User login
Consider patient-centered outcomes in ventral hernia repair decision
CHICAGO – Elective ventral hernia repair improves hernia-related quality of life for low- to moderate-risk patients, according to findings from a prospective patient-centered study.
The findings suggest that the risks and benefits of a conservative operative strategy should be reassessed, and that patient-centered outcomes should be considered, Dr. Julie Holihan reported at the annual meeting of the American Surgical Association.
Of 152 patients with a ventral hernia from a single hernia clinic, 97 were managed non-operatively, and 55 were managed operatively. In a propensity-matched cohort of 90 patients with similar demographics, baseline comorbidities, and quality of life scores, only operatively managed patients had improved quality of life scores at 6 months (improvement from 34.7 to 56.9 vs. from 35.6 to 36.6), according to Dr. Holihan of the University of Texas, Houston.
Further, satisfaction scores increased significantly more in the operative than in the non-operative group at follow-up (from a median score of 2 at baseline in both groups to scores of 9 and 3, respectively), and pain scores decreased significantly more in the operative group than in the non-operative group (from a baseline score of 5 down to 3 in the operative group, with no change [score of 6] in the non-operative group).
Two surgical site infections and one hernia recurrence occurred in the operative group.
Notably, the predicted risk of surgery in the cohort was much greater than the observed risk.
“We may be overestimating surgical risk in these patients,” she said.
Based on a multivariable analysis in the overall cohort, non-operative management was strongly associated with lower quality of life score (coefficient, -26.5), Dr. Holihan said.
Nonoperative management of ventral hernias is often recommended for patients, particularly in those with increased risk of surgical complications due to factors such as obesity, poorly controlled diabetes, smoking, or significant comorbidities like coronary artery disease, but this approach to management has not been well studied with respect to patient-centered outcomes such as quality of life and function, she explained.
Traditional outcomes that have been studied, including infection and hernia recurrence, may not be the outcomes that are most important to patients, she added.
For the current study, patients with ventral hernias were prospectively enrolled between June 2014 and June 2015. Non-operative management was recommended for smokers, those with a body mass index greater than 33 kg/m2, and those with poorly controlled diabetes. Measured outcomes included surgical site infection, hernia recurrence, and quality of life using a validated quality of life measure.
This is the first prospective study comparing management strategies in ventral hernia patients with comorbidities, Dr. Holihan said.
She concluded that “the elective repair of ventral hernia, compared with non-operative management, improves patient-centered outcomes in similar-risk patients.”
“Furthermore, the low occurrence of complications suggests that we may be overestimating surgical risk and that we may be too conservative in our patient selection for elective ventral hernia repair. It may be time to reevaluate patient selection criteria in order to better incorporate patient-centered outcomes,” she said.
In response to a question about managing patients with higher risk and/or higher BMI, Dr. Holihan’s coauthor, Dr. Mike K. Liang, also of the University of Texas, Houston, noted that the findings of the study provide estimates for potential future randomized trials. He also noted that the moderate-risk patients at the center often undergo “prehabilitation,” or a preoperative exercise and diet program designed to help optimize outcomes. Currently, patients with BMI of 30-40 kg/m2 are randomized to preoperative rehabilitation vs. current care.
“BMI is a very important decision making factor. We were not able to pick a standardized point [with respect to BMI] for when to operate vs. non-operate. Because of that, we used BMI as a factor in developing our propensity score,” he said, explaining that this is why the propensity-matched groups had similar BMI, while the non-operative group in the overall cohort had substantially higher BMI.
A randomized trial on prehabilitation may be able to provide some insight into the effects of rapid changes in weight and how they affect outcomes in order to make the best choices regarding surgery.
“We do hypothesize that significant weight loss prior to surgery may improve outcomes, and may make the abdominal wall more compliant and enable us to tackle more challenging hernias. We also hypothesize that patients who have a sudden increase in weight after having their ventral hernia repaired may end up having worse outcomes. Hopefully in the next year we will be able to shed more light on these very important questions.”
The authors reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review.
CHICAGO – Elective ventral hernia repair improves hernia-related quality of life for low- to moderate-risk patients, according to findings from a prospective patient-centered study.
The findings suggest that the risks and benefits of a conservative operative strategy should be reassessed, and that patient-centered outcomes should be considered, Dr. Julie Holihan reported at the annual meeting of the American Surgical Association.
Of 152 patients with a ventral hernia from a single hernia clinic, 97 were managed non-operatively, and 55 were managed operatively. In a propensity-matched cohort of 90 patients with similar demographics, baseline comorbidities, and quality of life scores, only operatively managed patients had improved quality of life scores at 6 months (improvement from 34.7 to 56.9 vs. from 35.6 to 36.6), according to Dr. Holihan of the University of Texas, Houston.
Further, satisfaction scores increased significantly more in the operative than in the non-operative group at follow-up (from a median score of 2 at baseline in both groups to scores of 9 and 3, respectively), and pain scores decreased significantly more in the operative group than in the non-operative group (from a baseline score of 5 down to 3 in the operative group, with no change [score of 6] in the non-operative group).
Two surgical site infections and one hernia recurrence occurred in the operative group.
Notably, the predicted risk of surgery in the cohort was much greater than the observed risk.
“We may be overestimating surgical risk in these patients,” she said.
Based on a multivariable analysis in the overall cohort, non-operative management was strongly associated with lower quality of life score (coefficient, -26.5), Dr. Holihan said.
Nonoperative management of ventral hernias is often recommended for patients, particularly in those with increased risk of surgical complications due to factors such as obesity, poorly controlled diabetes, smoking, or significant comorbidities like coronary artery disease, but this approach to management has not been well studied with respect to patient-centered outcomes such as quality of life and function, she explained.
Traditional outcomes that have been studied, including infection and hernia recurrence, may not be the outcomes that are most important to patients, she added.
For the current study, patients with ventral hernias were prospectively enrolled between June 2014 and June 2015. Non-operative management was recommended for smokers, those with a body mass index greater than 33 kg/m2, and those with poorly controlled diabetes. Measured outcomes included surgical site infection, hernia recurrence, and quality of life using a validated quality of life measure.
This is the first prospective study comparing management strategies in ventral hernia patients with comorbidities, Dr. Holihan said.
She concluded that “the elective repair of ventral hernia, compared with non-operative management, improves patient-centered outcomes in similar-risk patients.”
“Furthermore, the low occurrence of complications suggests that we may be overestimating surgical risk and that we may be too conservative in our patient selection for elective ventral hernia repair. It may be time to reevaluate patient selection criteria in order to better incorporate patient-centered outcomes,” she said.
In response to a question about managing patients with higher risk and/or higher BMI, Dr. Holihan’s coauthor, Dr. Mike K. Liang, also of the University of Texas, Houston, noted that the findings of the study provide estimates for potential future randomized trials. He also noted that the moderate-risk patients at the center often undergo “prehabilitation,” or a preoperative exercise and diet program designed to help optimize outcomes. Currently, patients with BMI of 30-40 kg/m2 are randomized to preoperative rehabilitation vs. current care.
“BMI is a very important decision making factor. We were not able to pick a standardized point [with respect to BMI] for when to operate vs. non-operate. Because of that, we used BMI as a factor in developing our propensity score,” he said, explaining that this is why the propensity-matched groups had similar BMI, while the non-operative group in the overall cohort had substantially higher BMI.
A randomized trial on prehabilitation may be able to provide some insight into the effects of rapid changes in weight and how they affect outcomes in order to make the best choices regarding surgery.
“We do hypothesize that significant weight loss prior to surgery may improve outcomes, and may make the abdominal wall more compliant and enable us to tackle more challenging hernias. We also hypothesize that patients who have a sudden increase in weight after having their ventral hernia repaired may end up having worse outcomes. Hopefully in the next year we will be able to shed more light on these very important questions.”
The authors reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review.
CHICAGO – Elective ventral hernia repair improves hernia-related quality of life for low- to moderate-risk patients, according to findings from a prospective patient-centered study.
The findings suggest that the risks and benefits of a conservative operative strategy should be reassessed, and that patient-centered outcomes should be considered, Dr. Julie Holihan reported at the annual meeting of the American Surgical Association.
Of 152 patients with a ventral hernia from a single hernia clinic, 97 were managed non-operatively, and 55 were managed operatively. In a propensity-matched cohort of 90 patients with similar demographics, baseline comorbidities, and quality of life scores, only operatively managed patients had improved quality of life scores at 6 months (improvement from 34.7 to 56.9 vs. from 35.6 to 36.6), according to Dr. Holihan of the University of Texas, Houston.
Further, satisfaction scores increased significantly more in the operative than in the non-operative group at follow-up (from a median score of 2 at baseline in both groups to scores of 9 and 3, respectively), and pain scores decreased significantly more in the operative group than in the non-operative group (from a baseline score of 5 down to 3 in the operative group, with no change [score of 6] in the non-operative group).
Two surgical site infections and one hernia recurrence occurred in the operative group.
Notably, the predicted risk of surgery in the cohort was much greater than the observed risk.
“We may be overestimating surgical risk in these patients,” she said.
Based on a multivariable analysis in the overall cohort, non-operative management was strongly associated with lower quality of life score (coefficient, -26.5), Dr. Holihan said.
Nonoperative management of ventral hernias is often recommended for patients, particularly in those with increased risk of surgical complications due to factors such as obesity, poorly controlled diabetes, smoking, or significant comorbidities like coronary artery disease, but this approach to management has not been well studied with respect to patient-centered outcomes such as quality of life and function, she explained.
Traditional outcomes that have been studied, including infection and hernia recurrence, may not be the outcomes that are most important to patients, she added.
For the current study, patients with ventral hernias were prospectively enrolled between June 2014 and June 2015. Non-operative management was recommended for smokers, those with a body mass index greater than 33 kg/m2, and those with poorly controlled diabetes. Measured outcomes included surgical site infection, hernia recurrence, and quality of life using a validated quality of life measure.
This is the first prospective study comparing management strategies in ventral hernia patients with comorbidities, Dr. Holihan said.
She concluded that “the elective repair of ventral hernia, compared with non-operative management, improves patient-centered outcomes in similar-risk patients.”
“Furthermore, the low occurrence of complications suggests that we may be overestimating surgical risk and that we may be too conservative in our patient selection for elective ventral hernia repair. It may be time to reevaluate patient selection criteria in order to better incorporate patient-centered outcomes,” she said.
In response to a question about managing patients with higher risk and/or higher BMI, Dr. Holihan’s coauthor, Dr. Mike K. Liang, also of the University of Texas, Houston, noted that the findings of the study provide estimates for potential future randomized trials. He also noted that the moderate-risk patients at the center often undergo “prehabilitation,” or a preoperative exercise and diet program designed to help optimize outcomes. Currently, patients with BMI of 30-40 kg/m2 are randomized to preoperative rehabilitation vs. current care.
