User login
Overweight youth: Changing behaviors that are barriers to health
- To motivate change, help parents to realize that overweight in their child is a health risk and not merely an aesthetic concern (C).
- Keep in mind that children can be motivated by different goals, such as increased athleticism, appearance, or social acceptance (C).
- Several short bursts of physical activity are usually more feasible than longer bouts, and may be more reinforcing for children and adolescents (C).
- Changing specific eating and activity behaviors is more realistic than setting a weight management goal (C).
My child doesn’t have a weight problem. We’re a family of big eaters, that’s all.” If you’ve heard this explanation or ones like it after raising a concern about a child’s weight, chances are you will encounter barriers to recognizing obesity and to changing the behavior that encourages it.
Even when parents and a significantly overweight child or adolescent acknowledge the problem, they may not achieve goals for good nutrition or activity. Treating childhood obesity requires identifying and removing the barriers to change.
In this paper, we identify 3 domains of weight management barriers—family, personal, and sociocultural—and offer possible solutions for dismantling the barriers.
Barriers to weight loss
Family: When parents make poor choices
Ideally parents would model a healthy lifestyle, provide a supportive home atmosphere, and reduce family stressors to facilitate weight reduction. However, parental behavior—even when well intentioned—often interferes with what’s best for the child.
For more original research on weight problems in children, see “Detecting overweight children in primary care: Do national data reflect the typical urban practice?”
If parents make inadequate nutritional choices and have a sedentary lifestyle, their children will mimic them. In fact, parent self-report of activity accounted for some of the variance in overweight youth’s physical activity.1
Parents’ food choices and purchasing behaviors may affect how their children purchase both healthy and unhealthy foods.2 Regular family mealtimes with nutritious foods will help adolescents learn to make more positive dietary choices and adopt healthy behaviors.3
In addition, the weight of mothers and fathers influences the weight of their children,4-6 and parent obesity is associated with less physical activity among children.7,8
Parental disciplinary strategies also affect children’s behavior. Authoritarian parents tend to engage in a battle of wills with children, creating standoffs—eg, when children are forced to sit at the table for hours to try fruits and vegetables or other new items.9
Authoritarian parenting was associated with the highest risk of overweight among young children.10 However, parental control of food intake and structured planning of healthy behaviors is not always negative.11,12
Parents often do not see their children as overweight even when they are. Parents may actually view heavy children as being healthy and a sign of successful parenting.4,13 They may use terms such as “thick” or “solid” rather than “overweight.” Some parents acknowledge weight problems only if their child is the object of teasing or exhibits physical limitations.14
Deflected responsibility. Furthermore, parents often attribute weight difficulties to an inherited propensity, citing multiple overweight family members while disregarding the influence of the home environment on weight status.15
Personal barriers: A need for empowerment
In a behaviorally oriented weight-control program for youth, significant predictors of weight loss were the child’s beliefs regarding personal control over weight, perceived difficulty of losing weight, attribution of obesity to their medical problems or family problems, and perceived willingness of family members to diet.16
Sometimes motivation is lacking. The importance of motivation in getting obese children to exercise is well established.7,17 Inaction may be due to a lack of information or to insufficient maturity to see that change is needed to protect health.
Psychosocial problems are more prevalent among overweight youth than among their peers at normal weight.18 In the past 10 years, published research on the psychiatric aspects of pediatric obesity shows increased rates of depression, anxiety, and low self-esteem,19 which can be significant barriers to change.20 Emotional difficulties can increase distress that contributes to binging and overeating,19 limit physical activity, and impair motivation to change by increasing helplessness and hopelessness.20,21
Comorbid physical conditions can affect activity goals (juvenile arthritis, hemophilia, asthma, etc) or dietary goals (diabetes, food allergies, etc).
Limited knowledge about nutrition and exercise can hinder behavioral change. Weight management goals, for instance, are often too broad or vague to be of help to children and their families. They need specific details. Much of the public misunderstands important nutritional concepts—portion size, balanced meal, metabolism, healthy eating, and low fat. For example, children believed a food product labeled “diet” was healthy.
Physical activity concepts are also often misunderstood by patients; for example, “screen time,” moderate intensity, cardiovascular fitness, and low impact. Using nutrition and activity terminology with patients does not guarantee good communication or goal achievement. Information and awareness, as well as myths and misinformation, were found to be barriers to weight improvement.22
Sociocultural barriers: A “fast food” culture and ever-present bias
Multiple studies have cited increased consumption of high energy/low cost foods including carbohydrates,23,24 fats, and sugars23,25 as a cause of child obesity. Many foods thought to be central to a healthy diet are perceived by some caregivers as too costly.9 The good taste, convenient preparation, and lower cost of foods with refined grains and added sugars and fats increase their popularity.26,27
Some neighborhood environments limit access to fruits and vegetables,28 resulting in increased rates of obesity. Restaurants, including the “fast food” kind, often serve large portions of unhealthy foods and thereby promote the ingestion of portions that are, literally, out of proportion to reason.29 Nutrient-dense lean meats, fish, and fruits and vegetables cost more per serving and do not satiate appetites as readily.
Unsafe neighborhoods cause significant anxiety in inner city parents and children30 and may discourage physical activity, thus increasing risk of overweight.31 In a study involving 20 large US cities, mothers’ perceptions of neighborhood safety related to their children’s television viewing time,32 and television viewing time has been shown to have a negative relationship to increased body mass index (BMI) in youth.33-35
Obese children may avoid physical activities that involve peers. Peers exert increasing influence on children and adolescents and ostracize those who are different. Bell et al showed that young children were less willing to engage an obese peer in physical activities,36 and overweight and obese children are more likely to be the victims of bullying as well as more likely to be the perpetrators of bullying than are normal weight peers.37
Although rates of childhood obesity among the general population are alarmingly high, they are higher still in ethnic minority and low-income communities.38 Low-income and minority children watch more television than white, non-poor children do. Neighborhoods where low-income and minority children live typically have more fast food restaurants and fewer vendors of healthful foods than do wealthier or predominantly white neighborhoods. Obstacles cited by Kumanyika38 are unsafe streets, dilapidated parks, and lack of facilities. In Hispanic youth, barriers in the school system include lack of facilities, equipment, and trained staff for physical education.39 Hispanic children are more sedentary than are white children40 and resultantly overweight.41
Enlist other caregivers to strengthen a treatment plan
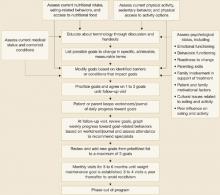
We promote a multidisciplinary approach—the short- and long-term benefits of which are supported by data59—to treating overweight youth: parental involvement, nutrition education, physical activity education, and behavior modification.42 Coordination among the healthcare professionals is important to avoid giving mixed messages to patients and to learn what each discipline uniquely discovers about barriers and ways to surmount them. Combining perspectives and information should lead to a stronger treatment plan (FIGURE) and greater treatment success. Online resources like the USDA’s MyPyramid.gov, are available to clinicians who do not have access to multidisciplinary clinic facilities.
Parents’ attitudes influence the child
Assess the family’s level of concern and willingness to participate in a treatment plan.44-46 Parents’ involvement is critical, especially given that parental concern about weight is a predictor of change in total fat mass over time, at least in Caucasian children.14 Only when parents see a child’s weight as a health problem are they likely to be motivated toward changing.43
Research suggests that the parents’ attitude toward physical activity affects a child’s attitude toward physical activity.19,47 In fact, parent changes in BMI have been found to predict child changes in BMI for overweight youth.48
Clinicians need to inform and engage family members in the assessment and behavioral change processes, uncover erroneous belief systems, identify family dynamics that may affect treatment, and assess parenting skills. For instance, feeding children every time they say they are hungry might not be in their best interest, especially if the food is used to satiate or modify emotions and behaviors. Parents need to understand how their roles in addressing nutrition and physical activity change as their children move through different developmental periods,49 suggesting a flexible parenting style that evolves as the child ages.
One method to determine the parental choices and behavior is to ask parents to keep a record of what the child eats and in what portion size. How much and what kind of exercise does the child receive? Over time, patterns emerge that allow a clinician to formulate a treatment plan based on eating and physical activity modification.
FIGURE
Key steps in managing overweight in children and youths
Identify the personal goals that motivate a child
Overweight youth motivated to change are more likely to exercise7,17 and make healthier nutritional choices.50 A child in the preparation/action stage of change is highly motivated to make changes.43 Often multiple discussions are needed before a patient is ready to make changes. Keep in mind when having these discussions that patients can be motivated by different goals (increased athleticism, appearance, social acceptance).
