User login
OBJECTIVE: To examine the association between unintended pregnancy and the initiation and duration of breastfeeding.
STUDY DESIGN: This was a secondary data analysis of the 1995 Cycle 5 of the National Survey of Family Growth.
POPULATION: We studied 6733 first singleton live births to US women aged 15 years to 44 years.
OUTCOMES MEASURED: Using the 1995 Institute of Medicine definitions, pregnancies were classified as intended or unintended; unintended pregnancies were further categorized as either mis-timed or unwanted. We measured initiation of breastfeeding and duration of nonexclusive breastfeeding for at least 16 weeks.
RESULTS: In this study, 51.5% of women never breastfed, 48.5% initiated breastfeeding, and 26.4% of all women continued breastfeeding for at least 16 weeks. US women with unwanted unintended pregnancies were more likely not to initiate breastfeeding (odds ratio [OR] = 1.76; 95% confidence interval [CI], 1.26-2.44) and more likely not to continue breastfeeding (OR =1.69; 95% CI, 1.12-2.55) than women with intended pregnancies. White women with unwanted unintended pregnancies were more likely not to breastfeed than those with intended ones (initiation: OR = 2.50; 95% CI, 1.54-4.05; continuation: OR = 2.56; 95% CI, 1.34-4.87). This finding was not seen for black or Hispanic women.
CONCLUSIONS: In the United States, women with unwanted pregnancies were less likely either to initiate or to continue breastfeeding than women with intended pregnancies. A strong inverse association between unwanted pregnancies and breastfeeding was observed only for white women. Education for women with unintended pregnancies may improve breastfeeding rates and subsequently, the health of women and infants.
- In the United States, women whose pregnancies were unwanted are at a higher risk of not breastfeeding than women whose pregnancies were intended.
- Future research to evaluate the importance of incorporating pregnancy intention status into patient-centered breastfeeding promotion is needed.
- For now, women with unwanted pregnancies, especially white women, should be targeted for breastfeeding counseling.
Unintended pregnancy is a significant public health issue. More than half of all pregnancies are unintended at the time of conception; approximately half of those end as births and half as induced abortions.1 Forty-eight percent of women have at least one unplanned pregnancy, and 28% of women have at least one unplanned birth during their reproductive lifetime.2 Unintended pregnancies and births are associated with numerous harmful behaviors and adverse outcomes.3,4
Breastfeeding is currently promoted as the preferred method of feeding for infants for at least 1 year because of its multiple immediate and long-term benefits for both mother and child.5,6 Yet in 1998 only 64% of US mothers were breastfeeding at the time of hospital discharge and 29% at 6 months postpartum, which is well below the Healthy People 2010 goals of 75% and 50%, respectively, for those intervals.7
We hypothesized that women with unintended pregnancies are less likely to breastfeed their infants than those with intended ones. We quantified the association between the intendedness of pregnancy at the time of conception and breastfeeding behavior, both the initiation of any breastfeeding and the continuation of nonexclusive breastfeeding for at least 16 weeks, for first singleton births to US mothers. We then explored other factors which might affect breastfeeding practices.
Methods
Study design
This study is a secondary data analysis of the 1995 Cycle 5 of the National Survey of Family Growth (NSFG), a periodic population-based survey conducted by the National Center for Health Statistics and the Centers for Disease Control which focuses on women’s health and pregnancy. A national probability sample of 14,000 civilian noninstitutionalized women aged 15 years to 44 years was selected from among households that responded to the 1993 National Health Interview Survey, with an oversampling of minority women. Personal interviews were conducted between January and October of 1995 with 10,847 of these women. The data were then adjusted for a response rate of 79% and weighted so that findings would reflect the US population as a whole. Full details of the NSFG survey methods are described elsewhere.8
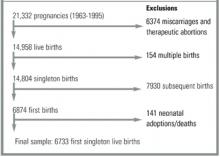
The data set contains information on 21,332 pregnancies and 14,958 live births (Figure). After excluding multiple gestations (n=154), subsequent births to the same mother (n=7930), and neonatal adoptions or deaths (n=141), the final sample contained 6733 first singleton live births. To study the initiation of breastfeeding, women who breastfed at all were compared with those who did not. To study duration of breastfeeding, women who breastfed for 16 or more weeks were compared with those who did not. In this second set of analyses, the 1459 women who breastfed for between 0 and 16 weeks and the 33 women who were breastfeeding at the time of the interview and whose children had been born within 16 weeks of that date were excluded.
FIGURE
Study sample
Variable definitions
Pregnancies were categorized as either intended or unintended at conception, using new definitions established by the Institute of Medicine in 1995.3 Pregnancies were considered intended if a woman had stopped using birth control because she wanted to become pregnant. Unintended pregnancies were classified into 1 of 2 categories: (1) mis-timed: wanted pregnancies that occurred sooner than desired, or (2) unwanted: pregnancies that occurred while a woman was using contraception and had not ever wanted to have a(nother) baby. The 170 women who described their pregnancy intention status as “didn’t know” or “didn’t care” were excluded from analyses involving intention status as defined above. There were 2 breastfeeding outcomes in this study: (1) initiation of breastfeeding, including women who reported any breastfeeding at all, and (2) duration of non-exclusive breastfeeding for at least 16 weeks.
Maternal demographics, intrapartum and postpartum behaviors, and birth outcomes were considered as potential confounders. As missing data were imputed in the public use data file, information on each variable was complete, except where noted below. Maternal age was determined at the time of conception. Education was defined as completed years of schooling at the time of the interview. Race was categorized as white, black, Hispanic, or other. Marital status was defined as either married or not married. Socioeconomic status was measured continuously as a percentage of the 1995 poverty level. Information on prenatal care was only available for births in the last 5 years (n=1266). For the 1241 women who reported that they had received prenatal care, the mean weeks of gestation at the time of the first prenatal visit were calculated. Maternity leave was defined as the use of maternity leave, paid or unpaid, for women who were working during the pregnancy (n=3662). For those who took any leave, the mean length of that leave was calculated in weeks. The 33 women for whom data were not available and the 5 women who answered that they took 0 weeks of maternity leave were not included in this calculation. Infant variables were considered categorically: mode of delivery, either vaginal or cesarean; prematurity, birth at less than or equal to 36 weeks; and low birth weight, less than or equal to 5.5 pounds.
Statistical analysis
The statistical significance of descriptive variables was determined using 2-sample t tests and chi-square tests, with women who did not breastfeed at all as the comparison group.
To compare our results with existing literature, we calculated crude odds ratios of not breastfeeding and used chi-square tests to assess the statistical significance of these associations. The reference group was always women whose pregnancies were intended. Variables identified as potential confounders were age, race, marital status, poverty level, education, maternity leave, mode of delivery, prematurity, and low birth weight. Final logistic regression models were adjusted for those variables that changed crude odds ratios by 10% or more: age, race, marital status, poverty level, and education. Adjusted odds ratios (ORs) of not breastfeeding and 95% confidence intervals (CIs) are reported.
Effect modification was assessed by dichotomizing each of the 5 confounding variables in the following manner: teen versus 20 years or older; white versus black versus Hispanic (here, the 193 women in the sample who defined their race as other were not included); married versus unmarried; high school education or higher versus less than a high school education; and below the poverty level versus at or above the poverty level. Each stratified analysis was adjusted for the other 4 factors. Interaction terms were created and P values for heterogeneity were calculated for all logistic models. For race, an additional interaction term was created to compare white with non-white (black and Hispanic combined) women.
These data are contained on the National Survey of Family Growth Cycle 5 1995 CD-ROM, Series 23, No. 3 and were exported using SETS version 1.22a (National Center for Health Statistics, Hyattsville, MD). All analyses were performed with SAS version 6.12 (SAS Institute, Cary, NC). Odds ratios are weighted using sampling weights provided in the data set. SUDAAN version 7.5.3 was used to obtain standard errors (Research Triangle Institute, Research Triangle Park, NC).
Results
In the total sample of 6733 first singleton live births to US mothers, 3267 (48.5%) of women initiated breastfeeding, compared with 3466 (51.5%) who did not. In the entire sample, 1775 (26.4%) continued to breastfeed nonexclusively for at least 16 weeks.
The breastfeeding initiation rate was 55.9%, 37.4%, and 28.0% for women with intended, mis-timed, and unwanted pregnancies, respectively. By 16 weeks, 32.6%, 17.0%, and 15.5% of women, respectively, were still breastfeeding. For all women who breastfed, the mean number of weeks of breastfeeding was 24.4 (standard deviation = 24.9; range = < 1 week to 4.0 years). Only 3.9% of women who breastfed did so for more than 2 years.
