User login
Nail disorders and systemic disease: What the nails tell us
Can you name these 2 nail conditions?
What underlying diseases do you suspect are behind these conditions?
If you said onycholysis (left) and red lunula (right), you are correct. As for the underlying diseases: The patient with onycholysis has hyperthyroidism and the patient with red lunula has chronic obstructive pulmonary disease (COPD). Onycholysis and red lunula are among the more common changes to the morphology (shape) and color of the nail—the 2 ways by which nail changes are classified.
Nail abnormalities can be a revealing sign of underlying disease, and because the nails are readily examined, a convenient diagnostic tool, as well.
This review of common—and not so common—nail disorders shows which changes to the nail are more likely to occur with which underlying internal diseases.
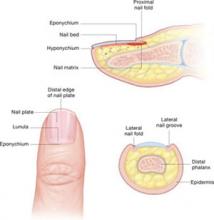
Nail anatomy
Nail changes are classified according to whether they occur in the morphology (shape) or color of the nail. Onycholysis, clubbing, and koilonychia are some of the most common changes in the morphology of the nail. Red lunula is one of the most common changes in the color of the nail.
- Amyloid and multiple myeloma
- Anemia
- Bronchiectasis
- Carcinoma (lung)
- Erythropoietic porphyria
- Histiocytosis X
- Ischemia (peripheral)
- Leprosy
- Lupus erythematosus
- Neuritis
- Pellagra
- Pemphigus vulgaris
- Pleural effusion
- Porphyria cutanea tarda
- Psoriatic arthritis
- Reiter’s syndrome
- Scleroderma
- Syphilis (secondary and tertiary)
- Thyroid disease
What you’ll see: Distal separation of the nail plate from the underlying nail bed. Nails with onycholysis are usually smooth, firm, and without nail bed inflammation. It is not a disease of the nail matrix, though nail discoloration may appear underneath the nail as a result of secondary infection.
What to suspect: Onycholysis is associated with many systemic conditions, including thyroid disease—especially hyperthyroidism. (See list at left.) The nail changes seen with hyperthyroidism usually consist of onycholysis beginning in the fourth or fifth nail, the so-called Plummer’s nails.1 Nakatsui and Lin2 have suggested that patients with unexplained onycholysis be screened for asymptomatic thyroid disease.
What you’ll see: Increased transverse and longitudinal nail curvature with fibrovascular hyperplasia of the soft tissue proximal to the cuticle. With clubbing, the Lovibond’s angle, formed between the dorsal surface of the distal phalanx and the nail plate, is greater than 180 degrees. Schamroth’s sign—the disappearance of the normal window between the back surfaces of opposite terminal phalanges—may also be present.3
What to suspect: Clubbing may be hereditary, idiopathic, or acquired in association with a variety of disorders. It may also be unilateral or bilateral. Unilateral clubbing has been associated with hemiplegia and vascular lesions, while bilateral clubbing has been linked to neoplastic, pulmonary, cardiac, gastrointestinal, infectious, endocrine, vascular, and multisystem diseases.
Cribier et al4 studied the frequency of nail disorders in HIV-infected patients and found that clubbing affects 5.8% of these patients. Moreover, Cribier’s data reinforced the notion that clubbing could be an early sign of AIDS in pediatric patients, and thus play a role in diagnosis.
What you’ll see: Concave thin nails with everted edges shaped like a spoon and capable of retaining a drop of water. It is more common in fingernails, but is occasionally seen in toenails.
What to suspect: This nail sign may result from trauma, constant exposure of hands to petroleum-based solvents, or nail-patella syndrome. Koilonychia is most commonly associated with iron deficiency anemia and occasionally occurs in patients with hemochromatosis. Other frequent systemic causes of koilonychia include coronary disease and hypothyroidism.5 In addition, koilonychia is sometimes a normal variant in infants; it usually disappears in the first few years of life.
What you’ll see: Proximal separation of the nail plate from the nail bed. This typically results in shedding of the nail.
What to suspect: Trauma is the usual cause. Less common causes include poor nutritional status, febrile illness, or drug sensitivity.
Wester et al6 observed the development of onychomadesis in a critically ill patient with a large pulmonary abscess. Onychomadesis is often a clinical manifestation of pemphigus vulgaris.7 It has also been associated with Kawasaki disease8 and hand, foot, and mouth disease.9
What you’ll see: Transverse depressions in the nail plate that occur as a result of a temporary cessation in nail growth.
What to suspect: The causes are similar to those of onychomadesis and include trauma, poor nutritional status, febrile illness, and drug sensitivity.
What you’ll see: Pinpoint (or larger) depressions in an otherwise normal nail.
