User login
New State of Hospital Medicine Report Better Than Ever
For the last six months or so, not a week has gone by in which someone hasn’t asked me when the new SHM survey report will be released. The anticipation level is high, and rightly so. This will be the first new look at hospitalist practice characteristics in two years, and boy, have they been an eventful two years!
On behalf of SHM and the SHM Practice Analysis Committee (PAC), I’m thrilled to introduce SHM’s 2014 State of Hospital Medicine Report (SOHM) and the resumption of the monthly “Survey Insights” article written by PAC members. Here are a few key things you should know about the new SOHM report:
- The content is more wide-ranging than ever. SHM leaves the collection of hospitalist compensation and productivity data to the Medical Group Management Association—SHM licenses compensation and production data from MGMA and has incorporated it into the new SOHM report—but covers just about every other aspect of hospitalist group structure and operations imaginable. In addition to traditional questions regarding scope of services, staffing and scheduling models, and financial support, this year’s report includes new information about hospitalist back-up staffing plans, how academic hospitalist time is allocated, accountable care organization participation, electronic health record use, and the presence of other hospital-focused practice specialties.

—Leslie Flores, MHA
- The number of survey participants is larger than ever. This year SHM received eligible responses from 499 different hospitalist groups, an increase of about 7% over 2012. Respondents continue to represent all employer/ownership models and geographic regions, in roughly similar proportions to previous surveys. And we continue to get good participation by both academic and nonacademic hospital medicine groups. This means we have more—and more reliable—information than ever for different subgroups of hospitalists.
- The report is more accessible and easier to read than it has ever been. This year SHM has produced the SOHM report in full color, with professional layout and graphics; it’s a pleasure to read compared to previous versions. And, for the first time, SHM is making available a web-based version of the full report, so that you can refer to it anywhere and at any time.
As a consultant, I refer to my copy of the SOHM report almost every day and find it indispensable as a source of context when offering advice to my clients. And I’m always interested to see the diverse ways in which hospitalist groups across the country use survey information to make decisions about how to run their practices and to explain their environments to hospital leaders and other stakeholders.
I encourage you to obtain a copy of the SOHM report and review it carefully; you’ll almost certainly find more than one interesting and useful tidbit of information. Use the report to assess how your practice compares to your peers, but always keep in mind that surveys don’t tell you what should be—they only tell you what currently is. New best practices not reflected in survey data are emerging all the time, and the ways others do things won’t always be right for your group’s unique situation and needs. Whether you are partners or employees, you and your colleagues “own” the success of your practice and are the best judges of what is right for you.
Leslie Flores is a PAC member and partner of Nelson Flores Hospital Medicine Consultants.
For the last six months or so, not a week has gone by in which someone hasn’t asked me when the new SHM survey report will be released. The anticipation level is high, and rightly so. This will be the first new look at hospitalist practice characteristics in two years, and boy, have they been an eventful two years!
On behalf of SHM and the SHM Practice Analysis Committee (PAC), I’m thrilled to introduce SHM’s 2014 State of Hospital Medicine Report (SOHM) and the resumption of the monthly “Survey Insights” article written by PAC members. Here are a few key things you should know about the new SOHM report:
- The content is more wide-ranging than ever. SHM leaves the collection of hospitalist compensation and productivity data to the Medical Group Management Association—SHM licenses compensation and production data from MGMA and has incorporated it into the new SOHM report—but covers just about every other aspect of hospitalist group structure and operations imaginable. In addition to traditional questions regarding scope of services, staffing and scheduling models, and financial support, this year’s report includes new information about hospitalist back-up staffing plans, how academic hospitalist time is allocated, accountable care organization participation, electronic health record use, and the presence of other hospital-focused practice specialties.

—Leslie Flores, MHA
- The number of survey participants is larger than ever. This year SHM received eligible responses from 499 different hospitalist groups, an increase of about 7% over 2012. Respondents continue to represent all employer/ownership models and geographic regions, in roughly similar proportions to previous surveys. And we continue to get good participation by both academic and nonacademic hospital medicine groups. This means we have more—and more reliable—information than ever for different subgroups of hospitalists.
- The report is more accessible and easier to read than it has ever been. This year SHM has produced the SOHM report in full color, with professional layout and graphics; it’s a pleasure to read compared to previous versions. And, for the first time, SHM is making available a web-based version of the full report, so that you can refer to it anywhere and at any time.
As a consultant, I refer to my copy of the SOHM report almost every day and find it indispensable as a source of context when offering advice to my clients. And I’m always interested to see the diverse ways in which hospitalist groups across the country use survey information to make decisions about how to run their practices and to explain their environments to hospital leaders and other stakeholders.
I encourage you to obtain a copy of the SOHM report and review it carefully; you’ll almost certainly find more than one interesting and useful tidbit of information. Use the report to assess how your practice compares to your peers, but always keep in mind that surveys don’t tell you what should be—they only tell you what currently is. New best practices not reflected in survey data are emerging all the time, and the ways others do things won’t always be right for your group’s unique situation and needs. Whether you are partners or employees, you and your colleagues “own” the success of your practice and are the best judges of what is right for you.
Leslie Flores is a PAC member and partner of Nelson Flores Hospital Medicine Consultants.
For the last six months or so, not a week has gone by in which someone hasn’t asked me when the new SHM survey report will be released. The anticipation level is high, and rightly so. This will be the first new look at hospitalist practice characteristics in two years, and boy, have they been an eventful two years!
On behalf of SHM and the SHM Practice Analysis Committee (PAC), I’m thrilled to introduce SHM’s 2014 State of Hospital Medicine Report (SOHM) and the resumption of the monthly “Survey Insights” article written by PAC members. Here are a few key things you should know about the new SOHM report:
- The content is more wide-ranging than ever. SHM leaves the collection of hospitalist compensation and productivity data to the Medical Group Management Association—SHM licenses compensation and production data from MGMA and has incorporated it into the new SOHM report—but covers just about every other aspect of hospitalist group structure and operations imaginable. In addition to traditional questions regarding scope of services, staffing and scheduling models, and financial support, this year’s report includes new information about hospitalist back-up staffing plans, how academic hospitalist time is allocated, accountable care organization participation, electronic health record use, and the presence of other hospital-focused practice specialties.

—Leslie Flores, MHA
- The number of survey participants is larger than ever. This year SHM received eligible responses from 499 different hospitalist groups, an increase of about 7% over 2012. Respondents continue to represent all employer/ownership models and geographic regions, in roughly similar proportions to previous surveys. And we continue to get good participation by both academic and nonacademic hospital medicine groups. This means we have more—and more reliable—information than ever for different subgroups of hospitalists.
- The report is more accessible and easier to read than it has ever been. This year SHM has produced the SOHM report in full color, with professional layout and graphics; it’s a pleasure to read compared to previous versions. And, for the first time, SHM is making available a web-based version of the full report, so that you can refer to it anywhere and at any time.
As a consultant, I refer to my copy of the SOHM report almost every day and find it indispensable as a source of context when offering advice to my clients. And I’m always interested to see the diverse ways in which hospitalist groups across the country use survey information to make decisions about how to run their practices and to explain their environments to hospital leaders and other stakeholders.
I encourage you to obtain a copy of the SOHM report and review it carefully; you’ll almost certainly find more than one interesting and useful tidbit of information. Use the report to assess how your practice compares to your peers, but always keep in mind that surveys don’t tell you what should be—they only tell you what currently is. New best practices not reflected in survey data are emerging all the time, and the ways others do things won’t always be right for your group’s unique situation and needs. Whether you are partners or employees, you and your colleagues “own” the success of your practice and are the best judges of what is right for you.
Leslie Flores is a PAC member and partner of Nelson Flores Hospital Medicine Consultants.
Principles and Characteristics of an HMG
With the continuing growth of the specialty of hospital medicine, the capabilities and performance of hospital medicine groups (HMGs) varies significantly. There are few guidelines that HMGs can reference as tools to guide self‐improvement. To address this deficiency, the Society of Hospital Medicine (SHM) Board of Directors authorized a process to identify the key principles and characteristics of an effective HMG.
METHODS
Topic Development and Validation Prework
In providing direction to this effort, the SHM board felt that the principles and characteristics should be directed at both hospitals and hospitalists, addressing the full range of managerial, organizational, clinical, and quality activities necessary to achieve effectiveness. Furthermore, the board defined effectiveness as consisting of 2 components. First, the HMG must assure that the patients managed by hospitalists receive high‐quality care that is sensitive to their needs and preferences. Second, the HMG must understand that the central role of the hospitalist is to coordinate patient care and foster interdisciplinary communication across the care continuum to provide optimal patient outcomes.
The SHM board appointed an HMG Characteristics Workgroup consisting of individuals who have experience with a wide array of HMG models and who could offer expert opinions on the subject. The HMG Characteristics Workgroup felt it important to review the work of other organizations that develop and administer criteria, standards, and/or requirements for healthcare organizations. Examples cited were the American College of Surgeons[1]; The Joint Commission[2]; American Nurse Credentialing Center[3]; the National Committee for Quality Assurance[4]; the American Medical Group Association[5]; and the American Association of Critical‐Care Nurses.[6]
In March 2012 and April 2012, SHM staff reviewed the websites and published materials of these organizations. For each program, information was captured on the qualifications of applicants, history of the program, timing of administering the program, the nature of recognition granted, and the program's keys to success. The summary of these findings was shared with the workgroup.
Background research and the broad scope of characteristics to be addressed led to the workgroup's decision to develop the principles and characteristics using a consensus process, emphasizing expert opinion supplemented by feedback from a broad group of stakeholders.
Initial Draft
During April 2012 and May 2012, the HMG Characteristics Workgroup identified 3 domains for the key characteristics: (1) program structure and operations, (2) clinical care delivery, and (3) organizational performance improvement. Over the course of several meetings, the HMG Characteristics Workgroup developed an initial draft of 83 characteristics, grouped into 29 subgroups within the 3 domains.
From June 2012 to November 2012, this initial draft was reviewed by a broad cross section of the hospital medicine community including members of SHM's committees, a group of academic hospitalists, focus groups in 2 communities (Philadelphia and Boston), and the leaders of several regional and national hospitalist management companies. Quantitative and qualitative feedback was obtained.
In November 2012, the SHM Board of Directors held its annual leadership meeting, attended by approximately 25 national hospitalist thought leaders and chairpersons of SHM committees. At this meeting, a series of exercises were conducted in which these leaders of the hospital medicine movement, including the SHM board members, were each assigned individual characteristics and asked to review and edit them for clarity and appropriateness.
As a result of feedback at that meeting and subsequent discussion by the SHM board, the workgroup was asked to modify the characteristics in 3 ways. First, the list should be streamlined, reducing the number of characteristics. Second, the 3 domains should be eliminated, and a better organizing framework should be created. Third, additional context should be added to the list of characteristics.
Second Draft
During the period from November 2012 to December 2012, the HMG Characteristics Workgroup went through a 2‐step Delphi process to consolidate characteristics and/or eliminate characteristics that were redundant or unnecessary. In the first step, members of the workgroup rated each characteristic from 1 to 3. A rating of 1 meant not important; good quality, but not required for an effective HMG. A rating of 2 meant important; most effective HMGs will meet requirement. A rating of 3 meant highly important; mandatory for an effective HMG. In the second step, members of the workgroup received feedback on the scores for each characteristic and came to a consensus on which characteristics should be eliminated or merged with other characteristics.
As a result, the number of characteristics was reduced and consolidated from 83 to 47, and a new framing structure was defined, replacing the 3 domains with 10 organizing principles. Finally, a rationale for each characteristic was added, defending its inclusion in the list. In addition, consideration was given to including a section describing how an HMG could demonstrate that their organization met each characteristic. However, the workgroup and the board decided that these demonstration requirements should be vetted before they were published.
From January 2013 to June 2013, the revised key principles and characteristics were reviewed by selected chairpersons of SHM committees and by 2 focus groups of HMG leaders. These reviews were conducted at the SHM Annual Meeting. Finally, in June 2013, the Committee on Clinical Leadership of the American Hospital Association reviewed and commented on the draft of the principles and characteristics.
In addition, based on feedback received from the reviewers, the wording of many of the characteristics went through revisions to assure precision and clarity. Before submission to the Journal of Hospital Medicine, a professional editor was engaged to assure that the format and language of the characteristics were clear and consistent.
