User login
How can I improve opioid safety at my hospital?
Quality improvement is essential
Case
A 67-year-old opioid-naive male with a history of obstructive sleep apnea and chronic kidney disease became unresponsive 2 days after hip replacement. Physical exam revealed a respiratory rate of 6 breaths/minute and oxygen saturation of 82%. He had received 6 doses of 6-mg IV morphine within the past 7 hours. How can I improve opioid safety at my hospital?
Background
Opioids are the most commonly prescribed class of medication in the hospital and the second–most common class causing adverse drug events (ADEs), the most serious being respiratory depression and death.1
Opioid ADEs and side effects can cause prolonged length of stay and patient suffering. These vary from potentially life-threatening events such as serotonin syndrome and adrenal insufficiency to more manageable problems still requiring intervention such as constipation, urinary retention, cognitive impairment, nausea, and vomiting. Treatment of side effects can lead to complications, including side effects from antiemetics and urinary tract infections from catheters.
A 4-year review found 700 deaths in the United States attributed to patient-controlled analgesia (PCA) use.2 Another study revealed that one out of every 200 patients has postoperative respiratory depression attributable to opioids.3
It is estimated that 2 million patients a year become chronic opioid users. Inpatient opioid prescribing contributes to this problem;4 for instance, 5.9% of patients after minor surgery and 6.5% after major surgery become chronic opioid users if discharged with an opioid.5 Calcaterra et al. found 25% of opioid-naive medical patients received an opioid at discharge from a medical service.6 Those patients had an odds ratio of 4.90 for becoming a chronic opioid user that year.6
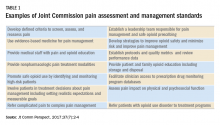
Most hospitals have incomplete or outdated policies and procedures for safe opioid prescribing and administration.7 The Joint Commission on Accreditation of Healthcare Organizations has specific pain standards for pain assessment, pain management, and safe opioid prescribing for hospitals. Additions and revisions were developed to go into effect Jan. 1, 2018. (Table 1)8
Quality improvement
Quality improvement (QI) is an effective way to improve opioid safety. The Society of Hospital Medicine has developed a QI guide, “Reducing adverse drug events related to opioids” or “RADEO,” to increase safety and decrease serious ADEs attributable to opioids.7
The steps in the RADEO program are as follows:
1. Assemble your team
It is critical to identify and include stakeholders from multiple disciplines on your project team. This team will be essential to develop a practical project, identify barriers, create solutions, and gain buy-in from medical staff and administrative leadership.
Front-line staff will have invaluable insight and need to be team members. The majority of interventions are performed by nurses; therefore, nursing leadership and input is essential. Representatives from pharmacy, information technology, and the quality department will be extremely valuable team members to guide you through the correct approach to a successful QI project.
A project champion can keep a high profile for the project and build and lead the team.
Identify an “executive sponsor” such as your CEO, CMO, or CNO. This leader will focus the team on issues critical to your organization, such as accreditation from governmental agencies, and help you obtain dedicated time and resources. Aligning with hospital goals will make your project a priority.
Coordinate with existing opioid initiative teams in the hospital to integrate efforts. This will keep the work of different departments aligned and allow you to learn from pitfalls and barriers the other groups experienced.
Patients/families contribute a unique and valuable perspective. Consider including a member of your hospital’s patient and family advisory council on your team.
2. Perform a needs assessment
Determine the current state of your hospital including: opioid prescribers; opioids prescribed; areas with increased ADEs or naloxone use; formulary restrictions, policies, or guidelines for monitoring, prescribing, and administering opioids; order sets; safety alerts; provider education; or patient education.
Your risk management or quality department may be able to a share root cause analysis of ADEs related to opioids. Joint Commission and CMS recommendations as well as other regulatory requirements may shape your QI interventions.8
Most importantly, review all of the concerns and priorities of your diverse team, which will identify areas of most pressing need and provide insight regarding needs you have not considered.
3. Develop SMART aims
Frame your QI project into a series of well-defined, clear SMART aims.9
Specific: Who will carry out the intervention? Who is your target population? What will be improved? In what way will it be improved?
Measurable: What will be measured? How it will be measured? Does it measure the outcome that needs to be improved?
Attainable/achievable: Ensure you have the resources and time to achieve the aim.
Relevant: Ensure each aim moves your team toward the project vision.
Timely: The aim should be achieved within a realistic time frame, long enough to meet goals but not so long that interest is lost.
An example of a poor aim is “Clinicians will improve knowledge of opioids.”
An example of a SMART aim is “75% of inpatient opioid prescribers including MDs, NPs, and PAs will complete and pass the opioid safety training module by July 1, 2018.”
4. Choose metrics
Outcome metrics measure if the intervention has improved patient safety, for example, measuring a decrease in opioid related ADEs. Structure metrics are the physical and organizational properties of the health care delivery setting, for example, the presence of EMR opioid safety. Processes are communication and practice patterns, for example, adherence to policy by examining nursing documentation of pain assessments.
5. Development and implementation 7,10
Use PDSA for development and implementation of the QI intervention.
