User login
SAN ANTONIO – The sequential use of a tumor cell vaccine, stereotactic body radiation therapy (SBRT), and a dose-modified FOLFIRINOX regimen as adjuvant treatment for resected pancreatic cancer produced ‘encouraging’ results in a pilot study presented at the annual scientific meeting of the American Society for Radiation Oncology.
This is the first time that the vaccine, SBRT, and mFOLFIRINOX have been prospectively assessed in the adjuvant setting, reported Dr. Joseph Herman of Johns Hopkins University, Baltimore, noting that “SBRT and the GVAX vaccine appear safe” and mFOLFIRINIOX for 6 months thereafter was “fairly tolerable.”
Overall survival (OS) and progression-free survival (PFS) appeared favorable, he said, noting that there was only failure for a patient in the target area where the radiation therapy was used. At a median follow-up of 16 months, OS was not met in patients who received the novel adjuvant strategy and median PFS was 19.6 months. At this point 47% patients have not recurred.
“Pancreatic cancer remains a challenging disease with high mortality,” observed Dr. Daniel Chang of Stanford (Calif.) University, who commented on the results of the study after the presentation and on the general use of radiotherapy in patients with pancreatic cancer. “Radiotherapy does not benefit all patients, but that does not mean that all patients will not benefit,” he said.
“This study showed good tolerance, a good safety profile, and no adverse events,” he said, as well as “very encouraging early results,” Dr. Chang noted. Although the results are early, studies such as this that test novel therapies “should continue to be explored as a way to synergize with radiation,” Dr. Chang said.
The use of radiotherapy remains somewhat controversial in the adjuvant setting, Dr. Herman acknowledged during his presentation, as its use does limit the duration for which chemotherapy can be used and it is unlikely to sterilize positive margins. Although most patients who recur following surgery have systemic disease, evidence from autopsy studies suggests that around 30% have localized disease only and potentially have a local tumor volume that could be targeted with radiation treatment.
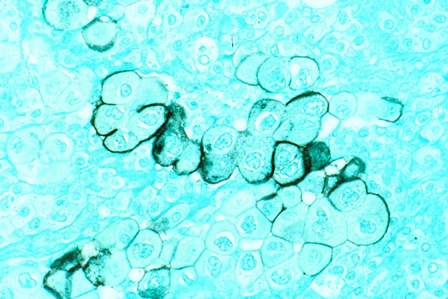
So one of the aims of the pilot study was to look at the use of SBRT and to investigate the potential for the use of the granulocyte-macrophage colony-stimulating factor (GM-CSF) whole pancreatic tumor cell vaccine (GVAX), the rationale being that SBRT might enhance the immune response to the vaccine. A final aim was to look at the adjuvant use of FOLFIRINOX as data had shown it was superior to gemcitabine in the metastatic setting but this had not been fully tested prospectively in patients at an earlier stage of the disease.
A total of 16 patients aged a median of 58 years at diagnosis were studied; 80% had stage IIB disease with all of tumors located in the head of the pancreas and most (67%) being 3 cm or smaller in size. Patients had a good performance (58% 0, 42% 1) at study entry and the majority (89.5%) had undergone a classic pancreaticoduodenectomy.
There were three treatment groups. In the first group, three patients received 5 days of SBRT (33 Gray as five 6.6 Gray fractions) to the tumor bed followed by six cycles of FOLFIRINOX. The standard is to use 5-6 weeks of radiotherapy, Dr. Herman said, so this trial looked at using a reduced radiotherapy course.
In the second group, four patients received SBRT and mFOLFIRINOX. The modified regimen (which removed 5-flurouracil) was used as patients found the full dose regimen intolerable. So an overall recommendation is that standard dose FOLFIRINOX should not be used in this setting, Dr. Herman said.
In the third arm, 12 patients were given a single dose of the vaccine together with low-dose cyclophosphamide, which was used to enhance T-cells’ response to the vaccine. This was followed by the 5 days of SBRT, mFOLFIRINOX for six cycles, and then four further doses of GVAX with low-dose cyclophosphamide were given 1 month apart starting at week 40 and then every 6 months as a boost.
GVAX resulted in minor skin reactions at the site of injection and SBRT was generally well tolerated. Grade 3-4 toxicities associated with mFOLFIRINOX included those previously reported with the regimen, such as neutropenia in two (12.5%), thrombocytopenia in three (18.75%), anemia in one (6.25%) and lymphopenia in seven (43.75%) patients. Other nonhematologic toxicities occurring in two (12.5%) patients each were diarrhea and hypokalemia and in one (6.25%) patient each were hypokalemia, hyponatremia, hypoalbuminuria, and syncope. There was also one case of small bowel obstruction, which resolved without the need for intervention.
“Future questions are whether SBRT should be given prior to or after chemotherapy,” Dr. Herman said. There is also the question of what the target area should be and if higher doses of SBRT would be needed.
The study was supported by the Viragh Family Foundation and the Gonzalez and McKnight Family Foundation, with partial funding by Aduro, which manufactures the tumor cell vaccine used in the study. Dr. Herman did not report having personal disclosures.