“BMI is a very important decision making factor. We were not able to pick a standardized point [with respect to BMI] for when to operate vs. non-operate. Because of that, we used BMI as a factor in developing our propensity score,” he said, explaining that this is why the propensity-matched groups had similar BMI, while the non-operative group in the overall cohort had substantially higher BMI.
A randomized trial on prehabilitation may be able to provide some insight into the effects of rapid changes in weight and how they affect outcomes in order to make the best choices regarding surgery.
“We do hypothesize that significant weight loss prior to surgery may improve outcomes, and may make the abdominal wall more compliant and enable us to tackle more challenging hernias. We also hypothesize that patients who have a sudden increase in weight after having their ventral hernia repaired may end up having worse outcomes. Hopefully in the next year we will be able to shed more light on these very important questions.”
The authors reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: Elective ventral hernia repair improves hernia-related quality of life for low- to moderate-risk patients, according to findings from a prospective patient-centered study.
Major finding: In a propensity-matched cohort, only operatively managed patients had improved quality of life scores at 6 months (improvement from 34.7 to 56.9 vs. from 35.6 to 36.6 for nonoperative patients).
Data source: A prospective patient-centered study of 152 patients.
Disclosures: The authors reported having no disclosures.
Oxandrolone, propranolol combo increases growth in severely burned children
CHICAGO – Combination therapy with oxandrolone and propranolol can attenuate burn-induced growth arrest and increase growth rate in severely burned children, according to findings from a prospective, randomized clinical trial.
Of 612 children with burns over at least 30% of their total body surface area (average of more than 50%), 103 were randomized to receive treatment with both oxandrolone and propranolol, 67 received oxandrolone alone, 194 received propranolol alone, and 248 served as controls. After a minimum of 1 year of treatment, the average growth rate was 5.9 cm in the control group and 7.6 cm in the group receiving combination therapy, Dr. David N. Herndon of the University of Texas Medical Branch at Galveston reported at the annual meeting of the American Surgical Association.
“The rate of growth with combination therapy was significantly greater than with either of the individual drugs alone,” Dr. Herndon said.
Further, the period of growth arrest was significantly shorter – by 84 days – among those in the combination-treatment group, compared with those in the control group.
Study subjects were children treated at Shriners Hospitals for Children – Galveston from 1997 to 2015. Boys aged 6 months to 14 years and girls aged 6 months to 12 years were included to eliminate the variable onset of postpubescent growth delay. About two-thirds in each group were boys, and the ages in the patient groups were similar. Mortality was low and was similar across the groups, as was hospital length of stay.
Dr. Herndon and his colleagues controlled for heterogeneous burn distribution between the groups in the course of their analyses, as well as age.
In children with severe, extensive burn injury, the hypercatabolic response is mediated by increased production of catecholamines and corticosteroids, coupled with decreased production of testosterone. This contributes to growth arrest and to decreased strength for up to 2 years after burn injury, he explained. Children with burns over 50% of their total body surface routinely survive acute hospitalization but, at 3 months post injury, are thin, have difficulty walking, and require occupational and physical therapy to help them perform even the simplest activities of daily living.
At 1 year, a raised inflammatory mass covers their wounds, they experience itching, and they have, in large part, stunted growth; there is severe loss of lean body mass and strength, and fracture risk is increased, Dr. Herndon said.
In previous work, he and his colleagues showed that administration of propranolol at an average dose of 4 mg/kg per day for 1 year decreased cardiac work and resting energy expenditure while increasing peripheral lean mass. Further, they found that the testosterone analog oxandrolone, given at 0.1 mg/kg twice per day for 1 year, improved lean body mass accretion and bone mineral content.
The current study was conducted to test the effects of administering both agents in combination.
“The combined use of oxandrolone and propranolol in severely burned children confers an additional benefit on growth over either treatment alone,” Dr. Herndon said, adding that the additive effects of combination therapy may be due to the effects of oxandrolone on bone growth and the anti-inflammatory effects of propranolol.
“The additional benefits point out mechanistic changes that may be eventful in the treatment of hypermetabolism generally and in inflammatory states,” he concluded.
Dr. Herndon reported having no disclosures.
CHICAGO – Combination therapy with oxandrolone and propranolol can attenuate burn-induced growth arrest and increase growth rate in severely burned children, according to findings from a prospective, randomized clinical trial.
Of 612 children with burns over at least 30% of their total body surface area (average of more than 50%), 103 were randomized to receive treatment with both oxandrolone and propranolol, 67 received oxandrolone alone, 194 received propranolol alone, and 248 served as controls. After a minimum of 1 year of treatment, the average growth rate was 5.9 cm in the control group and 7.6 cm in the group receiving combination therapy, Dr. David N. Herndon of the University of Texas Medical Branch at Galveston reported at the annual meeting of the American Surgical Association.
“The rate of growth with combination therapy was significantly greater than with either of the individual drugs alone,” Dr. Herndon said.
Further, the period of growth arrest was significantly shorter – by 84 days – among those in the combination-treatment group, compared with those in the control group.
Study subjects were children treated at Shriners Hospitals for Children – Galveston from 1997 to 2015. Boys aged 6 months to 14 years and girls aged 6 months to 12 years were included to eliminate the variable onset of postpubescent growth delay. About two-thirds in each group were boys, and the ages in the patient groups were similar. Mortality was low and was similar across the groups, as was hospital length of stay.
Dr. Herndon and his colleagues controlled for heterogeneous burn distribution between the groups in the course of their analyses, as well as age.
In children with severe, extensive burn injury, the hypercatabolic response is mediated by increased production of catecholamines and corticosteroids, coupled with decreased production of testosterone. This contributes to growth arrest and to decreased strength for up to 2 years after burn injury, he explained. Children with burns over 50% of their total body surface routinely survive acute hospitalization but, at 3 months post injury, are thin, have difficulty walking, and require occupational and physical therapy to help them perform even the simplest activities of daily living.
At 1 year, a raised inflammatory mass covers their wounds, they experience itching, and they have, in large part, stunted growth; there is severe loss of lean body mass and strength, and fracture risk is increased, Dr. Herndon said.
In previous work, he and his colleagues showed that administration of propranolol at an average dose of 4 mg/kg per day for 1 year decreased cardiac work and resting energy expenditure while increasing peripheral lean mass. Further, they found that the testosterone analog oxandrolone, given at 0.1 mg/kg twice per day for 1 year, improved lean body mass accretion and bone mineral content.
The current study was conducted to test the effects of administering both agents in combination.
“The combined use of oxandrolone and propranolol in severely burned children confers an additional benefit on growth over either treatment alone,” Dr. Herndon said, adding that the additive effects of combination therapy may be due to the effects of oxandrolone on bone growth and the anti-inflammatory effects of propranolol.
“The additional benefits point out mechanistic changes that may be eventful in the treatment of hypermetabolism generally and in inflammatory states,” he concluded.
Dr. Herndon reported having no disclosures.
CHICAGO – Combination therapy with oxandrolone and propranolol can attenuate burn-induced growth arrest and increase growth rate in severely burned children, according to findings from a prospective, randomized clinical trial.
Of 612 children with burns over at least 30% of their total body surface area (average of more than 50%), 103 were randomized to receive treatment with both oxandrolone and propranolol, 67 received oxandrolone alone, 194 received propranolol alone, and 248 served as controls. After a minimum of 1 year of treatment, the average growth rate was 5.9 cm in the control group and 7.6 cm in the group receiving combination therapy, Dr. David N. Herndon of the University of Texas Medical Branch at Galveston reported at the annual meeting of the American Surgical Association.
“The rate of growth with combination therapy was significantly greater than with either of the individual drugs alone,” Dr. Herndon said.
Further, the period of growth arrest was significantly shorter – by 84 days – among those in the combination-treatment group, compared with those in the control group.
Study subjects were children treated at Shriners Hospitals for Children – Galveston from 1997 to 2015. Boys aged 6 months to 14 years and girls aged 6 months to 12 years were included to eliminate the variable onset of postpubescent growth delay. About two-thirds in each group were boys, and the ages in the patient groups were similar. Mortality was low and was similar across the groups, as was hospital length of stay.
Dr. Herndon and his colleagues controlled for heterogeneous burn distribution between the groups in the course of their analyses, as well as age.
In children with severe, extensive burn injury, the hypercatabolic response is mediated by increased production of catecholamines and corticosteroids, coupled with decreased production of testosterone. This contributes to growth arrest and to decreased strength for up to 2 years after burn injury, he explained. Children with burns over 50% of their total body surface routinely survive acute hospitalization but, at 3 months post injury, are thin, have difficulty walking, and require occupational and physical therapy to help them perform even the simplest activities of daily living.
At 1 year, a raised inflammatory mass covers their wounds, they experience itching, and they have, in large part, stunted growth; there is severe loss of lean body mass and strength, and fracture risk is increased, Dr. Herndon said.
In previous work, he and his colleagues showed that administration of propranolol at an average dose of 4 mg/kg per day for 1 year decreased cardiac work and resting energy expenditure while increasing peripheral lean mass. Further, they found that the testosterone analog oxandrolone, given at 0.1 mg/kg twice per day for 1 year, improved lean body mass accretion and bone mineral content.
The current study was conducted to test the effects of administering both agents in combination.
“The combined use of oxandrolone and propranolol in severely burned children confers an additional benefit on growth over either treatment alone,” Dr. Herndon said, adding that the additive effects of combination therapy may be due to the effects of oxandrolone on bone growth and the anti-inflammatory effects of propranolol.
“The additional benefits point out mechanistic changes that may be eventful in the treatment of hypermetabolism generally and in inflammatory states,” he concluded.
Dr. Herndon reported having no disclosures.
AT THE ASA ANNUAL MEETING
Key clinical point: Combination therapy with oxandrolone and propranolol can attenuate burn-induced growth arrest and increase growth rate in severely burned children, according to findings from a prospective, randomized clinical trial.
Major finding: After a minimum of 1 year of treatment, the average growth rate was 5.9 cm in the control group and 7.6 cm in the group receiving combination therapy.
Data source: A prospective, randomized clinical trial involving 612 children.
Disclosures: Dr. Herndon reported having no disclosures.
Focus on patient-level factors, postop complications to reduce readmissions
CHICAGO – Preadmission and postdischarge factors were important predictors of postoperative readmission in a large cohort of surgical patients, but the hospital course had little incremental impact on either readmissions or postdischarge complications in the cohort, according to a retrospective study of Veterans Affairs data.
The findings suggest that efforts to reduce postoperative readmissions should focus on enhanced postdischarge surveillance and early intervention, Dr. Melanie S. Morris of the University of Alabama at Birmingham reported at the annual meeting of the American Surgical Association.
