User login
A 61-year-old woman without any known medical history presented with a chief complaint of right arm numbness and right-sided scalp numbness that had started 2 days earlier. She described a “pins and needles” sensation in her right upper extremity and right scalp, and said the numbness in her scalp was especially noticeable when she combed her hair. The patient denied any chest pain, shortness of breath, weakness in her arms or legs, headache, or blurred vision.
She said that 1 day prior to the onset of the paresthesias, she woke up fatigued and vomited once. Throughout that day, she had symptoms of nausea and fatigue, and sought treatment at an urgent care center that afternoon. At the urgent care center, she was diagnosed with a “stomach virus” and was given an antiemetic. The next day, her nausea improved, but the paresthesias began in her right hand and scalp. On the third day, the patient went to work, but the persistent paresthesias caused her to visit her primary care physician, who sent her to our ED for further work-up.
The patient said she had been in good health until 3 days ago. She reported no medical problems and was taking no medications. The patient denied smoking or using alcohol; her family history was significant only in that her father had a myocardial infarction (MI) while in his 50s.
On physical examination, the patient was alert, oriented, and in no apparent distress. Her body mass index was 28.3 kg/m2. Vital signs were: temperature, 99.2°F; blood pressure, 113/73 mm Hg; heart rate, 93 beats/minute; and respiratory rate, 18 breaths/minute. Oxygen saturation was 95% on room air.
Her head was normocephalic and atraumatic, and her eyes, ears, nose, and throat were normal. Her neck was supple and without jugular vein distension. The cardiac examination revealed normal heart sounds without murmurs, rubs, or gallops. Her lungs were clear without rales, wheezes, or rhonchi. Her abdomen was soft, without tenderness, guarding, or rebound, and she had normal bowel sounds.
Her musculoskeletal examination was normal, with +5/5 strength bilaterally in her upper and lower extremities. The patient’s skin examination also was normal. On neurological examination, her right upper extremity and right side of her face were noted to have decreased sensation via pinprick compared to the left side, but the examination was otherwise normal. The National Institutes of Health Stroke Scale score was 1.
The patient’s electrocardiogram (ECG) showed a normal sinus rhythm (rate, 90 beats/min), a lateral infarct of undetermined age, and a left atrial abnormality. Laboratory evaluation was significant only for a brain natriuretic peptide level of 334 pg/mL, a creatine phosphokinase (CPK) level of 782 IU/L, and a troponin I level of >50 ng/mL (Table). Serial cardiac enzyme levels were obtained and showed a decline of CPK from 782 IU/L to 331 IU/L over the following 36 hours. However, the troponin I levels remained >50 ng/mL for 5 days and then declined to 31.6 ng/mL.
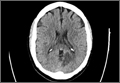
A computed tomography (CT) scan of the brain without contrast revealed an acute to subacute infarct in the left occipital and left thalamic regions (Figure). A stat transthoracic echocardiogram (ECHO) performed in the ED revealed a dilated left ventricle with an ejection fraction of 20% to 25%, along with a hypokinetic anterolateral wall and an akinetic inferolateral wall. No atrial thrombus was visible on the ECHO. Doppler studies of the patient’s lower extremities were negative for deep vein thrombosis. Magnetic resonance imaging of her brain showed an infarct in the posterior circulation distribution involving the left occipital lobes and small areas in the left thalamic and right parietal-occipital regions. Hemorrhagic conversion of the left occipital infarct without mass effect was also noted. The patient was admitted to the neurological intensive care unit for frequent neurological examinations and close monitoring for worsening cerebral hemorrhage.
When the patient had still been in the ED, cardiology services were consulted; the cardiologist initiated a heparin drip with close monitoring of the coagulation studies. Cardiac catheterization was not done immediately because the ECG did not show acute ST elevations. The day after her presentation to the ED, the patient underwent a primary percutaneous coronary catheterization and was found to have a small rudimentary left anterior descending artery, with only small branches supplying the septal region. The right circumflex artery was very large and was supplying the lateral wall. No stents were placed during this procedure. A transesophageal ECHO (TEE) showed no evidence of a left atrial appendage thrombus.
