User login
Point-of-care ultrasound is increasingly being integrated into clinical practice, as an adjunct to the physical examination and patient history,1 and into medical school curricula across North America.2,3 Research confirms that this technology improves patient survival in emergency medicine settings;4 however, the benefits of point-of-care ultrasound administered by family physicians (FPs) in the office setting are less well documented.
Here we provide a comprehensive review of the indications for ultrasound in the office setting, which range from diagnosing musculoskeletal injuries and guiding injections to screening for abdominal aortic aneurysm (AAA). We also address the accuracy and cost-effectiveness of ultrasound use and the training needed to make family medicine ultrasound (FAMUS) successful.
Ultrasound: A useful screening tool for abdominal aortic aneurysm
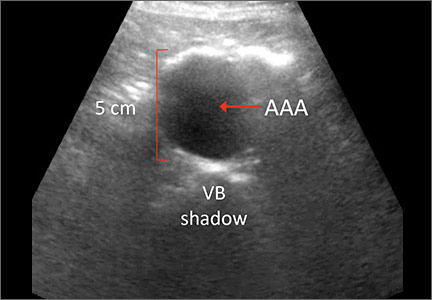
The US Preventive Services Task Force (USPSTF) recommends one-time screening for abdominal aortic aneurysm (AAA) in men ages 65 to 75 years who have ever smoked (See: http://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/abdominal-aortic-aneurysm-screening.) Ultrasound is a reliable tool for identifying AAA5 (FIGURE 1); its sensitivity and specificity range from 94% to 98.9% and 98% to 100%, respectively.6-9 It is also superior to physical examination for AAAs,10 which has a sensitivity of 29% for small AAAs (30-39 mm) and 76% for larger AAAs (>50 mm).11
Most importantly, research has demonstrated that long-term mortality benefits are associated with ultrasound screening of asymptomatic patients for AAA. For example, one study found that screening asymptomatic men ages 65 to 74 (a population-based sample, with no particular risk factors) for AAA resulted in a reduction in all-cause mortality and that the benefit of AAA-related mortality continued to accumulate throughout follow-up.12
In fact, nationwide programs to screen for AAA using ultrasound have been established in England, Northern Ireland, Scotland, Sweden, the United States, and Wales to help prevent deaths associated with AAA rupture.13 Despite the documented benefits of ultrasound screening for AAA, a large retrospective cohort study conducted in an American integrated health care system found that only about 9% of patients eligible for screening according to USPSTF guidelines were screened for AAA with ultrasound in primary care practices in 2012.14
While most AAA screening occurs in the hospital, screening for the condition can be just as easily and effectively performed in an FP’s office or outpatient clinic. A Canadian prospective observational study demonstrated that aortic diameter measurements were comparable whether they were obtained by ultrasound performed by an office-based physician (who had completed an emergency ultrasonography course and performed at least 50 ultrasonographer-supervised ultrasound scans of the aorta), or by a hospital-based technologist whose scans were then reviewed by a radiologist.15 (See the TABLE for an overview of the research involving family medicine ultrasound.)
The office-based scans had a high degree of correlation (0.81) with the hospital-based ones, a sensitivity and specificity of 100%, and lasted a mean of 3.5 minutes. The researchers concluded that ultrasound screening for AAA can be safely performed in the office setting by FPs who are trained to use point-of-care ultrasound technology, and that the screening can be completed within the time constraints of a typical family practice office visit.15
In a separate study, cardiologists compared hand-held ultrasound screening for AAA to standard 2-dimensional echocardiography. This study found that screening for AAA in an outpatient clinic with a hand-held ultrasound device is feasible and accurate with a sensitivity of 88% and a specificity of 98%.16
Ultrasound in the obstetrician’s office—and the FP’s office, too
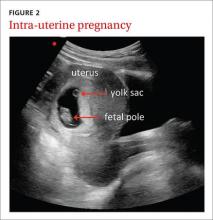
The use of ultrasound in obstetrics (FIGURE 2) is particularly well documented, with evidence supporting the use of FAMUS for various obstetrical indications dating back 30 years.17 The American Academy of Family Physicians has a position paper endorsing diagnostic ultrasound for women’s health care and has offered obstetric ultrasound courses organized by, and for, FPs since 1989.18
In a prospective observational study conducted in the United Kingdom, an FP and a nurse midwife used ultrasound to assess 240 pregnant women presenting with vaginal bleeding in early pregnancy.19 Fetal heartbeat detection by an office ultrasound scan predicted fetal progression to 20 weeks with a sensitivity of 97% and a specificity of 98%. The clinicians also detected anomalies such as molar pregnancy, blighted ovum, and ectopic pregnancy.
FAMUS and its ability to accurately estimate delivery date was examined in another prospective study involving 186 patients at a community health center.20 Accuracy for the estimated date of delivery was 96% using stratified confidence intervals for first-, second-, and third-trimester examinations. The office-based ultrasound scans also detected one case of placenta previa, one fetal death, and 2 unsuspected twin pregnancies. Another study showed no difference in estimations of gestational age provided by ultrasound performed by supervised FP residents with 3 years’ ultrasound training (including 3 lectures per year and an annual 4-hour workshop), and radiologists.21
Further evidence that FAMUS can confirm fetal death and multiple gestations was provided by a retrospective review of almost 498 obstetric ultrasound examinations.22 FPs accurately predicted the presence or absence of fetal death, multiple gestations, and the estimated date of confinement. Another study demonstrated that 86% of 248 FP obstetrical scans were judged acceptable by a radiologist, 10% were repeated due to technical errors and subsequently found to be acceptable, and 3% were unacceptable and referred for formal ultrasound.23 These scans were performed by FPs who completed 5 days of theory and hands-on training and 3 half-days of apprenticeship in an ultrasound laboratory.
In a study conducted in Tanzania, bedside ultrasound scans performed by nurse midwives had 100% agreement with scans performed by a sonographer when evaluating for twins, the presence of fetal heartbeat, or fetal positioning. Overall, bedside ultrasound aided in the diagnosis (39%) and management plan (22%) of 542 patients.24 It is important to note, as highlighted in a multisite study, that consultation with specialists when appropriate is paramount to the successful use of ultrasound by the FP for prenatal care.25
Guiding joint injections, assessing LV function
Sports/exercise medicine. FPs with expertise in sports and exercise medicine commonly use office ultrasound to diagnose musculoskeletal (MSK) injuries, including rotator cuff tears, muscle ruptures, tendinitis, and bursitis.26 It is superior to magnetic resonance imaging (MRI) in terms of cost-to-benefit ratio, precision, and sensitivity (due, in part, to the fact that clinicians can obtain patient feedback during the examination).26 In addition, a review of office-based procedures for MSK indications demonstrated the usefulness of ultrasound for the guidance of joint aspirations and joint and tendon injections.27 Ultrasound guidance is commonly used to ensure procedural accuracy during aspirations and injections of the shoulder (glenohumeral joint; subacromial bursa), elbow, wrist (carpal tunnel tendons), hip, knee, and ankle.27-29
Cardiology (FIGURE 3). General practitioners in Norway found that 8 hours of training on a hand-held ultrasound device was sufficient to assess left ventricular function with a sensitivity and specificity of 78% and 83%, respectively.30 Their measurements of septal mitral annular excursion (a surrogate measurement of left ventricular function) were similar to those of a cardiologist using the same device and added no more than 5 minutes to the examination.
Other uses. In a separate study, military FPs with 16 hours of training found that FAMUS was easy to learn and effective in the outpatient and inpatient setting for the detection of AAA, trauma, musculoskeletal injuries, and certain obstetric, echocardiographic, and biliary indications.31 They reported that the average time spent per ultrasound examination was one to 5 minutes for the majority of the indications.