What to suspect: Pitting is usually associated with psoriasis and affects 10% to 15% of patients with the disorder.10 Pitting has also been reported in patients with Reiter’s syndrome (and other connective tissue disorders), sarcoidosis, pemphigus, alopecia areata, and incontinentia pigmenti.5
What you’ll see: Transverse white bands parallel to the lunula. These bands usually occur in pairs and extend all the way across the nail.
This nail disorder is uncommon, and is 1 of 3 forms of leukonychia caused by abnormalities in nail bed vascularization. (The other 2 forms—Terry’s nails and half-and-half nails—are described on page 513.)
What to suspect: Muehrcke’s nails appear in patients with hypoalbuminemia and can improve if serum albumin levels return to normal. They may also occur in patients with:11,12
- nephrotic syndrome,
- glomerulonephritis,
- liver disease,
- malnutrition, and
- those who have undergone chemotherapy.
Muehrcke’s lines have also been described in a patient with Peutz-Jeghers syndrome,13 as well as in a heart transplant recipient.14
What you’ll see: Most of the nail plate is white, with a narrow pink distal band. All nails tend to be uniformly affected, with an appearance of ground glass.15 Terry’s nails have been found in 80% of patients with cirrhosis of the liver.15
What to suspect: One study found Terry’s nails in 25% of 512 consecutive hospital inpatients, with researchers linking the disorder with cirrhosis, chronic CHF, and adult-onset diabetes mellitus.16 On rare occasions, Terry’s nails have been reported in hemodialysis patients and renal transplant recipients.17 Terry’s nails have also been observed in HIV patients.4
Half-and-half nails (Lindsay’s nails)
What you’ll see: The proximal portion on the nail bed is white because of edema of the nail bed and capillary network; the distal portion is pink or reddish brown. The nail plate is unaffected.
What to suspect: This nail disorder has occurred in patients with renal disease associated with azotemia.18 Half-and-half nails have also been detected in hemodialysis patients, renal transplant recipients,17 and in HIV patients.4
What you’ll see: The lunula is red. In addition to the red lunula pictured here, there is also the absence of lunula and azure lunula.
What to suspect: Red lunula has been associated with alopecia areata, and collagen vascular disease. It has also occurred in patients on oral prednisone for rheumatoid arthritis. Red lunulae are seen in cardiac failure, COPD, cirrhosis, chronic urticaria, psoriasis, and carbon monoxide poisoning.19
Absence of lunula was the most common nail disorder in a group of hemodialysis patients (31.9%) and has also been reported in renal transplant recipients (17.1%).17 Azure lunula occurs in patients with Wilson disease. It has also occurred in argyria and in patients taking medications like 5-fluorouracil and azidothymidine.20
What you’ll see: Extravasations of blood from the longitudinally oriented vessels of the nail bed. These hemorrhages do not blanch. They form as a result of the nail plate-dermis structural relationship and tend to be seen in older patients.
What to suspect: While trauma is the most common cause, they may also occur with psoriasis and fungal infection.
Bacterial endocarditis is the most common systemic disease associated with splinter hemorrhages. These hemorrhages are more common in subacute, rather than acute, infection. Although splinter hemorrhages in subacute bacterial endocarditis have been described as proximally located,21 there are no sufficient data to confirm this—mainly because splinter lesions migrate distally as the nail grows.22
Splinter hemorrhages may also be associated with mitral stenosis, vasculitis, cirrhosis, trichinosis, scurvy, chronic glomerulonephritis, and Darier’s disease. However, due to the diverse and common causes of splinter hemorrhages, they cannot be used as an isolated sign of illness, except when they are accompanied by things like fever, Roth’s spots, Osler’s nodes, Janeway’s lesions, or a heart murmur, since any of the above would greatly increase their significance.
- Systemic disease typically affects more than 1 nail.5,23
- Fingernails usually provide more accurate information than toenails because clinical signs on toenails are often modified by trauma.23
- Fingernails grow at a rate of 0.1 mm/day and toenails grow at a rate of 0.03 mm/day.5,23 Thus, you can estimate the time at which an initial insult occurred by measuring the distance between the cuticle and the leading edge of any pigmentation change.
Correspondence
Dimitris Rigopoulos, assistant professor of dermatology, University of Athens Medical School, 5 Ionos Dragoumi Street, 16121 Athens, Greece; [email protected].
1. Jabbour SA. Cutaneous manifestations of endocrine disorders: a guide for dermatologists. Am J Clin Dermatol. 2003;4:315-331.
2. Nakatsui T, Lin AN. Onycholysis and thyroid disease: report of three cases. J Cutan Med Surg. 1998;3:40-42.
3. Spicknall KE, Zirwas MJ, English JC, III. Clubbing: an update on diagnosis, differential diagnosis, pathophysiology, and clinical relevance. J Am Acad Dermatol. 2005;52:1020-1028.