Final Approval
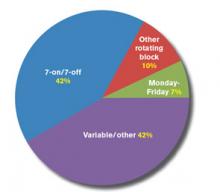
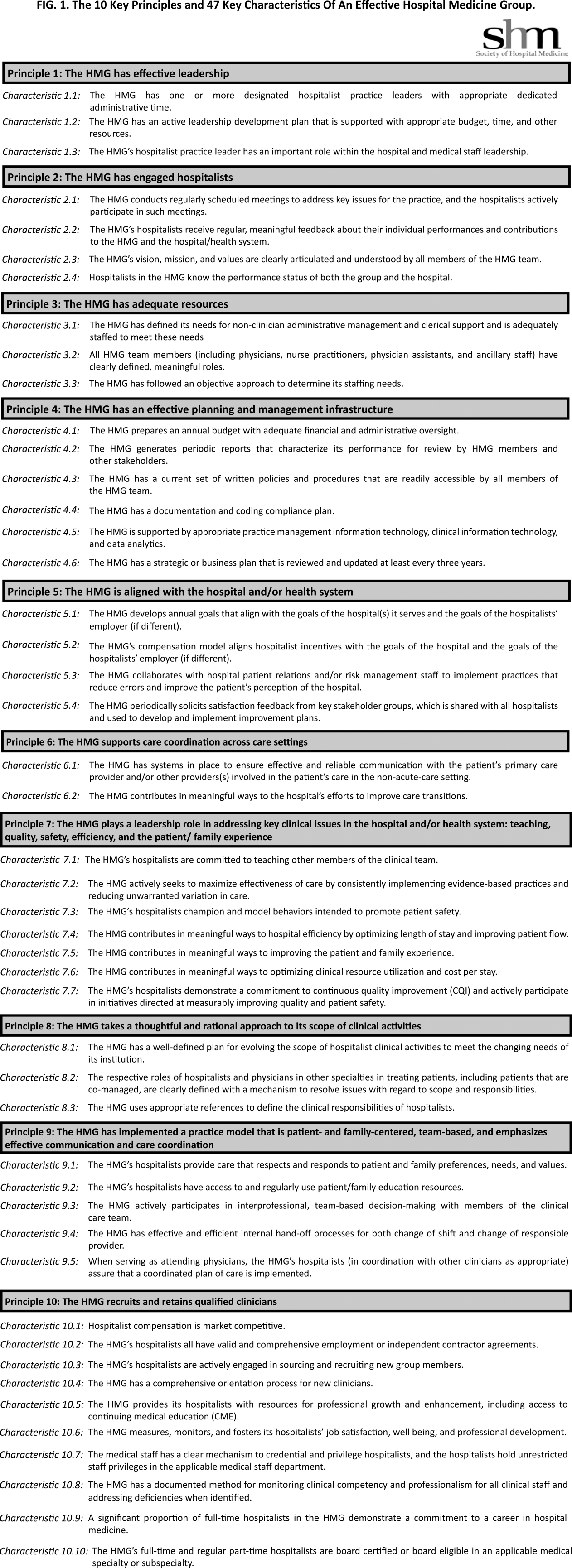
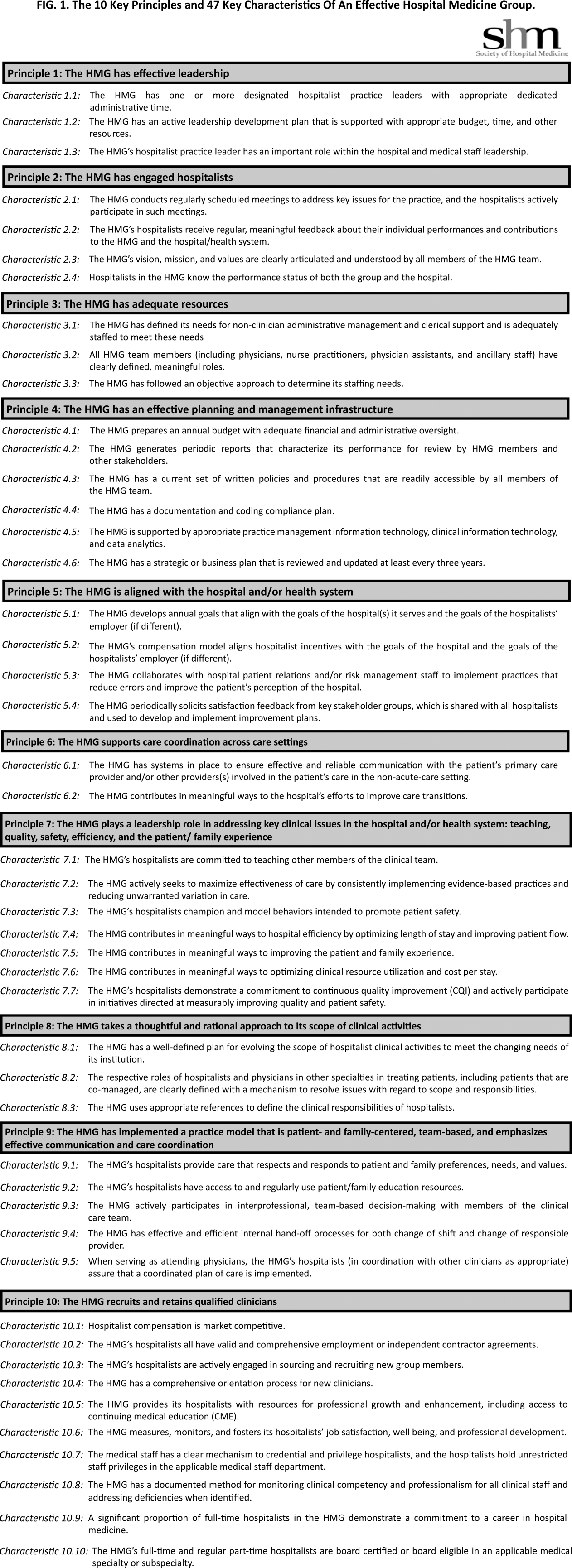
The final draft of the 10 principles and 47 characteristics was approved for publication at a meeting of the SHM Board of Directors in September 2013 (Figure 1).
RESULTS
A recurring issue that the workgroup addressed was the applicability of the characteristics from 1 practice setting to another. Confounding factors include the HMG's employment/organizational model (eg, hospital employed, academic, multispecialty group, private practice, and management company), its population served (eg, adult vs pediatric, more than 1 hospital), and the type of hospital served (eg, academic vs community, the hospital has more than 1 HMG). The workgroup has made an effort to assure that all 47 characteristics can be applied to every type of HMG.
In developing the 10 principles, the workgroup attempted to construct a list of the basic ingredients needed to build and sustain an effective HMG. These 10 principles stand on their own, independent of the 47 key characteristics, and include issues such as effective leadership, clinician engagement, adequate resources, management infrastructure, key hospitalist roles and responsibilities, alignment with the hospital, and the recruitment and retention of qualified hospitalists.
A more detailed version of the Key Principles and Characteristics of an Effective HMG is available in the online version of this article (see Supporting Information, Appendix, in the online version of this article). The online Appendix includes the rationales for each of the characteristics, guidance on how to provide feedback to the SHM on the framework, and the SHM's plan for further development of the key principles and characteristics.
DISCUSSION
To address the variability in capabilities and performance of HMGs, these principles and characteristics are designed to provide a framework for HMGs seeking to conduct self‐assessments and develop pathways for improvement.
Although there may be HMG arrangements that do not directly involve the hospital and its executive team, and therefore alternative approaches may make sense, for most HMGs hospitals are directly involved with the HMG as either an employer or a contractor. For that reason, the Key Principles and Characteristics of an Effective HMG is written for 2 audiences: the executive leadership of the hospital (most specifically the chief medical officer or a similar role) and the hospitalists in the HMG (most specifically the practice medical director). To address the key characteristics requires the active participation of both parties. For the hospital executives, the framework establishes expectations for the HMG. For the hospitalists, the framework provides guidance in the development of an improvement plan.
Hospital executives and hospitalists can use the key characteristics in a broad spectrum of ways. The easiest and least formalized approach would be to use the framework as the basis of an ongoing dialogue between the hospital leadership and the HMG. A more formal approach would be to use the framework to guide the planning and budgeting activities of the HMG. Finally, a hospital or health system can use the key principles and characteristics as a way to evaluate their affiliated HMG(s)for example, the HMG must address 80% of the 47 characteristics.
The Key Principles and Characteristics of an Effective HMG should be considered akin to the Core Competencies in Hospital Medicine previously published in the Journal of Hospital Medicine.[7] However, instead of focusing on the competencies of individual physicians, this framework focuses on the characteristics of hospitalist groups. Just as a physician or other healthcare provider is not expected to demonstrate competency for every element in the core competencies document, an HMG does not need to have all 47 characteristics to be effective. Effective hospitalists may have skills other than those listed in the Core Competencies in Hospital Medicine. Similarly, the 47 characteristics do not represent an exhaustive list of every desirable HMG attribute. In general, effective HMGs should possess most of the characteristics.
In applying the framework, the HMG should not simply attempt to evaluate each characteristic with a yes or no assessment. For HMGs responding yes, there may be a wide range of performancefrom meeting the bare minimum requirements to employing sophisticated, expansive measures to excel in the characteristic.
SHM encourages hospital leaders and HMG leaders to use these characteristics to perform an HMG self‐assessment and to develop a plan. The plan could address implementation of selected characteristics that are not currently being addressed by the HMG or the development of additional behaviors, tools, resources, and capabilities that more fully incorporate those characteristics for which the HMG meets only minimum requirements. In addition, the plan could address the impact that a larger organization (eg, health system, hospital, or employer) may have on a given characteristic.
As outlined above, the process used to develop the Key Principles and Characteristics of an Effective HMG was grounded in expert opinion and extensive review and feedback. HMGs that use the framework should recognize that others might have a different opinion. For example, characteristic 5.2 states, The HMG's compensation model aligns hospitalist incentives with the goals of the hospital and the goals of the hospitalist's employer (if different). There are likely to be experienced hospitalist leaders who believe that an effective HMG does not need to have an incentive compensation system. However, the consensus process employed to develop the key characteristics led to the conclusion that an effective HMG should have an incentive compensation system.
The publication of the Key Principles and Characteristics of an Effective HMG may lead to negative and/or unintended consequences. A self‐assessment by an HMG using this framework could require a significant level of effort on behalf of the HMG, whereas implementing remedial efforts to address the characteristics could require an investment of time and money that could take away from other important issues facing the HMG. Many HMGs may be held accountable for addressing these characteristics without the necessary financial support from their hospital or medical group. Finally, the publication of the document could create a backlash from members of the hospitalist community who do not think that the SHM should be in the business of defining what characterizes an effective HMG, rather that this definition should be left to the marketplace.
Despite these concerns, the leadership of the SHM expects that the publication of the Key Principles and Characteristics of an Effective HMG will lead to overall improvement in the capabilities and performance of HMGs.
CONCLUSIONS
The Key Principles and Characteristics of an Effective HMG have been designed to be aspirational, helping to raise the bar for the specialty of hospital medicine. These principles and characteristics could provide a framework for HMGs seeking to conduct self‐assessments, outlining a pathway for improvement, and better defining the central role of hospitalists in coordinating team‐based, patient‐centered care in the acute care setting.
Acknowledgments
Disclosures: Patrick Cawley, MD: none; Steven Deitelzweig, MD: none; Leslie Flores, MHA: provides consulting to hospital medicine groups; Joseph A. Miller, MS: none; John Nelson, MD: provides consulting to hospital medicine groups; Scott Rissmiller, MD: none; Laurence Wellikson, MD: none; Winthrop F. Whitcomb, MD: provides consulting to hospital medicine groups.
- American College of Surgeons. New verification site visit outcomes. Available at: http://www.facs.org/trauma/verifivisitoutcomes.html. Accessed September 3, 2013.
- Hospital accreditation standards 2012. Oakbrook Terrace, IL: The Joint Commission; 2012. Available at: Amazon.com: http://www.amazon.com/Hospital‐Accreditation‐Standards‐Joint‐Commission/dp/1599404257
- The magnet model: components and sources of evidence. Silver Spring, MD: American Nurse Credentialing Center; 2011. Available at: Amazon.com: http://www.amazon.com/Magnet‐Model‐Components‐Sources‐Evidence/dp/1935213229.
- Patient Centered Medical Home Standards and Guidelines. National Committee for Quality Assurance. Available at: https://inetshop01.pub.ncqa.org/Publications/deptCate.asp?dept_id=21(suppl 1):2–95.
With the continuing growth of the specialty of hospital medicine, the capabilities and performance of hospital medicine groups (HMGs) varies significantly. There are few guidelines that HMGs can reference as tools to guide self‐improvement. To address this deficiency, the Society of Hospital Medicine (SHM) Board of Directors authorized a process to identify the key principles and characteristics of an effective HMG.
METHODS
Topic Development and Validation Prework
In providing direction to this effort, the SHM board felt that the principles and characteristics should be directed at both hospitals and hospitalists, addressing the full range of managerial, organizational, clinical, and quality activities necessary to achieve effectiveness. Furthermore, the board defined effectiveness as consisting of 2 components. First, the HMG must assure that the patients managed by hospitalists receive high‐quality care that is sensitive to their needs and preferences. Second, the HMG must understand that the central role of the hospitalist is to coordinate patient care and foster interdisciplinary communication across the care continuum to provide optimal patient outcomes.
The SHM board appointed an HMG Characteristics Workgroup consisting of individuals who have experience with a wide array of HMG models and who could offer expert opinions on the subject. The HMG Characteristics Workgroup felt it important to review the work of other organizations that develop and administer criteria, standards, and/or requirements for healthcare organizations. Examples cited were the American College of Surgeons[1]; The Joint Commission[2]; American Nurse Credentialing Center[3]; the National Committee for Quality Assurance[4]; the American Medical Group Association[5]; and the American Association of Critical‐Care Nurses.[6]
In March 2012 and April 2012, SHM staff reviewed the websites and published materials of these organizations. For each program, information was captured on the qualifications of applicants, history of the program, timing of administering the program, the nature of recognition granted, and the program's keys to success. The summary of these findings was shared with the workgroup.
Background research and the broad scope of characteristics to be addressed led to the workgroup's decision to develop the principles and characteristics using a consensus process, emphasizing expert opinion supplemented by feedback from a broad group of stakeholders.
Initial Draft
During April 2012 and May 2012, the HMG Characteristics Workgroup identified 3 domains for the key characteristics: (1) program structure and operations, (2) clinical care delivery, and (3) organizational performance improvement. Over the course of several meetings, the HMG Characteristics Workgroup developed an initial draft of 83 characteristics, grouped into 29 subgroups within the 3 domains.