Table 1 shows characteristics of mothers and infants by breastfeeding behavior. Women who breastfed, both initially and for at least 16 weeks, were older at conception and had had more years of education than women who did not breastfeed at all. They were more likely to be white and less likely to be black. A similar percentage of women in each group were Hispanic. Percentage of the poverty level, a proxy for socioeconomic status, was higher for those who breastfed at all, but similar for those who continued breastfeeding and those who did not breastfeed. Rates of prenatal care and mean weeks at first prenatal visit were similar in all groups. Among women who were employed during their pregnancies, almost two thirds took maternity leave, regardless of breastfeeding behavior. Mean length of maternity leave was 3.4 weeks longer among women who continued to breastfeed than among women who did not breastfeed at all. The percentage of vaginal deliveries was similar among groups. Both premature and low birth weight infants were more common among women who did not breastfeed.
The association between the intendedness of pregnancy and breastfeeding behavior is reported in Table 2. Crude odds ratios show that women with any type of unintended pregnancy were more likely not to initiate breastfeeding than women whose pregnancies were intended. Some, but not all, of this association can be attributed to confounding by demographic factors. Having an unintended pregnancy was not associated with any significant difference in the initiation of breastfeeding, after adjusting for age, race, marital status, poverty level, and education. While women with mis-timed pregnancies were as likely to initiate breastfeeding as those whose pregnancies were intended (OR = 1.03; 95% CI, 0.88-1.21), women with unwanted pregnancies were more likely not to start breastfeeding (OR = 1.76; 95% CI, 1.26-2.44).
Table 2 also describes the association between pregnancy intention status and the continuation of nonexclusive breastfeeding for at least 16 weeks. In contrast to the initiation of breastfeeding, duration of breastfeeding was affected by the intendedness of pregnancy in every comparison. Adjusted odds ratios show that women with either type of unintended pregnancy were more likely not to continue breastfeeding than those with intended ones (OR = 1.28; 95% CI, 1.06-1.54). As with breastfeeding initiation, this association is being driven by the unwanted pregnancies. Women with unwanted pregnancies were more likely not to continue breastfeeding (OR = 1.69; 95% CI, 1.12-2.55).
Each of these associations was then evaluated for effect modification. As seen in Table 3, only race was an important factor. In the total sample, 56.3% of white women, 55.4% of Hispanic women, and 24.7% of black women breastfed at all; and 41.6%, 41.2%, and 12.6% of white, Hispanic, and black women breastfed for at least 16 weeks. White women with unwanted pregnancies were more likely not to initiate breastfeeding (OR = 2.50; 95% CI, 1.54-4.05) and more likely not to continue breastfeeding (OR = 2.56; 95% CI, 1.34-4.87) than white women with intended pregnancies. These differences in breastfeeding behaviors for unwanted pregnancies were not seen for either Hispanic or black women. For each stratified analysis, a single P value for heterogeneity was calculated to compare white women with non-white women (Hispanic and black women combined). The only significant difference by race was for unwanted pregnancies. The P value for heterogeneity was 0.01 for both initiation and continuation of breastfeeding. Stratified analyses for age, marital status, education, poverty level, and year of birth showed similar odds ratios across strata and nonsignificant P values for heterogeneity in every case (analyses not shown).
TABLE 1
Characteristics of mothers and infants by breastfeeding status (n=6733)
| Characteristic | Any breastfeeding (n = 3267) | Breastfeeding for ≥ 16 weeks (n = 1775) | No breastfeeding (n = 3466) |
|---|---|---|---|
| Age (mean years, SD) | 23.5 (5.0)* | 24.0 (5.1)* | 20.5 (4.3) |
| Race (%) | |||
| White | 64.8* | 65.9* | 47.4 |
| Black | 12.8 | 10.3 | 36.6 |
| Hispanic | 18.4 | 19.1 | 14.0 |
| Other | 4.0 | 4.7 | 2.0 |
| Married (%) | 65.0* | 68.8* | 37.3 |
| Percentage of the 1995 poverty level (SD) | 320 (207)* | 235 (205)* | 246 (189) |
| Education (mean years, SD) | 13.1 (3.0)* | 13.3 (3.2)* | 11.9 (2.3) |
| Prenatal care (%)† | 98.5 | 97.4 | 97.6 |
| Mean weeks at 1st visit (SD) | 7.8 (3.9) | 7.8 (4.0) | 9.1 (5.4) |
| Maternity leave ‡ | 65.2 | 60.7 | 64.6 |
| Mean weeks (SD) | 12.2 (9.4) | 13.8 (10.8) | 10.4 (8.3) |
| Vaginal delivery (%) | 78.5 | 78.9 | 80.7 |
| Prematurity (%) | 7.4* | 6.4* | 9.9 |
| Low birth weight (%) | 4.8* | 3.9* | 9.4 |
| SD denotes standard deviation. | |||
| *P ≤ .001 in comparison with women who did not breastfeed. | |||
| † For births during 1990-1994, n=1266. | |||
| ‡ Percentage of women employed during that pregnancy, n=3662. | |||
TABLE 2
Unintended pregnancy and breastfeeding behavior in the United States
| Intendedness of pregnancy | Number breastfeeding | Number not breastfeeding | Weighted crude odds ratio of NOT breastfeeding (95% CI)* | Weighted adjusted odds ratio of NOT breastfeeding (95% CI)* † |
|---|---|---|---|---|
| Initiation of breastfeeding (any) | ||||
| Intended | 2263 | 1758 | reference | reference |
| Unintended | 924 | 1618 | 2.15 (1.91-2.43) | 1.09 (0.93-1.28) |
| Mis-timed | 822 | 1361 | 2.02 (1.79-2.29) | 1.03 (0.88-1.21) |
| Unwanted | 102 | 257 | 3.54 (2.69-4.66) | 1.76 (1.26-2.44) |
| Continuation of breastfeeding (16 ≥ weeks) | ||||
| Intended | 1304 | 1758 | reference | reference |
| Unintended | 426 | 1618 | 2.79 (2.42-3.23) | 1.28 (1.06-1.54) |
| Mis-timed | 371 | 1361 | 2.68 (2.30-3.12) | 1.22 (1.01-1.47) |
| Unwanted | 55 | 257 | 3.82 (2.69-5.42) | 1.69 (1.12-2.55) |
| * National Survey of Family Growth sampling weights applied. | ||||
| † Adjusted for age, race, marital status, poverty level, and education. | ||||
TABLE 3
Effect of race on unintended pregnancy and breastfeeding behavior
| Weighted adjusted odds ratio of NOT breastfeeding*† | ||||
|---|---|---|---|---|
| Intendedness of pregnancy | White (n=3661) | Hispanic (n=1063) | Black (n=1646) | |
| Initiation of breastfeeding (any) | ||||
| Intended | reference | reference | reference | |
| Unintended | 1.15 (0.93-1.42) | 0.94 (0.66-1.35) | 0.81 (0.56-1.17) | |
| Mis-timed | 1.07 (0.87-1.32) | 0.93 (0.64-1.35) | 0.78 (0.53-1.15) | |
| Unwanted | 2.50 (1.54-4.05) | 0.97 (0.55-1.70) | 0.93 (0.52-1.65) | |
| Continuation of breastfeeding (16 ≥ weeks) | ||||
| Intended | reference | reference | reference | |
| Unintended | 1.39 (1.07-1.81) | 1.08 (0.74-1.58) | 0.73 (0.44-1.20) | |
| Mis-timed | 1.29 (0.99-1.68) | 1.10 (0.76-1.60) | 0.70 (0.41-1.20) | |
| Unwanted | 2.56 (1.34-4.87) | 0.90 (0.47-1.72) | 0.78 (0.34-1.76) | |
| * National Survey of Family Growth sampling weights applied. | ||||
| † Adjusted for age, marital status, poverty level, and education. | ||||
Discussion
In this study of first-time US mothers, women who breastfed were demographically different from those who did not, but had relatively similar maternal behaviors and infant characteristics. After controlling for these demographic differences, having an unwanted pregnancy was associated with a lower likelihood of both initiating breastfeeding and continuing to breastfeed. In addition, race was an important effect modifier for unwanted pregnancies.
