User login
Thrombolytics for VTE: Current Practice
More than a decade ago, we surveyed a group of practicing pulmonologists to determine their attitudes regarding the use of thrombolytic therapy in various settings of acute venous thromboembolism (VTE).1 Since that time, the literature regarding the treatment of acute VTE has grown dramatically.214 However, despite the available evidence, there remains considerable controversy regarding the appropriate setting for thrombolysis in acute pulmonary embolism (PE) or deep‐vein thrombosis (DVT). We therefore sought to better describe the current patterns of thrombolytic use among practicing pulmonologists and to determine if these patterns have changed over the last decade.
Methods
Five‐hundred and ten physicians in the southeastern US were selected from the American Thoracic Society (ATS) membership roster and were e‐mailed a link to an online questionnaire. The roster was searched for physicians who described their subspecialty as pulmonary disease or pulmonary and critical care.
Participants were asked background information and questions regarding hypothetical clinical scenarios. All participants were offered a $50 stipend, and to further improve the response rate, 2 reminder e‐mail messages were sent 30 days and 45 days after the initial request.
Baseline findings of the survey were summarized using descriptive statistics. Differences among participants and their responses were determined by Fisher's exact test. Analyses were performed using SAS E‐Guide Version 3.0 for Windows (SAS Institute, Cary, NC) with 2‐sided P values at the standard 0.05 level used to determine statistical significance.
Results
Baseline Characteristics
Eighty‐one physicians completed the questionnaire; their baseline characteristics are shown in Table 1. During the previous 2 years, all physicians surveyed had treated at least 1 patient with acute PE and all but 1 had treated at least 1 patient with DVT. Also, 68 respondents reported that they had used thrombolytic therapy in at least 1 case of PE in the past 2 years.
| |
| Age, mean (years) | 45.6 |
| Training completed, n (%) | |
| 1980‐1989 | 28 (34.5) |
| 1990‐1999 | 25 (31.0) |
| 2000‐2007 | 28 (34.5) |
| Practice type n (%) | |
| Academic | 35 (43) |
| Private practice | 37 (46) |
| Private practice with academic appointment | 6 (7) |
| Other | 3 (4) |
| Practice setting, n (%) | |
| Predominantly outpatient | 8 (10) |
| Predominantly inpatient | 29 (36) |
| Equal inpatient and outpatient | 44 (54) |
| Hospital size (beds), n (%) | |
| 50 | 1 (1) |
| 50‐100 | 1 (1) |
| 100‐300 | 20 (25) |
| 300‐500 | 22 (27) |
| >500 | 37 (46) |
| Number of patients treated with PE in the past 2 years, n (%) | |
| 0 | 0 (0) |
| 1‐5 | 3 (4) |
| 6‐10 | 14 (17) |
| 11‐15 | 12 (15) |
| 16‐20 | 17 (21) |
| >20 | 35 (43) |
| Number of patients treated with DVT in the past 2 years, n (%) | |
| 0 | 1 (1) |
| 1‐5 | 3 (4) |
| 6‐10 | 7 (9) |
| 11‐15 | 16 (20) |
| 16‐20 | 11 (14) |
| >20 | 43 (53) |
| Number of patients with PE treated with thrombolysis, n (%) | |
| 0 | 13 (16) |
| 1‐5 | 53 (65) |
| 6‐10 | 11 (14) |
| 11‐15 | 1 (1) |
| 16‐20 | 2 (2) |
| >20 | 1 (1) |
Use of Thrombolytic Therapy in Various Scenarios
The responses for the 8 clinical scenarios are shown in Table 2. Approximately equal numbers of academic and private practice physicians completed the questionnaire, and comparison between these groups showed no significant differences in decision‐making for each of the case scenarios. Less experienced physicians (>10 cases treated versus 10 cases treated) were more likely to consider thrombolytic therapy in a patient with a smaller PE but with poor cardiopulmonary reserve (P = 0.001), and with proximal symptomatic DVT of any size present less than 7 days (P = 0.047).
