User login
A guide for clinicians: Bariatric surgery and the ObGyn patient
CASE: New-onset abdominal pain and a history of bariatric surgery
A 28-year-old woman who is 14 weeks pregnant (G5P1A4) complains of abdominal pain, nausea, and vomiting for the past 3 days. Four years ago, she underwent a successful Roux-en-Y gastric bypass, and her body mass index (BMI) decreased from 61.1 to 34.8 as a result. Today, after unremarkable ultrasonography at an outside hospital, she is transferred to your facility, where she is noted to be afebrile and tachycardic (133 bpm) with a very tender abdomen and a white blood cell (WBC) count of 12.2×103/μL.
Could her symptoms be related to her history of gastric bypass? How should you manage her condition?
This case illustrates why it is imperative that Ob Gyns have a basic understanding of bariatric surgery—particularly the types of procedures being performed today and the complications that may arise.
In this case, urgent intervention is called for, given the elevated WBC count and extreme tenderness of the abdomen. This patient was taken to surgery without waiting for additional imaging studies. Operative findings included intussusception with necrosis, a late complication of the Roux-en-Y procedure, necessitating resection of 60 cm of small intestine ( FIGURE 1 ). Although fetal heart sounds remained encouraging overnight, fetal demise occurred the next day. The patient’s physical recovery was otherwise unremarkable.
This scenario is not as unlikely as you might imagine. A similar episode was described in 2004.1 The outcome: maternal and fetal death.

FIGURE 1 Life-threatening intestinal obstruction
Patchy and continuous necrosis is evident following reduction of an obstruction-causing intussusception.
A boom in bariatric surgery
The incidence of surgical weight-loss procedures increased sixfold over a recent 7-year time span.2 In 2008 alone, more than 200,000 people underwent this type of operation—at least half of them women of reproductive age.2,3 In my experience at the University Hospitals of Cleveland Bariatric Program, which I directed, 85% of patients were women.4 This percentage is similar to the gender breakdown in other bariatric programs.
Because you are called on to provide both primary and specialty care, you are very likely to encounter women who have undergone bariatric surgery or who are considering it. As the prevalence of morbid obesity continues to rise, so will the need for familiarity with surgical weight-loss reduction.
In this article, I offer an overview of bariatric surgery, focusing on:
- the different procedures performed today
- the potential complications associated with the most common operations
- the need for nutritional assessment.
In the process, I discuss the health benefits of bariatric surgery, including greater fertility and improved pregnancy outcomes.
How we talk about obesity
The language of obesity centers on a basic metric: the body mass index (BMI).5 This index was devised in the 19th century by Adolphe Quetelet to describe total body fat.
Consider its use to describe two markedly overweight individuals. One stands 6 ft and weighs 500 lb; the other stands 5 ft and weighs 400 lb. It is obvious which person is heavier; the BMI quantifies who is actually bigger. The first individual has a BMI of 67.8, whereas the shorter person has a BMI of 78, despite weighing 100 lb less.
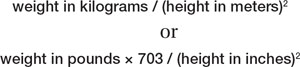
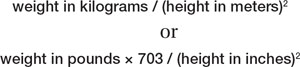
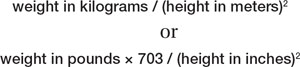
The formula for determining BMI is:
Among the imperfections of the BMI are its failure to differentiate between genders and its marked inaccuracy in persons who have significant muscle mass and limited body fat, such as body builders. However, it does make it possible to compare patients of different height and weight, thereby facilitating attempts to prognosticate the risk of illness and identify candidates for bariatric surgery ( TABLE 1 ).
The 1991 National Institutes of Health (NIH) Consensus Conference on Gastrointestinal Surgery for Severe Obesity recommended that bariatric surgery (restrictive and bypass procedures) be considered for patients who have a BMI of 40 or above and for patients who have a BMI of 35 or above with high-risk comorbidity.6
TABLE 1
How size is classified using the body mass index
| BMI | Classification | Risk of illness and comorbidity |
|---|---|---|
| <18.5 | Underweight | Increased |
| 18.5–24.9 | Normal | Average |
| 25–29.9 | Overweight | Increased |
| 30–34.9 | Obese (class I) | Moderate |
| 35–39.9 | Obese (class II) | Severe |
| ≥40 | Morbid obesity (class III) | Very severe |
| ≥50 | “Severe morbid obesity” | !!! Severe |
Most agree that bariatric surgery originated nearly 60 years ago with the jejunoileal bypass, a purely malabsorptive procedure in which the proximal jejunum was anastomosed to the distal ileum.7-9 This operation was based on the observation of dramatic weight loss following major small-bowel resection. The procedure was thought to allow obese patients to eat with abandon, thanks to the limited absorptive ability of the small intestine’s mucosal surface, which would impede digestion. However, the operation was fraught with complications, including protein calorie malnutrition, bacterial overgrowth, and even death. In addition, despite the dramatic reduction in the absorptive surface of the small intestine, some patients eventually regained weight.
One may still encounter patients who underwent jejunoileal bypass many years ago. One particular complication of this procedure is worth mentioning: hepatic cirrhosis. Any patient who has a history of jejunoileal bypass should have her liver function assessed before undergoing procedures that require general anesthesia.
At present, bariatric surgery may incorporate a component of malabsorption, but no other procedures are purely malabsorptive ( TABLE 2 ).
TABLE 2
Bariatric procedures for weight reduction, past and present
| Mechanism of action | Procedure |
|---|---|
| Malabsorptive | Jejunoileal bypass* |
| Restrictive | Vertical banded gastroplasty Gastric banding (Lap-Band) Laparoscopic sleeve gastrectomy Magenstrasse and Mill operation |
| Combination (malabsorptive and restrictive) | Roux-en-Y gastric bypass Biliopancreatic diversion Duodenal switch |
| Other | Gastric pacing† |
| * No longer performed | |
| †Experimental | |
Restrictive procedures
Vertical banded gastroplasty (VBG). This procedure is one of the earliest successful restrictive procedures ( FIGURE 2 ). Although it was originally performed via laparotomy, it is easily carried out laparoscopically. However, a risk of complication, such as severe reflux, and a low long-term success rate have decreased its widespread application.
Laparoscopic adjustable silicone band. The most common restrictive procedure performed today is the laparoscopic adjustable silicone band (Lap-Band) ( FIGURE 2 ). Among its benefits are:
- easy insertion, especially in comparison with the gastric bypass
- ability to adjust the amount of restriction (not possible with VBG)
- elimination of the need for supplemental nutrition
- reversibility.
Long-term results from a US population are not available because FDA approval did not occur until 2001. However, some centers outside the United States have reported unfavorable long-term outcomes. (See “Lap-Band complications may be pervasive,”.)
Laparoscopic sleeve gastrectomy (LSG). This operation was originally devised as the first stage of a duodenal switch. However, weight loss with this stage alone made LSG a bariatric procedure in its own right ( FIGURE 2 ).
Although this operation is categorized as restrictive, gastric sleeve resection eliminates the gastric fundus, the major site where ghrelin—“the hunger hormone”—is produced. This hormonal alteration may contribute to weight loss that occurs after LSG.
Magenstrasse and Mill operation. This operation converts the stomach into a long tube similar to the gastric sleeve. The greater curvature of the stomach is separated from the newly created tube but remains attached to the rest of the stomach at the antrum. (The greater curvature of the stomach is resected in the gastric sleeve procedure.)
Many insurers refuse to reimburse for restrictive operations other than the VBG and Lap-Band.

FIGURE 2 Three common surgeries
These restrictive procedures decrease the size of the stomach reservoir without impairing absorption of calories.
Combination procedures
Biliopancreatic diversion, duodenal switch. Despite the risk of protein malnutrition, these two procedures attempt to produce selective malabsorption of fat and carbohydrate as a means of treating the most severely obese patients. These operations carry the highest mortality rate and are therefore less likely to be offered routinely.
Roux-en-Y gastric bypass (RYGB). In the United States, the RYGB is performed more frequently than other procedures that combine malabsorption and restriction. It is considered by most to be the “gold standard” bariatric operation ( FIGURE 3 ).
The RYGB may induce weight loss through one or more of the following mechanisms:
- a decrease in the size of the gastric pouch. After the procedure, this pouch has a capacity of about 30 cc (size of a thumb)
- the small diameter of the gastrojejunal anastomosis, which is usually 1 cm
- glucose intolerance. About 50% of patients experience dumping symptoms when they ingest refined carbohydrates
- subclinical malabsorption. Food does not encounter the majority of digestive enzymes until it reaches the jejunojejunostomy anastomosis
- suppression of ghrelin production. Ghrelin is a hormone produced primarily in the gastric fundus and secondarily in the duodenum, both of which are bypassed with the RYGB. Plasma ghrelin levels peak before meals and are suppressed with food intake. After RYGB, patients demonstrate a flattening of this pattern, which appears to correlate with a suppression of appetite.10

FIGURE 3 Roux-en-Y gastric bypass
A gastric pouch is created at the top of the stomach and connected directly to the jejunum, bypassing the rest of the stomach and duodenum.