The authors of a retrospective study involving a suburban family practice reported that FAMUS was successfully used to identify the causes of epigastric and right upper quadrant pain, and to check post-void residual urinary bladder volume.32
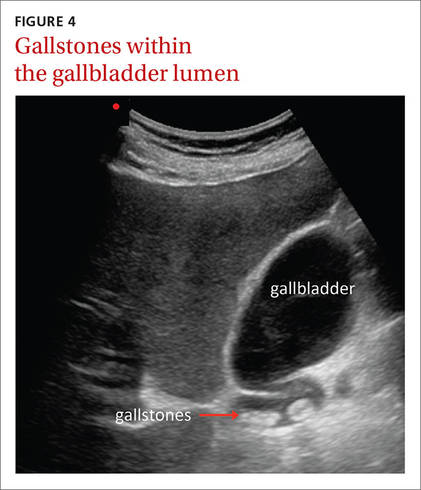
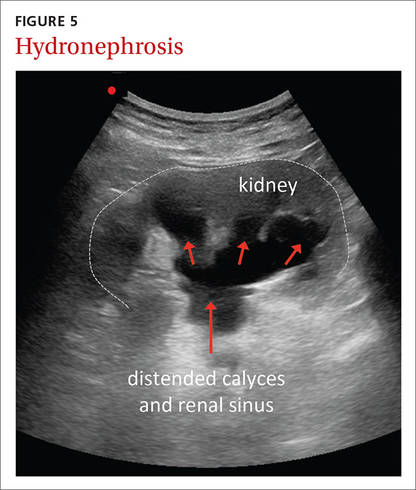
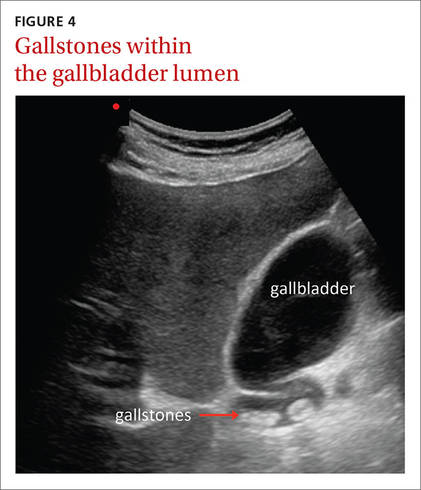
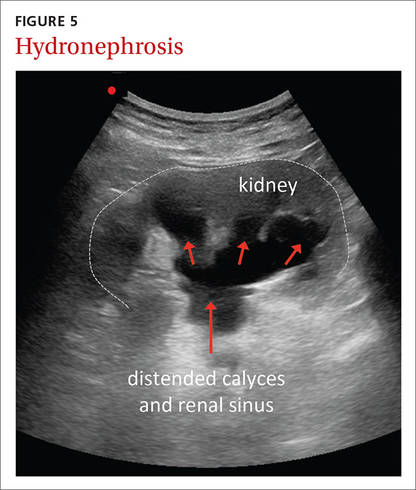
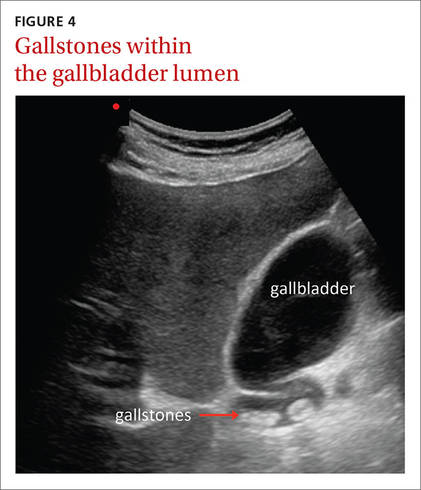
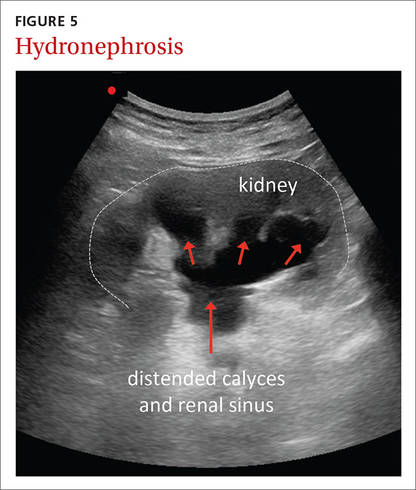
The ultrasound-assisted physical examination can detect pathologies not apparent on history and physical examination alone (FIGURES 4 and 5). In one study, an FP used ultrasound in the office to identify pathologies in 31% of patients that were not detected on physical examination alone. The pathologies included AAAs, a thyroid cyst, mitral stenosis, gallstones, renal cysts, urinary retention, hydronephrosis, ectopic kidney, and an endometrial tumor.33
| 
|
In another study, an FP performed ultrasound examinations on 189 patients during their annual exams.34 The technology identified pathologies that were not suspected after clinical assessment in 22% of these patients. With the emphasis in the current clinical landscape on choosing diagnostic tests wisely, it will be important to determine if findings like these positively impact patient care.35,36
Portable ultrasound machines are affordable
The relative affordability of portable ultrasound contributes to the cost-effectiveness of FAMUS. For FPs seeking to initiate an office-based ultrasound program, expenses to consider include the price of the machine itself, which ranges from $7500 to $50,000, depending on the technology included. Other expenses include the cost of disposables (eg, ultrasound gel and disinfectant wipes or spray), which may total about $400 per year.
In-office exams facilitate savings elsewhere. Other factors that contribute to the cost-effectiveness of FAMUS include reduced radiologist expenses and hospital visits. The cost savings of in-office ultrasound was highlighted almost 30 years ago when the cost of a FAMUS obstetrical scan was reported to be half that of a radiologist scan.23 This same study reported that increased costs for additional investigations caused by incidental findings using FAMUS could be offset by the decreased costs associated with an earlier diagnosis of serious conditions.23
A 2002 study demonstrated that office-based FAMUS scans (N=131) reduced the number of hospital scans, emergency admissions, and outpatient and inpatient hospital visits.37 Although the unit cost of a FAMUS scan was higher than an inpatient one, the total cost of the FAMUS scan was lower due to decreased hospital visits. In addition, research has shown that patients are more satisfied with office-based ultrasound examinations and prefer ultrasound performed by their FP to hospital-based ultrasound scans.31,37
Training: Cost and availability
Training in office-based ultrasound is available at the undergraduate, postgraduate, and continuing medical education levels. Undergraduate bedside ultrasound education is evident in medical schools around the globe including in Australia, Austria, Canada, China, Germany, France, the United States, and the United Kingdom.3 In an American survey of family medicine residency programs published in 2015, only 2.2% reported an established ultrasound curriculum; however, 29% had started a program within the past year.38 In Canada, one- and 2-day bedside ultrasound courses are offered to family medicine residents at a number of universities. And continuing medical education (CME) courses in bedside ultrasound are available to physicians on a regular basis internationally.39 In North America, CME courses exist specifically for urban and rural family medicine clinicians,40-43 and offer training for a wide range of applications.
Courses are often available for $1000 to $2000. Many of these courses run over a one- to 3-day period. Some provide a general overview of ultrasound for the primary care physician while others specialize in topics such as musculoskeletal uses, obstetric uses, or emergency department echocardiography.40-44
Challenges remain
More research is necessary to demonstrate that office-based ultrasound produces patient outcomes that are comparable to those resulting from hospital-based ultrasound. Also, bedside ultrasound is only as good as the operator who performs the examination,45 which highlights the importance of developing bedside ultrasound training programs tailored for FPs. National policies are essential for standardizing indications, training, and credentialing so that this effective tool can be used in a safe and effective manner.