| Scenario | Current Study (%) | Previous Study1 (%) | P |
|---|---|---|---|
| |||
| Massive PE with hypotension | 80 (99) | 56 (100) | NS |
| Large PE with hypoxemia | 67 (83) | 41 (73) | NS |
| PE with RV strain or failure | 50 (62) | 31 (55) | NS |
| Large PE without hypotension, hypoxemia, or RV strain | 9 (11) | 6 (11) | NS |
| Smaller PE in a patient with poor cardiopulmonary reserve | 11 (14) | ||
| Massive symptomatic DVT, 7 days | 41 (51) | 33 (59) | NS |
| Massive symptomatic DVT, >7 days | 14 (17) | ||
| Proximal DVT, any size, 7 days | 6 (7) | 7 (13) | NS |
Use of Thrombolytic Therapy When Contraindications Exist
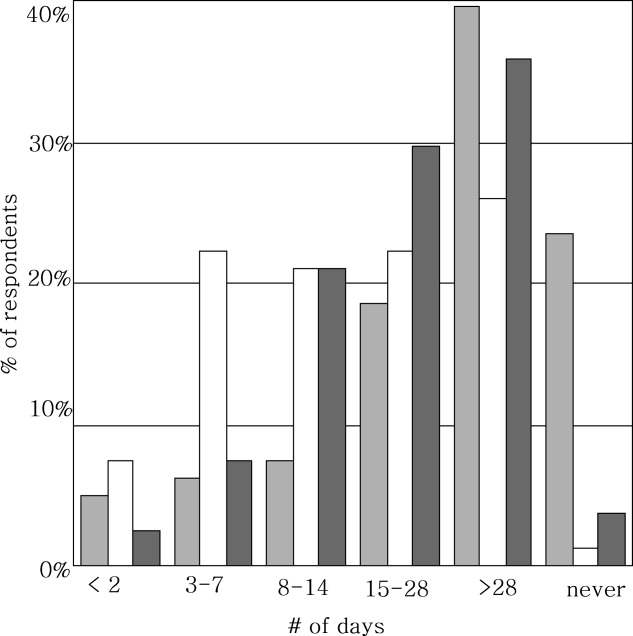
The vast majority of respondents reported that they would consider giving thrombolytic therapy to a patient with massive PE and hypotension requiring vasopressor therapy despite having a traditional contraindication (relative or absolute) to thrombolysis (Table 3). Most respondents would consider giving thrombolytic therapy to postoperative orthopedic, abdominal, or thoracic surgery patients if they were more than 2 weeks postoperation, and very few would give thrombolytic therapy to patients who were less than 2 days postoperation. Many respondents would also consider giving thrombolytic therapy to a patient with a massive PE and with a history of major gastrointestinal (GI) bleeding (requiring blood transfusion) if the bleed was more than 4 weeks prior to the embolism (Figure 1).

| Condition | Number of Physicians (%) |
|---|---|
| |
| Age >75 years | 58 (72) |
| Guaiac + stool | 54 (67) |
| CPR in past 10 days | 39 (48) |
| History of ischemic stroke | 37 (46) |
| Recent venipuncture of a noncompressible vessel | 33 (41) |
| History of ICH | 6 (7) |
| Brain tumor | 6 (7) |
| Would never use thrombolytics in these scenarios | 7 (9) |
Discussion
Given the paucity of data from randomized controlled trials, there remains considerable controversy regarding the indications for thrombolytic therapy. It may be difficult to define those patients in whom the benefit of a rapid reduction in clot burden outweighs the increased hemorrhagic risk. The case for thrombolysis is the strongest in patients with massive PE complicated by hypotension, in whom the mortality rate may be 30%.15 Our survey confirms that the vast majority of practicing pulmonologists would strongly consider systemic thrombolysis in this clinical setting, which is in accordance with current guidelines and with our previous survey results.1, 5, 10, 12
No clinical trial has specifically evaluated thrombolytic therapy in patients with large PE and hypoxemia but without hypotension, and it is interesting that so many physicians would consider thrombolytic therapy in this scenario. As right heart failure is the cause of death in PE, the absence of significant hypotension would imply less cardiovascular risk and thrombolytic use would seemingly be less justifiable from a physiologic point of view. It may be that further study and education is warranted in this area.
Many patients who present with acute, life‐threatening PE have contraindications or relative contraindications to systemic thrombolysis. Our study suggests that most practicing pulmonologists would consider giving thrombolytic therapy in some of these situations, such as if the patient was more than 2 weeks postoperative from major thoracic or abdominal surgery (or even a few days following orthopedic surgery), or in the setting of advanced age or guaiac positive stools. Physicians were appropriately very reluctant to use thrombolytic therapy in the setting of a brain tumor or prior intracranial hemorrhage. These scenarios emphasize the vagaries of the current guidelines and real‐world complexities of considering thrombolytic therapy in clinical practice, in which the risks and benefits must be weighed on a case‐by‐case basis.
