was by Paschal in the city of New Orleans.[17] After Charity Hospital and the Veterans Affairs Hospital in New Orleans were lost to hurricane Katrina, an urgent care clinic was set up where potentially severe diseases such as cancer, leukemia, and autoimmune and endocrine disorders were diagnosed efficiently, although safety data were not reported.
The reported studies used different study designs and evaluated different primary outcomes. These limitations can be overcome with a well‐designed prospective trial, which could also evaluate the actual impact on patient care, safety, and healthcare savings in the United States.
Safety data were reported in detail only in 1 study,[6] and the rates of admissions were reported by 2 other studies.[7, 8] These suggest that QDUs may be safe for a selected group of patients. Patients evaluated in these units preferred this approach as shown by the overwhelming majority of the patients who chose QDU care over inpatient admissions when patient surveys were performed.
CONCLUSION
In this era of healthcare reform and emphasis on value‐based care, we must optimize the efficiency of our care delivery systems and challenge our preexisting resource‐intensive healthcare models. One source of potential savings is avoiding hospitalizations for purely diagnostic purposes, utilizing quick diagnostic units for patients who are able to return for outpatient evaluations. Such units are established, have been studied in Europe, and our systematic review shows that they are cost‐effective, time‐ and resource‐efficient, and preferred by patients. In our healthcare system, with the high cost of inpatient care, the QDU can yield large savings of healthcare dollars while expediting diagnostic workup, increasing patient satisfaction, and preventing lost productivity from hospital stays. Further exploration and study of alternative care delivery models, such as quick diagnostic units, is required to achieve the goal of cost‐effective high‐quality care for all.
Disclosure: Nothing to report.
Inpatient admissions are a major component of healthcare costs in the United States,[1] where the number of annual inpatient hospital admissions has increased by 15% from 34.3 million in 1993 to 39.5 million in 2006.2 Studies performed predominantly in Europe have shown that inappropriate use of hospital beds exceeds 20% across various specialties.[3] A study by Campbell et al. showed that if given the choice, 60% of physicians would consider an alternative to admission for such patients, if such an option were available, and 70% of patients would prefer not to be admitted for workup.[4] Based on similar findings, various hospitals across the world have tried to make organizational changes to allocate healthcare resources more efficiently. The concept of quick and early diagnosis was first introduced in 1996 by Kendall et al., and it included a hospital unit in the United Kingdom managed by consultants receiving referrals from primary care doctors and led to early diagnostic workup without hospitalization.[5] A more refined version of this concept, a potentially cost‐saving and efficient alternative to inpatient hospitalization for diagnostic purposes, was described by Bosch et al., and named the quick diagnosis unit (QDU).[1]
The basic objectives of QDUs include early diagnosis of potentially severe diseases such as cancer, avoiding unnecessary hospitalization, minimizing hospital morbidity, reducing costs, and improving patient satisfaction. The first described QDU was managed by internists, where patients with specific symptoms such as undiagnosed lumps or masses, anemia, hematuria, or gastrointestinal symptoms could be referred for a diagnostic evaluation. Patients were required to be well enough to travel to the QDU on an outpatient basis, and patients unable to do so were thought to be better suited for hospitalization.[1]
In the present study, we conduct a systematic review, the first one on this subject to our knowledge, of studies that tested established QDUs or similar units in hospital settings. The majority of established units were tested and exist in Europe.[1, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14] They have been studied in Spain, from where much of these data have been obtained.[1]
METHODS
Study Selection
We searched MEDLINE (January 1946 to November 2012) via OVID and EMBASE (January 1974 to November 2012) via SCOPUS using keywords and Medical Subject Heading terms for quick diagnosis units and rapid diagnosis units. The detailed search strategy can be found in Table 1. A screening of titles and abstracts was done by 2 independent reviewers and followed by full‐text screening. We screened for additional articles by reviewing the bibliography of the articles selected for full‐text screening. We included in our review all studies that (1) were published in any language, (2) focused on the design and implementation of a quick diagnosis unit or a rapid diagnosis unit in a hospital setting, and (3) included at least 2 of the primary outcomes, as described below.
