User login
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Key Elements of Critical Care
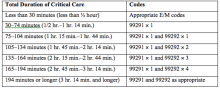
Code 99291 is used for critical care, evaluation, and management of the critically ill or critically injured patient, first 30–74 minutes.1 It is to be reported only once per day per physician or group member of the same specialty.
Code 99292 is for critical care, evaluation, and management of the critically ill or critically injured patient, each additional 30 minutes. It is to be listed separately in addition to the code for primary service.1 Code 99292 is categorized as an add-on code. It must be reported on the same invoice as its primary code, 99291. Multiple units of code 99292 can be reported per day per physician/group.
Despite the increased resources and references for critical care billing, critical care reporting issues persist. Medicare data analysis continues to identify 99291 as high risk for claim payment errors, perpetuating prepayment claim edits for outlier utilization and location discrepancies (i.e., settings other than inpatient hospital, outpatient hospital, or the emergency department). 2,3,4
Bolster your documentation with these three key elements.
Critical Illness, Injury Management
Current Procedural Terminology (CPT) and the Centers for Medicare & Medicaid Services (CMS) define “critical illness or injury” as a condition that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition (e.g., central nervous system failure; circulatory failure; shock; renal, hepatic, metabolic, and/or respiratory failure).5
Hospitalists providing care to the critically ill patient must perform highly complex decision making and interventions of high intensity that are required to prevent the patient’s inevitable decline. CMS further elaborates that “the patient shall be critically ill or injured at the time of the physician’s visit.”6 This is to ensure that hospitalists and other specialists support the medical necessity of the service and do not continue to report critical care codes on days after the patient has become stable and improved.
Consider the following scenarios:
CMS examples of patients whose medical condition may warrant critical care services (99291, 99292):6
- An 81-year-old male patient is admitted to the ICU following abdominal aortic aneurysm resection. Two days after surgery, he requires fluids and pressors to maintain adequate perfusion and arterial pressures. He remains ventilator dependent.
- A 67-year-old female patient is three days post mitral valve repair. She develops petechiae, hypotension, and hypoxia requiring respiratory and circulatory support.
- A 70-year-old admitted for right lower lobe pneumococcal pneumonia with a history of COPD becomes hypoxic and hypotensive two days after admission.
- A 68-year-old admitted for an acute anterior wall myocardial infarction continues to have symptomatic ventricular tachycardia that is marginally responsive to antiarrhythmic therapy.
CMS examples of patients who may not satisfy Medicare medical necessity criteria, or do not meet critical care criteria, or who do not have a critical care illness or injury and, therefore, are not eligible for critical care payment but may be reported using another appropriate hospital care code, such as subsequent hospital care codes (99231–99233), initial hospital care codes (99221–99223), or hospital consultation codes (99251–99255) when applicable:1,6
- Patients admitted to a critical care unit because no other hospital beds were available;
- Patients admitted to a critical care unit for close nursing observation and/or frequent monitoring of vital signs (e.g., drug toxicity or overdose);
- Patients admitted to a critical care unit because hospital rules require certain treatments (e.g., insulin infusions) to be administered in the critical care unit; and
- Patients receiving only care of a chronic illness in absence of care for a critical illness (e.g., daily management of a chronic ventilator patient, management of or care related to dialysis for end-stage renal disease). Services considered palliative in nature as this type of care do not meet the definition of critical care services.7
Concurrent Care
Critically ill patients often require the care of hospitalists and other specialists throughout the course of treatment. Payors are sensitive to the multiple hours billed by multiple providers for a single patient on a given day. Claim logic provides an automated response to only allow reimbursement for 99291 once per day when reported by physicians of the same group and specialty.8 Physicians of different specialties can separately report critical care hours as long as they are caring for a condition that meets the definition of critical care.
The CMS example of this: A dermatologist evaluates and treats a rash on an ICU patient who is maintained on a ventilator and nitroglycerine infusion that are being managed by an intensivist. The dermatologist should not report a service for critical care.6
Similarly for hospitalists, if an intensivist is taking care of the critical condition and there is nothing more for the hospitalist to add to the plan of care for the critical condition, critical care services may not be justified.
When different specialists are reporting critical care on the same day, it is imperative for the documentation to demonstrate that care is not duplicative of any other provider’s care (i.e., identify management of different conditions or revising elements of the plan). The care cannot overlap the same time period of any other physician reporting critical care services.