One major difference between our current and past findings is the general experience with thrombolytic therapy in acute PE. In our first study, only 54% of physicians queried had employed systemic thrombolysis for acute PE. Our current findings were that 84% of physicians had used thrombolysis for acute PE within the last 2 years, perhaps suggesting a greater comfort with this therapy.
Response bias is a major limitation of our study. We sought to keep questions short and clear, and offered a small stipend to improve the return rate. Despite these measures, only 81 of 510 questionnaires were completed. We selected our list of participants from the ATS roster and by geographic location. As suggested by our findings, the results may have been different had we focused solely on VTE experts or those treating large numbers of VTE patients. One strength of this study is that our sample had approximately even numbers of academic and private practice physicians, and that we could compare current results with our prior findings.
In conclusion, practicing pulmonologists generally agreed that in the absence of contraindications, thrombolytic therapy should be considered in patients with massive PE and hypotension, which is in accordance with current guidelines. Furthermore, a majority would still consider thrombolytic therapy in this scenario even if certain contraindications were present. Although there is less agreement in other scenarios, a majority of physicians would consider using thrombolytics in patients with PE and severe hypoxemia or right ventricular (RV) dysfunction. Despite the evolving data and guidelines, our findings are similar to prior survey results, with the notable exception that more physicians reported thrombolytic therapy use in acute PE in the current study. This emphasizes the need for further physician education and future randomized clinical trials to delineate and unify therapeutic strategies in cases of VTE.
- ,,.Thrombolytic therapy for venous thromboembolism. Utilization by practicing pulmonologists.Arch Intern Med.1994;154:1601–1604.
- ,,, et al.Streptokinase vs alteplase in massive pulmonary embolism. A randomized trial assessing right heart haemodynamics and pulmonary vascular obstruction.Eur Heart J.1997;18:1141–1148.
- ,,, et al.Comparative efficacy of a two‐hour regimen of streptokinase versus alteplase in acute massive pulmonary embolism: immediate clinical and hemodynamic outcome and one‐year follow‐up.J Am Coll Cardiol.1998;31:1057–1063.
- ,,.Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER).Lancet.1999;353:1386–1389.
- ,,, et al.Guidelines on diagnosis and management of acute pulmonary embolism. Task Force on Pulmonary Embolism, European Society of Cardiology.Eur Heart J.2000;21:1301–1336.
- ,,,.Long‐term benefit of thrombolytic therapy in patients with pulmonary embolism.Vasc Med.2000;5:91–95.
- ,,, et al.Thrombolytic therapy of pulmonary embolism: a meta‐analysis.J Am Coll Cardiol.2002;40:1660–1667.
- ,,, et al.Heparin plus alteplase compared with heparin alone in patients with submassive pulmonary embolism.N Engl J Med.2002;347:1143–1150.
- ,,.Thrombolysis vs heparin in the treatment of pulmonary embolism: a clinical outcome‐based meta‐analysis.Arch Intern Med.2002;162:2537–2541.
- ,,, et al.British Thoracic Society guidelines for the management of suspected acute pulmonary embolism.Thorax.2003;58:470–483.
- ,.Thrombolysis for acute deep vein thrombosis.Cochrane Database Syst Rev.2004;CD002783.
- ,,, et al.Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy.Chest.2004;126:401S–428S.
- ,,, et al.Thrombolysis compared with heparin for the initial treatment of pulmonary embolism: a meta‐analysis of the randomized controlled trials.Circulation.2004;110:744–749.
- ,,, et al.Thrombolytic therapy for pulmonary embolism.Cochrane Database Syst Rev.2006;CD004437.
- ,,Thrombolytic therapy for pulmonary embolism: is it effective? Is it safe? When is it indicated?Arch Intern Med.1997;157:2550–2556.
More than a decade ago, we surveyed a group of practicing pulmonologists to determine their attitudes regarding the use of thrombolytic therapy in various settings of acute venous thromboembolism (VTE).1 Since that time, the literature regarding the treatment of acute VTE has grown dramatically.214 However, despite the available evidence, there remains considerable controversy regarding the appropriate setting for thrombolysis in acute pulmonary embolism (PE) or deep‐vein thrombosis (DVT). We therefore sought to better describe the current patterns of thrombolytic use among practicing pulmonologists and to determine if these patterns have changed over the last decade.
