User login
Heat-related illnesses can affect people of any age who are subjected to extreme heat and humidity regardless of physical fitness level or baseline health status. The most serious of the heat-related illnesses is heat stroke. Prompt identification, early initiation of cooling measures (including cold-water immersion [CWI]), and transport to a higher level of care, when appropriate, are imperative. This article reviews heat-related illness identification, as well as management strategies.
Heat-related illnesses: From the benign to the severe
Some of the less severe forms of heat-related illness include heat cramps (which are due to dehydration and salt loss), heat rash, and heat edema. Heat rash and heat edema are benign. Heat rash typically resolves with cooler clothing and a cooler environment. Heat edema tends to improve after sleeping in a cooler environment with legs elevated. Heat syncope is the result of decreased cerebral perfusion due to fluid loss and vasodilation that results in a distributive hypovolemia. It commonly occurs after vigorous exercise when the athlete is standing still.
Heat exhaustion requires a more careful clinical assessment. It is the inability to continue activity in the heat, often with weakness and collapse. Also due to salt and water losses, it results in cardiovascular output that is insufficient to meet the circulatory and metabolic demands of the body. The body temperature is often elevated but <40° C (104° F), vomiting can occur, and mild central nervous system (CNS) dysfunction may be present.
Heat stroke is the most severe form of heat-related illness and can be life-threatening.1
It is important to understand that these heat-related illnesses do not progress along a continuum. Patients develop heat stroke without having had milder forms of heat illness, and patients with a milder type of heat illness usually do not progress to heat stroke.
Heat stroke: Definition, types, risk factors
Heat stroke is defined as a core body temperature ≥40° C (104° F) with CNS dysfunction in the setting of environmental heat stress. The mortality rate can reach over 50%.2-6
There are 2 main types of heat stroke: exertional heat stroke and nonexertional (classic) heat stroke. Exertional heat stroke more commonly affects healthy, young people, such as athletes or military personnel. Classic (nonexertional) heat stroke patients are typically elderly and/or have a chronic illness, although occasionally it involves children who are unable to escape from a hot environment.5,7 While exertional heat stroke typically develops over a period of a few hours in participants of prolonged activities, such as marathons, classic heat stroke in the elderly typically develops over a period of days in the setting of high environmental temperatures. In both conditions, there is an inability to maintain a normal body temperature leading to CNS dysregulation with altered mental status and often multisystem organ dysfunction.7
Continue to: Risk factors
Risk factors. Heat-related illness can affect patients of all ages and levels of physical fitness; however, certain factors place patients at increased risk. These include physical deconditioning, dehydration, high levels of exercise intensity, obesity, elevated environmental temperatures, sleep deprivation, certain medications, alcohol and drug abuse, concurrent illness, and wearing excessive clothing or equipment. It is imperative that severe cases of heat illness be identified early and treatment be initiated rapidly, as delays in cooling can significantly increase the fatality rate.5
Management: First suspect the diagnosis
Health care providers must first suspect heat-related illness and then accurately diagnose it. It is important to differentiate heat-related illness from syncope, cardiac abnormalities, gastroenteritis, hypoglycemia, and other entities that require alternate management. For cases of collapse, syncope or near-syncope, or altered mental status during exertion, heat stroke should be the default diagnosis until proven otherwise.
Obtain a core body temperature. While attending to airway, breathing, and circulation, obtain a core body temperature. Rectal (or esophageal) core temperatures provide a reliable reading that can assist in determining the severity of the heat illness. Axillary, tympanic, temporal, oral, and skin temperatures are affected by environmental factors and are not accurate determinants of core body temperature.8
Once heat stroke is diagnosed, the physician must immediately initiate cooling by removing clothing, placing the patient in the shade or an air-conditioned area, and beginning aggressive cooling measures (more on this in a bit). While field management requires an accurate diagnosis of the severity of a patient’s heat-related illness, one should not delay treatment in order to obtain a rectal temperature.
When treating the milder forms of heat illness, administer oral or intravenous (IV) isotonic fluids. For heat cramps, stretching the affected muscle can help. For heat syncope, lying the patient down and elevating the legs restores perfusion. Patients with heat exhaustion will require some cooling measures such as relocation to a shaded area, removal of excess clothing, and the use of cold towels, along with hydration and elevation of the feet.
Continue to: Cooling techniques for heat stroke
Cooling techniques for heat stroke
In order to adequately cool a patient suffering from heat stroke, health care providers must create a gradient for heat to escape the body through the skin into the environment by conduction, convection, or evaporation.3 Cooling heat stroke patients to less than 40° C (104° F) within 30 minutes after collapse decreases the fatality rate to almost zero.8
CWI comes out on top. CWI, also called an ice-bath, is typically performed in the field. The patient is submerged up to the neck in a tub containing ice and water. Circulating the water and ice mixture helps accelerate cooling.
