User login
Male with Arthritis and Scaly Skin Rash
A 32‐year‐old male presented to the emergency department complaining of pain and swelling in the right knee and left hand, along with a skin rash on both feet. He denied any fever or recent history of travel. Symptoms started 1 week before presentation. Recent medical history was significant for Chlamydia trachomatis urethritis 10 weeks prior, which had been successfully treated.
Physical examination revealed right knee effusion, dactylitis manifested by both swelling of the digits of the left hand and finger‐tip ulcerations (Figure 1), as well as hyperkeratotic plaques with erythematous bases on the soles of both feet, consistent with keratoderma blenorrhagica (Figure 2). Furthermore, scaly erythematous lesions over the penis and the scrotum were recognized, indicating circinate balanitis (Figure 3).



Laboratory tests including human immunodeficiency virus (HIV) were unremarkable aside from an elevated sedimentation rate and positive human leukocyte antigen (HLA)‐B27.
The patient was diagnosed with reactive arthritis (Reiter's syndrome). A treatment regimen was initiated consisting of nonsteroidal antiinflammatory drugs (NSAIDs), prednisone, and sulfasalazine. Close outpatient follow‐up was established. Four months later, the patient remained debilitated by the disease, and etanercept was added resulting in significant improvement.
Reactive arthritis, also known as Reiter's syndrome, is an autoimmune disease that usually develops 2 to 4 weeks after a genitourinary or gastrointestinal infection. The classic triad of arthritis, urethritis, and conjunctivitis does not occur in all patients. Diagnosis is made by medical history and clinical findings. Numerous therapeutic modalities have been used with variable success, including short‐term antibiotics, NSAIDs, systemic corticosteroids, sulfasalazine, methotrexate, cyclosporine, etretinate, and tumor‐necrosis factor (TNF) inhibitors.
A 32‐year‐old male presented to the emergency department complaining of pain and swelling in the right knee and left hand, along with a skin rash on both feet. He denied any fever or recent history of travel. Symptoms started 1 week before presentation. Recent medical history was significant for Chlamydia trachomatis urethritis 10 weeks prior, which had been successfully treated.
Physical examination revealed right knee effusion, dactylitis manifested by both swelling of the digits of the left hand and finger‐tip ulcerations (Figure 1), as well as hyperkeratotic plaques with erythematous bases on the soles of both feet, consistent with keratoderma blenorrhagica (Figure 2). Furthermore, scaly erythematous lesions over the penis and the scrotum were recognized, indicating circinate balanitis (Figure 3).



Laboratory tests including human immunodeficiency virus (HIV) were unremarkable aside from an elevated sedimentation rate and positive human leukocyte antigen (HLA)‐B27.
The patient was diagnosed with reactive arthritis (Reiter's syndrome). A treatment regimen was initiated consisting of nonsteroidal antiinflammatory drugs (NSAIDs), prednisone, and sulfasalazine. Close outpatient follow‐up was established. Four months later, the patient remained debilitated by the disease, and etanercept was added resulting in significant improvement.
Reactive arthritis, also known as Reiter's syndrome, is an autoimmune disease that usually develops 2 to 4 weeks after a genitourinary or gastrointestinal infection. The classic triad of arthritis, urethritis, and conjunctivitis does not occur in all patients. Diagnosis is made by medical history and clinical findings. Numerous therapeutic modalities have been used with variable success, including short‐term antibiotics, NSAIDs, systemic corticosteroids, sulfasalazine, methotrexate, cyclosporine, etretinate, and tumor‐necrosis factor (TNF) inhibitors.
A 32‐year‐old male presented to the emergency department complaining of pain and swelling in the right knee and left hand, along with a skin rash on both feet. He denied any fever or recent history of travel. Symptoms started 1 week before presentation. Recent medical history was significant for Chlamydia trachomatis urethritis 10 weeks prior, which had been successfully treated.
Physical examination revealed right knee effusion, dactylitis manifested by both swelling of the digits of the left hand and finger‐tip ulcerations (Figure 1), as well as hyperkeratotic plaques with erythematous bases on the soles of both feet, consistent with keratoderma blenorrhagica (Figure 2). Furthermore, scaly erythematous lesions over the penis and the scrotum were recognized, indicating circinate balanitis (Figure 3).