4. Cribier B, Mena ML, Rey D, et al. Nail changes in patients infected with human immunodeficiency virus. A prospective controlled study. Arch Dermatol. 1998;134:1216-1220.
5. Zaiac MN, Daniel CR, III. Nails in systemic disease. Dermatol Ther. 2002;5:99-106.
6. Wester JP, van Eps RS, Stouthamer A, Girbes AR. Critical illness onychomadesis. Intensive Care Med. 2000;26:1698-700.
7. Engineer L, Norton LA, Ahmed AR. Nail involvement in pemphigus vulgaris. J Am Acad Dermatol. 2000;43:529-535.
8. Ciastko AR. Onychomadesis and Kawasaki disease. CMAJ. 2002;166:1069.-
9. Clementz GC, Mancini AJ. Nail matrix arrest following hand-foot-mouth disease: a report of five children. Pediatr Dermatol. 2000;17(1):7-11.
10. Mayeaux EJ, Jr. Nail disorders. Prim Care. 2000;27:333-351.
11. Muehrcke RC. The fingernails in chronic hypoalbuminemia. BMJ. 1956;1:1327.-
12. D’Alessandro A, Muzi G, Monaco A, Filiberto S, Barboni A, Abbritti G. Yellow nail syndrome: does protein leakage play a role? Eur Respir J. 2001;87:5435-5441.
13. Skoog S, Boardman L. Muehrcke’s nails in Peutz-Jeghers syndrome with hepatic adenoma. Clin Gastroenterol Hepatol. 2004;2:XXIV.-
14. Nabai H. Nail changes before and after heart transplantation: personal observation by a physician. Cutis. 1998;61:31-32.
15. Dupont AS, Magy N, Humbert P, Dupond JL. Nail manifestations of systemic diseases. Rev Prat. 2000;50:2236-2240.
16. Holzberg M, Walker HK. Terry’s nails: revised definition and new correlations. Lancet. 1984;2:896.-
17. Saray Y, Seckin D, Gulec AT, Akgun S, Haberal M. Nail disorders in hemodialysis patients and renal transplant recipients: a case-control study. J Am Acad Dermatol. 2004;50:197-202.
18. Dyachenko P, Monselise A, Shustak A, et al. Nail disorders in patients with chronic renal failure and undergoing haemodialysis treatment: a case control study. J Eur Acad Dermatol Venereol. 2007;21:340-344.
19. Cohen PR. Red lunulae: case report and literature review. J AM Acad Dermatol. 1992;26:292.-
20. Tanner LS, Gross DJ. Generalized argyria. Cutis. 1990;45:237.-
21. Saccente M, Cobbs CG. Clinical approach to infective endocarditis. Cardio Clin. 1996;14:351-362.
22. Swartz MN, Weiburg AN. Infections due to gram-positive bacteria. In: Fitzpatrick TB, Elsen AZ, Wolff K, Freedberg IM, Austen KF, eds. Dermatology in General Medicine. 4th ed. New York: McGraw-Hill;1993:2309-2334.
23. Lawry M, Daniel CR. Nails in systemic disease. In: Scher RK, Daniel CR III, eds. Nails: Diagnosis, Therapy, Surgery. 3rd ed. Philadelphia: Elsevier Saunders; 2005:147-176.
Can you name these 2 nail conditions?
What underlying diseases do you suspect are behind these conditions?
If you said onycholysis (left) and red lunula (right), you are correct. As for the underlying diseases: The patient with onycholysis has hyperthyroidism and the patient with red lunula has chronic obstructive pulmonary disease (COPD). Onycholysis and red lunula are among the more common changes to the morphology (shape) and color of the nail—the 2 ways by which nail changes are classified.
Nail abnormalities can be a revealing sign of underlying disease, and because the nails are readily examined, a convenient diagnostic tool, as well.
This review of common—and not so common—nail disorders shows which changes to the nail are more likely to occur with which underlying internal diseases.
Nail anatomy
Nail changes are classified according to whether they occur in the morphology (shape) or color of the nail. Onycholysis, clubbing, and koilonychia are some of the most common changes in the morphology of the nail. Red lunula is one of the most common changes in the color of the nail.
- Amyloid and multiple myeloma
- Anemia
- Bronchiectasis
- Carcinoma (lung)
- Erythropoietic porphyria
- Histiocytosis X
- Ischemia (peripheral)
- Leprosy
- Lupus erythematosus
- Neuritis
- Pellagra
- Pemphigus vulgaris
- Pleural effusion
- Porphyria cutanea tarda
- Psoriatic arthritis
- Reiter’s syndrome
- Scleroderma
- Syphilis (secondary and tertiary)
- Thyroid disease
What you’ll see: Distal separation of the nail plate from the underlying nail bed. Nails with onycholysis are usually smooth, firm, and without nail bed inflammation. It is not a disease of the nail matrix, though nail discoloration may appear underneath the nail as a result of secondary infection.