The patient experienced an episode of coffee ground emesis while undergoing the TEE. Her hemoglobin declined from 11.9 g/dL to 7.9 g/dL, which led to a transfusion of 2 U of packed red blood cells and platelets. Heparin was discontinued and a proton pump inhibitor was started; however, no endoscopy was done at that time.
Throughout her stay, the patient was continuously monitored, but no evidence of arrhythmia or atrial fibrillation was found. Upon discharge, the neurologist recommended the patient receive clopidogrel and aspirin therapy for 3 months with subsequent aspirin monotherapy afterward. The patient was discharged after 10 days in the hospital.
Discussion
Although she had an MI, the patient presented here did not experience any chest pain. Her chief complaint in the ED was paresthesias related to her concomitant stroke, and only on further probing did she describe the additional symptoms of fatigability and vomiting.
Since heart disease and stroke share common risk factors and pathophysiology, acute cerebral ischemic events may happen concurrently with MIs. In a review of studies that included approximately 2,900 patients who had an acute stroke, Kerr et al1 found that 20% had elevated troponin levels within 7 days of the stroke. In 2013, the American Heart Association and American Stroke Association published guidelines advising that all patients who present with acute cerebral ischemia have an emergent ECG and baseline troponin level.2 This was in response to evidence that even low positive troponin levels have been associated with an increased risk of mortality.3 Positive troponin levels are especially important because fatal and nonfatal stroke post-MI events have been found to be increasing in frequency for women, even though there has been a significant overall reduction in post-MI mortality.4 Patients who have an ischemic stroke concurrently with an acute MI or soon after have an overall poorer clinical prognosis.5
For emergency physicians (EPs), this is a “chicken or the egg” scenario. It is difficult to determine which came first: the MI or the cerebral ischemia. Similar risk factors can result in an acute embolic event from revascularization, atrial fibrillation without proper anticoagulation, or a poorly functioning left ventricle.6 It is important to remember that regardless of the order of occurrence, the incidence of ischemic stroke is markedly increased in conjunction with an acute MI.7 Several theories have been advanced regarding the relationship between ischemic stroke and acute MI. One theory proposes that elevated troponin levels could be related to a large catecholamine release after a cerebral ischemic stroke, resulting in subsequent myocardial injury or cardiomyopathy.7 However, this theory remains controversial.
Management
The major consideration for the EP is whether or not to give thrombolytics to a patient who presents with concomitant acute MI and ischemic stroke. An acute MI within the 3 months preceding an acute stroke is considered a relative contraindication for intravenous tissue plasminogen activator (tPA).8 It has also been found, albeit rarely, that there is an increased risk of cardiac rupture or tamponade due to the breakdown of the fibrin clot within the necrotic cardiac tissue.8
How should patients with stroke complicated by acute cardiac compromise be managed in the ED? One acute vascular event cannot be ignored while addressing the other. There are no evidence-based guidelines for the management of patients who present with this picture.8 In addition, no published clinical studies have focused on the decision-making process for these patients.8
Immediate percutaneous coronary intervention for the MI performed on such patients would prevent the use of tPA for the acute stroke. Though any anticoagulation increases the risk for postischemic cerebral hemorrhage, heparin is necessary to prevent the formation of a left ventricle thrombus.7 Alternately, mechanical thrombectomy and cardiac catheterization may be combined as emergent treatments for these patients, but performing these two procedures simultaneously is not widely available.
For a patient who presents to the ED within both the cardiac and stroke treatment windows, tPA might be a viable option, and the only one readily valuable.8 However, the EP must be mindful of the varying dosages of tPA and means of administration for different thrombosis sites. Also, care must be taken when treating a patient with dual or triple antiplatelet therapy because of the increased risk of hemorrhage.9 Currently, no safe standardized regimens have been established, and further trials need to be performed.10
If the patient in this case report had presented at our ED with only signs and symptoms of an MI, typically she would have been treated with heparin, aspirin, and an urgent cardiac catheterization. If she had presented with only signs and symptoms of a stroke, she would have been treated with full-dose aspirin and worked up from a neurological perspective. Because she had signs and symptoms of both, she presented a dilemma. She was initially treated with heparin to prevent a thrombus formation, but then later changed to only clopidogrel and aspirin to prevent further episodes of coffee ground emesis or worsening hemorrhagic conversion.