From June 2012 to November 2012, this initial draft was reviewed by a broad cross section of the hospital medicine community including members of SHM's committees, a group of academic hospitalists, focus groups in 2 communities (Philadelphia and Boston), and the leaders of several regional and national hospitalist management companies. Quantitative and qualitative feedback was obtained.
In November 2012, the SHM Board of Directors held its annual leadership meeting, attended by approximately 25 national hospitalist thought leaders and chairpersons of SHM committees. At this meeting, a series of exercises were conducted in which these leaders of the hospital medicine movement, including the SHM board members, were each assigned individual characteristics and asked to review and edit them for clarity and appropriateness.
As a result of feedback at that meeting and subsequent discussion by the SHM board, the workgroup was asked to modify the characteristics in 3 ways. First, the list should be streamlined, reducing the number of characteristics. Second, the 3 domains should be eliminated, and a better organizing framework should be created. Third, additional context should be added to the list of characteristics.
Second Draft
During the period from November 2012 to December 2012, the HMG Characteristics Workgroup went through a 2‐step Delphi process to consolidate characteristics and/or eliminate characteristics that were redundant or unnecessary. In the first step, members of the workgroup rated each characteristic from 1 to 3. A rating of 1 meant not important; good quality, but not required for an effective HMG. A rating of 2 meant important; most effective HMGs will meet requirement. A rating of 3 meant highly important; mandatory for an effective HMG. In the second step, members of the workgroup received feedback on the scores for each characteristic and came to a consensus on which characteristics should be eliminated or merged with other characteristics.
As a result, the number of characteristics was reduced and consolidated from 83 to 47, and a new framing structure was defined, replacing the 3 domains with 10 organizing principles. Finally, a rationale for each characteristic was added, defending its inclusion in the list. In addition, consideration was given to including a section describing how an HMG could demonstrate that their organization met each characteristic. However, the workgroup and the board decided that these demonstration requirements should be vetted before they were published.
From January 2013 to June 2013, the revised key principles and characteristics were reviewed by selected chairpersons of SHM committees and by 2 focus groups of HMG leaders. These reviews were conducted at the SHM Annual Meeting. Finally, in June 2013, the Committee on Clinical Leadership of the American Hospital Association reviewed and commented on the draft of the principles and characteristics.
In addition, based on feedback received from the reviewers, the wording of many of the characteristics went through revisions to assure precision and clarity. Before submission to the Journal of Hospital Medicine, a professional editor was engaged to assure that the format and language of the characteristics were clear and consistent.
Final Approval
The final draft of the 10 principles and 47 characteristics was approved for publication at a meeting of the SHM Board of Directors in September 2013 (Figure 1).
RESULTS
A recurring issue that the workgroup addressed was the applicability of the characteristics from 1 practice setting to another. Confounding factors include the HMG's employment/organizational model (eg, hospital employed, academic, multispecialty group, private practice, and management company), its population served (eg, adult vs pediatric, more than 1 hospital), and the type of hospital served (eg, academic vs community, the hospital has more than 1 HMG). The workgroup has made an effort to assure that all 47 characteristics can be applied to every type of HMG.
In developing the 10 principles, the workgroup attempted to construct a list of the basic ingredients needed to build and sustain an effective HMG. These 10 principles stand on their own, independent of the 47 key characteristics, and include issues such as effective leadership, clinician engagement, adequate resources, management infrastructure, key hospitalist roles and responsibilities, alignment with the hospital, and the recruitment and retention of qualified hospitalists.
A more detailed version of the Key Principles and Characteristics of an Effective HMG is available in the online version of this article (see Supporting Information, Appendix, in the online version of this article). The online Appendix includes the rationales for each of the characteristics, guidance on how to provide feedback to the SHM on the framework, and the SHM's plan for further development of the key principles and characteristics.
DISCUSSION
To address the variability in capabilities and performance of HMGs, these principles and characteristics are designed to provide a framework for HMGs seeking to conduct self‐assessments and develop pathways for improvement.
Although there may be HMG arrangements that do not directly involve the hospital and its executive team, and therefore alternative approaches may make sense, for most HMGs hospitals are directly involved with the HMG as either an employer or a contractor. For that reason, the Key Principles and Characteristics of an Effective HMG is written for 2 audiences: the executive leadership of the hospital (most specifically the chief medical officer or a similar role) and the hospitalists in the HMG (most specifically the practice medical director). To address the key characteristics requires the active participation of both parties. For the hospital executives, the framework establishes expectations for the HMG. For the hospitalists, the framework provides guidance in the development of an improvement plan.
Hospital executives and hospitalists can use the key characteristics in a broad spectrum of ways. The easiest and least formalized approach would be to use the framework as the basis of an ongoing dialogue between the hospital leadership and the HMG. A more formal approach would be to use the framework to guide the planning and budgeting activities of the HMG. Finally, a hospital or health system can use the key principles and characteristics as a way to evaluate their affiliated HMG(s)for example, the HMG must address 80% of the 47 characteristics.
The Key Principles and Characteristics of an Effective HMG should be considered akin to the Core Competencies in Hospital Medicine previously published in the Journal of Hospital Medicine.[7] However, instead of focusing on the competencies of individual physicians, this framework focuses on the characteristics of hospitalist groups. Just as a physician or other healthcare provider is not expected to demonstrate competency for every element in the core competencies document, an HMG does not need to have all 47 characteristics to be effective. Effective hospitalists may have skills other than those listed in the Core Competencies in Hospital Medicine. Similarly, the 47 characteristics do not represent an exhaustive list of every desirable HMG attribute. In general, effective HMGs should possess most of the characteristics.
In applying the framework, the HMG should not simply attempt to evaluate each characteristic with a yes or no assessment. For HMGs responding yes, there may be a wide range of performancefrom meeting the bare minimum requirements to employing sophisticated, expansive measures to excel in the characteristic.
SHM encourages hospital leaders and HMG leaders to use these characteristics to perform an HMG self‐assessment and to develop a plan. The plan could address implementation of selected characteristics that are not currently being addressed by the HMG or the development of additional behaviors, tools, resources, and capabilities that more fully incorporate those characteristics for which the HMG meets only minimum requirements. In addition, the plan could address the impact that a larger organization (eg, health system, hospital, or employer) may have on a given characteristic.
As outlined above, the process used to develop the Key Principles and Characteristics of an Effective HMG was grounded in expert opinion and extensive review and feedback. HMGs that use the framework should recognize that others might have a different opinion. For example, characteristic 5.2 states, The HMG's compensation model aligns hospitalist incentives with the goals of the hospital and the goals of the hospitalist's employer (if different). There are likely to be experienced hospitalist leaders who believe that an effective HMG does not need to have an incentive compensation system. However, the consensus process employed to develop the key characteristics led to the conclusion that an effective HMG should have an incentive compensation system.
The publication of the Key Principles and Characteristics of an Effective HMG may lead to negative and/or unintended consequences. A self‐assessment by an HMG using this framework could require a significant level of effort on behalf of the HMG, whereas implementing remedial efforts to address the characteristics could require an investment of time and money that could take away from other important issues facing the HMG. Many HMGs may be held accountable for addressing these characteristics without the necessary financial support from their hospital or medical group. Finally, the publication of the document could create a backlash from members of the hospitalist community who do not think that the SHM should be in the business of defining what characterizes an effective HMG, rather that this definition should be left to the marketplace.
Despite these concerns, the leadership of the SHM expects that the publication of the Key Principles and Characteristics of an Effective HMG will lead to overall improvement in the capabilities and performance of HMGs.
CONCLUSIONS
The Key Principles and Characteristics of an Effective HMG have been designed to be aspirational, helping to raise the bar for the specialty of hospital medicine. These principles and characteristics could provide a framework for HMGs seeking to conduct self‐assessments, outlining a pathway for improvement, and better defining the central role of hospitalists in coordinating team‐based, patient‐centered care in the acute care setting.
Acknowledgments
Disclosures: Patrick Cawley, MD: none; Steven Deitelzweig, MD: none; Leslie Flores, MHA: provides consulting to hospital medicine groups; Joseph A. Miller, MS: none; John Nelson, MD: provides consulting to hospital medicine groups; Scott Rissmiller, MD: none; Laurence Wellikson, MD: none; Winthrop F. Whitcomb, MD: provides consulting to hospital medicine groups.
With the continuing growth of the specialty of hospital medicine, the capabilities and performance of hospital medicine groups (HMGs) varies significantly. There are few guidelines that HMGs can reference as tools to guide self‐improvement. To address this deficiency, the Society of Hospital Medicine (SHM) Board of Directors authorized a process to identify the key principles and characteristics of an effective HMG.
METHODS
Topic Development and Validation Prework
In providing direction to this effort, the SHM board felt that the principles and characteristics should be directed at both hospitals and hospitalists, addressing the full range of managerial, organizational, clinical, and quality activities necessary to achieve effectiveness. Furthermore, the board defined effectiveness as consisting of 2 components. First, the HMG must assure that the patients managed by hospitalists receive high‐quality care that is sensitive to their needs and preferences. Second, the HMG must understand that the central role of the hospitalist is to coordinate patient care and foster interdisciplinary communication across the care continuum to provide optimal patient outcomes.
The SHM board appointed an HMG Characteristics Workgroup consisting of individuals who have experience with a wide array of HMG models and who could offer expert opinions on the subject. The HMG Characteristics Workgroup felt it important to review the work of other organizations that develop and administer criteria, standards, and/or requirements for healthcare organizations. Examples cited were the American College of Surgeons[1]; The Joint Commission[2]; American Nurse Credentialing Center[3]; the National Committee for Quality Assurance[4]; the American Medical Group Association[5]; and the American Association of Critical‐Care Nurses.[6]
In March 2012 and April 2012, SHM staff reviewed the websites and published materials of these organizations. For each program, information was captured on the qualifications of applicants, history of the program, timing of administering the program, the nature of recognition granted, and the program's keys to success. The summary of these findings was shared with the workgroup.
Background research and the broad scope of characteristics to be addressed led to the workgroup's decision to develop the principles and characteristics using a consensus process, emphasizing expert opinion supplemented by feedback from a broad group of stakeholders.
Initial Draft
During April 2012 and May 2012, the HMG Characteristics Workgroup identified 3 domains for the key characteristics: (1) program structure and operations, (2) clinical care delivery, and (3) organizational performance improvement. Over the course of several meetings, the HMG Characteristics Workgroup developed an initial draft of 83 characteristics, grouped into 29 subgroups within the 3 domains.
From June 2012 to November 2012, this initial draft was reviewed by a broad cross section of the hospital medicine community including members of SHM's committees, a group of academic hospitalists, focus groups in 2 communities (Philadelphia and Boston), and the leaders of several regional and national hospitalist management companies. Quantitative and qualitative feedback was obtained.
In November 2012, the SHM Board of Directors held its annual leadership meeting, attended by approximately 25 national hospitalist thought leaders and chairpersons of SHM committees. At this meeting, a series of exercises were conducted in which these leaders of the hospital medicine movement, including the SHM board members, were each assigned individual characteristics and asked to review and edit them for clarity and appropriateness.
As a result of feedback at that meeting and subsequent discussion by the SHM board, the workgroup was asked to modify the characteristics in 3 ways. First, the list should be streamlined, reducing the number of characteristics. Second, the 3 domains should be eliminated, and a better organizing framework should be created. Third, additional context should be added to the list of characteristics.
Second Draft
During the period from November 2012 to December 2012, the HMG Characteristics Workgroup went through a 2‐step Delphi process to consolidate characteristics and/or eliminate characteristics that were redundant or unnecessary. In the first step, members of the workgroup rated each characteristic from 1 to 3. A rating of 1 meant not important; good quality, but not required for an effective HMG. A rating of 2 meant important; most effective HMGs will meet requirement. A rating of 3 meant highly important; mandatory for an effective HMG. In the second step, members of the workgroup received feedback on the scores for each characteristic and came to a consensus on which characteristics should be eliminated or merged with other characteristics.
As a result, the number of characteristics was reduced and consolidated from 83 to 47, and a new framing structure was defined, replacing the 3 domains with 10 organizing principles. Finally, a rationale for each characteristic was added, defending its inclusion in the list. In addition, consideration was given to including a section describing how an HMG could demonstrate that their organization met each characteristic. However, the workgroup and the board decided that these demonstration requirements should be vetted before they were published.
From January 2013 to June 2013, the revised key principles and characteristics were reviewed by selected chairpersons of SHM committees and by 2 focus groups of HMG leaders. These reviews were conducted at the SHM Annual Meeting. Finally, in June 2013, the Committee on Clinical Leadership of the American Hospital Association reviewed and commented on the draft of the principles and characteristics.
In addition, based on feedback received from the reviewers, the wording of many of the characteristics went through revisions to assure precision and clarity. Before submission to the Journal of Hospital Medicine, a professional editor was engaged to assure that the format and language of the characteristics were clear and consistent.
Final Approval
The final draft of the 10 principles and 47 characteristics was approved for publication at a meeting of the SHM Board of Directors in September 2013 (Figure 1).
RESULTS
A recurring issue that the workgroup addressed was the applicability of the characteristics from 1 practice setting to another. Confounding factors include the HMG's employment/organizational model (eg, hospital employed, academic, multispecialty group, private practice, and management company), its population served (eg, adult vs pediatric, more than 1 hospital), and the type of hospital served (eg, academic vs community, the hospital has more than 1 HMG). The workgroup has made an effort to assure that all 47 characteristics can be applied to every type of HMG.
In developing the 10 principles, the workgroup attempted to construct a list of the basic ingredients needed to build and sustain an effective HMG. These 10 principles stand on their own, independent of the 47 key characteristics, and include issues such as effective leadership, clinician engagement, adequate resources, management infrastructure, key hospitalist roles and responsibilities, alignment with the hospital, and the recruitment and retention of qualified hospitalists.