What to suspect: Onycholysis is associated with many systemic conditions, including thyroid disease—especially hyperthyroidism. (See list at left.) The nail changes seen with hyperthyroidism usually consist of onycholysis beginning in the fourth or fifth nail, the so-called Plummer’s nails.1 Nakatsui and Lin2 have suggested that patients with unexplained onycholysis be screened for asymptomatic thyroid disease.
What you’ll see: Increased transverse and longitudinal nail curvature with fibrovascular hyperplasia of the soft tissue proximal to the cuticle. With clubbing, the Lovibond’s angle, formed between the dorsal surface of the distal phalanx and the nail plate, is greater than 180 degrees. Schamroth’s sign—the disappearance of the normal window between the back surfaces of opposite terminal phalanges—may also be present.3
What to suspect: Clubbing may be hereditary, idiopathic, or acquired in association with a variety of disorders. It may also be unilateral or bilateral. Unilateral clubbing has been associated with hemiplegia and vascular lesions, while bilateral clubbing has been linked to neoplastic, pulmonary, cardiac, gastrointestinal, infectious, endocrine, vascular, and multisystem diseases.
Cribier et al4 studied the frequency of nail disorders in HIV-infected patients and found that clubbing affects 5.8% of these patients. Moreover, Cribier’s data reinforced the notion that clubbing could be an early sign of AIDS in pediatric patients, and thus play a role in diagnosis.
What you’ll see: Concave thin nails with everted edges shaped like a spoon and capable of retaining a drop of water. It is more common in fingernails, but is occasionally seen in toenails.
What to suspect: This nail sign may result from trauma, constant exposure of hands to petroleum-based solvents, or nail-patella syndrome. Koilonychia is most commonly associated with iron deficiency anemia and occasionally occurs in patients with hemochromatosis. Other frequent systemic causes of koilonychia include coronary disease and hypothyroidism.5 In addition, koilonychia is sometimes a normal variant in infants; it usually disappears in the first few years of life.
What you’ll see: Proximal separation of the nail plate from the nail bed. This typically results in shedding of the nail.
What to suspect: Trauma is the usual cause. Less common causes include poor nutritional status, febrile illness, or drug sensitivity.
Wester et al6 observed the development of onychomadesis in a critically ill patient with a large pulmonary abscess. Onychomadesis is often a clinical manifestation of pemphigus vulgaris.7 It has also been associated with Kawasaki disease8 and hand, foot, and mouth disease.9
What you’ll see: Transverse depressions in the nail plate that occur as a result of a temporary cessation in nail growth.
What to suspect: The causes are similar to those of onychomadesis and include trauma, poor nutritional status, febrile illness, and drug sensitivity.
What you’ll see: Pinpoint (or larger) depressions in an otherwise normal nail.
What to suspect: Pitting is usually associated with psoriasis and affects 10% to 15% of patients with the disorder.10 Pitting has also been reported in patients with Reiter’s syndrome (and other connective tissue disorders), sarcoidosis, pemphigus, alopecia areata, and incontinentia pigmenti.5
What you’ll see: Transverse white bands parallel to the lunula. These bands usually occur in pairs and extend all the way across the nail.
This nail disorder is uncommon, and is 1 of 3 forms of leukonychia caused by abnormalities in nail bed vascularization. (The other 2 forms—Terry’s nails and half-and-half nails—are described on page 513.)
What to suspect: Muehrcke’s nails appear in patients with hypoalbuminemia and can improve if serum albumin levels return to normal. They may also occur in patients with:11,12
- nephrotic syndrome,
- glomerulonephritis,
- liver disease,
- malnutrition, and
- those who have undergone chemotherapy.
Muehrcke’s lines have also been described in a patient with Peutz-Jeghers syndrome,13 as well as in a heart transplant recipient.14
What you’ll see: Most of the nail plate is white, with a narrow pink distal band. All nails tend to be uniformly affected, with an appearance of ground glass.15 Terry’s nails have been found in 80% of patients with cirrhosis of the liver.15
What to suspect: One study found Terry’s nails in 25% of 512 consecutive hospital inpatients, with researchers linking the disorder with cirrhosis, chronic CHF, and adult-onset diabetes mellitus.16 On rare occasions, Terry’s nails have been reported in hemodialysis patients and renal transplant recipients.17 Terry’s nails have also been observed in HIV patients.4
Half-and-half nails (Lindsay’s nails)
What you’ll see: The proximal portion on the nail bed is white because of edema of the nail bed and capillary network; the distal portion is pink or reddish brown. The nail plate is unaffected.