The demographic findings of this study are consistent with the current breastfeeding literature: US women who breastfeed tend to be older, white, married, well-educated, and of a higher socioeconomic status than those who do not.9 The main findings of this study are also consistent with the only other study that has examined the relationship between unintended pregnancy and breastfeeding behavior.10 A cross-sectional sample of 27,700 women who gave birth to a live baby were asked prior to postpartum discharge whether they had intended to become pregnant and their plans for breastfeeding. After controlling for education, race, Medicaid status, maternal age younger than 20, and any tobacco use during pregnancy, the authors found that women whose pregnancies were unintended were more likely not to initiate breastfeeding or to breastfeed exclusively. Adjusted odds ratios of not breastfeeding ranged from 1.10 to 1.41, depending on intention status, and all were statistically significant. In contrast to our study, a major limitation of that study was that the measured outcome was intent to breastfeed at hospital discharge, which may have differed greatly from actual breastfeeding behavior.
The interaction seen in our analysis between intention status and race is initially surprising because, in general, white and Hispanic women breastfeed at much higher rates than black women. But if a pregnancy was unwanted, white women were much less likely to breastfeed than either black or Hispanic women. Neither socioeconomic status nor educational level is the explanation, as both of these factors were controlled for in stratified analyses. Perhaps Hispanic and black women are more accepting of unintended pregnancy than white women and these results reflect cultural differences. Further studies which examine other aspects of unintended pregnancy with respect to race will help to further clarify the reasons for this finding.
Strengths and limitations
Our population-based study has several strengths. The data set provides a large national sample with excellent representation of minority women; statistical oversampling and weighting allow these data to reflect the entire national population. Adjustment of data for nonresponse lessens the risk of selection bias. Furthermore, the study sample was restricted to first births to limit the effect of previous birth experiences on postpartum behaviors. Therefore our results are generalizable to all first-time mothers in the United States.
A major limitation of our study is that information was not collected on several factors, such as substance use both during pregnancy and after birth, that might influence the relationship between pregnancy intention status and breastfeeding behavior. The work of Dye and colleagues,10 discussed above, found that prenatal tobacco, but not alcohol or drug use, was a significant confounder. Information was also not available on health service–related factors that may contribute to breastfeeding success, such as breastfeeding in the delivery room, length of hospital stay, and participation in educational programs.11
Given that data were collected for the NSFG during personal interviews at differing lengths of time after a pregnancy, inaccuracy is possible. Although the survey does not include corroboration from other sources, such as medical records or birth certificates, it is reassuring that, as an example, rates of prenatal care in our study are similar to those of other nationally reported rates for 1995 (98.1% in our study and 98.8% in National Vital Statistics Reports).12 Potential misclassification with respect to such medical outcomes as prematurity would be nondifferential and only bias odds ratios toward the null. The extended time between conception and measurement of maternal attitudes increases the uncertainty that a mother will accurately recall both her pregnancy intentions at conception and her breastfeeding practices. Women are more likely to recall a pregnancy carried to birth as intended, but this phenomenon would only bias the results if it also applied to breastfeeding practices, which is unlikely.13 While breastfeeding practices may not be exactly recalled, there is no obvious reason for differential reporting.
Conclusions
Our study has clinical implications for first-time US mothers. A recent national goal of the Institute of Medicine is that all pregnancies be planned.3 One of the many benefits of decreasing unintended pregnancy may be to increase breastfeeding rates closer to the Healthy People 2010 goals. In addition, a new hypothesis is suggested by the results of this study: Clinicians should promote breastfeeding differently for women with intended and unintended pregnancies. Future research will evaluate the importance of incorporating pregnancy intention status into patient-centered counseling. In the interim, women with unwanted pregnancies, especially white women, should be targeted for counseling, as they could benefit from breastfeeding, not just for medical reasons but for psychological and economic ones as well.
Acknowledgments
We would like to thank Larry Culpepper, MD, MPH, for his guidance.
1. Forrest JD. Unintended pregnancy among American women. Fam Plann Perspect 1987;19:76-7.
2. Henshaw SK. Unintended pregnancy in the United States. Fam Plann Perspectives 1998;30:24-9,46.-
3. Institute of Medicine Committee on Unintended Pregnancy. The best intentions: unintended pregnancy and the well-being of children and families. Washington, DC: National Academy Press, 1995.
4. Orr ST, Miller CA. Unintended pregnancy and the psychosocial well-being of pregnant women. Womens Health Issues 1997;7:38-46.
5. Institute of Medicine Subcommittee on Nutrition during Lactation. Nutrition during lactation. Washington, DC: National Academy Press, 1991.
6. American Academy of Pediatrics, Work Group on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 1997;100:1035-9.
7. US Department of Health and Human Services. Healthy People 2010. 2nd ed. With understanding and improving health and objectives for improving health. 2 vols. Washington, DC: US Government Printing Office, November 2000.
8. Abma JC, Chandra A, Mosher WD, Peterson LS, Piccinino LJ. Fertility, family planning, and women’s health: new data from the 1995 National Survey of Family Growth. Vital Health Stat 1997;23.19:1-114.
9. Scott JA, Binns CW. Factors associated with the initiation and duration of breastfeeding: a review of the literature. Breastfeed Rev 1999;7:5-16.
10. Dye TD, Wojtowycz MA, Aubry RH, Quade J, Kilburn H. Unintended pregnancy and breastfeeding behavior. Am J Public Health 1997;87:1709-11.
11. Kuan LW, Britto M, Decolongon J, Schoettker PJ, Atherton HD, Kotagal UR. Health system factors contributing to breastfeeding success. Pediatrics 1999;104:e28.-
12. Ventura SJ, Martin JA, Curtin SC, Mathews TJ. Births: final data for 1997. Natl Vital Stat Reports 1999;47.18:1-96.
13. Petersen R, Moos MK. Defining and measuring unintended pregnancy: issues and concerns. Womens Health Issues 1997;7:234-40.
OBJECTIVE: To examine the association between unintended pregnancy and the initiation and duration of breastfeeding.
STUDY DESIGN: This was a secondary data analysis of the 1995 Cycle 5 of the National Survey of Family Growth.
POPULATION: We studied 6733 first singleton live births to US women aged 15 years to 44 years.
OUTCOMES MEASURED: Using the 1995 Institute of Medicine definitions, pregnancies were classified as intended or unintended; unintended pregnancies were further categorized as either mis-timed or unwanted. We measured initiation of breastfeeding and duration of nonexclusive breastfeeding for at least 16 weeks.
RESULTS: In this study, 51.5% of women never breastfed, 48.5% initiated breastfeeding, and 26.4% of all women continued breastfeeding for at least 16 weeks. US women with unwanted unintended pregnancies were more likely not to initiate breastfeeding (odds ratio [OR] = 1.76; 95% confidence interval [CI], 1.26-2.44) and more likely not to continue breastfeeding (OR =1.69; 95% CI, 1.12-2.55) than women with intended pregnancies. White women with unwanted unintended pregnancies were more likely not to breastfeed than those with intended ones (initiation: OR = 2.50; 95% CI, 1.54-4.05; continuation: OR = 2.56; 95% CI, 1.34-4.87). This finding was not seen for black or Hispanic women.
CONCLUSIONS: In the United States, women with unwanted pregnancies were less likely either to initiate or to continue breastfeeding than women with intended pregnancies. A strong inverse association between unwanted pregnancies and breastfeeding was observed only for white women. Education for women with unintended pregnancies may improve breastfeeding rates and subsequently, the health of women and infants.
- In the United States, women whose pregnancies were unwanted are at a higher risk of not breastfeeding than women whose pregnancies were intended.
- Future research to evaluate the importance of incorporating pregnancy intention status into patient-centered breastfeeding promotion is needed.
- For now, women with unwanted pregnancies, especially white women, should be targeted for breastfeeding counseling.
Unintended pregnancy is a significant public health issue. More than half of all pregnancies are unintended at the time of conception; approximately half of those end as births and half as induced abortions.1 Forty-eight percent of women have at least one unplanned pregnancy, and 28% of women have at least one unplanned birth during their reproductive lifetime.2 Unintended pregnancies and births are associated with numerous harmful behaviors and adverse outcomes.3,4
Breastfeeding is currently promoted as the preferred method of feeding for infants for at least 1 year because of its multiple immediate and long-term benefits for both mother and child.5,6 Yet in 1998 only 64% of US mothers were breastfeeding at the time of hospital discharge and 29% at 6 months postpartum, which is well below the Healthy People 2010 goals of 75% and 50%, respectively, for those intervals.7
We hypothesized that women with unintended pregnancies are less likely to breastfeed their infants than those with intended ones. We quantified the association between the intendedness of pregnancy at the time of conception and breastfeeding behavior, both the initiation of any breastfeeding and the continuation of nonexclusive breastfeeding for at least 16 weeks, for first singleton births to US mothers. We then explored other factors which might affect breastfeeding practices.
