User login
Clinical hypnosis for reduction of atrial fibrillation after coronary artery bypass graft surgery
Postoperative atrial fibrillation (PAF) is the most common complication of coronary artery bypass graft surgery (CABG), affecting approximately 20% to 40% of patients undergoing this procedure.1 Occurrence of PAF has been associated with prolonged hospital and intensive care unit (ICU) stays, a decline in neurocognitive ability, an increased risk of stroke and transient ischemic attacks, increased surgical mortality, and increased resource utilization and cost.2
The role of the autonomic nervous system in atrial fibrillation (AF) has been studied extensively, but the impact of the autonomic nervous system on PAF has received little attention. Research on the mechanisms of AF has shown imbalance in the autonomic nervous system when measured using heart rate variability. These studies have demonstrated an increase in sympathetic activity approximately 20 minutes prior to the onset of AF, with a shift to parasympathetic activity directly prior to onset. A correlation between mental stress and changes in the autonomic nervous system, as assessed by heart rate variability, has also been shown.3–7
Pharmacologic interventions, including beta-blockers and amiodarone, have been proposed as preventive measures for PAF, but the incidence of PAF remains high.1 Beta-blockade may not be tolerated by patients postoperatively, and there is no consensus on dosing parameters. A meta-analysis on the use of amiodarone in the prevention of PAF was inconclusive,8 and the optimal dosing regimen and incidence of adverse events with amiodarone have not been determined.
There are a small number of studies linking clinical hypnosis to changes in the autonomic nervous system.9 Clinical hypnosis also has been associated with reductions in anxiety and depression before and after surgical procedures.10,11 If PAF is a result of transient autonomic dysfunction, then interventions that alter autonomic tone should influence the incidence and duration of PAF. We report here a retrospective analysis of the impact of clinical hypnosis on the occurrence of PAF in patients undergoing CABG.
METHODOLOGY
Fifty consecutive patients undergoing first-time CABG between October 2004 and May 2005 received preoperative hypnoidal explanation of the surgical procedure as part of their preparation for surgery. A group of 50 case-matched patients who had undergone CABG at the same center between October 2003 and May 2004 were chosen as historical controls.
The treatment group (hypnosis group) and the control group were case-matched for presence of diabetes mellitus, use of beta-adrenergic blocking agents, and use of antiarrhythmic medications. The groups were also matched for various predictors of postoperative PAF, such as age, gender, and coronary artery disease. The patients were all treated by the same surgeon (R.N.), with no significant alterations to surgical or pharmacologic protocols.
The surgeon used indirect Ericksonian techniques during the preoperative explanation of the surgery. Milton Erickson, one of the most prominent hypnotherapists in recent times, used an indirect approach to weave suggestions into the dialogue rather than giving direct commands. This approach encourages active participation and gives the patient a sense of greater control in the hospital environment. The surgeon also instructed patients in self-hypnosis using respiration and imagery.
RESULTS
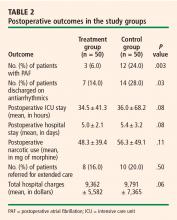
Table 2 presents outcomes in the two study groups. Patients who were treated with clinical hypnosis were less likely to experience PAF: the percentage of patients with one or more episodes of PAF was 6.0% in the treatment group versus 24.0% in the control group (P = .003). Likewise, the percentage of patients who were discharged on amiodarone was 14.0% in the treatment group versus 28.0% in the control group (P = .03).
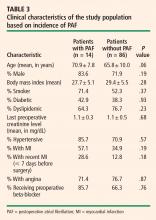
Clinical characteristics were tabulated and compared between the subjects who experienced new-onset PAF and those who did not experience PAF to determine whether there was a covariate responsible for the results observed. With the exception of age, the difference in clinical characteristics between these groups of patients was not statistically significant (using P > .10 as the threshold for significance) (Table 3).