Plan: Determine the intervention group such as a specific unit, number of units, and if there will be a control group. Determine who will collect the data, if baseline data will be collected, and who will analyze the data. Your information technology department will be essential to determine if the data can be collected via the EMR and how. Input from your multidisciplinary team is critical to anticipate unintended consequences, such as limiting opioid prescribing at discharge inadvertently increasing emergency department visits for pain control.
Do: Start as a small pilot study to make it as easy as possible to implement the project and begin data collection. A small-scale intervention will be more manageable and allow rapid responses to unanticipated problems.
Study: Analyze the data early to determine if the intervention is improving opioid safety and if alterations are needed. At this stage both process metrics (are processes being followed?) and outcome metrics (is the process leading to a desired outcome?) are important.
Act: Based on data analysis, refine the intervention as necessary. You may have to repeat cycles of PDSA to develop the final intervention. Then implement the final intervention to the entire hospital.
The Joint Commission recommendations for opioid QI
The Joint Commission recommends7 the following to reduce opioid-related respiratory depression:
- Effective processes which include processes such as tracking and analyzing ADEs related to opioids.
- Safe technology which includes using technology such as the EMR to monitor opioid prescribing of greater than 90 morphine milligram equivalents.
- Effective tools which include valid and reliable tools to improve opioid safety, such as the Pasero Opioid Induced Sedation Scale (POSS).
- Opioid education and training which includes provider and patient education such as patient discharge education.
Education
Develop educational interventions to ensure medical and hospital staff are aware of new processes, with an emphasis on “why.”7 If possible, use web-based programs that provide CME. Improve education interventions by using multiple live, interactive, and multimedia exposures.
Principles for successful interventions
- Keep it simple for the end user. This makes it more likely that the intervention is performed. Minimize complex tasks such as calculations and if possible design automated processes.
- Build your process into current work flow. If possible simplify or streamline work flow. A project that competes with staff’s other tasks and competing priorities is doomed to fail. It is critical to have input from those performing the intervention to develop a user-friendly and less disruptive intervention.
- Design reliability into the process. Make your intervention the default action. Build prompts into the work flow. Standardize the intervention into the work flow. And, consider having the intervention at scheduled intervals.7
Opioid safety QI interventions
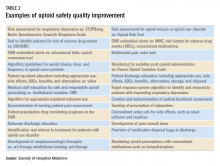
Interventions for improving opioid safety and reducing opioid -elated ADEs may be generalized into areas including risk screening and assessment, pain treatment, opioid administration, pain assessment, post opioid administration monitoring, and patient and provider education (Table 2).7
Back to the case
The patient received naloxone. His respiratory rate and oxygen saturation returned to normal. His dose of morphine was reduced and his interval increased. A multimodal approach was implemented including low-dose scheduled acetaminophen. There were no further ADEs while maintaining good pain control.
A multidisciplinary opioid task force was created and performed a hospital-wide review of opioid ADEs. Opportunities for improvement were identified and new procedures implemented. The Pasero opioid sedation scale (POSS) was added to the nursing work flow to monitor patients who received an opioid for sedation. An algorithm was developed for opioid-naive patients including guidance for opioid selection, dosing, and frequency. Multiple pain control modalities were added to pain control order sets. Annual training was developed for opioid prescribers, pharmacists, and nurses regarding safe and responsible use of opioids.
And, lastly, in-hospital and discharge patient education was developed for patients and families to be well-informed of opioid risk and benefit including how to identify and respond to ADEs.
Bottom line
Quality improvement is an effective method to improve patient safety and reduce serious adverse events related to opioids in the hospital setting.
Dr. Holmes-Maybank, is codirector, Fundamentals of Patient Care Year 1 and Internship 101, and chair, Clinical Competency Examination Committee, division of hospital medicine, Medical University of South Carolina. Dr. Frederickson is medical director, Hospital Medicine and Palliative Care at CHI Health, Omaha, Neb., and assistant professor at Creighton University School of Medicine, Omaha.
References
1. Davies EC et al. Adverse drug reactions in hospital inpatients: a prospective analysis of 3695 patient-episodes. PLoS One. 2009;4(2):e4439. doi: 10.1371/journal.pone.0004439. Epub 2009 Feb 11.
2. Association for the Advancement of Medical Instrumentation. Infusing patients safely: Priority issues from the AAMI/FDA Infusion Device Summit. 2010;1-39.
3. Dahan Aet al. Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology. 2010;112:226-238. doi: 10.1097/ALN.0b013e3181c38c25.
4. Estimate about opioid users.
5. Brummett CM et al. New persistent opioid use after minor and major surgical procedures in U.S. adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504.
6. Calcaterra SL et al. Opioid prescribing at hospital discharge contributes to chronic opioid use. J Gen Intern Med. 2016;31(5):478-85. doi: 10.1007/s11606-015-3539-4.
7. Frederickson TW et al. Reducing adverse drug events related to opioids implementation guide. Philadelphia: Society of Hospital Medicine, 2015.
8. Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
9. Minnesota Department of Health. SMART objectives.
10. Agency for Healthcare Research and Quality. Health Literacy Universal Precautions Toolkit, 2nd Edition.
Plan-Do-Study-Act (PDSA) Directions and Examples.