CORRESPONDENCE
Peter Steinmetz, MD, CCFP, St. Mary’s Hospital, 3830 Ave Lacombe, Montreal, Quebec, Canada H3T1M5; [email protected].
ACKNOWLEDGEMENTS
We thank Assistant Professor Marion Dove, MD, CCFP, Department of Family Medicine, McGill University, for her suggestions and critical review of an earlier version of the manuscript. The term FAMUS is pending registration and is advertised with the Canadian Intellectual Property Office (Steinmetz, Volume 63, Issue 3217).
1. Solomon SD, Saldana F. Point-of-care ultrasound in medical education - stop listening and look. N Engl J Med. 2014;370:1083-1085.
2. Bahner DP, Goldman E, Way D, et al. The state of ultrasound education in U.S. medical schools: results of a national survey. Acad Med. 2014;89:1681-1686.
3. Steinmetz P, Dobrescu O, Oleskevich S, et al. Bedside ultrasound education in Canadian medical schools: a national survey. Can Med Educ J. 2016;7:e78-e86.
4. Deshpande R, Akhtar S, Haddadin AS. Utility of ultrasound in the ICU. Curr Opin Anaesthesiol. 2014;27:123-132.
5. Wilmink ABM, Hubbard CSFF, Quick CRG. Quality of the measurement of the infrarenal aortic diameter by ultrasound. J Med Screen. 1997;4:49-53.
6. Costantino TG, Bruno EC, Handly N, et al. Accuracy of emergency medicine ultrasound in the evaluation of abdominal aortic aneurysm. J Emerg Med. 2005;29:455-460.
7. Lindholt JS, Vammen S, Juul S, et al. The validity of ultrasonographic scanning as screening method for abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 1999;17:472-475.
8. Nusbaum JW, Freimanis AK, Thomford NR. Echography in the diagnosis of abdominal aortic aneurysm. Arch Surg. 1971;102:385-388.
9. Wilmink ABM, Forshaw M, Quick CRG, et al. Accuracy of serial screening for abdominal aortic aneurysms by ultrasound. J Med Screen. 2002;9:125-127.
10. Lynch RM. Accuracy of abdominal examination in the diagnosis of non-ruptured abdominal aortic aneurysm. Accid Emerg Nurs. 2004;12:99-107.
11. Lederle FA, Simel DL. The rational clinical examination. Does this patient have abdominal aortic aneurysm? JAMA. 1999;281:77-82.
12. Thompson SG, Ashton HA, Gao L, et al; Multicentre Aneurysm Screening Study (MASS) Group. Final follow-up of the Multicentre Aneurysm Screening Study (MASS) randomized trial of abdominal aortic aneurysm screening. Br J Surg. 2012;99:1649-1656.
13. Stather PW, Dattani N, Bown MJ, et al. International variations in AAA screening. Eur J Vasc Endovasc Surg. 2013;45:231-234.
14. Ruff AL, Teng K, Hu B, et al. Screening for abdominal aortic aneurysms in outpatient primary care clinics. Am J Med. 2015;128:283-288.
15. Blois B. Office-based ultrasound screening for abdominal aortic aneurysm. Can Fam Physician. 2012;58:e172-178.
16. Vourvouri EC, Poldermans D, Schinkel AF, et al. Abdominal aortic aneurysm screening using a hand-held ultrasound device. “A pilot study”. Eur J Vasc Endovasc Surg. 2001;22:352-354.
17. Hahn RG, Davies TC, Rodney WM. Diagnostic ultrasound in general practice. Fam Pract. 1988;5:129-135.
18. American Academy of Family Physicians. Position Paper: Diagnostic ultrasonography in women’s health care. 2013. Available at http://www.aafp.org/about/policies/all/ultrasonography-diagnostic.html. Accessed 2013.
19. Everett CB, Preece E. Women with bleeding in the first 20 weeks of pregnancy: value of general practice ultrasound in detecting fetal heart movement. Br J Gen Pract. 1996;46:7-9.
20. Rodney WM, Prislin MD, Orientale E, et al. Family practice obstetric ultrasound in an urban community health center. Birth outcomes and examination accuracy of the initial 227 cases. J Fam Pract. 1990;30:163-168.
21. Keith R, Frisch L. Fetal biometry: a comparison of family physicians and radiologists. Fam Med. 2001;33:111-114.
22. Ornstein SM, Smith MA, Peggs J, et al. Obstetric ultrasound by family physicians. Adequacy as assessed by pregnancy outcome. J Fam Pract. 1990;30:403-408.
23. Hahn RG, Ho S, Roi LD, et al. Cost-effectiveness of office obstetrical ultrasound in family practice: preliminary considerations. J Am Board Fam Pract. 1988;1:33-38.
24. Stein W, Katunda I, Butoto C. A two-level ultrasonographic service in a maternity care unit of a rural district hospital in Tanzania. Trop Doct. 2008;38:125-126.
25. Morgan WC, Rodney WM, Hahn R, et al. Ultrasound for the primary care physician. Applications in family-centered obstetrics. Postgrad Med. 1988;83:103-107.
26. Coris EE, Pescasio M, Zwygart K, et al. Office-based ultrasound in sports medicine practice. Clin J Sport Med. 2011;21:57-61.
27. Royall NA, Farrin E, Bahner DP, et al. Ultrasound-assisted musculoskeletal procedures: A practical overview of current literature. World J Orthop. 2011;2:57-66.
28. Bianchi S, Martinoli C. Ultrasound of the musculoskeletal system. Berlin; New York: Springer; 2007.
29. Narouze SN. Atlas of ultrasound-guided procedures in interventional pain management. New York: Springer; 2011.
30. Mjolstad OC, Snare SR, Folkvord L, et al. Assessment of left ventricular function by GPs using pocket-sized ultrasound. Fam Pract. 2012;29:534-540.
31. Bornemann P, Bornemann G. Military family physicians’ perceptions of a pocket point-of-care ultrasound device in clinical practice. Mil Med. 2014;179:1474-477.
32. Chan VSP, Piterman L, McCall L. Use of clinical ultrasonography in an Australian suburban family practice: its indications and findings. Hong Kong Practitioner. 1999;21:405-415.
33. Siepel T, Clifford DS, James PA, et al. The ultrasound-assisted physical examination in the periodic health evaluation of the elderly. J Fam Pract. 2000;49:628-632.
34. Rosenthal TC, Siepel T, Zubler J, et al. The use of ultrasonography to scan the abdomen of patients presenting for routine physical examinations. J Fam Pract. 1994;38:380-385.
35. Choosing Wisely Canada. Available at: http://www.choosingwiselycanada.org. Accessed 2016.
36. Hale I. Add to cart? Can Fam Physician. 2015;61:937-939.
37. Wordsworth S, Scott A. Ultrasound scanning by general practitioners: is it worthwhile? J Public Health Med. 2002;24:88-94.
38. Hall JW, Holman H, Bornemann P, et al. Point of Care Ultrasound in Family Medicine Residency Programs: A CERA Study. Fam Med. 2015;47:706-711.
39. WINFOCUS-World Interactive Network Focused on Critical UltraSound. Available at: http://www.winfocus.it/#winfocus. Accessed 2016.
40. McGill University. McGill Ultrasound Evaluation Program (MUSE). Bedside ultrasound course for primary care clinicians (MUSE 1.0). Available at: www.mcgill.ca/medsimcentre/muse. Accessed 2016.
41. The University of British Columbia. Faculty of Medicine UBC CPD (Continuing Professional Development). CPD/CME courses. Available at: http://ubccpd.ca/courses?combine=ultrasound&field_target_audience_tid=3&field_learning_type_tid=All&field_location_tid=All&field_cost_tid=All&
field_credit_type_tid=All&field_number_of_credits_tid=All&field_event_date_value_1%5Bvalue%5D%5Bdate%5D=. Accessed 2016.
