User login
A 60-year-old man presented to our emergency department with a 4-day history of frontal headaches he described as “stinging.” He had also had a large swollen area on his forehead for the past 8 weeks.
He denied fevers, chills, nausea, vomiting, blurry vision, tinnitus, and neck pain, as well as any recent sinus infection, intransanal cocaine use, rhinorrhea, or head trauma. A month ago, he had presented to our emergency department with forehead swelling but no headaches. At that time, the swelling was thought to be an allergic reaction to lisinopril or metformin, medications he takes for hypertension and type 2 diabetes. He had been discharged home with a prescription for a course of prednisone in tapering doses, but that had failed to resolve the swelling.
Physical examination revealed a well-circumscribed area of swelling, 3 by 4 cm, in the central forehead (Figure 1). The area was warm, erythematous, fluctuant, and tender to palpation. The nasal septum was intact and the nasal mucosa appeared pink and healthy. The remainder of the examination was unremarkable.
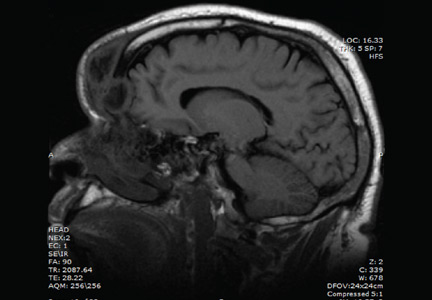
He was afebrile and hemodynamically stable. His peripheral white blood cell count was mildly elevated at 11.1 × 109. Computed tomography of the brain and sinuses revealed a fluid collection in the frontal scalp associated with erosion of the anterior frontal sinus with posterior extension and enhancement of the adjacent meninges. Magnetic resonance imaging (Figure 2) revealed similar findings. A diagnosis of Pott puffy tumor was made based on the imaging findings.
The name of this condition is misleading, as it is not a neoplasm but an infection. It requires urgent antibiotic therapy and surgical management because of the high risk of the infection spreading to the brain. Our patient was started on a broad-spectrum antibiotic regimen of intravenous vancomycin, ceftriaxone, and metronidazole pending tissue culture to identify the causative organism.
POTT PUFFY TUMOR: A BRIEF OVERVIEW
First described in 1760 by Sir Percivall Pott,1 the same English surgeon who first described tuberculosis of the spine, Pott puffy tumor is a well-demarcated area of swelling that occurs when a frontal sinus infection breaks through the anterior portion of the frontal sinus and forms an abscess between the frontal bone and periosteum with associated osteomyelitis.2 Though rare in adults (it is more common in children and adolescents),3 Pott puffy tumor is caused by conditions often encountered in internal medicine practice, such as bacterial sinusitis, head trauma, and intranasal cocaine use.
The infection can spread to the brain either directly by destruction of the posterior frontal sinus (as in our patient) or by way of the veins that drain the frontal sinus. Meningitis, epidural empyema, frontal lobe abscess, and cavernous sinus thrombosis2 have all been described. Intracranial complications are seen in nearly 100% of children and adolescents with Pott puffy tumor. The rate in adults is 30%,4,5 which is much lower but is nevertheless worrisome because patients can be initially misdiagnosed with scalp abscess,3 cellulitis, or epidermoid cyst,4 and then sent home from the emergency department or physician’s office. In a case series of 32 adult patients with Pott puffy tumor, nearly 45% were initially misdiagnosed, most often by an internist, dermatologist, ophthalmologist, or emergency room physician.4
The most common infective organisms are streptococci, staphylococci, and anaerobes,4 but Haemophilus, Aspergillus species, and invasive mucormycosis have also been described.
MANAGEMENT OPTIONS
Because of the risk of spread of the infection to the brain, rapid initiation of a broad-spectrum antibiotic is warranted in all patients with Pott puffy tumor pending results of tissue culture. Antibiotics may be necessary for at least 4 to 6 weeks to resolve osteomyelitis of the frontal bone and to decrease inflammation before surgery.6
Endoscopic sinus surgery is routinely done to drain the infected sinus and to remove or debride infected bone. Patients with intracranial extension of infection may require a combined endoscopic and neurosurgical approach.