For patients with comorbid medical disorders, modify nutrition and activity recommendations accordingly. Patients with emotional or behavioral disorders may need to see a psychologist or psychiatrist who can evaluate for and treat the issues.46 Psychologist-led group therapy sessions for the youth and/or their parents can also be helpful in providing support and positive peer modeling.51 If significant family stress or negative family dynamics are present, a referral for family therapy could be helpful.
Educate patients and caregivers about nutritional foods
Some patients and their families need assistance in learning how to buy healthful foods on a limited income. For others, learning how to budget and distribute food throughout the month is important.
Omar et al9 reported that male caregivers were most interested in learning about nutritional food choices, and that female caregivers were most interested in time-cutting measures for feeding their children. Caregivers, in general, relied on other family members for most nutrition information, some of which was inaccurate. This disparity among caregivers opens avenues for educating families, and in some cases must include the extended family. Furthermore, misunderstandings of the meanings of common terms can be avoided with a review or educational handouts.52
Finally, your advocacy for better laws, school policies, and social services can positively affect the cost of food, access to healthy foods, and neighborhood safety.
Provide physical activity choices
Provide a list of no-cost or low-cost options for exercise.52 With the child’s or teen’s input, list all the physical activities they enjoy7 and review other activities that they might like to try. Contact community centers and local parks and recreation services for a list of child-appropriate low-cost or no-cost physical activities available and add them to the list. Emphasizing activities that the child/teen finds enjoyable will enhance willingness to participate and consistency.
Sometimes, several short bursts of physical activity are more logistically possible than a longer bout, and may be more reinforcing for children and adolescents.53 Sothern et al54 recommend physical exercise that is both structured and progressive. Walking 15 minutes a day, 3 times a week, and gradually increasing the time and intensity is both structured and progressive.
Introduce behavior modification
Prioritize changes or goals. Changing specific eating and activity behaviors is more realistic than setting a weight management goal,44 because behaviors are easily identifiable, and changing them will likely yield health benefits before weight loss occurs.55 Overweight children need reminding that even if they maintain their weight, they will often grow in height, improving their BMI.
Once you have emphasized the importance of behavioral changes, set specific changes as goals. For example, “decrease intake of drinks containing sugar such as juice, sweet tea, or soft drinks to 1 or less per week” or “move from 0 minutes of physical activity to 15 minutes per day.” Move toward initial goals slowly so they can be achieved, and build positive momentum toward further changes. Assess nutrition and activity goals regularly and refine and revise goals as needed.
Carefully tracking progress toward treatment goals will also help you assess where additional barriers might be and motivate and energize patients who are making changes. When goals are not met, ask patients “why” in a nonjudgmental manner; this approach might disclose other unforeseen barriers and lead to a problem-solving discussion that can overcome them.
Traditional behavioral modification techniques apply to nutrition and physical activity changes. Rewarding progress can increase compliance and motivation to maintain changes and set new goals. Stimulus control techniques can also be helpful (eating at the table, not in front of the TV). Another technique that can work is making sedentary activities such as time spent in front of a television or computer contingent upon completion of physical activity.56,57 This technique, called the Premack Principle58 involves using a favorite, high-frequency activity as a reward for a behavior you would like to increase, such as physical activity. The patient is only allowed to engage in this favorite, high frequency activity as a reward for achieving a daily goal.
Conclusion: On transcending barriers to change
Multiple barriers to controlling childhood overweight are possible. Addressing weight status and related nutritional and activity behaviors is difficult if potential barriers are not recognized and addressed at the outset. Careful tracking of progress toward treatment goals is also important to find additional barriers and motivate patients. When goals are not met, asking the patients why in a nonjudgmental manner might disclose other unforeseen barriers and lead to a problem-solving discussion.
Data support the short- and long-term benefits of a multidisciplinary approach to treating overweight youth.59 Parents can help children change their eating and activity behaviors by modeling healthful behaviors, providing a home environment that makes it easy to make healthful choices, focusing less on weight and more on overall health, and providing a supportive environment for their children to enhance communication.60
Transcending the barriers to change involves lifestyle interventions. A multidisciplinary treatment approach is recommended, one that addresses family-centered treatment, nutrition and physical activity education, and behavior modification.61 Coordination between healthcare professionals is important to avoid giving mixed messages to patients. Combining perspectives and information should lead to a stronger treatment plan and greater treatment success.
CORRESPONDENCE
Wendy Ward-Begnoche, PhD, Assistant Professor, Department of Pediatrics, College of Medicine, University of Arkansas for Medical Sciences, 800 Marshall St. $ 512-21, Little Rock, AR 72202. E-mail: [email protected]
1. Epstein LH, Paluch RA, Coleman KJ, Vito D, Anderson K. Determinants of physical activity in obese children assessed by accelerometer and self-report. Med Sci Sports Exerc 1996;28:1157-1164.
2. Epstein LH, Dearing KK, Handley EA, Roemmich JN, Paluch RA. Relationship of mother and child food purchases as a function of price: a pilot study. Appetite 2006;47:115-118.
3. Cason KL. Family mealtimes: more than just eating together. J Am Diet Assoc 2006;106:532-533.
4. Baughcum AE, Chamberlin LA, Deeks CM, Powers SW, Whitaker RC. Maternal perceptions of overweight preschool children. Pediatrics 2000;106:1380-1386.
5. Golan M, Weizman A, Fainaru M. Impact of treatment for childhood obesity on parental risk factors for cardiovascular disease. Prev Med 1999;29:519-526.
6. Strauss RS, Knight J. Influence of the home environment on the development of obesity in children. Pediatrics 1999;103(6):e85-92.
7. Sallis J, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc 2000;32:963-975.
8. Treuth MS, Butte NF, Adolph AL, Puyau MR. A longitudinal study of fitness and activity in girls predisposed to obesity. Med Sci Sports Exerc 2004;36:198-204.
9. Omar MA, Coleman G, Hoerr S. Healthy eating for rural low-income toddlers: caregivers’ perceptions. J Community Health Nurs 2001;18:93-106.
10. Rhee KE, Lumeng JC, Appugliese DP, Kaciroti N, Bradley RH. Parenting styles and overweight status in first grade. Pediatrics 2006;117:2047-2054.
11. Chen JL, Kennedy C. Family functioning parenting style and Chinese children’s weight status. J Fam Nursing 2004;10:262-279.
12. Ogden J, Reynolds R, Smith A. Expanding the concept of parental control: a role for overt and covert control in children’s snacking behaviour? Appetite 2006;7(1):100-106.
13. Adams AK, Quinn RA, Prince RJ. Low recognition of childhood overweight and disease risk among Native-American caregivers. Obes Res 2005;13:146-152.
14. Jain A, Sherman SN, Chamberlin LA, Carter Y, Powers SW, Whitaker RC. Why don’t low-income mothers worry about their preschoolers being overweight? Pediatrics 2001;107:1138-1146.
15. Faulkner MS. Low income mothers of overweight children had personal and environmental challenges in preventing and managing obesity. Evidence-Based Nursing 2002;5:27.-
16. Uzark KC, Becker MH, Dielman TE, Rocchini AP. Psychosocial predictors of compliance with a weight control intervention for obese children and adolescents. J Compliance Health Care 1987;2:167-178.
17. McWhorter JW, Wallmann HW, Alpert PT. The obese child: motivation as a tool for exercise. J Pediatr Healthcare 2003;17:11-17.
18. Young-Hyman D, Schlundt DG, Herman-Wenderoth L, Bozylinski K. Obesity appearance and psychosocial adaptation on young African American children. J Pediatr Psychol 2003;28:463-472.
19. Zametkin AJ, Zoon CK, Klein HW, Munson S. Psychiatric aspects of child and adolescent obesity: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 2004;43:134-150.
20. Strauss RS. Childhood obesity and self-esteem. Pediatrics 2000;105:e15-19.
21. Pesa JA, Syre TR, Jones E. Psychosocial differences associated with body weight among female adolescents: the importance of body image. J Adolesc Health 2000;26:330-337.
22. Hesketh K, Waters E, Green J, Salmon L, Williams J. Healthy eating activity and obesity prevention: a qualitative study of parent and child perceptions in Australia. Health Promotion Intl 2005;20:19-26.
23. Nicklas TA, Yang S-J, Baranowski T, Zakeri I, Berenson G. Eating patterns and obesity in children: the Bogalusa heart study. Am J Prev Med 2003;25:9-16.
24. Nielsen BM, Bjørnsbo K, Tetens I, Heitmann BL. Dietary glycaemic index and glycaemic load in Danish children in relation to body fatness. Br J Nutr 2005;94:992-997.