DISCUSSION
Adverse effects of PAF are well established
The onset of PAF following CABG is a common complication that has been linked to increases in morbidity and mortality, length of stay in the ICU and hospital, and total hospital charges. Villareal et al found that the odds ratio for early mortality (within 30 days) for patients who experienced PAF after CABG was 1.4 (95% confidence interval, 1.12 to 1.68; P = .002).12 In addition, patients with PAF had significantly higher rates of postoperative infections, renal failure, shock, failure of multiple organ systems, and cardiac arrest compared with those who did not have PAF.12 A literature analysis by Maisel et al found that PAF increases the likelihood that cardiac surgery patients will need to return to the operating room, be readmitted to the ICU, and require prolonged ventilation or reintubation.13 Nickerson et al showed that PAF following cardiac surgery corresponded with an increase in length of stay in both the ICU and hospital.14
Our study showed statistically significant increases in postoperative hospital charges, postoperative hospital stay, and ICU stay among patients who experienced PAF following CABG. These findings are consistent with the current literature. In a study of 720 subjects undergoing CABG, Hravnak et al reported a 1.4-day increase in length of hospital stay and a 0.3day increase in length of ICU stay among patients who had PAF compared with those who did not.15 A significant increase in postoperative hospital charges was also observed.15 Similarly, in a multicenter study of 2,417 patients undergoing isolated CABG procedures, Mathew et al observed increases in ICU stay and hospital stay among those patients who experienced PAF.2 These findings indicate that the onset of PAF after CABG is a serious complication and that further study is warranted.
Hypnosis to prevent PAF: Suggestive evidence and mechanisms
Clinical hypnosis has been shown to reduce stress and anxiety in surgical patients and can be highly individualized to address the patient’s needs during the stressful preoperative period. Saadat et al found that hypnosis administered directly before ambulatory surgery using Ericksonian techniques reduced patients’ levels of anxiety by 56% from baseline.11 In a South African study specifically in men undergoing CABG, de Klerk et al found that preoperative hypnotherapy led to reductions in both anxiety and depression at discharge that were maintained through 6-week follow-up.10
These findings, taken together with research linking clinical hypnosis to changes in the autonomic nervous system9 and the belief that PAF may result from transient autonomic dysfunction, suggest that hypnosis may reduce the incidence of PAF.
In a study of R-R interval dynamics prior to PAF in patients who had undergone CABG, Hogue et al showed that patients who experienced PAF had higher heart rates directly before PAF onset.16 Higher heart rates are associated with increased activity of the sympathetic nervous system and/or decreased activity of the parasympathetic nervous system. This finding supports our hypothesis of a relationship between PAF following CABG and excessive adrenergic activation. Chen et al have noted that catecholamine-mediated AF usually occurs in the presence of heart disease and that these types of attacks often happen during the daytime in association with physical or emotional stress.4
Bettoni and Zimmermann found that the onset of AF is preceded by a primary increase in adrenergic drive, which changes to increased vagal activity immediately before the occurrence.3 Tomita et al reported that sympathetic tone increases immediately before an occurrence of daytime AF.7 These results were supported by Lombardi et al, who detected signs of predominant sympathetic modulation and reduced vagal modulation of sinus node in AF episodes that started during the daytime.6 These episodes were characterized by atrial ectopic beats prior to onset.6
Modulations in baroreceptor reflex activity may provide further evidence of the importance of the sympathetic/parasympathetic balance in the initiation of AF. Suboptimal functioning of the baroreceptor reflex has been associated with arrhythmias and adverse cardiac events in patients and animal models. Loss of the protective effects of vagal activation has been postulated to increase vulnerability to sympathetically driven ischemia and malignant arrhythmias.17
Multiple studies have shown that the only conclusive predictor of PAF is age. Notably, heart rate variability is reduced with increased age.18 By measuring heart rate variability, Taggart et al showed that autonomic balance was improved in patients under induced stress when they were in a hypnotic state.19 Although no attempts were made to determine heart rate variability in our patient set, other studies have demonstrated an increase in heart rate variability during hypnosis. The results of our study suggest that clinical hypnosis using a personalized Ericksonian approach may have a beneficial effect on the incidence of PAF.
CONCLUSIONS
Clinical hypnosis appears to lower the incidence of PAF in patients undergoing CABG as well as to yield favorable trends toward reduced ICU and postoperative hospital stays, reduced hospital charges, and reduced use of narcotics. Although our study had a small sample size and lacked randomization, its positive results and the absence of side effects suggest that prospective randomized trials should be conducted to further delineate the role of hypnosis in the prevention of PAF. A better understanding of AF, and of the autonomic nervous system’s role in triggering and maintaining PAF, will allow more appropriate treatment of this condition.
- Halonen J, Hakala T, Auvinen T, et al. Intravenous administration of metoprolol is more effective than oral administration in the prevention of atrial fibrillation after cardiac surgery. Circulation 2006; 114(1 Suppl):I1–I4.
- Mathew JP, Parks R, Savino JS, et al. Atrial fibrillation following coronary artery bypass graft surgery: predictors, outcomes, and resource utilization. MultiCenter Study of Perioperative Ischemia Research Group. JAMA 1996; 276:300–306.
- Bettoni M, Zimmermann M. Autonomic tone variations before the onset of paroxysmal atrial fibrillation. Circulation 2002; 105:2753–2759.