What to suspect: This nail disorder has occurred in patients with renal disease associated with azotemia.18 Half-and-half nails have also been detected in hemodialysis patients, renal transplant recipients,17 and in HIV patients.4
What you’ll see: The lunula is red. In addition to the red lunula pictured here, there is also the absence of lunula and azure lunula.
What to suspect: Red lunula has been associated with alopecia areata, and collagen vascular disease. It has also occurred in patients on oral prednisone for rheumatoid arthritis. Red lunulae are seen in cardiac failure, COPD, cirrhosis, chronic urticaria, psoriasis, and carbon monoxide poisoning.19
Absence of lunula was the most common nail disorder in a group of hemodialysis patients (31.9%) and has also been reported in renal transplant recipients (17.1%).17 Azure lunula occurs in patients with Wilson disease. It has also occurred in argyria and in patients taking medications like 5-fluorouracil and azidothymidine.20
What you’ll see: Extravasations of blood from the longitudinally oriented vessels of the nail bed. These hemorrhages do not blanch. They form as a result of the nail plate-dermis structural relationship and tend to be seen in older patients.
What to suspect: While trauma is the most common cause, they may also occur with psoriasis and fungal infection.
Bacterial endocarditis is the most common systemic disease associated with splinter hemorrhages. These hemorrhages are more common in subacute, rather than acute, infection. Although splinter hemorrhages in subacute bacterial endocarditis have been described as proximally located,21 there are no sufficient data to confirm this—mainly because splinter lesions migrate distally as the nail grows.22
Splinter hemorrhages may also be associated with mitral stenosis, vasculitis, cirrhosis, trichinosis, scurvy, chronic glomerulonephritis, and Darier’s disease. However, due to the diverse and common causes of splinter hemorrhages, they cannot be used as an isolated sign of illness, except when they are accompanied by things like fever, Roth’s spots, Osler’s nodes, Janeway’s lesions, or a heart murmur, since any of the above would greatly increase their significance.
- Systemic disease typically affects more than 1 nail.5,23
- Fingernails usually provide more accurate information than toenails because clinical signs on toenails are often modified by trauma.23
- Fingernails grow at a rate of 0.1 mm/day and toenails grow at a rate of 0.03 mm/day.5,23 Thus, you can estimate the time at which an initial insult occurred by measuring the distance between the cuticle and the leading edge of any pigmentation change.
Correspondence
Dimitris Rigopoulos, assistant professor of dermatology, University of Athens Medical School, 5 Ionos Dragoumi Street, 16121 Athens, Greece; [email protected].
Can you name these 2 nail conditions?
What underlying diseases do you suspect are behind these conditions?
If you said onycholysis (left) and red lunula (right), you are correct. As for the underlying diseases: The patient with onycholysis has hyperthyroidism and the patient with red lunula has chronic obstructive pulmonary disease (COPD). Onycholysis and red lunula are among the more common changes to the morphology (shape) and color of the nail—the 2 ways by which nail changes are classified.
Nail abnormalities can be a revealing sign of underlying disease, and because the nails are readily examined, a convenient diagnostic tool, as well.
This review of common—and not so common—nail disorders shows which changes to the nail are more likely to occur with which underlying internal diseases.
Nail anatomy
Nail changes are classified according to whether they occur in the morphology (shape) or color of the nail. Onycholysis, clubbing, and koilonychia are some of the most common changes in the morphology of the nail. Red lunula is one of the most common changes in the color of the nail.
- Amyloid and multiple myeloma
- Anemia
- Bronchiectasis
- Carcinoma (lung)
- Erythropoietic porphyria
- Histiocytosis X
- Ischemia (peripheral)
- Leprosy
- Lupus erythematosus
- Neuritis
- Pellagra
- Pemphigus vulgaris
- Pleural effusion
- Porphyria cutanea tarda
- Psoriatic arthritis
- Reiter’s syndrome
- Scleroderma
- Syphilis (secondary and tertiary)
- Thyroid disease
What you’ll see: Distal separation of the nail plate from the underlying nail bed. Nails with onycholysis are usually smooth, firm, and without nail bed inflammation. It is not a disease of the nail matrix, though nail discoloration may appear underneath the nail as a result of secondary infection.
What to suspect: Onycholysis is associated with many systemic conditions, including thyroid disease—especially hyperthyroidism. (See list at left.) The nail changes seen with hyperthyroidism usually consist of onycholysis beginning in the fourth or fifth nail, the so-called Plummer’s nails.1 Nakatsui and Lin2 have suggested that patients with unexplained onycholysis be screened for asymptomatic thyroid disease.