Methods
Five‐hundred and ten physicians in the southeastern US were selected from the American Thoracic Society (ATS) membership roster and were e‐mailed a link to an online questionnaire. The roster was searched for physicians who described their subspecialty as pulmonary disease or pulmonary and critical care.
Participants were asked background information and questions regarding hypothetical clinical scenarios. All participants were offered a $50 stipend, and to further improve the response rate, 2 reminder e‐mail messages were sent 30 days and 45 days after the initial request.
Baseline findings of the survey were summarized using descriptive statistics. Differences among participants and their responses were determined by Fisher's exact test. Analyses were performed using SAS E‐Guide Version 3.0 for Windows (SAS Institute, Cary, NC) with 2‐sided P values at the standard 0.05 level used to determine statistical significance.
Results
Baseline Characteristics
Eighty‐one physicians completed the questionnaire; their baseline characteristics are shown in Table 1. During the previous 2 years, all physicians surveyed had treated at least 1 patient with acute PE and all but 1 had treated at least 1 patient with DVT. Also, 68 respondents reported that they had used thrombolytic therapy in at least 1 case of PE in the past 2 years.
| |
| Age, mean (years) | 45.6 |
| Training completed, n (%) | |
| 1980‐1989 | 28 (34.5) |
| 1990‐1999 | 25 (31.0) |
| 2000‐2007 | 28 (34.5) |
| Practice type n (%) | |
| Academic | 35 (43) |
| Private practice | 37 (46) |
| Private practice with academic appointment | 6 (7) |
| Other | 3 (4) |
| Practice setting, n (%) | |
| Predominantly outpatient | 8 (10) |
| Predominantly inpatient | 29 (36) |
| Equal inpatient and outpatient | 44 (54) |
| Hospital size (beds), n (%) | |
| 50 | 1 (1) |
| 50‐100 | 1 (1) |
| 100‐300 | 20 (25) |
| 300‐500 | 22 (27) |
| >500 | 37 (46) |
| Number of patients treated with PE in the past 2 years, n (%) | |
| 0 | 0 (0) |
| 1‐5 | 3 (4) |
| 6‐10 | 14 (17) |
| 11‐15 | 12 (15) |
| 16‐20 | 17 (21) |
| >20 | 35 (43) |
| Number of patients treated with DVT in the past 2 years, n (%) | |
| 0 | 1 (1) |
| 1‐5 | 3 (4) |
| 6‐10 | 7 (9) |
| 11‐15 | 16 (20) |
| 16‐20 | 11 (14) |
| >20 | 43 (53) |
| Number of patients with PE treated with thrombolysis, n (%) | |
| 0 | 13 (16) |
| 1‐5 | 53 (65) |
| 6‐10 | 11 (14) |
| 11‐15 | 1 (1) |
| 16‐20 | 2 (2) |
| >20 | 1 (1) |
Use of Thrombolytic Therapy in Various Scenarios
The responses for the 8 clinical scenarios are shown in Table 2. Approximately equal numbers of academic and private practice physicians completed the questionnaire, and comparison between these groups showed no significant differences in decision‐making for each of the case scenarios. Less experienced physicians (>10 cases treated versus 10 cases treated) were more likely to consider thrombolytic therapy in a patient with a smaller PE but with poor cardiopulmonary reserve (P = 0.001), and with proximal symptomatic DVT of any size present less than 7 days (P = 0.047).
| Scenario | Current Study (%) | Previous Study1 (%) | P |
|---|---|---|---|
| |||
| Massive PE with hypotension | 80 (99) | 56 (100) | NS |
| Large PE with hypoxemia | 67 (83) | 41 (73) | NS |
| PE with RV strain or failure | 50 (62) | 31 (55) | NS |
| Large PE without hypotension, hypoxemia, or RV strain | 9 (11) | 6 (11) | NS |
| Smaller PE in a patient with poor cardiopulmonary reserve | 11 (14) | ||
| Massive symptomatic DVT, 7 days | 41 (51) | 33 (59) | NS |
| Massive symptomatic DVT, >7 days | 14 (17) | ||
| Proximal DVT, any size, 7 days | 6 (7) | 7 (13) | NS |
Use of Thrombolytic Therapy When Contraindications Exist
The vast majority of respondents reported that they would consider giving thrombolytic therapy to a patient with massive PE and hypotension requiring vasopressor therapy despite having a traditional contraindication (relative or absolute) to thrombolysis (Table 3). Most respondents would consider giving thrombolytic therapy to postoperative orthopedic, abdominal, or thoracic surgery patients if they were more than 2 weeks postoperation, and very few would give thrombolytic therapy to patients who were less than 2 days postoperation. Many respondents would also consider giving thrombolytic therapy to a patient with a massive PE and with a history of major gastrointestinal (GI) bleeding (requiring blood transfusion) if the bleed was more than 4 weeks prior to the embolism (Figure 1).