When is bariatric surgery indicated?
The NIH Consensus Conference identified patients who might be candidates for bariatric surgery, as I noted:
- patients who have a BMI of 40 or above, whether or not they have comorbidity
- patients who have a BMI of 35 or above and comorbidity.6
These recommendations have been adopted by third-party payers.
Potential comorbidities include hypertension, coronary artery disease (CAD), lipid abnormality, diabetes, obstructive sleep apnea (OSA), and severe osteoarthritis, among others.
When identified together, several of these comorbidities constitute metabolic syndrome, a risk factor for CAD. More than 50 million Americans are thought to exhibit this syndrome, which is diagnosed when three or more of the following are present:
- waist circumference ≥40 in (102 cm) in men; ≥35 in (88 cm) in women
- triglycerides ≥150 mg/dL
- high-density lipoprotein cholesterol <40 mg/dL in men; <50 mg/dL in women
- blood pressure ≥130/85 mm Hg
- fasting glucose ≥100 mg/dL.
Postsurgery weight loss has many benefits
Obstructive sleep apnea may resolve
Although this condition is known to be associated with obesity, it is drastically underdiagnosed.11 In our program, only 21% of patients had been given a diagnosis of OSA at the time of initial evaluation for surgery. After we obtained a polysomnogram (sleep study) for each of them, however, the true prevalence was determined to be 91%.
OSA can have serious consequences if it is untreated, and it may increase the risks associated with surgery and general anesthesia. By identifying and treating OSA before gastric bypass (RYGB), we were able to eliminate the respiratory ICU stay—a benefit that should be applicable to nonbariatric surgeries in the morbidly obese patient as well.12
With successful bariatric surgery, OSA abnormalities identified during polysomnography are dramatically improved or eliminated. Treatment with continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BIPAP) can usually be discontinued 6 months to 1 year after the dramatic weight loss associated with RYGB.
Cancer death rate may be reduced
Three consequences of morbid obesity not generally thought to be indications for bariatric surgery are:
- obesity-associated cancer
- decreased longevity
- infertility.
However, each of these conditions may be improved through successful bariatric surgery.
In a prospective study of more than 900,000 adults in the United States who were followed for 16 years, overweight or obesity was thought to account for 14% of cancer deaths in men and 20% of cancer deaths in women.13 Death rates for persons who had a BMI of at least 40 were 52% higher in men and 62% higher in women than they were in people who had a BMI below that threshold. BMI was significantly associated with cancer of the esophagus, colon and rectum, liver, gallbladder, pancreas, and kidney, as well as with non-Hodgkin’s lymphoma and multiple myeloma.
A trend toward an increasing risk of death with higher BMI was observed for cancer of the stomach (men), prostate, breast (women), uterus, ovary, and cervix.
The benefits of bariatric surgery in regard to cancer incidence and longevity were revealed in a 15-year, nonrandomized, prospective study involving more than 4,000 patients.14 At 10.9 years of follow-up, with a follow-up rate of 99.9%, this investigation concluded that bariatric surgery reduces mortality attributable to cardiovascular disease and cancer.14 Most surprising was the finding of a reduced incidence of cancer in patients who underwent bariatric surgery, compared with matched controls.14 An editorial accompanying this study summed it up in the headline: “The missing link—lose weight, live longer.”15
The Framingham risk score estimates the 10-year risk of CAD. This score is reduced by more than 50% after successful gastric bypass surgery.16
After surgery, fertility improves and pregnancy has better outcomes
From your practice, you’re certainly aware of the detrimental effects that obesity has on fertility, pregnancy, and fetal health.17-22 Although neither pregnancy nor impaired fertility is a primary indication for surgical weight reduction in an obese woman, bariatric surgery can improve the likelihood of fertility and successful pregnancy.
Advise patients to delay pregnancy after bariatric surgery. Although none of the bariatric operations performed today are contraindications to pregnancy, we caution all women to delay pregnancy—using two forms of birth control—until weight loss has stabilized. This usually takes about 12 to 18 months after surgery.
In our program, we identified 28 women who became pregnant following gastric bypass. Although we had cautioned all women to avoid early pregnancy, 10 became pregnant within 1 year of the bypass. Among these women, the rate of miscarriage was 40%, compared with 17% among the 18 women who waited more than 1 year to conceive. These percentages merit concern despite the small sample size.
Dao and colleagues concluded that the timing of pregnancy after gastric bypass is irrelevant.23 However, critical review of their data reveals an average weight gain of 4 lb in the group of women who became pregnant within a year after surgery (range, -70 to +45 lb), compared with 34 lb in the group that waited at least 1 year to conceive (range, +13 to +75 lb). As it was among our own patients, miscarriage was more common in the early group (24% vs 8% in the late group). Although these data are not statistically significant, they should arouse concern. I believe the most prudent advice to give women following bariatric surgery is to delay pregnancy until weight loss has stabilized.
The World Health Organization has estimated that there are 1 billion overweight adults on the planet. The problem of obesity, however, is concentrated in the United States. For well over a decade, the problem has escalated, with the US obesity rate referred to as “epidemic” and “a crisis”—among both adults and children.24
Among adults 20 years and older, the prevalence of obesity in the United States is 32%, and the prevalence of morbid obesity is almost 5%. Among adult women 20 to 39 years old, the prevalence of obesity and morbid obesity is 29% and 8%, respectively.27
Complications of bariatric surgery
Complications following bariatric surgery are intrinsic to the specific procedure performed. Because RYGB and the Lap-Band procedure constitute the overwhelming majority of bariatric operations, the most important complications associated with these surgeries will be addressed.
After RYGB, greatest risk is intestinal obstruction
Some of the early postoperative complications following RYGB are unlikely to be seen by physicians other than bariatric surgeons. They include anastomotic leaks, peritonitis, and bleeding. Pulmonary emboli should be managed as usual during the postoperative course. The amount of heparin necessary to achieve therapeutic anticoagulation may be quite substantial, but this fact should not deter the treating physician.
Nausea is almost universally present during the first few days after RYGB. When nausea and increasing food intolerance occur later (after the patient has demonstrated that food can be tolerated), it may indicate stenosis of the gastrojejunal anastomosis. The optimal study to evaluate these symptoms is a barium upper gastrointestinal (GI) swallow study. Stenosis can usually be managed by endoscopic dilatation.24
Intestinal obstruction. One of the most serious problems following RYGB is intestinal obstruction, which may be caused by internal hernia, adhesion, intussusception (not rare in the gastric bypass patient), and other less common causes ( FIGURE 1 ). Intestinal obstruction may occur early or years after the procedure.
In the RYGB patient, obstruction manifests with prominent pain, but distension and vomiting are usually absent, and plain abdominal radiographs are generally normal. The reason for this unusual presentation? The biliopancreatic limb tends to be the segment involved in the blockage, thereby creating a closed-loop obstruction. The most efficient way to diagnose this potentially life-threatening problem is by computed tomography (CT) ( FIGURE 4 ).
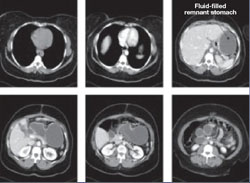
FIGURE 4 CT facilitates diagnosis of closed-loop obstruction
These computed tomography images reveal obstruction of the remnant stomach, duodenum, and proximal jejunum (the biliopancreatic limb) in a patient who has undergone Roux-en-Y gastric bypass.
Lap-Band complications may be pervasive
The Lap-Band procedure is often touted as having very low morbidity and mortality. However, data from outside the United States, where longer follow-up has been conducted, have cast a shadow of doubt on the supposed benefits of this restrictive procedure.
One study involving nearly 900 patients and 12 years of follow-up identified a rate of late complication of nearly 28% (2.3%, band erosion; 15.5%, pouch dilatation; 8.9%, port problems) and a rate of major reoperation of nearly 30%. The failure rate increased over time, reaching 65% at 10 years.
Despite these concerns, there is widespread enthusiasm among patients and bariatric surgeons who are proponents of this procedure.
A life-threatening complication. Any physician who might care for a patient who has undergone a Lap-Band procedure should be aware of one potentially life-threatening consequence: a slipped band. This complication can lead to incarceration of the stomach—usually the fundus—which, if left untreated, causes gastric infarction.
The main symptom of band slippage is pain. Any patient who has a Lap-Band and who reports significant upper abdominal pain must be evaluated to exclude slippage. Evaluation usually consists of a swallow study. Surgical correction is mandatory and urgent.