42. Emergency Department Echo (EDE). Available at: www.edecourse.com. Accessed 2016.
43. McGill University. MUSE 2.0 Advanced Bedside Ultrasound Course. Available at: http://www.mcgill.ca/medsimcentre/channels/event/muse-20-advanced-bedside-ultrasound-course-256963. Accessed 2016.
44. Gulfcoast Ultrasound Institute. Available at: https://www.gcus.com. Accessed 2016.
45. Allen GM, Wilson DJ. Ultrasound in sports medicine—a critical evaluation. Eur J Radiol. 2007;62:79-85.
Point-of-care ultrasound is increasingly being integrated into clinical practice, as an adjunct to the physical examination and patient history,1 and into medical school curricula across North America.2,3 Research confirms that this technology improves patient survival in emergency medicine settings;4 however, the benefits of point-of-care ultrasound administered by family physicians (FPs) in the office setting are less well documented.
Here we provide a comprehensive review of the indications for ultrasound in the office setting, which range from diagnosing musculoskeletal injuries and guiding injections to screening for abdominal aortic aneurysm (AAA). We also address the accuracy and cost-effectiveness of ultrasound use and the training needed to make family medicine ultrasound (FAMUS) successful.
Ultrasound: A useful screening tool for abdominal aortic aneurysm
The US Preventive Services Task Force (USPSTF) recommends one-time screening for abdominal aortic aneurysm (AAA) in men ages 65 to 75 years who have ever smoked (See: http://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/abdominal-aortic-aneurysm-screening.) Ultrasound is a reliable tool for identifying AAA5 (FIGURE 1); its sensitivity and specificity range from 94% to 98.9% and 98% to 100%, respectively.6-9 It is also superior to physical examination for AAAs,10 which has a sensitivity of 29% for small AAAs (30-39 mm) and 76% for larger AAAs (>50 mm).11
Most importantly, research has demonstrated that long-term mortality benefits are associated with ultrasound screening of asymptomatic patients for AAA. For example, one study found that screening asymptomatic men ages 65 to 74 (a population-based sample, with no particular risk factors) for AAA resulted in a reduction in all-cause mortality and that the benefit of AAA-related mortality continued to accumulate throughout follow-up.12
In fact, nationwide programs to screen for AAA using ultrasound have been established in England, Northern Ireland, Scotland, Sweden, the United States, and Wales to help prevent deaths associated with AAA rupture.13 Despite the documented benefits of ultrasound screening for AAA, a large retrospective cohort study conducted in an American integrated health care system found that only about 9% of patients eligible for screening according to USPSTF guidelines were screened for AAA with ultrasound in primary care practices in 2012.14
While most AAA screening occurs in the hospital, screening for the condition can be just as easily and effectively performed in an FP’s office or outpatient clinic. A Canadian prospective observational study demonstrated that aortic diameter measurements were comparable whether they were obtained by ultrasound performed by an office-based physician (who had completed an emergency ultrasonography course and performed at least 50 ultrasonographer-supervised ultrasound scans of the aorta), or by a hospital-based technologist whose scans were then reviewed by a radiologist.15 (See the TABLE for an overview of the research involving family medicine ultrasound.)
The office-based scans had a high degree of correlation (0.81) with the hospital-based ones, a sensitivity and specificity of 100%, and lasted a mean of 3.5 minutes. The researchers concluded that ultrasound screening for AAA can be safely performed in the office setting by FPs who are trained to use point-of-care ultrasound technology, and that the screening can be completed within the time constraints of a typical family practice office visit.15
In a separate study, cardiologists compared hand-held ultrasound screening for AAA to standard 2-dimensional echocardiography. This study found that screening for AAA in an outpatient clinic with a hand-held ultrasound device is feasible and accurate with a sensitivity of 88% and a specificity of 98%.16
Ultrasound in the obstetrician’s office—and the FP’s office, too
The use of ultrasound in obstetrics (FIGURE 2) is particularly well documented, with evidence supporting the use of FAMUS for various obstetrical indications dating back 30 years.17 The American Academy of Family Physicians has a position paper endorsing diagnostic ultrasound for women’s health care and has offered obstetric ultrasound courses organized by, and for, FPs since 1989.18
In a prospective observational study conducted in the United Kingdom, an FP and a nurse midwife used ultrasound to assess 240 pregnant women presenting with vaginal bleeding in early pregnancy.19 Fetal heartbeat detection by an office ultrasound scan predicted fetal progression to 20 weeks with a sensitivity of 97% and a specificity of 98%. The clinicians also detected anomalies such as molar pregnancy, blighted ovum, and ectopic pregnancy.
FAMUS and its ability to accurately estimate delivery date was examined in another prospective study involving 186 patients at a community health center.20 Accuracy for the estimated date of delivery was 96% using stratified confidence intervals for first-, second-, and third-trimester examinations. The office-based ultrasound scans also detected one case of placenta previa, one fetal death, and 2 unsuspected twin pregnancies. Another study showed no difference in estimations of gestational age provided by ultrasound performed by supervised FP residents with 3 years’ ultrasound training (including 3 lectures per year and an annual 4-hour workshop), and radiologists.21
Further evidence that FAMUS can confirm fetal death and multiple gestations was provided by a retrospective review of almost 498 obstetric ultrasound examinations.22 FPs accurately predicted the presence or absence of fetal death, multiple gestations, and the estimated date of confinement. Another study demonstrated that 86% of 248 FP obstetrical scans were judged acceptable by a radiologist, 10% were repeated due to technical errors and subsequently found to be acceptable, and 3% were unacceptable and referred for formal ultrasound.23 These scans were performed by FPs who completed 5 days of theory and hands-on training and 3 half-days of apprenticeship in an ultrasound laboratory.
In a study conducted in Tanzania, bedside ultrasound scans performed by nurse midwives had 100% agreement with scans performed by a sonographer when evaluating for twins, the presence of fetal heartbeat, or fetal positioning. Overall, bedside ultrasound aided in the diagnosis (39%) and management plan (22%) of 542 patients.24 It is important to note, as highlighted in a multisite study, that consultation with specialists when appropriate is paramount to the successful use of ultrasound by the FP for prenatal care.25
Guiding joint injections, assessing LV function
Sports/exercise medicine. FPs with expertise in sports and exercise medicine commonly use office ultrasound to diagnose musculoskeletal (MSK) injuries, including rotator cuff tears, muscle ruptures, tendinitis, and bursitis.26 It is superior to magnetic resonance imaging (MRI) in terms of cost-to-benefit ratio, precision, and sensitivity (due, in part, to the fact that clinicians can obtain patient feedback during the examination).26 In addition, a review of office-based procedures for MSK indications demonstrated the usefulness of ultrasound for the guidance of joint aspirations and joint and tendon injections.27 Ultrasound guidance is commonly used to ensure procedural accuracy during aspirations and injections of the shoulder (glenohumeral joint; subacromial bursa), elbow, wrist (carpal tunnel tendons), hip, knee, and ankle.27-29
Cardiology (FIGURE 3). General practitioners in Norway found that 8 hours of training on a hand-held ultrasound device was sufficient to assess left ventricular function with a sensitivity and specificity of 78% and 83%, respectively.30 Their measurements of septal mitral annular excursion (a surrogate measurement of left ventricular function) were similar to those of a cardiologist using the same device and added no more than 5 minutes to the examination.
Other uses. In a separate study, military FPs with 16 hours of training found that FAMUS was easy to learn and effective in the outpatient and inpatient setting for the detection of AAA, trauma, musculoskeletal injuries, and certain obstetric, echocardiographic, and biliary indications.31 They reported that the average time spent per ultrasound examination was one to 5 minutes for the majority of the indications.