Methods
Study design
This study is a secondary data analysis of the 1995 Cycle 5 of the National Survey of Family Growth (NSFG), a periodic population-based survey conducted by the National Center for Health Statistics and the Centers for Disease Control which focuses on women’s health and pregnancy. A national probability sample of 14,000 civilian noninstitutionalized women aged 15 years to 44 years was selected from among households that responded to the 1993 National Health Interview Survey, with an oversampling of minority women. Personal interviews were conducted between January and October of 1995 with 10,847 of these women. The data were then adjusted for a response rate of 79% and weighted so that findings would reflect the US population as a whole. Full details of the NSFG survey methods are described elsewhere.8
The data set contains information on 21,332 pregnancies and 14,958 live births (Figure). After excluding multiple gestations (n=154), subsequent births to the same mother (n=7930), and neonatal adoptions or deaths (n=141), the final sample contained 6733 first singleton live births. To study the initiation of breastfeeding, women who breastfed at all were compared with those who did not. To study duration of breastfeeding, women who breastfed for 16 or more weeks were compared with those who did not. In this second set of analyses, the 1459 women who breastfed for between 0 and 16 weeks and the 33 women who were breastfeeding at the time of the interview and whose children had been born within 16 weeks of that date were excluded.
FIGURE
Study sample
Variable definitions
Pregnancies were categorized as either intended or unintended at conception, using new definitions established by the Institute of Medicine in 1995.3 Pregnancies were considered intended if a woman had stopped using birth control because she wanted to become pregnant. Unintended pregnancies were classified into 1 of 2 categories: (1) mis-timed: wanted pregnancies that occurred sooner than desired, or (2) unwanted: pregnancies that occurred while a woman was using contraception and had not ever wanted to have a(nother) baby. The 170 women who described their pregnancy intention status as “didn’t know” or “didn’t care” were excluded from analyses involving intention status as defined above. There were 2 breastfeeding outcomes in this study: (1) initiation of breastfeeding, including women who reported any breastfeeding at all, and (2) duration of non-exclusive breastfeeding for at least 16 weeks.
Maternal demographics, intrapartum and postpartum behaviors, and birth outcomes were considered as potential confounders. As missing data were imputed in the public use data file, information on each variable was complete, except where noted below. Maternal age was determined at the time of conception. Education was defined as completed years of schooling at the time of the interview. Race was categorized as white, black, Hispanic, or other. Marital status was defined as either married or not married. Socioeconomic status was measured continuously as a percentage of the 1995 poverty level. Information on prenatal care was only available for births in the last 5 years (n=1266). For the 1241 women who reported that they had received prenatal care, the mean weeks of gestation at the time of the first prenatal visit were calculated. Maternity leave was defined as the use of maternity leave, paid or unpaid, for women who were working during the pregnancy (n=3662). For those who took any leave, the mean length of that leave was calculated in weeks. The 33 women for whom data were not available and the 5 women who answered that they took 0 weeks of maternity leave were not included in this calculation. Infant variables were considered categorically: mode of delivery, either vaginal or cesarean; prematurity, birth at less than or equal to 36 weeks; and low birth weight, less than or equal to 5.5 pounds.
Statistical analysis
The statistical significance of descriptive variables was determined using 2-sample t tests and chi-square tests, with women who did not breastfeed at all as the comparison group.
To compare our results with existing literature, we calculated crude odds ratios of not breastfeeding and used chi-square tests to assess the statistical significance of these associations. The reference group was always women whose pregnancies were intended. Variables identified as potential confounders were age, race, marital status, poverty level, education, maternity leave, mode of delivery, prematurity, and low birth weight. Final logistic regression models were adjusted for those variables that changed crude odds ratios by 10% or more: age, race, marital status, poverty level, and education. Adjusted odds ratios (ORs) of not breastfeeding and 95% confidence intervals (CIs) are reported.
Effect modification was assessed by dichotomizing each of the 5 confounding variables in the following manner: teen versus 20 years or older; white versus black versus Hispanic (here, the 193 women in the sample who defined their race as other were not included); married versus unmarried; high school education or higher versus less than a high school education; and below the poverty level versus at or above the poverty level. Each stratified analysis was adjusted for the other 4 factors. Interaction terms were created and P values for heterogeneity were calculated for all logistic models. For race, an additional interaction term was created to compare white with non-white (black and Hispanic combined) women.
These data are contained on the National Survey of Family Growth Cycle 5 1995 CD-ROM, Series 23, No. 3 and were exported using SETS version 1.22a (National Center for Health Statistics, Hyattsville, MD). All analyses were performed with SAS version 6.12 (SAS Institute, Cary, NC). Odds ratios are weighted using sampling weights provided in the data set. SUDAAN version 7.5.3 was used to obtain standard errors (Research Triangle Institute, Research Triangle Park, NC).
Results
In the total sample of 6733 first singleton live births to US mothers, 3267 (48.5%) of women initiated breastfeeding, compared with 3466 (51.5%) who did not. In the entire sample, 1775 (26.4%) continued to breastfeed nonexclusively for at least 16 weeks.
The breastfeeding initiation rate was 55.9%, 37.4%, and 28.0% for women with intended, mis-timed, and unwanted pregnancies, respectively. By 16 weeks, 32.6%, 17.0%, and 15.5% of women, respectively, were still breastfeeding. For all women who breastfed, the mean number of weeks of breastfeeding was 24.4 (standard deviation = 24.9; range = < 1 week to 4.0 years). Only 3.9% of women who breastfed did so for more than 2 years.
Table 1 shows characteristics of mothers and infants by breastfeeding behavior. Women who breastfed, both initially and for at least 16 weeks, were older at conception and had had more years of education than women who did not breastfeed at all. They were more likely to be white and less likely to be black. A similar percentage of women in each group were Hispanic. Percentage of the poverty level, a proxy for socioeconomic status, was higher for those who breastfed at all, but similar for those who continued breastfeeding and those who did not breastfeed. Rates of prenatal care and mean weeks at first prenatal visit were similar in all groups. Among women who were employed during their pregnancies, almost two thirds took maternity leave, regardless of breastfeeding behavior. Mean length of maternity leave was 3.4 weeks longer among women who continued to breastfeed than among women who did not breastfeed at all. The percentage of vaginal deliveries was similar among groups. Both premature and low birth weight infants were more common among women who did not breastfeed.
The association between the intendedness of pregnancy and breastfeeding behavior is reported in Table 2. Crude odds ratios show that women with any type of unintended pregnancy were more likely not to initiate breastfeeding than women whose pregnancies were intended. Some, but not all, of this association can be attributed to confounding by demographic factors. Having an unintended pregnancy was not associated with any significant difference in the initiation of breastfeeding, after adjusting for age, race, marital status, poverty level, and education. While women with mis-timed pregnancies were as likely to initiate breastfeeding as those whose pregnancies were intended (OR = 1.03; 95% CI, 0.88-1.21), women with unwanted pregnancies were more likely not to start breastfeeding (OR = 1.76; 95% CI, 1.26-2.44).
Table 2 also describes the association between pregnancy intention status and the continuation of nonexclusive breastfeeding for at least 16 weeks. In contrast to the initiation of breastfeeding, duration of breastfeeding was affected by the intendedness of pregnancy in every comparison. Adjusted odds ratios show that women with either type of unintended pregnancy were more likely not to continue breastfeeding than those with intended ones (OR = 1.28; 95% CI, 1.06-1.54). As with breastfeeding initiation, this association is being driven by the unwanted pregnancies. Women with unwanted pregnancies were more likely not to continue breastfeeding (OR = 1.69; 95% CI, 1.12-2.55).
Each of these associations was then evaluated for effect modification. As seen in Table 3, only race was an important factor. In the total sample, 56.3% of white women, 55.4% of Hispanic women, and 24.7% of black women breastfed at all; and 41.6%, 41.2%, and 12.6% of white, Hispanic, and black women breastfed for at least 16 weeks. White women with unwanted pregnancies were more likely not to initiate breastfeeding (OR = 2.50; 95% CI, 1.54-4.05) and more likely not to continue breastfeeding (OR = 2.56; 95% CI, 1.34-4.87) than white women with intended pregnancies. These differences in breastfeeding behaviors for unwanted pregnancies were not seen for either Hispanic or black women. For each stratified analysis, a single P value for heterogeneity was calculated to compare white women with non-white women (Hispanic and black women combined). The only significant difference by race was for unwanted pregnancies. The P value for heterogeneity was 0.01 for both initiation and continuation of breastfeeding. Stratified analyses for age, marital status, education, poverty level, and year of birth showed similar odds ratios across strata and nonsignificant P values for heterogeneity in every case (analyses not shown).
