User login
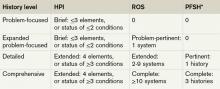
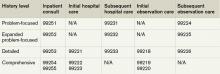
Each visit category and level of service has corresponding documentation requirements.1 Selecting an evaluation and management (E/M) level is based upon 1) the content of the three “key” components: history, exam, and decision-making, or 2) time, but only when counseling or coordination of care dominates more than 50% of the physician’s total visit time. Failure to document any essential element in a given visit level (e.g. family history required but missing for 99222 and 99223) could result in downcoding or service denial. Be aware of what an auditor expects when reviewing the key component of “history.”
Documentation Options
Auditors recognize two sets of documentation guidelines: “1995” and “1997” guidelines.2,3,4 Each set of guidelines has received valid criticism. The 1995 guidelines undoubtedly are vague and subjective in some areas, whereas the 1997 guidelines are known for arduous specificity.
However, to benefit all physicians and specialties, both sets of guidelines apply to visit-level selection. In other words, physicians can utilize either set when documenting their services, and auditors must review provider records against both styles. The final audited outcome reflects the highest visit level supported upon comparison.
Elements of History2,3,4
Chief complaint. The chief complaint (CC) is the reason for the visit, as stated in the patient’s own words. Every encounter, regardless of visit type, must include a CC. The physician must personally document and/or validate the CC with reference to a specific condition or symptom (e.g. patient complains of abdominal pain).
History of present illness (HPI). The HPI is a description of the patient’s present illness as it developed. It characteristically is referenced as location, quality, severity, timing, context, modifying factors, and associated signs/symptoms, as related to the chief complaint. The 1997 guidelines allow physicians to receive HPI credit for providing the status of the patient’s chronic or inactive conditions, such as “extrinsic asthma without acute exacerbation in past six months.” An auditor will not assign HPI credit to a chronic or inactive condition that does not have a corresponding status (e.g. “asthma”). This will be considered “past medical history.”
The HPI is classified as brief (a comment on <3 HPI elements, or the status of <2 conditions) or extended (a comment on >4 HPI elements, or the status of >3 conditions). Consider these examples of an extended HPI:
- “The patient has intermittent (duration), sharp (quality) pain in the right upper quadrant (location) without associated nausea, vomiting, or diarrhea (associated signs/symptoms).”
- “Diabetes controlled by oral medication; hyperlipidemia stable on simvastatin with increased dietary efforts; hypertension stable with pressures ranging from 130-140/80-90.” (Status of three chronic conditions.)
Physicians receive credit for confirming and personally documenting the HPI, or linking to documentation recorded by residents (residents, fellows, interns) or nonphysician providers (NPPs) when performing services according to the Teaching Physician Rules or Split-Shared Billing Rules, respectively. An auditor will not assign physician credit for HPI elements documented by ancillary staff (registered nurses, medical assistants) or students.
Review of systems (ROS). The ROS is a series of questions used to elicit information about additional signs, symptoms, or problems currently or previously experienced by the patient: constitutional; eyes, ears, nose, mouth, throat; cardiovascular; respiratory; gastrointestinal; genitourinary; musculoskeletal; integumentary (including skin and/or breast); neurological; psychiatric; endocrine; hematologic/ lymphatic; and allergic/immunologic. Auditors classify the ROS as brief (a comment on one system), extended (a comment on two to nine systems), or complete (a comment on >10 systems). Physicians can document a complete ROS by noting individual systems: “no fever/chills (constitutional) or blurred vision (eyes); no chest pain (cardiovascular) or shortness of breath (respiratory); intermittent nausea (gastrointestinal); and occasional runny nose (ears, nose, mouth, throat),” or by eliciting a complete system review but documenting only the positive and pertinent negative findings related to the chief complaint, along with an additional comment that “all other systems are negative.”
Although the latter method is formally included in Medicare’s documentation guidelines and accepted by some Medicare contractors (e.g. Highmark, WPS), be aware that it is not universally accepted.5,6
Documentation involving the ROS can be provided by anyone, including the patient. The physician should reference ROS information that is completed by individuals other than residents or NPPs during services provided under the Teaching Physician Rules or Split-Shared Billing Rules. Physician duplication of ROS information is unnecessary unless an update or revision is required.
Past, family, and social history (PFSH). The PFSH involves data obtained about the patient’s previous illness or medical conditions/therapies, family occurrences with illness, and relevant patient activities. The PFSH could be classified as pertinent (a comment on one history) or complete (a comment in each of the three histories). The physician merely needs a single comment associated with each history for the PFSH to be regarded as complete. Refrain from using “noncontributory” to describe any of the histories, as previous misuse of this term has resulted in its prohibition. An example of a complete PFSH documentation includes: “Patient currently on Prilosec 20 mg daily; family history of Barrett’s esophagus; no tobacco or alcohol use.”