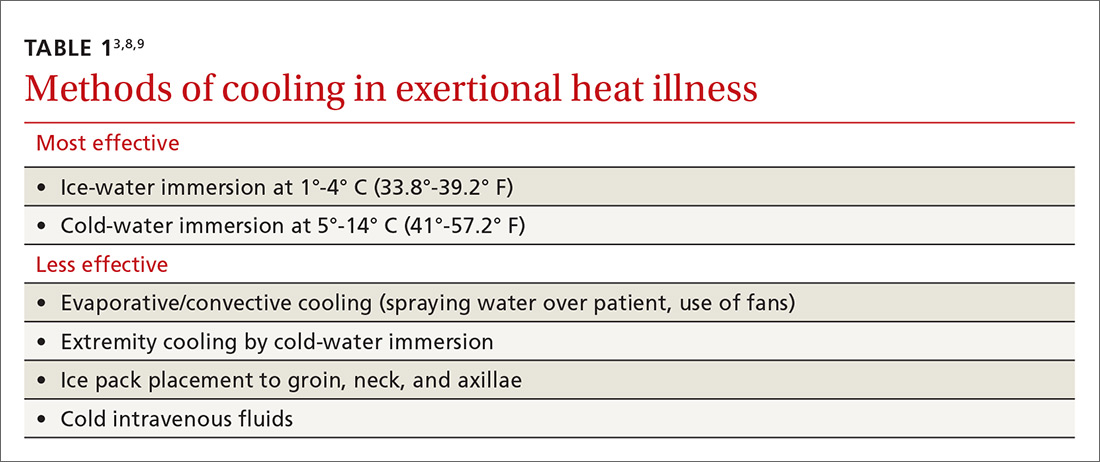
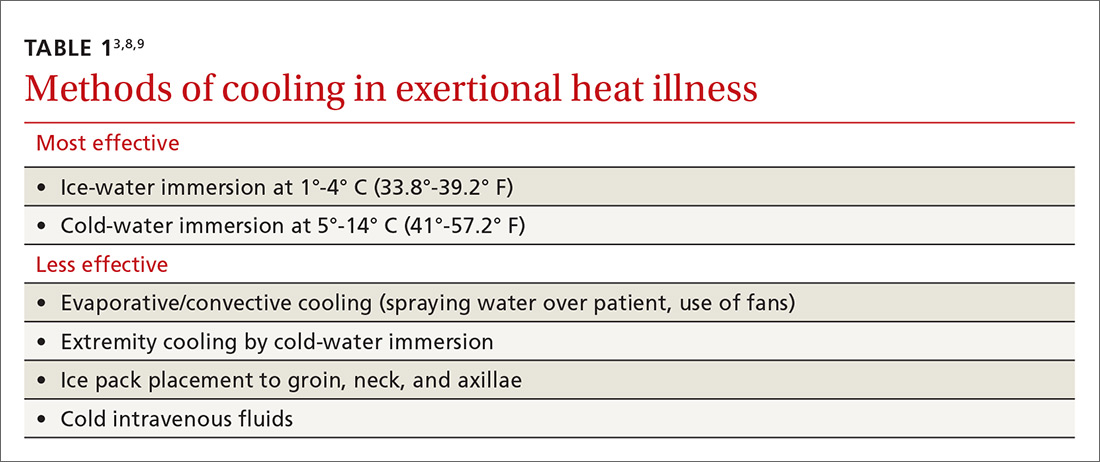
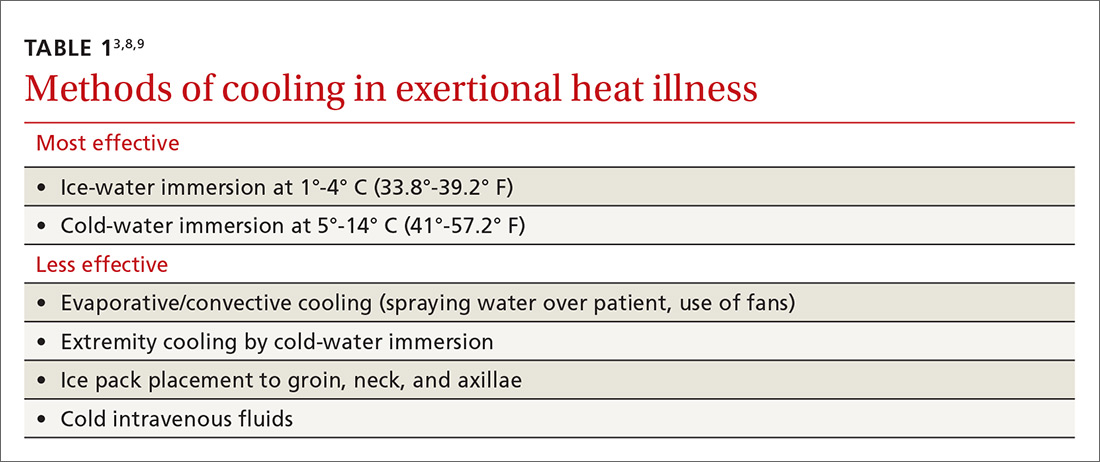
There have been differences in opinion regarding which cooling method is superior3 (TABLE 13,8,9). Traditionally, there were some concerns that CWI might actually increase body temperature via peripheral vasoconstriction and shivering. But current research suggests that for exertional heat stroke, CWI to promote conductive cooling is the most effective strategy.3,8,10,11 A review of cooling rates in healthy hyperthermic athletes and heat stroke victims showed that ice-water immersion or CWI at 1° to 14° C (35.6°-57.2° F) is superior to all other types of cooling, including ice packs, fans, and partial-body ice-water immersion.10
Furthermore, a 2015 meta-analysis looking at optimal procedures for cooling found that CWI cooled patients twice as fast as passive cooling (without any treatment).11 When cooling with CWI, core temperature drops about 0.2° C/min (0.36° F/min).10 Therefore, the temperature can be expected to drop about 1° C (1.8° F) for every 5 minutes of immersion. When unable to monitor a rectal temperature continuously, 10 to 15 minutes of immersion should get most patients below 40° C (104° F).
Extremity cooling. While CWI is the standard for cases of exertional heat illness, whole-body immersion is not always possible. In such cases, extremity cooling can be an effective body cooling method for exertional heat-related illness.12 Research has shown evaporative and convective cooling methods to have benefits for nonexertional heat-related illnesses.3,8,9 These methods usually involve directing air currents over exposed skin and spraying water on the affected individual.3
Contine to: Guidlines for transport
Guidelines for transport: Cool first, transport second
Most patients suspected of suffering from heat stroke should be transported to a hospital for further evaluation because of the high morbidity and mortality rates associated with it. However, cooling techniques should be implemented while awaiting transport. The current standard is “cool first, transport second.”7 Cooling interventions should continue in the ambulance if the core body temperature is still elevated. Techniques that can be used include the use of air conditioning, convective methods, and administration of IV fluids. As previously discussed, core body temperature should be continuously monitored. Cooling measures should be discontinued only when the patient’s rectal temperature reaches 38.9° C (102° F). Overly aggressive prehospital cooling beyond this point can result in prolonged hypothermia as well as cardiac arrhythmias.6
