User login
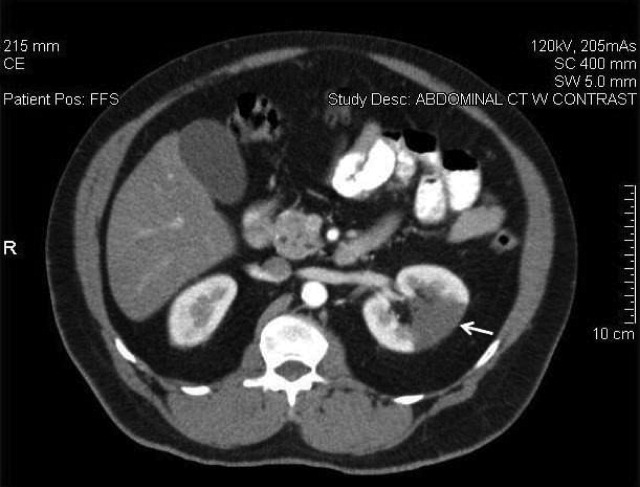
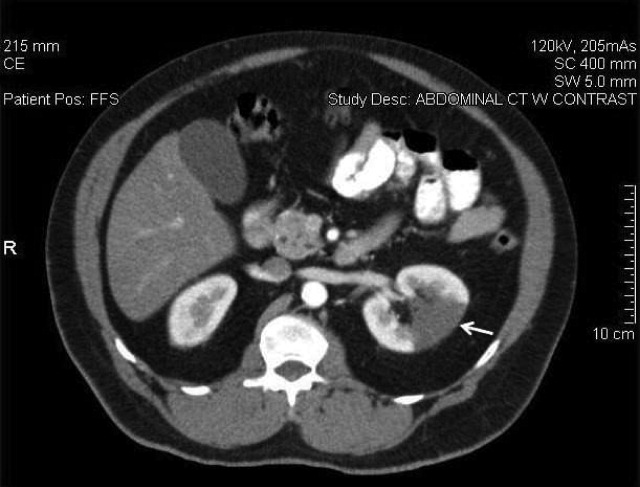
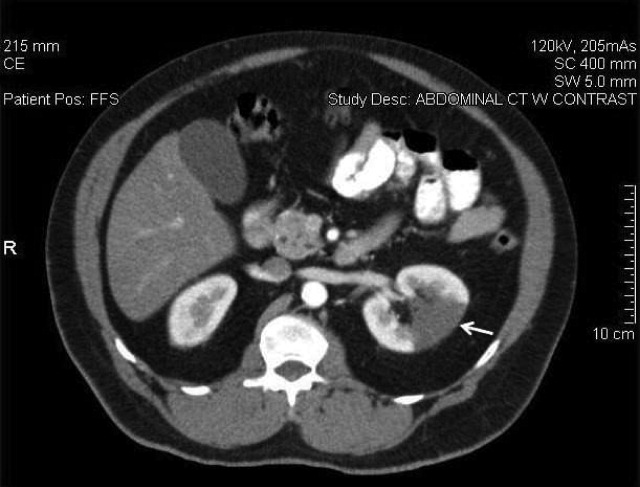
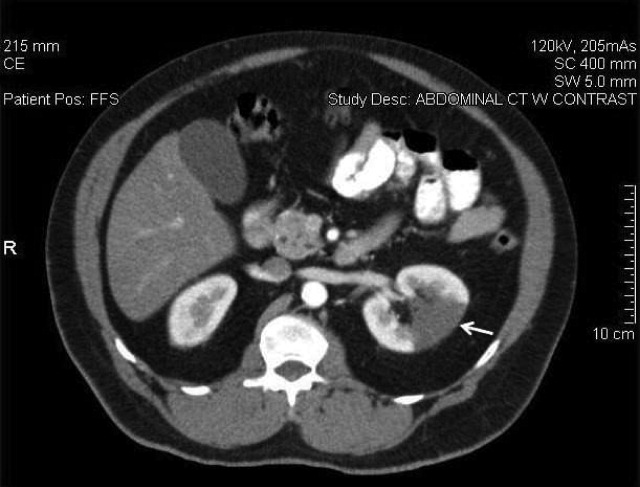
A 58‐year‐old man presented with a 1‐day history of left lower quadrant abdominal pain. He had a history of remote tobacco use, hypertension, hypercholesterolemia, deep venous thrombosis, and pulmonary embolism. His white cell count was 18,500/mm,3 and urinalysis revealed hematuria. Contrast‐enhanced abdominal computed tomography (CT) scan showed decreased perfusion of a large section of the lower pole of the left kidney (Figure 1). On day 3, his flank pain persisted, despite hydration, analgesics, and intravenous (IV) antibiotics. His serum lactate dehydrogenase (LDH) was elevated and renal infarction was suspected. Heparin was started and the patient was later discharged on warfarin. One month later, repeat contrast‐enhanced abdominal CT showed a less extensive wedge defect with scarring of the left kidney.