| No. | Searches |
|---|---|
| 1 | Quick diagnosis units.mp. |
| 2 | Quick diagnosis unit.mp. |
| 3 | (Quick adj diagnosis adj units).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 4 | (Quick adj diagnosis adj unit).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 5 | (Quick adj diagnosis).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 6 | (Diagnosis adj unit).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 7 | (Diagnosis adj units).mp [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 8 | Rapid diagnosis units.mp. |
| 9 | Rapid diagnosis unit.mp. |
| 10 | (Rapid adj diagnosis adj units).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 11 | (Rapid adj diagnosis adj unit).mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier] |
| 12 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 |
Outcome Measures
Our primary outcome measures were categories of final diagnosis, mean time to final diagnosis in an outpatient setting, inpatient bed‐days per patient saved, and costs saved per patient for QDUs versus in‐hospital stay. Secondary outcomes included disposition of patients after completion of this initial evaluation (whether admitted to the hospital or discharged to clinics) and the patients' care preferences, if available. For cost outcomes, currency exchange rates used for conversion were provided by Citibank National Bank Association, powered by Google online currency converter service (accessed June 16, 2013).
Data Extraction
We extracted data on the specifics of the early diagnostic unit setup including staffing and hours of operation, hospital setting, sources of referral, referring diagnosis, patient population, and the role of the diagnostic units in expediting workup and duration of study. For multiple studies done in the same institution by the same principal author, we used the study with the largest patient population to avoid duplication of data. The primary outcome measures for comparing costs were calculated by different methods and in different currencies by different investigators, which we have attempted to reconcile by using current currency conversion rates. We also evaluated patient preferences (if available) via patient surveys. The data were extracted by 2 independent reviewers, and disagreements were resolved by consensus.
RESULTS
Study Selection
Our literature search initially yielded 2047 publications, out of which 2034 were excluded after title and abstract screening. Thirteen studies were selected for full‐text review, out of which 5 were selected for detailed review based on our inclusion criteria (Figure 1). Three of the studies were in Spanish, and the results were analyzed with the help of a Spanish translator. The other 2 studies were in English.
Study Characteristics
Four studies that were included were descriptive longitudinal studies,[6, 7, 9, 10] and 1 was a retrospective study[8] (Table 2). There were a total of 8895 patients included in all of the studies. All of the studies except 1 described a similar organizational arrangement for the QDU, with 1 internist and 1 registered nurse, administrative support, and the ability to expedite the scheduling of diagnostic tests. The exception was a dedicated lung cancer rapid diagnostic unit (RDU) set up by Sanz‐Santos et al.[9] The study durations ranged from 6 months to 5 years. Patients were referred from local emergency rooms, primary care clinics, and specialty care clinics. The most common reasons for referral were anemia, adenopathy, visceromegaly, febrile syndromes, and incidentally detected masses or nodules on imaging. Two studies included some form of cost analysis,[6, 7] and 3 included patient surveys on satisfaction with patient care.[6, 7, 10]
| Author | Methods | Setup of Rapid Diagnosis Units | Sources of Referrals to the Unit | Reasons for Referrals to the Unit | Cases | Duration | Intervention |
|---|---|---|---|---|---|---|---|
| |||||||