The authors of a retrospective study involving a suburban family practice reported that FAMUS was successfully used to identify the causes of epigastric and right upper quadrant pain, and to check post-void residual urinary bladder volume.32
The ultrasound-assisted physical examination can detect pathologies not apparent on history and physical examination alone (FIGURES 4 and 5). In one study, an FP used ultrasound in the office to identify pathologies in 31% of patients that were not detected on physical examination alone. The pathologies included AAAs, a thyroid cyst, mitral stenosis, gallstones, renal cysts, urinary retention, hydronephrosis, ectopic kidney, and an endometrial tumor.33
| 
|
In another study, an FP performed ultrasound examinations on 189 patients during their annual exams.34 The technology identified pathologies that were not suspected after clinical assessment in 22% of these patients. With the emphasis in the current clinical landscape on choosing diagnostic tests wisely, it will be important to determine if findings like these positively impact patient care.35,36
Portable ultrasound machines are affordable
The relative affordability of portable ultrasound contributes to the cost-effectiveness of FAMUS. For FPs seeking to initiate an office-based ultrasound program, expenses to consider include the price of the machine itself, which ranges from $7500 to $50,000, depending on the technology included. Other expenses include the cost of disposables (eg, ultrasound gel and disinfectant wipes or spray), which may total about $400 per year.
In-office exams facilitate savings elsewhere. Other factors that contribute to the cost-effectiveness of FAMUS include reduced radiologist expenses and hospital visits. The cost savings of in-office ultrasound was highlighted almost 30 years ago when the cost of a FAMUS obstetrical scan was reported to be half that of a radiologist scan.23 This same study reported that increased costs for additional investigations caused by incidental findings using FAMUS could be offset by the decreased costs associated with an earlier diagnosis of serious conditions.23
A 2002 study demonstrated that office-based FAMUS scans (N=131) reduced the number of hospital scans, emergency admissions, and outpatient and inpatient hospital visits.37 Although the unit cost of a FAMUS scan was higher than an inpatient one, the total cost of the FAMUS scan was lower due to decreased hospital visits. In addition, research has shown that patients are more satisfied with office-based ultrasound examinations and prefer ultrasound performed by their FP to hospital-based ultrasound scans.31,37
Training: Cost and availability
Training in office-based ultrasound is available at the undergraduate, postgraduate, and continuing medical education levels. Undergraduate bedside ultrasound education is evident in medical schools around the globe including in Australia, Austria, Canada, China, Germany, France, the United States, and the United Kingdom.3 In an American survey of family medicine residency programs published in 2015, only 2.2% reported an established ultrasound curriculum; however, 29% had started a program within the past year.38 In Canada, one- and 2-day bedside ultrasound courses are offered to family medicine residents at a number of universities. And continuing medical education (CME) courses in bedside ultrasound are available to physicians on a regular basis internationally.39 In North America, CME courses exist specifically for urban and rural family medicine clinicians,40-43 and offer training for a wide range of applications.
Courses are often available for $1000 to $2000. Many of these courses run over a one- to 3-day period. Some provide a general overview of ultrasound for the primary care physician while others specialize in topics such as musculoskeletal uses, obstetric uses, or emergency department echocardiography.40-44
Challenges remain
More research is necessary to demonstrate that office-based ultrasound produces patient outcomes that are comparable to those resulting from hospital-based ultrasound. Also, bedside ultrasound is only as good as the operator who performs the examination,45 which highlights the importance of developing bedside ultrasound training programs tailored for FPs. National policies are essential for standardizing indications, training, and credentialing so that this effective tool can be used in a safe and effective manner.
CORRESPONDENCE
Peter Steinmetz, MD, CCFP, St. Mary’s Hospital, 3830 Ave Lacombe, Montreal, Quebec, Canada H3T1M5; [email protected].
ACKNOWLEDGEMENTS
We thank Assistant Professor Marion Dove, MD, CCFP, Department of Family Medicine, McGill University, for her suggestions and critical review of an earlier version of the manuscript. The term FAMUS is pending registration and is advertised with the Canadian Intellectual Property Office (Steinmetz, Volume 63, Issue 3217).
Point-of-care ultrasound is increasingly being integrated into clinical practice, as an adjunct to the physical examination and patient history,1 and into medical school curricula across North America.2,3 Research confirms that this technology improves patient survival in emergency medicine settings;4 however, the benefits of point-of-care ultrasound administered by family physicians (FPs) in the office setting are less well documented.
Here we provide a comprehensive review of the indications for ultrasound in the office setting, which range from diagnosing musculoskeletal injuries and guiding injections to screening for abdominal aortic aneurysm (AAA). We also address the accuracy and cost-effectiveness of ultrasound use and the training needed to make family medicine ultrasound (FAMUS) successful.
Ultrasound: A useful screening tool for abdominal aortic aneurysm
The US Preventive Services Task Force (USPSTF) recommends one-time screening for abdominal aortic aneurysm (AAA) in men ages 65 to 75 years who have ever smoked (See: http://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/abdominal-aortic-aneurysm-screening.) Ultrasound is a reliable tool for identifying AAA5 (FIGURE 1); its sensitivity and specificity range from 94% to 98.9% and 98% to 100%, respectively.6-9 It is also superior to physical examination for AAAs,10 which has a sensitivity of 29% for small AAAs (30-39 mm) and 76% for larger AAAs (>50 mm).11
Most importantly, research has demonstrated that long-term mortality benefits are associated with ultrasound screening of asymptomatic patients for AAA. For example, one study found that screening asymptomatic men ages 65 to 74 (a population-based sample, with no particular risk factors) for AAA resulted in a reduction in all-cause mortality and that the benefit of AAA-related mortality continued to accumulate throughout follow-up.12
In fact, nationwide programs to screen for AAA using ultrasound have been established in England, Northern Ireland, Scotland, Sweden, the United States, and Wales to help prevent deaths associated with AAA rupture.13 Despite the documented benefits of ultrasound screening for AAA, a large retrospective cohort study conducted in an American integrated health care system found that only about 9% of patients eligible for screening according to USPSTF guidelines were screened for AAA with ultrasound in primary care practices in 2012.14
While most AAA screening occurs in the hospital, screening for the condition can be just as easily and effectively performed in an FP’s office or outpatient clinic. A Canadian prospective observational study demonstrated that aortic diameter measurements were comparable whether they were obtained by ultrasound performed by an office-based physician (who had completed an emergency ultrasonography course and performed at least 50 ultrasonographer-supervised ultrasound scans of the aorta), or by a hospital-based technologist whose scans were then reviewed by a radiologist.15 (See the TABLE for an overview of the research involving family medicine ultrasound.)
The office-based scans had a high degree of correlation (0.81) with the hospital-based ones, a sensitivity and specificity of 100%, and lasted a mean of 3.5 minutes. The researchers concluded that ultrasound screening for AAA can be safely performed in the office setting by FPs who are trained to use point-of-care ultrasound technology, and that the screening can be completed within the time constraints of a typical family practice office visit.15
In a separate study, cardiologists compared hand-held ultrasound screening for AAA to standard 2-dimensional echocardiography. This study found that screening for AAA in an outpatient clinic with a hand-held ultrasound device is feasible and accurate with a sensitivity of 88% and a specificity of 98%.16
Ultrasound in the obstetrician’s office—and the FP’s office, too
The use of ultrasound in obstetrics (FIGURE 2) is particularly well documented, with evidence supporting the use of FAMUS for various obstetrical indications dating back 30 years.17 The American Academy of Family Physicians has a position paper endorsing diagnostic ultrasound for women’s health care and has offered obstetric ultrasound courses organized by, and for, FPs since 1989.18
In a prospective observational study conducted in the United Kingdom, an FP and a nurse midwife used ultrasound to assess 240 pregnant women presenting with vaginal bleeding in early pregnancy.19 Fetal heartbeat detection by an office ultrasound scan predicted fetal progression to 20 weeks with a sensitivity of 97% and a specificity of 98%. The clinicians also detected anomalies such as molar pregnancy, blighted ovum, and ectopic pregnancy.