Conclusion
Common risk factors for cardiac and cerebral ischemic events may result in a patient presenting with both acute MI and an acute cerebral ischemic event. There have not been sufficient clinical studies to determine the best decision-making process for these patients. Therefore, patients with this complicated presentation must be assessed on an individual basis. Current treatment options are varied and are based according to history of the present illness, time of presentation to the ED, and the available resources within the hospital.
1. Kerr G, Ray G, Wu O, Stott DJ, Langhorne P. Elevated troponin after stroke: a systematic review. Cerebrovasc Dis. 2009;28(3):220-226.
2. Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870-947.
3. Di Angelantonio E, Fiorelli M, Toni D, et al. Prognostic significance of admission levels of troponin I in patients with acute ischaemic stroke. J Neurol Neurosurg Psychiatry. 2005;76(1):76-81.
4. Shiue I, Hristova K, Sharma J. Correspondence: gender and outcome from acute myocardial infarction and secondary stoke. Br J Cardiology. 2014;21:90.
5. Park S, Jung J. Risk factors for acute cardioembolic brain stroke in acute myocardial infarction. Korean Circulation J. 2005;35:353-356.
6. Witt BJ, Ballman KV, Brown RD Jr, Meverden RA, Jacobsen SJ, Roger VL. The incidence of stroke after myocardial infarction: a meta-analysis. Am J Med. 2006;119(4):354.e1-e9.
7. Feher G, Tibold A, Kotlani K, Szapary L. The clinical importance of troponin elevation in ischaemic cerebrovascular events: a clinical review. Journal of Cardiology and Therapy. 2014;1(7):141-149.
8. Maciel R, Palma R, Sousa P, Ferreira F, Nzwalo H. Acute stroke with concomitant acute myocardial infarction: will you thrombolyse? J Stroke. 2015;17(1):84-86.
9. Toyoda K, Yasaka M, Iwade K, et al; Bleeding with Antithrombotic Therapy (BAT) Study Group. Dual antithrombotic therapy increases severe bleeding events in patients with stroke and cardiovascular disease: a prospective, multicenter, observational study. Stroke. 2008;39(6):1740-1745.
10. Omar HR, Mangar D, Camporesi EM. Simultaneous thrombosis of 2 vascular territories: is thrombolytic therapy a better option? Am J Emerg Med. 2013;31(9):1412-1413.
A 61-year-old woman without any known medical history presented with a chief complaint of right arm numbness and right-sided scalp numbness that had started 2 days earlier. She described a “pins and needles” sensation in her right upper extremity and right scalp, and said the numbness in her scalp was especially noticeable when she combed her hair. The patient denied any chest pain, shortness of breath, weakness in her arms or legs, headache, or blurred vision.
She said that 1 day prior to the onset of the paresthesias, she woke up fatigued and vomited once. Throughout that day, she had symptoms of nausea and fatigue, and sought treatment at an urgent care center that afternoon. At the urgent care center, she was diagnosed with a “stomach virus” and was given an antiemetic. The next day, her nausea improved, but the paresthesias began in her right hand and scalp. On the third day, the patient went to work, but the persistent paresthesias caused her to visit her primary care physician, who sent her to our ED for further work-up.
The patient said she had been in good health until 3 days ago. She reported no medical problems and was taking no medications. The patient denied smoking or using alcohol; her family history was significant only in that her father had a myocardial infarction (MI) while in his 50s.
On physical examination, the patient was alert, oriented, and in no apparent distress. Her body mass index was 28.3 kg/m2. Vital signs were: temperature, 99.2°F; blood pressure, 113/73 mm Hg; heart rate, 93 beats/minute; and respiratory rate, 18 breaths/minute. Oxygen saturation was 95% on room air.
