User login
Advanced-practice providers (APPs) continue to make their presence felt in the world of hospital medicine. According to survey data from the 2012 State of Hospital Medicine report, more than half (53.9%) of respondent groups serving adults have nurse practitioners (NP) and/or physician assistants (PA) integrated into their practices. The median ratio of APPs to hospitalist physicians in these groups has remained about the same as in previous surveys, with respondents reporting 0.2 FTE NPs per FTE physician, and 0.1 FTE PAs per FTE physician. We’ve also learned that APPs tend to be stable members of most hospitalist practices, with more than 70% of groups reporting no turnover among their APPs during the survey period.
Unfortunately, we don’t yet have much information on the specific roles APPs are filling in HM practices; hopefully, this will be a subject for the next State of Hospital Medicine survey, scheduled to launch in January 2014.
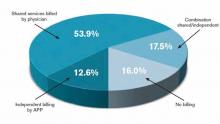
The 2012 survey did provide new information about how APP work is billed by HM groups. More than half the time, APP work is billed as a shared service under a physician’s provider number (see Table 1). Only on rare occasions is APP work billed separately under the APP’s provider number.
Perhaps most surprising of all, 16% of adult HM groups with APPs reported that their APPs don’t generally provide billable services, or no charges were submitted to payors for their services. This figure rose to 23% for hospital-employed groups.
Almost everywhere I go in my consulting work, we are asked about the value APPs can provide to hospitalist practice, and what their optimal roles are. I am extremely supportive of integrating APPs into hospitalist practice and believe they can play valuable roles supporting both excellent patient care and overall group efficiency.
But in my experience, many HM groups fail to execute well on this promise. As the survey results suggest, sometimes APPs are relegated to nonbillable tasks that could be performed by individuals at a lower skill level. Sometimes the hospitalists tend to think of the APPs as “free” help, and no real attempt is made to account for their contribution or capture their billable work. And some groups are so focused on ensuring they capture the 100% reimbursement available by billing under the physician’s name (rather than the 85% reimbursement typically available to APPs) that they lose sight of the fact that the extra physician time and effort involved might cost more than the incremental additional reimbursement received.
As a specialty, we still have a lot to learn about the optimal ways to deploy APPs to support high-quality, effective hospitalist practice. In the meantime, it can be valuable for HM groups to ensure that APPs are functioning in roles that take advantage of their advanced skills and licensure scope, and that efforts are being made to ensure the capture of all billable services provided.
I hope you will plan to participate in the 2014 State of Hospital Medicine survey and share your own practice’s experience with APPs.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
Advanced-practice providers (APPs) continue to make their presence felt in the world of hospital medicine. According to survey data from the 2012 State of Hospital Medicine report, more than half (53.9%) of respondent groups serving adults have nurse practitioners (NP) and/or physician assistants (PA) integrated into their practices. The median ratio of APPs to hospitalist physicians in these groups has remained about the same as in previous surveys, with respondents reporting 0.2 FTE NPs per FTE physician, and 0.1 FTE PAs per FTE physician. We’ve also learned that APPs tend to be stable members of most hospitalist practices, with more than 70% of groups reporting no turnover among their APPs during the survey period.
Unfortunately, we don’t yet have much information on the specific roles APPs are filling in HM practices; hopefully, this will be a subject for the next State of Hospital Medicine survey, scheduled to launch in January 2014.
The 2012 survey did provide new information about how APP work is billed by HM groups. More than half the time, APP work is billed as a shared service under a physician’s provider number (see Table 1). Only on rare occasions is APP work billed separately under the APP’s provider number.
Perhaps most surprising of all, 16% of adult HM groups with APPs reported that their APPs don’t generally provide billable services, or no charges were submitted to payors for their services. This figure rose to 23% for hospital-employed groups.
Almost everywhere I go in my consulting work, we are asked about the value APPs can provide to hospitalist practice, and what their optimal roles are. I am extremely supportive of integrating APPs into hospitalist practice and believe they can play valuable roles supporting both excellent patient care and overall group efficiency.
But in my experience, many HM groups fail to execute well on this promise. As the survey results suggest, sometimes APPs are relegated to nonbillable tasks that could be performed by individuals at a lower skill level. Sometimes the hospitalists tend to think of the APPs as “free” help, and no real attempt is made to account for their contribution or capture their billable work. And some groups are so focused on ensuring they capture the 100% reimbursement available by billing under the physician’s name (rather than the 85% reimbursement typically available to APPs) that they lose sight of the fact that the extra physician time and effort involved might cost more than the incremental additional reimbursement received.
As a specialty, we still have a lot to learn about the optimal ways to deploy APPs to support high-quality, effective hospitalist practice. In the meantime, it can be valuable for HM groups to ensure that APPs are functioning in roles that take advantage of their advanced skills and licensure scope, and that efforts are being made to ensure the capture of all billable services provided.
I hope you will plan to participate in the 2014 State of Hospital Medicine survey and share your own practice’s experience with APPs.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
Advanced-practice providers (APPs) continue to make their presence felt in the world of hospital medicine. According to survey data from the 2012 State of Hospital Medicine report, more than half (53.9%) of respondent groups serving adults have nurse practitioners (NP) and/or physician assistants (PA) integrated into their practices. The median ratio of APPs to hospitalist physicians in these groups has remained about the same as in previous surveys, with respondents reporting 0.2 FTE NPs per FTE physician, and 0.1 FTE PAs per FTE physician. We’ve also learned that APPs tend to be stable members of most hospitalist practices, with more than 70% of groups reporting no turnover among their APPs during the survey period.
Unfortunately, we don’t yet have much information on the specific roles APPs are filling in HM practices; hopefully, this will be a subject for the next State of Hospital Medicine survey, scheduled to launch in January 2014.
The 2012 survey did provide new information about how APP work is billed by HM groups. More than half the time, APP work is billed as a shared service under a physician’s provider number (see Table 1). Only on rare occasions is APP work billed separately under the APP’s provider number.
Perhaps most surprising of all, 16% of adult HM groups with APPs reported that their APPs don’t generally provide billable services, or no charges were submitted to payors for their services. This figure rose to 23% for hospital-employed groups.
Almost everywhere I go in my consulting work, we are asked about the value APPs can provide to hospitalist practice, and what their optimal roles are. I am extremely supportive of integrating APPs into hospitalist practice and believe they can play valuable roles supporting both excellent patient care and overall group efficiency.
But in my experience, many HM groups fail to execute well on this promise. As the survey results suggest, sometimes APPs are relegated to nonbillable tasks that could be performed by individuals at a lower skill level. Sometimes the hospitalists tend to think of the APPs as “free” help, and no real attempt is made to account for their contribution or capture their billable work. And some groups are so focused on ensuring they capture the 100% reimbursement available by billing under the physician’s name (rather than the 85% reimbursement typically available to APPs) that they lose sight of the fact that the extra physician time and effort involved might cost more than the incremental additional reimbursement received.
As a specialty, we still have a lot to learn about the optimal ways to deploy APPs to support high-quality, effective hospitalist practice. In the meantime, it can be valuable for HM groups to ensure that APPs are functioning in roles that take advantage of their advanced skills and licensure scope, and that efforts are being made to ensure the capture of all billable services provided.
I hope you will plan to participate in the 2014 State of Hospital Medicine survey and share your own practice’s experience with APPs.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.