Monitoring and further evaluation
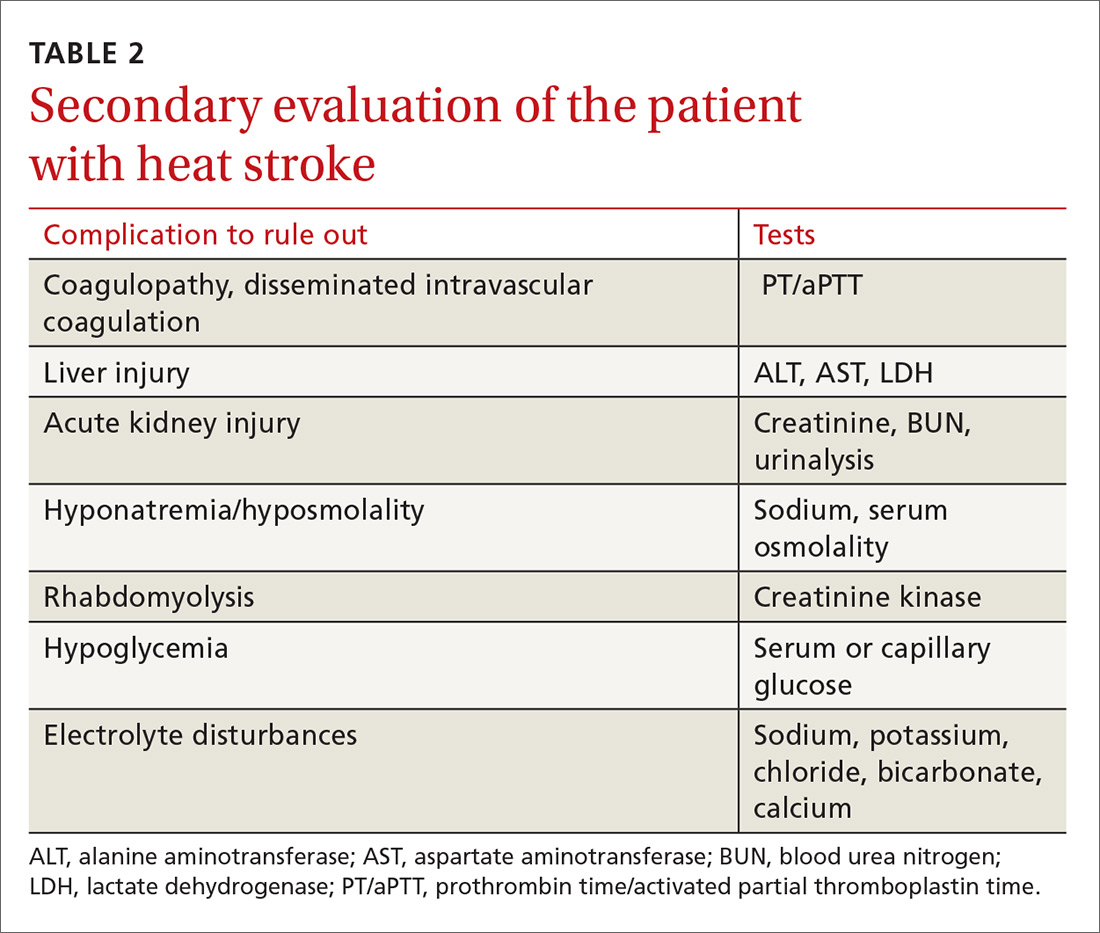
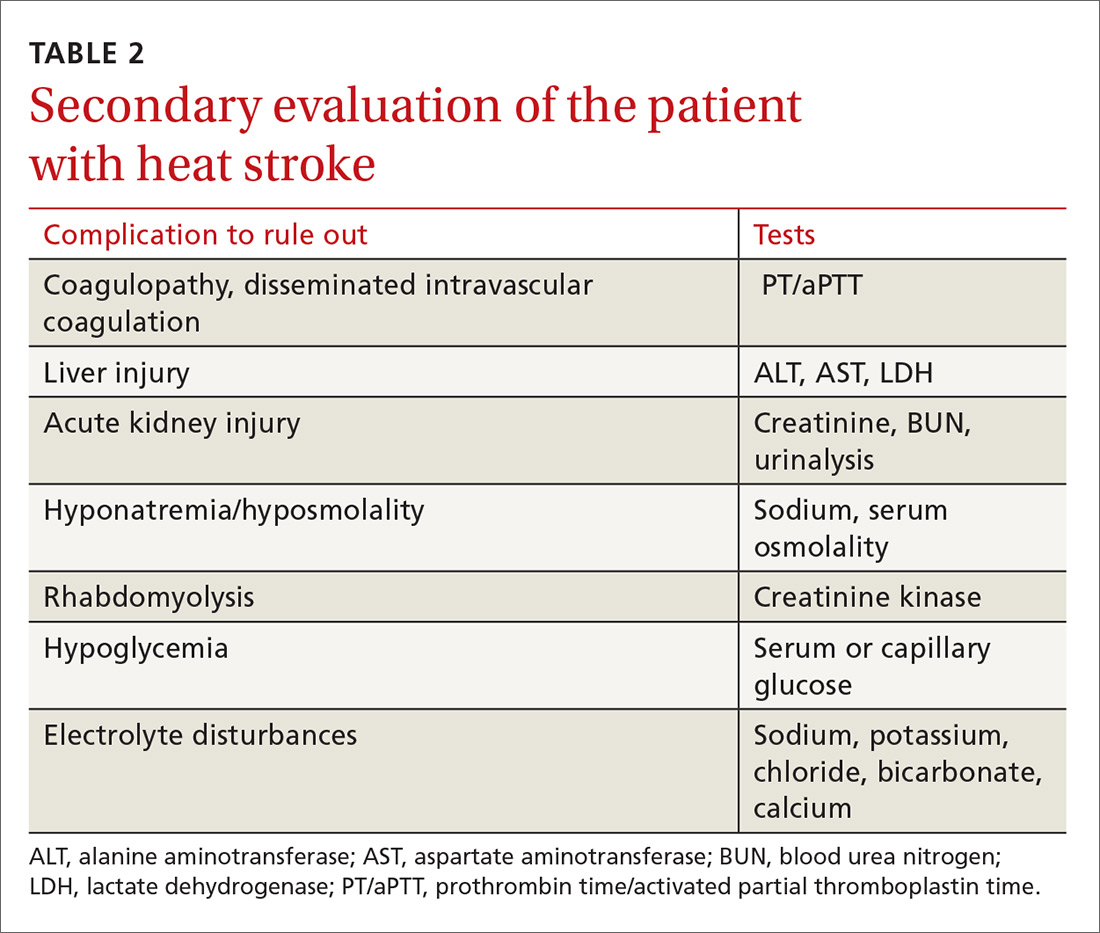
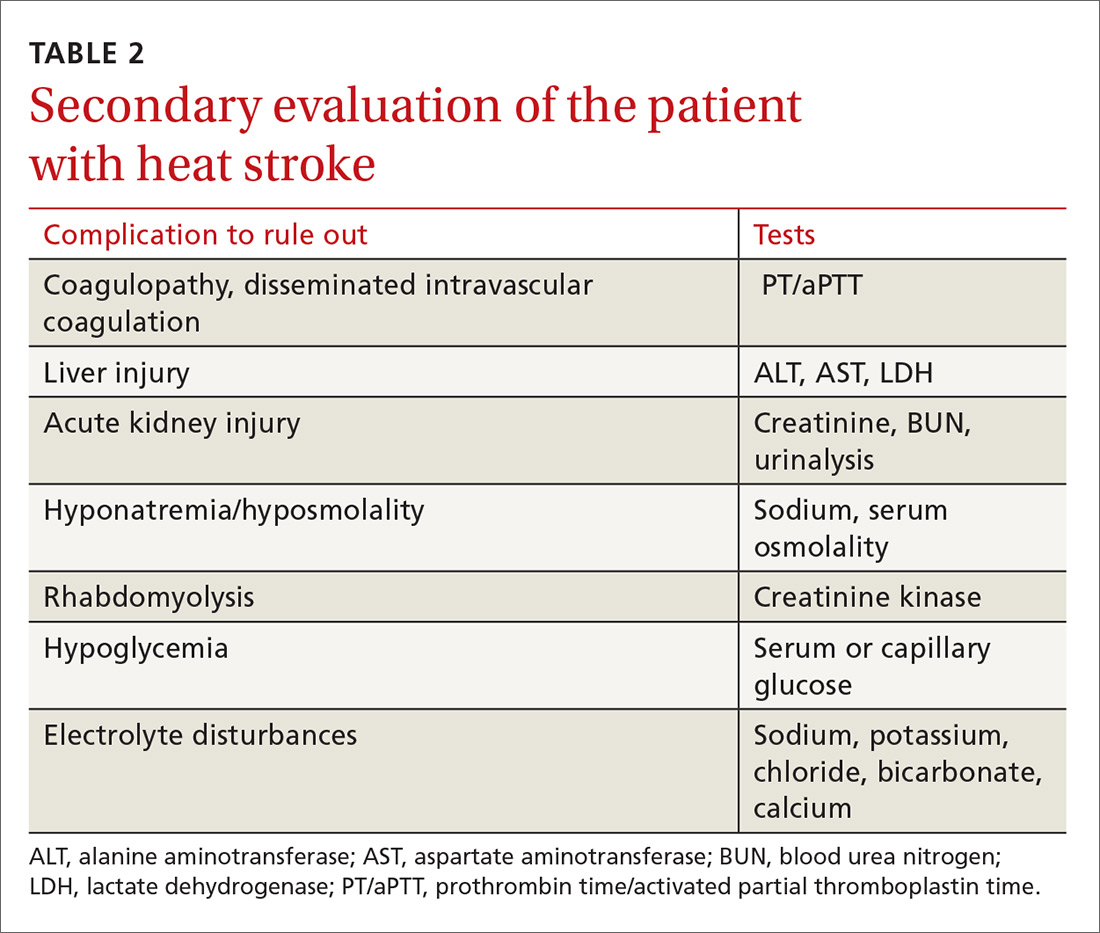
Monitoring patients with heat-related illness can be difficult, especially when utilizing CWI, as this may limit the ability to use devices such as a cardiac monitor or to continuously monitor rectal temperature. Beyond lowering core body temperature to below 39° C (102.2° F), early evaluation and treatment of other organ systems is vital, keeping in mind that these patients may develop multisystem organ failure. The initial work-up is listed in TABLE 2.
Depending on the severity of the injury and whether you suspect another diagnosis at work, additional studies may include urine output monitoring with a Foley catheter, electrocardiogram, chest radiograph, toxicology screen, a serum lactate level, and cardiac biomarkers.
Imaging. When evaluating for heat stroke, it usually isn’t necessary to obtain head imaging initially, as there are rarely abnormal findings in the early stages. Imaging may be obtained, however, if there is concern about a head injury or if neurologic abnormalities persist into later stages of treatment.5
Pharmacologic agents have not been shown to be of benefit in the treatment of heat-related illness. While dantrolene is commonly used in the treatment of neuroleptic malignant syndrome and malignant hyperthermia, the literature has not described any benefit associated with this agent in relation to heat-related illness. The same goes for antipyretics. Researchers have hypothesized that the reason these agents are ineffective is because body temperature is raised via a different mechanism in these conditions vs heat stroke.3
Continue to: Prevention
Prevention: Modifications and acclimatization are key
People who know they will be exposed to extreme heat should attempt to modify activities. There are many predisposing risk factors ranging from fever and illness to fatigue and dehydration. Risks can be minimized with physiologic adaptation through acclimatization, as well as making various behavioral changes such as adjusting activities, ensuring adequate hydration, and wearing appropriate clothing.13
Certain types of equipment, such as football helmets, can increase the risk of heat-related illness because they prevent heat exchange; however, the benefits sometimes outweigh the risks. With this in mind, consider modification of clothing and equipment if possible.1
In order to prevent heat-related illness, individuals should prehydrate prior to an event and replace fluids orally in order to prevent a >2% loss in body weight. Greater than a 2% loss directly correlates with increased core temperatures during exercise.1