| Condition | Number of Physicians (%) |
|---|---|
| |
| Age >75 years | 58 (72) |
| Guaiac + stool | 54 (67) |
| CPR in past 10 days | 39 (48) |
| History of ischemic stroke | 37 (46) |
| Recent venipuncture of a noncompressible vessel | 33 (41) |
| History of ICH | 6 (7) |
| Brain tumor | 6 (7) |
| Would never use thrombolytics in these scenarios | 7 (9) |
Discussion
Given the paucity of data from randomized controlled trials, there remains considerable controversy regarding the indications for thrombolytic therapy. It may be difficult to define those patients in whom the benefit of a rapid reduction in clot burden outweighs the increased hemorrhagic risk. The case for thrombolysis is the strongest in patients with massive PE complicated by hypotension, in whom the mortality rate may be 30%.15 Our survey confirms that the vast majority of practicing pulmonologists would strongly consider systemic thrombolysis in this clinical setting, which is in accordance with current guidelines and with our previous survey results.1, 5, 10, 12
No clinical trial has specifically evaluated thrombolytic therapy in patients with large PE and hypoxemia but without hypotension, and it is interesting that so many physicians would consider thrombolytic therapy in this scenario. As right heart failure is the cause of death in PE, the absence of significant hypotension would imply less cardiovascular risk and thrombolytic use would seemingly be less justifiable from a physiologic point of view. It may be that further study and education is warranted in this area.
Many patients who present with acute, life‐threatening PE have contraindications or relative contraindications to systemic thrombolysis. Our study suggests that most practicing pulmonologists would consider giving thrombolytic therapy in some of these situations, such as if the patient was more than 2 weeks postoperative from major thoracic or abdominal surgery (or even a few days following orthopedic surgery), or in the setting of advanced age or guaiac positive stools. Physicians were appropriately very reluctant to use thrombolytic therapy in the setting of a brain tumor or prior intracranial hemorrhage. These scenarios emphasize the vagaries of the current guidelines and real‐world complexities of considering thrombolytic therapy in clinical practice, in which the risks and benefits must be weighed on a case‐by‐case basis.
One major difference between our current and past findings is the general experience with thrombolytic therapy in acute PE. In our first study, only 54% of physicians queried had employed systemic thrombolysis for acute PE. Our current findings were that 84% of physicians had used thrombolysis for acute PE within the last 2 years, perhaps suggesting a greater comfort with this therapy.
Response bias is a major limitation of our study. We sought to keep questions short and clear, and offered a small stipend to improve the return rate. Despite these measures, only 81 of 510 questionnaires were completed. We selected our list of participants from the ATS roster and by geographic location. As suggested by our findings, the results may have been different had we focused solely on VTE experts or those treating large numbers of VTE patients. One strength of this study is that our sample had approximately even numbers of academic and private practice physicians, and that we could compare current results with our prior findings.
In conclusion, practicing pulmonologists generally agreed that in the absence of contraindications, thrombolytic therapy should be considered in patients with massive PE and hypotension, which is in accordance with current guidelines. Furthermore, a majority would still consider thrombolytic therapy in this scenario even if certain contraindications were present. Although there is less agreement in other scenarios, a majority of physicians would consider using thrombolytics in patients with PE and severe hypoxemia or right ventricular (RV) dysfunction. Despite the evolving data and guidelines, our findings are similar to prior survey results, with the notable exception that more physicians reported thrombolytic therapy use in acute PE in the current study. This emphasizes the need for further physician education and future randomized clinical trials to delineate and unify therapeutic strategies in cases of VTE.
More than a decade ago, we surveyed a group of practicing pulmonologists to determine their attitudes regarding the use of thrombolytic therapy in various settings of acute venous thromboembolism (VTE).1 Since that time, the literature regarding the treatment of acute VTE has grown dramatically.214 However, despite the available evidence, there remains considerable controversy regarding the appropriate setting for thrombolysis in acute pulmonary embolism (PE) or deep‐vein thrombosis (DVT). We therefore sought to better describe the current patterns of thrombolytic use among practicing pulmonologists and to determine if these patterns have changed over the last decade.