- Chen J, Wasmund SL, Hamdan MH. Back to the future: the role of the autonomic nervous system in atrial fibrillation. Pacing Clin Electrophysiol 2006; 29:413–421.
- Hogue CW Jr, Creswell LL, Gutterman DD, Fleisher LA; American College of Chest Physicians. Epidemiology, mechanisms, and risks: American College of Chest Physicians guidelines for the prevention and management of postoperative atrial fibrillation after cardiac surgery. Chest 2005; 128(2 Suppl):9S–16S.
- Lombardi F, Tarricone D, Tundo F, Colombo F, Belletti S, Fiorentini C. Autonomic nervous system and paroxysmal atrial fibrillation: a study based on the analysis of RR interval changes before, during and after paroxysmal atrial fibrillation. Eur Heart J 2004; 25:1242–1248.
- Tomita T, Takei M, Saikawa Y, et al. Role of autonomic tone in the initiation and termination of paroxysmal atrial fibrillation in patients without structural heart disease. J Cardiovasc Electrophysiol 2003; 14:559–564.
- Aasbo JD, Lawrence AT, Krishnan K, Kim MH, Trohman RG. Amiodarone prophylaxis reduces major cardiovascular morbidity and length of stay after cardiac surgery: a meta-analysis. Ann Intern Med 2005; 143:327–336.
- Hippel CV, Hole G, Kaschka WP. Autonomic profile under hypnosis as assessed by heart rate variability and spectral analysis. Pharmacopsychiatry 2001; 34:111–113.
- de Klerk JE, du Plessis WF, Steyn HS, Botha M. Hypnotherapeutic ego strengthening with male South African coronary artery bypass patients. Am J Clin Hypn 2004; 47:79–92.
- Saadat H, Drummond-Lewis J, Maranets I, et al. Hypnosis reduces preoperative anxiety in adult patients. Anesth Analg 2006; 102:1394–1396.
- Villareal RP, Hariharan R, Liu BC, et al. Postoperative atrial fibrillation and mortality after coronary artery bypass surgery. J Am Coll Cardiol 2004; 43:742–748.
- Maisel WH, Rawn JD, Stevenson WG. Atrial fibrillation after cardiac surgery. Ann Intern Med 2001; 135:1061–1073.
- Nickerson NJ, Murphy SF, Dávila-Román VG, Schechtman KB, Kouchoukos NT. Obstacles to early discharge after cardiac surgery. Am J Manag Care 1999; 5:29–34.
- Hravnak M, Hoffman LA, Saul MI, et al. Resource utilization related to atrial fibrillation after coronary artery bypass grafting. Am J Crit Care 2002; 11:228–238.
- Hogue CW Jr, Domitrovich PP, Stein PK, et al. RR interval dynamics before atrial fibrillation in patients after coronary artery bypass graft surgery. Circulation 1998; 98:429–434.
- Olshansky B. Interrelationships between the autonomic nervous system and atrial fibrillation. Prog Cardiovasc Dis 2005; 48:57–78.
- Zhang J. Effect of age and sex on heart rate variability in healthy subjects. J Manipulative Physiol Ther 2007; 30:374–379.
- Taggart P, Sutton P, Redfern C, et al. The effect of mental stress on the non-dipolar components of the T wave: modulation by hypnosis. Psychosom Med 2005; 67:376–383.
Postoperative atrial fibrillation (PAF) is the most common complication of coronary artery bypass graft surgery (CABG), affecting approximately 20% to 40% of patients undergoing this procedure.1 Occurrence of PAF has been associated with prolonged hospital and intensive care unit (ICU) stays, a decline in neurocognitive ability, an increased risk of stroke and transient ischemic attacks, increased surgical mortality, and increased resource utilization and cost.2
The role of the autonomic nervous system in atrial fibrillation (AF) has been studied extensively, but the impact of the autonomic nervous system on PAF has received little attention. Research on the mechanisms of AF has shown imbalance in the autonomic nervous system when measured using heart rate variability. These studies have demonstrated an increase in sympathetic activity approximately 20 minutes prior to the onset of AF, with a shift to parasympathetic activity directly prior to onset. A correlation between mental stress and changes in the autonomic nervous system, as assessed by heart rate variability, has also been shown.3–7
Pharmacologic interventions, including beta-blockers and amiodarone, have been proposed as preventive measures for PAF, but the incidence of PAF remains high.1 Beta-blockade may not be tolerated by patients postoperatively, and there is no consensus on dosing parameters. A meta-analysis on the use of amiodarone in the prevention of PAF was inconclusive,8 and the optimal dosing regimen and incidence of adverse events with amiodarone have not been determined.
