User login
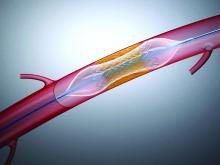
Clinicians should approach decisions regarding coronary revascularization based on clinical indications without an eye toward sex, race, or ethnicity, advises a joint clinical practice guideline released Dec. 8 by the American Heart Association and American College of Cardiology.
The new class 1 recommendation leads off the 109-page document and reflects evidence demonstrating that revascularization is equally beneficial for all patients. Still, studies show that women and non-White patients are less likely to receive reperfusion therapy or revascularization.
“This was extremely important to all the committee members because of all of the disparities that have been documented not only in diagnosis but [in] the care provided to underrepresented minorities, women, and other ethnic groups,” said Jennifer S. Lawton, MD, chief of cardiac surgery at Johns Hopkins University, Baltimore, and guideline writing committee chair.
“We wanted to make it clear right at the beginning of the document that these guidelines apply to everyone, and we want it to be known that care should be the same for everyone,” she said in an interview.
The guideline was simultaneously published Dec. 9, 2021, in the journal Circulation and the Journal of the American College of Cardiology.
It updates and consolidates the ACC/AHA 2011 coronary artery bypass surgery (CABG) guideline and the ACC/AHA/Society for Cardiovascular Angiography and Interventions 2011 and 2015 percutaneous coronary intervention (PCI) guidelines.
The new document emphasizes in a class 1 recommendation the importance of the multidisciplinary heart team in patients with coronary artery disease (CAD) where the best treatment strategy is unclear. But it also stresses that treatment decisions should be patient centered – taking into account patient preferences and goals, cultural beliefs, health literacy, and social determinants of cardiovascular health – and made in collaboration with the patient’s support system.
“Oftentimes we recommend a strategy of revascularization that may not be what the patient wants or hasn’t taken into account the patient’s preferences and also the family members,” Dr. Lawson said. “So we felt that was very important.”
Patients should also be provided with available evidence for various treatment options, including risks and benefits of each option, for informed consent. The two new class 1 recommendations are highlighted in a figure illustrating the shared decision-making algorithm that, by design, features a female clinician and Black patient.
“We spent 2 years debating the best revascularization strategies and we’re considered experts in the field – but when we talk to our patients, they really don’t know the benefits and risks,” she said. “In order to translate it to the layperson in basic terms, it’s important to say, ‘If you choose this option, you will likely live longer’ rather than using the jargon.”
DAPT, staged PCI, stable IHD
Among the top 10 take-home messages highlighted by the authors is a 2a recommendation that 1-3 months of dual antiplatelet therapy (DAPT) after PCI with a transition to P2Y12 inhibitor monotherapy is “reasonable” in selected patients to reduce the risk of bleeding events. Previous recommendations called for 6 or 12 months of DAPT.
“We really respect all of the clinical trials that came out showing that a shorter duration of DAPT is not inferior in terms of ischemic events but less bleeding, yet I don’t know how many clinicians are actually just using 3 months of DAPT followed by P2Y12 monotherapy,” guideline committee vice chair Jacqueline Tamis-Holland, MD, professor of medicine, Icahn School of Medicine at Mount Sinai, New York, said in an interview. “So while it’s not a big, glaring giant recommendation, I think it will change a lot of practice.”
Similarly, she suggested that practice may shift as a result of a class 1 recommendation for staged PCI of a significantly stenosed nonculprit artery to reduce the risk for death or MI in selected hemodynamically stable patients presenting with ST-segment elevation MI and multivessel disease. “When you survey physicians, 75% of them do staged PCI but I think there will probably be more of an approach to staged PCI, as opposed to doing multivessel PCI at the time of primary PCI.”
Newer evidence from meta-analyses and the landmark ISCHEMIA trial showing no advantage of CABG over medical therapy in stable ischemic heart disease is reflected in a new class 2b recommendation – downgraded from class 1 in 2011 – that CABG “may be reasonable” to improve survival in stable patients with triple-vessel CAD.
The writing committee concluded that the ability of PCI to improve survival, compared with medical therapy in multivessel CAD “remains uncertain.”
Other recommendations likely to be of interest are that the radial artery is preferred, after the left internal mammary artery, as a surgical revascularization conduit over use of a saphenous vein conduit. Benefits include superior patency, fewer adverse cardiac events, and improved survival, the committee noted.
The radial artery is also recommended (class 1) in patients undergoing PCI who have acute coronary syndromes or stable ischemic heart disease to reduce bleeding and vascular complications compared with a femoral approach.
“Having both new radial recommendations sort of makes a bit of tension because the interventionalist is going to want to use the radial artery, but also the surgeon is too,” observed Dr. Tamis-Holland. “We see that in our own practice, so we try to have a collaborative approach to the patient to say: ‘Maybe do the cardiac cath in the dominant radial and then we can use the nondominant radial for a bypass conduit,’ but using both for each revascularization strategy will benefit the patient.
“So, we just have to remember that we’re going to talk together as a heart team and try to make the best decisions for each patient.”