TABLE 1
Characteristics of mothers and infants by breastfeeding status (n=6733)
| Characteristic | Any breastfeeding (n = 3267) | Breastfeeding for ≥ 16 weeks (n = 1775) | No breastfeeding (n = 3466) |
|---|---|---|---|
| Age (mean years, SD) | 23.5 (5.0)* | 24.0 (5.1)* | 20.5 (4.3) |
| Race (%) | |||
| White | 64.8* | 65.9* | 47.4 |
| Black | 12.8 | 10.3 | 36.6 |
| Hispanic | 18.4 | 19.1 | 14.0 |
| Other | 4.0 | 4.7 | 2.0 |
| Married (%) | 65.0* | 68.8* | 37.3 |
| Percentage of the 1995 poverty level (SD) | 320 (207)* | 235 (205)* | 246 (189) |
| Education (mean years, SD) | 13.1 (3.0)* | 13.3 (3.2)* | 11.9 (2.3) |
| Prenatal care (%)† | 98.5 | 97.4 | 97.6 |
| Mean weeks at 1st visit (SD) | 7.8 (3.9) | 7.8 (4.0) | 9.1 (5.4) |
| Maternity leave ‡ | 65.2 | 60.7 | 64.6 |
| Mean weeks (SD) | 12.2 (9.4) | 13.8 (10.8) | 10.4 (8.3) |
| Vaginal delivery (%) | 78.5 | 78.9 | 80.7 |
| Prematurity (%) | 7.4* | 6.4* | 9.9 |
| Low birth weight (%) | 4.8* | 3.9* | 9.4 |
| SD denotes standard deviation. | |||
| *P ≤ .001 in comparison with women who did not breastfeed. | |||
| † For births during 1990-1994, n=1266. | |||
| ‡ Percentage of women employed during that pregnancy, n=3662. | |||
TABLE 2
Unintended pregnancy and breastfeeding behavior in the United States
| Intendedness of pregnancy | Number breastfeeding | Number not breastfeeding | Weighted crude odds ratio of NOT breastfeeding (95% CI)* | Weighted adjusted odds ratio of NOT breastfeeding (95% CI)* † |
|---|---|---|---|---|
| Initiation of breastfeeding (any) | ||||
| Intended | 2263 | 1758 | reference | reference |
| Unintended | 924 | 1618 | 2.15 (1.91-2.43) | 1.09 (0.93-1.28) |
| Mis-timed | 822 | 1361 | 2.02 (1.79-2.29) | 1.03 (0.88-1.21) |
| Unwanted | 102 | 257 | 3.54 (2.69-4.66) | 1.76 (1.26-2.44) |
| Continuation of breastfeeding (16 ≥ weeks) | ||||
| Intended | 1304 | 1758 | reference | reference |
| Unintended | 426 | 1618 | 2.79 (2.42-3.23) | 1.28 (1.06-1.54) |
| Mis-timed | 371 | 1361 | 2.68 (2.30-3.12) | 1.22 (1.01-1.47) |
| Unwanted | 55 | 257 | 3.82 (2.69-5.42) | 1.69 (1.12-2.55) |
| * National Survey of Family Growth sampling weights applied. | ||||
| † Adjusted for age, race, marital status, poverty level, and education. | ||||
TABLE 3
Effect of race on unintended pregnancy and breastfeeding behavior
| Weighted adjusted odds ratio of NOT breastfeeding*† | ||||
|---|---|---|---|---|
| Intendedness of pregnancy | White (n=3661) | Hispanic (n=1063) | Black (n=1646) | |
| Initiation of breastfeeding (any) | ||||
| Intended | reference | reference | reference | |
| Unintended | 1.15 (0.93-1.42) | 0.94 (0.66-1.35) | 0.81 (0.56-1.17) | |
| Mis-timed | 1.07 (0.87-1.32) | 0.93 (0.64-1.35) | 0.78 (0.53-1.15) | |
| Unwanted | 2.50 (1.54-4.05) | 0.97 (0.55-1.70) | 0.93 (0.52-1.65) | |
| Continuation of breastfeeding (16 ≥ weeks) | ||||
| Intended | reference | reference | reference | |
| Unintended | 1.39 (1.07-1.81) | 1.08 (0.74-1.58) | 0.73 (0.44-1.20) | |
| Mis-timed | 1.29 (0.99-1.68) | 1.10 (0.76-1.60) | 0.70 (0.41-1.20) | |
| Unwanted | 2.56 (1.34-4.87) | 0.90 (0.47-1.72) | 0.78 (0.34-1.76) | |
| * National Survey of Family Growth sampling weights applied. | ||||
| † Adjusted for age, marital status, poverty level, and education. | ||||
Discussion
In this study of first-time US mothers, women who breastfed were demographically different from those who did not, but had relatively similar maternal behaviors and infant characteristics. After controlling for these demographic differences, having an unwanted pregnancy was associated with a lower likelihood of both initiating breastfeeding and continuing to breastfeed. In addition, race was an important effect modifier for unwanted pregnancies.
The demographic findings of this study are consistent with the current breastfeeding literature: US women who breastfeed tend to be older, white, married, well-educated, and of a higher socioeconomic status than those who do not.9 The main findings of this study are also consistent with the only other study that has examined the relationship between unintended pregnancy and breastfeeding behavior.10 A cross-sectional sample of 27,700 women who gave birth to a live baby were asked prior to postpartum discharge whether they had intended to become pregnant and their plans for breastfeeding. After controlling for education, race, Medicaid status, maternal age younger than 20, and any tobacco use during pregnancy, the authors found that women whose pregnancies were unintended were more likely not to initiate breastfeeding or to breastfeed exclusively. Adjusted odds ratios of not breastfeeding ranged from 1.10 to 1.41, depending on intention status, and all were statistically significant. In contrast to our study, a major limitation of that study was that the measured outcome was intent to breastfeed at hospital discharge, which may have differed greatly from actual breastfeeding behavior.
The interaction seen in our analysis between intention status and race is initially surprising because, in general, white and Hispanic women breastfeed at much higher rates than black women. But if a pregnancy was unwanted, white women were much less likely to breastfeed than either black or Hispanic women. Neither socioeconomic status nor educational level is the explanation, as both of these factors were controlled for in stratified analyses. Perhaps Hispanic and black women are more accepting of unintended pregnancy than white women and these results reflect cultural differences. Further studies which examine other aspects of unintended pregnancy with respect to race will help to further clarify the reasons for this finding.
Strengths and limitations
Our population-based study has several strengths. The data set provides a large national sample with excellent representation of minority women; statistical oversampling and weighting allow these data to reflect the entire national population. Adjustment of data for nonresponse lessens the risk of selection bias. Furthermore, the study sample was restricted to first births to limit the effect of previous birth experiences on postpartum behaviors. Therefore our results are generalizable to all first-time mothers in the United States.
A major limitation of our study is that information was not collected on several factors, such as substance use both during pregnancy and after birth, that might influence the relationship between pregnancy intention status and breastfeeding behavior. The work of Dye and colleagues,10 discussed above, found that prenatal tobacco, but not alcohol or drug use, was a significant confounder. Information was also not available on health service–related factors that may contribute to breastfeeding success, such as breastfeeding in the delivery room, length of hospital stay, and participation in educational programs.11
Given that data were collected for the NSFG during personal interviews at differing lengths of time after a pregnancy, inaccuracy is possible. Although the survey does not include corroboration from other sources, such as medical records or birth certificates, it is reassuring that, as an example, rates of prenatal care in our study are similar to those of other nationally reported rates for 1995 (98.1% in our study and 98.8% in National Vital Statistics Reports).12 Potential misclassification with respect to such medical outcomes as prematurity would be nondifferential and only bias odds ratios toward the null. The extended time between conception and measurement of maternal attitudes increases the uncertainty that a mother will accurately recall both her pregnancy intentions at conception and her breastfeeding practices. Women are more likely to recall a pregnancy carried to birth as intended, but this phenomenon would only bias the results if it also applied to breastfeeding practices, which is unlikely.13 While breastfeeding practices may not be exactly recalled, there is no obvious reason for differential reporting.