There are a small number of studies linking clinical hypnosis to changes in the autonomic nervous system.9 Clinical hypnosis also has been associated with reductions in anxiety and depression before and after surgical procedures.10,11 If PAF is a result of transient autonomic dysfunction, then interventions that alter autonomic tone should influence the incidence and duration of PAF. We report here a retrospective analysis of the impact of clinical hypnosis on the occurrence of PAF in patients undergoing CABG.
METHODOLOGY
Fifty consecutive patients undergoing first-time CABG between October 2004 and May 2005 received preoperative hypnoidal explanation of the surgical procedure as part of their preparation for surgery. A group of 50 case-matched patients who had undergone CABG at the same center between October 2003 and May 2004 were chosen as historical controls.
The treatment group (hypnosis group) and the control group were case-matched for presence of diabetes mellitus, use of beta-adrenergic blocking agents, and use of antiarrhythmic medications. The groups were also matched for various predictors of postoperative PAF, such as age, gender, and coronary artery disease. The patients were all treated by the same surgeon (R.N.), with no significant alterations to surgical or pharmacologic protocols.
The surgeon used indirect Ericksonian techniques during the preoperative explanation of the surgery. Milton Erickson, one of the most prominent hypnotherapists in recent times, used an indirect approach to weave suggestions into the dialogue rather than giving direct commands. This approach encourages active participation and gives the patient a sense of greater control in the hospital environment. The surgeon also instructed patients in self-hypnosis using respiration and imagery.
RESULTS
Table 2 presents outcomes in the two study groups. Patients who were treated with clinical hypnosis were less likely to experience PAF: the percentage of patients with one or more episodes of PAF was 6.0% in the treatment group versus 24.0% in the control group (P = .003). Likewise, the percentage of patients who were discharged on amiodarone was 14.0% in the treatment group versus 28.0% in the control group (P = .03).
Clinical characteristics were tabulated and compared between the subjects who experienced new-onset PAF and those who did not experience PAF to determine whether there was a covariate responsible for the results observed. With the exception of age, the difference in clinical characteristics between these groups of patients was not statistically significant (using P > .10 as the threshold for significance) (Table 3).
DISCUSSION
Adverse effects of PAF are well established
The onset of PAF following CABG is a common complication that has been linked to increases in morbidity and mortality, length of stay in the ICU and hospital, and total hospital charges. Villareal et al found that the odds ratio for early mortality (within 30 days) for patients who experienced PAF after CABG was 1.4 (95% confidence interval, 1.12 to 1.68; P = .002).12 In addition, patients with PAF had significantly higher rates of postoperative infections, renal failure, shock, failure of multiple organ systems, and cardiac arrest compared with those who did not have PAF.12 A literature analysis by Maisel et al found that PAF increases the likelihood that cardiac surgery patients will need to return to the operating room, be readmitted to the ICU, and require prolonged ventilation or reintubation.13 Nickerson et al showed that PAF following cardiac surgery corresponded with an increase in length of stay in both the ICU and hospital.14
Our study showed statistically significant increases in postoperative hospital charges, postoperative hospital stay, and ICU stay among patients who experienced PAF following CABG. These findings are consistent with the current literature. In a study of 720 subjects undergoing CABG, Hravnak et al reported a 1.4-day increase in length of hospital stay and a 0.3day increase in length of ICU stay among patients who had PAF compared with those who did not.15 A significant increase in postoperative hospital charges was also observed.15 Similarly, in a multicenter study of 2,417 patients undergoing isolated CABG procedures, Mathew et al observed increases in ICU stay and hospital stay among those patients who experienced PAF.2 These findings indicate that the onset of PAF after CABG is a serious complication and that further study is warranted.
Hypnosis to prevent PAF: Suggestive evidence and mechanisms
Clinical hypnosis has been shown to reduce stress and anxiety in surgical patients and can be highly individualized to address the patient’s needs during the stressful preoperative period. Saadat et al found that hypnosis administered directly before ambulatory surgery using Ericksonian techniques reduced patients’ levels of anxiety by 56% from baseline.11 In a South African study specifically in men undergoing CABG, de Klerk et al found that preoperative hypnotherapy led to reductions in both anxiety and depression at discharge that were maintained through 6-week follow-up.10
These findings, taken together with research linking clinical hypnosis to changes in the autonomic nervous system9 and the belief that PAF may result from transient autonomic dysfunction, suggest that hypnosis may reduce the incidence of PAF.