Calculating Time
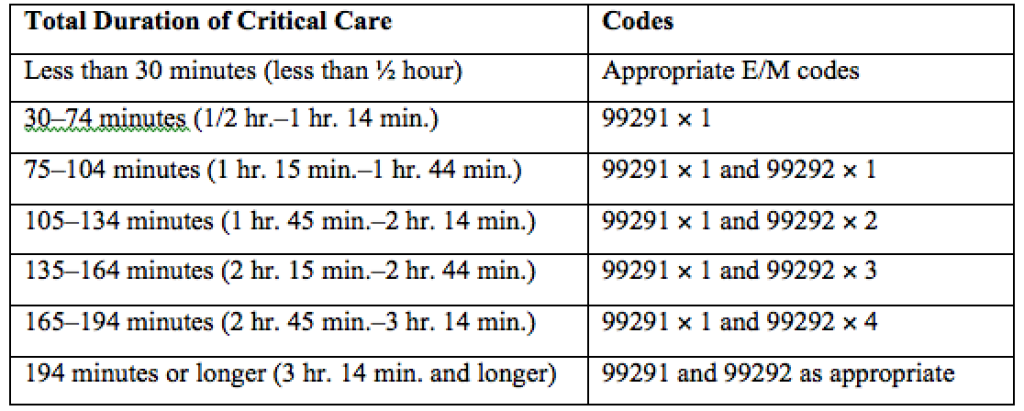
Critical care time constitutes bedside time and time spent on the patient’s unit/floor where the physician is immediately available to the patient (see Table 1). Certain labs, diagnostic studies, and procedures are considered inherent to critical care services and are not reported separately on the claim form: cardiac output measurements (93561, 93562); chest X-rays (71010, 71015, 71020); pulse oximetry (94760, 94761, 94762); blood gases and interpretation of data stored in computers, such as ECGs, blood pressures, and hematologic data (99090); gastric intubation (43752, 43753); temporary transcutaneous pacing (92953); ventilation management (94002–94004, 94660, 94662); and vascular access procedures (36000, 36410, 36415, 36591, 36600).1
Instead, physician time associated with the performance and/or interpretation of these services is toward the cumulative critical care time of the day. Services or procedures that are considered separately billable (e.g., central line placement, intubation, CPR) cannot contribute to critical care time.
When separately billable procedures are performed by the same provider/specialty group on the same day as critical care, physicians should make a notation in the medical record indicating the non-overlapping service times (e.g., “central line insertion is not included as critical care time”). This may assist with securing reimbursement when the payor requests the documentation for each reported claim item.
Activities on the floor/unit that do not directly contribute to patient care or management (e.g., review of literature, teaching rounds) cannot be counted toward critical care time. Do not count time associated with indirect care provided outside of the patient’s unit/floor (e.g., reviewing data or calling the family from the office) toward critical care time.
Family discussions can be counted toward critical care time but must take place at bedside or on the patient’s unit/floor. The patient must participate in the discussion unless medically unable or clinically incompetent to participate. If unable to participate, a notation in the chart must delineate the patient’s inability to participate and the reason.
Credited time can only involve obtaining a medical history and/or discussing treatment options or limitation(s) of treatment. The conversation must bear directly on patient management.1,7 Do not count time associated with providing periodic condition updates to the family, answering questions about the patient’s condition that are unrelated to decision making, or counseling the family during their grief process. If the conversation must take place via phone, it may be counted toward critical care time if the physician is calling from the patient’s unit/floor and the conversation involves the same criterion identified for face-to-face family meetings.10
Physicians should keep track of their critical care time throughout the day. Since critical care time is a cumulative service, each entry should include the total time that critical care services were provided (e.g., 45 minutes).10 Some payors may still impose the notation of “start-and-stop time” per encounter (e.g., 2–2:50 a.m.).
