User login
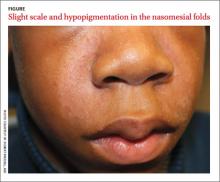
A 13-year-old African American male presented with a 2-year history of a mildly pruritic central facial rash (FIGURE) and dandruff. Recent treatment with hydrocortisone 1% cream and nystatin cream (100,000 U/gm) for 1 week resulted in no improvement.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Seborrheic dermatitis
Seborrheic dermatitis (SD) is a chronic dermatitis caused by Malassezia yeast species, including Malassezia (Pityrosporum ovale).1 SD affects 1% to 3% of the general population in the United States and has 2 incidence peaks: the first occurs during infancy and the second between 30 to 50 years of age.2 The abnormal response to the yeast organism leads to inflammation, proliferation, and desquamation.2
The diagnosis of SD is made based on the presence of sharply marginated scaled patches in areas with a high concentration of sebaceous glands including the scalp, eyebrows, and nasomesial folds. Pruritus, erythema, and greasy scales also are commonly seen.3 Raised lateral margins reminiscent of the advancing border of dermatophyte infections and postinflammatory hypopigmentation may also be present in African American patients. Both of these findings in the nasomesial folds, eyebrows, and scalp led to the diagnosis of SD in this patient.
Differential diagnosis includes psoriasis, lichen simplex chronicus
The differential for dandruff includes psoriasis, as well as lichen simplex chronicus and tinea capitis. Psoriasis often is associated with thicker, white micaceous scaling. The latter 2 conditions would not produce the symmetrical scaling in nasomesial folds that we saw with our patient.
SD in the central face can appear similar to pityriasis versicolor, allergic contact dermatitis, and irritant dermatitis (pityriasis alba), but these conditions are not associated with diffuse dandruff.
Antifungals are the mainstay of treatment
Because there is no cure for SD, the goal of therapy is to control the dermatitis. Topical antifungal agents are used to suppress the Malassezia yeast and topical steroids are used to suppress inflammation. Azole antifungal medications such as ketoconazole are effective and can be used for long periods of time with minimal risk of adverse effects3-5 (strength of recommendation [SOR]: C).
Our patient had used nystatin cream, which is effective against Candida yeast infections, but not especially effective for Malassezia sp.6
To reduce inflammation, mild topical steroids such as hydrocortisone cream 2.5% should be used. However, they must be used for short periods to avoid atrophy, telangiectasias, and steroid-induced acne. An alternative evolving treatment is to use a calcineurin inhibitor, such as pimecrolimus cream 1% or tacrolimus ointment 0.1%. These drugs do not exacerbate hypopigmentation, an effect that sometimes is attributed to topical steroids.7
Scalp treatments include shampoos such as ketoconazole 2%, selenium sulfide 2.5%, and ciclopirox 1%.3 Shampoos should be lathered up and left on the scalp for 3 to 5 minutes before rinsing.
Two forms of ketoconazole for our patient
Our patient responded well to ketoconazole cream 2% applied twice daily to the face and other areas without hair and ketoconazole 2% shampoo twice weekly. At a 6-week follow-up, the patient had significant improvement in scaling and pruritus on the central face and scalp. The associated facial hypopigmentation faded over 3 months.
CORRESPONDENCE
Robert T. Brodell MD, Division of Dermatology, University of Mississippi Medical Center, 2500 North State Street, Jackson, MS 39216; [email protected]
1. Nakabayashi A, Sei Y, Guillot J. Identification of Malassezia species isolated from patients with seborrhoeic dermatitis, atopic dermatitis, pityriasis versicolor and normal subjects. Med Mycology. 2000;38:337-341.
2. Sampaio AL, Mameri AC, Vargas TJ, et al. Seborrheic dermatitis. An Bras Dermatol. 2011;86:1061-1071;quiz 1072-1074.
3. Naldi L. Seborrhoeic dermatitis. Clin Evid (Online). 2010;2010:pii:1713.
4. Draelos ZD, Feldman SR, Butners V, et al. Long-term safety of ketoconazole foam, 2% in the treatment of seborrheic dermatitis: results of a phase IV, open-label study. J Drugs Dermatol. 2013;12:e1-e6.
5. Apasrawirote W, Udompataikul M, Rattanamongkolgul S. Topical antifungal agents for seborrheic dermatitis: systematic review and meta-analysis. J Med Assoc Thai. 2011;94:756-760.
6. Pedrosa AF, Lisboa, C, Rodrigues AG. Malassezia infections: A medical conundrum. J Am Acad Dermatol. 2014 Feb 22. Epub ahead of print.
7. High WA, Pandya AG. Pilot trial of 1% pimecrolimus cream in the treatment of seborrheic dermatitis in African American adults with associated hypopigmentation. J Am Acad Dermatol. 2006;54:1083-1088.