| Bosch et al., 2012 | Prospective descriptive study in 4,170 patients evaluated by a dedicated QDU in a university hospital in Barcelona, Spain, between December 2007 to December 2009 and January 2010 to January 2012. QDU costs compared with costs for randomly selected, retrospectively reviewed hospital admissions for similar diagnosis. Care preferences studied with random surveys. | Quick diagnostic unit consisting of an internist, and a registered nurse. Single consulting room with a family waiting room. Assisted by specialists from other specialties. | Local primary health center (40%), emergency room (56%), other sources (4%). | Anemia, anorexia‐cachexia syndrome, febrile syndrome, adenopathies, abdominal pain, chronic diarrhea, lung abnormalities. | 4,170 | 4 years | Outpatient workup with urgent first visit, preferential scheduling of diagnostic tests and follow‐up until diagnosis is made. |
| Capell et al., 2004 | Prospective descriptive study with retrospective controls in 2,748 patients evaluated by a QEDU in a university hospital in Barcelona, Spain, between September 1996 and 2001. QEDU costs compared with costs for randomly selected, retrospectively reviewed hospital admissions for similar diagnosis. Care preferences studied with random surveys. | UDR made up of an internist and a nurse, a consultation and waiting room. | Referrals from emergency rooms (64%), primary care (28.6%), specialty clinics (6.4%). | Abdominal pain (12%), focal neurological symptoms (11.5%), constitutional symptoms (11%), anemia (6%), abnormal chest radiology (5.8%), palpable tumors (5.3%), adenopathies (4.7%), rectal bleeding (4.6%), febrile syndrome (4.6%), hemoptysis (3.5%), others (30%). | 2,748 | 5 years | Preferential scheduling and urgent workup. |
| Rubio‐Rivas et al., 2008 | Retrospective, descriptive study for 1,132 patients evaluated by a dedicated RDU in a university hospital in Barcelona, Spain from October 2005 to March 2007. | RDU consisted of an internist, a radiologist, and a nurse. | Local primary health centers (71%), emergency rooms (26%), and others (3%). | FUO, adenopathies, visceromegalies, chronic diarrhea, rectal bleeding, dysphagia, jaundice, hypercalcemia. | 1,132 | 11.5 years | Prioritized scheduling and urgent workup. |
| Sanz‐Santos et al., 2010 | Prospective observational study in 678 patients referred to an LC RDU, at a tertiary care center in Barcelona, Spain from October 2005 to September 2009. | An LC‐RDU, with nursing staff, 3 pulmonologists, bronchoscopy suites with EBUS‐TBNA, facilities for mediastinoscopy, CT‐guided FNAC, thoracoscopy, and surgery. | Referrals from specialty clinics (59.4%), primary care (20.2%), and local emergency rooms (20.4%). | Cough, dyspnea, hemoptysis, weight loss, imaging evidence of lung masses. | 678 | 4 years | Specialized outpatient noninvasive and invasive workup. |
| Franco‐Hidalgo et al., 2012 | Prospective descriptive study on 167 patients, evaluated by an RDU in a tertiary care hospital in Palencia, Spain between November 2008 and April 2009. Care preferences studied with random surveys. | An RDU run by an internist and nursing staff with administrative support. Has a consulting room and a waiting room. | Referrals from primary care (70.7%), emergency room (21.6%), specialty clinics (7.8%). | Abdominal masses and visceromegalies, chronic diarrhea, dysphagia, ascites, icterus, transaminitis, heart failure, abnormal chest imaging, suspicion of pulmonary TB, or neoplasia, | 167 | 6 months | Early scheduling and urgent specialized workup. |
Outcomes
The most common final diagnosis was malignancy in 18% to 30% of the cases[6, 7, 8, 10] and in 55% of the lung cancer RDU cases[9] (Table 3). The time from initial contact to final diagnosis ranged from 6 to 11 days. Only 3% to 10% of the patients were admitted to the hospital from the QDUs; most patients were discharged to specialty‐care clinics or to primary care centers. Capell et al.[7] estimated that such a unit could save 7 inpatient bed‐days per patient, whereas Rubio‐Rivas et al.[8] estimated that value to be 4.5 bed‐days per patient. Bosch et al.[6] calculated that they saved 8.76 bed‐days per patient.