In a study of R-R interval dynamics prior to PAF in patients who had undergone CABG, Hogue et al showed that patients who experienced PAF had higher heart rates directly before PAF onset.16 Higher heart rates are associated with increased activity of the sympathetic nervous system and/or decreased activity of the parasympathetic nervous system. This finding supports our hypothesis of a relationship between PAF following CABG and excessive adrenergic activation. Chen et al have noted that catecholamine-mediated AF usually occurs in the presence of heart disease and that these types of attacks often happen during the daytime in association with physical or emotional stress.4
Bettoni and Zimmermann found that the onset of AF is preceded by a primary increase in adrenergic drive, which changes to increased vagal activity immediately before the occurrence.3 Tomita et al reported that sympathetic tone increases immediately before an occurrence of daytime AF.7 These results were supported by Lombardi et al, who detected signs of predominant sympathetic modulation and reduced vagal modulation of sinus node in AF episodes that started during the daytime.6 These episodes were characterized by atrial ectopic beats prior to onset.6
Modulations in baroreceptor reflex activity may provide further evidence of the importance of the sympathetic/parasympathetic balance in the initiation of AF. Suboptimal functioning of the baroreceptor reflex has been associated with arrhythmias and adverse cardiac events in patients and animal models. Loss of the protective effects of vagal activation has been postulated to increase vulnerability to sympathetically driven ischemia and malignant arrhythmias.17
Multiple studies have shown that the only conclusive predictor of PAF is age. Notably, heart rate variability is reduced with increased age.18 By measuring heart rate variability, Taggart et al showed that autonomic balance was improved in patients under induced stress when they were in a hypnotic state.19 Although no attempts were made to determine heart rate variability in our patient set, other studies have demonstrated an increase in heart rate variability during hypnosis. The results of our study suggest that clinical hypnosis using a personalized Ericksonian approach may have a beneficial effect on the incidence of PAF.
CONCLUSIONS
Clinical hypnosis appears to lower the incidence of PAF in patients undergoing CABG as well as to yield favorable trends toward reduced ICU and postoperative hospital stays, reduced hospital charges, and reduced use of narcotics. Although our study had a small sample size and lacked randomization, its positive results and the absence of side effects suggest that prospective randomized trials should be conducted to further delineate the role of hypnosis in the prevention of PAF. A better understanding of AF, and of the autonomic nervous system’s role in triggering and maintaining PAF, will allow more appropriate treatment of this condition.
Postoperative atrial fibrillation (PAF) is the most common complication of coronary artery bypass graft surgery (CABG), affecting approximately 20% to 40% of patients undergoing this procedure.1 Occurrence of PAF has been associated with prolonged hospital and intensive care unit (ICU) stays, a decline in neurocognitive ability, an increased risk of stroke and transient ischemic attacks, increased surgical mortality, and increased resource utilization and cost.2
The role of the autonomic nervous system in atrial fibrillation (AF) has been studied extensively, but the impact of the autonomic nervous system on PAF has received little attention. Research on the mechanisms of AF has shown imbalance in the autonomic nervous system when measured using heart rate variability. These studies have demonstrated an increase in sympathetic activity approximately 20 minutes prior to the onset of AF, with a shift to parasympathetic activity directly prior to onset. A correlation between mental stress and changes in the autonomic nervous system, as assessed by heart rate variability, has also been shown.3–7
Pharmacologic interventions, including beta-blockers and amiodarone, have been proposed as preventive measures for PAF, but the incidence of PAF remains high.1 Beta-blockade may not be tolerated by patients postoperatively, and there is no consensus on dosing parameters. A meta-analysis on the use of amiodarone in the prevention of PAF was inconclusive,8 and the optimal dosing regimen and incidence of adverse events with amiodarone have not been determined.
There are a small number of studies linking clinical hypnosis to changes in the autonomic nervous system.9 Clinical hypnosis also has been associated with reductions in anxiety and depression before and after surgical procedures.10,11 If PAF is a result of transient autonomic dysfunction, then interventions that alter autonomic tone should influence the incidence and duration of PAF. We report here a retrospective analysis of the impact of clinical hypnosis on the occurrence of PAF in patients undergoing CABG.
METHODOLOGY
Fifty consecutive patients undergoing first-time CABG between October 2004 and May 2005 received preoperative hypnoidal explanation of the surgical procedure as part of their preparation for surgery. A group of 50 case-matched patients who had undergone CABG at the same center between October 2003 and May 2004 were chosen as historical controls.
The treatment group (hypnosis group) and the control group were case-matched for presence of diabetes mellitus, use of beta-adrenergic blocking agents, and use of antiarrhythmic medications. The groups were also matched for various predictors of postoperative PAF, such as age, gender, and coronary artery disease. The patients were all treated by the same surgeon (R.N.), with no significant alterations to surgical or pharmacologic protocols.