A version of this article first appeared on Medscape.com.
Clinicians should approach decisions regarding coronary revascularization based on clinical indications without an eye toward sex, race, or ethnicity, advises a joint clinical practice guideline released Dec. 8 by the American Heart Association and American College of Cardiology.
The new class 1 recommendation leads off the 109-page document and reflects evidence demonstrating that revascularization is equally beneficial for all patients. Still, studies show that women and non-White patients are less likely to receive reperfusion therapy or revascularization.
“This was extremely important to all the committee members because of all of the disparities that have been documented not only in diagnosis but [in] the care provided to underrepresented minorities, women, and other ethnic groups,” said Jennifer S. Lawton, MD, chief of cardiac surgery at Johns Hopkins University, Baltimore, and guideline writing committee chair.
“We wanted to make it clear right at the beginning of the document that these guidelines apply to everyone, and we want it to be known that care should be the same for everyone,” she said in an interview.
The guideline was simultaneously published Dec. 9, 2021, in the journal Circulation and the Journal of the American College of Cardiology.
It updates and consolidates the ACC/AHA 2011 coronary artery bypass surgery (CABG) guideline and the ACC/AHA/Society for Cardiovascular Angiography and Interventions 2011 and 2015 percutaneous coronary intervention (PCI) guidelines.
The new document emphasizes in a class 1 recommendation the importance of the multidisciplinary heart team in patients with coronary artery disease (CAD) where the best treatment strategy is unclear. But it also stresses that treatment decisions should be patient centered – taking into account patient preferences and goals, cultural beliefs, health literacy, and social determinants of cardiovascular health – and made in collaboration with the patient’s support system.
“Oftentimes we recommend a strategy of revascularization that may not be what the patient wants or hasn’t taken into account the patient’s preferences and also the family members,” Dr. Lawson said. “So we felt that was very important.”
Patients should also be provided with available evidence for various treatment options, including risks and benefits of each option, for informed consent. The two new class 1 recommendations are highlighted in a figure illustrating the shared decision-making algorithm that, by design, features a female clinician and Black patient.
“We spent 2 years debating the best revascularization strategies and we’re considered experts in the field – but when we talk to our patients, they really don’t know the benefits and risks,” she said. “In order to translate it to the layperson in basic terms, it’s important to say, ‘If you choose this option, you will likely live longer’ rather than using the jargon.”
DAPT, staged PCI, stable IHD
Among the top 10 take-home messages highlighted by the authors is a 2a recommendation that 1-3 months of dual antiplatelet therapy (DAPT) after PCI with a transition to P2Y12 inhibitor monotherapy is “reasonable” in selected patients to reduce the risk of bleeding events. Previous recommendations called for 6 or 12 months of DAPT.
“We really respect all of the clinical trials that came out showing that a shorter duration of DAPT is not inferior in terms of ischemic events but less bleeding, yet I don’t know how many clinicians are actually just using 3 months of DAPT followed by P2Y12 monotherapy,” guideline committee vice chair Jacqueline Tamis-Holland, MD, professor of medicine, Icahn School of Medicine at Mount Sinai, New York, said in an interview. “So while it’s not a big, glaring giant recommendation, I think it will change a lot of practice.”
Similarly, she suggested that practice may shift as a result of a class 1 recommendation for staged PCI of a significantly stenosed nonculprit artery to reduce the risk for death or MI in selected hemodynamically stable patients presenting with ST-segment elevation MI and multivessel disease. “When you survey physicians, 75% of them do staged PCI but I think there will probably be more of an approach to staged PCI, as opposed to doing multivessel PCI at the time of primary PCI.”
Newer evidence from meta-analyses and the landmark ISCHEMIA trial showing no advantage of CABG over medical therapy in stable ischemic heart disease is reflected in a new class 2b recommendation – downgraded from class 1 in 2011 – that CABG “may be reasonable” to improve survival in stable patients with triple-vessel CAD.
The writing committee concluded that the ability of PCI to improve survival, compared with medical therapy in multivessel CAD “remains uncertain.”
Other recommendations likely to be of interest are that the radial artery is preferred, after the left internal mammary artery, as a surgical revascularization conduit over use of a saphenous vein conduit. Benefits include superior patency, fewer adverse cardiac events, and improved survival, the committee noted.
The radial artery is also recommended (class 1) in patients undergoing PCI who have acute coronary syndromes or stable ischemic heart disease to reduce bleeding and vascular complications compared with a femoral approach.
“Having both new radial recommendations sort of makes a bit of tension because the interventionalist is going to want to use the radial artery, but also the surgeon is too,” observed Dr. Tamis-Holland. “We see that in our own practice, so we try to have a collaborative approach to the patient to say: ‘Maybe do the cardiac cath in the dominant radial and then we can use the nondominant radial for a bypass conduit,’ but using both for each revascularization strategy will benefit the patient.
“So, we just have to remember that we’re going to talk together as a heart team and try to make the best decisions for each patient.”