25. Troiano RP, Briefel RR, Carroll MD, Bailostosky K. Energy and fat intakes of children and adolescents in the United States: data from the National Health and Nutrition Examination Surveys. Am J Clin Nutr 2000;72(Suppl):1343S-1353S.
26. Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr 2005;82:265S-273S.
27. Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr 2004;79:6-16.
28. Sallis JF, Glanz K. The role of built environments in physical activity eating and obesity in childhood. Future Child 2006;16:89-108.
29. Young LR, Nestle M. Expanding portion sizes in the US marketplace: implications for nutrition counseling. J Am Diet Assoc 2003;103:231-234.
30. Weir LA, Etelson D, Brand DA. Parents’ perceptions of neighborhood safety and children’s physical activity. Prev Med 2006;43:212-217.
31. Lumeng J. What can we do to prevent childhood obesity? Zero to Three 2005;25:13-19.
32. Burdette HL, Whitaker RC. A national study of neighborhood safety outdoor play television viewing and obesity in preschool children. Pediatrics 2005;116:657-662.
33. Andersen RE, Crespo CJ, Bartlett SJ, Cheskin LJ, Pratt M. Relationship of physical activity and television watching with body weight and level of fatness among children. JAMA 1998;279:938-942.
34. Proctor MH, Moore LL, Gao D, et al. Television viewing and change in body fat from preschool to early adolescence: the Framingham Children’s Study. Int J Obes 2003;27:827-833.
35. Salmon J, Campbell KJ, Crawford DA. Television viewing habits associated with obesity risk factors: a survey of Melbourne schoolchildren. Med J Aust 2006;184:64-67.
36. Bell SK, Morgan SB. Children’s attitudes and behavioral intentions toward a peer presented as obese: does a medical explanation for the obesity make a difference? J Pediatr Psychol 2000;25:137-145.
37. Janssen I, Craig WM, Boyce WF, Pickett W. Associations between overweight and obesity with bullying behaviors in school-aged children. Pediatrics 2004;113:1187-1194.
38. Kumanyika S, Grier S. Targeting interventions for ethnic minority and low-income populations. Future Child 2006;16:187-207.
39. Thompson JL, Davis SM, Gittelsohn J, et al. Patterns of physical activity among American Indian children: An assessment of barriers and support. J Comm Health 2001;26:407-421.
40. Mirza NM, Kadow K, Palmer M, Solano H, Rosche C, Yanovski JA. Prevalence of overweight among inner city Hispanic-American children and adolescents. Obes Res 2004;12:1298-1310.
41. Ritchie LD, Ivey SL, Woodward-Lopez G, Crawford PB. Alarming trends in pediatric overweight in the United States. Soz Praventivmed 2003;48:168-177.
42. Jefferson A. Breaking down barriers—examining health promoting behaviour in the family. Kellogg’s Family Health Study 2005. Nutr Bull 2006;31:60-64.
43. Rhee KE, DeLago CW, Arscott-Mills T, Mehta SD, Davis RK. Factors associated with parental readiness to make changes for overweight children. Pediatrics 2005;116:e94-101.
44. Dietz WH. Childhood obesity: susceptibility cause and management. J Pediatr 1983;103:676-686.
45. Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year outcomes of behavioral family-based treatment for childhood obesity. Health Psychol 1994;13:373-383.
46. Vila F, Zipper E, Dabbas M, et al. Mental disorders in obese children and adolescents. Psychosom Med 2004;66:387-394.
47. Levine MD, Ringham RM, Kalarchian MA, Wisniewski L, Marcus MD. Is family-based behavioral weight control appropriate for severe pediatric obesity? Int J Eat Disord 2001;30:318-328.
48. Wrotniak BH, Epstein LH, Paluch RA, Roemmich JN. Parent weight change as a predictor of child weight change in family-based behavioral obesity treatment. Arch Pediatr Adolesc Med 2004;158:342-347.
49. Lindsay AC, Sussner KM, Kim J, Gortmaker SL. The role of parents in preventing childhood obesity. Future Child 2006;16:169-186.
50. Carruth BR, Skinner JD. The role of dietary calcium and other nutrients in moderating body fat in preschool children. Int J Obes 2001;25:559-566.
51. Eissa MAH, Gunner KB. Evaluation and management of obesity in children and adolescents. J Pediatr Health Care 2003;18:35-38.
52. Ward-Begnoche W, Gance-Cleveland B. Promoting behavioral change in overweight youth. J Pediatr Health Care 2005;19:318-328.
53. Epstein LH, Paluch RA, Kalakanis LE, Goldfield GS, Cerny FJ, Roemmich JN. How much activity do youth get? A quantitative review of heart-rate measured activity. Pediatrics 2001;108:e44.-
54. Sothern MS, Hunter S, Suskind RM, Brown R, Udall JN, Blecker U. Motivating the obese child to move: the role of structured exercise in pediatric weight management. South Med J 1999;92:577-584.
55. Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson J-L, Garg A, et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care 2002;25:148-198.
56. Faith M, Berman N, Heo M, et al. Effects of contingent television on physical activity and television viewing in obese children. Pediatrics 2001;107:1043-1048.
57. Goldfield GS, Kalakanis LE, Ernst MM, Epstein LH. Open-loop feedback to increase physical activity on obese children. Int J Obes 2000;24:888-892.
58. Premack D. Reversibility of the reinforcement relation. Science 1962;136:255-257.
59. Nemet D, Barkan S, Epstein Y, Friedland O, Kowen G, Eliakim A. Short- and long-term beneficial effects of a combined dietary-behavioral-physical activity intervention for the treatment of childhood obesity. Pediatrics 2005;115:e443-449.
60. Neumark-Sztainer D. Preventing the broad spectrum of weight-related problems: working with parents to help teens achieve a healthy weight and a positive body image. J Nutr Educ Behav 2005;37(Suppl 2):S135-S139.
61. Flodmark C-E, Lissau I, Moreno LA, Pietrobelli A, Widhalm K. New insights into the field of children and adolescents’ obesity: the European perspective. Int J Obes 2004;28:1189-1196.
- To motivate change, help parents to realize that overweight in their child is a health risk and not merely an aesthetic concern (C).
- Keep in mind that children can be motivated by different goals, such as increased athleticism, appearance, or social acceptance (C).
- Several short bursts of physical activity are usually more feasible than longer bouts, and may be more reinforcing for children and adolescents (C).
- Changing specific eating and activity behaviors is more realistic than setting a weight management goal (C).
My child doesn’t have a weight problem. We’re a family of big eaters, that’s all.” If you’ve heard this explanation or ones like it after raising a concern about a child’s weight, chances are you will encounter barriers to recognizing obesity and to changing the behavior that encourages it.
Even when parents and a significantly overweight child or adolescent acknowledge the problem, they may not achieve goals for good nutrition or activity. Treating childhood obesity requires identifying and removing the barriers to change.
In this paper, we identify 3 domains of weight management barriers—family, personal, and sociocultural—and offer possible solutions for dismantling the barriers.
Barriers to weight loss
Family: When parents make poor choices
Ideally parents would model a healthy lifestyle, provide a supportive home atmosphere, and reduce family stressors to facilitate weight reduction. However, parental behavior—even when well intentioned—often interferes with what’s best for the child.
For more original research on weight problems in children, see “Detecting overweight children in primary care: Do national data reflect the typical urban practice?”
If parents make inadequate nutritional choices and have a sedentary lifestyle, their children will mimic them. In fact, parent self-report of activity accounted for some of the variance in overweight youth’s physical activity.1
Parents’ food choices and purchasing behaviors may affect how their children purchase both healthy and unhealthy foods.2 Regular family mealtimes with nutritious foods will help adolescents learn to make more positive dietary choices and adopt healthy behaviors.3
In addition, the weight of mothers and fathers influences the weight of their children,4-6 and parent obesity is associated with less physical activity among children.7,8
Parental disciplinary strategies also affect children’s behavior. Authoritarian parents tend to engage in a battle of wills with children, creating standoffs—eg, when children are forced to sit at the table for hours to try fruits and vegetables or other new items.9
Authoritarian parenting was associated with the highest risk of overweight among young children.10 However, parental control of food intake and structured planning of healthy behaviors is not always negative.11,12
Parents often do not see their children as overweight even when they are. Parents may actually view heavy children as being healthy and a sign of successful parenting.4,13 They may use terms such as “thick” or “solid” rather than “overweight.” Some parents acknowledge weight problems only if their child is the object of teasing or exhibits physical limitations.14
Deflected responsibility. Furthermore, parents often attribute weight difficulties to an inherited propensity, citing multiple overweight family members while disregarding the influence of the home environment on weight status.15
Personal barriers: A need for empowerment
In a behaviorally oriented weight-control program for youth, significant predictors of weight loss were the child’s beliefs regarding personal control over weight, perceived difficulty of losing weight, attribution of obesity to their medical problems or family problems, and perceived willingness of family members to diet.16
Sometimes motivation is lacking. The importance of motivation in getting obese children to exercise is well established.7,17 Inaction may be due to a lack of information or to insufficient maturity to see that change is needed to protect health.