FAMUS and its ability to accurately estimate delivery date was examined in another prospective study involving 186 patients at a community health center.20 Accuracy for the estimated date of delivery was 96% using stratified confidence intervals for first-, second-, and third-trimester examinations. The office-based ultrasound scans also detected one case of placenta previa, one fetal death, and 2 unsuspected twin pregnancies. Another study showed no difference in estimations of gestational age provided by ultrasound performed by supervised FP residents with 3 years’ ultrasound training (including 3 lectures per year and an annual 4-hour workshop), and radiologists.21
Further evidence that FAMUS can confirm fetal death and multiple gestations was provided by a retrospective review of almost 498 obstetric ultrasound examinations.22 FPs accurately predicted the presence or absence of fetal death, multiple gestations, and the estimated date of confinement. Another study demonstrated that 86% of 248 FP obstetrical scans were judged acceptable by a radiologist, 10% were repeated due to technical errors and subsequently found to be acceptable, and 3% were unacceptable and referred for formal ultrasound.23 These scans were performed by FPs who completed 5 days of theory and hands-on training and 3 half-days of apprenticeship in an ultrasound laboratory.
In a study conducted in Tanzania, bedside ultrasound scans performed by nurse midwives had 100% agreement with scans performed by a sonographer when evaluating for twins, the presence of fetal heartbeat, or fetal positioning. Overall, bedside ultrasound aided in the diagnosis (39%) and management plan (22%) of 542 patients.24 It is important to note, as highlighted in a multisite study, that consultation with specialists when appropriate is paramount to the successful use of ultrasound by the FP for prenatal care.25
Guiding joint injections, assessing LV function
Sports/exercise medicine. FPs with expertise in sports and exercise medicine commonly use office ultrasound to diagnose musculoskeletal (MSK) injuries, including rotator cuff tears, muscle ruptures, tendinitis, and bursitis.26 It is superior to magnetic resonance imaging (MRI) in terms of cost-to-benefit ratio, precision, and sensitivity (due, in part, to the fact that clinicians can obtain patient feedback during the examination).26 In addition, a review of office-based procedures for MSK indications demonstrated the usefulness of ultrasound for the guidance of joint aspirations and joint and tendon injections.27 Ultrasound guidance is commonly used to ensure procedural accuracy during aspirations and injections of the shoulder (glenohumeral joint; subacromial bursa), elbow, wrist (carpal tunnel tendons), hip, knee, and ankle.27-29
Cardiology (FIGURE 3). General practitioners in Norway found that 8 hours of training on a hand-held ultrasound device was sufficient to assess left ventricular function with a sensitivity and specificity of 78% and 83%, respectively.30 Their measurements of septal mitral annular excursion (a surrogate measurement of left ventricular function) were similar to those of a cardiologist using the same device and added no more than 5 minutes to the examination.
Other uses. In a separate study, military FPs with 16 hours of training found that FAMUS was easy to learn and effective in the outpatient and inpatient setting for the detection of AAA, trauma, musculoskeletal injuries, and certain obstetric, echocardiographic, and biliary indications.31 They reported that the average time spent per ultrasound examination was one to 5 minutes for the majority of the indications.
The authors of a retrospective study involving a suburban family practice reported that FAMUS was successfully used to identify the causes of epigastric and right upper quadrant pain, and to check post-void residual urinary bladder volume.32
The ultrasound-assisted physical examination can detect pathologies not apparent on history and physical examination alone (FIGURES 4 and 5). In one study, an FP used ultrasound in the office to identify pathologies in 31% of patients that were not detected on physical examination alone. The pathologies included AAAs, a thyroid cyst, mitral stenosis, gallstones, renal cysts, urinary retention, hydronephrosis, ectopic kidney, and an endometrial tumor.33
| 
|
In another study, an FP performed ultrasound examinations on 189 patients during their annual exams.34 The technology identified pathologies that were not suspected after clinical assessment in 22% of these patients. With the emphasis in the current clinical landscape on choosing diagnostic tests wisely, it will be important to determine if findings like these positively impact patient care.35,36
Portable ultrasound machines are affordable
The relative affordability of portable ultrasound contributes to the cost-effectiveness of FAMUS. For FPs seeking to initiate an office-based ultrasound program, expenses to consider include the price of the machine itself, which ranges from $7500 to $50,000, depending on the technology included. Other expenses include the cost of disposables (eg, ultrasound gel and disinfectant wipes or spray), which may total about $400 per year.
In-office exams facilitate savings elsewhere. Other factors that contribute to the cost-effectiveness of FAMUS include reduced radiologist expenses and hospital visits. The cost savings of in-office ultrasound was highlighted almost 30 years ago when the cost of a FAMUS obstetrical scan was reported to be half that of a radiologist scan.23 This same study reported that increased costs for additional investigations caused by incidental findings using FAMUS could be offset by the decreased costs associated with an earlier diagnosis of serious conditions.23
A 2002 study demonstrated that office-based FAMUS scans (N=131) reduced the number of hospital scans, emergency admissions, and outpatient and inpatient hospital visits.37 Although the unit cost of a FAMUS scan was higher than an inpatient one, the total cost of the FAMUS scan was lower due to decreased hospital visits. In addition, research has shown that patients are more satisfied with office-based ultrasound examinations and prefer ultrasound performed by their FP to hospital-based ultrasound scans.31,37
Training: Cost and availability
Training in office-based ultrasound is available at the undergraduate, postgraduate, and continuing medical education levels. Undergraduate bedside ultrasound education is evident in medical schools around the globe including in Australia, Austria, Canada, China, Germany, France, the United States, and the United Kingdom.3 In an American survey of family medicine residency programs published in 2015, only 2.2% reported an established ultrasound curriculum; however, 29% had started a program within the past year.38 In Canada, one- and 2-day bedside ultrasound courses are offered to family medicine residents at a number of universities. And continuing medical education (CME) courses in bedside ultrasound are available to physicians on a regular basis internationally.39 In North America, CME courses exist specifically for urban and rural family medicine clinicians,40-43 and offer training for a wide range of applications.
Courses are often available for $1000 to $2000. Many of these courses run over a one- to 3-day period. Some provide a general overview of ultrasound for the primary care physician while others specialize in topics such as musculoskeletal uses, obstetric uses, or emergency department echocardiography.40-44
Challenges remain
More research is necessary to demonstrate that office-based ultrasound produces patient outcomes that are comparable to those resulting from hospital-based ultrasound. Also, bedside ultrasound is only as good as the operator who performs the examination,45 which highlights the importance of developing bedside ultrasound training programs tailored for FPs. National policies are essential for standardizing indications, training, and credentialing so that this effective tool can be used in a safe and effective manner.
CORRESPONDENCE
Peter Steinmetz, MD, CCFP, St. Mary’s Hospital, 3830 Ave Lacombe, Montreal, Quebec, Canada H3T1M5; [email protected].
ACKNOWLEDGEMENTS
We thank Assistant Professor Marion Dove, MD, CCFP, Department of Family Medicine, McGill University, for her suggestions and critical review of an earlier version of the manuscript. The term FAMUS is pending registration and is advertised with the Canadian Intellectual Property Office (Steinmetz, Volume 63, Issue 3217).
1. Solomon SD, Saldana F. Point-of-care ultrasound in medical education - stop listening and look. N Engl J Med. 2014;370:1083-1085.
2. Bahner DP, Goldman E, Way D, et al. The state of ultrasound education in U.S. medical schools: results of a national survey. Acad Med. 2014;89:1681-1686.