To assess the relative contributions of patient factors, operative characteristics, and postoperative hospital course on readmissions, she and her colleagues evaluated 243,956 general, vascular, and orthopedic surgery patients in 121 VA hospitals. The overall readmission rate among the cohort was 11.1%, and for general, vascular, and orthopedic surgeries, the rates were 12.9%, 15.4%, and 7.6%, respectively; the average postoperative length of stay was 6.9 days, and 6.1% of patients experienced a predischarge complication.
Almost all readmissions occurred within 2 weeks of discharge, and for general surgery patients, most occurred within 1 week. The readmission rate for vascular surgery patients remained high beyond the 2-week mark.
An examination of the reasons for readmission showed that wound complications were the most common reason for readmission, and this was particularly true for vascular surgery patients, in whom 44% of readmissions were for wound complications, Dr. Morris said.
Gastrointestinal complications including ileus and obstruction were also common, accounting for nearly 28% of readmissions among general surgery patients, she said.
Importantly, when including preoperative data (such as demographics, comorbidities, social and behavioral factors, labs and vital signs, and planned procedure type), the variability in readmissions could only be explained 8.6% of the time, she said.
“Adding in operative data, such as procedure complexity and intraoperative blood transfusions, as well as postoperative course, added very little to our predictive ability. Including both of those groups, we could only explain 10% of the variation in readmission,” she said.
Including postdischarge data such as complications and emergency department utilization in the model increased predictive ability to 18%.
R2 and C-statistics comparing the sequentially built model showed that demographics and comorbidities contributed the most to predicting readmission risk, Dr. Morris said.
Modeling based on readmission reason and specialty improved predictive ability. For example, almost 12% of readmissions for wound complications among vascular surgery patients were predictable.
“Our best predictive ability was for orthopedic patients who were readmitted with pneumonia. We were able to predict that 14% of the time,” she said.
The findings were derived by merging VA Surgical Quality Improvement Program data from inpatient operations performed between 2007 and 2014 and involving at least a 2-day postoperative hospital stay, with clinical data including laboratory findings, vitals, prior health care utilization, and postoperative complications.
“We then grouped our variables of interest into the following categories: preoperative, operative, postoperative but predischarge, and postdischarge,” she explained, noting that logistic models predicting 30-day readmission were constructed by sequentially adding groups into the model. Models were compared by way of adjusted R2 and C-statistics.
Assuming postoperative readmissions are preventable suggests that they are linked to the quality of care during the index hospitalization. The current findings demonstrate the challenges in predicting readmissions, and are important given that hospitals with higher-than-expected readmission rates for certain diagnoses and procedures are fined by the Centers for Medicare & Medicaid Services; 54% of hospitals were fined in 2015, she said.
“Readmission is difficult to predict at the time of discharge despite exhaustive statistical modeling with very granular clinical patient-level detail. Preoperative patient factors and postdischarge complications contribute the most to predictive models. Efforts to decrease readmissions should focus on modifiable patient-level factors, transitions of care, and minimizing postoperative complications,” she concluded.
Dr. Morris reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in Annals of Surgery pending editorial review.
CHICAGO – Preadmission and postdischarge factors were important predictors of postoperative readmission in a large cohort of surgical patients, but the hospital course had little incremental impact on either readmissions or postdischarge complications in the cohort, according to a retrospective study of Veterans Affairs data.
The findings suggest that efforts to reduce postoperative readmissions should focus on enhanced postdischarge surveillance and early intervention, Dr. Melanie S. Morris of the University of Alabama at Birmingham reported at the annual meeting of the American Surgical Association.
To assess the relative contributions of patient factors, operative characteristics, and postoperative hospital course on readmissions, she and her colleagues evaluated 243,956 general, vascular, and orthopedic surgery patients in 121 VA hospitals. The overall readmission rate among the cohort was 11.1%, and for general, vascular, and orthopedic surgeries, the rates were 12.9%, 15.4%, and 7.6%, respectively; the average postoperative length of stay was 6.9 days, and 6.1% of patients experienced a predischarge complication.
Almost all readmissions occurred within 2 weeks of discharge, and for general surgery patients, most occurred within 1 week. The readmission rate for vascular surgery patients remained high beyond the 2-week mark.
An examination of the reasons for readmission showed that wound complications were the most common reason for readmission, and this was particularly true for vascular surgery patients, in whom 44% of readmissions were for wound complications, Dr. Morris said.
Gastrointestinal complications including ileus and obstruction were also common, accounting for nearly 28% of readmissions among general surgery patients, she said.
Importantly, when including preoperative data (such as demographics, comorbidities, social and behavioral factors, labs and vital signs, and planned procedure type), the variability in readmissions could only be explained 8.6% of the time, she said.
“Adding in operative data, such as procedure complexity and intraoperative blood transfusions, as well as postoperative course, added very little to our predictive ability. Including both of those groups, we could only explain 10% of the variation in readmission,” she said.
Including postdischarge data such as complications and emergency department utilization in the model increased predictive ability to 18%.
R2 and C-statistics comparing the sequentially built model showed that demographics and comorbidities contributed the most to predicting readmission risk, Dr. Morris said.
Modeling based on readmission reason and specialty improved predictive ability. For example, almost 12% of readmissions for wound complications among vascular surgery patients were predictable.
“Our best predictive ability was for orthopedic patients who were readmitted with pneumonia. We were able to predict that 14% of the time,” she said.
The findings were derived by merging VA Surgical Quality Improvement Program data from inpatient operations performed between 2007 and 2014 and involving at least a 2-day postoperative hospital stay, with clinical data including laboratory findings, vitals, prior health care utilization, and postoperative complications.
“We then grouped our variables of interest into the following categories: preoperative, operative, postoperative but predischarge, and postdischarge,” she explained, noting that logistic models predicting 30-day readmission were constructed by sequentially adding groups into the model. Models were compared by way of adjusted R2 and C-statistics.
Assuming postoperative readmissions are preventable suggests that they are linked to the quality of care during the index hospitalization. The current findings demonstrate the challenges in predicting readmissions, and are important given that hospitals with higher-than-expected readmission rates for certain diagnoses and procedures are fined by the Centers for Medicare & Medicaid Services; 54% of hospitals were fined in 2015, she said.
“Readmission is difficult to predict at the time of discharge despite exhaustive statistical modeling with very granular clinical patient-level detail. Preoperative patient factors and postdischarge complications contribute the most to predictive models. Efforts to decrease readmissions should focus on modifiable patient-level factors, transitions of care, and minimizing postoperative complications,” she concluded.
Dr. Morris reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in Annals of Surgery pending editorial review.
CHICAGO – Preadmission and postdischarge factors were important predictors of postoperative readmission in a large cohort of surgical patients, but the hospital course had little incremental impact on either readmissions or postdischarge complications in the cohort, according to a retrospective study of Veterans Affairs data.
The findings suggest that efforts to reduce postoperative readmissions should focus on enhanced postdischarge surveillance and early intervention, Dr. Melanie S. Morris of the University of Alabama at Birmingham reported at the annual meeting of the American Surgical Association.
To assess the relative contributions of patient factors, operative characteristics, and postoperative hospital course on readmissions, she and her colleagues evaluated 243,956 general, vascular, and orthopedic surgery patients in 121 VA hospitals. The overall readmission rate among the cohort was 11.1%, and for general, vascular, and orthopedic surgeries, the rates were 12.9%, 15.4%, and 7.6%, respectively; the average postoperative length of stay was 6.9 days, and 6.1% of patients experienced a predischarge complication.
Almost all readmissions occurred within 2 weeks of discharge, and for general surgery patients, most occurred within 1 week. The readmission rate for vascular surgery patients remained high beyond the 2-week mark.
An examination of the reasons for readmission showed that wound complications were the most common reason for readmission, and this was particularly true for vascular surgery patients, in whom 44% of readmissions were for wound complications, Dr. Morris said.
Gastrointestinal complications including ileus and obstruction were also common, accounting for nearly 28% of readmissions among general surgery patients, she said.
Importantly, when including preoperative data (such as demographics, comorbidities, social and behavioral factors, labs and vital signs, and planned procedure type), the variability in readmissions could only be explained 8.6% of the time, she said.
“Adding in operative data, such as procedure complexity and intraoperative blood transfusions, as well as postoperative course, added very little to our predictive ability. Including both of those groups, we could only explain 10% of the variation in readmission,” she said.
Including postdischarge data such as complications and emergency department utilization in the model increased predictive ability to 18%.
R2 and C-statistics comparing the sequentially built model showed that demographics and comorbidities contributed the most to predicting readmission risk, Dr. Morris said.
Modeling based on readmission reason and specialty improved predictive ability. For example, almost 12% of readmissions for wound complications among vascular surgery patients were predictable.
“Our best predictive ability was for orthopedic patients who were readmitted with pneumonia. We were able to predict that 14% of the time,” she said.
The findings were derived by merging VA Surgical Quality Improvement Program data from inpatient operations performed between 2007 and 2014 and involving at least a 2-day postoperative hospital stay, with clinical data including laboratory findings, vitals, prior health care utilization, and postoperative complications.
“We then grouped our variables of interest into the following categories: preoperative, operative, postoperative but predischarge, and postdischarge,” she explained, noting that logistic models predicting 30-day readmission were constructed by sequentially adding groups into the model. Models were compared by way of adjusted R2 and C-statistics.
Assuming postoperative readmissions are preventable suggests that they are linked to the quality of care during the index hospitalization. The current findings demonstrate the challenges in predicting readmissions, and are important given that hospitals with higher-than-expected readmission rates for certain diagnoses and procedures are fined by the Centers for Medicare & Medicaid Services; 54% of hospitals were fined in 2015, she said.
“Readmission is difficult to predict at the time of discharge despite exhaustive statistical modeling with very granular clinical patient-level detail. Preoperative patient factors and postdischarge complications contribute the most to predictive models. Efforts to decrease readmissions should focus on modifiable patient-level factors, transitions of care, and minimizing postoperative complications,” she concluded.
Dr. Morris reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: Preadmission and postdischarge factors were important predictors of postoperative readmission in a large cohort of surgical patients, but the hospital course had little incremental impact on either readmissions or postdischarge complications.
Major finding: Including both preoperative and operative data in the model predicted only 10% of the variability in readmission rates.
Data source: A retrospective study of data for nearly 244,000 VA patients.
Disclosures: Dr. Morris reported having no disclosures.
Algorithm reduces CT use in pediatric appendicitis
CHICAGO – Use of a diagnostic algorithm for pediatric appendicitis significantly decreases computed tomography utilization without compromising high sensitivity and specificity, according to findings from a study of emergency cases.