The diagnosis of acute renal infarction is often missed due to its nonspecific symptoms and the fact that it is an uncommon disease. It should be suspected in patients with acute flank pain and risk factors for thromboembolism including: valvular or ischemic heart disease, atrial fibrillation, and previous thromboembolic events.1, 2 Hypertension, which our patient had, is also a risk factor. In the appropriate setting hematuria and elevated LDH strongly suggest the diagnosis.3 Angiography remains the gold‐standard for diagnosis, but contrast‐enhanced CT is an acceptable alternative.3 In the setting of gross hematuria, we recommend that acute renal infarction should be suspected in all patients with the triad of persistent flank pain, high thromboembolic risk, and an increased LDH.
- ,,, et al.ED presentations of acute renal infarction.Am J Emerg Med.2007;25:164–169.
- ,,,.Renal artery embolism: clinical features and long‐term follow‐up of 17 cases.Ann Intern Med.1978;89:477–482.
- ,,, et al.Acute renal infarction. Clinical characteristics of 17 patients.Medicine (Baltimore).1999;78:386–394.
A 58‐year‐old man presented with a 1‐day history of left lower quadrant abdominal pain. He had a history of remote tobacco use, hypertension, hypercholesterolemia, deep venous thrombosis, and pulmonary embolism. His white cell count was 18,500/mm,3 and urinalysis revealed hematuria. Contrast‐enhanced abdominal computed tomography (CT) scan showed decreased perfusion of a large section of the lower pole of the left kidney (Figure 1). On day 3, his flank pain persisted, despite hydration, analgesics, and intravenous (IV) antibiotics. His serum lactate dehydrogenase (LDH) was elevated and renal infarction was suspected. Heparin was started and the patient was later discharged on warfarin. One month later, repeat contrast‐enhanced abdominal CT showed a less extensive wedge defect with scarring of the left kidney.
The diagnosis of acute renal infarction is often missed due to its nonspecific symptoms and the fact that it is an uncommon disease. It should be suspected in patients with acute flank pain and risk factors for thromboembolism including: valvular or ischemic heart disease, atrial fibrillation, and previous thromboembolic events.1, 2 Hypertension, which our patient had, is also a risk factor. In the appropriate setting hematuria and elevated LDH strongly suggest the diagnosis.3 Angiography remains the gold‐standard for diagnosis, but contrast‐enhanced CT is an acceptable alternative.3 In the setting of gross hematuria, we recommend that acute renal infarction should be suspected in all patients with the triad of persistent flank pain, high thromboembolic risk, and an increased LDH.
A 58‐year‐old man presented with a 1‐day history of left lower quadrant abdominal pain. He had a history of remote tobacco use, hypertension, hypercholesterolemia, deep venous thrombosis, and pulmonary embolism. His white cell count was 18,500/mm,3 and urinalysis revealed hematuria. Contrast‐enhanced abdominal computed tomography (CT) scan showed decreased perfusion of a large section of the lower pole of the left kidney (Figure 1). On day 3, his flank pain persisted, despite hydration, analgesics, and intravenous (IV) antibiotics. His serum lactate dehydrogenase (LDH) was elevated and renal infarction was suspected. Heparin was started and the patient was later discharged on warfarin. One month later, repeat contrast‐enhanced abdominal CT showed a less extensive wedge defect with scarring of the left kidney.
The diagnosis of acute renal infarction is often missed due to its nonspecific symptoms and the fact that it is an uncommon disease. It should be suspected in patients with acute flank pain and risk factors for thromboembolism including: valvular or ischemic heart disease, atrial fibrillation, and previous thromboembolic events.1, 2 Hypertension, which our patient had, is also a risk factor. In the appropriate setting hematuria and elevated LDH strongly suggest the diagnosis.3 Angiography remains the gold‐standard for diagnosis, but contrast‐enhanced CT is an acceptable alternative.3 In the setting of gross hematuria, we recommend that acute renal infarction should be suspected in all patients with the triad of persistent flank pain, high thromboembolic risk, and an increased LDH.
- ,,, et al.ED presentations of acute renal infarction.Am J Emerg Med.2007;25:164–169.
- ,,,.Renal artery embolism: clinical features and long‐term follow‐up of 17 cases.Ann Intern Med.1978;89:477–482.
- ,,, et al.Acute renal infarction. Clinical characteristics of 17 patients.Medicine (Baltimore).1999;78:386–394.
- ,,, et al.ED presentations of acute renal infarction.Am J Emerg Med.2007;25:164–169.
- ,,,.Renal artery embolism: clinical features and long‐term follow‐up of 17 cases.Ann Intern Med.1978;89:477–482.
- ,,, et al.Acute renal infarction. Clinical characteristics of 17 patients.Medicine (Baltimore).1999;78:386–394.