Conclusions
Our study has clinical implications for first-time US mothers. A recent national goal of the Institute of Medicine is that all pregnancies be planned.3 One of the many benefits of decreasing unintended pregnancy may be to increase breastfeeding rates closer to the Healthy People 2010 goals. In addition, a new hypothesis is suggested by the results of this study: Clinicians should promote breastfeeding differently for women with intended and unintended pregnancies. Future research will evaluate the importance of incorporating pregnancy intention status into patient-centered counseling. In the interim, women with unwanted pregnancies, especially white women, should be targeted for counseling, as they could benefit from breastfeeding, not just for medical reasons but for psychological and economic ones as well.
Acknowledgments
We would like to thank Larry Culpepper, MD, MPH, for his guidance.
OBJECTIVE: To examine the association between unintended pregnancy and the initiation and duration of breastfeeding.
STUDY DESIGN: This was a secondary data analysis of the 1995 Cycle 5 of the National Survey of Family Growth.
POPULATION: We studied 6733 first singleton live births to US women aged 15 years to 44 years.
OUTCOMES MEASURED: Using the 1995 Institute of Medicine definitions, pregnancies were classified as intended or unintended; unintended pregnancies were further categorized as either mis-timed or unwanted. We measured initiation of breastfeeding and duration of nonexclusive breastfeeding for at least 16 weeks.
RESULTS: In this study, 51.5% of women never breastfed, 48.5% initiated breastfeeding, and 26.4% of all women continued breastfeeding for at least 16 weeks. US women with unwanted unintended pregnancies were more likely not to initiate breastfeeding (odds ratio [OR] = 1.76; 95% confidence interval [CI], 1.26-2.44) and more likely not to continue breastfeeding (OR =1.69; 95% CI, 1.12-2.55) than women with intended pregnancies. White women with unwanted unintended pregnancies were more likely not to breastfeed than those with intended ones (initiation: OR = 2.50; 95% CI, 1.54-4.05; continuation: OR = 2.56; 95% CI, 1.34-4.87). This finding was not seen for black or Hispanic women.
CONCLUSIONS: In the United States, women with unwanted pregnancies were less likely either to initiate or to continue breastfeeding than women with intended pregnancies. A strong inverse association between unwanted pregnancies and breastfeeding was observed only for white women. Education for women with unintended pregnancies may improve breastfeeding rates and subsequently, the health of women and infants.
- In the United States, women whose pregnancies were unwanted are at a higher risk of not breastfeeding than women whose pregnancies were intended.
- Future research to evaluate the importance of incorporating pregnancy intention status into patient-centered breastfeeding promotion is needed.
- For now, women with unwanted pregnancies, especially white women, should be targeted for breastfeeding counseling.
Unintended pregnancy is a significant public health issue. More than half of all pregnancies are unintended at the time of conception; approximately half of those end as births and half as induced abortions.1 Forty-eight percent of women have at least one unplanned pregnancy, and 28% of women have at least one unplanned birth during their reproductive lifetime.2 Unintended pregnancies and births are associated with numerous harmful behaviors and adverse outcomes.3,4
Breastfeeding is currently promoted as the preferred method of feeding for infants for at least 1 year because of its multiple immediate and long-term benefits for both mother and child.5,6 Yet in 1998 only 64% of US mothers were breastfeeding at the time of hospital discharge and 29% at 6 months postpartum, which is well below the Healthy People 2010 goals of 75% and 50%, respectively, for those intervals.7
We hypothesized that women with unintended pregnancies are less likely to breastfeed their infants than those with intended ones. We quantified the association between the intendedness of pregnancy at the time of conception and breastfeeding behavior, both the initiation of any breastfeeding and the continuation of nonexclusive breastfeeding for at least 16 weeks, for first singleton births to US mothers. We then explored other factors which might affect breastfeeding practices.
Methods
Study design
This study is a secondary data analysis of the 1995 Cycle 5 of the National Survey of Family Growth (NSFG), a periodic population-based survey conducted by the National Center for Health Statistics and the Centers for Disease Control which focuses on women’s health and pregnancy. A national probability sample of 14,000 civilian noninstitutionalized women aged 15 years to 44 years was selected from among households that responded to the 1993 National Health Interview Survey, with an oversampling of minority women. Personal interviews were conducted between January and October of 1995 with 10,847 of these women. The data were then adjusted for a response rate of 79% and weighted so that findings would reflect the US population as a whole. Full details of the NSFG survey methods are described elsewhere.8
The data set contains information on 21,332 pregnancies and 14,958 live births (Figure). After excluding multiple gestations (n=154), subsequent births to the same mother (n=7930), and neonatal adoptions or deaths (n=141), the final sample contained 6733 first singleton live births. To study the initiation of breastfeeding, women who breastfed at all were compared with those who did not. To study duration of breastfeeding, women who breastfed for 16 or more weeks were compared with those who did not. In this second set of analyses, the 1459 women who breastfed for between 0 and 16 weeks and the 33 women who were breastfeeding at the time of the interview and whose children had been born within 16 weeks of that date were excluded.
FIGURE
Study sample
Variable definitions
Pregnancies were categorized as either intended or unintended at conception, using new definitions established by the Institute of Medicine in 1995.3 Pregnancies were considered intended if a woman had stopped using birth control because she wanted to become pregnant. Unintended pregnancies were classified into 1 of 2 categories: (1) mis-timed: wanted pregnancies that occurred sooner than desired, or (2) unwanted: pregnancies that occurred while a woman was using contraception and had not ever wanted to have a(nother) baby. The 170 women who described their pregnancy intention status as “didn’t know” or “didn’t care” were excluded from analyses involving intention status as defined above. There were 2 breastfeeding outcomes in this study: (1) initiation of breastfeeding, including women who reported any breastfeeding at all, and (2) duration of non-exclusive breastfeeding for at least 16 weeks.
Maternal demographics, intrapartum and postpartum behaviors, and birth outcomes were considered as potential confounders. As missing data were imputed in the public use data file, information on each variable was complete, except where noted below. Maternal age was determined at the time of conception. Education was defined as completed years of schooling at the time of the interview. Race was categorized as white, black, Hispanic, or other. Marital status was defined as either married or not married. Socioeconomic status was measured continuously as a percentage of the 1995 poverty level. Information on prenatal care was only available for births in the last 5 years (n=1266). For the 1241 women who reported that they had received prenatal care, the mean weeks of gestation at the time of the first prenatal visit were calculated. Maternity leave was defined as the use of maternity leave, paid or unpaid, for women who were working during the pregnancy (n=3662). For those who took any leave, the mean length of that leave was calculated in weeks. The 33 women for whom data were not available and the 5 women who answered that they took 0 weeks of maternity leave were not included in this calculation. Infant variables were considered categorically: mode of delivery, either vaginal or cesarean; prematurity, birth at less than or equal to 36 weeks; and low birth weight, less than or equal to 5.5 pounds.
Statistical analysis
The statistical significance of descriptive variables was determined using 2-sample t tests and chi-square tests, with women who did not breastfeed at all as the comparison group.
To compare our results with existing literature, we calculated crude odds ratios of not breastfeeding and used chi-square tests to assess the statistical significance of these associations. The reference group was always women whose pregnancies were intended. Variables identified as potential confounders were age, race, marital status, poverty level, education, maternity leave, mode of delivery, prematurity, and low birth weight. Final logistic regression models were adjusted for those variables that changed crude odds ratios by 10% or more: age, race, marital status, poverty level, and education. Adjusted odds ratios (ORs) of not breastfeeding and 95% confidence intervals (CIs) are reported.
Effect modification was assessed by dichotomizing each of the 5 confounding variables in the following manner: teen versus 20 years or older; white versus black versus Hispanic (here, the 193 women in the sample who defined their race as other were not included); married versus unmarried; high school education or higher versus less than a high school education; and below the poverty level versus at or above the poverty level. Each stratified analysis was adjusted for the other 4 factors. Interaction terms were created and P values for heterogeneity were calculated for all logistic models. For race, an additional interaction term was created to compare white with non-white (black and Hispanic combined) women.
These data are contained on the National Survey of Family Growth Cycle 5 1995 CD-ROM, Series 23, No. 3 and were exported using SETS version 1.22a (National Center for Health Statistics, Hyattsville, MD). All analyses were performed with SAS version 6.12 (SAS Institute, Cary, NC). Odds ratios are weighted using sampling weights provided in the data set. SUDAAN version 7.5.3 was used to obtain standard errors (Research Triangle Institute, Research Triangle Park, NC).