Care should also be taken to perform regular physical activity prior to extreme heat exposure.1 Heat acclimatization takes place when a person’s body adapts to a hotter climate than they are accustomed to. This process can take up to 2 weeks, but once heat acclimation is accomplished, the person will have undergone physical changes, such as reduced metabolic heat production, which will decrease the risk of heat-related illness.13
Return to activity: Customize the approach
Each heat-related injury case is different; thus, return to activity should be individualized. In patients whose heat injury was believed to be secondary to a modifiable risk factor, efforts should be made to correct the predisposing factors that placed the patient at increased risk in the first place.
Additionally, the patient should allow sufficient time to recover. Guidelines recommend at least 1 to 2 weeks recovery before return to activity after heat stroke.8 Moreover, a graded return to activity, starting in a cool environment, is recommended. Gradual introduction of activity in the heat with close monitoring can help with acclimatization and help identify participants who continue to have cooling dysregulation. In the military and among athletes, tools such as heat-tolerance testing can be used to gauge the person’s readiness to return to play or duty.8 Heat tolerance testing is performed in a lab using continuous core temperature monitoring while having the subject exercise in a heated room.
CORRESPONDENCE
Scott Kinkade, MD, EdD, MA303 Medical Sciences Building, DC032.00, Columbia, MO 65212; [email protected].
1. Lipman GS, Eifling KP, Ellis MA, et al. Wilderness Medical Society practice guidelines for the prevention and treatment of heat-related illness: 2014 update. Wilderness Environ Med. 2014;25(4 Suppl):S55-S65.
2. Update: Heat injuries, active component, U.S. Armed Forces, 2014. MSMR. 2015;22:17-20.
3. Gaudio FG, Grissom CK. Cooling methods in heat stroke. J Emerg Med. 2016;50:607-616.
4. Hess JJ, Saha S, Luber G. Summertime acute heat illness in U.S. emergency departments from 2006 through 2010: analysis of a nationally representative sample. Environ Health Perspect. 2014;122:1209-1215.
5. People’s Liberation Army Professional Committee of Critical Care Medicine. Expert consensus on standardized diagnosis and treatment for heat stroke. Mil Med Res. 2016;3:1.
6. Stewart TE, Whitford AC. Dangers of prehospital cooling: a case report of afterdrop in a patient with exertional heat stroke. J Emerg Med. 2015;49:630-633.