What you’ll see: Increased transverse and longitudinal nail curvature with fibrovascular hyperplasia of the soft tissue proximal to the cuticle. With clubbing, the Lovibond’s angle, formed between the dorsal surface of the distal phalanx and the nail plate, is greater than 180 degrees. Schamroth’s sign—the disappearance of the normal window between the back surfaces of opposite terminal phalanges—may also be present.3
What to suspect: Clubbing may be hereditary, idiopathic, or acquired in association with a variety of disorders. It may also be unilateral or bilateral. Unilateral clubbing has been associated with hemiplegia and vascular lesions, while bilateral clubbing has been linked to neoplastic, pulmonary, cardiac, gastrointestinal, infectious, endocrine, vascular, and multisystem diseases.
Cribier et al4 studied the frequency of nail disorders in HIV-infected patients and found that clubbing affects 5.8% of these patients. Moreover, Cribier’s data reinforced the notion that clubbing could be an early sign of AIDS in pediatric patients, and thus play a role in diagnosis.
What you’ll see: Concave thin nails with everted edges shaped like a spoon and capable of retaining a drop of water. It is more common in fingernails, but is occasionally seen in toenails.
What to suspect: This nail sign may result from trauma, constant exposure of hands to petroleum-based solvents, or nail-patella syndrome. Koilonychia is most commonly associated with iron deficiency anemia and occasionally occurs in patients with hemochromatosis. Other frequent systemic causes of koilonychia include coronary disease and hypothyroidism.5 In addition, koilonychia is sometimes a normal variant in infants; it usually disappears in the first few years of life.
What you’ll see: Proximal separation of the nail plate from the nail bed. This typically results in shedding of the nail.
What to suspect: Trauma is the usual cause. Less common causes include poor nutritional status, febrile illness, or drug sensitivity.
Wester et al6 observed the development of onychomadesis in a critically ill patient with a large pulmonary abscess. Onychomadesis is often a clinical manifestation of pemphigus vulgaris.7 It has also been associated with Kawasaki disease8 and hand, foot, and mouth disease.9
What you’ll see: Transverse depressions in the nail plate that occur as a result of a temporary cessation in nail growth.
What to suspect: The causes are similar to those of onychomadesis and include trauma, poor nutritional status, febrile illness, and drug sensitivity.
What you’ll see: Pinpoint (or larger) depressions in an otherwise normal nail.
What to suspect: Pitting is usually associated with psoriasis and affects 10% to 15% of patients with the disorder.10 Pitting has also been reported in patients with Reiter’s syndrome (and other connective tissue disorders), sarcoidosis, pemphigus, alopecia areata, and incontinentia pigmenti.5
What you’ll see: Transverse white bands parallel to the lunula. These bands usually occur in pairs and extend all the way across the nail.
This nail disorder is uncommon, and is 1 of 3 forms of leukonychia caused by abnormalities in nail bed vascularization. (The other 2 forms—Terry’s nails and half-and-half nails—are described on page 513.)
What to suspect: Muehrcke’s nails appear in patients with hypoalbuminemia and can improve if serum albumin levels return to normal. They may also occur in patients with:11,12
- nephrotic syndrome,
- glomerulonephritis,
- liver disease,
- malnutrition, and
- those who have undergone chemotherapy.
Muehrcke’s lines have also been described in a patient with Peutz-Jeghers syndrome,13 as well as in a heart transplant recipient.14
What you’ll see: Most of the nail plate is white, with a narrow pink distal band. All nails tend to be uniformly affected, with an appearance of ground glass.15 Terry’s nails have been found in 80% of patients with cirrhosis of the liver.15
What to suspect: One study found Terry’s nails in 25% of 512 consecutive hospital inpatients, with researchers linking the disorder with cirrhosis, chronic CHF, and adult-onset diabetes mellitus.16 On rare occasions, Terry’s nails have been reported in hemodialysis patients and renal transplant recipients.17 Terry’s nails have also been observed in HIV patients.4
Half-and-half nails (Lindsay’s nails)
What you’ll see: The proximal portion on the nail bed is white because of edema of the nail bed and capillary network; the distal portion is pink or reddish brown. The nail plate is unaffected.
What to suspect: This nail disorder has occurred in patients with renal disease associated with azotemia.18 Half-and-half nails have also been detected in hemodialysis patients, renal transplant recipients,17 and in HIV patients.4
What you’ll see: The lunula is red. In addition to the red lunula pictured here, there is also the absence of lunula and azure lunula.
