User login
CHICAGO – Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggested.
Admission of patients with adhesive small-bowel obstruction (SBO) to medical teams is associated with higher health care costs and worse outcomes; thus, policies favoring primary admission to surgical services could substantially reduce costs and improve outcomes, Dr. Fergal J. Fleming of the University of Rochester (N.Y.) Medical Center reported at the annual meeting of the American Surgical Association.
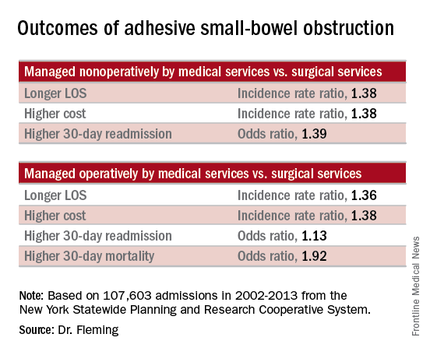
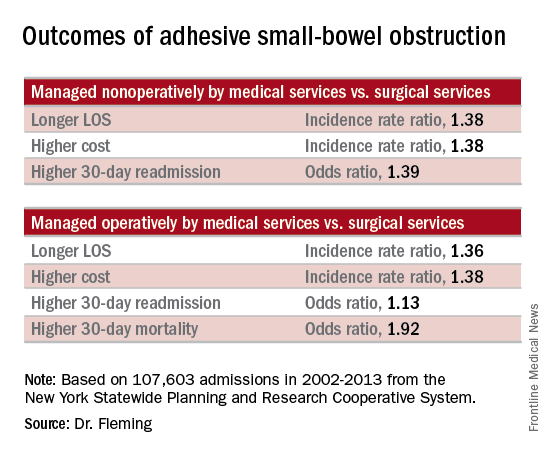
Of 107,603 admissions among patients in the data set, including 78% who were nonoperative and 22% who were operative, 43% were admitted to medical services, and 57% were admitted to surgical services. After several variables, including patient, physician, and hospital-level factors, were controlled for, patients managed nonoperatively primarily by medical services (vs. surgical services) had a longer length of stay (incidence rate ratio, 1.38), higher total cost (incidence rate ratio, 1.38), and higher 30-day readmission rate (odds ratio, 1.39). In addition, those managed operatively primarily by medical services (vs. surgical services) had a greater delay in time to surgical intervention (incidence rate ratio, 1.84), a longer length of stay (incidence rate ratio, 1.36), greater inpatient costs (incidence rate ratio, 1.38), and higher 30-day mortality and 30-day readmission rates (odds ratios, 1.92 and 1.13, respectively), Dr. Fleming said.
Based on these findings and on adjusted population-attributable risk estimates, management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion. In addition, 2,500 deaths and 30,000 readmissions could be avoided annually in the United States, he noted.
Patients with adhesive small-bowel obstruction are known to have high health care utilization. Many patients are admitted to hospitalists – perhaps because most patients are managed nonoperatively, but outcome comparisons between primary medical and surgical services have been limited to single-institution studies, Dr. Fleming said.
Historically, patients with adhesive SBO were managed by surgical services, but with current management strategies, the vast majority are successfully managed without surgery, and a shift over time has resulted in more patients receiving primary management by medical services, he explained.
The current study evaluated the impact of admission to primary medical vs. surgical services on health care utilization and outcomes for adhesive SBO using a population-based data set: the New York Statewide Planning and Research Cooperative System. The system was queried for unscheduled adhesive small bowl obstruction admissions from 2002 to 2013.
Even after adjustment for the older age and increased medical comorbidities of those managed by medical vs. surgical services, the findings demonstrated that outcomes are better with primary management by surgical services, he said, adding that “experience undoubtedly plays a role,” as surgical attendings admit a higher volume of adhesive SBO patients per year.
“We feel this data strongly supports the notion that small-bowel obstruction is a surgical disease and issue, and is best managed by surgeons. … Patients with adhesive small-bowel obstruction should be admitted to surgical service,” he said.
Further, while health care delivery is continually evolving and changing, changes in models of care like that seen over time in the surgical vs. medical service management of adhesive small-bowel obstruction should be studied prospectively before widespread adoption, he said.
Dr. Fleming reported having no relevant financial disclosures.
CHICAGO – Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggested.
Admission of patients with adhesive small-bowel obstruction (SBO) to medical teams is associated with higher health care costs and worse outcomes; thus, policies favoring primary admission to surgical services could substantially reduce costs and improve outcomes, Dr. Fergal J. Fleming of the University of Rochester (N.Y.) Medical Center reported at the annual meeting of the American Surgical Association.
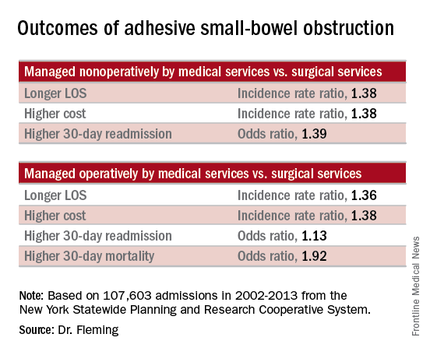
Of 107,603 admissions among patients in the data set, including 78% who were nonoperative and 22% who were operative, 43% were admitted to medical services, and 57% were admitted to surgical services. After several variables, including patient, physician, and hospital-level factors, were controlled for, patients managed nonoperatively primarily by medical services (vs. surgical services) had a longer length of stay (incidence rate ratio, 1.38), higher total cost (incidence rate ratio, 1.38), and higher 30-day readmission rate (odds ratio, 1.39). In addition, those managed operatively primarily by medical services (vs. surgical services) had a greater delay in time to surgical intervention (incidence rate ratio, 1.84), a longer length of stay (incidence rate ratio, 1.36), greater inpatient costs (incidence rate ratio, 1.38), and higher 30-day mortality and 30-day readmission rates (odds ratios, 1.92 and 1.13, respectively), Dr. Fleming said.