A 13-year-old African American male presented with a 2-year history of a mildly pruritic central facial rash (FIGURE) and dandruff. Recent treatment with hydrocortisone 1% cream and nystatin cream (100,000 U/gm) for 1 week resulted in no improvement.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Seborrheic dermatitis
Seborrheic dermatitis (SD) is a chronic dermatitis caused by Malassezia yeast species, including Malassezia (Pityrosporum ovale).1 SD affects 1% to 3% of the general population in the United States and has 2 incidence peaks: the first occurs during infancy and the second between 30 to 50 years of age.2 The abnormal response to the yeast organism leads to inflammation, proliferation, and desquamation.2
The diagnosis of SD is made based on the presence of sharply marginated scaled patches in areas with a high concentration of sebaceous glands including the scalp, eyebrows, and nasomesial folds. Pruritus, erythema, and greasy scales also are commonly seen.3 Raised lateral margins reminiscent of the advancing border of dermatophyte infections and postinflammatory hypopigmentation may also be present in African American patients. Both of these findings in the nasomesial folds, eyebrows, and scalp led to the diagnosis of SD in this patient.
Differential diagnosis includes psoriasis, lichen simplex chronicus
The differential for dandruff includes psoriasis, as well as lichen simplex chronicus and tinea capitis. Psoriasis often is associated with thicker, white micaceous scaling. The latter 2 conditions would not produce the symmetrical scaling in nasomesial folds that we saw with our patient.
SD in the central face can appear similar to pityriasis versicolor, allergic contact dermatitis, and irritant dermatitis (pityriasis alba), but these conditions are not associated with diffuse dandruff.
Antifungals are the mainstay of treatment
Because there is no cure for SD, the goal of therapy is to control the dermatitis. Topical antifungal agents are used to suppress the Malassezia yeast and topical steroids are used to suppress inflammation. Azole antifungal medications such as ketoconazole are effective and can be used for long periods of time with minimal risk of adverse effects3-5 (strength of recommendation [SOR]: C).
Our patient had used nystatin cream, which is effective against Candida yeast infections, but not especially effective for Malassezia sp.6
To reduce inflammation, mild topical steroids such as hydrocortisone cream 2.5% should be used. However, they must be used for short periods to avoid atrophy, telangiectasias, and steroid-induced acne. An alternative evolving treatment is to use a calcineurin inhibitor, such as pimecrolimus cream 1% or tacrolimus ointment 0.1%. These drugs do not exacerbate hypopigmentation, an effect that sometimes is attributed to topical steroids.7
Scalp treatments include shampoos such as ketoconazole 2%, selenium sulfide 2.5%, and ciclopirox 1%.3 Shampoos should be lathered up and left on the scalp for 3 to 5 minutes before rinsing.
Two forms of ketoconazole for our patient
Our patient responded well to ketoconazole cream 2% applied twice daily to the face and other areas without hair and ketoconazole 2% shampoo twice weekly. At a 6-week follow-up, the patient had significant improvement in scaling and pruritus on the central face and scalp. The associated facial hypopigmentation faded over 3 months.
CORRESPONDENCE
Robert T. Brodell MD, Division of Dermatology, University of Mississippi Medical Center, 2500 North State Street, Jackson, MS 39216; [email protected]
A 13-year-old African American male presented with a 2-year history of a mildly pruritic central facial rash (FIGURE) and dandruff. Recent treatment with hydrocortisone 1% cream and nystatin cream (100,000 U/gm) for 1 week resulted in no improvement.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Seborrheic dermatitis
Seborrheic dermatitis (SD) is a chronic dermatitis caused by Malassezia yeast species, including Malassezia (Pityrosporum ovale).1 SD affects 1% to 3% of the general population in the United States and has 2 incidence peaks: the first occurs during infancy and the second between 30 to 50 years of age.2 The abnormal response to the yeast organism leads to inflammation, proliferation, and desquamation.2
The diagnosis of SD is made based on the presence of sharply marginated scaled patches in areas with a high concentration of sebaceous glands including the scalp, eyebrows, and nasomesial folds. Pruritus, erythema, and greasy scales also are commonly seen.3 Raised lateral margins reminiscent of the advancing border of dermatophyte infections and postinflammatory hypopigmentation may also be present in African American patients. Both of these findings in the nasomesial folds, eyebrows, and scalp led to the diagnosis of SD in this patient.
Differential diagnosis includes psoriasis, lichen simplex chronicus
The differential for dandruff includes psoriasis, as well as lichen simplex chronicus and tinea capitis. Psoriasis often is associated with thicker, white micaceous scaling. The latter 2 conditions would not produce the symmetrical scaling in nasomesial folds that we saw with our patient.