Recommended reading
Dowell D et al. CDC guideline for prescribing opioids for chronic pain – United States, 2016. Recommendations and Reports. 2016 Mar 18;65(1):1-49.
Frederickson TW et al. Using the 2018 guidelines from the Joint Commission to kickstart your hospital’s program to reduce opioid-induced ventilatory impairment. Anesthesia Patient Safety Foundation Newsletter. 2018;33(1):1-32.
Herzig SJ et al. Safe opioid prescribing for acute noncancer pain in hospitalized adults: a systematic review of existing guidelines. J Hosp Med. 2018 Apr;13(4):256-62. doi: 10.12788/jhm.2979.
Herzig SJ et al. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med. 2018 Apr;13(4):263-71. doi: 10.12788/jhm.2980.
Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
Key points
- Quality improvement is required by the Joint Commission and is an effective method to improve opioid safety in the hospital setting.
- It is critical to the success of a QI project to develop a multidisciplinary team.
- Input from frontline users of the intervention is essential to produce an effective intervention.
- Executive sponsorship and aligning the goals of your QI project with those of your institution will prioritize your project and increase resource availability.
Quiz
1. Based on a needs assessment at your hospital you assemble a multidisciplinary team to improve education for patients discharged on opioids. You recognize the importance of multidisciplinary input to develop a successful intervention for discharge education. Essential team members include all EXCEPT the following:
a. Executive sponsor
b. Patient representative
c. Nursing
d. Medical student representative ---- CORRECT
Explanation: The assembly of a multidisciplinary team is critical to the success of a QI intervention. An executive sponsor may assist you in aligning your goals with that of the hospital and provide resources for its development and implementation. Patient input would help determine how to best deliver the education. Lastly, the individuals carrying out the intervention are essential to develop an intervention that will easy for the end user and increase the likelihood of being used, in this case nursing.
2. You performed a review of naloxone use at your hospital and find that it is greater than similar hospitals. Prior to starting the QI project, you review SHM’s “Reducing adverse events related to opioids implementation guide” and learn that keys to success for QI implementation include:
a. A team of primarily hospitalists
b. Implementing the intervention hospital wide
c. Information technology input for data collection ---- CORRECT
d. No team – it is more effective to work alone
Explanation: Successful implementation of a QI project involves a multidisciplinary team. It is critical to involve information technology early in the development of the project to determine how and if the data can be collected from the EMR. It is best to pilot the intervention on one or two units to make alterations as needed rapidly and perfect the final intervention prior to rolling it out to the entire hospital.
3. You have assembled a multidisciplinary team to respond to the newly revised JCAHO pain standards. An example of a requirement from the new and revised JCAHO standards for pain assessment and management includes:
a. Programs for physician wellness
b. No opioids for chronic pain
c. No more than 5 days of opioids for acute pain
d. Nonpharmacologic pain management options ---- CORRECT
Explanation: JCAHO released new and revised requirements for pain assessment and management including offering nonpharmacologic pain management options. (See Table 1)
4. Your multidisciplinary QI team decides to develop a project to reduce respiratory depression in patients receiving opioids by monitoring for sedation with the Pasero Opioid Induced Sedation Scale. Principles for successful QI interventions include:
a. Complex tasks
b. Make the intervention a default action ---- CORRECT
c. Avoid EMR prompts
d. Competing with other hospital priorities
Explanation: Principles for successful QI interventions include keeping tasks simple, ensuring the intervention does not compete with other priorities, making the intervention the default action, installing prompts in the EMR, and standardizing the intervention into the work flow.
Quality improvement is essential
Quality improvement is essential
Case
A 67-year-old opioid-naive male with a history of obstructive sleep apnea and chronic kidney disease became unresponsive 2 days after hip replacement. Physical exam revealed a respiratory rate of 6 breaths/minute and oxygen saturation of 82%. He had received 6 doses of 6-mg IV morphine within the past 7 hours. How can I improve opioid safety at my hospital?
Background
Opioids are the most commonly prescribed class of medication in the hospital and the second–most common class causing adverse drug events (ADEs), the most serious being respiratory depression and death.1
Opioid ADEs and side effects can cause prolonged length of stay and patient suffering. These vary from potentially life-threatening events such as serotonin syndrome and adrenal insufficiency to more manageable problems still requiring intervention such as constipation, urinary retention, cognitive impairment, nausea, and vomiting. Treatment of side effects can lead to complications, including side effects from antiemetics and urinary tract infections from catheters.