Results
In the total sample of 6733 first singleton live births to US mothers, 3267 (48.5%) of women initiated breastfeeding, compared with 3466 (51.5%) who did not. In the entire sample, 1775 (26.4%) continued to breastfeed nonexclusively for at least 16 weeks.
The breastfeeding initiation rate was 55.9%, 37.4%, and 28.0% for women with intended, mis-timed, and unwanted pregnancies, respectively. By 16 weeks, 32.6%, 17.0%, and 15.5% of women, respectively, were still breastfeeding. For all women who breastfed, the mean number of weeks of breastfeeding was 24.4 (standard deviation = 24.9; range = < 1 week to 4.0 years). Only 3.9% of women who breastfed did so for more than 2 years.
Table 1 shows characteristics of mothers and infants by breastfeeding behavior. Women who breastfed, both initially and for at least 16 weeks, were older at conception and had had more years of education than women who did not breastfeed at all. They were more likely to be white and less likely to be black. A similar percentage of women in each group were Hispanic. Percentage of the poverty level, a proxy for socioeconomic status, was higher for those who breastfed at all, but similar for those who continued breastfeeding and those who did not breastfeed. Rates of prenatal care and mean weeks at first prenatal visit were similar in all groups. Among women who were employed during their pregnancies, almost two thirds took maternity leave, regardless of breastfeeding behavior. Mean length of maternity leave was 3.4 weeks longer among women who continued to breastfeed than among women who did not breastfeed at all. The percentage of vaginal deliveries was similar among groups. Both premature and low birth weight infants were more common among women who did not breastfeed.
The association between the intendedness of pregnancy and breastfeeding behavior is reported in Table 2. Crude odds ratios show that women with any type of unintended pregnancy were more likely not to initiate breastfeeding than women whose pregnancies were intended. Some, but not all, of this association can be attributed to confounding by demographic factors. Having an unintended pregnancy was not associated with any significant difference in the initiation of breastfeeding, after adjusting for age, race, marital status, poverty level, and education. While women with mis-timed pregnancies were as likely to initiate breastfeeding as those whose pregnancies were intended (OR = 1.03; 95% CI, 0.88-1.21), women with unwanted pregnancies were more likely not to start breastfeeding (OR = 1.76; 95% CI, 1.26-2.44).
Table 2 also describes the association between pregnancy intention status and the continuation of nonexclusive breastfeeding for at least 16 weeks. In contrast to the initiation of breastfeeding, duration of breastfeeding was affected by the intendedness of pregnancy in every comparison. Adjusted odds ratios show that women with either type of unintended pregnancy were more likely not to continue breastfeeding than those with intended ones (OR = 1.28; 95% CI, 1.06-1.54). As with breastfeeding initiation, this association is being driven by the unwanted pregnancies. Women with unwanted pregnancies were more likely not to continue breastfeeding (OR = 1.69; 95% CI, 1.12-2.55).
Each of these associations was then evaluated for effect modification. As seen in Table 3, only race was an important factor. In the total sample, 56.3% of white women, 55.4% of Hispanic women, and 24.7% of black women breastfed at all; and 41.6%, 41.2%, and 12.6% of white, Hispanic, and black women breastfed for at least 16 weeks. White women with unwanted pregnancies were more likely not to initiate breastfeeding (OR = 2.50; 95% CI, 1.54-4.05) and more likely not to continue breastfeeding (OR = 2.56; 95% CI, 1.34-4.87) than white women with intended pregnancies. These differences in breastfeeding behaviors for unwanted pregnancies were not seen for either Hispanic or black women. For each stratified analysis, a single P value for heterogeneity was calculated to compare white women with non-white women (Hispanic and black women combined). The only significant difference by race was for unwanted pregnancies. The P value for heterogeneity was 0.01 for both initiation and continuation of breastfeeding. Stratified analyses for age, marital status, education, poverty level, and year of birth showed similar odds ratios across strata and nonsignificant P values for heterogeneity in every case (analyses not shown).
TABLE 1
Characteristics of mothers and infants by breastfeeding status (n=6733)
| Characteristic | Any breastfeeding (n = 3267) | Breastfeeding for ≥ 16 weeks (n = 1775) | No breastfeeding (n = 3466) |
|---|---|---|---|
| Age (mean years, SD) | 23.5 (5.0)* | 24.0 (5.1)* | 20.5 (4.3) |
| Race (%) | |||
| White | 64.8* | 65.9* | 47.4 |
| Black | 12.8 | 10.3 | 36.6 |
| Hispanic | 18.4 | 19.1 | 14.0 |
| Other | 4.0 | 4.7 | 2.0 |
| Married (%) | 65.0* | 68.8* | 37.3 |
| Percentage of the 1995 poverty level (SD) | 320 (207)* | 235 (205)* | 246 (189) |
| Education (mean years, SD) | 13.1 (3.0)* | 13.3 (3.2)* | 11.9 (2.3) |
| Prenatal care (%)† | 98.5 | 97.4 | 97.6 |
| Mean weeks at 1st visit (SD) | 7.8 (3.9) | 7.8 (4.0) | 9.1 (5.4) |
| Maternity leave ‡ | 65.2 | 60.7 | 64.6 |
| Mean weeks (SD) | 12.2 (9.4) | 13.8 (10.8) | 10.4 (8.3) |
| Vaginal delivery (%) | 78.5 | 78.9 | 80.7 |
| Prematurity (%) | 7.4* | 6.4* | 9.9 |
| Low birth weight (%) | 4.8* | 3.9* | 9.4 |
| SD denotes standard deviation. | |||
| *P ≤ .001 in comparison with women who did not breastfeed. | |||
| † For births during 1990-1994, n=1266. | |||
| ‡ Percentage of women employed during that pregnancy, n=3662. | |||
TABLE 2
Unintended pregnancy and breastfeeding behavior in the United States
| Intendedness of pregnancy | Number breastfeeding | Number not breastfeeding | Weighted crude odds ratio of NOT breastfeeding (95% CI)* | Weighted adjusted odds ratio of NOT breastfeeding (95% CI)* † |
|---|---|---|---|---|
| Initiation of breastfeeding (any) | ||||
| Intended | 2263 | 1758 | reference | reference |
| Unintended | 924 | 1618 | 2.15 (1.91-2.43) | 1.09 (0.93-1.28) |
| Mis-timed | 822 | 1361 | 2.02 (1.79-2.29) | 1.03 (0.88-1.21) |
| Unwanted | 102 | 257 | 3.54 (2.69-4.66) | 1.76 (1.26-2.44) |
| Continuation of breastfeeding (16 ≥ weeks) | ||||
| Intended | 1304 | 1758 | reference | reference |
| Unintended | 426 | 1618 | 2.79 (2.42-3.23) | 1.28 (1.06-1.54) |
| Mis-timed | 371 | 1361 | 2.68 (2.30-3.12) | 1.22 (1.01-1.47) |
| Unwanted | 55 | 257 | 3.82 (2.69-5.42) | 1.69 (1.12-2.55) |
| * National Survey of Family Growth sampling weights applied. | ||||
| † Adjusted for age, race, marital status, poverty level, and education. | ||||
TABLE 3
Effect of race on unintended pregnancy and breastfeeding behavior
| Weighted adjusted odds ratio of NOT breastfeeding*† | ||||
|---|---|---|---|---|
| Intendedness of pregnancy | White (n=3661) | Hispanic (n=1063) | Black (n=1646) | |
| Initiation of breastfeeding (any) | ||||
| Intended | reference | reference | reference | |
| Unintended | 1.15 (0.93-1.42) | 0.94 (0.66-1.35) | 0.81 (0.56-1.17) | |
| Mis-timed | 1.07 (0.87-1.32) | 0.93 (0.64-1.35) | 0.78 (0.53-1.15) | |
| Unwanted | 2.50 (1.54-4.05) | 0.97 (0.55-1.70) | 0.93 (0.52-1.65) | |
| Continuation of breastfeeding (16 ≥ weeks) | ||||
| Intended | reference | reference | reference | |
| Unintended | 1.39 (1.07-1.81) | 1.08 (0.74-1.58) | 0.73 (0.44-1.20) | |
| Mis-timed | 1.29 (0.99-1.68) | 1.10 (0.76-1.60) | 0.70 (0.41-1.20) | |
| Unwanted | 2.56 (1.34-4.87) | 0.90 (0.47-1.72) | 0.78 (0.34-1.76) | |
| * National Survey of Family Growth sampling weights applied. | ||||
| † Adjusted for age, marital status, poverty level, and education. | ||||
Discussion
In this study of first-time US mothers, women who breastfed were demographically different from those who did not, but had relatively similar maternal behaviors and infant characteristics. After controlling for these demographic differences, having an unwanted pregnancy was associated with a lower likelihood of both initiating breastfeeding and continuing to breastfeed. In addition, race was an important effect modifier for unwanted pregnancies.