3. Steinmetz P, Dobrescu O, Oleskevich S, et al. Bedside ultrasound education in Canadian medical schools: a national survey. Can Med Educ J. 2016;7:e78-e86.
4. Deshpande R, Akhtar S, Haddadin AS. Utility of ultrasound in the ICU. Curr Opin Anaesthesiol. 2014;27:123-132.
5. Wilmink ABM, Hubbard CSFF, Quick CRG. Quality of the measurement of the infrarenal aortic diameter by ultrasound. J Med Screen. 1997;4:49-53.
6. Costantino TG, Bruno EC, Handly N, et al. Accuracy of emergency medicine ultrasound in the evaluation of abdominal aortic aneurysm. J Emerg Med. 2005;29:455-460.
7. Lindholt JS, Vammen S, Juul S, et al. The validity of ultrasonographic scanning as screening method for abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 1999;17:472-475.
8. Nusbaum JW, Freimanis AK, Thomford NR. Echography in the diagnosis of abdominal aortic aneurysm. Arch Surg. 1971;102:385-388.
9. Wilmink ABM, Forshaw M, Quick CRG, et al. Accuracy of serial screening for abdominal aortic aneurysms by ultrasound. J Med Screen. 2002;9:125-127.
10. Lynch RM. Accuracy of abdominal examination in the diagnosis of non-ruptured abdominal aortic aneurysm. Accid Emerg Nurs. 2004;12:99-107.
11. Lederle FA, Simel DL. The rational clinical examination. Does this patient have abdominal aortic aneurysm? JAMA. 1999;281:77-82.
12. Thompson SG, Ashton HA, Gao L, et al; Multicentre Aneurysm Screening Study (MASS) Group. Final follow-up of the Multicentre Aneurysm Screening Study (MASS) randomized trial of abdominal aortic aneurysm screening. Br J Surg. 2012;99:1649-1656.
13. Stather PW, Dattani N, Bown MJ, et al. International variations in AAA screening. Eur J Vasc Endovasc Surg. 2013;45:231-234.
14. Ruff AL, Teng K, Hu B, et al. Screening for abdominal aortic aneurysms in outpatient primary care clinics. Am J Med. 2015;128:283-288.
15. Blois B. Office-based ultrasound screening for abdominal aortic aneurysm. Can Fam Physician. 2012;58:e172-178.
16. Vourvouri EC, Poldermans D, Schinkel AF, et al. Abdominal aortic aneurysm screening using a hand-held ultrasound device. “A pilot study”. Eur J Vasc Endovasc Surg. 2001;22:352-354.
17. Hahn RG, Davies TC, Rodney WM. Diagnostic ultrasound in general practice. Fam Pract. 1988;5:129-135.
18. American Academy of Family Physicians. Position Paper: Diagnostic ultrasonography in women’s health care. 2013. Available at http://www.aafp.org/about/policies/all/ultrasonography-diagnostic.html. Accessed 2013.
19. Everett CB, Preece E. Women with bleeding in the first 20 weeks of pregnancy: value of general practice ultrasound in detecting fetal heart movement. Br J Gen Pract. 1996;46:7-9.
20. Rodney WM, Prislin MD, Orientale E, et al. Family practice obstetric ultrasound in an urban community health center. Birth outcomes and examination accuracy of the initial 227 cases. J Fam Pract. 1990;30:163-168.
21. Keith R, Frisch L. Fetal biometry: a comparison of family physicians and radiologists. Fam Med. 2001;33:111-114.
22. Ornstein SM, Smith MA, Peggs J, et al. Obstetric ultrasound by family physicians. Adequacy as assessed by pregnancy outcome. J Fam Pract. 1990;30:403-408.
23. Hahn RG, Ho S, Roi LD, et al. Cost-effectiveness of office obstetrical ultrasound in family practice: preliminary considerations. J Am Board Fam Pract. 1988;1:33-38.
24. Stein W, Katunda I, Butoto C. A two-level ultrasonographic service in a maternity care unit of a rural district hospital in Tanzania. Trop Doct. 2008;38:125-126.
25. Morgan WC, Rodney WM, Hahn R, et al. Ultrasound for the primary care physician. Applications in family-centered obstetrics. Postgrad Med. 1988;83:103-107.
26. Coris EE, Pescasio M, Zwygart K, et al. Office-based ultrasound in sports medicine practice. Clin J Sport Med. 2011;21:57-61.
27. Royall NA, Farrin E, Bahner DP, et al. Ultrasound-assisted musculoskeletal procedures: A practical overview of current literature. World J Orthop. 2011;2:57-66.
28. Bianchi S, Martinoli C. Ultrasound of the musculoskeletal system. Berlin; New York: Springer; 2007.
29. Narouze SN. Atlas of ultrasound-guided procedures in interventional pain management. New York: Springer; 2011.
30. Mjolstad OC, Snare SR, Folkvord L, et al. Assessment of left ventricular function by GPs using pocket-sized ultrasound. Fam Pract. 2012;29:534-540.
31. Bornemann P, Bornemann G. Military family physicians’ perceptions of a pocket point-of-care ultrasound device in clinical practice. Mil Med. 2014;179:1474-477.
32. Chan VSP, Piterman L, McCall L. Use of clinical ultrasonography in an Australian suburban family practice: its indications and findings. Hong Kong Practitioner. 1999;21:405-415.
33. Siepel T, Clifford DS, James PA, et al. The ultrasound-assisted physical examination in the periodic health evaluation of the elderly. J Fam Pract. 2000;49:628-632.
34. Rosenthal TC, Siepel T, Zubler J, et al. The use of ultrasonography to scan the abdomen of patients presenting for routine physical examinations. J Fam Pract. 1994;38:380-385.
35. Choosing Wisely Canada. Available at: http://www.choosingwiselycanada.org. Accessed 2016.
36. Hale I. Add to cart? Can Fam Physician. 2015;61:937-939.
37. Wordsworth S, Scott A. Ultrasound scanning by general practitioners: is it worthwhile? J Public Health Med. 2002;24:88-94.
38. Hall JW, Holman H, Bornemann P, et al. Point of Care Ultrasound in Family Medicine Residency Programs: A CERA Study. Fam Med. 2015;47:706-711.
39. WINFOCUS-World Interactive Network Focused on Critical UltraSound. Available at: http://www.winfocus.it/#winfocus. Accessed 2016.
40. McGill University. McGill Ultrasound Evaluation Program (MUSE). Bedside ultrasound course for primary care clinicians (MUSE 1.0). Available at: www.mcgill.ca/medsimcentre/muse. Accessed 2016.
41. The University of British Columbia. Faculty of Medicine UBC CPD (Continuing Professional Development). CPD/CME courses. Available at: http://ubccpd.ca/courses?combine=ultrasound&field_target_audience_tid=3&field_learning_type_tid=All&field_location_tid=All&field_cost_tid=All&
field_credit_type_tid=All&field_number_of_credits_tid=All&field_event_date_value_1%5Bvalue%5D%5Bdate%5D=. Accessed 2016.
42. Emergency Department Echo (EDE). Available at: www.edecourse.com. Accessed 2016.
43. McGill University. MUSE 2.0 Advanced Bedside Ultrasound Course. Available at: http://www.mcgill.ca/medsimcentre/channels/event/muse-20-advanced-bedside-ultrasound-course-256963. Accessed 2016.
44. Gulfcoast Ultrasound Institute. Available at: https://www.gcus.com. Accessed 2016.
45. Allen GM, Wilson DJ. Ultrasound in sports medicine—a critical evaluation. Eur J Radiol. 2007;62:79-85.
1. Solomon SD, Saldana F. Point-of-care ultrasound in medical education - stop listening and look. N Engl J Med. 2014;370:1083-1085.