Of 840 patients seen in an academic children’s hospital emergency department from Aug. 1, 2014 to July 31, 2015, after implementation of the diagnostic algorithm, 267 were diagnosed with appendicitis. CT utilization was 27.3% overall, and 24.2% in patients with appendicitis, compared with 75.4% among 557 patients with appendicitis seen from Jan. 1, 2011 to February 28, 2014, before implementation, Dr. Sohail R. Shah of Baylor College of Medicine/Texas Children’s Hospital, Houston reported at the annual meeting of the American Surgical Association
The work was completed at his prior position at Children’s Mercy Hospital Kansas City.
“Additionally, utilization of ultrasound prior to CT went from 24% up to 95%, surgical consultation prior to CT increased from 14.7% to 76.1% after implementation, and operative intervention without any imaging went from just under 2% to almost 10% after implementation of the diagnostic algorithm,” Dr. Shah said, adding that the pre- and postimplementation patient groups were similar with respect to demographics.
The diagnostic pathway had a sensitivity of 98.6% and specificity of 94.4%, he said.
Appendicitis is the most common abdominal condition leading to the hospitalization of children, and it accounts for about 70,000 children hospitalized annually in the United States, with an average related healthcare cost of $675 million each year, he said.
The diagnosis in children can be difficult, thus many centers rely heavily on CT scans. However, increasing use of CT in children could lead to an increased lifetime risk of radiation-induced malignancy.
“In fact, the American College of Radiology currently recommends that a CT scan not be done for the diagnosis of appendicitis until after ultrasound has been considered as an option. Our objective with this work was to decrease CT utilization for the diagnosis of appendicitis in children at our academic free-standing children’s hospital emergency department through the introduction of a diagnostic algorithm,” he said.
A multidisciplinary team at Children’s Mercy Hospital worked to develop an algorithm, which promoted earlier surgical consultation and prioritized ultrasound imaging over CT scans. The algorithm involved the use of the 10-point Pediatric Appendicitis Score for risk stratification. For a score of 1-3, with low probability of appendicitis, the patient was discharged home or received further work-up for an alternative diagnosis. For a score of 4-6, with intermediate probability of appendicitis, an ultrasound was ordered. If the ultrasound was negative, the patient was discharged home or received further work-up for an alternative diagnosis; if the ultrasound was positive, surgery was consulted; if the ultrasound was indeterminate, surgery was consulted prior to consideration of CT scan. For a score of 7-10, surgery was immediately consulted for further management.
“If this algorithm is followed appropriately for all patients, then no patient should have a CT scan without first having an ultrasound and surgical consultation,” Dr. Shah said.
He reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review.
CHICAGO – Use of a diagnostic algorithm for pediatric appendicitis significantly decreases computed tomography utilization without compromising high sensitivity and specificity, according to findings from a study of emergency cases.
Of 840 patients seen in an academic children’s hospital emergency department from Aug. 1, 2014 to July 31, 2015, after implementation of the diagnostic algorithm, 267 were diagnosed with appendicitis. CT utilization was 27.3% overall, and 24.2% in patients with appendicitis, compared with 75.4% among 557 patients with appendicitis seen from Jan. 1, 2011 to February 28, 2014, before implementation, Dr. Sohail R. Shah of Baylor College of Medicine/Texas Children’s Hospital, Houston reported at the annual meeting of the American Surgical Association
The work was completed at his prior position at Children’s Mercy Hospital Kansas City.
“Additionally, utilization of ultrasound prior to CT went from 24% up to 95%, surgical consultation prior to CT increased from 14.7% to 76.1% after implementation, and operative intervention without any imaging went from just under 2% to almost 10% after implementation of the diagnostic algorithm,” Dr. Shah said, adding that the pre- and postimplementation patient groups were similar with respect to demographics.
The diagnostic pathway had a sensitivity of 98.6% and specificity of 94.4%, he said.
Appendicitis is the most common abdominal condition leading to the hospitalization of children, and it accounts for about 70,000 children hospitalized annually in the United States, with an average related healthcare cost of $675 million each year, he said.
The diagnosis in children can be difficult, thus many centers rely heavily on CT scans. However, increasing use of CT in children could lead to an increased lifetime risk of radiation-induced malignancy.
“In fact, the American College of Radiology currently recommends that a CT scan not be done for the diagnosis of appendicitis until after ultrasound has been considered as an option. Our objective with this work was to decrease CT utilization for the diagnosis of appendicitis in children at our academic free-standing children’s hospital emergency department through the introduction of a diagnostic algorithm,” he said.
A multidisciplinary team at Children’s Mercy Hospital worked to develop an algorithm, which promoted earlier surgical consultation and prioritized ultrasound imaging over CT scans. The algorithm involved the use of the 10-point Pediatric Appendicitis Score for risk stratification. For a score of 1-3, with low probability of appendicitis, the patient was discharged home or received further work-up for an alternative diagnosis. For a score of 4-6, with intermediate probability of appendicitis, an ultrasound was ordered. If the ultrasound was negative, the patient was discharged home or received further work-up for an alternative diagnosis; if the ultrasound was positive, surgery was consulted; if the ultrasound was indeterminate, surgery was consulted prior to consideration of CT scan. For a score of 7-10, surgery was immediately consulted for further management.
“If this algorithm is followed appropriately for all patients, then no patient should have a CT scan without first having an ultrasound and surgical consultation,” Dr. Shah said.
He reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review.
CHICAGO – Use of a diagnostic algorithm for pediatric appendicitis significantly decreases computed tomography utilization without compromising high sensitivity and specificity, according to findings from a study of emergency cases.
Of 840 patients seen in an academic children’s hospital emergency department from Aug. 1, 2014 to July 31, 2015, after implementation of the diagnostic algorithm, 267 were diagnosed with appendicitis. CT utilization was 27.3% overall, and 24.2% in patients with appendicitis, compared with 75.4% among 557 patients with appendicitis seen from Jan. 1, 2011 to February 28, 2014, before implementation, Dr. Sohail R. Shah of Baylor College of Medicine/Texas Children’s Hospital, Houston reported at the annual meeting of the American Surgical Association
The work was completed at his prior position at Children’s Mercy Hospital Kansas City.
“Additionally, utilization of ultrasound prior to CT went from 24% up to 95%, surgical consultation prior to CT increased from 14.7% to 76.1% after implementation, and operative intervention without any imaging went from just under 2% to almost 10% after implementation of the diagnostic algorithm,” Dr. Shah said, adding that the pre- and postimplementation patient groups were similar with respect to demographics.
The diagnostic pathway had a sensitivity of 98.6% and specificity of 94.4%, he said.
Appendicitis is the most common abdominal condition leading to the hospitalization of children, and it accounts for about 70,000 children hospitalized annually in the United States, with an average related healthcare cost of $675 million each year, he said.
The diagnosis in children can be difficult, thus many centers rely heavily on CT scans. However, increasing use of CT in children could lead to an increased lifetime risk of radiation-induced malignancy.
“In fact, the American College of Radiology currently recommends that a CT scan not be done for the diagnosis of appendicitis until after ultrasound has been considered as an option. Our objective with this work was to decrease CT utilization for the diagnosis of appendicitis in children at our academic free-standing children’s hospital emergency department through the introduction of a diagnostic algorithm,” he said.
A multidisciplinary team at Children’s Mercy Hospital worked to develop an algorithm, which promoted earlier surgical consultation and prioritized ultrasound imaging over CT scans. The algorithm involved the use of the 10-point Pediatric Appendicitis Score for risk stratification. For a score of 1-3, with low probability of appendicitis, the patient was discharged home or received further work-up for an alternative diagnosis. For a score of 4-6, with intermediate probability of appendicitis, an ultrasound was ordered. If the ultrasound was negative, the patient was discharged home or received further work-up for an alternative diagnosis; if the ultrasound was positive, surgery was consulted; if the ultrasound was indeterminate, surgery was consulted prior to consideration of CT scan. For a score of 7-10, surgery was immediately consulted for further management.
“If this algorithm is followed appropriately for all patients, then no patient should have a CT scan without first having an ultrasound and surgical consultation,” Dr. Shah said.
He reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: Use of a diagnostic algorithm for pediatric appendicitis significantly decreases computed tomography utilization without compromising high sensitivity and specificity, according to findings from a study of nearly 1,400 cases.
Major finding: CT utilization in patients with appendicitis was 24.2% before, and 75.4% after, implementation of the algorithm.
Data source: A review of nearly 1,400 pediatric appendicitis cases.
Disclosures: Dr. Shah reported having no disclosures.
Plasma microRNA assay differentiates colorectal neoplasia
CHICAGO – A novel plasma microRNA assay and prediction model appears to successfully differentiate colorectal neoplasia from other neoplasms and from controls.
The assay includes seven microRNAs that were selected, based on P value, area under the curve (AUC), fold change, and biological plausibility, from among 380 microRNAs screened using microfluidic array technology from a “training” cohort of 60 patients. The training cohort included groups of patients, 10 each, with colorectal cancer, advanced adenoma, breast cancer, pancreatic cancer, and lung cancer – cancers chosen because they frequently develop at similar ages as colon cancer – and 10 controls.
A panel of seven “uniquely dysregulated” microRNAs specific for colorectal neoplasia was evaluated using single assays in a “test” cohort of 120 patients. A mathematical model was developed to predict sample identity in a 150-patient blinded “validation” cohort using repeat-subsampling validation of the testing dataset with 1,000 iterations each to assess model detection accuracy, Dr. Jane V. Carter of the University of Louisville (Ky.) explained at the annual meeting of the American Surgical Association.
The area under the curve for test cohort comparisons with the assay was 0.91, 0.79, and 0.98 for comparison No. 1 (comparing any neoplasia vs. controls), comparison No. 2 (comparing colorectal neoplasia with other cancers) and comparison No. 3 (comparing colorectal cancer with colorectal adenomas) respectively, Dr. Carter reported.
“Our prediction model identified blinded sample identity with 69%-77% accuracy in comparison No. 1, 66%-76% accuracy in comparison No. 2, and 86%-90% accuracy in comparison No. 3,” she said, noting that the sensitivity and specificity of the assay compare very well with current clinical standards.
Colorectal neoplasms frequently develop in individuals at ages when other common cancers also occur. Current screening methods, including endoscopic and imaging studies and fecal testing have poor patient compliance. Fecal and blood tests lack sensitivity and specificity for the detection of adenomas, limiting their use as screening methods, she said.
But this novel assay, which builds on the earlier work identifying miR-21 as a potential marker for colorectal cancer, provides a useful tool for identifying colorectal neoplasms, she said.
Efforts are underway to confirm the findings in a larger study population. If the findings are confirmed, the assay may have other potential uses such as monitoring therapy by comparing microRNA expression before and after treatment, and also for predicting response to treatment such as following preoperative neoadjuvant chemoradiation, Dr. Carter suggested.