Her head was normocephalic and atraumatic, and her eyes, ears, nose, and throat were normal. Her neck was supple and without jugular vein distension. The cardiac examination revealed normal heart sounds without murmurs, rubs, or gallops. Her lungs were clear without rales, wheezes, or rhonchi. Her abdomen was soft, without tenderness, guarding, or rebound, and she had normal bowel sounds.
Her musculoskeletal examination was normal, with +5/5 strength bilaterally in her upper and lower extremities. The patient’s skin examination also was normal. On neurological examination, her right upper extremity and right side of her face were noted to have decreased sensation via pinprick compared to the left side, but the examination was otherwise normal. The National Institutes of Health Stroke Scale score was 1.
The patient’s electrocardiogram (ECG) showed a normal sinus rhythm (rate, 90 beats/min), a lateral infarct of undetermined age, and a left atrial abnormality. Laboratory evaluation was significant only for a brain natriuretic peptide level of 334 pg/mL, a creatine phosphokinase (CPK) level of 782 IU/L, and a troponin I level of >50 ng/mL (Table). Serial cardiac enzyme levels were obtained and showed a decline of CPK from 782 IU/L to 331 IU/L over the following 36 hours. However, the troponin I levels remained >50 ng/mL for 5 days and then declined to 31.6 ng/mL.
A computed tomography (CT) scan of the brain without contrast revealed an acute to subacute infarct in the left occipital and left thalamic regions (Figure). A stat transthoracic echocardiogram (ECHO) performed in the ED revealed a dilated left ventricle with an ejection fraction of 20% to 25%, along with a hypokinetic anterolateral wall and an akinetic inferolateral wall. No atrial thrombus was visible on the ECHO. Doppler studies of the patient’s lower extremities were negative for deep vein thrombosis. Magnetic resonance imaging of her brain showed an infarct in the posterior circulation distribution involving the left occipital lobes and small areas in the left thalamic and right parietal-occipital regions. Hemorrhagic conversion of the left occipital infarct without mass effect was also noted. The patient was admitted to the neurological intensive care unit for frequent neurological examinations and close monitoring for worsening cerebral hemorrhage.
When the patient had still been in the ED, cardiology services were consulted; the cardiologist initiated a heparin drip with close monitoring of the coagulation studies. Cardiac catheterization was not done immediately because the ECG did not show acute ST elevations. The day after her presentation to the ED, the patient underwent a primary percutaneous coronary catheterization and was found to have a small rudimentary left anterior descending artery, with only small branches supplying the septal region. The right circumflex artery was very large and was supplying the lateral wall. No stents were placed during this procedure. A transesophageal ECHO (TEE) showed no evidence of a left atrial appendage thrombus.
The patient experienced an episode of coffee ground emesis while undergoing the TEE. Her hemoglobin declined from 11.9 g/dL to 7.9 g/dL, which led to a transfusion of 2 U of packed red blood cells and platelets. Heparin was discontinued and a proton pump inhibitor was started; however, no endoscopy was done at that time.
Throughout her stay, the patient was continuously monitored, but no evidence of arrhythmia or atrial fibrillation was found. Upon discharge, the neurologist recommended the patient receive clopidogrel and aspirin therapy for 3 months with subsequent aspirin monotherapy afterward. The patient was discharged after 10 days in the hospital.
Discussion
Although she had an MI, the patient presented here did not experience any chest pain. Her chief complaint in the ED was paresthesias related to her concomitant stroke, and only on further probing did she describe the additional symptoms of fatigability and vomiting.