Same-specialty physicians (i.e., two hospitalists from the same group practice) may require separate claims. The initial critical care hour (99291) must be met by a single physician. Medically necessary critical care time beyond the first hour (99292) may be met individually by the same physician or collectively with another physician from the same group. The physician performing the additional time, beyond the first hour, reports the appropriate units of 99292 (see Table 1) under the corresponding NPI.11
CMS has issued instructions for contractors to recognize this atypical reporting method. However, non-Medicare payors may not recognize this newer reporting method and maintain that the cumulative service (by the same-specialty physician in the same provider group) should be reported under one physician name. Be sure to query the payors for appropriate reporting methods. TH
References
- Abraham M, Ahlman J, Boudreau A, Connelly J, Crosslin, R. Current Procedural Terminology 2015 Professional Edition. Chicago: American Medical Association Press; 2014. 23-25.
- Widespread prepayment targeted review notification—CPT 99291. Cahaba website. Available at: www.cahabagba.com/news/widespread-prepayment-targeted-review-notification-part-b/. Accessed December 17, 2015.
- Critical care CPT 99291 widespread prepayment targeted review results. Cahaba website. Available at: https://www.cahabagba.com/news/critical-care-cpt-99291-widespread-prepayment-targeted-review-results-2/. Accessed December 17, 2015.
- Prepayment edit of evaluation and management (E/M) code 99291. First Coast Service Options, Inc. website. Available at: medicare.fcso.com/Publications_B/2013/251608.pdf. Accessed December 17, 2015.
- Medicare claims processing manual: chapter 12, section 30.6.12A. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed December 17, 2015.
- Medicare claims processing manual: chapter 12, section 30.6.12B. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed December 17, 2015.
- Critical care fact sheet. CGS Administrators, LLC website. Available at: www.cgsmedicare.com/partb/mr/pdf/critical_care_fact_sheet.pdf. Accessed December 17, 2015.
- Same day same service policy. United Healthcare website. Available at: www.unitedhealthcareonline.com/ccmcontent/ProviderII/UHC/en-US/Main%20Menu/Tools%20&%20Resources/Policies%20and%20Protocols/Medicare%20Advantage%20Reimbursement%20Policies/S/SameDaySameService.pdf. Accessed December 17, 2015.
- Medicare claims processing manual: chapter 12, section 30.6.12G. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed December 17, 2015.
- Medicare claims processing manual: chapter 12, section 30.6.12E. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed December 17, 2015.
- Medicare claims processing manual: chapter 12, section 30.6.12I. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed December 17, 2015.
Code 99291 is used for critical care, evaluation, and management of the critically ill or critically injured patient, first 30–74 minutes.1 It is to be reported only once per day per physician or group member of the same specialty.
Code 99292 is for critical care, evaluation, and management of the critically ill or critically injured patient, each additional 30 minutes. It is to be listed separately in addition to the code for primary service.1 Code 99292 is categorized as an add-on code. It must be reported on the same invoice as its primary code, 99291. Multiple units of code 99292 can be reported per day per physician/group.
Despite the increased resources and references for critical care billing, critical care reporting issues persist. Medicare data analysis continues to identify 99291 as high risk for claim payment errors, perpetuating prepayment claim edits for outlier utilization and location discrepancies (i.e., settings other than inpatient hospital, outpatient hospital, or the emergency department). 2,3,4
Bolster your documentation with these three key elements.
Critical Illness, Injury Management
Current Procedural Terminology (CPT) and the Centers for Medicare & Medicaid Services (CMS) define “critical illness or injury” as a condition that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition (e.g., central nervous system failure; circulatory failure; shock; renal, hepatic, metabolic, and/or respiratory failure).5
Hospitalists providing care to the critically ill patient must perform highly complex decision making and interventions of high intensity that are required to prevent the patient’s inevitable decline. CMS further elaborates that “the patient shall be critically ill or injured at the time of the physician’s visit.”6 This is to ensure that hospitalists and other specialists support the medical necessity of the service and do not continue to report critical care codes on days after the patient has become stable and improved.
Consider the following scenarios:
CMS examples of patients whose medical condition may warrant critical care services (99291, 99292):6
- An 81-year-old male patient is admitted to the ICU following abdominal aortic aneurysm resection. Two days after surgery, he requires fluids and pressors to maintain adequate perfusion and arterial pressures. He remains ventilator dependent.
- A 67-year-old female patient is three days post mitral valve repair. She develops petechiae, hypotension, and hypoxia requiring respiratory and circulatory support.
- A 70-year-old admitted for right lower lobe pneumococcal pneumonia with a history of COPD becomes hypoxic and hypotensive two days after admission.