| Author | Final Diagnosis | Time to Diagnosis | Final Disposition | Benefit Analysis | Care Preference Survey | Duration | Intervention |
|---|---|---|---|---|---|---|---|
| |||||||
| Bosch et al., 2012 | Malignancy (30%), IDA (19%), other benign GI disorders (12%), others (39%). | Mean=8.9 days (cases) (3.13 QDU visits) | Hospital for admission: 3%, primary health centers: 62%, outpatient follow‐up: 35%. | Estimated hospital days saved: mean length of stay 8.76 days. Average cost saved per process (admission to discharge): 2,514.64. | 88% preferred QDU care model over hospital stay. | 4 years | Outpatient workup with urgent first visit, preferential scheduling of diagnostic tests, and follow‐up until diagnosis is made. |
| Capell et al., 2004 | Malignancy (15%), GI disorders (24%), neurological disorders (14%). | Mean=5.7 days | Hospital for admission: 7%, primary care: 51%, outpatient hospital follow‐up: 38%,specialty clinics: 4%. | Estimated 7 inpatient bed/days per year during the period of study. Cost saved per encounter: 1,764. | 95% reported high satisfaction with QEDU. | 5 years | Prioritized scheduling and urgent workup. |
| Rubio‐Rivas et al., 2008 | Malignancy (18%). | Mean=9 days | Hospital for admission: 10%, outpatient follow‐up: 56%, discharged from follow‐up: 38%. | Hospitalizations avoided: 4.5 bed/days over the study period. Cost analysis not available. | None | 11.5 years | Prioritized scheduling and urgent workup. |
| Sanz‐Santos et al., 2010 | Lung cancer (55%). | Mean=11 days | Not available. | No available data on cost analysis or hospitalizations avoided. | None | 4 years | Specialized outpatient noninvasive and invasive workup. |
| Franco‐Hidalgo et al., 2012 | Neoplastic (19%), nonmalignant digestive diseases (23%,), infection 13%, and rheumatic (11%). | Mean=8 days | Not available. | No available data on cost analysis or hospitalizations avoided. | 97% reported high/very high satisfaction with the UDR. | 6 months | Early scheduling and urgent specialized workup. |
Two studies included a cost comparison between a conventional inpatient evaluation and a QDU evaluation. Bosch et al.[6] and Capell et al.[7] found an average saving of $3304 (2514) and $2353 (1764) per patient, respectively. Bosch et al.[6] calculated these savings by comparing QDU patients to randomly selected control patients with similar referring complaints, who had reached their final diagnosis during a conventional inpatient evaluation. Capell et al.[7] compared their QDU patient costs to estimated in‐hospital costs for similar diagnoses.
Safety data were reported in detail only by Bosch et al.[6] who showed that 125 (3%) patients who initially were stable for QDU evaluation were referred to the emergency department. A total of 15 patients required admission and 12 died, with an overall mortality for the QDU cohort of 0.3%. Causes of death in this group included sudden unexplained death in 8 patients, pulmonary embolism in 2, aspiration pneumonia in 1, and shock of unknown origin in 1. Capell et al.[7] described a 7% admission rate, and Rubio‐Rivas et al.[8] noted that number to be 10%. No mortality was reported in these 2 studies.
In terms of preference for care, an overwhelming majority (88%) of patients in 1 study[6] preferred the QDU care model over hospitalization, and 95% to 97% of patients in 2 other studies[7, 10] reported very high satisfaction rates.
DISCUSSION
Our systematic review evaluated the effectiveness of QDUs for the diagnostic evaluation of patients with potentially severe disease and showed that such units, where established, are cost‐effective, prevent unnecessary hospitalizations, and diagnose potentially severe diseases, particularly malignant conditions, in a timely manner.
QDUs can evaluate medically stable patients with a variety of complaints such as anemia, lymphadenopathy, undiagnosed lumps and masses, and gastrointestinal symptoms and accelerate the diagnostic evaluation without requiring inpatient hospitalization. Many times patients are admitted to the hospital for a diagnostic evaluation without actual treatment.[12] These patients may not be sick enough to warrant hospitalization and may be able to return to the clinic for an outpatient workup. The QDU approach can complete the evaluation in such patients with the added advantages of saving money and higher patient satisfaction, due to diminished disruption of the patient's daily life.[1, 12] As most primary care physicians are unlikely to provide regular and frequent access for unscheduled care and EDs are more likely to admit patients for diagnostic workup,[2] a QDU approach seems a reasonable alternative for making a quick diagnosis and at the same time avoiding unnecessary hospitalization. Bosch et al. have also evaluated the impact of the QDUs in the diagnosis of specific diseases such as cancer in 169 patients diagnosed at the QDU, and compared them to 53 patients who were diagnosed with cancer during an inpatient evaluation.[11] They found that although QDU patients were significantly younger than hospitalized patients, there was no difference in diagnoses established and the time to diagnosis at the QDU and length of stay in the hospital.