A more detailed version of the Key Principles and Characteristics of an Effective HMG is available in the online version of this article (see Supporting Information, Appendix, in the online version of this article). The online Appendix includes the rationales for each of the characteristics, guidance on how to provide feedback to the SHM on the framework, and the SHM's plan for further development of the key principles and characteristics.
DISCUSSION
To address the variability in capabilities and performance of HMGs, these principles and characteristics are designed to provide a framework for HMGs seeking to conduct self‐assessments and develop pathways for improvement.
Although there may be HMG arrangements that do not directly involve the hospital and its executive team, and therefore alternative approaches may make sense, for most HMGs hospitals are directly involved with the HMG as either an employer or a contractor. For that reason, the Key Principles and Characteristics of an Effective HMG is written for 2 audiences: the executive leadership of the hospital (most specifically the chief medical officer or a similar role) and the hospitalists in the HMG (most specifically the practice medical director). To address the key characteristics requires the active participation of both parties. For the hospital executives, the framework establishes expectations for the HMG. For the hospitalists, the framework provides guidance in the development of an improvement plan.
Hospital executives and hospitalists can use the key characteristics in a broad spectrum of ways. The easiest and least formalized approach would be to use the framework as the basis of an ongoing dialogue between the hospital leadership and the HMG. A more formal approach would be to use the framework to guide the planning and budgeting activities of the HMG. Finally, a hospital or health system can use the key principles and characteristics as a way to evaluate their affiliated HMG(s)for example, the HMG must address 80% of the 47 characteristics.
The Key Principles and Characteristics of an Effective HMG should be considered akin to the Core Competencies in Hospital Medicine previously published in the Journal of Hospital Medicine.[7] However, instead of focusing on the competencies of individual physicians, this framework focuses on the characteristics of hospitalist groups. Just as a physician or other healthcare provider is not expected to demonstrate competency for every element in the core competencies document, an HMG does not need to have all 47 characteristics to be effective. Effective hospitalists may have skills other than those listed in the Core Competencies in Hospital Medicine. Similarly, the 47 characteristics do not represent an exhaustive list of every desirable HMG attribute. In general, effective HMGs should possess most of the characteristics.
In applying the framework, the HMG should not simply attempt to evaluate each characteristic with a yes or no assessment. For HMGs responding yes, there may be a wide range of performancefrom meeting the bare minimum requirements to employing sophisticated, expansive measures to excel in the characteristic.
SHM encourages hospital leaders and HMG leaders to use these characteristics to perform an HMG self‐assessment and to develop a plan. The plan could address implementation of selected characteristics that are not currently being addressed by the HMG or the development of additional behaviors, tools, resources, and capabilities that more fully incorporate those characteristics for which the HMG meets only minimum requirements. In addition, the plan could address the impact that a larger organization (eg, health system, hospital, or employer) may have on a given characteristic.
As outlined above, the process used to develop the Key Principles and Characteristics of an Effective HMG was grounded in expert opinion and extensive review and feedback. HMGs that use the framework should recognize that others might have a different opinion. For example, characteristic 5.2 states, The HMG's compensation model aligns hospitalist incentives with the goals of the hospital and the goals of the hospitalist's employer (if different). There are likely to be experienced hospitalist leaders who believe that an effective HMG does not need to have an incentive compensation system. However, the consensus process employed to develop the key characteristics led to the conclusion that an effective HMG should have an incentive compensation system.
The publication of the Key Principles and Characteristics of an Effective HMG may lead to negative and/or unintended consequences. A self‐assessment by an HMG using this framework could require a significant level of effort on behalf of the HMG, whereas implementing remedial efforts to address the characteristics could require an investment of time and money that could take away from other important issues facing the HMG. Many HMGs may be held accountable for addressing these characteristics without the necessary financial support from their hospital or medical group. Finally, the publication of the document could create a backlash from members of the hospitalist community who do not think that the SHM should be in the business of defining what characterizes an effective HMG, rather that this definition should be left to the marketplace.
Despite these concerns, the leadership of the SHM expects that the publication of the Key Principles and Characteristics of an Effective HMG will lead to overall improvement in the capabilities and performance of HMGs.
CONCLUSIONS
The Key Principles and Characteristics of an Effective HMG have been designed to be aspirational, helping to raise the bar for the specialty of hospital medicine. These principles and characteristics could provide a framework for HMGs seeking to conduct self‐assessments, outlining a pathway for improvement, and better defining the central role of hospitalists in coordinating team‐based, patient‐centered care in the acute care setting.
Acknowledgments
Disclosures: Patrick Cawley, MD: none; Steven Deitelzweig, MD: none; Leslie Flores, MHA: provides consulting to hospital medicine groups; Joseph A. Miller, MS: none; John Nelson, MD: provides consulting to hospital medicine groups; Scott Rissmiller, MD: none; Laurence Wellikson, MD: none; Winthrop F. Whitcomb, MD: provides consulting to hospital medicine groups.
- American College of Surgeons. New verification site visit outcomes. Available at: http://www.facs.org/trauma/verifivisitoutcomes.html. Accessed September 3, 2013.
- Hospital accreditation standards 2012. Oakbrook Terrace, IL: The Joint Commission; 2012. Available at: Amazon.com: http://www.amazon.com/Hospital‐Accreditation‐Standards‐Joint‐Commission/dp/1599404257
- The magnet model: components and sources of evidence. Silver Spring, MD: American Nurse Credentialing Center; 2011. Available at: Amazon.com: http://www.amazon.com/Magnet‐Model‐Components‐Sources‐Evidence/dp/1935213229.
- Patient Centered Medical Home Standards and Guidelines. National Committee for Quality Assurance. Available at: https://inetshop01.pub.ncqa.org/Publications/deptCate.asp?dept_id=21(suppl 1):2–95.
- American College of Surgeons. New verification site visit outcomes. Available at: http://www.facs.org/trauma/verifivisitoutcomes.html. Accessed September 3, 2013.
- Hospital accreditation standards 2012. Oakbrook Terrace, IL: The Joint Commission; 2012. Available at: Amazon.com: http://www.amazon.com/Hospital‐Accreditation‐Standards‐Joint‐Commission/dp/1599404257
- The magnet model: components and sources of evidence. Silver Spring, MD: American Nurse Credentialing Center; 2011. Available at: Amazon.com: http://www.amazon.com/Magnet‐Model‐Components‐Sources‐Evidence/dp/1935213229.
- Patient Centered Medical Home Standards and Guidelines. National Committee for Quality Assurance. Available at: https://inetshop01.pub.ncqa.org/Publications/deptCate.asp?dept_id=21(suppl 1):2–95.
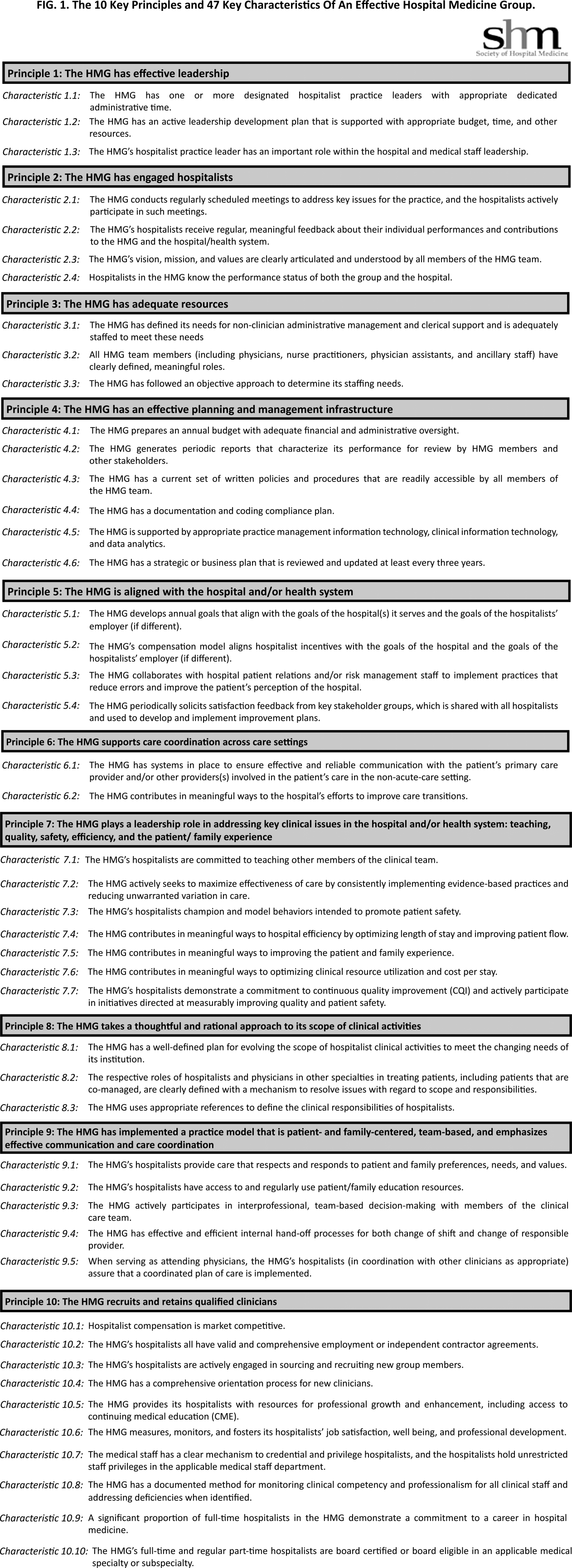
Advanced-Practice Providers Have More to Offer Hospital Medicine Groups
Advanced-practice providers (APPs) continue to make their presence felt in the world of hospital medicine. According to survey data from the 2012 State of Hospital Medicine report, more than half (53.9%) of respondent groups serving adults have nurse practitioners (NP) and/or physician assistants (PA) integrated into their practices. The median ratio of APPs to hospitalist physicians in these groups has remained about the same as in previous surveys, with respondents reporting 0.2 FTE NPs per FTE physician, and 0.1 FTE PAs per FTE physician. We’ve also learned that APPs tend to be stable members of most hospitalist practices, with more than 70% of groups reporting no turnover among their APPs during the survey period.
Unfortunately, we don’t yet have much information on the specific roles APPs are filling in HM practices; hopefully, this will be a subject for the next State of Hospital Medicine survey, scheduled to launch in January 2014.
The 2012 survey did provide new information about how APP work is billed by HM groups. More than half the time, APP work is billed as a shared service under a physician’s provider number (see Table 1). Only on rare occasions is APP work billed separately under the APP’s provider number.
Perhaps most surprising of all, 16% of adult HM groups with APPs reported that their APPs don’t generally provide billable services, or no charges were submitted to payors for their services. This figure rose to 23% for hospital-employed groups.
Almost everywhere I go in my consulting work, we are asked about the value APPs can provide to hospitalist practice, and what their optimal roles are. I am extremely supportive of integrating APPs into hospitalist practice and believe they can play valuable roles supporting both excellent patient care and overall group efficiency.
But in my experience, many HM groups fail to execute well on this promise. As the survey results suggest, sometimes APPs are relegated to nonbillable tasks that could be performed by individuals at a lower skill level. Sometimes the hospitalists tend to think of the APPs as “free” help, and no real attempt is made to account for their contribution or capture their billable work. And some groups are so focused on ensuring they capture the 100% reimbursement available by billing under the physician’s name (rather than the 85% reimbursement typically available to APPs) that they lose sight of the fact that the extra physician time and effort involved might cost more than the incremental additional reimbursement received.
As a specialty, we still have a lot to learn about the optimal ways to deploy APPs to support high-quality, effective hospitalist practice. In the meantime, it can be valuable for HM groups to ensure that APPs are functioning in roles that take advantage of their advanced skills and licensure scope, and that efforts are being made to ensure the capture of all billable services provided.
I hope you will plan to participate in the 2014 State of Hospital Medicine survey and share your own practice’s experience with APPs.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
Advanced-practice providers (APPs) continue to make their presence felt in the world of hospital medicine. According to survey data from the 2012 State of Hospital Medicine report, more than half (53.9%) of respondent groups serving adults have nurse practitioners (NP) and/or physician assistants (PA) integrated into their practices. The median ratio of APPs to hospitalist physicians in these groups has remained about the same as in previous surveys, with respondents reporting 0.2 FTE NPs per FTE physician, and 0.1 FTE PAs per FTE physician. We’ve also learned that APPs tend to be stable members of most hospitalist practices, with more than 70% of groups reporting no turnover among their APPs during the survey period.
Unfortunately, we don’t yet have much information on the specific roles APPs are filling in HM practices; hopefully, this will be a subject for the next State of Hospital Medicine survey, scheduled to launch in January 2014.
The 2012 survey did provide new information about how APP work is billed by HM groups. More than half the time, APP work is billed as a shared service under a physician’s provider number (see Table 1). Only on rare occasions is APP work billed separately under the APP’s provider number.
Perhaps most surprising of all, 16% of adult HM groups with APPs reported that their APPs don’t generally provide billable services, or no charges were submitted to payors for their services. This figure rose to 23% for hospital-employed groups.
Almost everywhere I go in my consulting work, we are asked about the value APPs can provide to hospitalist practice, and what their optimal roles are. I am extremely supportive of integrating APPs into hospitalist practice and believe they can play valuable roles supporting both excellent patient care and overall group efficiency.