Laboratory tests including human immunodeficiency virus (HIV) were unremarkable aside from an elevated sedimentation rate and positive human leukocyte antigen (HLA)‐B27.
The patient was diagnosed with reactive arthritis (Reiter's syndrome). A treatment regimen was initiated consisting of nonsteroidal antiinflammatory drugs (NSAIDs), prednisone, and sulfasalazine. Close outpatient follow‐up was established. Four months later, the patient remained debilitated by the disease, and etanercept was added resulting in significant improvement.
Reactive arthritis, also known as Reiter's syndrome, is an autoimmune disease that usually develops 2 to 4 weeks after a genitourinary or gastrointestinal infection. The classic triad of arthritis, urethritis, and conjunctivitis does not occur in all patients. Diagnosis is made by medical history and clinical findings. Numerous therapeutic modalities have been used with variable success, including short‐term antibiotics, NSAIDs, systemic corticosteroids, sulfasalazine, methotrexate, cyclosporine, etretinate, and tumor‐necrosis factor (TNF) inhibitors.
Soft‐tissue gangrene secondary to mixed cryoglobulinemia
A 61‐year‐old Hispanic male with chronic hepatitis C presented with a 4‐week history of a nonpruritic skin rash involving his lower extremities, hands, arms, and right ear. He also reported purple discoloration of his right foot, along with pain in the extremity that worsened with ambulation. Physical examination revealed diffuse purpura of both arms and legs (Figure 1). The right foot was cold to the touch and purple to black in color (Figure 2). There were multiple skin ulcers of various sizes covering the anterior aspect of his legs bilaterally. Pedal pulses were 2/4. Laboratory evaluation revealed positive cryoglobulins with low C4 and CH50 concentrations of 3 mg/dL (10‐40) and 2 units/mL (60‐144), respectively. Other immunological studies were negative. Lower extremity arterial Doppler studies were normal.


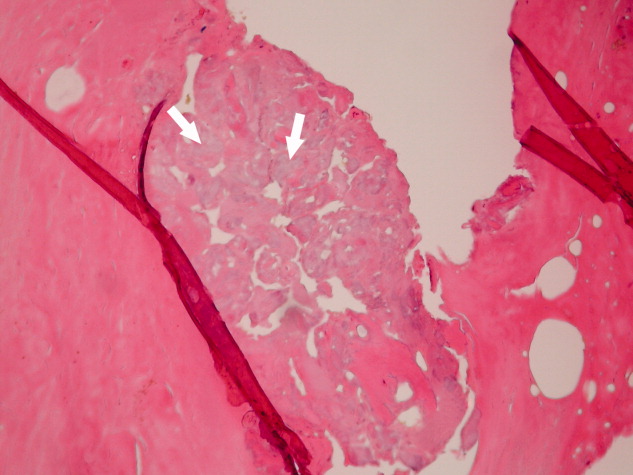
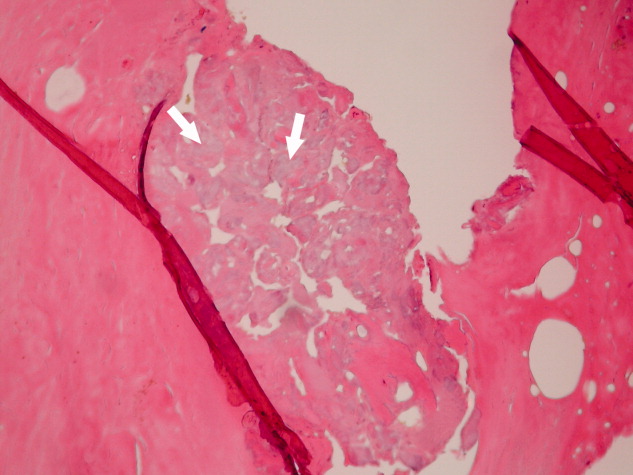
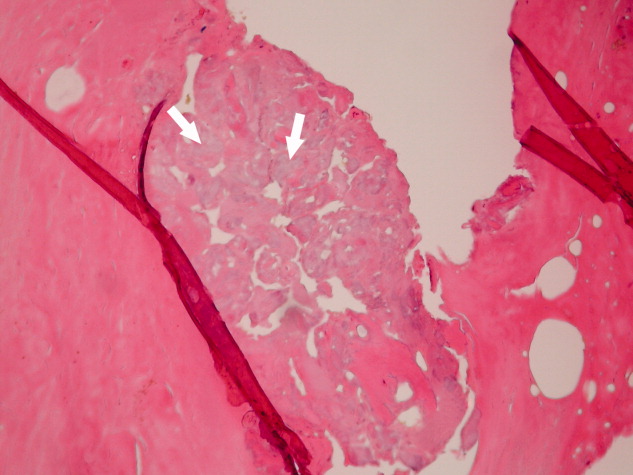
His clinical and laboratory findings were attributed to mixed cryoglobulinemia, and treatment, consisting of daily intravenous methylprednisolone, a single dose of intravenous cyclophosphamide, and plasmapheresis, was initiated. Despite these interventions, 5 days later, he developed severe burning pain in the right extremity with worsening discoloration and a line of demarcation at the level of his proximal midfoot. Eventually, right below the knee, amputation was performed, and histopathological examination showed soft‐tissue gangrene with avascular necrosis of the bone (Figure 3). The patient subsequently had an uneventful course. Plasmapheresis and oral prednisone were continued.
Cryoglobulinemia is a small‐ to medium‐vessel vasculitis due to cryoglobulin‐containing immune complexes. There are 3 types, with the classification based on an immunological analysis of the cryoglobulin composition. Hepatitis C virus infection is closely associated with type II mixed cryoglobulinemia. Cutaneous manifestations are the most common, consisting of palpable purpura, urticaria, postinflammatory hyperpigmentation, acrocyanosis, and skin ulcers. A serum cryoglobulin elevation is diagnostic and is usually accompanied by hypocomplementemia.
Treatment of the underlying disease is essential. However, aggressive therapy with plasmapheresis and immunosuppressive medications is warranted in severe cases involving limb‐ or organ‐threatening vasculitis.
A 61‐year‐old Hispanic male with chronic hepatitis C presented with a 4‐week history of a nonpruritic skin rash involving his lower extremities, hands, arms, and right ear. He also reported purple discoloration of his right foot, along with pain in the extremity that worsened with ambulation. Physical examination revealed diffuse purpura of both arms and legs (Figure 1). The right foot was cold to the touch and purple to black in color (Figure 2). There were multiple skin ulcers of various sizes covering the anterior aspect of his legs bilaterally. Pedal pulses were 2/4. Laboratory evaluation revealed positive cryoglobulins with low C4 and CH50 concentrations of 3 mg/dL (10‐40) and 2 units/mL (60‐144), respectively. Other immunological studies were negative. Lower extremity arterial Doppler studies were normal.