Like complications of surgery, the nutritional demands following bariatric surgery depend on the type of procedure that is performed.
After Lap-Band and other purely restrictive procedures,
nutritional levels remain stable
With restrictive procedures, such as the Lap-Band operation, the GI tract is essentially unaffected. Consequently, vitamin and micronutrient absorption remains intact. In these patients, we usually recommend a daily multivitamin. We assess serum levels to determine whether calcium and vitamin D supplementation might be necessary, which is especially important in female patients.
Close monitoring is needed after RYGB
After RYGB and other combined procedures, the question of nutritional supplementation becomes more complex.25 Bypass of the duodenum and upper jejunum affect absorption of iron, vitamin B12, calcium, and vitamin D. Serum calcium assessment is inadequate to determine the adequacy of calcium and vitamin D supplementation.
We evaluate parathyroid hormone and alkaline phosphatase levels in these patients. Any increase in these levels in the presence of normal serum calcium suggests the induction of secondary hyperparathyroidism and the need for additional calcium and vitamin D.26
Our recommendations for all patients following RYGB are a daily multivitamin, vitamin B12, and supplemental calcium and vitamin D. Vitamin B1 (thiamine) deficiency is extremely rare unless prolonged vomiting has been present. If B1 deficiency is suspected, administer thiamine before giving glucose because glucose can make symptoms worse.
Most women also need supplemental iron, which can be provided alone or in combination with the multivitamin, as in prenatal vitamins.
After RYGB, we measure vitamin and iron levels at 2 weeks, 3 months, 6 months, 12 months, 18 months, and then yearly thereafter unless a major abnormality is identified.
1. Moore KA, Ouyang DW, Whang EE. Maternal and fetal deaths after gastric bypass surgery for morbid obesity. N Engl J Med. 2004;351:721-722.
2. Bariatric Surgery in Women of Reproductive Age: Special Concerns for Pregnancy. Structured Abstract. Rockville, Md: Agency for Healthcare Research and Quality; November 2008. Available at: www.ahrq.gov/Clinic/tp/barireptp.htm. Accessed Dec. 8, 2009.
3. American Society for Metabolic and Bariatric Surgery. Metabolic and bariatric surgery fact sheet. Available at: www.asmbs.org/Newsite07/media/asmbs_fs_surgery.pdf. Accessed Dec. 8, 2009.
4. Stellato TA, Hallowell PT, Crouse C, Schuster M, Petrozzi MC. Two-day length of stay following open Roux-en-Y gastric bypass: is it feasible, safe and reasonable? Obes Surg. 2004;14:27-34.
5. Oria HE, Carrasquilla C, Cunningham P, et al. American Society for Bariatric Surgery Standards Committee, 2004–2005. Guidelines for weight calculations and follow-up in bariatric surgery. Surg Obes Relat Dis. 2005;1:67-68.
6. Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference Statement. Am J Clin Nutr. 1992;55(Suppl 2):615S-619S.
7. MacDonald KG, Jr. Overview of the epidemiology of obesity and the early history of procedures to remedy morbid obesity. Arch Surg. 2003;138:357-360.
8. Buchwald H. Overview of bariatric surgery. J Am Coll Surg. 2002;194:367-375.
9. DeMaria EJ. Bariatric surgery for morbid obesity. N Engl J Med. 2007;356:2176-2183.
10. Cummings DE, Weigle DS, Frayo RS, et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med. 2002;346:1623-1630.
11. Hallowell PT, Stellato TA, Schuster M, et al. Potentially life-threatening sleep apnea is unrecognized without aggressive evaluation. Am J Surg. 2007;193:364-367.
12. Hallowell PT, Stellato TA, Petrozzi MC, et al. Eliminating respiratory intensive care unit stay after gastric bypass surgery. Surgery. 2007;142:608-612.
13. Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625-1638.
14. Sjöström L, Narbro K, Sjöström CD, et al. Swedish Obese Subjects Study. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741-752.
15. Bray GA. The missing link—lose weight, live longer. N Engl J Med. 2007;357:818-820.
16. Kligman MD, Dexter DJ, Omer S, Park AE. Shrinking cardiovascular risk through bariatric surgery: application of Framingham risk score in gastric bypass. Surgery. 2008;143:533-538.
17. Linné Y. Effects of obesity on women’s reproduction and complications during pregnancy. Obes Rev. 2004;5:137-143.
18. Pasquali R, Pelusi C, Genghini S, Cacciari M, Gambineri A. Obesity and reproductive disorders in women. Hum Reprod Update. 2003;9:359-372.
19. Baeten JM, Bukusi EA, Lambe M. Pregnancy complications and outcomes among overweight and obese nulliparous women. Am J Public Health. 2001;91:436-440.
20. Lashen H, Fear K, Sturdee DW. Obesity is associated with increased risk of first trimester and recurrent miscarriage: matched case-control study. Hum Reprod. 2004;19:1644-1646.
21. Cnattingius S, Bergström R, Lipworth L, Kramer MS. Prepregnancy weight and the risk of adverse pregnancy outcomes. N Engl J Med. 1998;338:147-152.
22. Pathi A, Esen U, Hildreth A. A comparison of complications of pregnancy and delivery in morbidly obese and non-obese women. J Obstet Gynaecol. 2006;26:527-530.
23. Dao T, Kuhn J, Ehmer D, Fisher T, McCarty T. Pregnancy outcomes after gastric-bypass surgery. Am J Surg. 2006;192:762-766.
24. Stellato TA, Crouse C, Hallowell PT. Bariatric surgery: creating new challenges for the endoscopist. Gastrointest Endosc. 2003;57:86-94.
25. Poitou Bernert C, Ciangura C, Coupaye M, Czernichow S, Bouillot JL, Basdevant A. Nutritional deficiency after gastric bypass: diagnosis, prevention and treatment. Diabetes Metab. 2007;33:13-24.
26. Jin J, Robinson AV, Hallowell PT, Jasper JJ, Stellato TA, Wilhelm SM. Increases in parathyroid hormone (PTH) after gastric bypass surgery appear to be of a secondary nature. Surgery. 2007;142:914-920.
27. Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549-1555.
CASE: New-onset abdominal pain and a history of bariatric surgery
A 28-year-old woman who is 14 weeks pregnant (G5P1A4) complains of abdominal pain, nausea, and vomiting for the past 3 days. Four years ago, she underwent a successful Roux-en-Y gastric bypass, and her body mass index (BMI) decreased from 61.1 to 34.8 as a result. Today, after unremarkable ultrasonography at an outside hospital, she is transferred to your facility, where she is noted to be afebrile and tachycardic (133 bpm) with a very tender abdomen and a white blood cell (WBC) count of 12.2×103/μL.
Could her symptoms be related to her history of gastric bypass? How should you manage her condition?
This case illustrates why it is imperative that Ob Gyns have a basic understanding of bariatric surgery—particularly the types of procedures being performed today and the complications that may arise.
In this case, urgent intervention is called for, given the elevated WBC count and extreme tenderness of the abdomen. This patient was taken to surgery without waiting for additional imaging studies. Operative findings included intussusception with necrosis, a late complication of the Roux-en-Y procedure, necessitating resection of 60 cm of small intestine ( FIGURE 1 ). Although fetal heart sounds remained encouraging overnight, fetal demise occurred the next day. The patient’s physical recovery was otherwise unremarkable.
This scenario is not as unlikely as you might imagine. A similar episode was described in 2004.1 The outcome: maternal and fetal death.

FIGURE 1 Life-threatening intestinal obstruction
Patchy and continuous necrosis is evident following reduction of an obstruction-causing intussusception.
A boom in bariatric surgery
The incidence of surgical weight-loss procedures increased sixfold over a recent 7-year time span.2 In 2008 alone, more than 200,000 people underwent this type of operation—at least half of them women of reproductive age.2,3 In my experience at the University Hospitals of Cleveland Bariatric Program, which I directed, 85% of patients were women.4 This percentage is similar to the gender breakdown in other bariatric programs.
Because you are called on to provide both primary and specialty care, you are very likely to encounter women who have undergone bariatric surgery or who are considering it. As the prevalence of morbid obesity continues to rise, so will the need for familiarity with surgical weight-loss reduction.
In this article, I offer an overview of bariatric surgery, focusing on:
- the different procedures performed today
- the potential complications associated with the most common operations
- the need for nutritional assessment.
In the process, I discuss the health benefits of bariatric surgery, including greater fertility and improved pregnancy outcomes.
How we talk about obesity
The language of obesity centers on a basic metric: the body mass index (BMI).5 This index was devised in the 19th century by Adolphe Quetelet to describe total body fat.
Consider its use to describe two markedly overweight individuals. One stands 6 ft and weighs 500 lb; the other stands 5 ft and weighs 400 lb. It is obvious which person is heavier; the BMI quantifies who is actually bigger. The first individual has a BMI of 67.8, whereas the shorter person has a BMI of 78, despite weighing 100 lb less.