But in my experience, many HM groups fail to execute well on this promise. As the survey results suggest, sometimes APPs are relegated to nonbillable tasks that could be performed by individuals at a lower skill level. Sometimes the hospitalists tend to think of the APPs as “free” help, and no real attempt is made to account for their contribution or capture their billable work. And some groups are so focused on ensuring they capture the 100% reimbursement available by billing under the physician’s name (rather than the 85% reimbursement typically available to APPs) that they lose sight of the fact that the extra physician time and effort involved might cost more than the incremental additional reimbursement received.
As a specialty, we still have a lot to learn about the optimal ways to deploy APPs to support high-quality, effective hospitalist practice. In the meantime, it can be valuable for HM groups to ensure that APPs are functioning in roles that take advantage of their advanced skills and licensure scope, and that efforts are being made to ensure the capture of all billable services provided.
I hope you will plan to participate in the 2014 State of Hospital Medicine survey and share your own practice’s experience with APPs.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
Advanced-practice providers (APPs) continue to make their presence felt in the world of hospital medicine. According to survey data from the 2012 State of Hospital Medicine report, more than half (53.9%) of respondent groups serving adults have nurse practitioners (NP) and/or physician assistants (PA) integrated into their practices. The median ratio of APPs to hospitalist physicians in these groups has remained about the same as in previous surveys, with respondents reporting 0.2 FTE NPs per FTE physician, and 0.1 FTE PAs per FTE physician. We’ve also learned that APPs tend to be stable members of most hospitalist practices, with more than 70% of groups reporting no turnover among their APPs during the survey period.
Unfortunately, we don’t yet have much information on the specific roles APPs are filling in HM practices; hopefully, this will be a subject for the next State of Hospital Medicine survey, scheduled to launch in January 2014.
The 2012 survey did provide new information about how APP work is billed by HM groups. More than half the time, APP work is billed as a shared service under a physician’s provider number (see Table 1). Only on rare occasions is APP work billed separately under the APP’s provider number.
Perhaps most surprising of all, 16% of adult HM groups with APPs reported that their APPs don’t generally provide billable services, or no charges were submitted to payors for their services. This figure rose to 23% for hospital-employed groups.
Almost everywhere I go in my consulting work, we are asked about the value APPs can provide to hospitalist practice, and what their optimal roles are. I am extremely supportive of integrating APPs into hospitalist practice and believe they can play valuable roles supporting both excellent patient care and overall group efficiency.
But in my experience, many HM groups fail to execute well on this promise. As the survey results suggest, sometimes APPs are relegated to nonbillable tasks that could be performed by individuals at a lower skill level. Sometimes the hospitalists tend to think of the APPs as “free” help, and no real attempt is made to account for their contribution or capture their billable work. And some groups are so focused on ensuring they capture the 100% reimbursement available by billing under the physician’s name (rather than the 85% reimbursement typically available to APPs) that they lose sight of the fact that the extra physician time and effort involved might cost more than the incremental additional reimbursement received.
As a specialty, we still have a lot to learn about the optimal ways to deploy APPs to support high-quality, effective hospitalist practice. In the meantime, it can be valuable for HM groups to ensure that APPs are functioning in roles that take advantage of their advanced skills and licensure scope, and that efforts are being made to ensure the capture of all billable services provided.
I hope you will plan to participate in the 2014 State of Hospital Medicine survey and share your own practice’s experience with APPs.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
Survey Shows Five-Year Decrease in Employee Benefits, Paid Time Off for Hospitalists
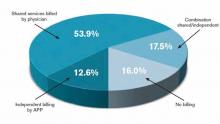
For the first time in several years, SHM included questions about employee benefits and paid time off in its 2012 State of Hospital Medicine survey. The median value of benefits per physician FTE reported by HM groups serving adults only was $26,000, according to the 2012 survey. But what a surprise it was when survey respondents in 2007 reported median benefits of $31,900.
I admit to being flummoxed by the decrease. The definition of “benefits” was identical in both surveys. The only difference is that in 2007, SHM collected actual benefit cost for each individual on the individual questionnaire; in 2012, we asked for the average benefits per FTE for the group. One possible explanation is that some respondents simply guessed about the average, because they didn’t have to report data for individual doctors. Of course, it’s also possible that groups are requiring physicians to pay a higher proportion of insurance premiums or are reducing retirement plan contributions due to the weak economy. But in the work I do with hospitalist groups around the country, I rarely see benefit costs below about $35,000.
Source: 2012 State of Hospital Medicine report
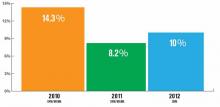
Another interesting finding from the 2012 survey is that 37% of adult medicine groups reported offering paid time off (PTO), down from 54% in 2007. Even among groups using a seven-on/seven-off schedule, the PTO rate was only 44%. Does this represent a survey design or respondent input error, differences in respondent populations, or an actual shift in the prevalence of PTO benefits? I suspect it’s the latter, because the median amount of PTO time awarded has also declined. In 2007, adult HMGs reported a median of 25 PTO days annually. In 2012, the median for those groups offering PTO was 160 hours of PTO, which represents somewhere around 13 to 20 days, depending on shift length.
Why might PTO benefits be declining? I suppose it could be belt-tightening associated with the poor economy. But I think many HM groups simply have found PTO benefits difficult to administer and fraught with unintended consequences. Many groups are so thinly staffed that for someone to take a PTO day, someone else must work extra to cover. Then, when the covering doctor takes PTO, the first doctor must work extra—effectively offsetting the value of PTO. And if a hospitalist takes PTO and also works extra shifts in the same pay period, do these two offset each other? Or does the doctor get paid for both the PTO days and the extra shift days?
For clinicians such as hospitalists, whose work is defined in highly variable, shift-based schedules that include a lot of night and weekend work, it becomes very difficult to determine which of the days not worked were PTO days versus just days the doctor wasn’t scheduled.
Personally, I don’t think it makes much sense for most hospitalists to have PTO. Don’t get me wrong—I think hospitalists should be paid well and have generous amounts of time off in exchange for long, challenging workdays and a disproportionate amount of night and weekend work. But arbitrarily assigning some of the days not worked as PTO while others are just unscheduled days seems unnecessarily complex.
Time will tell if the specialty as a whole agrees with me or not.
Leslie Flores is a principal in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
For the first time in several years, SHM included questions about employee benefits and paid time off in its 2012 State of Hospital Medicine survey. The median value of benefits per physician FTE reported by HM groups serving adults only was $26,000, according to the 2012 survey. But what a surprise it was when survey respondents in 2007 reported median benefits of $31,900.
I admit to being flummoxed by the decrease. The definition of “benefits” was identical in both surveys. The only difference is that in 2007, SHM collected actual benefit cost for each individual on the individual questionnaire; in 2012, we asked for the average benefits per FTE for the group. One possible explanation is that some respondents simply guessed about the average, because they didn’t have to report data for individual doctors. Of course, it’s also possible that groups are requiring physicians to pay a higher proportion of insurance premiums or are reducing retirement plan contributions due to the weak economy. But in the work I do with hospitalist groups around the country, I rarely see benefit costs below about $35,000.
Source: 2012 State of Hospital Medicine report
Another interesting finding from the 2012 survey is that 37% of adult medicine groups reported offering paid time off (PTO), down from 54% in 2007. Even among groups using a seven-on/seven-off schedule, the PTO rate was only 44%. Does this represent a survey design or respondent input error, differences in respondent populations, or an actual shift in the prevalence of PTO benefits? I suspect it’s the latter, because the median amount of PTO time awarded has also declined. In 2007, adult HMGs reported a median of 25 PTO days annually. In 2012, the median for those groups offering PTO was 160 hours of PTO, which represents somewhere around 13 to 20 days, depending on shift length.
Why might PTO benefits be declining? I suppose it could be belt-tightening associated with the poor economy. But I think many HM groups simply have found PTO benefits difficult to administer and fraught with unintended consequences. Many groups are so thinly staffed that for someone to take a PTO day, someone else must work extra to cover. Then, when the covering doctor takes PTO, the first doctor must work extra—effectively offsetting the value of PTO. And if a hospitalist takes PTO and also works extra shifts in the same pay period, do these two offset each other? Or does the doctor get paid for both the PTO days and the extra shift days?
For clinicians such as hospitalists, whose work is defined in highly variable, shift-based schedules that include a lot of night and weekend work, it becomes very difficult to determine which of the days not worked were PTO days versus just days the doctor wasn’t scheduled.
Personally, I don’t think it makes much sense for most hospitalists to have PTO. Don’t get me wrong—I think hospitalists should be paid well and have generous amounts of time off in exchange for long, challenging workdays and a disproportionate amount of night and weekend work. But arbitrarily assigning some of the days not worked as PTO while others are just unscheduled days seems unnecessarily complex.
Time will tell if the specialty as a whole agrees with me or not.
Leslie Flores is a principal in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
For the first time in several years, SHM included questions about employee benefits and paid time off in its 2012 State of Hospital Medicine survey. The median value of benefits per physician FTE reported by HM groups serving adults only was $26,000, according to the 2012 survey. But what a surprise it was when survey respondents in 2007 reported median benefits of $31,900.
I admit to being flummoxed by the decrease. The definition of “benefits” was identical in both surveys. The only difference is that in 2007, SHM collected actual benefit cost for each individual on the individual questionnaire; in 2012, we asked for the average benefits per FTE for the group. One possible explanation is that some respondents simply guessed about the average, because they didn’t have to report data for individual doctors. Of course, it’s also possible that groups are requiring physicians to pay a higher proportion of insurance premiums or are reducing retirement plan contributions due to the weak economy. But in the work I do with hospitalist groups around the country, I rarely see benefit costs below about $35,000.
Source: 2012 State of Hospital Medicine report
Another interesting finding from the 2012 survey is that 37% of adult medicine groups reported offering paid time off (PTO), down from 54% in 2007. Even among groups using a seven-on/seven-off schedule, the PTO rate was only 44%. Does this represent a survey design or respondent input error, differences in respondent populations, or an actual shift in the prevalence of PTO benefits? I suspect it’s the latter, because the median amount of PTO time awarded has also declined. In 2007, adult HMGs reported a median of 25 PTO days annually. In 2012, the median for those groups offering PTO was 160 hours of PTO, which represents somewhere around 13 to 20 days, depending on shift length.
Why might PTO benefits be declining? I suppose it could be belt-tightening associated with the poor economy. But I think many HM groups simply have found PTO benefits difficult to administer and fraught with unintended consequences. Many groups are so thinly staffed that for someone to take a PTO day, someone else must work extra to cover. Then, when the covering doctor takes PTO, the first doctor must work extra—effectively offsetting the value of PTO. And if a hospitalist takes PTO and also works extra shifts in the same pay period, do these two offset each other? Or does the doctor get paid for both the PTO days and the extra shift days?
For clinicians such as hospitalists, whose work is defined in highly variable, shift-based schedules that include a lot of night and weekend work, it becomes very difficult to determine which of the days not worked were PTO days versus just days the doctor wasn’t scheduled.
Personally, I don’t think it makes much sense for most hospitalists to have PTO. Don’t get me wrong—I think hospitalists should be paid well and have generous amounts of time off in exchange for long, challenging workdays and a disproportionate amount of night and weekend work. But arbitrarily assigning some of the days not worked as PTO while others are just unscheduled days seems unnecessarily complex.
Time will tell if the specialty as a whole agrees with me or not.
Leslie Flores is a principal in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
Accuracy Matters When Compensation for Hospitalists Is at Stake
Not long ago, I received an email from a hospitalist group leader who was working with her CMO on a new compensation plan. The CMO, wanting to ensure that the proposed compensation per unit of work was appropriate, had taken the MGMA national median annual compensation for internal-medicine hospitalists ($234,437) and divided it by the national median annual work RVUs (4,185) to arrive at a targeted compensation per wRVU of $56.01.
The hospitalist leader, however, had the benefit of referring to her 2012 State of Hospital Medicine report, in which Table 6.30 reported an MGMA median compensation per wRVU for internal-medicine hospitalists of $58.28. That variance of more than two dollars per wRVU could mean an additional $8,000 or so in annual compensation to her and her colleagues, so she was seeking to understand why the report has a different number than the one calculated by her CMO.
The answer is that the CMO got caught in a common error of logic: The CMO assumed that the compensation median and the wRVU median were derived from exactly the same population, failing to consider that the underlying data sets might be different. Here’s what happened: Compensation data were reported for 3,192 internal-medicine hospitalists, but wRVUs were reported for only 2,389 of those hospitalists. So the analysis of compensation per wRVU can be accurately calculated only for those 2,389 hospitalists for whom both compensation and wRVUs were reported. The other 803 hospitalists for whom no wRVUs were reported had to be excluded from the ratio calculation. The CMO’s error was to calculate a ratio of two medians based on different data sets, rather than calculating the individual comp-to-wRVU ratios, then determining the median for that smaller data set.
A similar thing has happened over the years with nocturnist data. In SHM’s 2007-2008 compensation and productivity survey, and again in the 2011 SHM/MGMA State of Hospital Medicine report, the median compensation reported for nocturnists actually was lower than that reported for all adult hospitalists. In my work with hospitalist practices across the country, I’ve only run into one or two where the nocturnists earned less than the daytime doctors, so I was flummoxed by this finding. Turns out, I was making the same mistake of assuming I was looking at “nocturnist” and “all adult hospitalist” compensation for the same hospitalist groups. But the adult medicine groups using nocturnists are actually a small subset of all adult medicine groups, and the nocturnist data likely included at least a few pediatric hospitalist nocturnists. Because the underlying data sets are different, the two medians aren’t directly comparable.