What to suspect: Red lunula has been associated with alopecia areata, and collagen vascular disease. It has also occurred in patients on oral prednisone for rheumatoid arthritis. Red lunulae are seen in cardiac failure, COPD, cirrhosis, chronic urticaria, psoriasis, and carbon monoxide poisoning.19
Absence of lunula was the most common nail disorder in a group of hemodialysis patients (31.9%) and has also been reported in renal transplant recipients (17.1%).17 Azure lunula occurs in patients with Wilson disease. It has also occurred in argyria and in patients taking medications like 5-fluorouracil and azidothymidine.20
What you’ll see: Extravasations of blood from the longitudinally oriented vessels of the nail bed. These hemorrhages do not blanch. They form as a result of the nail plate-dermis structural relationship and tend to be seen in older patients.
What to suspect: While trauma is the most common cause, they may also occur with psoriasis and fungal infection.
Bacterial endocarditis is the most common systemic disease associated with splinter hemorrhages. These hemorrhages are more common in subacute, rather than acute, infection. Although splinter hemorrhages in subacute bacterial endocarditis have been described as proximally located,21 there are no sufficient data to confirm this—mainly because splinter lesions migrate distally as the nail grows.22
Splinter hemorrhages may also be associated with mitral stenosis, vasculitis, cirrhosis, trichinosis, scurvy, chronic glomerulonephritis, and Darier’s disease. However, due to the diverse and common causes of splinter hemorrhages, they cannot be used as an isolated sign of illness, except when they are accompanied by things like fever, Roth’s spots, Osler’s nodes, Janeway’s lesions, or a heart murmur, since any of the above would greatly increase their significance.
- Systemic disease typically affects more than 1 nail.5,23
- Fingernails usually provide more accurate information than toenails because clinical signs on toenails are often modified by trauma.23
- Fingernails grow at a rate of 0.1 mm/day and toenails grow at a rate of 0.03 mm/day.5,23 Thus, you can estimate the time at which an initial insult occurred by measuring the distance between the cuticle and the leading edge of any pigmentation change.
Correspondence
Dimitris Rigopoulos, assistant professor of dermatology, University of Athens Medical School, 5 Ionos Dragoumi Street, 16121 Athens, Greece; [email protected].
1. Jabbour SA. Cutaneous manifestations of endocrine disorders: a guide for dermatologists. Am J Clin Dermatol. 2003;4:315-331.
2. Nakatsui T, Lin AN. Onycholysis and thyroid disease: report of three cases. J Cutan Med Surg. 1998;3:40-42.
3. Spicknall KE, Zirwas MJ, English JC, III. Clubbing: an update on diagnosis, differential diagnosis, pathophysiology, and clinical relevance. J Am Acad Dermatol. 2005;52:1020-1028.
4. Cribier B, Mena ML, Rey D, et al. Nail changes in patients infected with human immunodeficiency virus. A prospective controlled study. Arch Dermatol. 1998;134:1216-1220.
5. Zaiac MN, Daniel CR, III. Nails in systemic disease. Dermatol Ther. 2002;5:99-106.
6. Wester JP, van Eps RS, Stouthamer A, Girbes AR. Critical illness onychomadesis. Intensive Care Med. 2000;26:1698-700.
7. Engineer L, Norton LA, Ahmed AR. Nail involvement in pemphigus vulgaris. J Am Acad Dermatol. 2000;43:529-535.
8. Ciastko AR. Onychomadesis and Kawasaki disease. CMAJ. 2002;166:1069.-
9. Clementz GC, Mancini AJ. Nail matrix arrest following hand-foot-mouth disease: a report of five children. Pediatr Dermatol. 2000;17(1):7-11.
10. Mayeaux EJ, Jr. Nail disorders. Prim Care. 2000;27:333-351.
11. Muehrcke RC. The fingernails in chronic hypoalbuminemia. BMJ. 1956;1:1327.-
12. D’Alessandro A, Muzi G, Monaco A, Filiberto S, Barboni A, Abbritti G. Yellow nail syndrome: does protein leakage play a role? Eur Respir J. 2001;87:5435-5441.
13. Skoog S, Boardman L. Muehrcke’s nails in Peutz-Jeghers syndrome with hepatic adenoma. Clin Gastroenterol Hepatol. 2004;2:XXIV.-
14. Nabai H. Nail changes before and after heart transplantation: personal observation by a physician. Cutis. 1998;61:31-32.
15. Dupont AS, Magy N, Humbert P, Dupond JL. Nail manifestations of systemic diseases. Rev Prat. 2000;50:2236-2240.
16. Holzberg M, Walker HK. Terry’s nails: revised definition and new correlations. Lancet. 1984;2:896.-
17. Saray Y, Seckin D, Gulec AT, Akgun S, Haberal M. Nail disorders in hemodialysis patients and renal transplant recipients: a case-control study. J Am Acad Dermatol. 2004;50:197-202.
18. Dyachenko P, Monselise A, Shustak A, et al. Nail disorders in patients with chronic renal failure and undergoing haemodialysis treatment: a case control study. J Eur Acad Dermatol Venereol. 2007;21:340-344.