Similar to the ROS, PFSH documentation can be provided by anyone, including the patient, and the physician should reference the documented PFSH in his own progress note. Redocumentation of the PFSH is not necessary unless a revision is required.
PFSH documentation is only required for initial care services (i.e. initial hospital care, initial observation care, consultations). It is not warranted in subsequent care services unless additional, pertinent information is obtained during the hospital stay that impacts care.
Considerations
When a physician cannot elicit historical information from the patient directly, and no other source is available, they should document “unable to obtain” the history. A comment regarding the circumstances surrounding this problem (e.g. patient confused, no caregiver present) should be provided, along with the available information from the limited resources (e.g. emergency medical technicians, previous hospitalizations at the same facility). Some contractors will not penalize the physician for the inability to ascertain complete historical information, as long as a proven attempt to obtain the information is evident.
Never document any item for the purpose of “getting paid.” Only document information that is clinically relevant, lends to the quality of care provided, or demonstrates the delivery of healthcare services. This prevents accusations of fraud and abuse, promotes billing compliance, and supports medical necessity for the services provided.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Centers for Medicare & Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. CMS website. Available at: www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed July 7, 2011.
- Centers for Medicare & Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. CMS website. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed July 7, 2011.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011.
- History of E/M (Q&As). WPS Health Insurance website. Available at: http://www.wpsmedicare.com/j5macpartb/resources/provider_types/2009_0526_emqahistory.shtml. Accessed July 11, 2011.
- Frequently Asked Questions: Evaluation and Management Services (Part B). Highmark Medicare Services website. Available at: www.highmarkmedicareservices.com/faq/partb/pet/lpet-evaluation_management_services.html. Accessed on July 11, 2011.
Each visit category and level of service has corresponding documentation requirements.1 Selecting an evaluation and management (E/M) level is based upon 1) the content of the three “key” components: history, exam, and decision-making, or 2) time, but only when counseling or coordination of care dominates more than 50% of the physician’s total visit time. Failure to document any essential element in a given visit level (e.g. family history required but missing for 99222 and 99223) could result in downcoding or service denial. Be aware of what an auditor expects when reviewing the key component of “history.”
Documentation Options
Auditors recognize two sets of documentation guidelines: “1995” and “1997” guidelines.2,3,4 Each set of guidelines has received valid criticism. The 1995 guidelines undoubtedly are vague and subjective in some areas, whereas the 1997 guidelines are known for arduous specificity.
However, to benefit all physicians and specialties, both sets of guidelines apply to visit-level selection. In other words, physicians can utilize either set when documenting their services, and auditors must review provider records against both styles. The final audited outcome reflects the highest visit level supported upon comparison.
Elements of History2,3,4
Chief complaint. The chief complaint (CC) is the reason for the visit, as stated in the patient’s own words. Every encounter, regardless of visit type, must include a CC. The physician must personally document and/or validate the CC with reference to a specific condition or symptom (e.g. patient complains of abdominal pain).
History of present illness (HPI). The HPI is a description of the patient’s present illness as it developed. It characteristically is referenced as location, quality, severity, timing, context, modifying factors, and associated signs/symptoms, as related to the chief complaint. The 1997 guidelines allow physicians to receive HPI credit for providing the status of the patient’s chronic or inactive conditions, such as “extrinsic asthma without acute exacerbation in past six months.” An auditor will not assign HPI credit to a chronic or inactive condition that does not have a corresponding status (e.g. “asthma”). This will be considered “past medical history.”
The HPI is classified as brief (a comment on <3 HPI elements, or the status of <2 conditions) or extended (a comment on >4 HPI elements, or the status of >3 conditions). Consider these examples of an extended HPI:
- “The patient has intermittent (duration), sharp (quality) pain in the right upper quadrant (location) without associated nausea, vomiting, or diarrhea (associated signs/symptoms).”
- “Diabetes controlled by oral medication; hyperlipidemia stable on simvastatin with increased dietary efforts; hypertension stable with pressures ranging from 130-140/80-90.” (Status of three chronic conditions.)
Physicians receive credit for confirming and personally documenting the HPI, or linking to documentation recorded by residents (residents, fellows, interns) or nonphysician providers (NPPs) when performing services according to the Teaching Physician Rules or Split-Shared Billing Rules, respectively. An auditor will not assign physician credit for HPI elements documented by ancillary staff (registered nurses, medical assistants) or students.