When all is said and done, we don’t really care whether the average nocturnist earns more or less than the average non-nocturnist hospitalist. What we really want to know is, Do the nocturnists in a given group earn more than the non-nocturnists in the same group? That’s why this year SHM asked groups to report the average percent compensation differential between nocturnists and non-nocturnists in their groups. It turns out that groups serving adults only reported a median of 15% higher compensation for nocturnists, a far different result than users of previous surveys inferred.
The bottom line: Make sure you understand how the State of Hospital Medicine survey results are calculated. Many of the formulas used are described in Appendix B of the report, and if you have questions about others, feel free to contact SHM and ask.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants.
Not long ago, I received an email from a hospitalist group leader who was working with her CMO on a new compensation plan. The CMO, wanting to ensure that the proposed compensation per unit of work was appropriate, had taken the MGMA national median annual compensation for internal-medicine hospitalists ($234,437) and divided it by the national median annual work RVUs (4,185) to arrive at a targeted compensation per wRVU of $56.01.
The hospitalist leader, however, had the benefit of referring to her 2012 State of Hospital Medicine report, in which Table 6.30 reported an MGMA median compensation per wRVU for internal-medicine hospitalists of $58.28. That variance of more than two dollars per wRVU could mean an additional $8,000 or so in annual compensation to her and her colleagues, so she was seeking to understand why the report has a different number than the one calculated by her CMO.
The answer is that the CMO got caught in a common error of logic: The CMO assumed that the compensation median and the wRVU median were derived from exactly the same population, failing to consider that the underlying data sets might be different. Here’s what happened: Compensation data were reported for 3,192 internal-medicine hospitalists, but wRVUs were reported for only 2,389 of those hospitalists. So the analysis of compensation per wRVU can be accurately calculated only for those 2,389 hospitalists for whom both compensation and wRVUs were reported. The other 803 hospitalists for whom no wRVUs were reported had to be excluded from the ratio calculation. The CMO’s error was to calculate a ratio of two medians based on different data sets, rather than calculating the individual comp-to-wRVU ratios, then determining the median for that smaller data set.
A similar thing has happened over the years with nocturnist data. In SHM’s 2007-2008 compensation and productivity survey, and again in the 2011 SHM/MGMA State of Hospital Medicine report, the median compensation reported for nocturnists actually was lower than that reported for all adult hospitalists. In my work with hospitalist practices across the country, I’ve only run into one or two where the nocturnists earned less than the daytime doctors, so I was flummoxed by this finding. Turns out, I was making the same mistake of assuming I was looking at “nocturnist” and “all adult hospitalist” compensation for the same hospitalist groups. But the adult medicine groups using nocturnists are actually a small subset of all adult medicine groups, and the nocturnist data likely included at least a few pediatric hospitalist nocturnists. Because the underlying data sets are different, the two medians aren’t directly comparable.
When all is said and done, we don’t really care whether the average nocturnist earns more or less than the average non-nocturnist hospitalist. What we really want to know is, Do the nocturnists in a given group earn more than the non-nocturnists in the same group? That’s why this year SHM asked groups to report the average percent compensation differential between nocturnists and non-nocturnists in their groups. It turns out that groups serving adults only reported a median of 15% higher compensation for nocturnists, a far different result than users of previous surveys inferred.
The bottom line: Make sure you understand how the State of Hospital Medicine survey results are calculated. Many of the formulas used are described in Appendix B of the report, and if you have questions about others, feel free to contact SHM and ask.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants.
Not long ago, I received an email from a hospitalist group leader who was working with her CMO on a new compensation plan. The CMO, wanting to ensure that the proposed compensation per unit of work was appropriate, had taken the MGMA national median annual compensation for internal-medicine hospitalists ($234,437) and divided it by the national median annual work RVUs (4,185) to arrive at a targeted compensation per wRVU of $56.01.
The hospitalist leader, however, had the benefit of referring to her 2012 State of Hospital Medicine report, in which Table 6.30 reported an MGMA median compensation per wRVU for internal-medicine hospitalists of $58.28. That variance of more than two dollars per wRVU could mean an additional $8,000 or so in annual compensation to her and her colleagues, so she was seeking to understand why the report has a different number than the one calculated by her CMO.
The answer is that the CMO got caught in a common error of logic: The CMO assumed that the compensation median and the wRVU median were derived from exactly the same population, failing to consider that the underlying data sets might be different. Here’s what happened: Compensation data were reported for 3,192 internal-medicine hospitalists, but wRVUs were reported for only 2,389 of those hospitalists. So the analysis of compensation per wRVU can be accurately calculated only for those 2,389 hospitalists for whom both compensation and wRVUs were reported. The other 803 hospitalists for whom no wRVUs were reported had to be excluded from the ratio calculation. The CMO’s error was to calculate a ratio of two medians based on different data sets, rather than calculating the individual comp-to-wRVU ratios, then determining the median for that smaller data set.
A similar thing has happened over the years with nocturnist data. In SHM’s 2007-2008 compensation and productivity survey, and again in the 2011 SHM/MGMA State of Hospital Medicine report, the median compensation reported for nocturnists actually was lower than that reported for all adult hospitalists. In my work with hospitalist practices across the country, I’ve only run into one or two where the nocturnists earned less than the daytime doctors, so I was flummoxed by this finding. Turns out, I was making the same mistake of assuming I was looking at “nocturnist” and “all adult hospitalist” compensation for the same hospitalist groups. But the adult medicine groups using nocturnists are actually a small subset of all adult medicine groups, and the nocturnist data likely included at least a few pediatric hospitalist nocturnists. Because the underlying data sets are different, the two medians aren’t directly comparable.
When all is said and done, we don’t really care whether the average nocturnist earns more or less than the average non-nocturnist hospitalist. What we really want to know is, Do the nocturnists in a given group earn more than the non-nocturnists in the same group? That’s why this year SHM asked groups to report the average percent compensation differential between nocturnists and non-nocturnists in their groups. It turns out that groups serving adults only reported a median of 15% higher compensation for nocturnists, a far different result than users of previous surveys inferred.
The bottom line: Make sure you understand how the State of Hospital Medicine survey results are calculated. Many of the formulas used are described in Appendix B of the report, and if you have questions about others, feel free to contact SHM and ask.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants.
Turnover for Hospitalist Groups Steady at 10%
How many hospitalists left your group during the past year? If you're lucky, your group is one of the 36% of adult medicine groups that had no turnover at all. The proportion of groups with no turnover has ranged from a low of 32% (in the 2008-2009 SHM Focused Survey) to a high of 39% (2005-2006 and 2007-2008 SHM biannual surveys), so the 2012 results appear to be right in line with previous years.
But what about the groups that did encounter turnover? SHM's 2012 State of Hospital Medicine Report, which is based on 2011 data, reported a median turnover rate of 10% for nonacademic HM groups serving adults only. That's a little higher than last year's rate but lower than the rate reported in the 2010 SHM/MGMA survey. (It's worth keeping in mind that, in 2012, SHM conducted its own survey separate from MGMA, so the results might not be directly comparable to the previous two years' SHM/MGMA surveys.)
What part of the country you practice in and who employs you matters. In 2012, groups in the Western region of the U.S. reported only about 5% turnover, compared with 10% or 11% in other parts of the country. Turnover also varied by ownership/employment model: Groups employed by management companies and university/medical schools reported higher-than-median turnover; private hospitalist groups and those employed by multispecialty groups reported lower turnover. And medium-sized groups (five to 19 hospitalist FTEs) reported higher turnover than very small or larger groups.
The report also includes turnover rates for physician assistants (PAs) and nurse practitioners (NPs). Interestingly, turnover was much lower among NPs and PAs, with around 70% of the adult medicine groups who used NP/PAs reporting no NP/PA turnover at all.
Some folks have speculated that hospitalist turnover will decline as the supply of hospitalists begins to catch up with demand, which seems reasonable. Although we can't assess turnover data at this level of granularity, I'm guessing that turnover in highly-sought-after metropolitan markets, such as Washington, New York City, and Seattle, already is trending lower than in areas that are harder to recruit to.
But as far back as its 2005-2006 survey, SHM reported median turnover of 9%—not meaningfully different from this year's survey results. I suspect hospitalist turnover will continue to hover in the 10% to 15% range for the foreseeable future. Part of that figure can be attributed to the fact that significant numbers of hospitalists working in remote locations are international medical graduates on H-1B and J-1 visas. They typically make a three-year commitment, then move on to a more desirable location. But I think it's also because of the kinds of people who are attracted to hospital medicine.
As my colleague John Nelson, MD, MHM, likes to say, "hospitalists tend to want to date their practice, rather than marry it."
HM jobs have low barriers to entry and exit, at least compared with traditional primary care, which involves building an infrastructure and a panel of patients over many years. HM likely will continue to attract clinicians who enjoy looking around and changing jobs periodically. It will be interesting to see what the next few years bring to our specialty.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants and SHM Practice Analysis Committee member.
How many hospitalists left your group during the past year? If you're lucky, your group is one of the 36% of adult medicine groups that had no turnover at all. The proportion of groups with no turnover has ranged from a low of 32% (in the 2008-2009 SHM Focused Survey) to a high of 39% (2005-2006 and 2007-2008 SHM biannual surveys), so the 2012 results appear to be right in line with previous years.
But what about the groups that did encounter turnover? SHM's 2012 State of Hospital Medicine Report, which is based on 2011 data, reported a median turnover rate of 10% for nonacademic HM groups serving adults only. That's a little higher than last year's rate but lower than the rate reported in the 2010 SHM/MGMA survey. (It's worth keeping in mind that, in 2012, SHM conducted its own survey separate from MGMA, so the results might not be directly comparable to the previous two years' SHM/MGMA surveys.)
What part of the country you practice in and who employs you matters. In 2012, groups in the Western region of the U.S. reported only about 5% turnover, compared with 10% or 11% in other parts of the country. Turnover also varied by ownership/employment model: Groups employed by management companies and university/medical schools reported higher-than-median turnover; private hospitalist groups and those employed by multispecialty groups reported lower turnover. And medium-sized groups (five to 19 hospitalist FTEs) reported higher turnover than very small or larger groups.
The report also includes turnover rates for physician assistants (PAs) and nurse practitioners (NPs). Interestingly, turnover was much lower among NPs and PAs, with around 70% of the adult medicine groups who used NP/PAs reporting no NP/PA turnover at all.
Some folks have speculated that hospitalist turnover will decline as the supply of hospitalists begins to catch up with demand, which seems reasonable. Although we can't assess turnover data at this level of granularity, I'm guessing that turnover in highly-sought-after metropolitan markets, such as Washington, New York City, and Seattle, already is trending lower than in areas that are harder to recruit to.
But as far back as its 2005-2006 survey, SHM reported median turnover of 9%—not meaningfully different from this year's survey results. I suspect hospitalist turnover will continue to hover in the 10% to 15% range for the foreseeable future. Part of that figure can be attributed to the fact that significant numbers of hospitalists working in remote locations are international medical graduates on H-1B and J-1 visas. They typically make a three-year commitment, then move on to a more desirable location. But I think it's also because of the kinds of people who are attracted to hospital medicine.
As my colleague John Nelson, MD, MHM, likes to say, "hospitalists tend to want to date their practice, rather than marry it."
HM jobs have low barriers to entry and exit, at least compared with traditional primary care, which involves building an infrastructure and a panel of patients over many years. HM likely will continue to attract clinicians who enjoy looking around and changing jobs periodically. It will be interesting to see what the next few years bring to our specialty.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants and SHM Practice Analysis Committee member.
How many hospitalists left your group during the past year? If you're lucky, your group is one of the 36% of adult medicine groups that had no turnover at all. The proportion of groups with no turnover has ranged from a low of 32% (in the 2008-2009 SHM Focused Survey) to a high of 39% (2005-2006 and 2007-2008 SHM biannual surveys), so the 2012 results appear to be right in line with previous years.
But what about the groups that did encounter turnover? SHM's 2012 State of Hospital Medicine Report, which is based on 2011 data, reported a median turnover rate of 10% for nonacademic HM groups serving adults only. That's a little higher than last year's rate but lower than the rate reported in the 2010 SHM/MGMA survey. (It's worth keeping in mind that, in 2012, SHM conducted its own survey separate from MGMA, so the results might not be directly comparable to the previous two years' SHM/MGMA surveys.)
What part of the country you practice in and who employs you matters. In 2012, groups in the Western region of the U.S. reported only about 5% turnover, compared with 10% or 11% in other parts of the country. Turnover also varied by ownership/employment model: Groups employed by management companies and university/medical schools reported higher-than-median turnover; private hospitalist groups and those employed by multispecialty groups reported lower turnover. And medium-sized groups (five to 19 hospitalist FTEs) reported higher turnover than very small or larger groups.
The report also includes turnover rates for physician assistants (PAs) and nurse practitioners (NPs). Interestingly, turnover was much lower among NPs and PAs, with around 70% of the adult medicine groups who used NP/PAs reporting no NP/PA turnover at all.
Some folks have speculated that hospitalist turnover will decline as the supply of hospitalists begins to catch up with demand, which seems reasonable. Although we can't assess turnover data at this level of granularity, I'm guessing that turnover in highly-sought-after metropolitan markets, such as Washington, New York City, and Seattle, already is trending lower than in areas that are harder to recruit to.
But as far back as its 2005-2006 survey, SHM reported median turnover of 9%—not meaningfully different from this year's survey results. I suspect hospitalist turnover will continue to hover in the 10% to 15% range for the foreseeable future. Part of that figure can be attributed to the fact that significant numbers of hospitalists working in remote locations are international medical graduates on H-1B and J-1 visas. They typically make a three-year commitment, then move on to a more desirable location. But I think it's also because of the kinds of people who are attracted to hospital medicine.