Methods
Five‐hundred and ten physicians in the southeastern US were selected from the American Thoracic Society (ATS) membership roster and were e‐mailed a link to an online questionnaire. The roster was searched for physicians who described their subspecialty as pulmonary disease or pulmonary and critical care.
Participants were asked background information and questions regarding hypothetical clinical scenarios. All participants were offered a $50 stipend, and to further improve the response rate, 2 reminder e‐mail messages were sent 30 days and 45 days after the initial request.
Baseline findings of the survey were summarized using descriptive statistics. Differences among participants and their responses were determined by Fisher's exact test. Analyses were performed using SAS E‐Guide Version 3.0 for Windows (SAS Institute, Cary, NC) with 2‐sided P values at the standard 0.05 level used to determine statistical significance.
Results
Baseline Characteristics
Eighty‐one physicians completed the questionnaire; their baseline characteristics are shown in Table 1. During the previous 2 years, all physicians surveyed had treated at least 1 patient with acute PE and all but 1 had treated at least 1 patient with DVT. Also, 68 respondents reported that they had used thrombolytic therapy in at least 1 case of PE in the past 2 years.
| |
| Age, mean (years) | 45.6 |
| Training completed, n (%) | |
| 1980‐1989 | 28 (34.5) |
| 1990‐1999 | 25 (31.0) |
| 2000‐2007 | 28 (34.5) |
| Practice type n (%) | |
| Academic | 35 (43) |
| Private practice | 37 (46) |
| Private practice with academic appointment | 6 (7) |
| Other | 3 (4) |
| Practice setting, n (%) | |
| Predominantly outpatient | 8 (10) |
| Predominantly inpatient | 29 (36) |
| Equal inpatient and outpatient | 44 (54) |
| Hospital size (beds), n (%) | |
| 50 | 1 (1) |
| 50‐100 | 1 (1) |
| 100‐300 | 20 (25) |
| 300‐500 | 22 (27) |
| >500 | 37 (46) |
| Number of patients treated with PE in the past 2 years, n (%) | |
| 0 | 0 (0) |
| 1‐5 | 3 (4) |
| 6‐10 | 14 (17) |
| 11‐15 | 12 (15) |
| 16‐20 | 17 (21) |
| >20 | 35 (43) |
| Number of patients treated with DVT in the past 2 years, n (%) | |
| 0 | 1 (1) |
| 1‐5 | 3 (4) |
| 6‐10 | 7 (9) |
| 11‐15 | 16 (20) |
| 16‐20 | 11 (14) |
| >20 | 43 (53) |
| Number of patients with PE treated with thrombolysis, n (%) | |
| 0 | 13 (16) |
| 1‐5 | 53 (65) |
| 6‐10 | 11 (14) |
| 11‐15 | 1 (1) |
| 16‐20 | 2 (2) |
| >20 | 1 (1) |
Use of Thrombolytic Therapy in Various Scenarios
The responses for the 8 clinical scenarios are shown in Table 2. Approximately equal numbers of academic and private practice physicians completed the questionnaire, and comparison between these groups showed no significant differences in decision‐making for each of the case scenarios. Less experienced physicians (>10 cases treated versus 10 cases treated) were more likely to consider thrombolytic therapy in a patient with a smaller PE but with poor cardiopulmonary reserve (P = 0.001), and with proximal symptomatic DVT of any size present less than 7 days (P = 0.047).
| Scenario | Current Study (%) | Previous Study1 (%) | P |
|---|---|---|---|
| |||
| Massive PE with hypotension | 80 (99) | 56 (100) | NS |
| Large PE with hypoxemia | 67 (83) | 41 (73) | NS |
| PE with RV strain or failure | 50 (62) | 31 (55) | NS |
| Large PE without hypotension, hypoxemia, or RV strain | 9 (11) | 6 (11) | NS |
| Smaller PE in a patient with poor cardiopulmonary reserve | 11 (14) | ||
| Massive symptomatic DVT, 7 days | 41 (51) | 33 (59) | NS |
| Massive symptomatic DVT, >7 days | 14 (17) | ||
| Proximal DVT, any size, 7 days | 6 (7) | 7 (13) | NS |
Use of Thrombolytic Therapy When Contraindications Exist
The vast majority of respondents reported that they would consider giving thrombolytic therapy to a patient with massive PE and hypotension requiring vasopressor therapy despite having a traditional contraindication (relative or absolute) to thrombolysis (Table 3). Most respondents would consider giving thrombolytic therapy to postoperative orthopedic, abdominal, or thoracic surgery patients if they were more than 2 weeks postoperation, and very few would give thrombolytic therapy to patients who were less than 2 days postoperation. Many respondents would also consider giving thrombolytic therapy to a patient with a massive PE and with a history of major gastrointestinal (GI) bleeding (requiring blood transfusion) if the bleed was more than 4 weeks prior to the embolism (Figure 1).