Psychosocial problems are more prevalent among overweight youth than among their peers at normal weight.18 In the past 10 years, published research on the psychiatric aspects of pediatric obesity shows increased rates of depression, anxiety, and low self-esteem,19 which can be significant barriers to change.20 Emotional difficulties can increase distress that contributes to binging and overeating,19 limit physical activity, and impair motivation to change by increasing helplessness and hopelessness.20,21
Comorbid physical conditions can affect activity goals (juvenile arthritis, hemophilia, asthma, etc) or dietary goals (diabetes, food allergies, etc).
Limited knowledge about nutrition and exercise can hinder behavioral change. Weight management goals, for instance, are often too broad or vague to be of help to children and their families. They need specific details. Much of the public misunderstands important nutritional concepts—portion size, balanced meal, metabolism, healthy eating, and low fat. For example, children believed a food product labeled “diet” was healthy.
Physical activity concepts are also often misunderstood by patients; for example, “screen time,” moderate intensity, cardiovascular fitness, and low impact. Using nutrition and activity terminology with patients does not guarantee good communication or goal achievement. Information and awareness, as well as myths and misinformation, were found to be barriers to weight improvement.22
Sociocultural barriers: A “fast food” culture and ever-present bias
Multiple studies have cited increased consumption of high energy/low cost foods including carbohydrates,23,24 fats, and sugars23,25 as a cause of child obesity. Many foods thought to be central to a healthy diet are perceived by some caregivers as too costly.9 The good taste, convenient preparation, and lower cost of foods with refined grains and added sugars and fats increase their popularity.26,27
Some neighborhood environments limit access to fruits and vegetables,28 resulting in increased rates of obesity. Restaurants, including the “fast food” kind, often serve large portions of unhealthy foods and thereby promote the ingestion of portions that are, literally, out of proportion to reason.29 Nutrient-dense lean meats, fish, and fruits and vegetables cost more per serving and do not satiate appetites as readily.
Unsafe neighborhoods cause significant anxiety in inner city parents and children30 and may discourage physical activity, thus increasing risk of overweight.31 In a study involving 20 large US cities, mothers’ perceptions of neighborhood safety related to their children’s television viewing time,32 and television viewing time has been shown to have a negative relationship to increased body mass index (BMI) in youth.33-35
Obese children may avoid physical activities that involve peers. Peers exert increasing influence on children and adolescents and ostracize those who are different. Bell et al showed that young children were less willing to engage an obese peer in physical activities,36 and overweight and obese children are more likely to be the victims of bullying as well as more likely to be the perpetrators of bullying than are normal weight peers.37
Although rates of childhood obesity among the general population are alarmingly high, they are higher still in ethnic minority and low-income communities.38 Low-income and minority children watch more television than white, non-poor children do. Neighborhoods where low-income and minority children live typically have more fast food restaurants and fewer vendors of healthful foods than do wealthier or predominantly white neighborhoods. Obstacles cited by Kumanyika38 are unsafe streets, dilapidated parks, and lack of facilities. In Hispanic youth, barriers in the school system include lack of facilities, equipment, and trained staff for physical education.39 Hispanic children are more sedentary than are white children40 and resultantly overweight.41
Enlist other caregivers to strengthen a treatment plan
We promote a multidisciplinary approach—the short- and long-term benefits of which are supported by data59—to treating overweight youth: parental involvement, nutrition education, physical activity education, and behavior modification.42 Coordination among the healthcare professionals is important to avoid giving mixed messages to patients and to learn what each discipline uniquely discovers about barriers and ways to surmount them. Combining perspectives and information should lead to a stronger treatment plan (FIGURE) and greater treatment success. Online resources like the USDA’s MyPyramid.gov, are available to clinicians who do not have access to multidisciplinary clinic facilities.
Parents’ attitudes influence the child
Assess the family’s level of concern and willingness to participate in a treatment plan.44-46 Parents’ involvement is critical, especially given that parental concern about weight is a predictor of change in total fat mass over time, at least in Caucasian children.14 Only when parents see a child’s weight as a health problem are they likely to be motivated toward changing.43
Research suggests that the parents’ attitude toward physical activity affects a child’s attitude toward physical activity.19,47 In fact, parent changes in BMI have been found to predict child changes in BMI for overweight youth.48
Clinicians need to inform and engage family members in the assessment and behavioral change processes, uncover erroneous belief systems, identify family dynamics that may affect treatment, and assess parenting skills. For instance, feeding children every time they say they are hungry might not be in their best interest, especially if the food is used to satiate or modify emotions and behaviors. Parents need to understand how their roles in addressing nutrition and physical activity change as their children move through different developmental periods,49 suggesting a flexible parenting style that evolves as the child ages.
One method to determine the parental choices and behavior is to ask parents to keep a record of what the child eats and in what portion size. How much and what kind of exercise does the child receive? Over time, patterns emerge that allow a clinician to formulate a treatment plan based on eating and physical activity modification.
FIGURE
Key steps in managing overweight in children and youths
Identify the personal goals that motivate a child
Overweight youth motivated to change are more likely to exercise7,17 and make healthier nutritional choices.50 A child in the preparation/action stage of change is highly motivated to make changes.43 Often multiple discussions are needed before a patient is ready to make changes. Keep in mind when having these discussions that patients can be motivated by different goals (increased athleticism, appearance, social acceptance).
For patients with comorbid medical disorders, modify nutrition and activity recommendations accordingly. Patients with emotional or behavioral disorders may need to see a psychologist or psychiatrist who can evaluate for and treat the issues.46 Psychologist-led group therapy sessions for the youth and/or their parents can also be helpful in providing support and positive peer modeling.51 If significant family stress or negative family dynamics are present, a referral for family therapy could be helpful.
Educate patients and caregivers about nutritional foods
Some patients and their families need assistance in learning how to buy healthful foods on a limited income. For others, learning how to budget and distribute food throughout the month is important.
Omar et al9 reported that male caregivers were most interested in learning about nutritional food choices, and that female caregivers were most interested in time-cutting measures for feeding their children. Caregivers, in general, relied on other family members for most nutrition information, some of which was inaccurate. This disparity among caregivers opens avenues for educating families, and in some cases must include the extended family. Furthermore, misunderstandings of the meanings of common terms can be avoided with a review or educational handouts.52
Finally, your advocacy for better laws, school policies, and social services can positively affect the cost of food, access to healthy foods, and neighborhood safety.
Provide physical activity choices
Provide a list of no-cost or low-cost options for exercise.52 With the child’s or teen’s input, list all the physical activities they enjoy7 and review other activities that they might like to try. Contact community centers and local parks and recreation services for a list of child-appropriate low-cost or no-cost physical activities available and add them to the list. Emphasizing activities that the child/teen finds enjoyable will enhance willingness to participate and consistency.
Sometimes, several short bursts of physical activity are more logistically possible than a longer bout, and may be more reinforcing for children and adolescents.53 Sothern et al54 recommend physical exercise that is both structured and progressive. Walking 15 minutes a day, 3 times a week, and gradually increasing the time and intensity is both structured and progressive.
Introduce behavior modification
Prioritize changes or goals. Changing specific eating and activity behaviors is more realistic than setting a weight management goal,44 because behaviors are easily identifiable, and changing them will likely yield health benefits before weight loss occurs.55 Overweight children need reminding that even if they maintain their weight, they will often grow in height, improving their BMI.
Once you have emphasized the importance of behavioral changes, set specific changes as goals. For example, “decrease intake of drinks containing sugar such as juice, sweet tea, or soft drinks to 1 or less per week” or “move from 0 minutes of physical activity to 15 minutes per day.” Move toward initial goals slowly so they can be achieved, and build positive momentum toward further changes. Assess nutrition and activity goals regularly and refine and revise goals as needed.
Carefully tracking progress toward treatment goals will also help you assess where additional barriers might be and motivate and energize patients who are making changes. When goals are not met, ask patients “why” in a nonjudgmental manner; this approach might disclose other unforeseen barriers and lead to a problem-solving discussion that can overcome them.
Traditional behavioral modification techniques apply to nutrition and physical activity changes. Rewarding progress can increase compliance and motivation to maintain changes and set new goals. Stimulus control techniques can also be helpful (eating at the table, not in front of the TV). Another technique that can work is making sedentary activities such as time spent in front of a television or computer contingent upon completion of physical activity.56,57 This technique, called the Premack Principle58 involves using a favorite, high-frequency activity as a reward for a behavior you would like to increase, such as physical activity. The patient is only allowed to engage in this favorite, high frequency activity as a reward for achieving a daily goal.