- A 68-year-old admitted for an acute anterior wall myocardial infarction continues to have symptomatic ventricular tachycardia that is marginally responsive to antiarrhythmic therapy.
CMS examples of patients who may not satisfy Medicare medical necessity criteria, or do not meet critical care criteria, or who do not have a critical care illness or injury and, therefore, are not eligible for critical care payment but may be reported using another appropriate hospital care code, such as subsequent hospital care codes (99231–99233), initial hospital care codes (99221–99223), or hospital consultation codes (99251–99255) when applicable:1,6
- Patients admitted to a critical care unit because no other hospital beds were available;
- Patients admitted to a critical care unit for close nursing observation and/or frequent monitoring of vital signs (e.g., drug toxicity or overdose);
- Patients admitted to a critical care unit because hospital rules require certain treatments (e.g., insulin infusions) to be administered in the critical care unit; and
- Patients receiving only care of a chronic illness in absence of care for a critical illness (e.g., daily management of a chronic ventilator patient, management of or care related to dialysis for end-stage renal disease). Services considered palliative in nature as this type of care do not meet the definition of critical care services.7
Concurrent Care
Critically ill patients often require the care of hospitalists and other specialists throughout the course of treatment. Payors are sensitive to the multiple hours billed by multiple providers for a single patient on a given day. Claim logic provides an automated response to only allow reimbursement for 99291 once per day when reported by physicians of the same group and specialty.8 Physicians of different specialties can separately report critical care hours as long as they are caring for a condition that meets the definition of critical care.
The CMS example of this: A dermatologist evaluates and treats a rash on an ICU patient who is maintained on a ventilator and nitroglycerine infusion that are being managed by an intensivist. The dermatologist should not report a service for critical care.6
Similarly for hospitalists, if an intensivist is taking care of the critical condition and there is nothing more for the hospitalist to add to the plan of care for the critical condition, critical care services may not be justified.
When different specialists are reporting critical care on the same day, it is imperative for the documentation to demonstrate that care is not duplicative of any other provider’s care (i.e., identify management of different conditions or revising elements of the plan). The care cannot overlap the same time period of any other physician reporting critical care services.
Calculating Time
Critical care time constitutes bedside time and time spent on the patient’s unit/floor where the physician is immediately available to the patient (see Table 1). Certain labs, diagnostic studies, and procedures are considered inherent to critical care services and are not reported separately on the claim form: cardiac output measurements (93561, 93562); chest X-rays (71010, 71015, 71020); pulse oximetry (94760, 94761, 94762); blood gases and interpretation of data stored in computers, such as ECGs, blood pressures, and hematologic data (99090); gastric intubation (43752, 43753); temporary transcutaneous pacing (92953); ventilation management (94002–94004, 94660, 94662); and vascular access procedures (36000, 36410, 36415, 36591, 36600).1
Instead, physician time associated with the performance and/or interpretation of these services is toward the cumulative critical care time of the day. Services or procedures that are considered separately billable (e.g., central line placement, intubation, CPR) cannot contribute to critical care time.
When separately billable procedures are performed by the same provider/specialty group on the same day as critical care, physicians should make a notation in the medical record indicating the non-overlapping service times (e.g., “central line insertion is not included as critical care time”). This may assist with securing reimbursement when the payor requests the documentation for each reported claim item.
Activities on the floor/unit that do not directly contribute to patient care or management (e.g., review of literature, teaching rounds) cannot be counted toward critical care time. Do not count time associated with indirect care provided outside of the patient’s unit/floor (e.g., reviewing data or calling the family from the office) toward critical care time.
Family discussions can be counted toward critical care time but must take place at bedside or on the patient’s unit/floor. The patient must participate in the discussion unless medically unable or clinically incompetent to participate. If unable to participate, a notation in the chart must delineate the patient’s inability to participate and the reason.
Credited time can only involve obtaining a medical history and/or discussing treatment options or limitation(s) of treatment. The conversation must bear directly on patient management.1,7 Do not count time associated with providing periodic condition updates to the family, answering questions about the patient’s condition that are unrelated to decision making, or counseling the family during their grief process. If the conversation must take place via phone, it may be counted toward critical care time if the physician is calling from the patient’s unit/floor and the conversation involves the same criterion identified for face-to-face family meetings.10
Physicians should keep track of their critical care time throughout the day. Since critical care time is a cumulative service, each entry should include the total time that critical care services were provided (e.g., 45 minutes).10 Some payors may still impose the notation of “start-and-stop time” per encounter (e.g., 2–2:50 a.m.).