There is a significant cost saving associated with QDUs. The cost savings calculated by Bosch et al. and Capell et al. were for each patient enrolled in this protocol from index encounter to final diagnosis.[6, 7] These 2 studies describe primarily fixed costs saved per patient treated in the QDU versus an inpatient admission. Fixed costs in hospital care include personnel cost, buildings, and equipment, whereas variable costs include medication, test reagents, and disposable supplies.[15] In comparison with the US healthcare system, fixed costs in Europe are considerably lower, and certain variable costs (like medications and procedures) are significantly higher in the United States.[16] This suggests a greater opportunity for healthcare savings for carefully selected patients in the United States, where costs related to inpatient admissions are significantly higher.[16]
Another limitation of our analysis is the paucity of studies on this topic. Many of the publications are from Bosch et al.,[1, 6, 11, 12, 13, 14] a single group in Spain, and these show considerable cost savings, patient satisfaction, and patient safety. However, most of their data are either retrospective or from nonrandomized, prospective cohort studies. The only report describing a similar approach in the United States was by Paschal in the city of New Orleans.[17] After Charity Hospital and the Veterans Affairs Hospital in New Orleans were lost to hurricane Katrina, an urgent care clinic was set up where potentially severe diseases such as cancer, leukemia, and autoimmune and endocrine disorders were diagnosed efficiently, although safety data were not reported.
The reported studies used different study designs and evaluated different primary outcomes. These limitations can be overcome with a well‐designed prospective trial, which could also evaluate the actual impact on patient care, safety, and healthcare savings in the United States.
Safety data were reported in detail only in 1 study,[6] and the rates of admissions were reported by 2 other studies.[7, 8] These suggest that QDUs may be safe for a selected group of patients. Patients evaluated in these units preferred this approach as shown by the overwhelming majority of the patients who chose QDU care over inpatient admissions when patient surveys were performed.
CONCLUSION
In this era of healthcare reform and emphasis on value‐based care, we must optimize the efficiency of our care delivery systems and challenge our preexisting resource‐intensive healthcare models. One source of potential savings is avoiding hospitalizations for purely diagnostic purposes, utilizing quick diagnostic units for patients who are able to return for outpatient evaluations. Such units are established, have been studied in Europe, and our systematic review shows that they are cost‐effective, time‐ and resource‐efficient, and preferred by patients. In our healthcare system, with the high cost of inpatient care, the QDU can yield large savings of healthcare dollars while expediting diagnostic workup, increasing patient satisfaction, and preventing lost productivity from hospital stays. Further exploration and study of alternative care delivery models, such as quick diagnostic units, is required to achieve the goal of cost‐effective high‐quality care for all.
Disclosure: Nothing to report.
- , , , , . Quick diagnosis units: a potentially useful alternative to conventional hospitalization. Med J Aust. 2009;191:496–498.
- , . The growing role of emergency departments in hospital admissions. N Engl J Med. 2012;5:391–393.
- , , . Measuring appropriate use of acute beds. A Systematic review of methods and results. Health Policy. 2000;3:157–184.
- . Inappropriate admissions: thoughts of patients and referring doctors. J R Soc Med. 2001;12:628–631.
- , , . QED: quick and early diagnosis. Lancet. 1996;348:528–529.
- , , . Quick diagnosis units: avoiding referrals from primary care to the ED and hospitalizations. Am J Emerg Med. 2013;31(1):114–123.