The surgeon used indirect Ericksonian techniques during the preoperative explanation of the surgery. Milton Erickson, one of the most prominent hypnotherapists in recent times, used an indirect approach to weave suggestions into the dialogue rather than giving direct commands. This approach encourages active participation and gives the patient a sense of greater control in the hospital environment. The surgeon also instructed patients in self-hypnosis using respiration and imagery.
RESULTS
Table 2 presents outcomes in the two study groups. Patients who were treated with clinical hypnosis were less likely to experience PAF: the percentage of patients with one or more episodes of PAF was 6.0% in the treatment group versus 24.0% in the control group (P = .003). Likewise, the percentage of patients who were discharged on amiodarone was 14.0% in the treatment group versus 28.0% in the control group (P = .03).
Clinical characteristics were tabulated and compared between the subjects who experienced new-onset PAF and those who did not experience PAF to determine whether there was a covariate responsible for the results observed. With the exception of age, the difference in clinical characteristics between these groups of patients was not statistically significant (using P > .10 as the threshold for significance) (Table 3).
DISCUSSION
Adverse effects of PAF are well established
The onset of PAF following CABG is a common complication that has been linked to increases in morbidity and mortality, length of stay in the ICU and hospital, and total hospital charges. Villareal et al found that the odds ratio for early mortality (within 30 days) for patients who experienced PAF after CABG was 1.4 (95% confidence interval, 1.12 to 1.68; P = .002).12 In addition, patients with PAF had significantly higher rates of postoperative infections, renal failure, shock, failure of multiple organ systems, and cardiac arrest compared with those who did not have PAF.12 A literature analysis by Maisel et al found that PAF increases the likelihood that cardiac surgery patients will need to return to the operating room, be readmitted to the ICU, and require prolonged ventilation or reintubation.13 Nickerson et al showed that PAF following cardiac surgery corresponded with an increase in length of stay in both the ICU and hospital.14
Our study showed statistically significant increases in postoperative hospital charges, postoperative hospital stay, and ICU stay among patients who experienced PAF following CABG. These findings are consistent with the current literature. In a study of 720 subjects undergoing CABG, Hravnak et al reported a 1.4-day increase in length of hospital stay and a 0.3day increase in length of ICU stay among patients who had PAF compared with those who did not.15 A significant increase in postoperative hospital charges was also observed.15 Similarly, in a multicenter study of 2,417 patients undergoing isolated CABG procedures, Mathew et al observed increases in ICU stay and hospital stay among those patients who experienced PAF.2 These findings indicate that the onset of PAF after CABG is a serious complication and that further study is warranted.
Hypnosis to prevent PAF: Suggestive evidence and mechanisms
Clinical hypnosis has been shown to reduce stress and anxiety in surgical patients and can be highly individualized to address the patient’s needs during the stressful preoperative period. Saadat et al found that hypnosis administered directly before ambulatory surgery using Ericksonian techniques reduced patients’ levels of anxiety by 56% from baseline.11 In a South African study specifically in men undergoing CABG, de Klerk et al found that preoperative hypnotherapy led to reductions in both anxiety and depression at discharge that were maintained through 6-week follow-up.10
These findings, taken together with research linking clinical hypnosis to changes in the autonomic nervous system9 and the belief that PAF may result from transient autonomic dysfunction, suggest that hypnosis may reduce the incidence of PAF.
In a study of R-R interval dynamics prior to PAF in patients who had undergone CABG, Hogue et al showed that patients who experienced PAF had higher heart rates directly before PAF onset.16 Higher heart rates are associated with increased activity of the sympathetic nervous system and/or decreased activity of the parasympathetic nervous system. This finding supports our hypothesis of a relationship between PAF following CABG and excessive adrenergic activation. Chen et al have noted that catecholamine-mediated AF usually occurs in the presence of heart disease and that these types of attacks often happen during the daytime in association with physical or emotional stress.4
Bettoni and Zimmermann found that the onset of AF is preceded by a primary increase in adrenergic drive, which changes to increased vagal activity immediately before the occurrence.3 Tomita et al reported that sympathetic tone increases immediately before an occurrence of daytime AF.7 These results were supported by Lombardi et al, who detected signs of predominant sympathetic modulation and reduced vagal modulation of sinus node in AF episodes that started during the daytime.6 These episodes were characterized by atrial ectopic beats prior to onset.6
Modulations in baroreceptor reflex activity may provide further evidence of the importance of the sympathetic/parasympathetic balance in the initiation of AF. Suboptimal functioning of the baroreceptor reflex has been associated with arrhythmias and adverse cardiac events in patients and animal models. Loss of the protective effects of vagal activation has been postulated to increase vulnerability to sympathetically driven ischemia and malignant arrhythmias.17
Multiple studies have shown that the only conclusive predictor of PAF is age. Notably, heart rate variability is reduced with increased age.18 By measuring heart rate variability, Taggart et al showed that autonomic balance was improved in patients under induced stress when they were in a hypnotic state.19 Although no attempts were made to determine heart rate variability in our patient set, other studies have demonstrated an increase in heart rate variability during hypnosis. The results of our study suggest that clinical hypnosis using a personalized Ericksonian approach may have a beneficial effect on the incidence of PAF.