The demographic findings of this study are consistent with the current breastfeeding literature: US women who breastfeed tend to be older, white, married, well-educated, and of a higher socioeconomic status than those who do not.9 The main findings of this study are also consistent with the only other study that has examined the relationship between unintended pregnancy and breastfeeding behavior.10 A cross-sectional sample of 27,700 women who gave birth to a live baby were asked prior to postpartum discharge whether they had intended to become pregnant and their plans for breastfeeding. After controlling for education, race, Medicaid status, maternal age younger than 20, and any tobacco use during pregnancy, the authors found that women whose pregnancies were unintended were more likely not to initiate breastfeeding or to breastfeed exclusively. Adjusted odds ratios of not breastfeeding ranged from 1.10 to 1.41, depending on intention status, and all were statistically significant. In contrast to our study, a major limitation of that study was that the measured outcome was intent to breastfeed at hospital discharge, which may have differed greatly from actual breastfeeding behavior.
The interaction seen in our analysis between intention status and race is initially surprising because, in general, white and Hispanic women breastfeed at much higher rates than black women. But if a pregnancy was unwanted, white women were much less likely to breastfeed than either black or Hispanic women. Neither socioeconomic status nor educational level is the explanation, as both of these factors were controlled for in stratified analyses. Perhaps Hispanic and black women are more accepting of unintended pregnancy than white women and these results reflect cultural differences. Further studies which examine other aspects of unintended pregnancy with respect to race will help to further clarify the reasons for this finding.
Strengths and limitations
Our population-based study has several strengths. The data set provides a large national sample with excellent representation of minority women; statistical oversampling and weighting allow these data to reflect the entire national population. Adjustment of data for nonresponse lessens the risk of selection bias. Furthermore, the study sample was restricted to first births to limit the effect of previous birth experiences on postpartum behaviors. Therefore our results are generalizable to all first-time mothers in the United States.
A major limitation of our study is that information was not collected on several factors, such as substance use both during pregnancy and after birth, that might influence the relationship between pregnancy intention status and breastfeeding behavior. The work of Dye and colleagues,10 discussed above, found that prenatal tobacco, but not alcohol or drug use, was a significant confounder. Information was also not available on health service–related factors that may contribute to breastfeeding success, such as breastfeeding in the delivery room, length of hospital stay, and participation in educational programs.11
Given that data were collected for the NSFG during personal interviews at differing lengths of time after a pregnancy, inaccuracy is possible. Although the survey does not include corroboration from other sources, such as medical records or birth certificates, it is reassuring that, as an example, rates of prenatal care in our study are similar to those of other nationally reported rates for 1995 (98.1% in our study and 98.8% in National Vital Statistics Reports).12 Potential misclassification with respect to such medical outcomes as prematurity would be nondifferential and only bias odds ratios toward the null. The extended time between conception and measurement of maternal attitudes increases the uncertainty that a mother will accurately recall both her pregnancy intentions at conception and her breastfeeding practices. Women are more likely to recall a pregnancy carried to birth as intended, but this phenomenon would only bias the results if it also applied to breastfeeding practices, which is unlikely.13 While breastfeeding practices may not be exactly recalled, there is no obvious reason for differential reporting.
Conclusions
Our study has clinical implications for first-time US mothers. A recent national goal of the Institute of Medicine is that all pregnancies be planned.3 One of the many benefits of decreasing unintended pregnancy may be to increase breastfeeding rates closer to the Healthy People 2010 goals. In addition, a new hypothesis is suggested by the results of this study: Clinicians should promote breastfeeding differently for women with intended and unintended pregnancies. Future research will evaluate the importance of incorporating pregnancy intention status into patient-centered counseling. In the interim, women with unwanted pregnancies, especially white women, should be targeted for counseling, as they could benefit from breastfeeding, not just for medical reasons but for psychological and economic ones as well.
Acknowledgments
We would like to thank Larry Culpepper, MD, MPH, for his guidance.
1. Forrest JD. Unintended pregnancy among American women. Fam Plann Perspect 1987;19:76-7.
2. Henshaw SK. Unintended pregnancy in the United States. Fam Plann Perspectives 1998;30:24-9,46.-
3. Institute of Medicine Committee on Unintended Pregnancy. The best intentions: unintended pregnancy and the well-being of children and families. Washington, DC: National Academy Press, 1995.
4. Orr ST, Miller CA. Unintended pregnancy and the psychosocial well-being of pregnant women. Womens Health Issues 1997;7:38-46.
5. Institute of Medicine Subcommittee on Nutrition during Lactation. Nutrition during lactation. Washington, DC: National Academy Press, 1991.
6. American Academy of Pediatrics, Work Group on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 1997;100:1035-9.
7. US Department of Health and Human Services. Healthy People 2010. 2nd ed. With understanding and improving health and objectives for improving health. 2 vols. Washington, DC: US Government Printing Office, November 2000.
8. Abma JC, Chandra A, Mosher WD, Peterson LS, Piccinino LJ. Fertility, family planning, and women’s health: new data from the 1995 National Survey of Family Growth. Vital Health Stat 1997;23.19:1-114.
9. Scott JA, Binns CW. Factors associated with the initiation and duration of breastfeeding: a review of the literature. Breastfeed Rev 1999;7:5-16.
10. Dye TD, Wojtowycz MA, Aubry RH, Quade J, Kilburn H. Unintended pregnancy and breastfeeding behavior. Am J Public Health 1997;87:1709-11.
11. Kuan LW, Britto M, Decolongon J, Schoettker PJ, Atherton HD, Kotagal UR. Health system factors contributing to breastfeeding success. Pediatrics 1999;104:e28.-
12. Ventura SJ, Martin JA, Curtin SC, Mathews TJ. Births: final data for 1997. Natl Vital Stat Reports 1999;47.18:1-96.
13. Petersen R, Moos MK. Defining and measuring unintended pregnancy: issues and concerns. Womens Health Issues 1997;7:234-40.
1. Forrest JD. Unintended pregnancy among American women. Fam Plann Perspect 1987;19:76-7.
2. Henshaw SK. Unintended pregnancy in the United States. Fam Plann Perspectives 1998;30:24-9,46.-
3. Institute of Medicine Committee on Unintended Pregnancy. The best intentions: unintended pregnancy and the well-being of children and families. Washington, DC: National Academy Press, 1995.
4. Orr ST, Miller CA. Unintended pregnancy and the psychosocial well-being of pregnant women. Womens Health Issues 1997;7:38-46.
5. Institute of Medicine Subcommittee on Nutrition during Lactation. Nutrition during lactation. Washington, DC: National Academy Press, 1991.
6. American Academy of Pediatrics, Work Group on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 1997;100:1035-9.
7. US Department of Health and Human Services. Healthy People 2010. 2nd ed. With understanding and improving health and objectives for improving health. 2 vols. Washington, DC: US Government Printing Office, November 2000.
8. Abma JC, Chandra A, Mosher WD, Peterson LS, Piccinino LJ. Fertility, family planning, and women’s health: new data from the 1995 National Survey of Family Growth. Vital Health Stat 1997;23.19:1-114.
9. Scott JA, Binns CW. Factors associated with the initiation and duration of breastfeeding: a review of the literature. Breastfeed Rev 1999;7:5-16.
10. Dye TD, Wojtowycz MA, Aubry RH, Quade J, Kilburn H. Unintended pregnancy and breastfeeding behavior. Am J Public Health 1997;87:1709-11.
11. Kuan LW, Britto M, Decolongon J, Schoettker PJ, Atherton HD, Kotagal UR. Health system factors contributing to breastfeeding success. Pediatrics 1999;104:e28.-
12. Ventura SJ, Martin JA, Curtin SC, Mathews TJ. Births: final data for 1997. Natl Vital Stat Reports 1999;47.18:1-96.
13. Petersen R, Moos MK. Defining and measuring unintended pregnancy: issues and concerns. Womens Health Issues 1997;7:234-40.