His clinical and laboratory findings were attributed to mixed cryoglobulinemia, and treatment, consisting of daily intravenous methylprednisolone, a single dose of intravenous cyclophosphamide, and plasmapheresis, was initiated. Despite these interventions, 5 days later, he developed severe burning pain in the right extremity with worsening discoloration and a line of demarcation at the level of his proximal midfoot. Eventually, right below the knee, amputation was performed, and histopathological examination showed soft‐tissue gangrene with avascular necrosis of the bone (Figure 3). The patient subsequently had an uneventful course. Plasmapheresis and oral prednisone were continued.
Cryoglobulinemia is a small‐ to medium‐vessel vasculitis due to cryoglobulin‐containing immune complexes. There are 3 types, with the classification based on an immunological analysis of the cryoglobulin composition. Hepatitis C virus infection is closely associated with type II mixed cryoglobulinemia. Cutaneous manifestations are the most common, consisting of palpable purpura, urticaria, postinflammatory hyperpigmentation, acrocyanosis, and skin ulcers. A serum cryoglobulin elevation is diagnostic and is usually accompanied by hypocomplementemia.
Treatment of the underlying disease is essential. However, aggressive therapy with plasmapheresis and immunosuppressive medications is warranted in severe cases involving limb‐ or organ‐threatening vasculitis.
A 61‐year‐old Hispanic male with chronic hepatitis C presented with a 4‐week history of a nonpruritic skin rash involving his lower extremities, hands, arms, and right ear. He also reported purple discoloration of his right foot, along with pain in the extremity that worsened with ambulation. Physical examination revealed diffuse purpura of both arms and legs (Figure 1). The right foot was cold to the touch and purple to black in color (Figure 2). There were multiple skin ulcers of various sizes covering the anterior aspect of his legs bilaterally. Pedal pulses were 2/4. Laboratory evaluation revealed positive cryoglobulins with low C4 and CH50 concentrations of 3 mg/dL (10‐40) and 2 units/mL (60‐144), respectively. Other immunological studies were negative. Lower extremity arterial Doppler studies were normal.


His clinical and laboratory findings were attributed to mixed cryoglobulinemia, and treatment, consisting of daily intravenous methylprednisolone, a single dose of intravenous cyclophosphamide, and plasmapheresis, was initiated. Despite these interventions, 5 days later, he developed severe burning pain in the right extremity with worsening discoloration and a line of demarcation at the level of his proximal midfoot. Eventually, right below the knee, amputation was performed, and histopathological examination showed soft‐tissue gangrene with avascular necrosis of the bone (Figure 3). The patient subsequently had an uneventful course. Plasmapheresis and oral prednisone were continued.
Cryoglobulinemia is a small‐ to medium‐vessel vasculitis due to cryoglobulin‐containing immune complexes. There are 3 types, with the classification based on an immunological analysis of the cryoglobulin composition. Hepatitis C virus infection is closely associated with type II mixed cryoglobulinemia. Cutaneous manifestations are the most common, consisting of palpable purpura, urticaria, postinflammatory hyperpigmentation, acrocyanosis, and skin ulcers. A serum cryoglobulin elevation is diagnostic and is usually accompanied by hypocomplementemia.
Treatment of the underlying disease is essential. However, aggressive therapy with plasmapheresis and immunosuppressive medications is warranted in severe cases involving limb‐ or organ‐threatening vasculitis.