As my colleague John Nelson, MD, MHM, likes to say, "hospitalists tend to want to date their practice, rather than marry it."
HM jobs have low barriers to entry and exit, at least compared with traditional primary care, which involves building an infrastructure and a panel of patients over many years. HM likely will continue to attract clinicians who enjoy looking around and changing jobs periodically. It will be interesting to see what the next few years bring to our specialty.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants and SHM Practice Analysis Committee member.
Off-Label Use of Antipsychotics for Dementia Patients Discouraged
Hospitalists can play a major role in reducing deaths that come as a result of off-label prescriptions for antipsychotic drugs being given to dementia patients, according to the Centers for Medicare & Medicaid Services (CMS) and SHM.
In a letter to hospitalist leaders, SHM encouraged hospitalists to “partner with others in your clinical work environment to reduce the use of antipsychotics for treating behavioral problems in patients with dementia. We believe that hospitalists have an important role to play in this initiative; hospital-based clinicians frequently care for patients with dementia and are responsible for medications prescribed during a patient’s hospitalization and at discharge.”
The joint education effort by CMS and SHM is based on an April 2011 report from the U.S. Department of Health and Human Services’ Office of Inspector General (OIG) that found that antipsychotic medications sometimes are used to treat patients with dementia for off-label reasons (e.g. “behaviors”) or against black-box warnings despite potential dangers to patients’ health.
An earlier warning from the FDA in 2008 outlined the potential dangers as:
- Increased risk (60% to 70%) of death in older adults with dementia;
- Prolongation of the QT interval on electrocardiogram, particularly with intravenous haloperidol use;
- Increased risk of stroke and TIAs; and
- Worsening cognitive function.
The letter to hospitalists noted the necessary changes and the need for collaboration between SHM, its members, and hospital leaders. “Increased prescriber training and system practice changes will help reduce unnecessary antipsychotic drug prescribing,” the letter stated. “SHM looks forward to an ongoing collaboration with members and hospital leaders on this important patient safety concern.”
Hospitalists can play a major role in reducing deaths that come as a result of off-label prescriptions for antipsychotic drugs being given to dementia patients, according to the Centers for Medicare & Medicaid Services (CMS) and SHM.
In a letter to hospitalist leaders, SHM encouraged hospitalists to “partner with others in your clinical work environment to reduce the use of antipsychotics for treating behavioral problems in patients with dementia. We believe that hospitalists have an important role to play in this initiative; hospital-based clinicians frequently care for patients with dementia and are responsible for medications prescribed during a patient’s hospitalization and at discharge.”
The joint education effort by CMS and SHM is based on an April 2011 report from the U.S. Department of Health and Human Services’ Office of Inspector General (OIG) that found that antipsychotic medications sometimes are used to treat patients with dementia for off-label reasons (e.g. “behaviors”) or against black-box warnings despite potential dangers to patients’ health.
An earlier warning from the FDA in 2008 outlined the potential dangers as:
- Increased risk (60% to 70%) of death in older adults with dementia;
- Prolongation of the QT interval on electrocardiogram, particularly with intravenous haloperidol use;
- Increased risk of stroke and TIAs; and
- Worsening cognitive function.
The letter to hospitalists noted the necessary changes and the need for collaboration between SHM, its members, and hospital leaders. “Increased prescriber training and system practice changes will help reduce unnecessary antipsychotic drug prescribing,” the letter stated. “SHM looks forward to an ongoing collaboration with members and hospital leaders on this important patient safety concern.”
Hospitalists can play a major role in reducing deaths that come as a result of off-label prescriptions for antipsychotic drugs being given to dementia patients, according to the Centers for Medicare & Medicaid Services (CMS) and SHM.
In a letter to hospitalist leaders, SHM encouraged hospitalists to “partner with others in your clinical work environment to reduce the use of antipsychotics for treating behavioral problems in patients with dementia. We believe that hospitalists have an important role to play in this initiative; hospital-based clinicians frequently care for patients with dementia and are responsible for medications prescribed during a patient’s hospitalization and at discharge.”
The joint education effort by CMS and SHM is based on an April 2011 report from the U.S. Department of Health and Human Services’ Office of Inspector General (OIG) that found that antipsychotic medications sometimes are used to treat patients with dementia for off-label reasons (e.g. “behaviors”) or against black-box warnings despite potential dangers to patients’ health.
An earlier warning from the FDA in 2008 outlined the potential dangers as:
- Increased risk (60% to 70%) of death in older adults with dementia;
- Prolongation of the QT interval on electrocardiogram, particularly with intravenous haloperidol use;
- Increased risk of stroke and TIAs; and
- Worsening cognitive function.
The letter to hospitalists noted the necessary changes and the need for collaboration between SHM, its members, and hospital leaders. “Increased prescriber training and system practice changes will help reduce unnecessary antipsychotic drug prescribing,” the letter stated. “SHM looks forward to an ongoing collaboration with members and hospital leaders on this important patient safety concern.”
New Data on Hospitalist Schedules
With last month’s publication of the 2012 State of Hospital Medicine report (www.hospitalmedicine.org/survey), we have some fascinating new information about the scheduling choices of HM groups—some of which has never been collected by SHM before.
For example, we learned this year that 42% of respondent groups serving adult patients predominantly utilize a schedule of seven days on followed by seven days off (“seven-on, seven-off”), while another 42% use variable/other scheduling patterns. A small minority of groups utilize other types of rotating block schedules (e.g. five-on/five-off) or Monday-Friday schedules. The type of schedule used varies a lot by area of the country, ownership/employment model, and other group characteristics.
Full-time adult medicine hospitalists working shift-based schedules now work a median of 182 shifts, or work periods, annually, down from 188 the last time SHM asked this question in 2005. For doctors working hybrid schedules, including both shifts and on-call duties, the number of shifts declined to 204 from 215 in 2005. During the same period, hospitalists’ annual encounter volume also has declined, though compensation has continued its inexorable rise.
So if the number of shifts worked and patient encounters both have declined since 2005, why do hospitalists feel so much busier today?
Well, for one thing, we learned in this year’s survey that 75% of adult hospitalist groups schedule day shifts of 12 to 13.9 hours in length, while the other 25% use shorter day shifts. About 85% of night shifts are also 12 to 13.9 hours long, while the preponderance of evening/swing shifts fall into either the 10- to 11.9-hour range (45%) or the eight-hours-or-less range (33%). In 2005, the median shift length for all respondents—both adult and pediatric—was 11 hours for groups using shift-based models, and only eight hours for groups using hybrid or other scheduling models. So although this year’s data is not presented in the same way as it was in 2005, it would appear that the typical shift length might have increased some.
In addition, in 2005, only 51% of groups reported having an on-site provider at night. This year, 55% of groups reported having total on-site nighttime coverage, and an additional 28% reported using a combination of on-site and on-call coverage. And the proportion of groups reporting no responsibility for night coverage at all declined to about 1% from 8%. I’m guessing the need to work more nights also contributes to hospitalists’ feelings of increased workload.
Although encounters have decreased, hospitalist wRVUs have risen dramatically. In part, this is due to adjustments in Medicare wRVU values for typical E&M services, but I believe it also is the result of increased patient complexity and/or improved documentation and coding by hospitalists—both of which require more time.
And finally, hospitalists are being asked to do a lot more nonclinical work these days, such as participating in quality-improvement (QI) and patient-flow initiatives, and championing the implementation of electronic health records (EHRs).
All of these factors, and probably others, have combined to make the typical hospitalist’s job much more complex and demanding today than it was in 2005, despite working a few less shifts and have a few less patient encounters annually.
Leslie Flores is SHM senior advisor, practice management.
With last month’s publication of the 2012 State of Hospital Medicine report (www.hospitalmedicine.org/survey), we have some fascinating new information about the scheduling choices of HM groups—some of which has never been collected by SHM before.
For example, we learned this year that 42% of respondent groups serving adult patients predominantly utilize a schedule of seven days on followed by seven days off (“seven-on, seven-off”), while another 42% use variable/other scheduling patterns. A small minority of groups utilize other types of rotating block schedules (e.g. five-on/five-off) or Monday-Friday schedules. The type of schedule used varies a lot by area of the country, ownership/employment model, and other group characteristics.
Full-time adult medicine hospitalists working shift-based schedules now work a median of 182 shifts, or work periods, annually, down from 188 the last time SHM asked this question in 2005. For doctors working hybrid schedules, including both shifts and on-call duties, the number of shifts declined to 204 from 215 in 2005. During the same period, hospitalists’ annual encounter volume also has declined, though compensation has continued its inexorable rise.
So if the number of shifts worked and patient encounters both have declined since 2005, why do hospitalists feel so much busier today?
Well, for one thing, we learned in this year’s survey that 75% of adult hospitalist groups schedule day shifts of 12 to 13.9 hours in length, while the other 25% use shorter day shifts. About 85% of night shifts are also 12 to 13.9 hours long, while the preponderance of evening/swing shifts fall into either the 10- to 11.9-hour range (45%) or the eight-hours-or-less range (33%). In 2005, the median shift length for all respondents—both adult and pediatric—was 11 hours for groups using shift-based models, and only eight hours for groups using hybrid or other scheduling models. So although this year’s data is not presented in the same way as it was in 2005, it would appear that the typical shift length might have increased some.
In addition, in 2005, only 51% of groups reported having an on-site provider at night. This year, 55% of groups reported having total on-site nighttime coverage, and an additional 28% reported using a combination of on-site and on-call coverage. And the proportion of groups reporting no responsibility for night coverage at all declined to about 1% from 8%. I’m guessing the need to work more nights also contributes to hospitalists’ feelings of increased workload.
Although encounters have decreased, hospitalist wRVUs have risen dramatically. In part, this is due to adjustments in Medicare wRVU values for typical E&M services, but I believe it also is the result of increased patient complexity and/or improved documentation and coding by hospitalists—both of which require more time.
And finally, hospitalists are being asked to do a lot more nonclinical work these days, such as participating in quality-improvement (QI) and patient-flow initiatives, and championing the implementation of electronic health records (EHRs).
All of these factors, and probably others, have combined to make the typical hospitalist’s job much more complex and demanding today than it was in 2005, despite working a few less shifts and have a few less patient encounters annually.
Leslie Flores is SHM senior advisor, practice management.
With last month’s publication of the 2012 State of Hospital Medicine report (www.hospitalmedicine.org/survey), we have some fascinating new information about the scheduling choices of HM groups—some of which has never been collected by SHM before.
For example, we learned this year that 42% of respondent groups serving adult patients predominantly utilize a schedule of seven days on followed by seven days off (“seven-on, seven-off”), while another 42% use variable/other scheduling patterns. A small minority of groups utilize other types of rotating block schedules (e.g. five-on/five-off) or Monday-Friday schedules. The type of schedule used varies a lot by area of the country, ownership/employment model, and other group characteristics.
Full-time adult medicine hospitalists working shift-based schedules now work a median of 182 shifts, or work periods, annually, down from 188 the last time SHM asked this question in 2005. For doctors working hybrid schedules, including both shifts and on-call duties, the number of shifts declined to 204 from 215 in 2005. During the same period, hospitalists’ annual encounter volume also has declined, though compensation has continued its inexorable rise.
So if the number of shifts worked and patient encounters both have declined since 2005, why do hospitalists feel so much busier today?
Well, for one thing, we learned in this year’s survey that 75% of adult hospitalist groups schedule day shifts of 12 to 13.9 hours in length, while the other 25% use shorter day shifts. About 85% of night shifts are also 12 to 13.9 hours long, while the preponderance of evening/swing shifts fall into either the 10- to 11.9-hour range (45%) or the eight-hours-or-less range (33%). In 2005, the median shift length for all respondents—both adult and pediatric—was 11 hours for groups using shift-based models, and only eight hours for groups using hybrid or other scheduling models. So although this year’s data is not presented in the same way as it was in 2005, it would appear that the typical shift length might have increased some.
In addition, in 2005, only 51% of groups reported having an on-site provider at night. This year, 55% of groups reported having total on-site nighttime coverage, and an additional 28% reported using a combination of on-site and on-call coverage. And the proportion of groups reporting no responsibility for night coverage at all declined to about 1% from 8%. I’m guessing the need to work more nights also contributes to hospitalists’ feelings of increased workload.
Although encounters have decreased, hospitalist wRVUs have risen dramatically. In part, this is due to adjustments in Medicare wRVU values for typical E&M services, but I believe it also is the result of increased patient complexity and/or improved documentation and coding by hospitalists—both of which require more time.
And finally, hospitalists are being asked to do a lot more nonclinical work these days, such as participating in quality-improvement (QI) and patient-flow initiatives, and championing the implementation of electronic health records (EHRs).
All of these factors, and probably others, have combined to make the typical hospitalist’s job much more complex and demanding today than it was in 2005, despite working a few less shifts and have a few less patient encounters annually.
Leslie Flores is SHM senior advisor, practice management.
Survey Insights: HM's Financial Support Requirement
One of the most eagerly awaited results from an SHM compensation and productivity survey is the amount of financial support provided by hospitals or other organizations to HM groups (note that we’ve carefully avoided the dreaded “S” word). SHM has been asking this question since at least 2003, when the median annual support per hospitalist FTE was reported at $60,000. By 2007, that number had grown by 62% to $97,375. But the 2007 findings that might have caused the greatest uproar were that fully 37% of responding HM group leaders did not know their program’s annual expenses, and 35% did not know their program’s revenues.