The current findings have significant implications for the development of a noninvasive, reliable, and reproducible screening test for detection of colorectal neoplasia.
“If we can improve early-stage detection, we can improve survival,” she said.
Dr. Carter reported having no relevant disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review.
CHICAGO – A novel plasma microRNA assay and prediction model appears to successfully differentiate colorectal neoplasia from other neoplasms and from controls.
The assay includes seven microRNAs that were selected, based on P value, area under the curve (AUC), fold change, and biological plausibility, from among 380 microRNAs screened using microfluidic array technology from a “training” cohort of 60 patients. The training cohort included groups of patients, 10 each, with colorectal cancer, advanced adenoma, breast cancer, pancreatic cancer, and lung cancer – cancers chosen because they frequently develop at similar ages as colon cancer – and 10 controls.
A panel of seven “uniquely dysregulated” microRNAs specific for colorectal neoplasia was evaluated using single assays in a “test” cohort of 120 patients. A mathematical model was developed to predict sample identity in a 150-patient blinded “validation” cohort using repeat-subsampling validation of the testing dataset with 1,000 iterations each to assess model detection accuracy, Dr. Jane V. Carter of the University of Louisville (Ky.) explained at the annual meeting of the American Surgical Association.
The area under the curve for test cohort comparisons with the assay was 0.91, 0.79, and 0.98 for comparison No. 1 (comparing any neoplasia vs. controls), comparison No. 2 (comparing colorectal neoplasia with other cancers) and comparison No. 3 (comparing colorectal cancer with colorectal adenomas) respectively, Dr. Carter reported.
“Our prediction model identified blinded sample identity with 69%-77% accuracy in comparison No. 1, 66%-76% accuracy in comparison No. 2, and 86%-90% accuracy in comparison No. 3,” she said, noting that the sensitivity and specificity of the assay compare very well with current clinical standards.
Colorectal neoplasms frequently develop in individuals at ages when other common cancers also occur. Current screening methods, including endoscopic and imaging studies and fecal testing have poor patient compliance. Fecal and blood tests lack sensitivity and specificity for the detection of adenomas, limiting their use as screening methods, she said.
But this novel assay, which builds on the earlier work identifying miR-21 as a potential marker for colorectal cancer, provides a useful tool for identifying colorectal neoplasms, she said.
Efforts are underway to confirm the findings in a larger study population. If the findings are confirmed, the assay may have other potential uses such as monitoring therapy by comparing microRNA expression before and after treatment, and also for predicting response to treatment such as following preoperative neoadjuvant chemoradiation, Dr. Carter suggested.
The current findings have significant implications for the development of a noninvasive, reliable, and reproducible screening test for detection of colorectal neoplasia.
“If we can improve early-stage detection, we can improve survival,” she said.
Dr. Carter reported having no relevant disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review.
CHICAGO – A novel plasma microRNA assay and prediction model appears to successfully differentiate colorectal neoplasia from other neoplasms and from controls.
The assay includes seven microRNAs that were selected, based on P value, area under the curve (AUC), fold change, and biological plausibility, from among 380 microRNAs screened using microfluidic array technology from a “training” cohort of 60 patients. The training cohort included groups of patients, 10 each, with colorectal cancer, advanced adenoma, breast cancer, pancreatic cancer, and lung cancer – cancers chosen because they frequently develop at similar ages as colon cancer – and 10 controls.
A panel of seven “uniquely dysregulated” microRNAs specific for colorectal neoplasia was evaluated using single assays in a “test” cohort of 120 patients. A mathematical model was developed to predict sample identity in a 150-patient blinded “validation” cohort using repeat-subsampling validation of the testing dataset with 1,000 iterations each to assess model detection accuracy, Dr. Jane V. Carter of the University of Louisville (Ky.) explained at the annual meeting of the American Surgical Association.
The area under the curve for test cohort comparisons with the assay was 0.91, 0.79, and 0.98 for comparison No. 1 (comparing any neoplasia vs. controls), comparison No. 2 (comparing colorectal neoplasia with other cancers) and comparison No. 3 (comparing colorectal cancer with colorectal adenomas) respectively, Dr. Carter reported.
“Our prediction model identified blinded sample identity with 69%-77% accuracy in comparison No. 1, 66%-76% accuracy in comparison No. 2, and 86%-90% accuracy in comparison No. 3,” she said, noting that the sensitivity and specificity of the assay compare very well with current clinical standards.
Colorectal neoplasms frequently develop in individuals at ages when other common cancers also occur. Current screening methods, including endoscopic and imaging studies and fecal testing have poor patient compliance. Fecal and blood tests lack sensitivity and specificity for the detection of adenomas, limiting their use as screening methods, she said.
But this novel assay, which builds on the earlier work identifying miR-21 as a potential marker for colorectal cancer, provides a useful tool for identifying colorectal neoplasms, she said.
Efforts are underway to confirm the findings in a larger study population. If the findings are confirmed, the assay may have other potential uses such as monitoring therapy by comparing microRNA expression before and after treatment, and also for predicting response to treatment such as following preoperative neoadjuvant chemoradiation, Dr. Carter suggested.
The current findings have significant implications for the development of a noninvasive, reliable, and reproducible screening test for detection of colorectal neoplasia.
“If we can improve early-stage detection, we can improve survival,” she said.
Dr. Carter reported having no relevant disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: A novel plasma microRNA assay and prediction model appears to successfully differentiate colorectal neoplasia from other neoplasms and from controls.
Major finding: The prediction model identified sample identity with 69%-77% accuracy when comparing any neoplasia vs. controls, 66%-76% accuracy when comparing colorectal neoplasia with other cancers, and 86%-90% accuracy when comparing colorectal cancer with colorectal adenomas.
Data source: A prediction model used in a 60-person training cohort, a 120-person testing cohort, and a 150-person validation cohort.
Disclosures: Dr. Carter reported having no relevant disclosures.
Diverticulitis recurs more with observation vs. elective resection
CHICAGO – Observation, compared with elective resection, was associated with significantly increased recurrence rates in a single-center randomized, controlled trial of patients who had successfully recovered via nonoperative management from their first episode of acute sigmoid diverticulitis with extraluminal air/abscess.
Recurrence rates in 111 patients randomized to observation or elective resection were 31% in the observation group and 7% in the resection group, at 15 and 18 months, respectively, Dr. Ryan Bendl of State University of New York, Stony Brook reported at the annual meeting of the American Surgical Association.
Patients in the two groups were comparable with respect to age, sex, body mass index, Colorectal Physiologic and Operative Severity Score for the Enumeration of Mortality and Morbidity (CR-POSSUM), and comorbidities, he noted.
Subjects included in the single-center study were adults admitted for a first episode of acute diverticulitis with abscess or extraluminal air who were managed nonoperatively with intravenous antibiotics, a period of nothing by mouth, drainage, and total parenteral nutrition followed by colonoscopy. They were randomized 3:1 to observation or resection, and 68% of the elective resection patients underwent minimally invasive surgery. The study’s primary endpoint was recurrent diverticulitis defined as an acute episode confirmed by computed tomography and requiring hospitalization with intravenous antibiotics.
Diverticulitis accounted for more than 300,000 hospital admissions in 2010 in the United States alone, and 10%-20% of patients had abscess formation. At one time, most patients were managed with immediate operative intervention, but medical and radiologic advances have led to a shift toward nonoperative management, Dr. Bendl said.
Some prior studies have suggested that recurrence rates are higher with nonoperative management, and the current study supports those data.
However, despite the significant increase in the recurrence rate with observation vs. resection, most patients in the observation group did not experience recurrence, and of those who did, none had peritonitis.
“All those with recurrences were successfully treated again using nonoperative management,” he said.
This study was supported in part by grants from Merck and Covidien. Dr. Bendl reported having no relevant financial disclosures.
CHICAGO – Observation, compared with elective resection, was associated with significantly increased recurrence rates in a single-center randomized, controlled trial of patients who had successfully recovered via nonoperative management from their first episode of acute sigmoid diverticulitis with extraluminal air/abscess.
Recurrence rates in 111 patients randomized to observation or elective resection were 31% in the observation group and 7% in the resection group, at 15 and 18 months, respectively, Dr. Ryan Bendl of State University of New York, Stony Brook reported at the annual meeting of the American Surgical Association.
Patients in the two groups were comparable with respect to age, sex, body mass index, Colorectal Physiologic and Operative Severity Score for the Enumeration of Mortality and Morbidity (CR-POSSUM), and comorbidities, he noted.
Subjects included in the single-center study were adults admitted for a first episode of acute diverticulitis with abscess or extraluminal air who were managed nonoperatively with intravenous antibiotics, a period of nothing by mouth, drainage, and total parenteral nutrition followed by colonoscopy. They were randomized 3:1 to observation or resection, and 68% of the elective resection patients underwent minimally invasive surgery. The study’s primary endpoint was recurrent diverticulitis defined as an acute episode confirmed by computed tomography and requiring hospitalization with intravenous antibiotics.
Diverticulitis accounted for more than 300,000 hospital admissions in 2010 in the United States alone, and 10%-20% of patients had abscess formation. At one time, most patients were managed with immediate operative intervention, but medical and radiologic advances have led to a shift toward nonoperative management, Dr. Bendl said.
Some prior studies have suggested that recurrence rates are higher with nonoperative management, and the current study supports those data.
However, despite the significant increase in the recurrence rate with observation vs. resection, most patients in the observation group did not experience recurrence, and of those who did, none had peritonitis.
“All those with recurrences were successfully treated again using nonoperative management,” he said.
This study was supported in part by grants from Merck and Covidien. Dr. Bendl reported having no relevant financial disclosures.
CHICAGO – Observation, compared with elective resection, was associated with significantly increased recurrence rates in a single-center randomized, controlled trial of patients who had successfully recovered via nonoperative management from their first episode of acute sigmoid diverticulitis with extraluminal air/abscess.
Recurrence rates in 111 patients randomized to observation or elective resection were 31% in the observation group and 7% in the resection group, at 15 and 18 months, respectively, Dr. Ryan Bendl of State University of New York, Stony Brook reported at the annual meeting of the American Surgical Association.
Patients in the two groups were comparable with respect to age, sex, body mass index, Colorectal Physiologic and Operative Severity Score for the Enumeration of Mortality and Morbidity (CR-POSSUM), and comorbidities, he noted.
Subjects included in the single-center study were adults admitted for a first episode of acute diverticulitis with abscess or extraluminal air who were managed nonoperatively with intravenous antibiotics, a period of nothing by mouth, drainage, and total parenteral nutrition followed by colonoscopy. They were randomized 3:1 to observation or resection, and 68% of the elective resection patients underwent minimally invasive surgery. The study’s primary endpoint was recurrent diverticulitis defined as an acute episode confirmed by computed tomography and requiring hospitalization with intravenous antibiotics.