Same-specialty physicians (i.e., two hospitalists from the same group practice) may require separate claims. The initial critical care hour (99291) must be met by a single physician. Medically necessary critical care time beyond the first hour (99292) may be met individually by the same physician or collectively with another physician from the same group. The physician performing the additional time, beyond the first hour, reports the appropriate units of 99292 (see Table 1) under the corresponding NPI.11
CMS has issued instructions for contractors to recognize this atypical reporting method. However, non-Medicare payors may not recognize this newer reporting method and maintain that the cumulative service (by the same-specialty physician in the same provider group) should be reported under one physician name. Be sure to query the payors for appropriate reporting methods. TH
References
- Abraham M, Ahlman J, Boudreau A, Connelly J, Crosslin, R. Current Procedural Terminology 2015 Professional Edition. Chicago: American Medical Association Press; 2014. 23-25.
- Widespread prepayment targeted review notification—CPT 99291. Cahaba website. Available at: www.cahabagba.com/news/widespread-prepayment-targeted-review-notification-part-b/. Accessed December 17, 2015.
- Critical care CPT 99291 widespread prepayment targeted review results. Cahaba website. Available at: https://www.cahabagba.com/news/critical-care-cpt-99291-widespread-prepayment-targeted-review-results-2/. Accessed December 17, 2015.
- Prepayment edit of evaluation and management (E/M) code 99291. First Coast Service Options, Inc. website. Available at: medicare.fcso.com/Publications_B/2013/251608.pdf. Accessed December 17, 2015.
- Medicare claims processing manual: chapter 12, section 30.6.12A. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed December 17, 2015.
- Medicare claims processing manual: chapter 12, section 30.6.12B. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed December 17, 2015.
- Critical care fact sheet. CGS Administrators, LLC website. Available at: www.cgsmedicare.com/partb/mr/pdf/critical_care_fact_sheet.pdf. Accessed December 17, 2015.
- Same day same service policy. United Healthcare website. Available at: www.unitedhealthcareonline.com/ccmcontent/ProviderII/UHC/en-US/Main%20Menu/Tools%20&%20Resources/Policies%20and%20Protocols/Medicare%20Advantage%20Reimbursement%20Policies/S/SameDaySameService.pdf. Accessed December 17, 2015.
- Medicare claims processing manual: chapter 12, section 30.6.12G. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed December 17, 2015.
- Medicare claims processing manual: chapter 12, section 30.6.12E. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed December 17, 2015.
- Medicare claims processing manual: chapter 12, section 30.6.12I. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed December 17, 2015.
Code 99291 is used for critical care, evaluation, and management of the critically ill or critically injured patient, first 30–74 minutes.1 It is to be reported only once per day per physician or group member of the same specialty.
Code 99292 is for critical care, evaluation, and management of the critically ill or critically injured patient, each additional 30 minutes. It is to be listed separately in addition to the code for primary service.1 Code 99292 is categorized as an add-on code. It must be reported on the same invoice as its primary code, 99291. Multiple units of code 99292 can be reported per day per physician/group.
Despite the increased resources and references for critical care billing, critical care reporting issues persist. Medicare data analysis continues to identify 99291 as high risk for claim payment errors, perpetuating prepayment claim edits for outlier utilization and location discrepancies (i.e., settings other than inpatient hospital, outpatient hospital, or the emergency department). 2,3,4
Bolster your documentation with these three key elements.
Critical Illness, Injury Management
Current Procedural Terminology (CPT) and the Centers for Medicare & Medicaid Services (CMS) define “critical illness or injury” as a condition that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition (e.g., central nervous system failure; circulatory failure; shock; renal, hepatic, metabolic, and/or respiratory failure).5
Hospitalists providing care to the critically ill patient must perform highly complex decision making and interventions of high intensity that are required to prevent the patient’s inevitable decline. CMS further elaborates that “the patient shall be critically ill or injured at the time of the physician’s visit.”6 This is to ensure that hospitalists and other specialists support the medical necessity of the service and do not continue to report critical care codes on days after the patient has become stable and improved.