Conclusion: On transcending barriers to change
Multiple barriers to controlling childhood overweight are possible. Addressing weight status and related nutritional and activity behaviors is difficult if potential barriers are not recognized and addressed at the outset. Careful tracking of progress toward treatment goals is also important to find additional barriers and motivate patients. When goals are not met, asking the patients why in a nonjudgmental manner might disclose other unforeseen barriers and lead to a problem-solving discussion.
Data support the short- and long-term benefits of a multidisciplinary approach to treating overweight youth.59 Parents can help children change their eating and activity behaviors by modeling healthful behaviors, providing a home environment that makes it easy to make healthful choices, focusing less on weight and more on overall health, and providing a supportive environment for their children to enhance communication.60
Transcending the barriers to change involves lifestyle interventions. A multidisciplinary treatment approach is recommended, one that addresses family-centered treatment, nutrition and physical activity education, and behavior modification.61 Coordination between healthcare professionals is important to avoid giving mixed messages to patients. Combining perspectives and information should lead to a stronger treatment plan and greater treatment success.
CORRESPONDENCE
Wendy Ward-Begnoche, PhD, Assistant Professor, Department of Pediatrics, College of Medicine, University of Arkansas for Medical Sciences, 800 Marshall St. $ 512-21, Little Rock, AR 72202. E-mail: [email protected]
- To motivate change, help parents to realize that overweight in their child is a health risk and not merely an aesthetic concern (C).
- Keep in mind that children can be motivated by different goals, such as increased athleticism, appearance, or social acceptance (C).
- Several short bursts of physical activity are usually more feasible than longer bouts, and may be more reinforcing for children and adolescents (C).
- Changing specific eating and activity behaviors is more realistic than setting a weight management goal (C).
My child doesn’t have a weight problem. We’re a family of big eaters, that’s all.” If you’ve heard this explanation or ones like it after raising a concern about a child’s weight, chances are you will encounter barriers to recognizing obesity and to changing the behavior that encourages it.
Even when parents and a significantly overweight child or adolescent acknowledge the problem, they may not achieve goals for good nutrition or activity. Treating childhood obesity requires identifying and removing the barriers to change.
In this paper, we identify 3 domains of weight management barriers—family, personal, and sociocultural—and offer possible solutions for dismantling the barriers.
Barriers to weight loss
Family: When parents make poor choices
Ideally parents would model a healthy lifestyle, provide a supportive home atmosphere, and reduce family stressors to facilitate weight reduction. However, parental behavior—even when well intentioned—often interferes with what’s best for the child.
For more original research on weight problems in children, see “Detecting overweight children in primary care: Do national data reflect the typical urban practice?”
If parents make inadequate nutritional choices and have a sedentary lifestyle, their children will mimic them. In fact, parent self-report of activity accounted for some of the variance in overweight youth’s physical activity.1
Parents’ food choices and purchasing behaviors may affect how their children purchase both healthy and unhealthy foods.2 Regular family mealtimes with nutritious foods will help adolescents learn to make more positive dietary choices and adopt healthy behaviors.3
In addition, the weight of mothers and fathers influences the weight of their children,4-6 and parent obesity is associated with less physical activity among children.7,8
Parental disciplinary strategies also affect children’s behavior. Authoritarian parents tend to engage in a battle of wills with children, creating standoffs—eg, when children are forced to sit at the table for hours to try fruits and vegetables or other new items.9
Authoritarian parenting was associated with the highest risk of overweight among young children.10 However, parental control of food intake and structured planning of healthy behaviors is not always negative.11,12
Parents often do not see their children as overweight even when they are. Parents may actually view heavy children as being healthy and a sign of successful parenting.4,13 They may use terms such as “thick” or “solid” rather than “overweight.” Some parents acknowledge weight problems only if their child is the object of teasing or exhibits physical limitations.14
Deflected responsibility. Furthermore, parents often attribute weight difficulties to an inherited propensity, citing multiple overweight family members while disregarding the influence of the home environment on weight status.15
Personal barriers: A need for empowerment
In a behaviorally oriented weight-control program for youth, significant predictors of weight loss were the child’s beliefs regarding personal control over weight, perceived difficulty of losing weight, attribution of obesity to their medical problems or family problems, and perceived willingness of family members to diet.16
Sometimes motivation is lacking. The importance of motivation in getting obese children to exercise is well established.7,17 Inaction may be due to a lack of information or to insufficient maturity to see that change is needed to protect health.
Psychosocial problems are more prevalent among overweight youth than among their peers at normal weight.18 In the past 10 years, published research on the psychiatric aspects of pediatric obesity shows increased rates of depression, anxiety, and low self-esteem,19 which can be significant barriers to change.20 Emotional difficulties can increase distress that contributes to binging and overeating,19 limit physical activity, and impair motivation to change by increasing helplessness and hopelessness.20,21
Comorbid physical conditions can affect activity goals (juvenile arthritis, hemophilia, asthma, etc) or dietary goals (diabetes, food allergies, etc).
Limited knowledge about nutrition and exercise can hinder behavioral change. Weight management goals, for instance, are often too broad or vague to be of help to children and their families. They need specific details. Much of the public misunderstands important nutritional concepts—portion size, balanced meal, metabolism, healthy eating, and low fat. For example, children believed a food product labeled “diet” was healthy.
Physical activity concepts are also often misunderstood by patients; for example, “screen time,” moderate intensity, cardiovascular fitness, and low impact. Using nutrition and activity terminology with patients does not guarantee good communication or goal achievement. Information and awareness, as well as myths and misinformation, were found to be barriers to weight improvement.22
Sociocultural barriers: A “fast food” culture and ever-present bias
Multiple studies have cited increased consumption of high energy/low cost foods including carbohydrates,23,24 fats, and sugars23,25 as a cause of child obesity. Many foods thought to be central to a healthy diet are perceived by some caregivers as too costly.9 The good taste, convenient preparation, and lower cost of foods with refined grains and added sugars and fats increase their popularity.26,27
Some neighborhood environments limit access to fruits and vegetables,28 resulting in increased rates of obesity. Restaurants, including the “fast food” kind, often serve large portions of unhealthy foods and thereby promote the ingestion of portions that are, literally, out of proportion to reason.29 Nutrient-dense lean meats, fish, and fruits and vegetables cost more per serving and do not satiate appetites as readily.
Unsafe neighborhoods cause significant anxiety in inner city parents and children30 and may discourage physical activity, thus increasing risk of overweight.31 In a study involving 20 large US cities, mothers’ perceptions of neighborhood safety related to their children’s television viewing time,32 and television viewing time has been shown to have a negative relationship to increased body mass index (BMI) in youth.33-35
Obese children may avoid physical activities that involve peers. Peers exert increasing influence on children and adolescents and ostracize those who are different. Bell et al showed that young children were less willing to engage an obese peer in physical activities,36 and overweight and obese children are more likely to be the victims of bullying as well as more likely to be the perpetrators of bullying than are normal weight peers.37
Although rates of childhood obesity among the general population are alarmingly high, they are higher still in ethnic minority and low-income communities.38 Low-income and minority children watch more television than white, non-poor children do. Neighborhoods where low-income and minority children live typically have more fast food restaurants and fewer vendors of healthful foods than do wealthier or predominantly white neighborhoods. Obstacles cited by Kumanyika38 are unsafe streets, dilapidated parks, and lack of facilities. In Hispanic youth, barriers in the school system include lack of facilities, equipment, and trained staff for physical education.39 Hispanic children are more sedentary than are white children40 and resultantly overweight.41
Enlist other caregivers to strengthen a treatment plan
We promote a multidisciplinary approach—the short- and long-term benefits of which are supported by data59—to treating overweight youth: parental involvement, nutrition education, physical activity education, and behavior modification.42 Coordination among the healthcare professionals is important to avoid giving mixed messages to patients and to learn what each discipline uniquely discovers about barriers and ways to surmount them. Combining perspectives and information should lead to a stronger treatment plan (FIGURE) and greater treatment success. Online resources like the USDA’s MyPyramid.gov, are available to clinicians who do not have access to multidisciplinary clinic facilities.