OUTCOME
Our patient’s puffy tumor spontaneously ruptured externally on hospital day 3, and the purulent fluid was sent for culture that grew Streptococcus anginosus. His headaches improved almost immediately after this occurred. The antibiotic regimen was narrowed to ceftriaxone and metronidazole, and 1 week later he was discharged home with instructions to complete a 6-week course of antibiotics. Three weeks after he was discharged, he returned for outpatient endoscopic sinus surgery. At a follow-up visit 2 weeks after surgery, the forehead swelling had resolved, and he was well.
- Tattersall R, Tattersall R. Pott’s puffy tumor. Lancet 2002; 359:1060–1063.
- Forgie SE, Marrie TJ. Pott’s puffy tumor. Am J Med 2008; 121:1041–1042.
- Grewal HS, Dangaych NS, Esposito A. A tumor that is not a tumor but it sure can kill! Am J Case Rep 2012; 13:133–136.
- Akiyama K, Karaki M, Mori N. Evaluation of adult Pott’s puffy tumor: our five cases and 27 literature cases. Laryngoscope 2012; 122:2382–2388.
- Suwan PT, Mogal S, Chaudhary S. Pott’s puffy tumor: an uncommon clinical entity. Case Rep Pediatr 2012; 2012:386104.
- Lauria RA, Laffitte Fernandes F, Brito TP, Pereira PS, Chone CT. Extensive frontoparietal abscess: complication of frontal sinusitis (Pott’s puffy tumor). Case Rep Otolaryngol 2014; 2014:632464.
A 60-year-old man presented to our emergency department with a 4-day history of frontal headaches he described as “stinging.” He had also had a large swollen area on his forehead for the past 8 weeks.
He denied fevers, chills, nausea, vomiting, blurry vision, tinnitus, and neck pain, as well as any recent sinus infection, intransanal cocaine use, rhinorrhea, or head trauma. A month ago, he had presented to our emergency department with forehead swelling but no headaches. At that time, the swelling was thought to be an allergic reaction to lisinopril or metformin, medications he takes for hypertension and type 2 diabetes. He had been discharged home with a prescription for a course of prednisone in tapering doses, but that had failed to resolve the swelling.
Physical examination revealed a well-circumscribed area of swelling, 3 by 4 cm, in the central forehead (Figure 1). The area was warm, erythematous, fluctuant, and tender to palpation. The nasal septum was intact and the nasal mucosa appeared pink and healthy. The remainder of the examination was unremarkable.
He was afebrile and hemodynamically stable. His peripheral white blood cell count was mildly elevated at 11.1 × 109. Computed tomography of the brain and sinuses revealed a fluid collection in the frontal scalp associated with erosion of the anterior frontal sinus with posterior extension and enhancement of the adjacent meninges. Magnetic resonance imaging (Figure 2) revealed similar findings. A diagnosis of Pott puffy tumor was made based on the imaging findings.
The name of this condition is misleading, as it is not a neoplasm but an infection. It requires urgent antibiotic therapy and surgical management because of the high risk of the infection spreading to the brain. Our patient was started on a broad-spectrum antibiotic regimen of intravenous vancomycin, ceftriaxone, and metronidazole pending tissue culture to identify the causative organism.
POTT PUFFY TUMOR: A BRIEF OVERVIEW
First described in 1760 by Sir Percivall Pott,1 the same English surgeon who first described tuberculosis of the spine, Pott puffy tumor is a well-demarcated area of swelling that occurs when a frontal sinus infection breaks through the anterior portion of the frontal sinus and forms an abscess between the frontal bone and periosteum with associated osteomyelitis.2 Though rare in adults (it is more common in children and adolescents),3 Pott puffy tumor is caused by conditions often encountered in internal medicine practice, such as bacterial sinusitis, head trauma, and intranasal cocaine use.