7. Chan YK, Mamat M. Management of heat stroke. Trends Anaesthesia Crit Care. 2015;5:65-69.
8. Casa DJ, Armstrong LE, Kenny GP, et al. Exertional heat stroke: new concepts regarding cause and care. Curr Sports Med Rep. 2012;11:115-123.
9. Demartini JK, Casa DJ, Stearns R, et al. Effectiveness of cold water immersion in the treatment of exertional heat stroke at the Falmouth Road Race. Med Sci Sports Exerc. 2015;47:240-245.
10. Casa DJ, McDermott BP, Lee EC, et al. Cold water immersion: the gold standard for exertional heatstroke treatment. Exerc Sport Sci Rev. 2007;35:141-149.
11. Zhang Y, Davis JK, Casa DJ, et al. Optimizing cold water immersion for exercise-induced hyperthermia: a meta-analysis. Med Sci Sports Exerc. 2015;47:2464-2472.
12. DeGroot DW, Kenefick RW, Sawka MN. Impact of arm immersion cooling during ranger training on exertional heat illness and treatment costs. Mil Med. 2015;180:1178-1183.
13. Epstein Y, Druyan A, Heled Y. Heat injury prevention—a military perspective. J Strength Cond Res. 2012;26 (suppl 2):S82-S86.
Heat-related illnesses can affect people of any age who are subjected to extreme heat and humidity regardless of physical fitness level or baseline health status. The most serious of the heat-related illnesses is heat stroke. Prompt identification, early initiation of cooling measures (including cold-water immersion [CWI]), and transport to a higher level of care, when appropriate, are imperative. This article reviews heat-related illness identification, as well as management strategies.
Heat-related illnesses: From the benign to the severe
Some of the less severe forms of heat-related illness include heat cramps (which are due to dehydration and salt loss), heat rash, and heat edema. Heat rash and heat edema are benign. Heat rash typically resolves with cooler clothing and a cooler environment. Heat edema tends to improve after sleeping in a cooler environment with legs elevated. Heat syncope is the result of decreased cerebral perfusion due to fluid loss and vasodilation that results in a distributive hypovolemia. It commonly occurs after vigorous exercise when the athlete is standing still.
Heat exhaustion requires a more careful clinical assessment. It is the inability to continue activity in the heat, often with weakness and collapse. Also due to salt and water losses, it results in cardiovascular output that is insufficient to meet the circulatory and metabolic demands of the body. The body temperature is often elevated but <40° C (104° F), vomiting can occur, and mild central nervous system (CNS) dysfunction may be present.
Heat stroke is the most severe form of heat-related illness and can be life-threatening.1
It is important to understand that these heat-related illnesses do not progress along a continuum. Patients develop heat stroke without having had milder forms of heat illness, and patients with a milder type of heat illness usually do not progress to heat stroke.
Heat stroke: Definition, types, risk factors
Heat stroke is defined as a core body temperature ≥40° C (104° F) with CNS dysfunction in the setting of environmental heat stress. The mortality rate can reach over 50%.2-6
There are 2 main types of heat stroke: exertional heat stroke and nonexertional (classic) heat stroke. Exertional heat stroke more commonly affects healthy, young people, such as athletes or military personnel. Classic (nonexertional) heat stroke patients are typically elderly and/or have a chronic illness, although occasionally it involves children who are unable to escape from a hot environment.5,7 While exertional heat stroke typically develops over a period of a few hours in participants of prolonged activities, such as marathons, classic heat stroke in the elderly typically develops over a period of days in the setting of high environmental temperatures. In both conditions, there is an inability to maintain a normal body temperature leading to CNS dysregulation with altered mental status and often multisystem organ dysfunction.7
Continue to: Risk factors
Risk factors. Heat-related illness can affect patients of all ages and levels of physical fitness; however, certain factors place patients at increased risk. These include physical deconditioning, dehydration, high levels of exercise intensity, obesity, elevated environmental temperatures, sleep deprivation, certain medications, alcohol and drug abuse, concurrent illness, and wearing excessive clothing or equipment. It is imperative that severe cases of heat illness be identified early and treatment be initiated rapidly, as delays in cooling can significantly increase the fatality rate.5
Management: First suspect the diagnosis
Health care providers must first suspect heat-related illness and then accurately diagnose it. It is important to differentiate heat-related illness from syncope, cardiac abnormalities, gastroenteritis, hypoglycemia, and other entities that require alternate management. For cases of collapse, syncope or near-syncope, or altered mental status during exertion, heat stroke should be the default diagnosis until proven otherwise.
Obtain a core body temperature. While attending to airway, breathing, and circulation, obtain a core body temperature. Rectal (or esophageal) core temperatures provide a reliable reading that can assist in determining the severity of the heat illness. Axillary, tympanic, temporal, oral, and skin temperatures are affected by environmental factors and are not accurate determinants of core body temperature.8
Once heat stroke is diagnosed, the physician must immediately initiate cooling by removing clothing, placing the patient in the shade or an air-conditioned area, and beginning aggressive cooling measures (more on this in a bit). While field management requires an accurate diagnosis of the severity of a patient’s heat-related illness, one should not delay treatment in order to obtain a rectal temperature.
When treating the milder forms of heat illness, administer oral or intravenous (IV) isotonic fluids. For heat cramps, stretching the affected muscle can help. For heat syncope, lying the patient down and elevating the legs restores perfusion. Patients with heat exhaustion will require some cooling measures such as relocation to a shaded area, removal of excess clothing, and the use of cold towels, along with hydration and elevation of the feet.
Continue to: Cooling techniques for heat stroke
Cooling techniques for heat stroke
In order to adequately cool a patient suffering from heat stroke, health care providers must create a gradient for heat to escape the body through the skin into the environment by conduction, convection, or evaporation.3 Cooling heat stroke patients to less than 40° C (104° F) within 30 minutes after collapse decreases the fatality rate to almost zero.8
CWI comes out on top. CWI, also called an ice-bath, is typically performed in the field. The patient is submerged up to the neck in a tub containing ice and water. Circulating the water and ice mixture helps accelerate cooling.