Parents’ attitudes influence the child
Assess the family’s level of concern and willingness to participate in a treatment plan.44-46 Parents’ involvement is critical, especially given that parental concern about weight is a predictor of change in total fat mass over time, at least in Caucasian children.14 Only when parents see a child’s weight as a health problem are they likely to be motivated toward changing.43
Research suggests that the parents’ attitude toward physical activity affects a child’s attitude toward physical activity.19,47 In fact, parent changes in BMI have been found to predict child changes in BMI for overweight youth.48
Clinicians need to inform and engage family members in the assessment and behavioral change processes, uncover erroneous belief systems, identify family dynamics that may affect treatment, and assess parenting skills. For instance, feeding children every time they say they are hungry might not be in their best interest, especially if the food is used to satiate or modify emotions and behaviors. Parents need to understand how their roles in addressing nutrition and physical activity change as their children move through different developmental periods,49 suggesting a flexible parenting style that evolves as the child ages.
One method to determine the parental choices and behavior is to ask parents to keep a record of what the child eats and in what portion size. How much and what kind of exercise does the child receive? Over time, patterns emerge that allow a clinician to formulate a treatment plan based on eating and physical activity modification.
FIGURE
Key steps in managing overweight in children and youths
Identify the personal goals that motivate a child
Overweight youth motivated to change are more likely to exercise7,17 and make healthier nutritional choices.50 A child in the preparation/action stage of change is highly motivated to make changes.43 Often multiple discussions are needed before a patient is ready to make changes. Keep in mind when having these discussions that patients can be motivated by different goals (increased athleticism, appearance, social acceptance).
For patients with comorbid medical disorders, modify nutrition and activity recommendations accordingly. Patients with emotional or behavioral disorders may need to see a psychologist or psychiatrist who can evaluate for and treat the issues.46 Psychologist-led group therapy sessions for the youth and/or their parents can also be helpful in providing support and positive peer modeling.51 If significant family stress or negative family dynamics are present, a referral for family therapy could be helpful.
Educate patients and caregivers about nutritional foods
Some patients and their families need assistance in learning how to buy healthful foods on a limited income. For others, learning how to budget and distribute food throughout the month is important.
Omar et al9 reported that male caregivers were most interested in learning about nutritional food choices, and that female caregivers were most interested in time-cutting measures for feeding their children. Caregivers, in general, relied on other family members for most nutrition information, some of which was inaccurate. This disparity among caregivers opens avenues for educating families, and in some cases must include the extended family. Furthermore, misunderstandings of the meanings of common terms can be avoided with a review or educational handouts.52
Finally, your advocacy for better laws, school policies, and social services can positively affect the cost of food, access to healthy foods, and neighborhood safety.
Provide physical activity choices
Provide a list of no-cost or low-cost options for exercise.52 With the child’s or teen’s input, list all the physical activities they enjoy7 and review other activities that they might like to try. Contact community centers and local parks and recreation services for a list of child-appropriate low-cost or no-cost physical activities available and add them to the list. Emphasizing activities that the child/teen finds enjoyable will enhance willingness to participate and consistency.
Sometimes, several short bursts of physical activity are more logistically possible than a longer bout, and may be more reinforcing for children and adolescents.53 Sothern et al54 recommend physical exercise that is both structured and progressive. Walking 15 minutes a day, 3 times a week, and gradually increasing the time and intensity is both structured and progressive.
Introduce behavior modification
Prioritize changes or goals. Changing specific eating and activity behaviors is more realistic than setting a weight management goal,44 because behaviors are easily identifiable, and changing them will likely yield health benefits before weight loss occurs.55 Overweight children need reminding that even if they maintain their weight, they will often grow in height, improving their BMI.
Once you have emphasized the importance of behavioral changes, set specific changes as goals. For example, “decrease intake of drinks containing sugar such as juice, sweet tea, or soft drinks to 1 or less per week” or “move from 0 minutes of physical activity to 15 minutes per day.” Move toward initial goals slowly so they can be achieved, and build positive momentum toward further changes. Assess nutrition and activity goals regularly and refine and revise goals as needed.
Carefully tracking progress toward treatment goals will also help you assess where additional barriers might be and motivate and energize patients who are making changes. When goals are not met, ask patients “why” in a nonjudgmental manner; this approach might disclose other unforeseen barriers and lead to a problem-solving discussion that can overcome them.
Traditional behavioral modification techniques apply to nutrition and physical activity changes. Rewarding progress can increase compliance and motivation to maintain changes and set new goals. Stimulus control techniques can also be helpful (eating at the table, not in front of the TV). Another technique that can work is making sedentary activities such as time spent in front of a television or computer contingent upon completion of physical activity.56,57 This technique, called the Premack Principle58 involves using a favorite, high-frequency activity as a reward for a behavior you would like to increase, such as physical activity. The patient is only allowed to engage in this favorite, high frequency activity as a reward for achieving a daily goal.
Conclusion: On transcending barriers to change
Multiple barriers to controlling childhood overweight are possible. Addressing weight status and related nutritional and activity behaviors is difficult if potential barriers are not recognized and addressed at the outset. Careful tracking of progress toward treatment goals is also important to find additional barriers and motivate patients. When goals are not met, asking the patients why in a nonjudgmental manner might disclose other unforeseen barriers and lead to a problem-solving discussion.
Data support the short- and long-term benefits of a multidisciplinary approach to treating overweight youth.59 Parents can help children change their eating and activity behaviors by modeling healthful behaviors, providing a home environment that makes it easy to make healthful choices, focusing less on weight and more on overall health, and providing a supportive environment for their children to enhance communication.60
Transcending the barriers to change involves lifestyle interventions. A multidisciplinary treatment approach is recommended, one that addresses family-centered treatment, nutrition and physical activity education, and behavior modification.61 Coordination between healthcare professionals is important to avoid giving mixed messages to patients. Combining perspectives and information should lead to a stronger treatment plan and greater treatment success.
CORRESPONDENCE
Wendy Ward-Begnoche, PhD, Assistant Professor, Department of Pediatrics, College of Medicine, University of Arkansas for Medical Sciences, 800 Marshall St. $ 512-21, Little Rock, AR 72202. E-mail: [email protected]
1. Epstein LH, Paluch RA, Coleman KJ, Vito D, Anderson K. Determinants of physical activity in obese children assessed by accelerometer and self-report. Med Sci Sports Exerc 1996;28:1157-1164.
2. Epstein LH, Dearing KK, Handley EA, Roemmich JN, Paluch RA. Relationship of mother and child food purchases as a function of price: a pilot study. Appetite 2006;47:115-118.
3. Cason KL. Family mealtimes: more than just eating together. J Am Diet Assoc 2006;106:532-533.
4. Baughcum AE, Chamberlin LA, Deeks CM, Powers SW, Whitaker RC. Maternal perceptions of overweight preschool children. Pediatrics 2000;106:1380-1386.
5. Golan M, Weizman A, Fainaru M. Impact of treatment for childhood obesity on parental risk factors for cardiovascular disease. Prev Med 1999;29:519-526.
6. Strauss RS, Knight J. Influence of the home environment on the development of obesity in children. Pediatrics 1999;103(6):e85-92.
7. Sallis J, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc 2000;32:963-975.
8. Treuth MS, Butte NF, Adolph AL, Puyau MR. A longitudinal study of fitness and activity in girls predisposed to obesity. Med Sci Sports Exerc 2004;36:198-204.
9. Omar MA, Coleman G, Hoerr S. Healthy eating for rural low-income toddlers: caregivers’ perceptions. J Community Health Nurs 2001;18:93-106.
10. Rhee KE, Lumeng JC, Appugliese DP, Kaciroti N, Bradley RH. Parenting styles and overweight status in first grade. Pediatrics 2006;117:2047-2054.
11. Chen JL, Kennedy C. Family functioning parenting style and Chinese children’s weight status. J Fam Nursing 2004;10:262-279.
12. Ogden J, Reynolds R, Smith A. Expanding the concept of parental control: a role for overt and covert control in children’s snacking behaviour? Appetite 2006;7(1):100-106.
13. Adams AK, Quinn RA, Prince RJ. Low recognition of childhood overweight and disease risk among Native-American caregivers. Obes Res 2005;13:146-152.
14. Jain A, Sherman SN, Chamberlin LA, Carter Y, Powers SW, Whitaker RC. Why don’t low-income mothers worry about their preschoolers being overweight? Pediatrics 2001;107:1138-1146.
15. Faulkner MS. Low income mothers of overweight children had personal and environmental challenges in preventing and managing obesity. Evidence-Based Nursing 2002;5:27.-
16. Uzark KC, Becker MH, Dielman TE, Rocchini AP. Psychosocial predictors of compliance with a weight control intervention for obese children and adolescents. J Compliance Health Care 1987;2:167-178.
17. McWhorter JW, Wallmann HW, Alpert PT. The obese child: motivation as a tool for exercise. J Pediatr Healthcare 2003;17:11-17.