A 4-year review found 700 deaths in the United States attributed to patient-controlled analgesia (PCA) use.2 Another study revealed that one out of every 200 patients has postoperative respiratory depression attributable to opioids.3
It is estimated that 2 million patients a year become chronic opioid users. Inpatient opioid prescribing contributes to this problem;4 for instance, 5.9% of patients after minor surgery and 6.5% after major surgery become chronic opioid users if discharged with an opioid.5 Calcaterra et al. found 25% of opioid-naive medical patients received an opioid at discharge from a medical service.6 Those patients had an odds ratio of 4.90 for becoming a chronic opioid user that year.6
Most hospitals have incomplete or outdated policies and procedures for safe opioid prescribing and administration.7 The Joint Commission on Accreditation of Healthcare Organizations has specific pain standards for pain assessment, pain management, and safe opioid prescribing for hospitals. Additions and revisions were developed to go into effect Jan. 1, 2018. (Table 1)8
Quality improvement
Quality improvement (QI) is an effective way to improve opioid safety. The Society of Hospital Medicine has developed a QI guide, “Reducing adverse drug events related to opioids” or “RADEO,” to increase safety and decrease serious ADEs attributable to opioids.7
The steps in the RADEO program are as follows:
1. Assemble your team
It is critical to identify and include stakeholders from multiple disciplines on your project team. This team will be essential to develop a practical project, identify barriers, create solutions, and gain buy-in from medical staff and administrative leadership.
Front-line staff will have invaluable insight and need to be team members. The majority of interventions are performed by nurses; therefore, nursing leadership and input is essential. Representatives from pharmacy, information technology, and the quality department will be extremely valuable team members to guide you through the correct approach to a successful QI project.
A project champion can keep a high profile for the project and build and lead the team.
Identify an “executive sponsor” such as your CEO, CMO, or CNO. This leader will focus the team on issues critical to your organization, such as accreditation from governmental agencies, and help you obtain dedicated time and resources. Aligning with hospital goals will make your project a priority.
Coordinate with existing opioid initiative teams in the hospital to integrate efforts. This will keep the work of different departments aligned and allow you to learn from pitfalls and barriers the other groups experienced.
Patients/families contribute a unique and valuable perspective. Consider including a member of your hospital’s patient and family advisory council on your team.
2. Perform a needs assessment
Determine the current state of your hospital including: opioid prescribers; opioids prescribed; areas with increased ADEs or naloxone use; formulary restrictions, policies, or guidelines for monitoring, prescribing, and administering opioids; order sets; safety alerts; provider education; or patient education.
Your risk management or quality department may be able to a share root cause analysis of ADEs related to opioids. Joint Commission and CMS recommendations as well as other regulatory requirements may shape your QI interventions.8
Most importantly, review all of the concerns and priorities of your diverse team, which will identify areas of most pressing need and provide insight regarding needs you have not considered.
3. Develop SMART aims
Frame your QI project into a series of well-defined, clear SMART aims.9
Specific: Who will carry out the intervention? Who is your target population? What will be improved? In what way will it be improved?
Measurable: What will be measured? How it will be measured? Does it measure the outcome that needs to be improved?
Attainable/achievable: Ensure you have the resources and time to achieve the aim.
Relevant: Ensure each aim moves your team toward the project vision.
Timely: The aim should be achieved within a realistic time frame, long enough to meet goals but not so long that interest is lost.
An example of a poor aim is “Clinicians will improve knowledge of opioids.”
An example of a SMART aim is “75% of inpatient opioid prescribers including MDs, NPs, and PAs will complete and pass the opioid safety training module by July 1, 2018.”
4. Choose metrics
Outcome metrics measure if the intervention has improved patient safety, for example, measuring a decrease in opioid related ADEs. Structure metrics are the physical and organizational properties of the health care delivery setting, for example, the presence of EMR opioid safety. Processes are communication and practice patterns, for example, adherence to policy by examining nursing documentation of pain assessments.
5. Development and implementation 7,10
Use PDSA for development and implementation of the QI intervention.
Plan: Determine the intervention group such as a specific unit, number of units, and if there will be a control group. Determine who will collect the data, if baseline data will be collected, and who will analyze the data. Your information technology department will be essential to determine if the data can be collected via the EMR and how. Input from your multidisciplinary team is critical to anticipate unintended consequences, such as limiting opioid prescribing at discharge inadvertently increasing emergency department visits for pain control.
Do: Start as a small pilot study to make it as easy as possible to implement the project and begin data collection. A small-scale intervention will be more manageable and allow rapid responses to unanticipated problems.
Study: Analyze the data early to determine if the intervention is improving opioid safety and if alterations are needed. At this stage both process metrics (are processes being followed?) and outcome metrics (is the process leading to a desired outcome?) are important.
Act: Based on data analysis, refine the intervention as necessary. You may have to repeat cycles of PDSA to develop the final intervention. Then implement the final intervention to the entire hospital.
The Joint Commission recommendations for opioid QI
The Joint Commission recommends7 the following to reduce opioid-related respiratory depression:
- Effective processes which include processes such as tracking and analyzing ADEs related to opioids.
- Safe technology which includes using technology such as the EMR to monitor opioid prescribing of greater than 90 morphine milligram equivalents.
- Effective tools which include valid and reliable tools to improve opioid safety, such as the Pasero Opioid Induced Sedation Scale (POSS).
- Opioid education and training which includes provider and patient education such as patient discharge education.
Education
Develop educational interventions to ensure medical and hospital staff are aware of new processes, with an emphasis on “why.”7 If possible, use web-based programs that provide CME. Improve education interventions by using multiple live, interactive, and multimedia exposures.