The formula for determining BMI is:
Among the imperfections of the BMI are its failure to differentiate between genders and its marked inaccuracy in persons who have significant muscle mass and limited body fat, such as body builders. However, it does make it possible to compare patients of different height and weight, thereby facilitating attempts to prognosticate the risk of illness and identify candidates for bariatric surgery ( TABLE 1 ).
The 1991 National Institutes of Health (NIH) Consensus Conference on Gastrointestinal Surgery for Severe Obesity recommended that bariatric surgery (restrictive and bypass procedures) be considered for patients who have a BMI of 40 or above and for patients who have a BMI of 35 or above with high-risk comorbidity.6
TABLE 1
How size is classified using the body mass index
| BMI | Classification | Risk of illness and comorbidity |
|---|---|---|
| <18.5 | Underweight | Increased |
| 18.5–24.9 | Normal | Average |
| 25–29.9 | Overweight | Increased |
| 30–34.9 | Obese (class I) | Moderate |
| 35–39.9 | Obese (class II) | Severe |
| ≥40 | Morbid obesity (class III) | Very severe |
| ≥50 | “Severe morbid obesity” | !!! Severe |
Most agree that bariatric surgery originated nearly 60 years ago with the jejunoileal bypass, a purely malabsorptive procedure in which the proximal jejunum was anastomosed to the distal ileum.7-9 This operation was based on the observation of dramatic weight loss following major small-bowel resection. The procedure was thought to allow obese patients to eat with abandon, thanks to the limited absorptive ability of the small intestine’s mucosal surface, which would impede digestion. However, the operation was fraught with complications, including protein calorie malnutrition, bacterial overgrowth, and even death. In addition, despite the dramatic reduction in the absorptive surface of the small intestine, some patients eventually regained weight.
One may still encounter patients who underwent jejunoileal bypass many years ago. One particular complication of this procedure is worth mentioning: hepatic cirrhosis. Any patient who has a history of jejunoileal bypass should have her liver function assessed before undergoing procedures that require general anesthesia.
At present, bariatric surgery may incorporate a component of malabsorption, but no other procedures are purely malabsorptive ( TABLE 2 ).
TABLE 2
Bariatric procedures for weight reduction, past and present
| Mechanism of action | Procedure |
|---|---|
| Malabsorptive | Jejunoileal bypass* |
| Restrictive | Vertical banded gastroplasty Gastric banding (Lap-Band) Laparoscopic sleeve gastrectomy Magenstrasse and Mill operation |
| Combination (malabsorptive and restrictive) | Roux-en-Y gastric bypass Biliopancreatic diversion Duodenal switch |
| Other | Gastric pacing† |
| * No longer performed | |
| †Experimental | |
Restrictive procedures
Vertical banded gastroplasty (VBG). This procedure is one of the earliest successful restrictive procedures ( FIGURE 2 ). Although it was originally performed via laparotomy, it is easily carried out laparoscopically. However, a risk of complication, such as severe reflux, and a low long-term success rate have decreased its widespread application.
Laparoscopic adjustable silicone band. The most common restrictive procedure performed today is the laparoscopic adjustable silicone band (Lap-Band) ( FIGURE 2 ). Among its benefits are:
- easy insertion, especially in comparison with the gastric bypass
- ability to adjust the amount of restriction (not possible with VBG)
- elimination of the need for supplemental nutrition
- reversibility.
Long-term results from a US population are not available because FDA approval did not occur until 2001. However, some centers outside the United States have reported unfavorable long-term outcomes. (See “Lap-Band complications may be pervasive,”.)
Laparoscopic sleeve gastrectomy (LSG). This operation was originally devised as the first stage of a duodenal switch. However, weight loss with this stage alone made LSG a bariatric procedure in its own right ( FIGURE 2 ).
Although this operation is categorized as restrictive, gastric sleeve resection eliminates the gastric fundus, the major site where ghrelin—“the hunger hormone”—is produced. This hormonal alteration may contribute to weight loss that occurs after LSG.
Magenstrasse and Mill operation. This operation converts the stomach into a long tube similar to the gastric sleeve. The greater curvature of the stomach is separated from the newly created tube but remains attached to the rest of the stomach at the antrum. (The greater curvature of the stomach is resected in the gastric sleeve procedure.)
Many insurers refuse to reimburse for restrictive operations other than the VBG and Lap-Band.

FIGURE 2 Three common surgeries
These restrictive procedures decrease the size of the stomach reservoir without impairing absorption of calories.
Combination procedures
Biliopancreatic diversion, duodenal switch. Despite the risk of protein malnutrition, these two procedures attempt to produce selective malabsorption of fat and carbohydrate as a means of treating the most severely obese patients. These operations carry the highest mortality rate and are therefore less likely to be offered routinely.
Roux-en-Y gastric bypass (RYGB). In the United States, the RYGB is performed more frequently than other procedures that combine malabsorption and restriction. It is considered by most to be the “gold standard” bariatric operation ( FIGURE 3 ).
The RYGB may induce weight loss through one or more of the following mechanisms:
- a decrease in the size of the gastric pouch. After the procedure, this pouch has a capacity of about 30 cc (size of a thumb)
- the small diameter of the gastrojejunal anastomosis, which is usually 1 cm
- glucose intolerance. About 50% of patients experience dumping symptoms when they ingest refined carbohydrates
- subclinical malabsorption. Food does not encounter the majority of digestive enzymes until it reaches the jejunojejunostomy anastomosis
- suppression of ghrelin production. Ghrelin is a hormone produced primarily in the gastric fundus and secondarily in the duodenum, both of which are bypassed with the RYGB. Plasma ghrelin levels peak before meals and are suppressed with food intake. After RYGB, patients demonstrate a flattening of this pattern, which appears to correlate with a suppression of appetite.10

FIGURE 3 Roux-en-Y gastric bypass
A gastric pouch is created at the top of the stomach and connected directly to the jejunum, bypassing the rest of the stomach and duodenum.
When is bariatric surgery indicated?
The NIH Consensus Conference identified patients who might be candidates for bariatric surgery, as I noted:
- patients who have a BMI of 40 or above, whether or not they have comorbidity
- patients who have a BMI of 35 or above and comorbidity.6
These recommendations have been adopted by third-party payers.
Potential comorbidities include hypertension, coronary artery disease (CAD), lipid abnormality, diabetes, obstructive sleep apnea (OSA), and severe osteoarthritis, among others.
When identified together, several of these comorbidities constitute metabolic syndrome, a risk factor for CAD. More than 50 million Americans are thought to exhibit this syndrome, which is diagnosed when three or more of the following are present:
- waist circumference ≥40 in (102 cm) in men; ≥35 in (88 cm) in women
- triglycerides ≥150 mg/dL
- high-density lipoprotein cholesterol <40 mg/dL in men; <50 mg/dL in women
- blood pressure ≥130/85 mm Hg
- fasting glucose ≥100 mg/dL.
Postsurgery weight loss has many benefits
Obstructive sleep apnea may resolve
Although this condition is known to be associated with obesity, it is drastically underdiagnosed.11 In our program, only 21% of patients had been given a diagnosis of OSA at the time of initial evaluation for surgery. After we obtained a polysomnogram (sleep study) for each of them, however, the true prevalence was determined to be 91%.
OSA can have serious consequences if it is untreated, and it may increase the risks associated with surgery and general anesthesia. By identifying and treating OSA before gastric bypass (RYGB), we were able to eliminate the respiratory ICU stay—a benefit that should be applicable to nonbariatric surgeries in the morbidly obese patient as well.12
With successful bariatric surgery, OSA abnormalities identified during polysomnography are dramatically improved or eliminated. Treatment with continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BIPAP) can usually be discontinued 6 months to 1 year after the dramatic weight loss associated with RYGB.
Cancer death rate may be reduced
Three consequences of morbid obesity not generally thought to be indications for bariatric surgery are:
- obesity-associated cancer
- decreased longevity
- infertility.
However, each of these conditions may be improved through successful bariatric surgery.
In a prospective study of more than 900,000 adults in the United States who were followed for 16 years, overweight or obesity was thought to account for 14% of cancer deaths in men and 20% of cancer deaths in women.13 Death rates for persons who had a BMI of at least 40 were 52% higher in men and 62% higher in women than they were in people who had a BMI below that threshold. BMI was significantly associated with cancer of the esophagus, colon and rectum, liver, gallbladder, pancreas, and kidney, as well as with non-Hodgkin’s lymphoma and multiple myeloma.
A trend toward an increasing risk of death with higher BMI was observed for cancer of the stomach (men), prostate, breast (women), uterus, ovary, and cervix.