Consider the following scenarios:
CMS examples of patients whose medical condition may warrant critical care services (99291, 99292):6
- An 81-year-old male patient is admitted to the ICU following abdominal aortic aneurysm resection. Two days after surgery, he requires fluids and pressors to maintain adequate perfusion and arterial pressures. He remains ventilator dependent.
- A 67-year-old female patient is three days post mitral valve repair. She develops petechiae, hypotension, and hypoxia requiring respiratory and circulatory support.
- A 70-year-old admitted for right lower lobe pneumococcal pneumonia with a history of COPD becomes hypoxic and hypotensive two days after admission.
- A 68-year-old admitted for an acute anterior wall myocardial infarction continues to have symptomatic ventricular tachycardia that is marginally responsive to antiarrhythmic therapy.
CMS examples of patients who may not satisfy Medicare medical necessity criteria, or do not meet critical care criteria, or who do not have a critical care illness or injury and, therefore, are not eligible for critical care payment but may be reported using another appropriate hospital care code, such as subsequent hospital care codes (99231–99233), initial hospital care codes (99221–99223), or hospital consultation codes (99251–99255) when applicable:1,6
- Patients admitted to a critical care unit because no other hospital beds were available;
- Patients admitted to a critical care unit for close nursing observation and/or frequent monitoring of vital signs (e.g., drug toxicity or overdose);
- Patients admitted to a critical care unit because hospital rules require certain treatments (e.g., insulin infusions) to be administered in the critical care unit; and
- Patients receiving only care of a chronic illness in absence of care for a critical illness (e.g., daily management of a chronic ventilator patient, management of or care related to dialysis for end-stage renal disease). Services considered palliative in nature as this type of care do not meet the definition of critical care services.7
Concurrent Care
Critically ill patients often require the care of hospitalists and other specialists throughout the course of treatment. Payors are sensitive to the multiple hours billed by multiple providers for a single patient on a given day. Claim logic provides an automated response to only allow reimbursement for 99291 once per day when reported by physicians of the same group and specialty.8 Physicians of different specialties can separately report critical care hours as long as they are caring for a condition that meets the definition of critical care.
The CMS example of this: A dermatologist evaluates and treats a rash on an ICU patient who is maintained on a ventilator and nitroglycerine infusion that are being managed by an intensivist. The dermatologist should not report a service for critical care.6
Similarly for hospitalists, if an intensivist is taking care of the critical condition and there is nothing more for the hospitalist to add to the plan of care for the critical condition, critical care services may not be justified.
When different specialists are reporting critical care on the same day, it is imperative for the documentation to demonstrate that care is not duplicative of any other provider’s care (i.e., identify management of different conditions or revising elements of the plan). The care cannot overlap the same time period of any other physician reporting critical care services.
Calculating Time
Critical care time constitutes bedside time and time spent on the patient’s unit/floor where the physician is immediately available to the patient (see Table 1). Certain labs, diagnostic studies, and procedures are considered inherent to critical care services and are not reported separately on the claim form: cardiac output measurements (93561, 93562); chest X-rays (71010, 71015, 71020); pulse oximetry (94760, 94761, 94762); blood gases and interpretation of data stored in computers, such as ECGs, blood pressures, and hematologic data (99090); gastric intubation (43752, 43753); temporary transcutaneous pacing (92953); ventilation management (94002–94004, 94660, 94662); and vascular access procedures (36000, 36410, 36415, 36591, 36600).1
Instead, physician time associated with the performance and/or interpretation of these services is toward the cumulative critical care time of the day. Services or procedures that are considered separately billable (e.g., central line placement, intubation, CPR) cannot contribute to critical care time.
When separately billable procedures are performed by the same provider/specialty group on the same day as critical care, physicians should make a notation in the medical record indicating the non-overlapping service times (e.g., “central line insertion is not included as critical care time”). This may assist with securing reimbursement when the payor requests the documentation for each reported claim item.
Activities on the floor/unit that do not directly contribute to patient care or management (e.g., review of literature, teaching rounds) cannot be counted toward critical care time. Do not count time associated with indirect care provided outside of the patient’s unit/floor (e.g., reviewing data or calling the family from the office) toward critical care time.