Principles for successful interventions
- Keep it simple for the end user. This makes it more likely that the intervention is performed. Minimize complex tasks such as calculations and if possible design automated processes.
- Build your process into current work flow. If possible simplify or streamline work flow. A project that competes with staff’s other tasks and competing priorities is doomed to fail. It is critical to have input from those performing the intervention to develop a user-friendly and less disruptive intervention.
- Design reliability into the process. Make your intervention the default action. Build prompts into the work flow. Standardize the intervention into the work flow. And, consider having the intervention at scheduled intervals.7
Opioid safety QI interventions
Interventions for improving opioid safety and reducing opioid -elated ADEs may be generalized into areas including risk screening and assessment, pain treatment, opioid administration, pain assessment, post opioid administration monitoring, and patient and provider education (Table 2).7
Back to the case
The patient received naloxone. His respiratory rate and oxygen saturation returned to normal. His dose of morphine was reduced and his interval increased. A multimodal approach was implemented including low-dose scheduled acetaminophen. There were no further ADEs while maintaining good pain control.
A multidisciplinary opioid task force was created and performed a hospital-wide review of opioid ADEs. Opportunities for improvement were identified and new procedures implemented. The Pasero opioid sedation scale (POSS) was added to the nursing work flow to monitor patients who received an opioid for sedation. An algorithm was developed for opioid-naive patients including guidance for opioid selection, dosing, and frequency. Multiple pain control modalities were added to pain control order sets. Annual training was developed for opioid prescribers, pharmacists, and nurses regarding safe and responsible use of opioids.
And, lastly, in-hospital and discharge patient education was developed for patients and families to be well-informed of opioid risk and benefit including how to identify and respond to ADEs.
Bottom line
Quality improvement is an effective method to improve patient safety and reduce serious adverse events related to opioids in the hospital setting.
Dr. Holmes-Maybank, is codirector, Fundamentals of Patient Care Year 1 and Internship 101, and chair, Clinical Competency Examination Committee, division of hospital medicine, Medical University of South Carolina. Dr. Frederickson is medical director, Hospital Medicine and Palliative Care at CHI Health, Omaha, Neb., and assistant professor at Creighton University School of Medicine, Omaha.
References
1. Davies EC et al. Adverse drug reactions in hospital inpatients: a prospective analysis of 3695 patient-episodes. PLoS One. 2009;4(2):e4439. doi: 10.1371/journal.pone.0004439. Epub 2009 Feb 11.
2. Association for the Advancement of Medical Instrumentation. Infusing patients safely: Priority issues from the AAMI/FDA Infusion Device Summit. 2010;1-39.
3. Dahan Aet al. Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology. 2010;112:226-238. doi: 10.1097/ALN.0b013e3181c38c25.
4. Estimate about opioid users.
5. Brummett CM et al. New persistent opioid use after minor and major surgical procedures in U.S. adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504.
6. Calcaterra SL et al. Opioid prescribing at hospital discharge contributes to chronic opioid use. J Gen Intern Med. 2016;31(5):478-85. doi: 10.1007/s11606-015-3539-4.
7. Frederickson TW et al. Reducing adverse drug events related to opioids implementation guide. Philadelphia: Society of Hospital Medicine, 2015.
8. Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
9. Minnesota Department of Health. SMART objectives.
10. Agency for Healthcare Research and Quality. Health Literacy Universal Precautions Toolkit, 2nd Edition.
Plan-Do-Study-Act (PDSA) Directions and Examples.
Recommended reading
Dowell D et al. CDC guideline for prescribing opioids for chronic pain – United States, 2016. Recommendations and Reports. 2016 Mar 18;65(1):1-49.
Frederickson TW et al. Using the 2018 guidelines from the Joint Commission to kickstart your hospital’s program to reduce opioid-induced ventilatory impairment. Anesthesia Patient Safety Foundation Newsletter. 2018;33(1):1-32.
Herzig SJ et al. Safe opioid prescribing for acute noncancer pain in hospitalized adults: a systematic review of existing guidelines. J Hosp Med. 2018 Apr;13(4):256-62. doi: 10.12788/jhm.2979.
Herzig SJ et al. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med. 2018 Apr;13(4):263-71. doi: 10.12788/jhm.2980.
Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
Key points
- Quality improvement is required by the Joint Commission and is an effective method to improve opioid safety in the hospital setting.
- It is critical to the success of a QI project to develop a multidisciplinary team.
- Input from frontline users of the intervention is essential to produce an effective intervention.
- Executive sponsorship and aligning the goals of your QI project with those of your institution will prioritize your project and increase resource availability.
Quiz
1. Based on a needs assessment at your hospital you assemble a multidisciplinary team to improve education for patients discharged on opioids. You recognize the importance of multidisciplinary input to develop a successful intervention for discharge education. Essential team members include all EXCEPT the following:
a. Executive sponsor
b. Patient representative
c. Nursing
d. Medical student representative ---- CORRECT
Explanation: The assembly of a multidisciplinary team is critical to the success of a QI intervention. An executive sponsor may assist you in aligning your goals with that of the hospital and provide resources for its development and implementation. Patient input would help determine how to best deliver the education. Lastly, the individuals carrying out the intervention are essential to develop an intervention that will easy for the end user and increase the likelihood of being used, in this case nursing.