The benefits of bariatric surgery in regard to cancer incidence and longevity were revealed in a 15-year, nonrandomized, prospective study involving more than 4,000 patients.14 At 10.9 years of follow-up, with a follow-up rate of 99.9%, this investigation concluded that bariatric surgery reduces mortality attributable to cardiovascular disease and cancer.14 Most surprising was the finding of a reduced incidence of cancer in patients who underwent bariatric surgery, compared with matched controls.14 An editorial accompanying this study summed it up in the headline: “The missing link—lose weight, live longer.”15
The Framingham risk score estimates the 10-year risk of CAD. This score is reduced by more than 50% after successful gastric bypass surgery.16
After surgery, fertility improves and pregnancy has better outcomes
From your practice, you’re certainly aware of the detrimental effects that obesity has on fertility, pregnancy, and fetal health.17-22 Although neither pregnancy nor impaired fertility is a primary indication for surgical weight reduction in an obese woman, bariatric surgery can improve the likelihood of fertility and successful pregnancy.
Advise patients to delay pregnancy after bariatric surgery. Although none of the bariatric operations performed today are contraindications to pregnancy, we caution all women to delay pregnancy—using two forms of birth control—until weight loss has stabilized. This usually takes about 12 to 18 months after surgery.
In our program, we identified 28 women who became pregnant following gastric bypass. Although we had cautioned all women to avoid early pregnancy, 10 became pregnant within 1 year of the bypass. Among these women, the rate of miscarriage was 40%, compared with 17% among the 18 women who waited more than 1 year to conceive. These percentages merit concern despite the small sample size.
Dao and colleagues concluded that the timing of pregnancy after gastric bypass is irrelevant.23 However, critical review of their data reveals an average weight gain of 4 lb in the group of women who became pregnant within a year after surgery (range, -70 to +45 lb), compared with 34 lb in the group that waited at least 1 year to conceive (range, +13 to +75 lb). As it was among our own patients, miscarriage was more common in the early group (24% vs 8% in the late group). Although these data are not statistically significant, they should arouse concern. I believe the most prudent advice to give women following bariatric surgery is to delay pregnancy until weight loss has stabilized.
The World Health Organization has estimated that there are 1 billion overweight adults on the planet. The problem of obesity, however, is concentrated in the United States. For well over a decade, the problem has escalated, with the US obesity rate referred to as “epidemic” and “a crisis”—among both adults and children.24
Among adults 20 years and older, the prevalence of obesity in the United States is 32%, and the prevalence of morbid obesity is almost 5%. Among adult women 20 to 39 years old, the prevalence of obesity and morbid obesity is 29% and 8%, respectively.27
Complications of bariatric surgery
Complications following bariatric surgery are intrinsic to the specific procedure performed. Because RYGB and the Lap-Band procedure constitute the overwhelming majority of bariatric operations, the most important complications associated with these surgeries will be addressed.
After RYGB, greatest risk is intestinal obstruction
Some of the early postoperative complications following RYGB are unlikely to be seen by physicians other than bariatric surgeons. They include anastomotic leaks, peritonitis, and bleeding. Pulmonary emboli should be managed as usual during the postoperative course. The amount of heparin necessary to achieve therapeutic anticoagulation may be quite substantial, but this fact should not deter the treating physician.
Nausea is almost universally present during the first few days after RYGB. When nausea and increasing food intolerance occur later (after the patient has demonstrated that food can be tolerated), it may indicate stenosis of the gastrojejunal anastomosis. The optimal study to evaluate these symptoms is a barium upper gastrointestinal (GI) swallow study. Stenosis can usually be managed by endoscopic dilatation.24
Intestinal obstruction. One of the most serious problems following RYGB is intestinal obstruction, which may be caused by internal hernia, adhesion, intussusception (not rare in the gastric bypass patient), and other less common causes ( FIGURE 1 ). Intestinal obstruction may occur early or years after the procedure.
In the RYGB patient, obstruction manifests with prominent pain, but distension and vomiting are usually absent, and plain abdominal radiographs are generally normal. The reason for this unusual presentation? The biliopancreatic limb tends to be the segment involved in the blockage, thereby creating a closed-loop obstruction. The most efficient way to diagnose this potentially life-threatening problem is by computed tomography (CT) ( FIGURE 4 ).
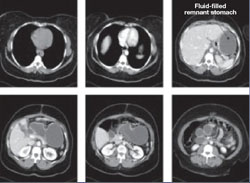
FIGURE 4 CT facilitates diagnosis of closed-loop obstruction
These computed tomography images reveal obstruction of the remnant stomach, duodenum, and proximal jejunum (the biliopancreatic limb) in a patient who has undergone Roux-en-Y gastric bypass.
Lap-Band complications may be pervasive
The Lap-Band procedure is often touted as having very low morbidity and mortality. However, data from outside the United States, where longer follow-up has been conducted, have cast a shadow of doubt on the supposed benefits of this restrictive procedure.
One study involving nearly 900 patients and 12 years of follow-up identified a rate of late complication of nearly 28% (2.3%, band erosion; 15.5%, pouch dilatation; 8.9%, port problems) and a rate of major reoperation of nearly 30%. The failure rate increased over time, reaching 65% at 10 years.
Despite these concerns, there is widespread enthusiasm among patients and bariatric surgeons who are proponents of this procedure.
A life-threatening complication. Any physician who might care for a patient who has undergone a Lap-Band procedure should be aware of one potentially life-threatening consequence: a slipped band. This complication can lead to incarceration of the stomach—usually the fundus—which, if left untreated, causes gastric infarction.
The main symptom of band slippage is pain. Any patient who has a Lap-Band and who reports significant upper abdominal pain must be evaluated to exclude slippage. Evaluation usually consists of a swallow study. Surgical correction is mandatory and urgent.
Like complications of surgery, the nutritional demands following bariatric surgery depend on the type of procedure that is performed.
After Lap-Band and other purely restrictive procedures,
nutritional levels remain stable
With restrictive procedures, such as the Lap-Band operation, the GI tract is essentially unaffected. Consequently, vitamin and micronutrient absorption remains intact. In these patients, we usually recommend a daily multivitamin. We assess serum levels to determine whether calcium and vitamin D supplementation might be necessary, which is especially important in female patients.
Close monitoring is needed after RYGB
After RYGB and other combined procedures, the question of nutritional supplementation becomes more complex.25 Bypass of the duodenum and upper jejunum affect absorption of iron, vitamin B12, calcium, and vitamin D. Serum calcium assessment is inadequate to determine the adequacy of calcium and vitamin D supplementation.
We evaluate parathyroid hormone and alkaline phosphatase levels in these patients. Any increase in these levels in the presence of normal serum calcium suggests the induction of secondary hyperparathyroidism and the need for additional calcium and vitamin D.26
Our recommendations for all patients following RYGB are a daily multivitamin, vitamin B12, and supplemental calcium and vitamin D. Vitamin B1 (thiamine) deficiency is extremely rare unless prolonged vomiting has been present. If B1 deficiency is suspected, administer thiamine before giving glucose because glucose can make symptoms worse.
Most women also need supplemental iron, which can be provided alone or in combination with the multivitamin, as in prenatal vitamins.
After RYGB, we measure vitamin and iron levels at 2 weeks, 3 months, 6 months, 12 months, 18 months, and then yearly thereafter unless a major abnormality is identified.
CASE: New-onset abdominal pain and a history of bariatric surgery
A 28-year-old woman who is 14 weeks pregnant (G5P1A4) complains of abdominal pain, nausea, and vomiting for the past 3 days. Four years ago, she underwent a successful Roux-en-Y gastric bypass, and her body mass index (BMI) decreased from 61.1 to 34.8 as a result. Today, after unremarkable ultrasonography at an outside hospital, she is transferred to your facility, where she is noted to be afebrile and tachycardic (133 bpm) with a very tender abdomen and a white blood cell (WBC) count of 12.2×103/μL.
Could her symptoms be related to her history of gastric bypass? How should you manage her condition?
This case illustrates why it is imperative that Ob Gyns have a basic understanding of bariatric surgery—particularly the types of procedures being performed today and the complications that may arise.
In this case, urgent intervention is called for, given the elevated WBC count and extreme tenderness of the abdomen. This patient was taken to surgery without waiting for additional imaging studies. Operative findings included intussusception with necrosis, a late complication of the Roux-en-Y procedure, necessitating resection of 60 cm of small intestine ( FIGURE 1 ). Although fetal heart sounds remained encouraging overnight, fetal demise occurred the next day. The patient’s physical recovery was otherwise unremarkable.
This scenario is not as unlikely as you might imagine. A similar episode was described in 2004.1 The outcome: maternal and fetal death.

FIGURE 1 Life-threatening intestinal obstruction
Patchy and continuous necrosis is evident following reduction of an obstruction-causing intussusception.