CONCLUSIONS
Clinical hypnosis appears to lower the incidence of PAF in patients undergoing CABG as well as to yield favorable trends toward reduced ICU and postoperative hospital stays, reduced hospital charges, and reduced use of narcotics. Although our study had a small sample size and lacked randomization, its positive results and the absence of side effects suggest that prospective randomized trials should be conducted to further delineate the role of hypnosis in the prevention of PAF. A better understanding of AF, and of the autonomic nervous system’s role in triggering and maintaining PAF, will allow more appropriate treatment of this condition.
- Halonen J, Hakala T, Auvinen T, et al. Intravenous administration of metoprolol is more effective than oral administration in the prevention of atrial fibrillation after cardiac surgery. Circulation 2006; 114(1 Suppl):I1–I4.
- Mathew JP, Parks R, Savino JS, et al. Atrial fibrillation following coronary artery bypass graft surgery: predictors, outcomes, and resource utilization. MultiCenter Study of Perioperative Ischemia Research Group. JAMA 1996; 276:300–306.
- Bettoni M, Zimmermann M. Autonomic tone variations before the onset of paroxysmal atrial fibrillation. Circulation 2002; 105:2753–2759.
- Chen J, Wasmund SL, Hamdan MH. Back to the future: the role of the autonomic nervous system in atrial fibrillation. Pacing Clin Electrophysiol 2006; 29:413–421.
- Hogue CW Jr, Creswell LL, Gutterman DD, Fleisher LA; American College of Chest Physicians. Epidemiology, mechanisms, and risks: American College of Chest Physicians guidelines for the prevention and management of postoperative atrial fibrillation after cardiac surgery. Chest 2005; 128(2 Suppl):9S–16S.
- Lombardi F, Tarricone D, Tundo F, Colombo F, Belletti S, Fiorentini C. Autonomic nervous system and paroxysmal atrial fibrillation: a study based on the analysis of RR interval changes before, during and after paroxysmal atrial fibrillation. Eur Heart J 2004; 25:1242–1248.
- Tomita T, Takei M, Saikawa Y, et al. Role of autonomic tone in the initiation and termination of paroxysmal atrial fibrillation in patients without structural heart disease. J Cardiovasc Electrophysiol 2003; 14:559–564.
- Aasbo JD, Lawrence AT, Krishnan K, Kim MH, Trohman RG. Amiodarone prophylaxis reduces major cardiovascular morbidity and length of stay after cardiac surgery: a meta-analysis. Ann Intern Med 2005; 143:327–336.
- Hippel CV, Hole G, Kaschka WP. Autonomic profile under hypnosis as assessed by heart rate variability and spectral analysis. Pharmacopsychiatry 2001; 34:111–113.
- de Klerk JE, du Plessis WF, Steyn HS, Botha M. Hypnotherapeutic ego strengthening with male South African coronary artery bypass patients. Am J Clin Hypn 2004; 47:79–92.
- Saadat H, Drummond-Lewis J, Maranets I, et al. Hypnosis reduces preoperative anxiety in adult patients. Anesth Analg 2006; 102:1394–1396.
- Villareal RP, Hariharan R, Liu BC, et al. Postoperative atrial fibrillation and mortality after coronary artery bypass surgery. J Am Coll Cardiol 2004; 43:742–748.
- Maisel WH, Rawn JD, Stevenson WG. Atrial fibrillation after cardiac surgery. Ann Intern Med 2001; 135:1061–1073.
- Nickerson NJ, Murphy SF, Dávila-Román VG, Schechtman KB, Kouchoukos NT. Obstacles to early discharge after cardiac surgery. Am J Manag Care 1999; 5:29–34.
- Hravnak M, Hoffman LA, Saul MI, et al. Resource utilization related to atrial fibrillation after coronary artery bypass grafting. Am J Crit Care 2002; 11:228–238.