There have been differences in opinion regarding which cooling method is superior3 (TABLE 13,8,9). Traditionally, there were some concerns that CWI might actually increase body temperature via peripheral vasoconstriction and shivering. But current research suggests that for exertional heat stroke, CWI to promote conductive cooling is the most effective strategy.3,8,10,11 A review of cooling rates in healthy hyperthermic athletes and heat stroke victims showed that ice-water immersion or CWI at 1° to 14° C (35.6°-57.2° F) is superior to all other types of cooling, including ice packs, fans, and partial-body ice-water immersion.10
Furthermore, a 2015 meta-analysis looking at optimal procedures for cooling found that CWI cooled patients twice as fast as passive cooling (without any treatment).11 When cooling with CWI, core temperature drops about 0.2° C/min (0.36° F/min).10 Therefore, the temperature can be expected to drop about 1° C (1.8° F) for every 5 minutes of immersion. When unable to monitor a rectal temperature continuously, 10 to 15 minutes of immersion should get most patients below 40° C (104° F).
Extremity cooling. While CWI is the standard for cases of exertional heat illness, whole-body immersion is not always possible. In such cases, extremity cooling can be an effective body cooling method for exertional heat-related illness.12 Research has shown evaporative and convective cooling methods to have benefits for nonexertional heat-related illnesses.3,8,9 These methods usually involve directing air currents over exposed skin and spraying water on the affected individual.3
Contine to: Guidlines for transport
Guidelines for transport: Cool first, transport second
Most patients suspected of suffering from heat stroke should be transported to a hospital for further evaluation because of the high morbidity and mortality rates associated with it. However, cooling techniques should be implemented while awaiting transport. The current standard is “cool first, transport second.”7 Cooling interventions should continue in the ambulance if the core body temperature is still elevated. Techniques that can be used include the use of air conditioning, convective methods, and administration of IV fluids. As previously discussed, core body temperature should be continuously monitored. Cooling measures should be discontinued only when the patient’s rectal temperature reaches 38.9° C (102° F). Overly aggressive prehospital cooling beyond this point can result in prolonged hypothermia as well as cardiac arrhythmias.6
Monitoring and further evaluation
Monitoring patients with heat-related illness can be difficult, especially when utilizing CWI, as this may limit the ability to use devices such as a cardiac monitor or to continuously monitor rectal temperature. Beyond lowering core body temperature to below 39° C (102.2° F), early evaluation and treatment of other organ systems is vital, keeping in mind that these patients may develop multisystem organ failure. The initial work-up is listed in TABLE 2.
Depending on the severity of the injury and whether you suspect another diagnosis at work, additional studies may include urine output monitoring with a Foley catheter, electrocardiogram, chest radiograph, toxicology screen, a serum lactate level, and cardiac biomarkers.
Imaging. When evaluating for heat stroke, it usually isn’t necessary to obtain head imaging initially, as there are rarely abnormal findings in the early stages. Imaging may be obtained, however, if there is concern about a head injury or if neurologic abnormalities persist into later stages of treatment.5
Pharmacologic agents have not been shown to be of benefit in the treatment of heat-related illness. While dantrolene is commonly used in the treatment of neuroleptic malignant syndrome and malignant hyperthermia, the literature has not described any benefit associated with this agent in relation to heat-related illness. The same goes for antipyretics. Researchers have hypothesized that the reason these agents are ineffective is because body temperature is raised via a different mechanism in these conditions vs heat stroke.3
Continue to: Prevention
Prevention: Modifications and acclimatization are key
People who know they will be exposed to extreme heat should attempt to modify activities. There are many predisposing risk factors ranging from fever and illness to fatigue and dehydration. Risks can be minimized with physiologic adaptation through acclimatization, as well as making various behavioral changes such as adjusting activities, ensuring adequate hydration, and wearing appropriate clothing.13
Certain types of equipment, such as football helmets, can increase the risk of heat-related illness because they prevent heat exchange; however, the benefits sometimes outweigh the risks. With this in mind, consider modification of clothing and equipment if possible.1
In order to prevent heat-related illness, individuals should prehydrate prior to an event and replace fluids orally in order to prevent a >2% loss in body weight. Greater than a 2% loss directly correlates with increased core temperatures during exercise.1
Care should also be taken to perform regular physical activity prior to extreme heat exposure.1 Heat acclimatization takes place when a person’s body adapts to a hotter climate than they are accustomed to. This process can take up to 2 weeks, but once heat acclimation is accomplished, the person will have undergone physical changes, such as reduced metabolic heat production, which will decrease the risk of heat-related illness.13
Return to activity: Customize the approach
Each heat-related injury case is different; thus, return to activity should be individualized. In patients whose heat injury was believed to be secondary to a modifiable risk factor, efforts should be made to correct the predisposing factors that placed the patient at increased risk in the first place.
Additionally, the patient should allow sufficient time to recover. Guidelines recommend at least 1 to 2 weeks recovery before return to activity after heat stroke.8 Moreover, a graded return to activity, starting in a cool environment, is recommended. Gradual introduction of activity in the heat with close monitoring can help with acclimatization and help identify participants who continue to have cooling dysregulation. In the military and among athletes, tools such as heat-tolerance testing can be used to gauge the person’s readiness to return to play or duty.8 Heat tolerance testing is performed in a lab using continuous core temperature monitoring while having the subject exercise in a heated room.
CORRESPONDENCE
Scott Kinkade, MD, EdD, MA303 Medical Sciences Building, DC032.00, Columbia, MO 65212; [email protected].
Heat-related illnesses can affect people of any age who are subjected to extreme heat and humidity regardless of physical fitness level or baseline health status. The most serious of the heat-related illnesses is heat stroke. Prompt identification, early initiation of cooling measures (including cold-water immersion [CWI]), and transport to a higher level of care, when appropriate, are imperative. This article reviews heat-related illness identification, as well as management strategies.
Heat-related illnesses: From the benign to the severe
Some of the less severe forms of heat-related illness include heat cramps (which are due to dehydration and salt loss), heat rash, and heat edema. Heat rash and heat edema are benign. Heat rash typically resolves with cooler clothing and a cooler environment. Heat edema tends to improve after sleeping in a cooler environment with legs elevated. Heat syncope is the result of decreased cerebral perfusion due to fluid loss and vasodilation that results in a distributive hypovolemia. It commonly occurs after vigorous exercise when the athlete is standing still.
Heat exhaustion requires a more careful clinical assessment. It is the inability to continue activity in the heat, often with weakness and collapse. Also due to salt and water losses, it results in cardiovascular output that is insufficient to meet the circulatory and metabolic demands of the body. The body temperature is often elevated but <40° C (104° F), vomiting can occur, and mild central nervous system (CNS) dysfunction may be present.
Heat stroke is the most severe form of heat-related illness and can be life-threatening.1
It is important to understand that these heat-related illnesses do not progress along a continuum. Patients develop heat stroke without having had milder forms of heat illness, and patients with a milder type of heat illness usually do not progress to heat stroke.