A boom in bariatric surgery
The incidence of surgical weight-loss procedures increased sixfold over a recent 7-year time span.2 In 2008 alone, more than 200,000 people underwent this type of operation—at least half of them women of reproductive age.2,3 In my experience at the University Hospitals of Cleveland Bariatric Program, which I directed, 85% of patients were women.4 This percentage is similar to the gender breakdown in other bariatric programs.
Because you are called on to provide both primary and specialty care, you are very likely to encounter women who have undergone bariatric surgery or who are considering it. As the prevalence of morbid obesity continues to rise, so will the need for familiarity with surgical weight-loss reduction.
In this article, I offer an overview of bariatric surgery, focusing on:
- the different procedures performed today
- the potential complications associated with the most common operations
- the need for nutritional assessment.
In the process, I discuss the health benefits of bariatric surgery, including greater fertility and improved pregnancy outcomes.
How we talk about obesity
The language of obesity centers on a basic metric: the body mass index (BMI).5 This index was devised in the 19th century by Adolphe Quetelet to describe total body fat.
Consider its use to describe two markedly overweight individuals. One stands 6 ft and weighs 500 lb; the other stands 5 ft and weighs 400 lb. It is obvious which person is heavier; the BMI quantifies who is actually bigger. The first individual has a BMI of 67.8, whereas the shorter person has a BMI of 78, despite weighing 100 lb less.
The formula for determining BMI is:
Among the imperfections of the BMI are its failure to differentiate between genders and its marked inaccuracy in persons who have significant muscle mass and limited body fat, such as body builders. However, it does make it possible to compare patients of different height and weight, thereby facilitating attempts to prognosticate the risk of illness and identify candidates for bariatric surgery ( TABLE 1 ).
The 1991 National Institutes of Health (NIH) Consensus Conference on Gastrointestinal Surgery for Severe Obesity recommended that bariatric surgery (restrictive and bypass procedures) be considered for patients who have a BMI of 40 or above and for patients who have a BMI of 35 or above with high-risk comorbidity.6
TABLE 1
How size is classified using the body mass index
| BMI | Classification | Risk of illness and comorbidity |
|---|---|---|
| <18.5 | Underweight | Increased |
| 18.5–24.9 | Normal | Average |
| 25–29.9 | Overweight | Increased |
| 30–34.9 | Obese (class I) | Moderate |
| 35–39.9 | Obese (class II) | Severe |
| ≥40 | Morbid obesity (class III) | Very severe |
| ≥50 | “Severe morbid obesity” | !!! Severe |
Most agree that bariatric surgery originated nearly 60 years ago with the jejunoileal bypass, a purely malabsorptive procedure in which the proximal jejunum was anastomosed to the distal ileum.7-9 This operation was based on the observation of dramatic weight loss following major small-bowel resection. The procedure was thought to allow obese patients to eat with abandon, thanks to the limited absorptive ability of the small intestine’s mucosal surface, which would impede digestion. However, the operation was fraught with complications, including protein calorie malnutrition, bacterial overgrowth, and even death. In addition, despite the dramatic reduction in the absorptive surface of the small intestine, some patients eventually regained weight.
One may still encounter patients who underwent jejunoileal bypass many years ago. One particular complication of this procedure is worth mentioning: hepatic cirrhosis. Any patient who has a history of jejunoileal bypass should have her liver function assessed before undergoing procedures that require general anesthesia.
At present, bariatric surgery may incorporate a component of malabsorption, but no other procedures are purely malabsorptive ( TABLE 2 ).
TABLE 2
Bariatric procedures for weight reduction, past and present
| Mechanism of action | Procedure |
|---|---|
| Malabsorptive | Jejunoileal bypass* |
| Restrictive | Vertical banded gastroplasty Gastric banding (Lap-Band) Laparoscopic sleeve gastrectomy Magenstrasse and Mill operation |
| Combination (malabsorptive and restrictive) | Roux-en-Y gastric bypass Biliopancreatic diversion Duodenal switch |
| Other | Gastric pacing† |
| * No longer performed | |
| †Experimental | |
Restrictive procedures
Vertical banded gastroplasty (VBG). This procedure is one of the earliest successful restrictive procedures ( FIGURE 2 ). Although it was originally performed via laparotomy, it is easily carried out laparoscopically. However, a risk of complication, such as severe reflux, and a low long-term success rate have decreased its widespread application.
Laparoscopic adjustable silicone band. The most common restrictive procedure performed today is the laparoscopic adjustable silicone band (Lap-Band) ( FIGURE 2 ). Among its benefits are:
- easy insertion, especially in comparison with the gastric bypass
- ability to adjust the amount of restriction (not possible with VBG)
- elimination of the need for supplemental nutrition
- reversibility.
Long-term results from a US population are not available because FDA approval did not occur until 2001. However, some centers outside the United States have reported unfavorable long-term outcomes. (See “Lap-Band complications may be pervasive,”.)
Laparoscopic sleeve gastrectomy (LSG). This operation was originally devised as the first stage of a duodenal switch. However, weight loss with this stage alone made LSG a bariatric procedure in its own right ( FIGURE 2 ).
Although this operation is categorized as restrictive, gastric sleeve resection eliminates the gastric fundus, the major site where ghrelin—“the hunger hormone”—is produced. This hormonal alteration may contribute to weight loss that occurs after LSG.
Magenstrasse and Mill operation. This operation converts the stomach into a long tube similar to the gastric sleeve. The greater curvature of the stomach is separated from the newly created tube but remains attached to the rest of the stomach at the antrum. (The greater curvature of the stomach is resected in the gastric sleeve procedure.)
Many insurers refuse to reimburse for restrictive operations other than the VBG and Lap-Band.

FIGURE 2 Three common surgeries
These restrictive procedures decrease the size of the stomach reservoir without impairing absorption of calories.
Combination procedures
Biliopancreatic diversion, duodenal switch. Despite the risk of protein malnutrition, these two procedures attempt to produce selective malabsorption of fat and carbohydrate as a means of treating the most severely obese patients. These operations carry the highest mortality rate and are therefore less likely to be offered routinely.
Roux-en-Y gastric bypass (RYGB). In the United States, the RYGB is performed more frequently than other procedures that combine malabsorption and restriction. It is considered by most to be the “gold standard” bariatric operation ( FIGURE 3 ).
The RYGB may induce weight loss through one or more of the following mechanisms:
- a decrease in the size of the gastric pouch. After the procedure, this pouch has a capacity of about 30 cc (size of a thumb)
- the small diameter of the gastrojejunal anastomosis, which is usually 1 cm
- glucose intolerance. About 50% of patients experience dumping symptoms when they ingest refined carbohydrates
- subclinical malabsorption. Food does not encounter the majority of digestive enzymes until it reaches the jejunojejunostomy anastomosis
- suppression of ghrelin production. Ghrelin is a hormone produced primarily in the gastric fundus and secondarily in the duodenum, both of which are bypassed with the RYGB. Plasma ghrelin levels peak before meals and are suppressed with food intake. After RYGB, patients demonstrate a flattening of this pattern, which appears to correlate with a suppression of appetite.10

FIGURE 3 Roux-en-Y gastric bypass
A gastric pouch is created at the top of the stomach and connected directly to the jejunum, bypassing the rest of the stomach and duodenum.
When is bariatric surgery indicated?
The NIH Consensus Conference identified patients who might be candidates for bariatric surgery, as I noted:
- patients who have a BMI of 40 or above, whether or not they have comorbidity
- patients who have a BMI of 35 or above and comorbidity.6
These recommendations have been adopted by third-party payers.
Potential comorbidities include hypertension, coronary artery disease (CAD), lipid abnormality, diabetes, obstructive sleep apnea (OSA), and severe osteoarthritis, among others.
When identified together, several of these comorbidities constitute metabolic syndrome, a risk factor for CAD. More than 50 million Americans are thought to exhibit this syndrome, which is diagnosed when three or more of the following are present:
- waist circumference ≥40 in (102 cm) in men; ≥35 in (88 cm) in women
- triglycerides ≥150 mg/dL
- high-density lipoprotein cholesterol <40 mg/dL in men; <50 mg/dL in women
- blood pressure ≥130/85 mm Hg
- fasting glucose ≥100 mg/dL.
Postsurgery weight loss has many benefits
Obstructive sleep apnea may resolve
Although this condition is known to be associated with obesity, it is drastically underdiagnosed.11 In our program, only 21% of patients had been given a diagnosis of OSA at the time of initial evaluation for surgery. After we obtained a polysomnogram (sleep study) for each of them, however, the true prevalence was determined to be 91%.