19. Cohen PR. Red lunulae: case report and literature review. J AM Acad Dermatol. 1992;26:292.-
20. Tanner LS, Gross DJ. Generalized argyria. Cutis. 1990;45:237.-
21. Saccente M, Cobbs CG. Clinical approach to infective endocarditis. Cardio Clin. 1996;14:351-362.
22. Swartz MN, Weiburg AN. Infections due to gram-positive bacteria. In: Fitzpatrick TB, Elsen AZ, Wolff K, Freedberg IM, Austen KF, eds. Dermatology in General Medicine. 4th ed. New York: McGraw-Hill;1993:2309-2334.
23. Lawry M, Daniel CR. Nails in systemic disease. In: Scher RK, Daniel CR III, eds. Nails: Diagnosis, Therapy, Surgery. 3rd ed. Philadelphia: Elsevier Saunders; 2005:147-176.
1. Jabbour SA. Cutaneous manifestations of endocrine disorders: a guide for dermatologists. Am J Clin Dermatol. 2003;4:315-331.
2. Nakatsui T, Lin AN. Onycholysis and thyroid disease: report of three cases. J Cutan Med Surg. 1998;3:40-42.
3. Spicknall KE, Zirwas MJ, English JC, III. Clubbing: an update on diagnosis, differential diagnosis, pathophysiology, and clinical relevance. J Am Acad Dermatol. 2005;52:1020-1028.
4. Cribier B, Mena ML, Rey D, et al. Nail changes in patients infected with human immunodeficiency virus. A prospective controlled study. Arch Dermatol. 1998;134:1216-1220.
5. Zaiac MN, Daniel CR, III. Nails in systemic disease. Dermatol Ther. 2002;5:99-106.
6. Wester JP, van Eps RS, Stouthamer A, Girbes AR. Critical illness onychomadesis. Intensive Care Med. 2000;26:1698-700.
7. Engineer L, Norton LA, Ahmed AR. Nail involvement in pemphigus vulgaris. J Am Acad Dermatol. 2000;43:529-535.
8. Ciastko AR. Onychomadesis and Kawasaki disease. CMAJ. 2002;166:1069.-
9. Clementz GC, Mancini AJ. Nail matrix arrest following hand-foot-mouth disease: a report of five children. Pediatr Dermatol. 2000;17(1):7-11.
10. Mayeaux EJ, Jr. Nail disorders. Prim Care. 2000;27:333-351.
11. Muehrcke RC. The fingernails in chronic hypoalbuminemia. BMJ. 1956;1:1327.-
12. D’Alessandro A, Muzi G, Monaco A, Filiberto S, Barboni A, Abbritti G. Yellow nail syndrome: does protein leakage play a role? Eur Respir J. 2001;87:5435-5441.
13. Skoog S, Boardman L. Muehrcke’s nails in Peutz-Jeghers syndrome with hepatic adenoma. Clin Gastroenterol Hepatol. 2004;2:XXIV.-
14. Nabai H. Nail changes before and after heart transplantation: personal observation by a physician. Cutis. 1998;61:31-32.
15. Dupont AS, Magy N, Humbert P, Dupond JL. Nail manifestations of systemic diseases. Rev Prat. 2000;50:2236-2240.
16. Holzberg M, Walker HK. Terry’s nails: revised definition and new correlations. Lancet. 1984;2:896.-
17. Saray Y, Seckin D, Gulec AT, Akgun S, Haberal M. Nail disorders in hemodialysis patients and renal transplant recipients: a case-control study. J Am Acad Dermatol. 2004;50:197-202.
18. Dyachenko P, Monselise A, Shustak A, et al. Nail disorders in patients with chronic renal failure and undergoing haemodialysis treatment: a case control study. J Eur Acad Dermatol Venereol. 2007;21:340-344.
19. Cohen PR. Red lunulae: case report and literature review. J AM Acad Dermatol. 1992;26:292.-
20. Tanner LS, Gross DJ. Generalized argyria. Cutis. 1990;45:237.-
21. Saccente M, Cobbs CG. Clinical approach to infective endocarditis. Cardio Clin. 1996;14:351-362.
22. Swartz MN, Weiburg AN. Infections due to gram-positive bacteria. In: Fitzpatrick TB, Elsen AZ, Wolff K, Freedberg IM, Austen KF, eds. Dermatology in General Medicine. 4th ed. New York: McGraw-Hill;1993:2309-2334.
23. Lawry M, Daniel CR. Nails in systemic disease. In: Scher RK, Daniel CR III, eds. Nails: Diagnosis, Therapy, Surgery. 3rd ed. Philadelphia: Elsevier Saunders; 2005:147-176.