18. Young-Hyman D, Schlundt DG, Herman-Wenderoth L, Bozylinski K. Obesity appearance and psychosocial adaptation on young African American children. J Pediatr Psychol 2003;28:463-472.
19. Zametkin AJ, Zoon CK, Klein HW, Munson S. Psychiatric aspects of child and adolescent obesity: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 2004;43:134-150.
20. Strauss RS. Childhood obesity and self-esteem. Pediatrics 2000;105:e15-19.
21. Pesa JA, Syre TR, Jones E. Psychosocial differences associated with body weight among female adolescents: the importance of body image. J Adolesc Health 2000;26:330-337.
22. Hesketh K, Waters E, Green J, Salmon L, Williams J. Healthy eating activity and obesity prevention: a qualitative study of parent and child perceptions in Australia. Health Promotion Intl 2005;20:19-26.
23. Nicklas TA, Yang S-J, Baranowski T, Zakeri I, Berenson G. Eating patterns and obesity in children: the Bogalusa heart study. Am J Prev Med 2003;25:9-16.
24. Nielsen BM, Bjørnsbo K, Tetens I, Heitmann BL. Dietary glycaemic index and glycaemic load in Danish children in relation to body fatness. Br J Nutr 2005;94:992-997.
25. Troiano RP, Briefel RR, Carroll MD, Bailostosky K. Energy and fat intakes of children and adolescents in the United States: data from the National Health and Nutrition Examination Surveys. Am J Clin Nutr 2000;72(Suppl):1343S-1353S.
26. Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr 2005;82:265S-273S.
27. Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr 2004;79:6-16.
28. Sallis JF, Glanz K. The role of built environments in physical activity eating and obesity in childhood. Future Child 2006;16:89-108.
29. Young LR, Nestle M. Expanding portion sizes in the US marketplace: implications for nutrition counseling. J Am Diet Assoc 2003;103:231-234.
30. Weir LA, Etelson D, Brand DA. Parents’ perceptions of neighborhood safety and children’s physical activity. Prev Med 2006;43:212-217.
31. Lumeng J. What can we do to prevent childhood obesity? Zero to Three 2005;25:13-19.
32. Burdette HL, Whitaker RC. A national study of neighborhood safety outdoor play television viewing and obesity in preschool children. Pediatrics 2005;116:657-662.
33. Andersen RE, Crespo CJ, Bartlett SJ, Cheskin LJ, Pratt M. Relationship of physical activity and television watching with body weight and level of fatness among children. JAMA 1998;279:938-942.
34. Proctor MH, Moore LL, Gao D, et al. Television viewing and change in body fat from preschool to early adolescence: the Framingham Children’s Study. Int J Obes 2003;27:827-833.
35. Salmon J, Campbell KJ, Crawford DA. Television viewing habits associated with obesity risk factors: a survey of Melbourne schoolchildren. Med J Aust 2006;184:64-67.
36. Bell SK, Morgan SB. Children’s attitudes and behavioral intentions toward a peer presented as obese: does a medical explanation for the obesity make a difference? J Pediatr Psychol 2000;25:137-145.
37. Janssen I, Craig WM, Boyce WF, Pickett W. Associations between overweight and obesity with bullying behaviors in school-aged children. Pediatrics 2004;113:1187-1194.
38. Kumanyika S, Grier S. Targeting interventions for ethnic minority and low-income populations. Future Child 2006;16:187-207.
39. Thompson JL, Davis SM, Gittelsohn J, et al. Patterns of physical activity among American Indian children: An assessment of barriers and support. J Comm Health 2001;26:407-421.
40. Mirza NM, Kadow K, Palmer M, Solano H, Rosche C, Yanovski JA. Prevalence of overweight among inner city Hispanic-American children and adolescents. Obes Res 2004;12:1298-1310.
41. Ritchie LD, Ivey SL, Woodward-Lopez G, Crawford PB. Alarming trends in pediatric overweight in the United States. Soz Praventivmed 2003;48:168-177.
42. Jefferson A. Breaking down barriers—examining health promoting behaviour in the family. Kellogg’s Family Health Study 2005. Nutr Bull 2006;31:60-64.
43. Rhee KE, DeLago CW, Arscott-Mills T, Mehta SD, Davis RK. Factors associated with parental readiness to make changes for overweight children. Pediatrics 2005;116:e94-101.
44. Dietz WH. Childhood obesity: susceptibility cause and management. J Pediatr 1983;103:676-686.
45. Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year outcomes of behavioral family-based treatment for childhood obesity. Health Psychol 1994;13:373-383.
46. Vila F, Zipper E, Dabbas M, et al. Mental disorders in obese children and adolescents. Psychosom Med 2004;66:387-394.
47. Levine MD, Ringham RM, Kalarchian MA, Wisniewski L, Marcus MD. Is family-based behavioral weight control appropriate for severe pediatric obesity? Int J Eat Disord 2001;30:318-328.
48. Wrotniak BH, Epstein LH, Paluch RA, Roemmich JN. Parent weight change as a predictor of child weight change in family-based behavioral obesity treatment. Arch Pediatr Adolesc Med 2004;158:342-347.
49. Lindsay AC, Sussner KM, Kim J, Gortmaker SL. The role of parents in preventing childhood obesity. Future Child 2006;16:169-186.
50. Carruth BR, Skinner JD. The role of dietary calcium and other nutrients in moderating body fat in preschool children. Int J Obes 2001;25:559-566.
51. Eissa MAH, Gunner KB. Evaluation and management of obesity in children and adolescents. J Pediatr Health Care 2003;18:35-38.
52. Ward-Begnoche W, Gance-Cleveland B. Promoting behavioral change in overweight youth. J Pediatr Health Care 2005;19:318-328.
53. Epstein LH, Paluch RA, Kalakanis LE, Goldfield GS, Cerny FJ, Roemmich JN. How much activity do youth get? A quantitative review of heart-rate measured activity. Pediatrics 2001;108:e44.-
54. Sothern MS, Hunter S, Suskind RM, Brown R, Udall JN, Blecker U. Motivating the obese child to move: the role of structured exercise in pediatric weight management. South Med J 1999;92:577-584.
55. Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson J-L, Garg A, et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care 2002;25:148-198.
56. Faith M, Berman N, Heo M, et al. Effects of contingent television on physical activity and television viewing in obese children. Pediatrics 2001;107:1043-1048.
57. Goldfield GS, Kalakanis LE, Ernst MM, Epstein LH. Open-loop feedback to increase physical activity on obese children. Int J Obes 2000;24:888-892.
58. Premack D. Reversibility of the reinforcement relation. Science 1962;136:255-257.
59. Nemet D, Barkan S, Epstein Y, Friedland O, Kowen G, Eliakim A. Short- and long-term beneficial effects of a combined dietary-behavioral-physical activity intervention for the treatment of childhood obesity. Pediatrics 2005;115:e443-449.
60. Neumark-Sztainer D. Preventing the broad spectrum of weight-related problems: working with parents to help teens achieve a healthy weight and a positive body image. J Nutr Educ Behav 2005;37(Suppl 2):S135-S139.
61. Flodmark C-E, Lissau I, Moreno LA, Pietrobelli A, Widhalm K. New insights into the field of children and adolescents’ obesity: the European perspective. Int J Obes 2004;28:1189-1196.
1. Epstein LH, Paluch RA, Coleman KJ, Vito D, Anderson K. Determinants of physical activity in obese children assessed by accelerometer and self-report. Med Sci Sports Exerc 1996;28:1157-1164.
2. Epstein LH, Dearing KK, Handley EA, Roemmich JN, Paluch RA. Relationship of mother and child food purchases as a function of price: a pilot study. Appetite 2006;47:115-118.
3. Cason KL. Family mealtimes: more than just eating together. J Am Diet Assoc 2006;106:532-533.
4. Baughcum AE, Chamberlin LA, Deeks CM, Powers SW, Whitaker RC. Maternal perceptions of overweight preschool children. Pediatrics 2000;106:1380-1386.
5. Golan M, Weizman A, Fainaru M. Impact of treatment for childhood obesity on parental risk factors for cardiovascular disease. Prev Med 1999;29:519-526.
6. Strauss RS, Knight J. Influence of the home environment on the development of obesity in children. Pediatrics 1999;103(6):e85-92.
7. Sallis J, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc 2000;32:963-975.
8. Treuth MS, Butte NF, Adolph AL, Puyau MR. A longitudinal study of fitness and activity in girls predisposed to obesity. Med Sci Sports Exerc 2004;36:198-204.
9. Omar MA, Coleman G, Hoerr S. Healthy eating for rural low-income toddlers: caregivers’ perceptions. J Community Health Nurs 2001;18:93-106.