- Hogue CW Jr, Domitrovich PP, Stein PK, et al. RR interval dynamics before atrial fibrillation in patients after coronary artery bypass graft surgery. Circulation 1998; 98:429–434.
- Olshansky B. Interrelationships between the autonomic nervous system and atrial fibrillation. Prog Cardiovasc Dis 2005; 48:57–78.
- Zhang J. Effect of age and sex on heart rate variability in healthy subjects. J Manipulative Physiol Ther 2007; 30:374–379.
- Taggart P, Sutton P, Redfern C, et al. The effect of mental stress on the non-dipolar components of the T wave: modulation by hypnosis. Psychosom Med 2005; 67:376–383.
- Halonen J, Hakala T, Auvinen T, et al. Intravenous administration of metoprolol is more effective than oral administration in the prevention of atrial fibrillation after cardiac surgery. Circulation 2006; 114(1 Suppl):I1–I4.
- Mathew JP, Parks R, Savino JS, et al. Atrial fibrillation following coronary artery bypass graft surgery: predictors, outcomes, and resource utilization. MultiCenter Study of Perioperative Ischemia Research Group. JAMA 1996; 276:300–306.
- Bettoni M, Zimmermann M. Autonomic tone variations before the onset of paroxysmal atrial fibrillation. Circulation 2002; 105:2753–2759.
- Chen J, Wasmund SL, Hamdan MH. Back to the future: the role of the autonomic nervous system in atrial fibrillation. Pacing Clin Electrophysiol 2006; 29:413–421.
- Hogue CW Jr, Creswell LL, Gutterman DD, Fleisher LA; American College of Chest Physicians. Epidemiology, mechanisms, and risks: American College of Chest Physicians guidelines for the prevention and management of postoperative atrial fibrillation after cardiac surgery. Chest 2005; 128(2 Suppl):9S–16S.
- Lombardi F, Tarricone D, Tundo F, Colombo F, Belletti S, Fiorentini C. Autonomic nervous system and paroxysmal atrial fibrillation: a study based on the analysis of RR interval changes before, during and after paroxysmal atrial fibrillation. Eur Heart J 2004; 25:1242–1248.
- Tomita T, Takei M, Saikawa Y, et al. Role of autonomic tone in the initiation and termination of paroxysmal atrial fibrillation in patients without structural heart disease. J Cardiovasc Electrophysiol 2003; 14:559–564.
- Aasbo JD, Lawrence AT, Krishnan K, Kim MH, Trohman RG. Amiodarone prophylaxis reduces major cardiovascular morbidity and length of stay after cardiac surgery: a meta-analysis. Ann Intern Med 2005; 143:327–336.
- Hippel CV, Hole G, Kaschka WP. Autonomic profile under hypnosis as assessed by heart rate variability and spectral analysis. Pharmacopsychiatry 2001; 34:111–113.
- de Klerk JE, du Plessis WF, Steyn HS, Botha M. Hypnotherapeutic ego strengthening with male South African coronary artery bypass patients. Am J Clin Hypn 2004; 47:79–92.
- Saadat H, Drummond-Lewis J, Maranets I, et al. Hypnosis reduces preoperative anxiety in adult patients. Anesth Analg 2006; 102:1394–1396.
- Villareal RP, Hariharan R, Liu BC, et al. Postoperative atrial fibrillation and mortality after coronary artery bypass surgery. J Am Coll Cardiol 2004; 43:742–748.
- Maisel WH, Rawn JD, Stevenson WG. Atrial fibrillation after cardiac surgery. Ann Intern Med 2001; 135:1061–1073.
- Nickerson NJ, Murphy SF, Dávila-Román VG, Schechtman KB, Kouchoukos NT. Obstacles to early discharge after cardiac surgery. Am J Manag Care 1999; 5:29–34.
- Hravnak M, Hoffman LA, Saul MI, et al. Resource utilization related to atrial fibrillation after coronary artery bypass grafting. Am J Crit Care 2002; 11:228–238.
- Hogue CW Jr, Domitrovich PP, Stein PK, et al. RR interval dynamics before atrial fibrillation in patients after coronary artery bypass graft surgery. Circulation 1998; 98:429–434.
- Olshansky B. Interrelationships between the autonomic nervous system and atrial fibrillation. Prog Cardiovasc Dis 2005; 48:57–78.
- Zhang J. Effect of age and sex on heart rate variability in healthy subjects. J Manipulative Physiol Ther 2007; 30:374–379.
- Taggart P, Sutton P, Redfern C, et al. The effect of mental stress on the non-dipolar components of the T wave: modulation by hypnosis. Psychosom Med 2005; 67:376–383.