Heat stroke: Definition, types, risk factors
Heat stroke is defined as a core body temperature ≥40° C (104° F) with CNS dysfunction in the setting of environmental heat stress. The mortality rate can reach over 50%.2-6
There are 2 main types of heat stroke: exertional heat stroke and nonexertional (classic) heat stroke. Exertional heat stroke more commonly affects healthy, young people, such as athletes or military personnel. Classic (nonexertional) heat stroke patients are typically elderly and/or have a chronic illness, although occasionally it involves children who are unable to escape from a hot environment.5,7 While exertional heat stroke typically develops over a period of a few hours in participants of prolonged activities, such as marathons, classic heat stroke in the elderly typically develops over a period of days in the setting of high environmental temperatures. In both conditions, there is an inability to maintain a normal body temperature leading to CNS dysregulation with altered mental status and often multisystem organ dysfunction.7
Continue to: Risk factors
Risk factors. Heat-related illness can affect patients of all ages and levels of physical fitness; however, certain factors place patients at increased risk. These include physical deconditioning, dehydration, high levels of exercise intensity, obesity, elevated environmental temperatures, sleep deprivation, certain medications, alcohol and drug abuse, concurrent illness, and wearing excessive clothing or equipment. It is imperative that severe cases of heat illness be identified early and treatment be initiated rapidly, as delays in cooling can significantly increase the fatality rate.5
Management: First suspect the diagnosis
Health care providers must first suspect heat-related illness and then accurately diagnose it. It is important to differentiate heat-related illness from syncope, cardiac abnormalities, gastroenteritis, hypoglycemia, and other entities that require alternate management. For cases of collapse, syncope or near-syncope, or altered mental status during exertion, heat stroke should be the default diagnosis until proven otherwise.
Obtain a core body temperature. While attending to airway, breathing, and circulation, obtain a core body temperature. Rectal (or esophageal) core temperatures provide a reliable reading that can assist in determining the severity of the heat illness. Axillary, tympanic, temporal, oral, and skin temperatures are affected by environmental factors and are not accurate determinants of core body temperature.8
Once heat stroke is diagnosed, the physician must immediately initiate cooling by removing clothing, placing the patient in the shade or an air-conditioned area, and beginning aggressive cooling measures (more on this in a bit). While field management requires an accurate diagnosis of the severity of a patient’s heat-related illness, one should not delay treatment in order to obtain a rectal temperature.
When treating the milder forms of heat illness, administer oral or intravenous (IV) isotonic fluids. For heat cramps, stretching the affected muscle can help. For heat syncope, lying the patient down and elevating the legs restores perfusion. Patients with heat exhaustion will require some cooling measures such as relocation to a shaded area, removal of excess clothing, and the use of cold towels, along with hydration and elevation of the feet.
Continue to: Cooling techniques for heat stroke
Cooling techniques for heat stroke
In order to adequately cool a patient suffering from heat stroke, health care providers must create a gradient for heat to escape the body through the skin into the environment by conduction, convection, or evaporation.3 Cooling heat stroke patients to less than 40° C (104° F) within 30 minutes after collapse decreases the fatality rate to almost zero.8
CWI comes out on top. CWI, also called an ice-bath, is typically performed in the field. The patient is submerged up to the neck in a tub containing ice and water. Circulating the water and ice mixture helps accelerate cooling.
There have been differences in opinion regarding which cooling method is superior3 (TABLE 13,8,9). Traditionally, there were some concerns that CWI might actually increase body temperature via peripheral vasoconstriction and shivering. But current research suggests that for exertional heat stroke, CWI to promote conductive cooling is the most effective strategy.3,8,10,11 A review of cooling rates in healthy hyperthermic athletes and heat stroke victims showed that ice-water immersion or CWI at 1° to 14° C (35.6°-57.2° F) is superior to all other types of cooling, including ice packs, fans, and partial-body ice-water immersion.10
Furthermore, a 2015 meta-analysis looking at optimal procedures for cooling found that CWI cooled patients twice as fast as passive cooling (without any treatment).11 When cooling with CWI, core temperature drops about 0.2° C/min (0.36° F/min).10 Therefore, the temperature can be expected to drop about 1° C (1.8° F) for every 5 minutes of immersion. When unable to monitor a rectal temperature continuously, 10 to 15 minutes of immersion should get most patients below 40° C (104° F).
Extremity cooling. While CWI is the standard for cases of exertional heat illness, whole-body immersion is not always possible. In such cases, extremity cooling can be an effective body cooling method for exertional heat-related illness.12 Research has shown evaporative and convective cooling methods to have benefits for nonexertional heat-related illnesses.3,8,9 These methods usually involve directing air currents over exposed skin and spraying water on the affected individual.3
Contine to: Guidlines for transport
Guidelines for transport: Cool first, transport second
Most patients suspected of suffering from heat stroke should be transported to a hospital for further evaluation because of the high morbidity and mortality rates associated with it. However, cooling techniques should be implemented while awaiting transport. The current standard is “cool first, transport second.”7 Cooling interventions should continue in the ambulance if the core body temperature is still elevated. Techniques that can be used include the use of air conditioning, convective methods, and administration of IV fluids. As previously discussed, core body temperature should be continuously monitored. Cooling measures should be discontinued only when the patient’s rectal temperature reaches 38.9° C (102° F). Overly aggressive prehospital cooling beyond this point can result in prolonged hypothermia as well as cardiac arrhythmias.6
Monitoring and further evaluation
Monitoring patients with heat-related illness can be difficult, especially when utilizing CWI, as this may limit the ability to use devices such as a cardiac monitor or to continuously monitor rectal temperature. Beyond lowering core body temperature to below 39° C (102.2° F), early evaluation and treatment of other organ systems is vital, keeping in mind that these patients may develop multisystem organ failure. The initial work-up is listed in TABLE 2.
Depending on the severity of the injury and whether you suspect another diagnosis at work, additional studies may include urine output monitoring with a Foley catheter, electrocardiogram, chest radiograph, toxicology screen, a serum lactate level, and cardiac biomarkers.