2. Bahner DP, Goldman E, Way D, et al. The state of ultrasound education in U.S. medical schools: results of a national survey. Acad Med. 2014;89:1681-1686.
3. Steinmetz P, Dobrescu O, Oleskevich S, et al. Bedside ultrasound education in Canadian medical schools: a national survey. Can Med Educ J. 2016;7:e78-e86.
4. Deshpande R, Akhtar S, Haddadin AS. Utility of ultrasound in the ICU. Curr Opin Anaesthesiol. 2014;27:123-132.
5. Wilmink ABM, Hubbard CSFF, Quick CRG. Quality of the measurement of the infrarenal aortic diameter by ultrasound. J Med Screen. 1997;4:49-53.
6. Costantino TG, Bruno EC, Handly N, et al. Accuracy of emergency medicine ultrasound in the evaluation of abdominal aortic aneurysm. J Emerg Med. 2005;29:455-460.
7. Lindholt JS, Vammen S, Juul S, et al. The validity of ultrasonographic scanning as screening method for abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 1999;17:472-475.
8. Nusbaum JW, Freimanis AK, Thomford NR. Echography in the diagnosis of abdominal aortic aneurysm. Arch Surg. 1971;102:385-388.
9. Wilmink ABM, Forshaw M, Quick CRG, et al. Accuracy of serial screening for abdominal aortic aneurysms by ultrasound. J Med Screen. 2002;9:125-127.
10. Lynch RM. Accuracy of abdominal examination in the diagnosis of non-ruptured abdominal aortic aneurysm. Accid Emerg Nurs. 2004;12:99-107.
11. Lederle FA, Simel DL. The rational clinical examination. Does this patient have abdominal aortic aneurysm? JAMA. 1999;281:77-82.
12. Thompson SG, Ashton HA, Gao L, et al; Multicentre Aneurysm Screening Study (MASS) Group. Final follow-up of the Multicentre Aneurysm Screening Study (MASS) randomized trial of abdominal aortic aneurysm screening. Br J Surg. 2012;99:1649-1656.
13. Stather PW, Dattani N, Bown MJ, et al. International variations in AAA screening. Eur J Vasc Endovasc Surg. 2013;45:231-234.
14. Ruff AL, Teng K, Hu B, et al. Screening for abdominal aortic aneurysms in outpatient primary care clinics. Am J Med. 2015;128:283-288.
15. Blois B. Office-based ultrasound screening for abdominal aortic aneurysm. Can Fam Physician. 2012;58:e172-178.
16. Vourvouri EC, Poldermans D, Schinkel AF, et al. Abdominal aortic aneurysm screening using a hand-held ultrasound device. “A pilot study”. Eur J Vasc Endovasc Surg. 2001;22:352-354.
17. Hahn RG, Davies TC, Rodney WM. Diagnostic ultrasound in general practice. Fam Pract. 1988;5:129-135.
18. American Academy of Family Physicians. Position Paper: Diagnostic ultrasonography in women’s health care. 2013. Available at http://www.aafp.org/about/policies/all/ultrasonography-diagnostic.html. Accessed 2013.
19. Everett CB, Preece E. Women with bleeding in the first 20 weeks of pregnancy: value of general practice ultrasound in detecting fetal heart movement. Br J Gen Pract. 1996;46:7-9.
20. Rodney WM, Prislin MD, Orientale E, et al. Family practice obstetric ultrasound in an urban community health center. Birth outcomes and examination accuracy of the initial 227 cases. J Fam Pract. 1990;30:163-168.
21. Keith R, Frisch L. Fetal biometry: a comparison of family physicians and radiologists. Fam Med. 2001;33:111-114.
22. Ornstein SM, Smith MA, Peggs J, et al. Obstetric ultrasound by family physicians. Adequacy as assessed by pregnancy outcome. J Fam Pract. 1990;30:403-408.
23. Hahn RG, Ho S, Roi LD, et al. Cost-effectiveness of office obstetrical ultrasound in family practice: preliminary considerations. J Am Board Fam Pract. 1988;1:33-38.
24. Stein W, Katunda I, Butoto C. A two-level ultrasonographic service in a maternity care unit of a rural district hospital in Tanzania. Trop Doct. 2008;38:125-126.
25. Morgan WC, Rodney WM, Hahn R, et al. Ultrasound for the primary care physician. Applications in family-centered obstetrics. Postgrad Med. 1988;83:103-107.
26. Coris EE, Pescasio M, Zwygart K, et al. Office-based ultrasound in sports medicine practice. Clin J Sport Med. 2011;21:57-61.
27. Royall NA, Farrin E, Bahner DP, et al. Ultrasound-assisted musculoskeletal procedures: A practical overview of current literature. World J Orthop. 2011;2:57-66.
28. Bianchi S, Martinoli C. Ultrasound of the musculoskeletal system. Berlin; New York: Springer; 2007.
29. Narouze SN. Atlas of ultrasound-guided procedures in interventional pain management. New York: Springer; 2011.
30. Mjolstad OC, Snare SR, Folkvord L, et al. Assessment of left ventricular function by GPs using pocket-sized ultrasound. Fam Pract. 2012;29:534-540.
31. Bornemann P, Bornemann G. Military family physicians’ perceptions of a pocket point-of-care ultrasound device in clinical practice. Mil Med. 2014;179:1474-477.
32. Chan VSP, Piterman L, McCall L. Use of clinical ultrasonography in an Australian suburban family practice: its indications and findings. Hong Kong Practitioner. 1999;21:405-415.
33. Siepel T, Clifford DS, James PA, et al. The ultrasound-assisted physical examination in the periodic health evaluation of the elderly. J Fam Pract. 2000;49:628-632.
34. Rosenthal TC, Siepel T, Zubler J, et al. The use of ultrasonography to scan the abdomen of patients presenting for routine physical examinations. J Fam Pract. 1994;38:380-385.
35. Choosing Wisely Canada. Available at: http://www.choosingwiselycanada.org. Accessed 2016.
36. Hale I. Add to cart? Can Fam Physician. 2015;61:937-939.
37. Wordsworth S, Scott A. Ultrasound scanning by general practitioners: is it worthwhile? J Public Health Med. 2002;24:88-94.
38. Hall JW, Holman H, Bornemann P, et al. Point of Care Ultrasound in Family Medicine Residency Programs: A CERA Study. Fam Med. 2015;47:706-711.
39. WINFOCUS-World Interactive Network Focused on Critical UltraSound. Available at: http://www.winfocus.it/#winfocus. Accessed 2016.
40. McGill University. McGill Ultrasound Evaluation Program (MUSE). Bedside ultrasound course for primary care clinicians (MUSE 1.0). Available at: www.mcgill.ca/medsimcentre/muse. Accessed 2016.
41. The University of British Columbia. Faculty of Medicine UBC CPD (Continuing Professional Development). CPD/CME courses. Available at: http://ubccpd.ca/courses?combine=ultrasound&field_target_audience_tid=3&field_learning_type_tid=All&field_location_tid=All&field_cost_tid=All&
field_credit_type_tid=All&field_number_of_credits_tid=All&field_event_date_value_1%5Bvalue%5D%5Bdate%5D=. Accessed 2016.
42. Emergency Department Echo (EDE). Available at: www.edecourse.com. Accessed 2016.
43. McGill University. MUSE 2.0 Advanced Bedside Ultrasound Course. Available at: http://www.mcgill.ca/medsimcentre/channels/event/muse-20-advanced-bedside-ultrasound-course-256963. Accessed 2016.
44. Gulfcoast Ultrasound Institute. Available at: https://www.gcus.com. Accessed 2016.
45. Allen GM, Wilson DJ. Ultrasound in sports medicine—a critical evaluation. Eur J Radiol. 2007;62:79-85.