SAN ANTONIO – The sequential use of a tumor cell vaccine, stereotactic body radiation therapy (SBRT), and a dose-modified FOLFIRINOX regimen as adjuvant treatment for resected pancreatic cancer produced ‘encouraging’ results in a pilot study presented at the annual scientific meeting of the American Society for Radiation Oncology.
This is the first time that the vaccine, SBRT, and mFOLFIRINOX have been prospectively assessed in the adjuvant setting, reported Dr. Joseph Herman of Johns Hopkins University, Baltimore, noting that “SBRT and the GVAX vaccine appear safe” and mFOLFIRINIOX for 6 months thereafter was “fairly tolerable.”
Overall survival (OS) and progression-free survival (PFS) appeared favorable, he said, noting that there was only failure for a patient in the target area where the radiation therapy was used. At a median follow-up of 16 months, OS was not met in patients who received the novel adjuvant strategy and median PFS was 19.6 months. At this point 47% patients have not recurred.
“Pancreatic cancer remains a challenging disease with high mortality,” observed Dr. Daniel Chang of Stanford (Calif.) University, who commented on the results of the study after the presentation and on the general use of radiotherapy in patients with pancreatic cancer. “Radiotherapy does not benefit all patients, but that does not mean that all patients will not benefit,” he said.
“This study showed good tolerance, a good safety profile, and no adverse events,” he said, as well as “very encouraging early results,” Dr. Chang noted. Although the results are early, studies such as this that test novel therapies “should continue to be explored as a way to synergize with radiation,” Dr. Chang said.
The use of radiotherapy remains somewhat controversial in the adjuvant setting, Dr. Herman acknowledged during his presentation, as its use does limit the duration for which chemotherapy can be used and it is unlikely to sterilize positive margins. Although most patients who recur following surgery have systemic disease, evidence from autopsy studies suggests that around 30% have localized disease only and potentially have a local tumor volume that could be targeted with radiation treatment.
So one of the aims of the pilot study was to look at the use of SBRT and to investigate the potential for the use of the granulocyte-macrophage colony-stimulating factor (GM-CSF) whole pancreatic tumor cell vaccine (GVAX), the rationale being that SBRT might enhance the immune response to the vaccine. A final aim was to look at the adjuvant use of FOLFIRINOX as data had shown it was superior to gemcitabine in the metastatic setting but this had not been fully tested prospectively in patients at an earlier stage of the disease.
A total of 16 patients aged a median of 58 years at diagnosis were studied; 80% had stage IIB disease with all of tumors located in the head of the pancreas and most (67%) being 3 cm or smaller in size. Patients had a good performance (58% 0, 42% 1) at study entry and the majority (89.5%) had undergone a classic pancreaticoduodenectomy.
There were three treatment groups. In the first group, three patients received 5 days of SBRT (33 Gray as five 6.6 Gray fractions) to the tumor bed followed by six cycles of FOLFIRINOX. The standard is to use 5-6 weeks of radiotherapy, Dr. Herman said, so this trial looked at using a reduced radiotherapy course.
In the second group, four patients received SBRT and mFOLFIRINOX. The modified regimen (which removed 5-flurouracil) was used as patients found the full dose regimen intolerable. So an overall recommendation is that standard dose FOLFIRINOX should not be used in this setting, Dr. Herman said.
In the third arm, 12 patients were given a single dose of the vaccine together with low-dose cyclophosphamide, which was used to enhance T-cells’ response to the vaccine. This was followed by the 5 days of SBRT, mFOLFIRINOX for six cycles, and then four further doses of GVAX with low-dose cyclophosphamide were given 1 month apart starting at week 40 and then every 6 months as a boost.
GVAX resulted in minor skin reactions at the site of injection and SBRT was generally well tolerated. Grade 3-4 toxicities associated with mFOLFIRINOX included those previously reported with the regimen, such as neutropenia in two (12.5%), thrombocytopenia in three (18.75%), anemia in one (6.25%) and lymphopenia in seven (43.75%) patients. Other nonhematologic toxicities occurring in two (12.5%) patients each were diarrhea and hypokalemia and in one (6.25%) patient each were hypokalemia, hyponatremia, hypoalbuminuria, and syncope. There was also one case of small bowel obstruction, which resolved without the need for intervention.
“Future questions are whether SBRT should be given prior to or after chemotherapy,” Dr. Herman said. There is also the question of what the target area should be and if higher doses of SBRT would be needed.
The study was supported by the Viragh Family Foundation and the Gonzalez and McKnight Family Foundation, with partial funding by Aduro, which manufactures the tumor cell vaccine used in the study. Dr. Herman did not report having personal disclosures.
SAN ANTONIO – The sequential use of a tumor cell vaccine, stereotactic body radiation therapy (SBRT), and a dose-modified FOLFIRINOX regimen as adjuvant treatment for resected pancreatic cancer produced ‘encouraging’ results in a pilot study presented at the annual scientific meeting of the American Society for Radiation Oncology.