| Condition | Number of Physicians (%) |
|---|---|
| |
| Age >75 years | 58 (72) |
| Guaiac + stool | 54 (67) |
| CPR in past 10 days | 39 (48) |
| History of ischemic stroke | 37 (46) |
| Recent venipuncture of a noncompressible vessel | 33 (41) |
| History of ICH | 6 (7) |
| Brain tumor | 6 (7) |
| Would never use thrombolytics in these scenarios | 7 (9) |
Discussion
Given the paucity of data from randomized controlled trials, there remains considerable controversy regarding the indications for thrombolytic therapy. It may be difficult to define those patients in whom the benefit of a rapid reduction in clot burden outweighs the increased hemorrhagic risk. The case for thrombolysis is the strongest in patients with massive PE complicated by hypotension, in whom the mortality rate may be 30%.15 Our survey confirms that the vast majority of practicing pulmonologists would strongly consider systemic thrombolysis in this clinical setting, which is in accordance with current guidelines and with our previous survey results.1, 5, 10, 12
No clinical trial has specifically evaluated thrombolytic therapy in patients with large PE and hypoxemia but without hypotension, and it is interesting that so many physicians would consider thrombolytic therapy in this scenario. As right heart failure is the cause of death in PE, the absence of significant hypotension would imply less cardiovascular risk and thrombolytic use would seemingly be less justifiable from a physiologic point of view. It may be that further study and education is warranted in this area.
Many patients who present with acute, life‐threatening PE have contraindications or relative contraindications to systemic thrombolysis. Our study suggests that most practicing pulmonologists would consider giving thrombolytic therapy in some of these situations, such as if the patient was more than 2 weeks postoperative from major thoracic or abdominal surgery (or even a few days following orthopedic surgery), or in the setting of advanced age or guaiac positive stools. Physicians were appropriately very reluctant to use thrombolytic therapy in the setting of a brain tumor or prior intracranial hemorrhage. These scenarios emphasize the vagaries of the current guidelines and real‐world complexities of considering thrombolytic therapy in clinical practice, in which the risks and benefits must be weighed on a case‐by‐case basis.
One major difference between our current and past findings is the general experience with thrombolytic therapy in acute PE. In our first study, only 54% of physicians queried had employed systemic thrombolysis for acute PE. Our current findings were that 84% of physicians had used thrombolysis for acute PE within the last 2 years, perhaps suggesting a greater comfort with this therapy.
Response bias is a major limitation of our study. We sought to keep questions short and clear, and offered a small stipend to improve the return rate. Despite these measures, only 81 of 510 questionnaires were completed. We selected our list of participants from the ATS roster and by geographic location. As suggested by our findings, the results may have been different had we focused solely on VTE experts or those treating large numbers of VTE patients. One strength of this study is that our sample had approximately even numbers of academic and private practice physicians, and that we could compare current results with our prior findings.
In conclusion, practicing pulmonologists generally agreed that in the absence of contraindications, thrombolytic therapy should be considered in patients with massive PE and hypotension, which is in accordance with current guidelines. Furthermore, a majority would still consider thrombolytic therapy in this scenario even if certain contraindications were present. Although there is less agreement in other scenarios, a majority of physicians would consider using thrombolytics in patients with PE and severe hypoxemia or right ventricular (RV) dysfunction. Despite the evolving data and guidelines, our findings are similar to prior survey results, with the notable exception that more physicians reported thrombolytic therapy use in acute PE in the current study. This emphasizes the need for further physician education and future randomized clinical trials to delineate and unify therapeutic strategies in cases of VTE.
- ,,.Thrombolytic therapy for venous thromboembolism. Utilization by practicing pulmonologists.Arch Intern Med.1994;154:1601–1604.