Since heart disease and stroke share common risk factors and pathophysiology, acute cerebral ischemic events may happen concurrently with MIs. In a review of studies that included approximately 2,900 patients who had an acute stroke, Kerr et al1 found that 20% had elevated troponin levels within 7 days of the stroke. In 2013, the American Heart Association and American Stroke Association published guidelines advising that all patients who present with acute cerebral ischemia have an emergent ECG and baseline troponin level.2 This was in response to evidence that even low positive troponin levels have been associated with an increased risk of mortality.3 Positive troponin levels are especially important because fatal and nonfatal stroke post-MI events have been found to be increasing in frequency for women, even though there has been a significant overall reduction in post-MI mortality.4 Patients who have an ischemic stroke concurrently with an acute MI or soon after have an overall poorer clinical prognosis.5
For emergency physicians (EPs), this is a “chicken or the egg” scenario. It is difficult to determine which came first: the MI or the cerebral ischemia. Similar risk factors can result in an acute embolic event from revascularization, atrial fibrillation without proper anticoagulation, or a poorly functioning left ventricle.6 It is important to remember that regardless of the order of occurrence, the incidence of ischemic stroke is markedly increased in conjunction with an acute MI.7 Several theories have been advanced regarding the relationship between ischemic stroke and acute MI. One theory proposes that elevated troponin levels could be related to a large catecholamine release after a cerebral ischemic stroke, resulting in subsequent myocardial injury or cardiomyopathy.7 However, this theory remains controversial.
Management
The major consideration for the EP is whether or not to give thrombolytics to a patient who presents with concomitant acute MI and ischemic stroke. An acute MI within the 3 months preceding an acute stroke is considered a relative contraindication for intravenous tissue plasminogen activator (tPA).8 It has also been found, albeit rarely, that there is an increased risk of cardiac rupture or tamponade due to the breakdown of the fibrin clot within the necrotic cardiac tissue.8
How should patients with stroke complicated by acute cardiac compromise be managed in the ED? One acute vascular event cannot be ignored while addressing the other. There are no evidence-based guidelines for the management of patients who present with this picture.8 In addition, no published clinical studies have focused on the decision-making process for these patients.8
Immediate percutaneous coronary intervention for the MI performed on such patients would prevent the use of tPA for the acute stroke. Though any anticoagulation increases the risk for postischemic cerebral hemorrhage, heparin is necessary to prevent the formation of a left ventricle thrombus.7 Alternately, mechanical thrombectomy and cardiac catheterization may be combined as emergent treatments for these patients, but performing these two procedures simultaneously is not widely available.
For a patient who presents to the ED within both the cardiac and stroke treatment windows, tPA might be a viable option, and the only one readily valuable.8 However, the EP must be mindful of the varying dosages of tPA and means of administration for different thrombosis sites. Also, care must be taken when treating a patient with dual or triple antiplatelet therapy because of the increased risk of hemorrhage.9 Currently, no safe standardized regimens have been established, and further trials need to be performed.10
If the patient in this case report had presented at our ED with only signs and symptoms of an MI, typically she would have been treated with heparin, aspirin, and an urgent cardiac catheterization. If she had presented with only signs and symptoms of a stroke, she would have been treated with full-dose aspirin and worked up from a neurological perspective. Because she had signs and symptoms of both, she presented a dilemma. She was initially treated with heparin to prevent a thrombus formation, but then later changed to only clopidogrel and aspirin to prevent further episodes of coffee ground emesis or worsening hemorrhagic conversion.
Conclusion
Common risk factors for cardiac and cerebral ischemic events may result in a patient presenting with both acute MI and an acute cerebral ischemic event. There have not been sufficient clinical studies to determine the best decision-making process for these patients. Therefore, patients with this complicated presentation must be assessed on an individual basis. Current treatment options are varied and are based according to history of the present illness, time of presentation to the ED, and the available resources within the hospital.
A 61-year-old woman without any known medical history presented with a chief complaint of right arm numbness and right-sided scalp numbness that had started 2 days earlier. She described a “pins and needles” sensation in her right upper extremity and right scalp, and said the numbness in her scalp was especially noticeable when she combed her hair. The patient denied any chest pain, shortness of breath, weakness in her arms or legs, headache, or blurred vision.