Review of systems (ROS). The ROS is a series of questions used to elicit information about additional signs, symptoms, or problems currently or previously experienced by the patient: constitutional; eyes, ears, nose, mouth, throat; cardiovascular; respiratory; gastrointestinal; genitourinary; musculoskeletal; integumentary (including skin and/or breast); neurological; psychiatric; endocrine; hematologic/ lymphatic; and allergic/immunologic. Auditors classify the ROS as brief (a comment on one system), extended (a comment on two to nine systems), or complete (a comment on >10 systems). Physicians can document a complete ROS by noting individual systems: “no fever/chills (constitutional) or blurred vision (eyes); no chest pain (cardiovascular) or shortness of breath (respiratory); intermittent nausea (gastrointestinal); and occasional runny nose (ears, nose, mouth, throat),” or by eliciting a complete system review but documenting only the positive and pertinent negative findings related to the chief complaint, along with an additional comment that “all other systems are negative.”
Although the latter method is formally included in Medicare’s documentation guidelines and accepted by some Medicare contractors (e.g. Highmark, WPS), be aware that it is not universally accepted.5,6
Documentation involving the ROS can be provided by anyone, including the patient. The physician should reference ROS information that is completed by individuals other than residents or NPPs during services provided under the Teaching Physician Rules or Split-Shared Billing Rules. Physician duplication of ROS information is unnecessary unless an update or revision is required.
Past, family, and social history (PFSH). The PFSH involves data obtained about the patient’s previous illness or medical conditions/therapies, family occurrences with illness, and relevant patient activities. The PFSH could be classified as pertinent (a comment on one history) or complete (a comment in each of the three histories). The physician merely needs a single comment associated with each history for the PFSH to be regarded as complete. Refrain from using “noncontributory” to describe any of the histories, as previous misuse of this term has resulted in its prohibition. An example of a complete PFSH documentation includes: “Patient currently on Prilosec 20 mg daily; family history of Barrett’s esophagus; no tobacco or alcohol use.”
Similar to the ROS, PFSH documentation can be provided by anyone, including the patient, and the physician should reference the documented PFSH in his own progress note. Redocumentation of the PFSH is not necessary unless a revision is required.
PFSH documentation is only required for initial care services (i.e. initial hospital care, initial observation care, consultations). It is not warranted in subsequent care services unless additional, pertinent information is obtained during the hospital stay that impacts care.
Considerations
When a physician cannot elicit historical information from the patient directly, and no other source is available, they should document “unable to obtain” the history. A comment regarding the circumstances surrounding this problem (e.g. patient confused, no caregiver present) should be provided, along with the available information from the limited resources (e.g. emergency medical technicians, previous hospitalizations at the same facility). Some contractors will not penalize the physician for the inability to ascertain complete historical information, as long as a proven attempt to obtain the information is evident.
Never document any item for the purpose of “getting paid.” Only document information that is clinically relevant, lends to the quality of care provided, or demonstrates the delivery of healthcare services. This prevents accusations of fraud and abuse, promotes billing compliance, and supports medical necessity for the services provided.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Centers for Medicare & Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. CMS website. Available at: www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed July 7, 2011.
- Centers for Medicare & Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. CMS website. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed July 7, 2011.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011.
- History of E/M (Q&As). WPS Health Insurance website. Available at: http://www.wpsmedicare.com/j5macpartb/resources/provider_types/2009_0526_emqahistory.shtml. Accessed July 11, 2011.
- Frequently Asked Questions: Evaluation and Management Services (Part B). Highmark Medicare Services website. Available at: www.highmarkmedicareservices.com/faq/partb/pet/lpet-evaluation_management_services.html. Accessed on July 11, 2011.
Each visit category and level of service has corresponding documentation requirements.1 Selecting an evaluation and management (E/M) level is based upon 1) the content of the three “key” components: history, exam, and decision-making, or 2) time, but only when counseling or coordination of care dominates more than 50% of the physician’s total visit time. Failure to document any essential element in a given visit level (e.g. family history required but missing for 99222 and 99223) could result in downcoding or service denial. Be aware of what an auditor expects when reviewing the key component of “history.”
Documentation Options
Auditors recognize two sets of documentation guidelines: “1995” and “1997” guidelines.2,3,4 Each set of guidelines has received valid criticism. The 1995 guidelines undoubtedly are vague and subjective in some areas, whereas the 1997 guidelines are known for arduous specificity.
However, to benefit all physicians and specialties, both sets of guidelines apply to visit-level selection. In other words, physicians can utilize either set when documenting their services, and auditors must review provider records against both styles. The final audited outcome reflects the highest visit level supported upon comparison.
Elements of History2,3,4
Chief complaint. The chief complaint (CC) is the reason for the visit, as stated in the patient’s own words. Every encounter, regardless of visit type, must include a CC. The physician must personally document and/or validate the CC with reference to a specific condition or symptom (e.g. patient complains of abdominal pain).
History of present illness (HPI). The HPI is a description of the patient’s present illness as it developed. It characteristically is referenced as location, quality, severity, timing, context, modifying factors, and associated signs/symptoms, as related to the chief complaint. The 1997 guidelines allow physicians to receive HPI credit for providing the status of the patient’s chronic or inactive conditions, such as “extrinsic asthma without acute exacerbation in past six months.” An auditor will not assign HPI credit to a chronic or inactive condition that does not have a corresponding status (e.g. “asthma”). This will be considered “past medical history.”