OSA can have serious consequences if it is untreated, and it may increase the risks associated with surgery and general anesthesia. By identifying and treating OSA before gastric bypass (RYGB), we were able to eliminate the respiratory ICU stay—a benefit that should be applicable to nonbariatric surgeries in the morbidly obese patient as well.12
With successful bariatric surgery, OSA abnormalities identified during polysomnography are dramatically improved or eliminated. Treatment with continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BIPAP) can usually be discontinued 6 months to 1 year after the dramatic weight loss associated with RYGB.
Cancer death rate may be reduced
Three consequences of morbid obesity not generally thought to be indications for bariatric surgery are:
- obesity-associated cancer
- decreased longevity
- infertility.
However, each of these conditions may be improved through successful bariatric surgery.
In a prospective study of more than 900,000 adults in the United States who were followed for 16 years, overweight or obesity was thought to account for 14% of cancer deaths in men and 20% of cancer deaths in women.13 Death rates for persons who had a BMI of at least 40 were 52% higher in men and 62% higher in women than they were in people who had a BMI below that threshold. BMI was significantly associated with cancer of the esophagus, colon and rectum, liver, gallbladder, pancreas, and kidney, as well as with non-Hodgkin’s lymphoma and multiple myeloma.
A trend toward an increasing risk of death with higher BMI was observed for cancer of the stomach (men), prostate, breast (women), uterus, ovary, and cervix.
The benefits of bariatric surgery in regard to cancer incidence and longevity were revealed in a 15-year, nonrandomized, prospective study involving more than 4,000 patients.14 At 10.9 years of follow-up, with a follow-up rate of 99.9%, this investigation concluded that bariatric surgery reduces mortality attributable to cardiovascular disease and cancer.14 Most surprising was the finding of a reduced incidence of cancer in patients who underwent bariatric surgery, compared with matched controls.14 An editorial accompanying this study summed it up in the headline: “The missing link—lose weight, live longer.”15
The Framingham risk score estimates the 10-year risk of CAD. This score is reduced by more than 50% after successful gastric bypass surgery.16
After surgery, fertility improves and pregnancy has better outcomes
From your practice, you’re certainly aware of the detrimental effects that obesity has on fertility, pregnancy, and fetal health.17-22 Although neither pregnancy nor impaired fertility is a primary indication for surgical weight reduction in an obese woman, bariatric surgery can improve the likelihood of fertility and successful pregnancy.
Advise patients to delay pregnancy after bariatric surgery. Although none of the bariatric operations performed today are contraindications to pregnancy, we caution all women to delay pregnancy—using two forms of birth control—until weight loss has stabilized. This usually takes about 12 to 18 months after surgery.
In our program, we identified 28 women who became pregnant following gastric bypass. Although we had cautioned all women to avoid early pregnancy, 10 became pregnant within 1 year of the bypass. Among these women, the rate of miscarriage was 40%, compared with 17% among the 18 women who waited more than 1 year to conceive. These percentages merit concern despite the small sample size.
Dao and colleagues concluded that the timing of pregnancy after gastric bypass is irrelevant.23 However, critical review of their data reveals an average weight gain of 4 lb in the group of women who became pregnant within a year after surgery (range, -70 to +45 lb), compared with 34 lb in the group that waited at least 1 year to conceive (range, +13 to +75 lb). As it was among our own patients, miscarriage was more common in the early group (24% vs 8% in the late group). Although these data are not statistically significant, they should arouse concern. I believe the most prudent advice to give women following bariatric surgery is to delay pregnancy until weight loss has stabilized.
The World Health Organization has estimated that there are 1 billion overweight adults on the planet. The problem of obesity, however, is concentrated in the United States. For well over a decade, the problem has escalated, with the US obesity rate referred to as “epidemic” and “a crisis”—among both adults and children.24
Among adults 20 years and older, the prevalence of obesity in the United States is 32%, and the prevalence of morbid obesity is almost 5%. Among adult women 20 to 39 years old, the prevalence of obesity and morbid obesity is 29% and 8%, respectively.27
Complications of bariatric surgery
Complications following bariatric surgery are intrinsic to the specific procedure performed. Because RYGB and the Lap-Band procedure constitute the overwhelming majority of bariatric operations, the most important complications associated with these surgeries will be addressed.
After RYGB, greatest risk is intestinal obstruction
Some of the early postoperative complications following RYGB are unlikely to be seen by physicians other than bariatric surgeons. They include anastomotic leaks, peritonitis, and bleeding. Pulmonary emboli should be managed as usual during the postoperative course. The amount of heparin necessary to achieve therapeutic anticoagulation may be quite substantial, but this fact should not deter the treating physician.
Nausea is almost universally present during the first few days after RYGB. When nausea and increasing food intolerance occur later (after the patient has demonstrated that food can be tolerated), it may indicate stenosis of the gastrojejunal anastomosis. The optimal study to evaluate these symptoms is a barium upper gastrointestinal (GI) swallow study. Stenosis can usually be managed by endoscopic dilatation.24
Intestinal obstruction. One of the most serious problems following RYGB is intestinal obstruction, which may be caused by internal hernia, adhesion, intussusception (not rare in the gastric bypass patient), and other less common causes ( FIGURE 1 ). Intestinal obstruction may occur early or years after the procedure.
In the RYGB patient, obstruction manifests with prominent pain, but distension and vomiting are usually absent, and plain abdominal radiographs are generally normal. The reason for this unusual presentation? The biliopancreatic limb tends to be the segment involved in the blockage, thereby creating a closed-loop obstruction. The most efficient way to diagnose this potentially life-threatening problem is by computed tomography (CT) ( FIGURE 4 ).
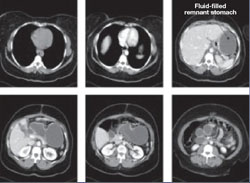
FIGURE 4 CT facilitates diagnosis of closed-loop obstruction
These computed tomography images reveal obstruction of the remnant stomach, duodenum, and proximal jejunum (the biliopancreatic limb) in a patient who has undergone Roux-en-Y gastric bypass.
Lap-Band complications may be pervasive
The Lap-Band procedure is often touted as having very low morbidity and mortality. However, data from outside the United States, where longer follow-up has been conducted, have cast a shadow of doubt on the supposed benefits of this restrictive procedure.
One study involving nearly 900 patients and 12 years of follow-up identified a rate of late complication of nearly 28% (2.3%, band erosion; 15.5%, pouch dilatation; 8.9%, port problems) and a rate of major reoperation of nearly 30%. The failure rate increased over time, reaching 65% at 10 years.
Despite these concerns, there is widespread enthusiasm among patients and bariatric surgeons who are proponents of this procedure.
A life-threatening complication. Any physician who might care for a patient who has undergone a Lap-Band procedure should be aware of one potentially life-threatening consequence: a slipped band. This complication can lead to incarceration of the stomach—usually the fundus—which, if left untreated, causes gastric infarction.
The main symptom of band slippage is pain. Any patient who has a Lap-Band and who reports significant upper abdominal pain must be evaluated to exclude slippage. Evaluation usually consists of a swallow study. Surgical correction is mandatory and urgent.
Like complications of surgery, the nutritional demands following bariatric surgery depend on the type of procedure that is performed.
After Lap-Band and other purely restrictive procedures,
nutritional levels remain stable
With restrictive procedures, such as the Lap-Band operation, the GI tract is essentially unaffected. Consequently, vitamin and micronutrient absorption remains intact. In these patients, we usually recommend a daily multivitamin. We assess serum levels to determine whether calcium and vitamin D supplementation might be necessary, which is especially important in female patients.
Close monitoring is needed after RYGB
After RYGB and other combined procedures, the question of nutritional supplementation becomes more complex.25 Bypass of the duodenum and upper jejunum affect absorption of iron, vitamin B12, calcium, and vitamin D. Serum calcium assessment is inadequate to determine the adequacy of calcium and vitamin D supplementation.
We evaluate parathyroid hormone and alkaline phosphatase levels in these patients. Any increase in these levels in the presence of normal serum calcium suggests the induction of secondary hyperparathyroidism and the need for additional calcium and vitamin D.26
Our recommendations for all patients following RYGB are a daily multivitamin, vitamin B12, and supplemental calcium and vitamin D. Vitamin B1 (thiamine) deficiency is extremely rare unless prolonged vomiting has been present. If B1 deficiency is suspected, administer thiamine before giving glucose because glucose can make symptoms worse.
Most women also need supplemental iron, which can be provided alone or in combination with the multivitamin, as in prenatal vitamins.
After RYGB, we measure vitamin and iron levels at 2 weeks, 3 months, 6 months, 12 months, 18 months, and then yearly thereafter unless a major abnormality is identified.
1. Moore KA, Ouyang DW, Whang EE. Maternal and fetal deaths after gastric bypass surgery for morbid obesity. N Engl J Med. 2004;351:721-722.