She said that 1 day prior to the onset of the paresthesias, she woke up fatigued and vomited once. Throughout that day, she had symptoms of nausea and fatigue, and sought treatment at an urgent care center that afternoon. At the urgent care center, she was diagnosed with a “stomach virus” and was given an antiemetic. The next day, her nausea improved, but the paresthesias began in her right hand and scalp. On the third day, the patient went to work, but the persistent paresthesias caused her to visit her primary care physician, who sent her to our ED for further work-up.
The patient said she had been in good health until 3 days ago. She reported no medical problems and was taking no medications. The patient denied smoking or using alcohol; her family history was significant only in that her father had a myocardial infarction (MI) while in his 50s.
On physical examination, the patient was alert, oriented, and in no apparent distress. Her body mass index was 28.3 kg/m2. Vital signs were: temperature, 99.2°F; blood pressure, 113/73 mm Hg; heart rate, 93 beats/minute; and respiratory rate, 18 breaths/minute. Oxygen saturation was 95% on room air.
Her head was normocephalic and atraumatic, and her eyes, ears, nose, and throat were normal. Her neck was supple and without jugular vein distension. The cardiac examination revealed normal heart sounds without murmurs, rubs, or gallops. Her lungs were clear without rales, wheezes, or rhonchi. Her abdomen was soft, without tenderness, guarding, or rebound, and she had normal bowel sounds.
Her musculoskeletal examination was normal, with +5/5 strength bilaterally in her upper and lower extremities. The patient’s skin examination also was normal. On neurological examination, her right upper extremity and right side of her face were noted to have decreased sensation via pinprick compared to the left side, but the examination was otherwise normal. The National Institutes of Health Stroke Scale score was 1.
The patient’s electrocardiogram (ECG) showed a normal sinus rhythm (rate, 90 beats/min), a lateral infarct of undetermined age, and a left atrial abnormality. Laboratory evaluation was significant only for a brain natriuretic peptide level of 334 pg/mL, a creatine phosphokinase (CPK) level of 782 IU/L, and a troponin I level of >50 ng/mL (Table). Serial cardiac enzyme levels were obtained and showed a decline of CPK from 782 IU/L to 331 IU/L over the following 36 hours. However, the troponin I levels remained >50 ng/mL for 5 days and then declined to 31.6 ng/mL.
A computed tomography (CT) scan of the brain without contrast revealed an acute to subacute infarct in the left occipital and left thalamic regions (Figure). A stat transthoracic echocardiogram (ECHO) performed in the ED revealed a dilated left ventricle with an ejection fraction of 20% to 25%, along with a hypokinetic anterolateral wall and an akinetic inferolateral wall. No atrial thrombus was visible on the ECHO. Doppler studies of the patient’s lower extremities were negative for deep vein thrombosis. Magnetic resonance imaging of her brain showed an infarct in the posterior circulation distribution involving the left occipital lobes and small areas in the left thalamic and right parietal-occipital regions. Hemorrhagic conversion of the left occipital infarct without mass effect was also noted. The patient was admitted to the neurological intensive care unit for frequent neurological examinations and close monitoring for worsening cerebral hemorrhage.
When the patient had still been in the ED, cardiology services were consulted; the cardiologist initiated a heparin drip with close monitoring of the coagulation studies. Cardiac catheterization was not done immediately because the ECG did not show acute ST elevations. The day after her presentation to the ED, the patient underwent a primary percutaneous coronary catheterization and was found to have a small rudimentary left anterior descending artery, with only small branches supplying the septal region. The right circumflex artery was very large and was supplying the lateral wall. No stents were placed during this procedure. A transesophageal ECHO (TEE) showed no evidence of a left atrial appendage thrombus.
The patient experienced an episode of coffee ground emesis while undergoing the TEE. Her hemoglobin declined from 11.9 g/dL to 7.9 g/dL, which led to a transfusion of 2 U of packed red blood cells and platelets. Heparin was discontinued and a proton pump inhibitor was started; however, no endoscopy was done at that time.
Throughout her stay, the patient was continuously monitored, but no evidence of arrhythmia or atrial fibrillation was found. Upon discharge, the neurologist recommended the patient receive clopidogrel and aspirin therapy for 3 months with subsequent aspirin monotherapy afterward. The patient was discharged after 10 days in the hospital.