The infection can spread to the brain either directly by destruction of the posterior frontal sinus (as in our patient) or by way of the veins that drain the frontal sinus. Meningitis, epidural empyema, frontal lobe abscess, and cavernous sinus thrombosis2 have all been described. Intracranial complications are seen in nearly 100% of children and adolescents with Pott puffy tumor. The rate in adults is 30%,4,5 which is much lower but is nevertheless worrisome because patients can be initially misdiagnosed with scalp abscess,3 cellulitis, or epidermoid cyst,4 and then sent home from the emergency department or physician’s office. In a case series of 32 adult patients with Pott puffy tumor, nearly 45% were initially misdiagnosed, most often by an internist, dermatologist, ophthalmologist, or emergency room physician.4
The most common infective organisms are streptococci, staphylococci, and anaerobes,4 but Haemophilus, Aspergillus species, and invasive mucormycosis have also been described.
MANAGEMENT OPTIONS
Because of the risk of spread of the infection to the brain, rapid initiation of a broad-spectrum antibiotic is warranted in all patients with Pott puffy tumor pending results of tissue culture. Antibiotics may be necessary for at least 4 to 6 weeks to resolve osteomyelitis of the frontal bone and to decrease inflammation before surgery.6
Endoscopic sinus surgery is routinely done to drain the infected sinus and to remove or debride infected bone. Patients with intracranial extension of infection may require a combined endoscopic and neurosurgical approach.
OUTCOME
Our patient’s puffy tumor spontaneously ruptured externally on hospital day 3, and the purulent fluid was sent for culture that grew Streptococcus anginosus. His headaches improved almost immediately after this occurred. The antibiotic regimen was narrowed to ceftriaxone and metronidazole, and 1 week later he was discharged home with instructions to complete a 6-week course of antibiotics. Three weeks after he was discharged, he returned for outpatient endoscopic sinus surgery. At a follow-up visit 2 weeks after surgery, the forehead swelling had resolved, and he was well.
A 60-year-old man presented to our emergency department with a 4-day history of frontal headaches he described as “stinging.” He had also had a large swollen area on his forehead for the past 8 weeks.
He denied fevers, chills, nausea, vomiting, blurry vision, tinnitus, and neck pain, as well as any recent sinus infection, intransanal cocaine use, rhinorrhea, or head trauma. A month ago, he had presented to our emergency department with forehead swelling but no headaches. At that time, the swelling was thought to be an allergic reaction to lisinopril or metformin, medications he takes for hypertension and type 2 diabetes. He had been discharged home with a prescription for a course of prednisone in tapering doses, but that had failed to resolve the swelling.
Physical examination revealed a well-circumscribed area of swelling, 3 by 4 cm, in the central forehead (Figure 1). The area was warm, erythematous, fluctuant, and tender to palpation. The nasal septum was intact and the nasal mucosa appeared pink and healthy. The remainder of the examination was unremarkable.
He was afebrile and hemodynamically stable. His peripheral white blood cell count was mildly elevated at 11.1 × 109. Computed tomography of the brain and sinuses revealed a fluid collection in the frontal scalp associated with erosion of the anterior frontal sinus with posterior extension and enhancement of the adjacent meninges. Magnetic resonance imaging (Figure 2) revealed similar findings. A diagnosis of Pott puffy tumor was made based on the imaging findings.
The name of this condition is misleading, as it is not a neoplasm but an infection. It requires urgent antibiotic therapy and surgical management because of the high risk of the infection spreading to the brain. Our patient was started on a broad-spectrum antibiotic regimen of intravenous vancomycin, ceftriaxone, and metronidazole pending tissue culture to identify the causative organism.
POTT PUFFY TUMOR: A BRIEF OVERVIEW
First described in 1760 by Sir Percivall Pott,1 the same English surgeon who first described tuberculosis of the spine, Pott puffy tumor is a well-demarcated area of swelling that occurs when a frontal sinus infection breaks through the anterior portion of the frontal sinus and forms an abscess between the frontal bone and periosteum with associated osteomyelitis.2 Though rare in adults (it is more common in children and adolescents),3 Pott puffy tumor is caused by conditions often encountered in internal medicine practice, such as bacterial sinusitis, head trauma, and intranasal cocaine use.