Diverticulitis accounted for more than 300,000 hospital admissions in 2010 in the United States alone, and 10%-20% of patients had abscess formation. At one time, most patients were managed with immediate operative intervention, but medical and radiologic advances have led to a shift toward nonoperative management, Dr. Bendl said.
Some prior studies have suggested that recurrence rates are higher with nonoperative management, and the current study supports those data.
However, despite the significant increase in the recurrence rate with observation vs. resection, most patients in the observation group did not experience recurrence, and of those who did, none had peritonitis.
“All those with recurrences were successfully treated again using nonoperative management,” he said.
This study was supported in part by grants from Merck and Covidien. Dr. Bendl reported having no relevant financial disclosures.
AT THE ASA ANNUAL MEETING
Key clinical point: Observation vs. elective resection was associated with significantly increased recurrence rates in patients who had recovered via nonoperative management from their first episode of acute sigmoid diverticulitis with extraluminal air/abscess.
Major finding: Recurrence rates in 111 patients randomized to observation or elective resection were 31% in the observation group and 7% in the resection group, at 15 and 18 months, respectively.
Data source: A randomized, controlled trial involving 111 patients.
Disclosures: This study was supported in part by grants from Merck and Covidien. Dr. Bendl reported having no relevant financial disclosures.
Admission to surgical service appears optimal for adhesive small-bowel obstruction
CHICAGO – Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggested.
Admission of patients with adhesive small-bowel obstruction (SBO) to medical teams is associated with higher health care costs and worse outcomes; thus, policies favoring primary admission to surgical services could substantially reduce costs and improve outcomes, Dr. Fergal J. Fleming of the University of Rochester (N.Y.) Medical Center reported at the annual meeting of the American Surgical Association.
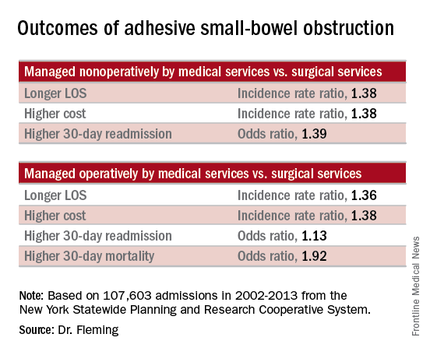
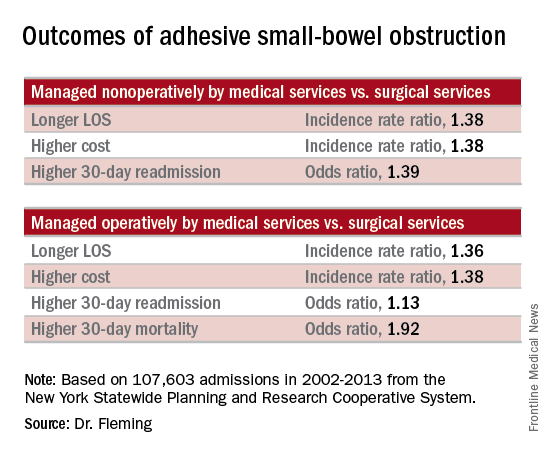
Of 107,603 admissions among patients in the data set, including 78% who were nonoperative and 22% who were operative, 43% were admitted to medical services, and 57% were admitted to surgical services. After several variables, including patient, physician, and hospital-level factors, were controlled for, patients managed nonoperatively primarily by medical services (vs. surgical services) had a longer length of stay (incidence rate ratio, 1.38), higher total cost (incidence rate ratio, 1.38), and higher 30-day readmission rate (odds ratio, 1.39). In addition, those managed operatively primarily by medical services (vs. surgical services) had a greater delay in time to surgical intervention (incidence rate ratio, 1.84), a longer length of stay (incidence rate ratio, 1.36), greater inpatient costs (incidence rate ratio, 1.38), and higher 30-day mortality and 30-day readmission rates (odds ratios, 1.92 and 1.13, respectively), Dr. Fleming said.
Based on these findings and on adjusted population-attributable risk estimates, management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion. In addition, 2,500 deaths and 30,000 readmissions could be avoided annually in the United States, he noted.
Patients with adhesive small-bowel obstruction are known to have high health care utilization. Many patients are admitted to hospitalists – perhaps because most patients are managed nonoperatively, but outcome comparisons between primary medical and surgical services have been limited to single-institution studies, Dr. Fleming said.
Historically, patients with adhesive SBO were managed by surgical services, but with current management strategies, the vast majority are successfully managed without surgery, and a shift over time has resulted in more patients receiving primary management by medical services, he explained.
The current study evaluated the impact of admission to primary medical vs. surgical services on health care utilization and outcomes for adhesive SBO using a population-based data set: the New York Statewide Planning and Research Cooperative System. The system was queried for unscheduled adhesive small bowl obstruction admissions from 2002 to 2013.
Even after adjustment for the older age and increased medical comorbidities of those managed by medical vs. surgical services, the findings demonstrated that outcomes are better with primary management by surgical services, he said, adding that “experience undoubtedly plays a role,” as surgical attendings admit a higher volume of adhesive SBO patients per year.
“We feel this data strongly supports the notion that small-bowel obstruction is a surgical disease and issue, and is best managed by surgeons. … Patients with adhesive small-bowel obstruction should be admitted to surgical service,” he said.
Further, while health care delivery is continually evolving and changing, changes in models of care like that seen over time in the surgical vs. medical service management of adhesive small-bowel obstruction should be studied prospectively before widespread adoption, he said.
Dr. Fleming reported having no relevant financial disclosures.
CHICAGO – Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggested.
Admission of patients with adhesive small-bowel obstruction (SBO) to medical teams is associated with higher health care costs and worse outcomes; thus, policies favoring primary admission to surgical services could substantially reduce costs and improve outcomes, Dr. Fergal J. Fleming of the University of Rochester (N.Y.) Medical Center reported at the annual meeting of the American Surgical Association.
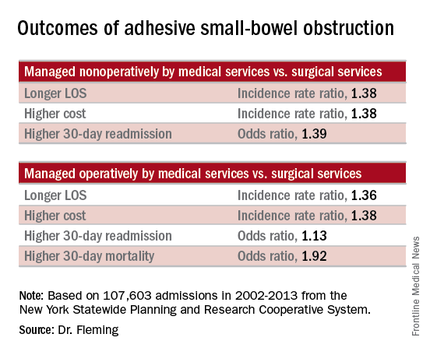
Of 107,603 admissions among patients in the data set, including 78% who were nonoperative and 22% who were operative, 43% were admitted to medical services, and 57% were admitted to surgical services. After several variables, including patient, physician, and hospital-level factors, were controlled for, patients managed nonoperatively primarily by medical services (vs. surgical services) had a longer length of stay (incidence rate ratio, 1.38), higher total cost (incidence rate ratio, 1.38), and higher 30-day readmission rate (odds ratio, 1.39). In addition, those managed operatively primarily by medical services (vs. surgical services) had a greater delay in time to surgical intervention (incidence rate ratio, 1.84), a longer length of stay (incidence rate ratio, 1.36), greater inpatient costs (incidence rate ratio, 1.38), and higher 30-day mortality and 30-day readmission rates (odds ratios, 1.92 and 1.13, respectively), Dr. Fleming said.
Based on these findings and on adjusted population-attributable risk estimates, management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion. In addition, 2,500 deaths and 30,000 readmissions could be avoided annually in the United States, he noted.
Patients with adhesive small-bowel obstruction are known to have high health care utilization. Many patients are admitted to hospitalists – perhaps because most patients are managed nonoperatively, but outcome comparisons between primary medical and surgical services have been limited to single-institution studies, Dr. Fleming said.
Historically, patients with adhesive SBO were managed by surgical services, but with current management strategies, the vast majority are successfully managed without surgery, and a shift over time has resulted in more patients receiving primary management by medical services, he explained.
The current study evaluated the impact of admission to primary medical vs. surgical services on health care utilization and outcomes for adhesive SBO using a population-based data set: the New York Statewide Planning and Research Cooperative System. The system was queried for unscheduled adhesive small bowl obstruction admissions from 2002 to 2013.
Even after adjustment for the older age and increased medical comorbidities of those managed by medical vs. surgical services, the findings demonstrated that outcomes are better with primary management by surgical services, he said, adding that “experience undoubtedly plays a role,” as surgical attendings admit a higher volume of adhesive SBO patients per year.
“We feel this data strongly supports the notion that small-bowel obstruction is a surgical disease and issue, and is best managed by surgeons. … Patients with adhesive small-bowel obstruction should be admitted to surgical service,” he said.
Further, while health care delivery is continually evolving and changing, changes in models of care like that seen over time in the surgical vs. medical service management of adhesive small-bowel obstruction should be studied prospectively before widespread adoption, he said.
Dr. Fleming reported having no relevant financial disclosures.
CHICAGO – Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggested.
Admission of patients with adhesive small-bowel obstruction (SBO) to medical teams is associated with higher health care costs and worse outcomes; thus, policies favoring primary admission to surgical services could substantially reduce costs and improve outcomes, Dr. Fergal J. Fleming of the University of Rochester (N.Y.) Medical Center reported at the annual meeting of the American Surgical Association.
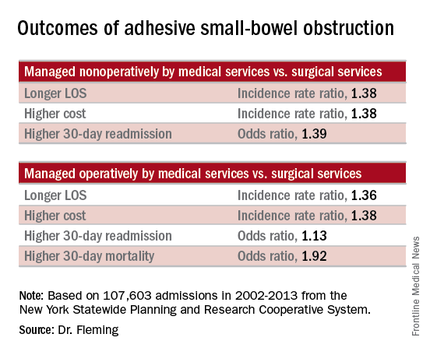
Of 107,603 admissions among patients in the data set, including 78% who were nonoperative and 22% who were operative, 43% were admitted to medical services, and 57% were admitted to surgical services. After several variables, including patient, physician, and hospital-level factors, were controlled for, patients managed nonoperatively primarily by medical services (vs. surgical services) had a longer length of stay (incidence rate ratio, 1.38), higher total cost (incidence rate ratio, 1.38), and higher 30-day readmission rate (odds ratio, 1.39). In addition, those managed operatively primarily by medical services (vs. surgical services) had a greater delay in time to surgical intervention (incidence rate ratio, 1.84), a longer length of stay (incidence rate ratio, 1.36), greater inpatient costs (incidence rate ratio, 1.38), and higher 30-day mortality and 30-day readmission rates (odds ratios, 1.92 and 1.13, respectively), Dr. Fleming said.