Discussion
Although she had an MI, the patient presented here did not experience any chest pain. Her chief complaint in the ED was paresthesias related to her concomitant stroke, and only on further probing did she describe the additional symptoms of fatigability and vomiting.
Since heart disease and stroke share common risk factors and pathophysiology, acute cerebral ischemic events may happen concurrently with MIs. In a review of studies that included approximately 2,900 patients who had an acute stroke, Kerr et al1 found that 20% had elevated troponin levels within 7 days of the stroke. In 2013, the American Heart Association and American Stroke Association published guidelines advising that all patients who present with acute cerebral ischemia have an emergent ECG and baseline troponin level.2 This was in response to evidence that even low positive troponin levels have been associated with an increased risk of mortality.3 Positive troponin levels are especially important because fatal and nonfatal stroke post-MI events have been found to be increasing in frequency for women, even though there has been a significant overall reduction in post-MI mortality.4 Patients who have an ischemic stroke concurrently with an acute MI or soon after have an overall poorer clinical prognosis.5
For emergency physicians (EPs), this is a “chicken or the egg” scenario. It is difficult to determine which came first: the MI or the cerebral ischemia. Similar risk factors can result in an acute embolic event from revascularization, atrial fibrillation without proper anticoagulation, or a poorly functioning left ventricle.6 It is important to remember that regardless of the order of occurrence, the incidence of ischemic stroke is markedly increased in conjunction with an acute MI.7 Several theories have been advanced regarding the relationship between ischemic stroke and acute MI. One theory proposes that elevated troponin levels could be related to a large catecholamine release after a cerebral ischemic stroke, resulting in subsequent myocardial injury or cardiomyopathy.7 However, this theory remains controversial.
Management
The major consideration for the EP is whether or not to give thrombolytics to a patient who presents with concomitant acute MI and ischemic stroke. An acute MI within the 3 months preceding an acute stroke is considered a relative contraindication for intravenous tissue plasminogen activator (tPA).8 It has also been found, albeit rarely, that there is an increased risk of cardiac rupture or tamponade due to the breakdown of the fibrin clot within the necrotic cardiac tissue.8
How should patients with stroke complicated by acute cardiac compromise be managed in the ED? One acute vascular event cannot be ignored while addressing the other. There are no evidence-based guidelines for the management of patients who present with this picture.8 In addition, no published clinical studies have focused on the decision-making process for these patients.8
Immediate percutaneous coronary intervention for the MI performed on such patients would prevent the use of tPA for the acute stroke. Though any anticoagulation increases the risk for postischemic cerebral hemorrhage, heparin is necessary to prevent the formation of a left ventricle thrombus.7 Alternately, mechanical thrombectomy and cardiac catheterization may be combined as emergent treatments for these patients, but performing these two procedures simultaneously is not widely available.
For a patient who presents to the ED within both the cardiac and stroke treatment windows, tPA might be a viable option, and the only one readily valuable.8 However, the EP must be mindful of the varying dosages of tPA and means of administration for different thrombosis sites. Also, care must be taken when treating a patient with dual or triple antiplatelet therapy because of the increased risk of hemorrhage.9 Currently, no safe standardized regimens have been established, and further trials need to be performed.10
If the patient in this case report had presented at our ED with only signs and symptoms of an MI, typically she would have been treated with heparin, aspirin, and an urgent cardiac catheterization. If she had presented with only signs and symptoms of a stroke, she would have been treated with full-dose aspirin and worked up from a neurological perspective. Because she had signs and symptoms of both, she presented a dilemma. She was initially treated with heparin to prevent a thrombus formation, but then later changed to only clopidogrel and aspirin to prevent further episodes of coffee ground emesis or worsening hemorrhagic conversion.
Conclusion
Common risk factors for cardiac and cerebral ischemic events may result in a patient presenting with both acute MI and an acute cerebral ischemic event. There have not been sufficient clinical studies to determine the best decision-making process for these patients. Therefore, patients with this complicated presentation must be assessed on an individual basis. Current treatment options are varied and are based according to history of the present illness, time of presentation to the ED, and the available resources within the hospital.