2. Bariatric Surgery in Women of Reproductive Age: Special Concerns for Pregnancy. Structured Abstract. Rockville, Md: Agency for Healthcare Research and Quality; November 2008. Available at: www.ahrq.gov/Clinic/tp/barireptp.htm. Accessed Dec. 8, 2009.
3. American Society for Metabolic and Bariatric Surgery. Metabolic and bariatric surgery fact sheet. Available at: www.asmbs.org/Newsite07/media/asmbs_fs_surgery.pdf. Accessed Dec. 8, 2009.
4. Stellato TA, Hallowell PT, Crouse C, Schuster M, Petrozzi MC. Two-day length of stay following open Roux-en-Y gastric bypass: is it feasible, safe and reasonable? Obes Surg. 2004;14:27-34.
5. Oria HE, Carrasquilla C, Cunningham P, et al. American Society for Bariatric Surgery Standards Committee, 2004–2005. Guidelines for weight calculations and follow-up in bariatric surgery. Surg Obes Relat Dis. 2005;1:67-68.
6. Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference Statement. Am J Clin Nutr. 1992;55(Suppl 2):615S-619S.
7. MacDonald KG, Jr. Overview of the epidemiology of obesity and the early history of procedures to remedy morbid obesity. Arch Surg. 2003;138:357-360.
8. Buchwald H. Overview of bariatric surgery. J Am Coll Surg. 2002;194:367-375.
9. DeMaria EJ. Bariatric surgery for morbid obesity. N Engl J Med. 2007;356:2176-2183.
10. Cummings DE, Weigle DS, Frayo RS, et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med. 2002;346:1623-1630.
11. Hallowell PT, Stellato TA, Schuster M, et al. Potentially life-threatening sleep apnea is unrecognized without aggressive evaluation. Am J Surg. 2007;193:364-367.
12. Hallowell PT, Stellato TA, Petrozzi MC, et al. Eliminating respiratory intensive care unit stay after gastric bypass surgery. Surgery. 2007;142:608-612.
13. Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625-1638.
14. Sjöström L, Narbro K, Sjöström CD, et al. Swedish Obese Subjects Study. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741-752.
15. Bray GA. The missing link—lose weight, live longer. N Engl J Med. 2007;357:818-820.
16. Kligman MD, Dexter DJ, Omer S, Park AE. Shrinking cardiovascular risk through bariatric surgery: application of Framingham risk score in gastric bypass. Surgery. 2008;143:533-538.
17. Linné Y. Effects of obesity on women’s reproduction and complications during pregnancy. Obes Rev. 2004;5:137-143.
18. Pasquali R, Pelusi C, Genghini S, Cacciari M, Gambineri A. Obesity and reproductive disorders in women. Hum Reprod Update. 2003;9:359-372.
19. Baeten JM, Bukusi EA, Lambe M. Pregnancy complications and outcomes among overweight and obese nulliparous women. Am J Public Health. 2001;91:436-440.
20. Lashen H, Fear K, Sturdee DW. Obesity is associated with increased risk of first trimester and recurrent miscarriage: matched case-control study. Hum Reprod. 2004;19:1644-1646.
21. Cnattingius S, Bergström R, Lipworth L, Kramer MS. Prepregnancy weight and the risk of adverse pregnancy outcomes. N Engl J Med. 1998;338:147-152.
22. Pathi A, Esen U, Hildreth A. A comparison of complications of pregnancy and delivery in morbidly obese and non-obese women. J Obstet Gynaecol. 2006;26:527-530.
23. Dao T, Kuhn J, Ehmer D, Fisher T, McCarty T. Pregnancy outcomes after gastric-bypass surgery. Am J Surg. 2006;192:762-766.
24. Stellato TA, Crouse C, Hallowell PT. Bariatric surgery: creating new challenges for the endoscopist. Gastrointest Endosc. 2003;57:86-94.
25. Poitou Bernert C, Ciangura C, Coupaye M, Czernichow S, Bouillot JL, Basdevant A. Nutritional deficiency after gastric bypass: diagnosis, prevention and treatment. Diabetes Metab. 2007;33:13-24.
26. Jin J, Robinson AV, Hallowell PT, Jasper JJ, Stellato TA, Wilhelm SM. Increases in parathyroid hormone (PTH) after gastric bypass surgery appear to be of a secondary nature. Surgery. 2007;142:914-920.
27. Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549-1555.
1. Moore KA, Ouyang DW, Whang EE. Maternal and fetal deaths after gastric bypass surgery for morbid obesity. N Engl J Med. 2004;351:721-722.
2. Bariatric Surgery in Women of Reproductive Age: Special Concerns for Pregnancy. Structured Abstract. Rockville, Md: Agency for Healthcare Research and Quality; November 2008. Available at: www.ahrq.gov/Clinic/tp/barireptp.htm. Accessed Dec. 8, 2009.
3. American Society for Metabolic and Bariatric Surgery. Metabolic and bariatric surgery fact sheet. Available at: www.asmbs.org/Newsite07/media/asmbs_fs_surgery.pdf. Accessed Dec. 8, 2009.
4. Stellato TA, Hallowell PT, Crouse C, Schuster M, Petrozzi MC. Two-day length of stay following open Roux-en-Y gastric bypass: is it feasible, safe and reasonable? Obes Surg. 2004;14:27-34.
5. Oria HE, Carrasquilla C, Cunningham P, et al. American Society for Bariatric Surgery Standards Committee, 2004–2005. Guidelines for weight calculations and follow-up in bariatric surgery. Surg Obes Relat Dis. 2005;1:67-68.
6. Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference Statement. Am J Clin Nutr. 1992;55(Suppl 2):615S-619S.
7. MacDonald KG, Jr. Overview of the epidemiology of obesity and the early history of procedures to remedy morbid obesity. Arch Surg. 2003;138:357-360.
8. Buchwald H. Overview of bariatric surgery. J Am Coll Surg. 2002;194:367-375.
9. DeMaria EJ. Bariatric surgery for morbid obesity. N Engl J Med. 2007;356:2176-2183.
10. Cummings DE, Weigle DS, Frayo RS, et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med. 2002;346:1623-1630.
11. Hallowell PT, Stellato TA, Schuster M, et al. Potentially life-threatening sleep apnea is unrecognized without aggressive evaluation. Am J Surg. 2007;193:364-367.
12. Hallowell PT, Stellato TA, Petrozzi MC, et al. Eliminating respiratory intensive care unit stay after gastric bypass surgery. Surgery. 2007;142:608-612.
13. Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625-1638.
14. Sjöström L, Narbro K, Sjöström CD, et al. Swedish Obese Subjects Study. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741-752.
15. Bray GA. The missing link—lose weight, live longer. N Engl J Med. 2007;357:818-820.
16. Kligman MD, Dexter DJ, Omer S, Park AE. Shrinking cardiovascular risk through bariatric surgery: application of Framingham risk score in gastric bypass. Surgery. 2008;143:533-538.
17. Linné Y. Effects of obesity on women’s reproduction and complications during pregnancy. Obes Rev. 2004;5:137-143.
18. Pasquali R, Pelusi C, Genghini S, Cacciari M, Gambineri A. Obesity and reproductive disorders in women. Hum Reprod Update. 2003;9:359-372.
19. Baeten JM, Bukusi EA, Lambe M. Pregnancy complications and outcomes among overweight and obese nulliparous women. Am J Public Health. 2001;91:436-440.
20. Lashen H, Fear K, Sturdee DW. Obesity is associated with increased risk of first trimester and recurrent miscarriage: matched case-control study. Hum Reprod. 2004;19:1644-1646.
21. Cnattingius S, Bergström R, Lipworth L, Kramer MS. Prepregnancy weight and the risk of adverse pregnancy outcomes. N Engl J Med. 1998;338:147-152.
22. Pathi A, Esen U, Hildreth A. A comparison of complications of pregnancy and delivery in morbidly obese and non-obese women. J Obstet Gynaecol. 2006;26:527-530.
23. Dao T, Kuhn J, Ehmer D, Fisher T, McCarty T. Pregnancy outcomes after gastric-bypass surgery. Am J Surg. 2006;192:762-766.
24. Stellato TA, Crouse C, Hallowell PT. Bariatric surgery: creating new challenges for the endoscopist. Gastrointest Endosc. 2003;57:86-94.
25. Poitou Bernert C, Ciangura C, Coupaye M, Czernichow S, Bouillot JL, Basdevant A. Nutritional deficiency after gastric bypass: diagnosis, prevention and treatment. Diabetes Metab. 2007;33:13-24.
26. Jin J, Robinson AV, Hallowell PT, Jasper JJ, Stellato TA, Wilhelm SM. Increases in parathyroid hormone (PTH) after gastric bypass surgery appear to be of a secondary nature. Surgery. 2007;142:914-920.
27. Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549-1555.