This is the first time that the vaccine, SBRT, and mFOLFIRINOX have been prospectively assessed in the adjuvant setting, reported Dr. Joseph Herman of Johns Hopkins University, Baltimore, noting that “SBRT and the GVAX vaccine appear safe” and mFOLFIRINIOX for 6 months thereafter was “fairly tolerable.”
Overall survival (OS) and progression-free survival (PFS) appeared favorable, he said, noting that there was only failure for a patient in the target area where the radiation therapy was used. At a median follow-up of 16 months, OS was not met in patients who received the novel adjuvant strategy and median PFS was 19.6 months. At this point 47% patients have not recurred.
“Pancreatic cancer remains a challenging disease with high mortality,” observed Dr. Daniel Chang of Stanford (Calif.) University, who commented on the results of the study after the presentation and on the general use of radiotherapy in patients with pancreatic cancer. “Radiotherapy does not benefit all patients, but that does not mean that all patients will not benefit,” he said.
“This study showed good tolerance, a good safety profile, and no adverse events,” he said, as well as “very encouraging early results,” Dr. Chang noted. Although the results are early, studies such as this that test novel therapies “should continue to be explored as a way to synergize with radiation,” Dr. Chang said.
The use of radiotherapy remains somewhat controversial in the adjuvant setting, Dr. Herman acknowledged during his presentation, as its use does limit the duration for which chemotherapy can be used and it is unlikely to sterilize positive margins. Although most patients who recur following surgery have systemic disease, evidence from autopsy studies suggests that around 30% have localized disease only and potentially have a local tumor volume that could be targeted with radiation treatment.
So one of the aims of the pilot study was to look at the use of SBRT and to investigate the potential for the use of the granulocyte-macrophage colony-stimulating factor (GM-CSF) whole pancreatic tumor cell vaccine (GVAX), the rationale being that SBRT might enhance the immune response to the vaccine. A final aim was to look at the adjuvant use of FOLFIRINOX as data had shown it was superior to gemcitabine in the metastatic setting but this had not been fully tested prospectively in patients at an earlier stage of the disease.
A total of 16 patients aged a median of 58 years at diagnosis were studied; 80% had stage IIB disease with all of tumors located in the head of the pancreas and most (67%) being 3 cm or smaller in size. Patients had a good performance (58% 0, 42% 1) at study entry and the majority (89.5%) had undergone a classic pancreaticoduodenectomy.
There were three treatment groups. In the first group, three patients received 5 days of SBRT (33 Gray as five 6.6 Gray fractions) to the tumor bed followed by six cycles of FOLFIRINOX. The standard is to use 5-6 weeks of radiotherapy, Dr. Herman said, so this trial looked at using a reduced radiotherapy course.
In the second group, four patients received SBRT and mFOLFIRINOX. The modified regimen (which removed 5-flurouracil) was used as patients found the full dose regimen intolerable. So an overall recommendation is that standard dose FOLFIRINOX should not be used in this setting, Dr. Herman said.
In the third arm, 12 patients were given a single dose of the vaccine together with low-dose cyclophosphamide, which was used to enhance T-cells’ response to the vaccine. This was followed by the 5 days of SBRT, mFOLFIRINOX for six cycles, and then four further doses of GVAX with low-dose cyclophosphamide were given 1 month apart starting at week 40 and then every 6 months as a boost.
GVAX resulted in minor skin reactions at the site of injection and SBRT was generally well tolerated. Grade 3-4 toxicities associated with mFOLFIRINOX included those previously reported with the regimen, such as neutropenia in two (12.5%), thrombocytopenia in three (18.75%), anemia in one (6.25%) and lymphopenia in seven (43.75%) patients. Other nonhematologic toxicities occurring in two (12.5%) patients each were diarrhea and hypokalemia and in one (6.25%) patient each were hypokalemia, hyponatremia, hypoalbuminuria, and syncope. There was also one case of small bowel obstruction, which resolved without the need for intervention.
“Future questions are whether SBRT should be given prior to or after chemotherapy,” Dr. Herman said. There is also the question of what the target area should be and if higher doses of SBRT would be needed.
The study was supported by the Viragh Family Foundation and the Gonzalez and McKnight Family Foundation, with partial funding by Aduro, which manufactures the tumor cell vaccine used in the study. Dr. Herman did not report having personal disclosures.
AT THE ASTRO ANNUAL MEETING
Key clinical point: Stereotactic body radiation therapy used with a novel tumor cell vaccine and a dose-modified FOLFIRINOX regimen represents a novel adjuvant approach in pancreatic cancer.
Major finding: The novel adjuvant approach was well tolerated and produced promising, if early, clinical results.
Data source: Prospective pilot study of 16 patients with mostly stage IIb resected pancreatic cancer.
Disclosures: The study was supported by the Viragh Family Foundation and the Gonzalez and McKnight Family Foundation, with partial funding by Aduro, which manufactures the tumor cell vaccine used in the study. Dr. Herman did not report having personal disclosures.