1. Kerr G, Ray G, Wu O, Stott DJ, Langhorne P. Elevated troponin after stroke: a systematic review. Cerebrovasc Dis. 2009;28(3):220-226.
2. Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870-947.
3. Di Angelantonio E, Fiorelli M, Toni D, et al. Prognostic significance of admission levels of troponin I in patients with acute ischaemic stroke. J Neurol Neurosurg Psychiatry. 2005;76(1):76-81.
4. Shiue I, Hristova K, Sharma J. Correspondence: gender and outcome from acute myocardial infarction and secondary stoke. Br J Cardiology. 2014;21:90.
5. Park S, Jung J. Risk factors for acute cardioembolic brain stroke in acute myocardial infarction. Korean Circulation J. 2005;35:353-356.
6. Witt BJ, Ballman KV, Brown RD Jr, Meverden RA, Jacobsen SJ, Roger VL. The incidence of stroke after myocardial infarction: a meta-analysis. Am J Med. 2006;119(4):354.e1-e9.
7. Feher G, Tibold A, Kotlani K, Szapary L. The clinical importance of troponin elevation in ischaemic cerebrovascular events: a clinical review. Journal of Cardiology and Therapy. 2014;1(7):141-149.
8. Maciel R, Palma R, Sousa P, Ferreira F, Nzwalo H. Acute stroke with concomitant acute myocardial infarction: will you thrombolyse? J Stroke. 2015;17(1):84-86.
9. Toyoda K, Yasaka M, Iwade K, et al; Bleeding with Antithrombotic Therapy (BAT) Study Group. Dual antithrombotic therapy increases severe bleeding events in patients with stroke and cardiovascular disease: a prospective, multicenter, observational study. Stroke. 2008;39(6):1740-1745.
10. Omar HR, Mangar D, Camporesi EM. Simultaneous thrombosis of 2 vascular territories: is thrombolytic therapy a better option? Am J Emerg Med. 2013;31(9):1412-1413.
1. Kerr G, Ray G, Wu O, Stott DJ, Langhorne P. Elevated troponin after stroke: a systematic review. Cerebrovasc Dis. 2009;28(3):220-226.
2. Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870-947.
3. Di Angelantonio E, Fiorelli M, Toni D, et al. Prognostic significance of admission levels of troponin I in patients with acute ischaemic stroke. J Neurol Neurosurg Psychiatry. 2005;76(1):76-81.
4. Shiue I, Hristova K, Sharma J. Correspondence: gender and outcome from acute myocardial infarction and secondary stoke. Br J Cardiology. 2014;21:90.
5. Park S, Jung J. Risk factors for acute cardioembolic brain stroke in acute myocardial infarction. Korean Circulation J. 2005;35:353-356.
6. Witt BJ, Ballman KV, Brown RD Jr, Meverden RA, Jacobsen SJ, Roger VL. The incidence of stroke after myocardial infarction: a meta-analysis. Am J Med. 2006;119(4):354.e1-e9.
7. Feher G, Tibold A, Kotlani K, Szapary L. The clinical importance of troponin elevation in ischaemic cerebrovascular events: a clinical review. Journal of Cardiology and Therapy. 2014;1(7):141-149.
8. Maciel R, Palma R, Sousa P, Ferreira F, Nzwalo H. Acute stroke with concomitant acute myocardial infarction: will you thrombolyse? J Stroke. 2015;17(1):84-86.
9. Toyoda K, Yasaka M, Iwade K, et al; Bleeding with Antithrombotic Therapy (BAT) Study Group. Dual antithrombotic therapy increases severe bleeding events in patients with stroke and cardiovascular disease: a prospective, multicenter, observational study. Stroke. 2008;39(6):1740-1745.
10. Omar HR, Mangar D, Camporesi EM. Simultaneous thrombosis of 2 vascular territories: is thrombolytic therapy a better option? Am J Emerg Med. 2013;31(9):1412-1413.