Fast-forward to today. The median annual financial support per FTE reported in the 2011 SHM/MGMA State of Hospital Medicine report is $136,403, a whopping 39% increase over the 2010 median of $98,253.
What caused this big increase in HM’s financial support requirement? Did costs go up that dramatically in just one year? Well, the median compensation for adult medicine hospitalists (the vast majority of hospitalists in the data set) went up by a mere 2.6% during the same period. The amount of support staffing reported by HM groups did not change appreciably. And since labor accounts for the vast majority of virtually every HM practice’s costs, it’s unlikely that the increase in financial support per FTE was caused by a dramatic increase in program costs.
Perhaps program revenues went down significantly, then. It’s true that the median professional fee collections per FTE for adult hospitalists declined between the 2010 and 2011 reports, but only by about 3.3%—probably a result of gearing up for healthcare reform, increases in indigent care and bad debt due to the weak economy, and similar revenue pressures. So it doesn’t appear that declining revenues can explain the big jump in financial support per FTE, either.
I’d like to think that one of the reasons financial support per FTE has increased so much is that we are getting better at how we ask the question. Early on, we simply asked, “If your group receives OTHER INCOME (besides collections for direct patient care), indicate source and amount of payments.” In recent years, the question has been fine-tuned to ask about “financial support over and above professional fee revenues from one or more hospitals or integrated delivery systems (or other sources),” and the survey guide has given even more detailed instructions. But in truth, the question was worded almost identically in 2010 and 2011.
All of this leads me to the unavoidable speculation that HM groups (and/or the hospitals they work for) probably are becoming more sophisticated about how they account for the costs of their hospitalist programs, and that HM group leaders are becoming more knowledgeable about their own programs’ costs and revenues (and, yes, the amount of financial support they receive). We haven’t asked respondents recently whether they know their practice’s costs and revenues, but maybe next time we should. I’ll bet the results will differ a lot from 2007.
—Leslie Flores, MHA, SHM senior advisor
One of the most eagerly awaited results from an SHM compensation and productivity survey is the amount of financial support provided by hospitals or other organizations to HM groups (note that we’ve carefully avoided the dreaded “S” word). SHM has been asking this question since at least 2003, when the median annual support per hospitalist FTE was reported at $60,000. By 2007, that number had grown by 62% to $97,375. But the 2007 findings that might have caused the greatest uproar were that fully 37% of responding HM group leaders did not know their program’s annual expenses, and 35% did not know their program’s revenues.
Fast-forward to today. The median annual financial support per FTE reported in the 2011 SHM/MGMA State of Hospital Medicine report is $136,403, a whopping 39% increase over the 2010 median of $98,253.
What caused this big increase in HM’s financial support requirement? Did costs go up that dramatically in just one year? Well, the median compensation for adult medicine hospitalists (the vast majority of hospitalists in the data set) went up by a mere 2.6% during the same period. The amount of support staffing reported by HM groups did not change appreciably. And since labor accounts for the vast majority of virtually every HM practice’s costs, it’s unlikely that the increase in financial support per FTE was caused by a dramatic increase in program costs.
Perhaps program revenues went down significantly, then. It’s true that the median professional fee collections per FTE for adult hospitalists declined between the 2010 and 2011 reports, but only by about 3.3%—probably a result of gearing up for healthcare reform, increases in indigent care and bad debt due to the weak economy, and similar revenue pressures. So it doesn’t appear that declining revenues can explain the big jump in financial support per FTE, either.
I’d like to think that one of the reasons financial support per FTE has increased so much is that we are getting better at how we ask the question. Early on, we simply asked, “If your group receives OTHER INCOME (besides collections for direct patient care), indicate source and amount of payments.” In recent years, the question has been fine-tuned to ask about “financial support over and above professional fee revenues from one or more hospitals or integrated delivery systems (or other sources),” and the survey guide has given even more detailed instructions. But in truth, the question was worded almost identically in 2010 and 2011.
All of this leads me to the unavoidable speculation that HM groups (and/or the hospitals they work for) probably are becoming more sophisticated about how they account for the costs of their hospitalist programs, and that HM group leaders are becoming more knowledgeable about their own programs’ costs and revenues (and, yes, the amount of financial support they receive). We haven’t asked respondents recently whether they know their practice’s costs and revenues, but maybe next time we should. I’ll bet the results will differ a lot from 2007.
—Leslie Flores, MHA, SHM senior advisor
One of the most eagerly awaited results from an SHM compensation and productivity survey is the amount of financial support provided by hospitals or other organizations to HM groups (note that we’ve carefully avoided the dreaded “S” word). SHM has been asking this question since at least 2003, when the median annual support per hospitalist FTE was reported at $60,000. By 2007, that number had grown by 62% to $97,375. But the 2007 findings that might have caused the greatest uproar were that fully 37% of responding HM group leaders did not know their program’s annual expenses, and 35% did not know their program’s revenues.
Fast-forward to today. The median annual financial support per FTE reported in the 2011 SHM/MGMA State of Hospital Medicine report is $136,403, a whopping 39% increase over the 2010 median of $98,253.
What caused this big increase in HM’s financial support requirement? Did costs go up that dramatically in just one year? Well, the median compensation for adult medicine hospitalists (the vast majority of hospitalists in the data set) went up by a mere 2.6% during the same period. The amount of support staffing reported by HM groups did not change appreciably. And since labor accounts for the vast majority of virtually every HM practice’s costs, it’s unlikely that the increase in financial support per FTE was caused by a dramatic increase in program costs.
Perhaps program revenues went down significantly, then. It’s true that the median professional fee collections per FTE for adult hospitalists declined between the 2010 and 2011 reports, but only by about 3.3%—probably a result of gearing up for healthcare reform, increases in indigent care and bad debt due to the weak economy, and similar revenue pressures. So it doesn’t appear that declining revenues can explain the big jump in financial support per FTE, either.
I’d like to think that one of the reasons financial support per FTE has increased so much is that we are getting better at how we ask the question. Early on, we simply asked, “If your group receives OTHER INCOME (besides collections for direct patient care), indicate source and amount of payments.” In recent years, the question has been fine-tuned to ask about “financial support over and above professional fee revenues from one or more hospitals or integrated delivery systems (or other sources),” and the survey guide has given even more detailed instructions. But in truth, the question was worded almost identically in 2010 and 2011.
All of this leads me to the unavoidable speculation that HM groups (and/or the hospitals they work for) probably are becoming more sophisticated about how they account for the costs of their hospitalist programs, and that HM group leaders are becoming more knowledgeable about their own programs’ costs and revenues (and, yes, the amount of financial support they receive). We haven’t asked respondents recently whether they know their practice’s costs and revenues, but maybe next time we should. I’ll bet the results will differ a lot from 2007.
—Leslie Flores, MHA, SHM senior advisor
Survey Insights: The Unique Connection between Compensation and Productivity
Perhaps one of the most interesting concepts in the 2011 SHM/MGMA State of Hospital Medicine report is illustrated by the potentially confusing graph, at right, which is reproduced from the report. By taking a few minutes to fully understand what the graph portrays, users can gain valuable insights into the relationship between productivity and compensation.
Let’s say I’m a hospitalist and my annual work RVU (wRVU) productivity is in the bottom 25% (first quartile) of all of the hospitalists who responded to the survey. My total compensation is likely to be relatively low—a median of $188,800—but my compensation per unit of work is likely to be relatively high—a median of $73.85 per wRVU.
On the other hand, if I’m a hospitalist with productivity in the top 25% of all hospitalists (fourth quartile), my overall compensation will probably be much higher—a median of $260,283—but my average compensation per unit of work has probably gone down quite a bit (note the median of $40.82 per wRVU).
Why is it that my compensation has gone up, but not at the same rate as my productivity?
Well, despite the increasing popularity of productivity incentives among HM groups in recent years, the majority of hospitalists still receive most of their pay in the form of a fixed salary. In fact, the survey, at right, found that the average hospitalist compensation package consists of about 80% fixed-base compensation, 16% productivity incentive, and 4% quality/performance incentive. Such compensation models give clear advantages to hospitalists with low productivity, and disadvantages to those with very high productivity.
Yes, many hospitalists can earn at least a bit more if they increase their productivity, but it’s often pennies on the dollar because neither their base salary nor their quality bonus components increase as their productivity goes up. Some of you might argue that compensation should rise in a straight line along with productivity, as it does in a practice with a 100% productivity-based compensation plan (some know this as the “eat what you treat” plan).
But what rises in a straight line can also fall in a straight line, and few hospitalists are comfortable with the risk of significant drops in income if their volume decreases for some reason.
Others might argue that it’s a good thing for compensation increases to taper off at high productivity levels, since this provides at least some reward for working harder but is less likely to incentivize people to work at unreasonable levels. And a few might argue that compensation per unit of work should actually increase at high productivity levels because once a hospitalist has covered their base salary and contribution to practice overhead, any additional revenue they bring into the practice is pure profit.
I have my opinions about these things, and I’m sure you do, too. But one of the things I like best about HM is the wide variety of practices out there. With so many hospitalist practices and so much variety, there’s a compensation model out there somewhere to suit everyone.
Perhaps one of the most interesting concepts in the 2011 SHM/MGMA State of Hospital Medicine report is illustrated by the potentially confusing graph, at right, which is reproduced from the report. By taking a few minutes to fully understand what the graph portrays, users can gain valuable insights into the relationship between productivity and compensation.
Let’s say I’m a hospitalist and my annual work RVU (wRVU) productivity is in the bottom 25% (first quartile) of all of the hospitalists who responded to the survey. My total compensation is likely to be relatively low—a median of $188,800—but my compensation per unit of work is likely to be relatively high—a median of $73.85 per wRVU.
On the other hand, if I’m a hospitalist with productivity in the top 25% of all hospitalists (fourth quartile), my overall compensation will probably be much higher—a median of $260,283—but my average compensation per unit of work has probably gone down quite a bit (note the median of $40.82 per wRVU).
Why is it that my compensation has gone up, but not at the same rate as my productivity?
Well, despite the increasing popularity of productivity incentives among HM groups in recent years, the majority of hospitalists still receive most of their pay in the form of a fixed salary. In fact, the survey, at right, found that the average hospitalist compensation package consists of about 80% fixed-base compensation, 16% productivity incentive, and 4% quality/performance incentive. Such compensation models give clear advantages to hospitalists with low productivity, and disadvantages to those with very high productivity.
Yes, many hospitalists can earn at least a bit more if they increase their productivity, but it’s often pennies on the dollar because neither their base salary nor their quality bonus components increase as their productivity goes up. Some of you might argue that compensation should rise in a straight line along with productivity, as it does in a practice with a 100% productivity-based compensation plan (some know this as the “eat what you treat” plan).
But what rises in a straight line can also fall in a straight line, and few hospitalists are comfortable with the risk of significant drops in income if their volume decreases for some reason.
Others might argue that it’s a good thing for compensation increases to taper off at high productivity levels, since this provides at least some reward for working harder but is less likely to incentivize people to work at unreasonable levels. And a few might argue that compensation per unit of work should actually increase at high productivity levels because once a hospitalist has covered their base salary and contribution to practice overhead, any additional revenue they bring into the practice is pure profit.
I have my opinions about these things, and I’m sure you do, too. But one of the things I like best about HM is the wide variety of practices out there. With so many hospitalist practices and so much variety, there’s a compensation model out there somewhere to suit everyone.
Perhaps one of the most interesting concepts in the 2011 SHM/MGMA State of Hospital Medicine report is illustrated by the potentially confusing graph, at right, which is reproduced from the report. By taking a few minutes to fully understand what the graph portrays, users can gain valuable insights into the relationship between productivity and compensation.
Let’s say I’m a hospitalist and my annual work RVU (wRVU) productivity is in the bottom 25% (first quartile) of all of the hospitalists who responded to the survey. My total compensation is likely to be relatively low—a median of $188,800—but my compensation per unit of work is likely to be relatively high—a median of $73.85 per wRVU.
On the other hand, if I’m a hospitalist with productivity in the top 25% of all hospitalists (fourth quartile), my overall compensation will probably be much higher—a median of $260,283—but my average compensation per unit of work has probably gone down quite a bit (note the median of $40.82 per wRVU).
Why is it that my compensation has gone up, but not at the same rate as my productivity?
Well, despite the increasing popularity of productivity incentives among HM groups in recent years, the majority of hospitalists still receive most of their pay in the form of a fixed salary. In fact, the survey, at right, found that the average hospitalist compensation package consists of about 80% fixed-base compensation, 16% productivity incentive, and 4% quality/performance incentive. Such compensation models give clear advantages to hospitalists with low productivity, and disadvantages to those with very high productivity.
Yes, many hospitalists can earn at least a bit more if they increase their productivity, but it’s often pennies on the dollar because neither their base salary nor their quality bonus components increase as their productivity goes up. Some of you might argue that compensation should rise in a straight line along with productivity, as it does in a practice with a 100% productivity-based compensation plan (some know this as the “eat what you treat” plan).
But what rises in a straight line can also fall in a straight line, and few hospitalists are comfortable with the risk of significant drops in income if their volume decreases for some reason.
Others might argue that it’s a good thing for compensation increases to taper off at high productivity levels, since this provides at least some reward for working harder but is less likely to incentivize people to work at unreasonable levels. And a few might argue that compensation per unit of work should actually increase at high productivity levels because once a hospitalist has covered their base salary and contribution to practice overhead, any additional revenue they bring into the practice is pure profit.
I have my opinions about these things, and I’m sure you do, too. But one of the things I like best about HM is the wide variety of practices out there. With so many hospitalist practices and so much variety, there’s a compensation model out there somewhere to suit everyone.