A version of this article first appeared on Medscape.com.
Clinicians should approach decisions regarding coronary revascularization based on clinical indications without an eye toward sex, race, or ethnicity, advises a joint clinical practice guideline released Dec. 8 by the American Heart Association and American College of Cardiology.
The new class 1 recommendation leads off the 109-page document and reflects evidence demonstrating that revascularization is equally beneficial for all patients. Still, studies show that women and non-White patients are less likely to receive reperfusion therapy or revascularization.
“This was extremely important to all the committee members because of all of the disparities that have been documented not only in diagnosis but [in] the care provided to underrepresented minorities, women, and other ethnic groups,” said Jennifer S. Lawton, MD, chief of cardiac surgery at Johns Hopkins University, Baltimore, and guideline writing committee chair.
“We wanted to make it clear right at the beginning of the document that these guidelines apply to everyone, and we want it to be known that care should be the same for everyone,” she said in an interview.
The guideline was simultaneously published Dec. 9, 2021, in the journal Circulation and the Journal of the American College of Cardiology.
It updates and consolidates the ACC/AHA 2011 coronary artery bypass surgery (CABG) guideline and the ACC/AHA/Society for Cardiovascular Angiography and Interventions 2011 and 2015 percutaneous coronary intervention (PCI) guidelines.
The new document emphasizes in a class 1 recommendation the importance of the multidisciplinary heart team in patients with coronary artery disease (CAD) where the best treatment strategy is unclear. But it also stresses that treatment decisions should be patient centered – taking into account patient preferences and goals, cultural beliefs, health literacy, and social determinants of cardiovascular health – and made in collaboration with the patient’s support system.
“Oftentimes we recommend a strategy of revascularization that may not be what the patient wants or hasn’t taken into account the patient’s preferences and also the family members,” Dr. Lawson said. “So we felt that was very important.”
Patients should also be provided with available evidence for various treatment options, including risks and benefits of each option, for informed consent. The two new class 1 recommendations are highlighted in a figure illustrating the shared decision-making algorithm that, by design, features a female clinician and Black patient.
“We spent 2 years debating the best revascularization strategies and we’re considered experts in the field – but when we talk to our patients, they really don’t know the benefits and risks,” she said. “In order to translate it to the layperson in basic terms, it’s important to say, ‘If you choose this option, you will likely live longer’ rather than using the jargon.”
DAPT, staged PCI, stable IHD
Among the top 10 take-home messages highlighted by the authors is a 2a recommendation that 1-3 months of dual antiplatelet therapy (DAPT) after PCI with a transition to P2Y12 inhibitor monotherapy is “reasonable” in selected patients to reduce the risk of bleeding events. Previous recommendations called for 6 or 12 months of DAPT.
“We really respect all of the clinical trials that came out showing that a shorter duration of DAPT is not inferior in terms of ischemic events but less bleeding, yet I don’t know how many clinicians are actually just using 3 months of DAPT followed by P2Y12 monotherapy,” guideline committee vice chair Jacqueline Tamis-Holland, MD, professor of medicine, Icahn School of Medicine at Mount Sinai, New York, said in an interview. “So while it’s not a big, glaring giant recommendation, I think it will change a lot of practice.”
Similarly, she suggested that practice may shift as a result of a class 1 recommendation for staged PCI of a significantly stenosed nonculprit artery to reduce the risk for death or MI in selected hemodynamically stable patients presenting with ST-segment elevation MI and multivessel disease. “When you survey physicians, 75% of them do staged PCI but I think there will probably be more of an approach to staged PCI, as opposed to doing multivessel PCI at the time of primary PCI.”
Newer evidence from meta-analyses and the landmark ISCHEMIA trial showing no advantage of CABG over medical therapy in stable ischemic heart disease is reflected in a new class 2b recommendation – downgraded from class 1 in 2011 – that CABG “may be reasonable” to improve survival in stable patients with triple-vessel CAD.
The writing committee concluded that the ability of PCI to improve survival, compared with medical therapy in multivessel CAD “remains uncertain.”
Other recommendations likely to be of interest are that the radial artery is preferred, after the left internal mammary artery, as a surgical revascularization conduit over use of a saphenous vein conduit. Benefits include superior patency, fewer adverse cardiac events, and improved survival, the committee noted.
The radial artery is also recommended (class 1) in patients undergoing PCI who have acute coronary syndromes or stable ischemic heart disease to reduce bleeding and vascular complications compared with a femoral approach.
“Having both new radial recommendations sort of makes a bit of tension because the interventionalist is going to want to use the radial artery, but also the surgeon is too,” observed Dr. Tamis-Holland. “We see that in our own practice, so we try to have a collaborative approach to the patient to say: ‘Maybe do the cardiac cath in the dominant radial and then we can use the nondominant radial for a bypass conduit,’ but using both for each revascularization strategy will benefit the patient.
“So, we just have to remember that we’re going to talk together as a heart team and try to make the best decisions for each patient.”
A version of this article first appeared on Medscape.com.