SD in the central face can appear similar to pityriasis versicolor, allergic contact dermatitis, and irritant dermatitis (pityriasis alba), but these conditions are not associated with diffuse dandruff.
Antifungals are the mainstay of treatment
Because there is no cure for SD, the goal of therapy is to control the dermatitis. Topical antifungal agents are used to suppress the Malassezia yeast and topical steroids are used to suppress inflammation. Azole antifungal medications such as ketoconazole are effective and can be used for long periods of time with minimal risk of adverse effects3-5 (strength of recommendation [SOR]: C).
Our patient had used nystatin cream, which is effective against Candida yeast infections, but not especially effective for Malassezia sp.6
To reduce inflammation, mild topical steroids such as hydrocortisone cream 2.5% should be used. However, they must be used for short periods to avoid atrophy, telangiectasias, and steroid-induced acne. An alternative evolving treatment is to use a calcineurin inhibitor, such as pimecrolimus cream 1% or tacrolimus ointment 0.1%. These drugs do not exacerbate hypopigmentation, an effect that sometimes is attributed to topical steroids.7
Scalp treatments include shampoos such as ketoconazole 2%, selenium sulfide 2.5%, and ciclopirox 1%.3 Shampoos should be lathered up and left on the scalp for 3 to 5 minutes before rinsing.
Two forms of ketoconazole for our patient
Our patient responded well to ketoconazole cream 2% applied twice daily to the face and other areas without hair and ketoconazole 2% shampoo twice weekly. At a 6-week follow-up, the patient had significant improvement in scaling and pruritus on the central face and scalp. The associated facial hypopigmentation faded over 3 months.
CORRESPONDENCE
Robert T. Brodell MD, Division of Dermatology, University of Mississippi Medical Center, 2500 North State Street, Jackson, MS 39216; [email protected]
1. Nakabayashi A, Sei Y, Guillot J. Identification of Malassezia species isolated from patients with seborrhoeic dermatitis, atopic dermatitis, pityriasis versicolor and normal subjects. Med Mycology. 2000;38:337-341.
2. Sampaio AL, Mameri AC, Vargas TJ, et al. Seborrheic dermatitis. An Bras Dermatol. 2011;86:1061-1071;quiz 1072-1074.
3. Naldi L. Seborrhoeic dermatitis. Clin Evid (Online). 2010;2010:pii:1713.
4. Draelos ZD, Feldman SR, Butners V, et al. Long-term safety of ketoconazole foam, 2% in the treatment of seborrheic dermatitis: results of a phase IV, open-label study. J Drugs Dermatol. 2013;12:e1-e6.
5. Apasrawirote W, Udompataikul M, Rattanamongkolgul S. Topical antifungal agents for seborrheic dermatitis: systematic review and meta-analysis. J Med Assoc Thai. 2011;94:756-760.
6. Pedrosa AF, Lisboa, C, Rodrigues AG. Malassezia infections: A medical conundrum. J Am Acad Dermatol. 2014 Feb 22. Epub ahead of print.
7. High WA, Pandya AG. Pilot trial of 1% pimecrolimus cream in the treatment of seborrheic dermatitis in African American adults with associated hypopigmentation. J Am Acad Dermatol. 2006;54:1083-1088.
1. Nakabayashi A, Sei Y, Guillot J. Identification of Malassezia species isolated from patients with seborrhoeic dermatitis, atopic dermatitis, pityriasis versicolor and normal subjects. Med Mycology. 2000;38:337-341.
2. Sampaio AL, Mameri AC, Vargas TJ, et al. Seborrheic dermatitis. An Bras Dermatol. 2011;86:1061-1071;quiz 1072-1074.
3. Naldi L. Seborrhoeic dermatitis. Clin Evid (Online). 2010;2010:pii:1713.
4. Draelos ZD, Feldman SR, Butners V, et al. Long-term safety of ketoconazole foam, 2% in the treatment of seborrheic dermatitis: results of a phase IV, open-label study. J Drugs Dermatol. 2013;12:e1-e6.
5. Apasrawirote W, Udompataikul M, Rattanamongkolgul S. Topical antifungal agents for seborrheic dermatitis: systematic review and meta-analysis. J Med Assoc Thai. 2011;94:756-760.
6. Pedrosa AF, Lisboa, C, Rodrigues AG. Malassezia infections: A medical conundrum. J Am Acad Dermatol. 2014 Feb 22. Epub ahead of print.
7. High WA, Pandya AG. Pilot trial of 1% pimecrolimus cream in the treatment of seborrheic dermatitis in African American adults with associated hypopigmentation. J Am Acad Dermatol. 2006;54:1083-1088.