2. You performed a review of naloxone use at your hospital and find that it is greater than similar hospitals. Prior to starting the QI project, you review SHM’s “Reducing adverse events related to opioids implementation guide” and learn that keys to success for QI implementation include:
a. A team of primarily hospitalists
b. Implementing the intervention hospital wide
c. Information technology input for data collection ---- CORRECT
d. No team – it is more effective to work alone
Explanation: Successful implementation of a QI project involves a multidisciplinary team. It is critical to involve information technology early in the development of the project to determine how and if the data can be collected from the EMR. It is best to pilot the intervention on one or two units to make alterations as needed rapidly and perfect the final intervention prior to rolling it out to the entire hospital.
3. You have assembled a multidisciplinary team to respond to the newly revised JCAHO pain standards. An example of a requirement from the new and revised JCAHO standards for pain assessment and management includes:
a. Programs for physician wellness
b. No opioids for chronic pain
c. No more than 5 days of opioids for acute pain
d. Nonpharmacologic pain management options ---- CORRECT
Explanation: JCAHO released new and revised requirements for pain assessment and management including offering nonpharmacologic pain management options. (See Table 1)
4. Your multidisciplinary QI team decides to develop a project to reduce respiratory depression in patients receiving opioids by monitoring for sedation with the Pasero Opioid Induced Sedation Scale. Principles for successful QI interventions include:
a. Complex tasks
b. Make the intervention a default action ---- CORRECT
c. Avoid EMR prompts
d. Competing with other hospital priorities
Explanation: Principles for successful QI interventions include keeping tasks simple, ensuring the intervention does not compete with other priorities, making the intervention the default action, installing prompts in the EMR, and standardizing the intervention into the work flow.
Case
A 67-year-old opioid-naive male with a history of obstructive sleep apnea and chronic kidney disease became unresponsive 2 days after hip replacement. Physical exam revealed a respiratory rate of 6 breaths/minute and oxygen saturation of 82%. He had received 6 doses of 6-mg IV morphine within the past 7 hours. How can I improve opioid safety at my hospital?
Background
Opioids are the most commonly prescribed class of medication in the hospital and the second–most common class causing adverse drug events (ADEs), the most serious being respiratory depression and death.1
Opioid ADEs and side effects can cause prolonged length of stay and patient suffering. These vary from potentially life-threatening events such as serotonin syndrome and adrenal insufficiency to more manageable problems still requiring intervention such as constipation, urinary retention, cognitive impairment, nausea, and vomiting. Treatment of side effects can lead to complications, including side effects from antiemetics and urinary tract infections from catheters.
A 4-year review found 700 deaths in the United States attributed to patient-controlled analgesia (PCA) use.2 Another study revealed that one out of every 200 patients has postoperative respiratory depression attributable to opioids.3
It is estimated that 2 million patients a year become chronic opioid users. Inpatient opioid prescribing contributes to this problem;4 for instance, 5.9% of patients after minor surgery and 6.5% after major surgery become chronic opioid users if discharged with an opioid.5 Calcaterra et al. found 25% of opioid-naive medical patients received an opioid at discharge from a medical service.6 Those patients had an odds ratio of 4.90 for becoming a chronic opioid user that year.6
Most hospitals have incomplete or outdated policies and procedures for safe opioid prescribing and administration.7 The Joint Commission on Accreditation of Healthcare Organizations has specific pain standards for pain assessment, pain management, and safe opioid prescribing for hospitals. Additions and revisions were developed to go into effect Jan. 1, 2018. (Table 1)8
Quality improvement
Quality improvement (QI) is an effective way to improve opioid safety. The Society of Hospital Medicine has developed a QI guide, “Reducing adverse drug events related to opioids” or “RADEO,” to increase safety and decrease serious ADEs attributable to opioids.7
The steps in the RADEO program are as follows:
1. Assemble your team
It is critical to identify and include stakeholders from multiple disciplines on your project team. This team will be essential to develop a practical project, identify barriers, create solutions, and gain buy-in from medical staff and administrative leadership.
Front-line staff will have invaluable insight and need to be team members. The majority of interventions are performed by nurses; therefore, nursing leadership and input is essential. Representatives from pharmacy, information technology, and the quality department will be extremely valuable team members to guide you through the correct approach to a successful QI project.
A project champion can keep a high profile for the project and build and lead the team.
Identify an “executive sponsor” such as your CEO, CMO, or CNO. This leader will focus the team on issues critical to your organization, such as accreditation from governmental agencies, and help you obtain dedicated time and resources. Aligning with hospital goals will make your project a priority.
Coordinate with existing opioid initiative teams in the hospital to integrate efforts. This will keep the work of different departments aligned and allow you to learn from pitfalls and barriers the other groups experienced.
Patients/families contribute a unique and valuable perspective. Consider including a member of your hospital’s patient and family advisory council on your team.
2. Perform a needs assessment
Determine the current state of your hospital including: opioid prescribers; opioids prescribed; areas with increased ADEs or naloxone use; formulary restrictions, policies, or guidelines for monitoring, prescribing, and administering opioids; order sets; safety alerts; provider education; or patient education.