Based on these findings and on adjusted population-attributable risk estimates, management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion. In addition, 2,500 deaths and 30,000 readmissions could be avoided annually in the United States, he noted.
Patients with adhesive small-bowel obstruction are known to have high health care utilization. Many patients are admitted to hospitalists – perhaps because most patients are managed nonoperatively, but outcome comparisons between primary medical and surgical services have been limited to single-institution studies, Dr. Fleming said.
Historically, patients with adhesive SBO were managed by surgical services, but with current management strategies, the vast majority are successfully managed without surgery, and a shift over time has resulted in more patients receiving primary management by medical services, he explained.
The current study evaluated the impact of admission to primary medical vs. surgical services on health care utilization and outcomes for adhesive SBO using a population-based data set: the New York Statewide Planning and Research Cooperative System. The system was queried for unscheduled adhesive small bowl obstruction admissions from 2002 to 2013.
Even after adjustment for the older age and increased medical comorbidities of those managed by medical vs. surgical services, the findings demonstrated that outcomes are better with primary management by surgical services, he said, adding that “experience undoubtedly plays a role,” as surgical attendings admit a higher volume of adhesive SBO patients per year.
“We feel this data strongly supports the notion that small-bowel obstruction is a surgical disease and issue, and is best managed by surgeons. … Patients with adhesive small-bowel obstruction should be admitted to surgical service,” he said.
Further, while health care delivery is continually evolving and changing, changes in models of care like that seen over time in the surgical vs. medical service management of adhesive small-bowel obstruction should be studied prospectively before widespread adoption, he said.
Dr. Fleming reported having no relevant financial disclosures.
CHICAGO – Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggested.
Admission of patients with adhesive small-bowel obstruction (SBO) to medical teams is associated with higher health care costs and worse outcomes; thus, policies favoring primary admission to surgical services could substantially reduce costs and improve outcomes, Dr. Fergal J. Fleming of the University of Rochester (N.Y.) Medical Center reported at the annual meeting of the American Surgical Association.
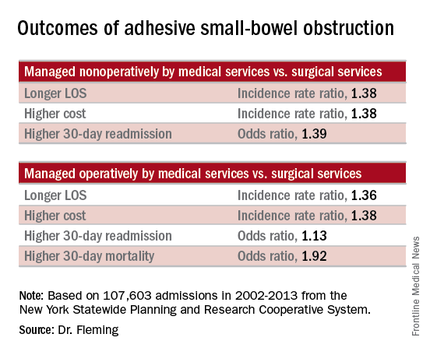
Of 107,603 admissions among patients in the data set, including 78% who were nonoperative and 22% who were operative, 43% were admitted to medical services, and 57% were admitted to surgical services. After several variables, including patient, physician, and hospital-level factors, were controlled for, patients managed nonoperatively primarily by medical services (vs. surgical services) had a longer length of stay (incidence rate ratio, 1.38), higher total cost (incidence rate ratio, 1.38), and higher 30-day readmission rate (odds ratio, 1.39). In addition, those managed operatively primarily by medical services (vs. surgical services) had a greater delay in time to surgical intervention (incidence rate ratio, 1.84), a longer length of stay (incidence rate ratio, 1.36), greater inpatient costs (incidence rate ratio, 1.38), and higher 30-day mortality and 30-day readmission rates (odds ratios, 1.92 and 1.13, respectively), Dr. Fleming said.
Based on these findings and on adjusted population-attributable risk estimates, management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion. In addition, 2,500 deaths and 30,000 readmissions could be avoided annually in the United States, he noted.
Patients with adhesive small-bowel obstruction are known to have high health care utilization. Many patients are admitted to hospitalists – perhaps because most patients are managed nonoperatively, but outcome comparisons between primary medical and surgical services have been limited to single-institution studies, Dr. Fleming said.
Historically, patients with adhesive SBO were managed by surgical services, but with current management strategies, the vast majority are successfully managed without surgery, and a shift over time has resulted in more patients receiving primary management by medical services, he explained.
The current study evaluated the impact of admission to primary medical vs. surgical services on health care utilization and outcomes for adhesive SBO using a population-based data set: the New York Statewide Planning and Research Cooperative System. The system was queried for unscheduled adhesive small bowl obstruction admissions from 2002 to 2013.
Even after adjustment for the older age and increased medical comorbidities of those managed by medical vs. surgical services, the findings demonstrated that outcomes are better with primary management by surgical services, he said, adding that “experience undoubtedly plays a role,” as surgical attendings admit a higher volume of adhesive SBO patients per year.
“We feel this data strongly supports the notion that small-bowel obstruction is a surgical disease and issue, and is best managed by surgeons. … Patients with adhesive small-bowel obstruction should be admitted to surgical service,” he said.
Further, while health care delivery is continually evolving and changing, changes in models of care like that seen over time in the surgical vs. medical service management of adhesive small-bowel obstruction should be studied prospectively before widespread adoption, he said.
Dr. Fleming reported having no relevant financial disclosures.
AT THE ASA ANNUAL MEETING
Key clinical point: Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggest.
Major finding: Management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion.
Data source: A population-based study of more than 107,600 hospital admissions
Disclosures: Dr. Fleming reported having no relevant financial disclosures.