10. Rhee KE, Lumeng JC, Appugliese DP, Kaciroti N, Bradley RH. Parenting styles and overweight status in first grade. Pediatrics 2006;117:2047-2054.
11. Chen JL, Kennedy C. Family functioning parenting style and Chinese children’s weight status. J Fam Nursing 2004;10:262-279.
12. Ogden J, Reynolds R, Smith A. Expanding the concept of parental control: a role for overt and covert control in children’s snacking behaviour? Appetite 2006;7(1):100-106.
13. Adams AK, Quinn RA, Prince RJ. Low recognition of childhood overweight and disease risk among Native-American caregivers. Obes Res 2005;13:146-152.
14. Jain A, Sherman SN, Chamberlin LA, Carter Y, Powers SW, Whitaker RC. Why don’t low-income mothers worry about their preschoolers being overweight? Pediatrics 2001;107:1138-1146.
15. Faulkner MS. Low income mothers of overweight children had personal and environmental challenges in preventing and managing obesity. Evidence-Based Nursing 2002;5:27.-
16. Uzark KC, Becker MH, Dielman TE, Rocchini AP. Psychosocial predictors of compliance with a weight control intervention for obese children and adolescents. J Compliance Health Care 1987;2:167-178.
17. McWhorter JW, Wallmann HW, Alpert PT. The obese child: motivation as a tool for exercise. J Pediatr Healthcare 2003;17:11-17.
18. Young-Hyman D, Schlundt DG, Herman-Wenderoth L, Bozylinski K. Obesity appearance and psychosocial adaptation on young African American children. J Pediatr Psychol 2003;28:463-472.
19. Zametkin AJ, Zoon CK, Klein HW, Munson S. Psychiatric aspects of child and adolescent obesity: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 2004;43:134-150.
20. Strauss RS. Childhood obesity and self-esteem. Pediatrics 2000;105:e15-19.
21. Pesa JA, Syre TR, Jones E. Psychosocial differences associated with body weight among female adolescents: the importance of body image. J Adolesc Health 2000;26:330-337.
22. Hesketh K, Waters E, Green J, Salmon L, Williams J. Healthy eating activity and obesity prevention: a qualitative study of parent and child perceptions in Australia. Health Promotion Intl 2005;20:19-26.
23. Nicklas TA, Yang S-J, Baranowski T, Zakeri I, Berenson G. Eating patterns and obesity in children: the Bogalusa heart study. Am J Prev Med 2003;25:9-16.
24. Nielsen BM, Bjørnsbo K, Tetens I, Heitmann BL. Dietary glycaemic index and glycaemic load in Danish children in relation to body fatness. Br J Nutr 2005;94:992-997.
25. Troiano RP, Briefel RR, Carroll MD, Bailostosky K. Energy and fat intakes of children and adolescents in the United States: data from the National Health and Nutrition Examination Surveys. Am J Clin Nutr 2000;72(Suppl):1343S-1353S.
26. Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr 2005;82:265S-273S.
27. Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr 2004;79:6-16.
28. Sallis JF, Glanz K. The role of built environments in physical activity eating and obesity in childhood. Future Child 2006;16:89-108.
29. Young LR, Nestle M. Expanding portion sizes in the US marketplace: implications for nutrition counseling. J Am Diet Assoc 2003;103:231-234.
30. Weir LA, Etelson D, Brand DA. Parents’ perceptions of neighborhood safety and children’s physical activity. Prev Med 2006;43:212-217.
31. Lumeng J. What can we do to prevent childhood obesity? Zero to Three 2005;25:13-19.
32. Burdette HL, Whitaker RC. A national study of neighborhood safety outdoor play television viewing and obesity in preschool children. Pediatrics 2005;116:657-662.
33. Andersen RE, Crespo CJ, Bartlett SJ, Cheskin LJ, Pratt M. Relationship of physical activity and television watching with body weight and level of fatness among children. JAMA 1998;279:938-942.
34. Proctor MH, Moore LL, Gao D, et al. Television viewing and change in body fat from preschool to early adolescence: the Framingham Children’s Study. Int J Obes 2003;27:827-833.
35. Salmon J, Campbell KJ, Crawford DA. Television viewing habits associated with obesity risk factors: a survey of Melbourne schoolchildren. Med J Aust 2006;184:64-67.
36. Bell SK, Morgan SB. Children’s attitudes and behavioral intentions toward a peer presented as obese: does a medical explanation for the obesity make a difference? J Pediatr Psychol 2000;25:137-145.
37. Janssen I, Craig WM, Boyce WF, Pickett W. Associations between overweight and obesity with bullying behaviors in school-aged children. Pediatrics 2004;113:1187-1194.
38. Kumanyika S, Grier S. Targeting interventions for ethnic minority and low-income populations. Future Child 2006;16:187-207.
39. Thompson JL, Davis SM, Gittelsohn J, et al. Patterns of physical activity among American Indian children: An assessment of barriers and support. J Comm Health 2001;26:407-421.
40. Mirza NM, Kadow K, Palmer M, Solano H, Rosche C, Yanovski JA. Prevalence of overweight among inner city Hispanic-American children and adolescents. Obes Res 2004;12:1298-1310.
41. Ritchie LD, Ivey SL, Woodward-Lopez G, Crawford PB. Alarming trends in pediatric overweight in the United States. Soz Praventivmed 2003;48:168-177.
42. Jefferson A. Breaking down barriers—examining health promoting behaviour in the family. Kellogg’s Family Health Study 2005. Nutr Bull 2006;31:60-64.
43. Rhee KE, DeLago CW, Arscott-Mills T, Mehta SD, Davis RK. Factors associated with parental readiness to make changes for overweight children. Pediatrics 2005;116:e94-101.
44. Dietz WH. Childhood obesity: susceptibility cause and management. J Pediatr 1983;103:676-686.
45. Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year outcomes of behavioral family-based treatment for childhood obesity. Health Psychol 1994;13:373-383.
46. Vila F, Zipper E, Dabbas M, et al. Mental disorders in obese children and adolescents. Psychosom Med 2004;66:387-394.
47. Levine MD, Ringham RM, Kalarchian MA, Wisniewski L, Marcus MD. Is family-based behavioral weight control appropriate for severe pediatric obesity? Int J Eat Disord 2001;30:318-328.
48. Wrotniak BH, Epstein LH, Paluch RA, Roemmich JN. Parent weight change as a predictor of child weight change in family-based behavioral obesity treatment. Arch Pediatr Adolesc Med 2004;158:342-347.
49. Lindsay AC, Sussner KM, Kim J, Gortmaker SL. The role of parents in preventing childhood obesity. Future Child 2006;16:169-186.
50. Carruth BR, Skinner JD. The role of dietary calcium and other nutrients in moderating body fat in preschool children. Int J Obes 2001;25:559-566.
51. Eissa MAH, Gunner KB. Evaluation and management of obesity in children and adolescents. J Pediatr Health Care 2003;18:35-38.
52. Ward-Begnoche W, Gance-Cleveland B. Promoting behavioral change in overweight youth. J Pediatr Health Care 2005;19:318-328.
53. Epstein LH, Paluch RA, Kalakanis LE, Goldfield GS, Cerny FJ, Roemmich JN. How much activity do youth get? A quantitative review of heart-rate measured activity. Pediatrics 2001;108:e44.-
54. Sothern MS, Hunter S, Suskind RM, Brown R, Udall JN, Blecker U. Motivating the obese child to move: the role of structured exercise in pediatric weight management. South Med J 1999;92:577-584.
55. Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson J-L, Garg A, et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care 2002;25:148-198.
56. Faith M, Berman N, Heo M, et al. Effects of contingent television on physical activity and television viewing in obese children. Pediatrics 2001;107:1043-1048.
57. Goldfield GS, Kalakanis LE, Ernst MM, Epstein LH. Open-loop feedback to increase physical activity on obese children. Int J Obes 2000;24:888-892.
58. Premack D. Reversibility of the reinforcement relation. Science 1962;136:255-257.
59. Nemet D, Barkan S, Epstein Y, Friedland O, Kowen G, Eliakim A. Short- and long-term beneficial effects of a combined dietary-behavioral-physical activity intervention for the treatment of childhood obesity. Pediatrics 2005;115:e443-449.
60. Neumark-Sztainer D. Preventing the broad spectrum of weight-related problems: working with parents to help teens achieve a healthy weight and a positive body image. J Nutr Educ Behav 2005;37(Suppl 2):S135-S139.
61. Flodmark C-E, Lissau I, Moreno LA, Pietrobelli A, Widhalm K. New insights into the field of children and adolescents’ obesity: the European perspective. Int J Obes 2004;28:1189-1196.