Your risk management or quality department may be able to a share root cause analysis of ADEs related to opioids. Joint Commission and CMS recommendations as well as other regulatory requirements may shape your QI interventions.8
Most importantly, review all of the concerns and priorities of your diverse team, which will identify areas of most pressing need and provide insight regarding needs you have not considered.
3. Develop SMART aims
Frame your QI project into a series of well-defined, clear SMART aims.9
Specific: Who will carry out the intervention? Who is your target population? What will be improved? In what way will it be improved?
Measurable: What will be measured? How it will be measured? Does it measure the outcome that needs to be improved?
Attainable/achievable: Ensure you have the resources and time to achieve the aim.
Relevant: Ensure each aim moves your team toward the project vision.
Timely: The aim should be achieved within a realistic time frame, long enough to meet goals but not so long that interest is lost.
An example of a poor aim is “Clinicians will improve knowledge of opioids.”
An example of a SMART aim is “75% of inpatient opioid prescribers including MDs, NPs, and PAs will complete and pass the opioid safety training module by July 1, 2018.”
4. Choose metrics
Outcome metrics measure if the intervention has improved patient safety, for example, measuring a decrease in opioid related ADEs. Structure metrics are the physical and organizational properties of the health care delivery setting, for example, the presence of EMR opioid safety. Processes are communication and practice patterns, for example, adherence to policy by examining nursing documentation of pain assessments.
5. Development and implementation 7,10
Use PDSA for development and implementation of the QI intervention.
Plan: Determine the intervention group such as a specific unit, number of units, and if there will be a control group. Determine who will collect the data, if baseline data will be collected, and who will analyze the data. Your information technology department will be essential to determine if the data can be collected via the EMR and how. Input from your multidisciplinary team is critical to anticipate unintended consequences, such as limiting opioid prescribing at discharge inadvertently increasing emergency department visits for pain control.
Do: Start as a small pilot study to make it as easy as possible to implement the project and begin data collection. A small-scale intervention will be more manageable and allow rapid responses to unanticipated problems.
Study: Analyze the data early to determine if the intervention is improving opioid safety and if alterations are needed. At this stage both process metrics (are processes being followed?) and outcome metrics (is the process leading to a desired outcome?) are important.
Act: Based on data analysis, refine the intervention as necessary. You may have to repeat cycles of PDSA to develop the final intervention. Then implement the final intervention to the entire hospital.
The Joint Commission recommendations for opioid QI
The Joint Commission recommends7 the following to reduce opioid-related respiratory depression:
- Effective processes which include processes such as tracking and analyzing ADEs related to opioids.
- Safe technology which includes using technology such as the EMR to monitor opioid prescribing of greater than 90 morphine milligram equivalents.
- Effective tools which include valid and reliable tools to improve opioid safety, such as the Pasero Opioid Induced Sedation Scale (POSS).
- Opioid education and training which includes provider and patient education such as patient discharge education.
Education
Develop educational interventions to ensure medical and hospital staff are aware of new processes, with an emphasis on “why.”7 If possible, use web-based programs that provide CME. Improve education interventions by using multiple live, interactive, and multimedia exposures.
Principles for successful interventions
- Keep it simple for the end user. This makes it more likely that the intervention is performed. Minimize complex tasks such as calculations and if possible design automated processes.
- Build your process into current work flow. If possible simplify or streamline work flow. A project that competes with staff’s other tasks and competing priorities is doomed to fail. It is critical to have input from those performing the intervention to develop a user-friendly and less disruptive intervention.
- Design reliability into the process. Make your intervention the default action. Build prompts into the work flow. Standardize the intervention into the work flow. And, consider having the intervention at scheduled intervals.7
Opioid safety QI interventions
Interventions for improving opioid safety and reducing opioid -elated ADEs may be generalized into areas including risk screening and assessment, pain treatment, opioid administration, pain assessment, post opioid administration monitoring, and patient and provider education (Table 2).7
Back to the case
The patient received naloxone. His respiratory rate and oxygen saturation returned to normal. His dose of morphine was reduced and his interval increased. A multimodal approach was implemented including low-dose scheduled acetaminophen. There were no further ADEs while maintaining good pain control.
A multidisciplinary opioid task force was created and performed a hospital-wide review of opioid ADEs. Opportunities for improvement were identified and new procedures implemented. The Pasero opioid sedation scale (POSS) was added to the nursing work flow to monitor patients who received an opioid for sedation. An algorithm was developed for opioid-naive patients including guidance for opioid selection, dosing, and frequency. Multiple pain control modalities were added to pain control order sets. Annual training was developed for opioid prescribers, pharmacists, and nurses regarding safe and responsible use of opioids.
And, lastly, in-hospital and discharge patient education was developed for patients and families to be well-informed of opioid risk and benefit including how to identify and respond to ADEs.
Bottom line
Quality improvement is an effective method to improve patient safety and reduce serious adverse events related to opioids in the hospital setting.