- ,,, et al.Streptokinase vs alteplase in massive pulmonary embolism. A randomized trial assessing right heart haemodynamics and pulmonary vascular obstruction.Eur Heart J.1997;18:1141–1148.
- ,,, et al.Comparative efficacy of a two‐hour regimen of streptokinase versus alteplase in acute massive pulmonary embolism: immediate clinical and hemodynamic outcome and one‐year follow‐up.J Am Coll Cardiol.1998;31:1057–1063.
- ,,.Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER).Lancet.1999;353:1386–1389.
- ,,, et al.Guidelines on diagnosis and management of acute pulmonary embolism. Task Force on Pulmonary Embolism, European Society of Cardiology.Eur Heart J.2000;21:1301–1336.
- ,,,.Long‐term benefit of thrombolytic therapy in patients with pulmonary embolism.Vasc Med.2000;5:91–95.
- ,,, et al.Thrombolytic therapy of pulmonary embolism: a meta‐analysis.J Am Coll Cardiol.2002;40:1660–1667.
- ,,, et al.Heparin plus alteplase compared with heparin alone in patients with submassive pulmonary embolism.N Engl J Med.2002;347:1143–1150.
- ,,.Thrombolysis vs heparin in the treatment of pulmonary embolism: a clinical outcome‐based meta‐analysis.Arch Intern Med.2002;162:2537–2541.
- ,,, et al.British Thoracic Society guidelines for the management of suspected acute pulmonary embolism.Thorax.2003;58:470–483.
- ,.Thrombolysis for acute deep vein thrombosis.Cochrane Database Syst Rev.2004;CD002783.
- ,,, et al.Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy.Chest.2004;126:401S–428S.
- ,,, et al.Thrombolysis compared with heparin for the initial treatment of pulmonary embolism: a meta‐analysis of the randomized controlled trials.Circulation.2004;110:744–749.
- ,,, et al.Thrombolytic therapy for pulmonary embolism.Cochrane Database Syst Rev.2006;CD004437.
- ,,Thrombolytic therapy for pulmonary embolism: is it effective? Is it safe? When is it indicated?Arch Intern Med.1997;157:2550–2556.
- ,,.Thrombolytic therapy for venous thromboembolism. Utilization by practicing pulmonologists.Arch Intern Med.1994;154:1601–1604.
- ,,, et al.Streptokinase vs alteplase in massive pulmonary embolism. A randomized trial assessing right heart haemodynamics and pulmonary vascular obstruction.Eur Heart J.1997;18:1141–1148.
- ,,, et al.Comparative efficacy of a two‐hour regimen of streptokinase versus alteplase in acute massive pulmonary embolism: immediate clinical and hemodynamic outcome and one‐year follow‐up.J Am Coll Cardiol.1998;31:1057–1063.
- ,,.Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER).Lancet.1999;353:1386–1389.
- ,,, et al.Guidelines on diagnosis and management of acute pulmonary embolism. Task Force on Pulmonary Embolism, European Society of Cardiology.Eur Heart J.2000;21:1301–1336.
- ,,,.Long‐term benefit of thrombolytic therapy in patients with pulmonary embolism.Vasc Med.2000;5:91–95.
- ,,, et al.Thrombolytic therapy of pulmonary embolism: a meta‐analysis.J Am Coll Cardiol.2002;40:1660–1667.
- ,,, et al.Heparin plus alteplase compared with heparin alone in patients with submassive pulmonary embolism.N Engl J Med.2002;347:1143–1150.
- ,,.Thrombolysis vs heparin in the treatment of pulmonary embolism: a clinical outcome‐based meta‐analysis.Arch Intern Med.2002;162:2537–2541.
- ,,, et al.British Thoracic Society guidelines for the management of suspected acute pulmonary embolism.Thorax.2003;58:470–483.
- ,.Thrombolysis for acute deep vein thrombosis.Cochrane Database Syst Rev.2004;CD002783.
- ,,, et al.Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy.Chest.2004;126:401S–428S.
- ,,, et al.Thrombolysis compared with heparin for the initial treatment of pulmonary embolism: a meta‐analysis of the randomized controlled trials.Circulation.2004;110:744–749.
- ,,, et al.Thrombolytic therapy for pulmonary embolism.Cochrane Database Syst Rev.2006;CD004437.
- ,,Thrombolytic therapy for pulmonary embolism: is it effective? Is it safe? When is it indicated?Arch Intern Med.1997;157:2550–2556.