The HPI is classified as brief (a comment on <3 HPI elements, or the status of <2 conditions) or extended (a comment on >4 HPI elements, or the status of >3 conditions). Consider these examples of an extended HPI:
- “The patient has intermittent (duration), sharp (quality) pain in the right upper quadrant (location) without associated nausea, vomiting, or diarrhea (associated signs/symptoms).”
- “Diabetes controlled by oral medication; hyperlipidemia stable on simvastatin with increased dietary efforts; hypertension stable with pressures ranging from 130-140/80-90.” (Status of three chronic conditions.)
Physicians receive credit for confirming and personally documenting the HPI, or linking to documentation recorded by residents (residents, fellows, interns) or nonphysician providers (NPPs) when performing services according to the Teaching Physician Rules or Split-Shared Billing Rules, respectively. An auditor will not assign physician credit for HPI elements documented by ancillary staff (registered nurses, medical assistants) or students.
Review of systems (ROS). The ROS is a series of questions used to elicit information about additional signs, symptoms, or problems currently or previously experienced by the patient: constitutional; eyes, ears, nose, mouth, throat; cardiovascular; respiratory; gastrointestinal; genitourinary; musculoskeletal; integumentary (including skin and/or breast); neurological; psychiatric; endocrine; hematologic/ lymphatic; and allergic/immunologic. Auditors classify the ROS as brief (a comment on one system), extended (a comment on two to nine systems), or complete (a comment on >10 systems). Physicians can document a complete ROS by noting individual systems: “no fever/chills (constitutional) or blurred vision (eyes); no chest pain (cardiovascular) or shortness of breath (respiratory); intermittent nausea (gastrointestinal); and occasional runny nose (ears, nose, mouth, throat),” or by eliciting a complete system review but documenting only the positive and pertinent negative findings related to the chief complaint, along with an additional comment that “all other systems are negative.”
Although the latter method is formally included in Medicare’s documentation guidelines and accepted by some Medicare contractors (e.g. Highmark, WPS), be aware that it is not universally accepted.5,6
Documentation involving the ROS can be provided by anyone, including the patient. The physician should reference ROS information that is completed by individuals other than residents or NPPs during services provided under the Teaching Physician Rules or Split-Shared Billing Rules. Physician duplication of ROS information is unnecessary unless an update or revision is required.
Past, family, and social history (PFSH). The PFSH involves data obtained about the patient’s previous illness or medical conditions/therapies, family occurrences with illness, and relevant patient activities. The PFSH could be classified as pertinent (a comment on one history) or complete (a comment in each of the three histories). The physician merely needs a single comment associated with each history for the PFSH to be regarded as complete. Refrain from using “noncontributory” to describe any of the histories, as previous misuse of this term has resulted in its prohibition. An example of a complete PFSH documentation includes: “Patient currently on Prilosec 20 mg daily; family history of Barrett’s esophagus; no tobacco or alcohol use.”
Similar to the ROS, PFSH documentation can be provided by anyone, including the patient, and the physician should reference the documented PFSH in his own progress note. Redocumentation of the PFSH is not necessary unless a revision is required.
PFSH documentation is only required for initial care services (i.e. initial hospital care, initial observation care, consultations). It is not warranted in subsequent care services unless additional, pertinent information is obtained during the hospital stay that impacts care.
Considerations
When a physician cannot elicit historical information from the patient directly, and no other source is available, they should document “unable to obtain” the history. A comment regarding the circumstances surrounding this problem (e.g. patient confused, no caregiver present) should be provided, along with the available information from the limited resources (e.g. emergency medical technicians, previous hospitalizations at the same facility). Some contractors will not penalize the physician for the inability to ascertain complete historical information, as long as a proven attempt to obtain the information is evident.
Never document any item for the purpose of “getting paid.” Only document information that is clinically relevant, lends to the quality of care provided, or demonstrates the delivery of healthcare services. This prevents accusations of fraud and abuse, promotes billing compliance, and supports medical necessity for the services provided.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Centers for Medicare & Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. CMS website. Available at: www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed July 7, 2011.
- Centers for Medicare & Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. CMS website. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed July 7, 2011.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011.
- History of E/M (Q&As). WPS Health Insurance website. Available at: http://www.wpsmedicare.com/j5macpartb/resources/provider_types/2009_0526_emqahistory.shtml. Accessed July 11, 2011.
- Frequently Asked Questions: Evaluation and Management Services (Part B). Highmark Medicare Services website. Available at: www.highmarkmedicareservices.com/faq/partb/pet/lpet-evaluation_management_services.html. Accessed on July 11, 2011.