The infection can spread to the brain either directly by destruction of the posterior frontal sinus (as in our patient) or by way of the veins that drain the frontal sinus. Meningitis, epidural empyema, frontal lobe abscess, and cavernous sinus thrombosis2 have all been described. Intracranial complications are seen in nearly 100% of children and adolescents with Pott puffy tumor. The rate in adults is 30%,4,5 which is much lower but is nevertheless worrisome because patients can be initially misdiagnosed with scalp abscess,3 cellulitis, or epidermoid cyst,4 and then sent home from the emergency department or physician’s office. In a case series of 32 adult patients with Pott puffy tumor, nearly 45% were initially misdiagnosed, most often by an internist, dermatologist, ophthalmologist, or emergency room physician.4
The most common infective organisms are streptococci, staphylococci, and anaerobes,4 but Haemophilus, Aspergillus species, and invasive mucormycosis have also been described.
MANAGEMENT OPTIONS
Because of the risk of spread of the infection to the brain, rapid initiation of a broad-spectrum antibiotic is warranted in all patients with Pott puffy tumor pending results of tissue culture. Antibiotics may be necessary for at least 4 to 6 weeks to resolve osteomyelitis of the frontal bone and to decrease inflammation before surgery.6
Endoscopic sinus surgery is routinely done to drain the infected sinus and to remove or debride infected bone. Patients with intracranial extension of infection may require a combined endoscopic and neurosurgical approach.
OUTCOME
Our patient’s puffy tumor spontaneously ruptured externally on hospital day 3, and the purulent fluid was sent for culture that grew Streptococcus anginosus. His headaches improved almost immediately after this occurred. The antibiotic regimen was narrowed to ceftriaxone and metronidazole, and 1 week later he was discharged home with instructions to complete a 6-week course of antibiotics. Three weeks after he was discharged, he returned for outpatient endoscopic sinus surgery. At a follow-up visit 2 weeks after surgery, the forehead swelling had resolved, and he was well.
- Tattersall R, Tattersall R. Pott’s puffy tumor. Lancet 2002; 359:1060–1063.
- Forgie SE, Marrie TJ. Pott’s puffy tumor. Am J Med 2008; 121:1041–1042.
- Grewal HS, Dangaych NS, Esposito A. A tumor that is not a tumor but it sure can kill! Am J Case Rep 2012; 13:133–136.
- Akiyama K, Karaki M, Mori N. Evaluation of adult Pott’s puffy tumor: our five cases and 27 literature cases. Laryngoscope 2012; 122:2382–2388.
- Suwan PT, Mogal S, Chaudhary S. Pott’s puffy tumor: an uncommon clinical entity. Case Rep Pediatr 2012; 2012:386104.
- Lauria RA, Laffitte Fernandes F, Brito TP, Pereira PS, Chone CT. Extensive frontoparietal abscess: complication of frontal sinusitis (Pott’s puffy tumor). Case Rep Otolaryngol 2014; 2014:632464.
- Tattersall R, Tattersall R. Pott’s puffy tumor. Lancet 2002; 359:1060–1063.
- Forgie SE, Marrie TJ. Pott’s puffy tumor. Am J Med 2008; 121:1041–1042.
- Grewal HS, Dangaych NS, Esposito A. A tumor that is not a tumor but it sure can kill! Am J Case Rep 2012; 13:133–136.
- Akiyama K, Karaki M, Mori N. Evaluation of adult Pott’s puffy tumor: our five cases and 27 literature cases. Laryngoscope 2012; 122:2382–2388.
- Suwan PT, Mogal S, Chaudhary S. Pott’s puffy tumor: an uncommon clinical entity. Case Rep Pediatr 2012; 2012:386104.
- Lauria RA, Laffitte Fernandes F, Brito TP, Pereira PS, Chone CT. Extensive frontoparietal abscess: complication of frontal sinusitis (Pott’s puffy tumor). Case Rep Otolaryngol 2014; 2014:632464.