User login
ANSWER
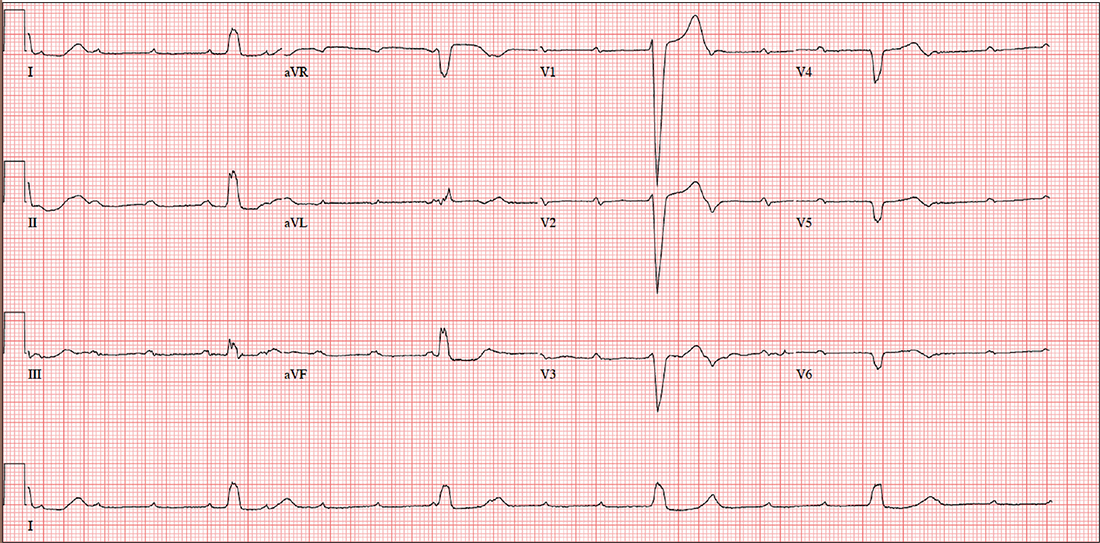
The correct interpretation includes sinus tachycardia with complete heart block and an idioventricular rhythm. Careful review of this ECG confirms complete atrioventricular dissociation, which is indicative of complete heart block.
Sinus tachycardia is indicated by a consistent P-P interval at a rate of 110 beats/min, idioventricular rhythm with a regular (but not normal) rate, and prolonged QRS interval of 148 ms. In this patient’s case, the tachycardia was presumed to be due to his upper respiratory infection. He underwent permanent pacemaker placement and resumed his normal activities without restriction.
ANSWER
The correct interpretation includes sinus tachycardia with complete heart block and an idioventricular rhythm. Careful review of this ECG confirms complete atrioventricular dissociation, which is indicative of complete heart block.
Sinus tachycardia is indicated by a consistent P-P interval at a rate of 110 beats/min, idioventricular rhythm with a regular (but not normal) rate, and prolonged QRS interval of 148 ms. In this patient’s case, the tachycardia was presumed to be due to his upper respiratory infection. He underwent permanent pacemaker placement and resumed his normal activities without restriction.
ANSWER
The correct interpretation includes sinus tachycardia with complete heart block and an idioventricular rhythm. Careful review of this ECG confirms complete atrioventricular dissociation, which is indicative of complete heart block.
Sinus tachycardia is indicated by a consistent P-P interval at a rate of 110 beats/min, idioventricular rhythm with a regular (but not normal) rate, and prolonged QRS interval of 148 ms. In this patient’s case, the tachycardia was presumed to be due to his upper respiratory infection. He underwent permanent pacemaker placement and resumed his normal activities without restriction.
Until three weeks ago, this 74-year-old man walked three miles every day without difficulty. But now, shortness of breath forces him to stop walking before he even reaches the end of his driveway. He denies chest pain (at rest or on exertion), palpitations, dyspnea at rest, and paroxysmal nocturnal dyspnea. There have been no recent weight changes.
Four years ago, he was diagnosed with coronary artery disease after experiencing chest pain at rest. A coronary angiography revealed stenosis in the proximal right coronary artery and the second obtuse marginal branch of his circumflex coronary artery; drug-eluting stents were placed, and he has had no further symptoms. An echocardiogram performed at a routine clinic visit six months ago showed mild aortic valve sclerosis, a left ventricular ejection fraction of 64%, and no regional wall motion abnormalities.
Surgical history is also remarkable for an open reduction and stabilization of a right high ankle fracture 10 years ago. Medical history includes type 2 diabetes and hyperlipidemia; treatment has normalized his A1C and his lipid panel.
His current medication list includes metoprolol, isosorbide dinitrate, metformin, and atorvastatin. He has no known drug allergies. He is unaware of any medical issues with his parents or grandparents.
The patient has two adult sons who live abroad and visit once a year. He was married for 53 years but lost his wife to lung cancer three years ago; her diagnosis prompted him to quit his long-term smoking habit. He consumes alcohol socially, having “one or two beers with friends on the weekends,” but denies current or previous use of marijuana or nonprescribed medications.
Review of systems is remarkable for a three-day history of upper respiratory infection with cough and rhinitis. He denies any change in bowel or bladder function.
Vital signs include a blood pressure of 104/54 mm Hg; pulse, 30 beats/min; respiratory rate, 16 breaths/min-1; and temperature, 99.4°F. His weight is 169 lb and his height, 70 in.
On physical exam, you note a thin, healthy-looking male in no acute distress. Pertinent findings include internally inflamed nares and oropharynx, a few scattered rales in both lower lung fields that clear with coughing, and no wheezing. There are no palpable lymph nodes in the head or neck.
Cardiac exam reveals a regular rhythm of 30 beats/min with no murmurs, rubs, or extra heart sounds. The abdomen is soft and nontender. Peripheral pulses are strong and palpable in both upper and lower extremities, and there is no peripheral edema. The neurologic exam is intact, without evidence of diabetic neuropathy.
Given the slow heart rate observed on physical exam, an ECG is ordered. It shows a ventricular rate of 29 beats/min; no discernable PR interval; QRS duration, 148 ms; QT/QTc interval, 584/405 ms; P axis, 64°; R axis, 55°; and T axis, 83°. What is your interpretation?