Dr. Holmes-Maybank, is codirector, Fundamentals of Patient Care Year 1 and Internship 101, and chair, Clinical Competency Examination Committee, division of hospital medicine, Medical University of South Carolina. Dr. Frederickson is medical director, Hospital Medicine and Palliative Care at CHI Health, Omaha, Neb., and assistant professor at Creighton University School of Medicine, Omaha.
References
1. Davies EC et al. Adverse drug reactions in hospital inpatients: a prospective analysis of 3695 patient-episodes. PLoS One. 2009;4(2):e4439. doi: 10.1371/journal.pone.0004439. Epub 2009 Feb 11.
2. Association for the Advancement of Medical Instrumentation. Infusing patients safely: Priority issues from the AAMI/FDA Infusion Device Summit. 2010;1-39.
3. Dahan Aet al. Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology. 2010;112:226-238. doi: 10.1097/ALN.0b013e3181c38c25.
4. Estimate about opioid users.
5. Brummett CM et al. New persistent opioid use after minor and major surgical procedures in U.S. adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504.
6. Calcaterra SL et al. Opioid prescribing at hospital discharge contributes to chronic opioid use. J Gen Intern Med. 2016;31(5):478-85. doi: 10.1007/s11606-015-3539-4.
7. Frederickson TW et al. Reducing adverse drug events related to opioids implementation guide. Philadelphia: Society of Hospital Medicine, 2015.
8. Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
9. Minnesota Department of Health. SMART objectives.
10. Agency for Healthcare Research and Quality. Health Literacy Universal Precautions Toolkit, 2nd Edition.
Plan-Do-Study-Act (PDSA) Directions and Examples.
Recommended reading
Dowell D et al. CDC guideline for prescribing opioids for chronic pain – United States, 2016. Recommendations and Reports. 2016 Mar 18;65(1):1-49.
Frederickson TW et al. Using the 2018 guidelines from the Joint Commission to kickstart your hospital’s program to reduce opioid-induced ventilatory impairment. Anesthesia Patient Safety Foundation Newsletter. 2018;33(1):1-32.
Herzig SJ et al. Safe opioid prescribing for acute noncancer pain in hospitalized adults: a systematic review of existing guidelines. J Hosp Med. 2018 Apr;13(4):256-62. doi: 10.12788/jhm.2979.
Herzig SJ et al. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med. 2018 Apr;13(4):263-71. doi: 10.12788/jhm.2980.
Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
Key points
- Quality improvement is required by the Joint Commission and is an effective method to improve opioid safety in the hospital setting.
- It is critical to the success of a QI project to develop a multidisciplinary team.
- Input from frontline users of the intervention is essential to produce an effective intervention.
- Executive sponsorship and aligning the goals of your QI project with those of your institution will prioritize your project and increase resource availability.
Quiz
1. Based on a needs assessment at your hospital you assemble a multidisciplinary team to improve education for patients discharged on opioids. You recognize the importance of multidisciplinary input to develop a successful intervention for discharge education. Essential team members include all EXCEPT the following:
a. Executive sponsor
b. Patient representative
c. Nursing
d. Medical student representative ---- CORRECT
Explanation: The assembly of a multidisciplinary team is critical to the success of a QI intervention. An executive sponsor may assist you in aligning your goals with that of the hospital and provide resources for its development and implementation. Patient input would help determine how to best deliver the education. Lastly, the individuals carrying out the intervention are essential to develop an intervention that will easy for the end user and increase the likelihood of being used, in this case nursing.
2. You performed a review of naloxone use at your hospital and find that it is greater than similar hospitals. Prior to starting the QI project, you review SHM’s “Reducing adverse events related to opioids implementation guide” and learn that keys to success for QI implementation include:
a. A team of primarily hospitalists
b. Implementing the intervention hospital wide
c. Information technology input for data collection ---- CORRECT
d. No team – it is more effective to work alone
Explanation: Successful implementation of a QI project involves a multidisciplinary team. It is critical to involve information technology early in the development of the project to determine how and if the data can be collected from the EMR. It is best to pilot the intervention on one or two units to make alterations as needed rapidly and perfect the final intervention prior to rolling it out to the entire hospital.
3. You have assembled a multidisciplinary team to respond to the newly revised JCAHO pain standards. An example of a requirement from the new and revised JCAHO standards for pain assessment and management includes:
a. Programs for physician wellness
b. No opioids for chronic pain
c. No more than 5 days of opioids for acute pain
d. Nonpharmacologic pain management options ---- CORRECT
Explanation: JCAHO released new and revised requirements for pain assessment and management including offering nonpharmacologic pain management options. (See Table 1)
4. Your multidisciplinary QI team decides to develop a project to reduce respiratory depression in patients receiving opioids by monitoring for sedation with the Pasero Opioid Induced Sedation Scale. Principles for successful QI interventions include:
a. Complex tasks
b. Make the intervention a default action ---- CORRECT
c. Avoid EMR prompts
d. Competing with other hospital priorities
Explanation: Principles for successful QI interventions include keeping tasks simple, ensuring the intervention does not compete with other priorities, making the intervention the default action, installing prompts in the EMR, and standardizing the intervention into the work flow.