- , , , et al. Quick and early diagnostic outpatient unit: an effective and efficient assistential model. Five years experience. Med Clin (Barc). 2004;123(7):247–250.
- , , , . Rapid diagnosis unit in a third level hospital. Descriptive study of the first year and a half. Rev Clin Esp. 2008;208(11):561–563.
- , , , et al. Usefulness of a lung cancer rapid diagnosis specialist clinic. Contribution of ultrasound bronchoscopy. Arch Bronconeumol. 2010;46(12):640–645.
- , , , . Rapid diagnosis units or immediate health care clinics in internal medicine. Analysis of the first six months of operation in Palencia (Spain). Semergen. 2012;38(2):126–130.
- , , , , . Comparison of quick diagnosis units and conventional hospitalization for the diagnosis of cancer in Spain: a descriptive cohort study. Oncology (Switzerland). 2012;83(5):283–291.
- , , , . Quick diagnosis units versus hospitalization for the diagnosis of potentially severe diseases in Spain. J Hosp Med. 2012;7(1):41–47.
- , , , , . Outpatient quick diagnosis units for the evaluation of suspected severe diseases: an observational study. Clinics. 2011;66(5):737–741.
- , , , et al. Quick diagnosis units or conventional hospitalization for the diagnostic evaluation of severe anemia: a paradigm shift in public health systems? Eur J Int Med. 2012;23(2):159–164.
- , , , et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999;281(7):644–649.
- . Explaining high healthcare spending in the united states: an international comparison of supply, utilization, prices and quality. Issue Brief (Commonw Fund). 2012;10:1–14.
- . Launching complex medical workups from an urgent care platform. Ann Int Med. 2012;156:232–233.
- , , , , . Quick diagnosis units: a potentially useful alternative to conventional hospitalization. Med J Aust. 2009;191:496–498.
- , . The growing role of emergency departments in hospital admissions. N Engl J Med. 2012;5:391–393.
- , , . Measuring appropriate use of acute beds. A Systematic review of methods and results. Health Policy. 2000;3:157–184.
- . Inappropriate admissions: thoughts of patients and referring doctors. J R Soc Med. 2001;12:628–631.
- , , . QED: quick and early diagnosis. Lancet. 1996;348:528–529.
- , , . Quick diagnosis units: avoiding referrals from primary care to the ED and hospitalizations. Am J Emerg Med. 2013;31(1):114–123.
- , , , et al. Quick and early diagnostic outpatient unit: an effective and efficient assistential model. Five years experience. Med Clin (Barc). 2004;123(7):247–250.
- , , , . Rapid diagnosis unit in a third level hospital. Descriptive study of the first year and a half. Rev Clin Esp. 2008;208(11):561–563.
- , , , et al. Usefulness of a lung cancer rapid diagnosis specialist clinic. Contribution of ultrasound bronchoscopy. Arch Bronconeumol. 2010;46(12):640–645.
- , , , . Rapid diagnosis units or immediate health care clinics in internal medicine. Analysis of the first six months of operation in Palencia (Spain). Semergen. 2012;38(2):126–130.
- , , , , . Comparison of quick diagnosis units and conventional hospitalization for the diagnosis of cancer in Spain: a descriptive cohort study. Oncology (Switzerland). 2012;83(5):283–291.
- , , , . Quick diagnosis units versus hospitalization for the diagnosis of potentially severe diseases in Spain. J Hosp Med. 2012;7(1):41–47.
- , , , , . Outpatient quick diagnosis units for the evaluation of suspected severe diseases: an observational study. Clinics. 2011;66(5):737–741.
- , , , et al. Quick diagnosis units or conventional hospitalization for the diagnostic evaluation of severe anemia: a paradigm shift in public health systems? Eur J Int Med. 2012;23(2):159–164.
- , , , et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999;281(7):644–649.
- . Explaining high healthcare spending in the united states: an international comparison of supply, utilization, prices and quality. Issue Brief (Commonw Fund). 2012;10:1–14.
- . Launching complex medical workups from an urgent care platform. Ann Int Med. 2012;156:232–233.