Imaging. When evaluating for heat stroke, it usually isn’t necessary to obtain head imaging initially, as there are rarely abnormal findings in the early stages. Imaging may be obtained, however, if there is concern about a head injury or if neurologic abnormalities persist into later stages of treatment.5
Pharmacologic agents have not been shown to be of benefit in the treatment of heat-related illness. While dantrolene is commonly used in the treatment of neuroleptic malignant syndrome and malignant hyperthermia, the literature has not described any benefit associated with this agent in relation to heat-related illness. The same goes for antipyretics. Researchers have hypothesized that the reason these agents are ineffective is because body temperature is raised via a different mechanism in these conditions vs heat stroke.3
Continue to: Prevention
Prevention: Modifications and acclimatization are key
People who know they will be exposed to extreme heat should attempt to modify activities. There are many predisposing risk factors ranging from fever and illness to fatigue and dehydration. Risks can be minimized with physiologic adaptation through acclimatization, as well as making various behavioral changes such as adjusting activities, ensuring adequate hydration, and wearing appropriate clothing.13
Certain types of equipment, such as football helmets, can increase the risk of heat-related illness because they prevent heat exchange; however, the benefits sometimes outweigh the risks. With this in mind, consider modification of clothing and equipment if possible.1
In order to prevent heat-related illness, individuals should prehydrate prior to an event and replace fluids orally in order to prevent a >2% loss in body weight. Greater than a 2% loss directly correlates with increased core temperatures during exercise.1
Care should also be taken to perform regular physical activity prior to extreme heat exposure.1 Heat acclimatization takes place when a person’s body adapts to a hotter climate than they are accustomed to. This process can take up to 2 weeks, but once heat acclimation is accomplished, the person will have undergone physical changes, such as reduced metabolic heat production, which will decrease the risk of heat-related illness.13
Return to activity: Customize the approach
Each heat-related injury case is different; thus, return to activity should be individualized. In patients whose heat injury was believed to be secondary to a modifiable risk factor, efforts should be made to correct the predisposing factors that placed the patient at increased risk in the first place.
Additionally, the patient should allow sufficient time to recover. Guidelines recommend at least 1 to 2 weeks recovery before return to activity after heat stroke.8 Moreover, a graded return to activity, starting in a cool environment, is recommended. Gradual introduction of activity in the heat with close monitoring can help with acclimatization and help identify participants who continue to have cooling dysregulation. In the military and among athletes, tools such as heat-tolerance testing can be used to gauge the person’s readiness to return to play or duty.8 Heat tolerance testing is performed in a lab using continuous core temperature monitoring while having the subject exercise in a heated room.
CORRESPONDENCE
Scott Kinkade, MD, EdD, MA303 Medical Sciences Building, DC032.00, Columbia, MO 65212; [email protected].
1. Lipman GS, Eifling KP, Ellis MA, et al. Wilderness Medical Society practice guidelines for the prevention and treatment of heat-related illness: 2014 update. Wilderness Environ Med. 2014;25(4 Suppl):S55-S65.
2. Update: Heat injuries, active component, U.S. Armed Forces, 2014. MSMR. 2015;22:17-20.
3. Gaudio FG, Grissom CK. Cooling methods in heat stroke. J Emerg Med. 2016;50:607-616.
4. Hess JJ, Saha S, Luber G. Summertime acute heat illness in U.S. emergency departments from 2006 through 2010: analysis of a nationally representative sample. Environ Health Perspect. 2014;122:1209-1215.
5. People’s Liberation Army Professional Committee of Critical Care Medicine. Expert consensus on standardized diagnosis and treatment for heat stroke. Mil Med Res. 2016;3:1.
6. Stewart TE, Whitford AC. Dangers of prehospital cooling: a case report of afterdrop in a patient with exertional heat stroke. J Emerg Med. 2015;49:630-633.
7. Chan YK, Mamat M. Management of heat stroke. Trends Anaesthesia Crit Care. 2015;5:65-69.
8. Casa DJ, Armstrong LE, Kenny GP, et al. Exertional heat stroke: new concepts regarding cause and care. Curr Sports Med Rep. 2012;11:115-123.
9. Demartini JK, Casa DJ, Stearns R, et al. Effectiveness of cold water immersion in the treatment of exertional heat stroke at the Falmouth Road Race. Med Sci Sports Exerc. 2015;47:240-245.
10. Casa DJ, McDermott BP, Lee EC, et al. Cold water immersion: the gold standard for exertional heatstroke treatment. Exerc Sport Sci Rev. 2007;35:141-149.
11. Zhang Y, Davis JK, Casa DJ, et al. Optimizing cold water immersion for exercise-induced hyperthermia: a meta-analysis. Med Sci Sports Exerc. 2015;47:2464-2472.
12. DeGroot DW, Kenefick RW, Sawka MN. Impact of arm immersion cooling during ranger training on exertional heat illness and treatment costs. Mil Med. 2015;180:1178-1183.
13. Epstein Y, Druyan A, Heled Y. Heat injury prevention—a military perspective. J Strength Cond Res. 2012;26 (suppl 2):S82-S86.
1. Lipman GS, Eifling KP, Ellis MA, et al. Wilderness Medical Society practice guidelines for the prevention and treatment of heat-related illness: 2014 update. Wilderness Environ Med. 2014;25(4 Suppl):S55-S65.
2. Update: Heat injuries, active component, U.S. Armed Forces, 2014. MSMR. 2015;22:17-20.
3. Gaudio FG, Grissom CK. Cooling methods in heat stroke. J Emerg Med. 2016;50:607-616.
4. Hess JJ, Saha S, Luber G. Summertime acute heat illness in U.S. emergency departments from 2006 through 2010: analysis of a nationally representative sample. Environ Health Perspect. 2014;122:1209-1215.
5. People’s Liberation Army Professional Committee of Critical Care Medicine. Expert consensus on standardized diagnosis and treatment for heat stroke. Mil Med Res. 2016;3:1.
6. Stewart TE, Whitford AC. Dangers of prehospital cooling: a case report of afterdrop in a patient with exertional heat stroke. J Emerg Med. 2015;49:630-633.
7. Chan YK, Mamat M. Management of heat stroke. Trends Anaesthesia Crit Care. 2015;5:65-69.
8. Casa DJ, Armstrong LE, Kenny GP, et al. Exertional heat stroke: new concepts regarding cause and care. Curr Sports Med Rep. 2012;11:115-123.
9. Demartini JK, Casa DJ, Stearns R, et al. Effectiveness of cold water immersion in the treatment of exertional heat stroke at the Falmouth Road Race. Med Sci Sports Exerc. 2015;47:240-245.
10. Casa DJ, McDermott BP, Lee EC, et al. Cold water immersion: the gold standard for exertional heatstroke treatment. Exerc Sport Sci Rev. 2007;35:141-149.
11. Zhang Y, Davis JK, Casa DJ, et al. Optimizing cold water immersion for exercise-induced hyperthermia: a meta-analysis. Med Sci Sports Exerc. 2015;47:2464-2472.
12. DeGroot DW, Kenefick RW, Sawka MN. Impact of arm immersion cooling during ranger training on exertional heat illness and treatment costs. Mil Med. 2015;180:1178-1183.
13. Epstein Y, Druyan A, Heled Y. Heat injury prevention—a military perspective. J Strength Cond Res. 2012;26 (suppl 2):S82-S86.