Based on these findings and on adjusted population-attributable risk estimates, management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion. In addition, 2,500 deaths and 30,000 readmissions could be avoided annually in the United States, he noted.
Patients with adhesive small-bowel obstruction are known to have high health care utilization. Many patients are admitted to hospitalists – perhaps because most patients are managed nonoperatively, but outcome comparisons between primary medical and surgical services have been limited to single-institution studies, Dr. Fleming said.
Historically, patients with adhesive SBO were managed by surgical services, but with current management strategies, the vast majority are successfully managed without surgery, and a shift over time has resulted in more patients receiving primary management by medical services, he explained.
The current study evaluated the impact of admission to primary medical vs. surgical services on health care utilization and outcomes for adhesive SBO using a population-based data set: the New York Statewide Planning and Research Cooperative System. The system was queried for unscheduled adhesive small bowl obstruction admissions from 2002 to 2013.
Even after adjustment for the older age and increased medical comorbidities of those managed by medical vs. surgical services, the findings demonstrated that outcomes are better with primary management by surgical services, he said, adding that “experience undoubtedly plays a role,” as surgical attendings admit a higher volume of adhesive SBO patients per year.
“We feel this data strongly supports the notion that small-bowel obstruction is a surgical disease and issue, and is best managed by surgeons. … Patients with adhesive small-bowel obstruction should be admitted to surgical service,” he said.
Further, while health care delivery is continually evolving and changing, changes in models of care like that seen over time in the surgical vs. medical service management of adhesive small-bowel obstruction should be studied prospectively before widespread adoption, he said.
Dr. Fleming reported having no relevant financial disclosures.
AT THE ASA ANNUAL MEETING
Key clinical point: Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggest.
Major finding: Management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion.
Data source: A population-based study of more than 107,600 hospital admissions
Disclosures: Dr. Fleming reported having no relevant financial disclosures.
ACOSOG Z0011: Good long-term results with SLND without ALND
CHICAGO – Sentinel lymph node dissection without axillary lymph node dissection offers excellent regional control in select patients with early metastatic breast cancer who are treated using breast-conserving therapy and adjuvant systemic therapy, according to 10-year results from the American College of Surgeons Oncology Group (ACOSOG) Z0011 Randomized Trial. ACOSOG is now part of Alliance for Clinical Trials in Oncology.
The findings confirm the previously reported 5-year outcomes, which demonstrated no significant difference in locoregional recurrence for patients with positive sentinel nodes who were randomized to undergo axillary lymph node dissection (ALND) or no further axillary treatment, Dr. Armando E. Giuliano of Cedars-Sinai Medical Center, Los Angeles, reported at the annual meeting of the American Surgical Association.
“In fact, the [5-year] results were highly significant showing noninferiority of sentinel lymph node dissection,” he said.
At a median follow-up of 9.25 years, there still was no statistically significant difference between 446 sentinel lymph node dissection (SLND)–only patients and 445 completion ALND patients with respect to the rate of locoregional recurrence, Dr. Giuliano said.
“The 10-year locoregional recurrence incidence after axillary lymph node dissection is 6.2%, compared to 5.3% after sentinel lymph node dissection alone,” he said, noting that most recurrences were seen in the first 5 years.
Of the ALND patients, 27% had additional positive nodes removed beyond the sentinel nodes.
“Therefore, about 27% of patients who underwent sentinel node dissection alone had residual disease remaining in the axilla undissected. Despite this high possibility of residual disease, very few regional recurrences were seen in either arm,” he noted.
Local recurrences occurred in 19 (5.6%) of patients in the ALND group and 12 (3.8%) in the SLND group, and regional recurrence was seen in 2 (0.5%) patients in the ALND group and 5 (1.5%) in the SLND group. The differences were not statistically significant.
Only hormone receptor status, Bloom-Richardson score, and tumor size were associated with locoregional recurrence. Omission of radiation increased local but not regional recurrence, but numbers were too few to draw further conclusions, he said.
“We can conclude, however, that sentinel lymph node dissection provides excellent locoregional control comparable to completion axillary lymph node dissection in these selected patients,” he said.
ACOSOG Z0011 subjects were patients with hematoxylin-eosin (H&E)–detected sentinel lymph node metastases undergoing breast-conserving therapy. The groups randomized to undergo ALND or to receive no further axillary treatment were similar with respect to age, Bloom-Richardson score, estrogen-receptor status, adjuvant systemic therapy, histology, and tumor size.
Nearly all patients had adjuvant systemic therapy (96% and 97% in the ALND and SLND groups, respectively), and about 60% in each group received chemotherapy.
Dr. Giuliano concluded that, despite the potential for residual axillary disease after SLND, SLND without ALND offers excellent regional control for selected patients with early metastatic breast cancer treated with breast-conserving therapy and adjuvant systemic therapy.
“Axillary lymph node dissection is not necessary for patients with early metastatic breast cancer and should be abandoned,” he said.
Dr. Giuliano had no disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review
CHICAGO – Sentinel lymph node dissection without axillary lymph node dissection offers excellent regional control in select patients with early metastatic breast cancer who are treated using breast-conserving therapy and adjuvant systemic therapy, according to 10-year results from the American College of Surgeons Oncology Group (ACOSOG) Z0011 Randomized Trial. ACOSOG is now part of Alliance for Clinical Trials in Oncology.
The findings confirm the previously reported 5-year outcomes, which demonstrated no significant difference in locoregional recurrence for patients with positive sentinel nodes who were randomized to undergo axillary lymph node dissection (ALND) or no further axillary treatment, Dr. Armando E. Giuliano of Cedars-Sinai Medical Center, Los Angeles, reported at the annual meeting of the American Surgical Association.
“In fact, the [5-year] results were highly significant showing noninferiority of sentinel lymph node dissection,” he said.
At a median follow-up of 9.25 years, there still was no statistically significant difference between 446 sentinel lymph node dissection (SLND)–only patients and 445 completion ALND patients with respect to the rate of locoregional recurrence, Dr. Giuliano said.
“The 10-year locoregional recurrence incidence after axillary lymph node dissection is 6.2%, compared to 5.3% after sentinel lymph node dissection alone,” he said, noting that most recurrences were seen in the first 5 years.
Of the ALND patients, 27% had additional positive nodes removed beyond the sentinel nodes.
“Therefore, about 27% of patients who underwent sentinel node dissection alone had residual disease remaining in the axilla undissected. Despite this high possibility of residual disease, very few regional recurrences were seen in either arm,” he noted.
Local recurrences occurred in 19 (5.6%) of patients in the ALND group and 12 (3.8%) in the SLND group, and regional recurrence was seen in 2 (0.5%) patients in the ALND group and 5 (1.5%) in the SLND group. The differences were not statistically significant.
Only hormone receptor status, Bloom-Richardson score, and tumor size were associated with locoregional recurrence. Omission of radiation increased local but not regional recurrence, but numbers were too few to draw further conclusions, he said.
“We can conclude, however, that sentinel lymph node dissection provides excellent locoregional control comparable to completion axillary lymph node dissection in these selected patients,” he said.
ACOSOG Z0011 subjects were patients with hematoxylin-eosin (H&E)–detected sentinel lymph node metastases undergoing breast-conserving therapy. The groups randomized to undergo ALND or to receive no further axillary treatment were similar with respect to age, Bloom-Richardson score, estrogen-receptor status, adjuvant systemic therapy, histology, and tumor size.
Nearly all patients had adjuvant systemic therapy (96% and 97% in the ALND and SLND groups, respectively), and about 60% in each group received chemotherapy.
Dr. Giuliano concluded that, despite the potential for residual axillary disease after SLND, SLND without ALND offers excellent regional control for selected patients with early metastatic breast cancer treated with breast-conserving therapy and adjuvant systemic therapy.
“Axillary lymph node dissection is not necessary for patients with early metastatic breast cancer and should be abandoned,” he said.
Dr. Giuliano had no disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review
CHICAGO – Sentinel lymph node dissection without axillary lymph node dissection offers excellent regional control in select patients with early metastatic breast cancer who are treated using breast-conserving therapy and adjuvant systemic therapy, according to 10-year results from the American College of Surgeons Oncology Group (ACOSOG) Z0011 Randomized Trial. ACOSOG is now part of Alliance for Clinical Trials in Oncology.
The findings confirm the previously reported 5-year outcomes, which demonstrated no significant difference in locoregional recurrence for patients with positive sentinel nodes who were randomized to undergo axillary lymph node dissection (ALND) or no further axillary treatment, Dr. Armando E. Giuliano of Cedars-Sinai Medical Center, Los Angeles, reported at the annual meeting of the American Surgical Association.
“In fact, the [5-year] results were highly significant showing noninferiority of sentinel lymph node dissection,” he said.
At a median follow-up of 9.25 years, there still was no statistically significant difference between 446 sentinel lymph node dissection (SLND)–only patients and 445 completion ALND patients with respect to the rate of locoregional recurrence, Dr. Giuliano said.
“The 10-year locoregional recurrence incidence after axillary lymph node dissection is 6.2%, compared to 5.3% after sentinel lymph node dissection alone,” he said, noting that most recurrences were seen in the first 5 years.
Of the ALND patients, 27% had additional positive nodes removed beyond the sentinel nodes.
“Therefore, about 27% of patients who underwent sentinel node dissection alone had residual disease remaining in the axilla undissected. Despite this high possibility of residual disease, very few regional recurrences were seen in either arm,” he noted.
Local recurrences occurred in 19 (5.6%) of patients in the ALND group and 12 (3.8%) in the SLND group, and regional recurrence was seen in 2 (0.5%) patients in the ALND group and 5 (1.5%) in the SLND group. The differences were not statistically significant.
Only hormone receptor status, Bloom-Richardson score, and tumor size were associated with locoregional recurrence. Omission of radiation increased local but not regional recurrence, but numbers were too few to draw further conclusions, he said.
“We can conclude, however, that sentinel lymph node dissection provides excellent locoregional control comparable to completion axillary lymph node dissection in these selected patients,” he said.
ACOSOG Z0011 subjects were patients with hematoxylin-eosin (H&E)–detected sentinel lymph node metastases undergoing breast-conserving therapy. The groups randomized to undergo ALND or to receive no further axillary treatment were similar with respect to age, Bloom-Richardson score, estrogen-receptor status, adjuvant systemic therapy, histology, and tumor size.
Nearly all patients had adjuvant systemic therapy (96% and 97% in the ALND and SLND groups, respectively), and about 60% in each group received chemotherapy.
Dr. Giuliano concluded that, despite the potential for residual axillary disease after SLND, SLND without ALND offers excellent regional control for selected patients with early metastatic breast cancer treated with breast-conserving therapy and adjuvant systemic therapy.
“Axillary lymph node dissection is not necessary for patients with early metastatic breast cancer and should be abandoned,” he said.
Dr. Giuliano had no disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review
AT THE ASA ANNUAL MEETING
Key clinical point: Sentinel lymph node dissection without axillary lymph node dissection offers excellent long-term regional control in select patients with early metastatic breast cancer who are treated using breast-conserving therapy and adjuvant systemic therapy.
Major finding: The 10-year locoregional recurrence after axillary lymph node dissection was 6.2%, compared with 5.3% after SLND alone.
Data source: The American College of Surgeons Oncology Group (ACOSOG) Z0011 Randomized Trial involving 891 patients.
Disclosures: Dr. Giuliano had no disclosures.
Thromboprophylaxis efficacy similar before and after colorectal surgery
CHICAGO – Lower extremity duplex scans should be performed prior to colorectal surgery, and anticoagulation should be tailored to the result, findings from a randomized clinical trial suggest.
The findings also raise questions about the fairness of financial penalties imposed by the Centers for Medicare & Medicaid Services for perioperative venous thromboembolism, Dr. Karen Zaghiyan of Cedars Sinai Medical Center, Los Angeles said at the annual meeting of the American Surgical Association.
In 376 consecutive adult patients undergoing laparoscopic or open major colorectal surgery who had no occult preoperative deep vein thrombosis (DVT) on lower extremity venous duplex scan and who were randomized to preoperative or postoperative chemical thromboprophylaxis (CTP) with 5,000 U of subcutaneous heparin, no differences were seen with respect to the primary outcome of venous thromboembolism within 48 hours of surgery, Dr. Zaghiyan said.
“There was no significant difference in our primary outcome – early postoperative VTE [venous thromboembolism] – in patients managed with postoperative or preoperative prophylaxis,” she said, noting that three patients in each group developed asymptomatic intraoperative DVT, and two additional patients in the postoperative treatment group developed asymptomatic DVT between postoperative day 0 and 2.
Two additional patients in the postoperative treatment group developed clinically significant DVT between postoperative day 2 and 30.
“Both patients had a complicated prolonged hospital course, and developed DVT while still hospitalized. This difference still did not reach statistical significance, and there were no post-discharge DVT or PEs [pulmonary embolisms] in the entire cohort,” she said.
Bleeding complications, including estimated blood loss and number receiving transfusion, were similar in the two groups, she said, noting that no patients developed heparin-induced thrombocytopenia, and that hospital stay, readmissions, and overall complications were similar between the two groups.
Study subjects had a mean age of 53 years, and 52% were women. The preoperative- and postoperative treatment groups were similar with respect to demographics and preoperative characteristics. They underwent lower extremity venous duplex just prior to surgery, immediately after surgery in the recovery room, on day 2 after surgery, and subsequently as clinically indicated.
Thromboprophylaxis in the preoperative treatment group was given in the “pre-op holding area” then 8 hours after surgery and every 8 hours thereafter until discharge. Thromboprophylaxis in the postoperative treatment group was given within 24 hours after surgery, and then every 8 hours until discharge.
Preoperative and postoperative CTP were equally safe and effective, and since occult preoperative DVT is twice as common as postoperative DVT, occurring in a surprising 4% of patients in this study, the findings support preoperative scans and anticoagulation based on the results – especially in older patients and those with comorbid disease, Dr. Zaghiyan said.
The findings could help improve patients care; although VTE prevention and chemical prophylaxis in colorectal surgery have been extensively studied, current guidelines are vague, with both the American College of Chest Physicians and the Surgical Care Improvement Project recommending that prophylaxis be initiated 24 hours prior to or after major colorectal surgery, she said.
The findings could also help avoid CMS penalties for postoperatively identified VTE,” she added.
Further, those penalties may not be supported by the clinical data; in this study, the majority of early postoperative DVTs were unpreventable, with no additional protection provided with preoperative prophylaxis, she explained.
“CMS should reevaluate the financial penalties, taking preventability into account,” she said.
Dr. Zaghiyan reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review.
CHICAGO – Lower extremity duplex scans should be performed prior to colorectal surgery, and anticoagulation should be tailored to the result, findings from a randomized clinical trial suggest.
The findings also raise questions about the fairness of financial penalties imposed by the Centers for Medicare & Medicaid Services for perioperative venous thromboembolism, Dr. Karen Zaghiyan of Cedars Sinai Medical Center, Los Angeles said at the annual meeting of the American Surgical Association.
In 376 consecutive adult patients undergoing laparoscopic or open major colorectal surgery who had no occult preoperative deep vein thrombosis (DVT) on lower extremity venous duplex scan and who were randomized to preoperative or postoperative chemical thromboprophylaxis (CTP) with 5,000 U of subcutaneous heparin, no differences were seen with respect to the primary outcome of venous thromboembolism within 48 hours of surgery, Dr. Zaghiyan said.
“There was no significant difference in our primary outcome – early postoperative VTE [venous thromboembolism] – in patients managed with postoperative or preoperative prophylaxis,” she said, noting that three patients in each group developed asymptomatic intraoperative DVT, and two additional patients in the postoperative treatment group developed asymptomatic DVT between postoperative day 0 and 2.
Two additional patients in the postoperative treatment group developed clinically significant DVT between postoperative day 2 and 30.
“Both patients had a complicated prolonged hospital course, and developed DVT while still hospitalized. This difference still did not reach statistical significance, and there were no post-discharge DVT or PEs [pulmonary embolisms] in the entire cohort,” she said.
Bleeding complications, including estimated blood loss and number receiving transfusion, were similar in the two groups, she said, noting that no patients developed heparin-induced thrombocytopenia, and that hospital stay, readmissions, and overall complications were similar between the two groups.
Study subjects had a mean age of 53 years, and 52% were women. The preoperative- and postoperative treatment groups were similar with respect to demographics and preoperative characteristics. They underwent lower extremity venous duplex just prior to surgery, immediately after surgery in the recovery room, on day 2 after surgery, and subsequently as clinically indicated.
Thromboprophylaxis in the preoperative treatment group was given in the “pre-op holding area” then 8 hours after surgery and every 8 hours thereafter until discharge. Thromboprophylaxis in the postoperative treatment group was given within 24 hours after surgery, and then every 8 hours until discharge.
Preoperative and postoperative CTP were equally safe and effective, and since occult preoperative DVT is twice as common as postoperative DVT, occurring in a surprising 4% of patients in this study, the findings support preoperative scans and anticoagulation based on the results – especially in older patients and those with comorbid disease, Dr. Zaghiyan said.
The findings could help improve patients care; although VTE prevention and chemical prophylaxis in colorectal surgery have been extensively studied, current guidelines are vague, with both the American College of Chest Physicians and the Surgical Care Improvement Project recommending that prophylaxis be initiated 24 hours prior to or after major colorectal surgery, she said.
The findings could also help avoid CMS penalties for postoperatively identified VTE,” she added.
Further, those penalties may not be supported by the clinical data; in this study, the majority of early postoperative DVTs were unpreventable, with no additional protection provided with preoperative prophylaxis, she explained.
“CMS should reevaluate the financial penalties, taking preventability into account,” she said.
Dr. Zaghiyan reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review.
CHICAGO – Lower extremity duplex scans should be performed prior to colorectal surgery, and anticoagulation should be tailored to the result, findings from a randomized clinical trial suggest.
The findings also raise questions about the fairness of financial penalties imposed by the Centers for Medicare & Medicaid Services for perioperative venous thromboembolism, Dr. Karen Zaghiyan of Cedars Sinai Medical Center, Los Angeles said at the annual meeting of the American Surgical Association.
In 376 consecutive adult patients undergoing laparoscopic or open major colorectal surgery who had no occult preoperative deep vein thrombosis (DVT) on lower extremity venous duplex scan and who were randomized to preoperative or postoperative chemical thromboprophylaxis (CTP) with 5,000 U of subcutaneous heparin, no differences were seen with respect to the primary outcome of venous thromboembolism within 48 hours of surgery, Dr. Zaghiyan said.
“There was no significant difference in our primary outcome – early postoperative VTE [venous thromboembolism] – in patients managed with postoperative or preoperative prophylaxis,” she said, noting that three patients in each group developed asymptomatic intraoperative DVT, and two additional patients in the postoperative treatment group developed asymptomatic DVT between postoperative day 0 and 2.
Two additional patients in the postoperative treatment group developed clinically significant DVT between postoperative day 2 and 30.
“Both patients had a complicated prolonged hospital course, and developed DVT while still hospitalized. This difference still did not reach statistical significance, and there were no post-discharge DVT or PEs [pulmonary embolisms] in the entire cohort,” she said.
Bleeding complications, including estimated blood loss and number receiving transfusion, were similar in the two groups, she said, noting that no patients developed heparin-induced thrombocytopenia, and that hospital stay, readmissions, and overall complications were similar between the two groups.
Study subjects had a mean age of 53 years, and 52% were women. The preoperative- and postoperative treatment groups were similar with respect to demographics and preoperative characteristics. They underwent lower extremity venous duplex just prior to surgery, immediately after surgery in the recovery room, on day 2 after surgery, and subsequently as clinically indicated.
Thromboprophylaxis in the preoperative treatment group was given in the “pre-op holding area” then 8 hours after surgery and every 8 hours thereafter until discharge. Thromboprophylaxis in the postoperative treatment group was given within 24 hours after surgery, and then every 8 hours until discharge.
Preoperative and postoperative CTP were equally safe and effective, and since occult preoperative DVT is twice as common as postoperative DVT, occurring in a surprising 4% of patients in this study, the findings support preoperative scans and anticoagulation based on the results – especially in older patients and those with comorbid disease, Dr. Zaghiyan said.
The findings could help improve patients care; although VTE prevention and chemical prophylaxis in colorectal surgery have been extensively studied, current guidelines are vague, with both the American College of Chest Physicians and the Surgical Care Improvement Project recommending that prophylaxis be initiated 24 hours prior to or after major colorectal surgery, she said.
The findings could also help avoid CMS penalties for postoperatively identified VTE,” she added.
Further, those penalties may not be supported by the clinical data; in this study, the majority of early postoperative DVTs were unpreventable, with no additional protection provided with preoperative prophylaxis, she explained.
“CMS should reevaluate the financial penalties, taking preventability into account,” she said.
Dr. Zaghiyan reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: Lower extremity duplex scans should be performed prior to colorectal surgery, and anticoagulation should be tailored to the result, findings from a randomized clinical trial suggest.
Major finding: No differences were seen with respect to the primary outcome of venous thromboembolism within 48 hours of surgery in patients treated with pre- or post-operative chemical thromboprophylaxis.
Data source: A randomized clinical trial of 376 patients.
Disclosures: Dr. Zaghiyan reported having no disclosures.