Family discussions can be counted toward critical care time but must take place at bedside or on the patient’s unit/floor. The patient must participate in the discussion unless medically unable or clinically incompetent to participate. If unable to participate, a notation in the chart must delineate the patient’s inability to participate and the reason.
Credited time can only involve obtaining a medical history and/or discussing treatment options or limitation(s) of treatment. The conversation must bear directly on patient management.1,7 Do not count time associated with providing periodic condition updates to the family, answering questions about the patient’s condition that are unrelated to decision making, or counseling the family during their grief process. If the conversation must take place via phone, it may be counted toward critical care time if the physician is calling from the patient’s unit/floor and the conversation involves the same criterion identified for face-to-face family meetings.10
Physicians should keep track of their critical care time throughout the day. Since critical care time is a cumulative service, each entry should include the total time that critical care services were provided (e.g., 45 minutes).10 Some payors may still impose the notation of “start-and-stop time” per encounter (e.g., 2–2:50 a.m.).
Same-specialty physicians (i.e., two hospitalists from the same group practice) may require separate claims. The initial critical care hour (99291) must be met by a single physician. Medically necessary critical care time beyond the first hour (99292) may be met individually by the same physician or collectively with another physician from the same group. The physician performing the additional time, beyond the first hour, reports the appropriate units of 99292 (see Table 1) under the corresponding NPI.11
CMS has issued instructions for contractors to recognize this atypical reporting method. However, non-Medicare payors may not recognize this newer reporting method and maintain that the cumulative service (by the same-specialty physician in the same provider group) should be reported under one physician name. Be sure to query the payors for appropriate reporting methods. TH
References
- Abraham M, Ahlman J, Boudreau A, Connelly J, Crosslin, R. Current Procedural Terminology 2015 Professional Edition. Chicago: American Medical Association Press; 2014. 23-25.
- Widespread prepayment targeted review notification—CPT 99291. Cahaba website. Available at: www.cahabagba.com/news/widespread-prepayment-targeted-review-notification-part-b/. Accessed December 17, 2015.
- Critical care CPT 99291 widespread prepayment targeted review results. Cahaba website. Available at: https://www.cahabagba.com/news/critical-care-cpt-99291-widespread-prepayment-targeted-review-results-2/. Accessed December 17, 2015.
- Prepayment edit of evaluation and management (E/M) code 99291. First Coast Service Options, Inc. website. Available at: medicare.fcso.com/Publications_B/2013/251608.pdf. Accessed December 17, 2015.
- Medicare claims processing manual: chapter 12, section 30.6.12A. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed December 17, 2015.
- Medicare claims processing manual: chapter 12, section 30.6.12B. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed December 17, 2015.
- Critical care fact sheet. CGS Administrators, LLC website. Available at: www.cgsmedicare.com/partb/mr/pdf/critical_care_fact_sheet.pdf. Accessed December 17, 2015.
- Same day same service policy. United Healthcare website. Available at: www.unitedhealthcareonline.com/ccmcontent/ProviderII/UHC/en-US/Main%20Menu/Tools%20&%20Resources/Policies%20and%20Protocols/Medicare%20Advantage%20Reimbursement%20Policies/S/SameDaySameService.pdf. Accessed December 17, 2015.
- Medicare claims processing manual: chapter 12, section 30.6.12G. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed December 17, 2015.
- Medicare claims processing manual: chapter 12, section 30.6.12E. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed December 17, 2015.
- Medicare claims processing manual: chapter 12, section 30.6.12I. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed December 17, 2015.
ICD-10 Flexibility Helps Transition to New Coding Systems, Principles, Payer Policy Requirements
Effective October 1, providers submit claims with ICD-10-CM codes. As they adapt to this new system, physicians, clinical staff, and billers should be relying on feedback from each other to achieve a successful transition. On July 6, the Centers for Medicare and Medicaid Services (CMS), in conjunction with the AMA, issued a letter to the provider community offering ICD-10-CM guidance. The joint announcement and guidance regarding ICD-10 flexibilities minimizes the anxiety that often accompanies change and clarifies a few key points about claim scrutiny.1
According to the correspondence, “CMS is releasing additional guidance that will allow for flexibility in the claims auditing and quality reporting process as the medical community gains experience using the new ICD-10 code set.”1 The guidance specifies the flexibility that will be used during the first 12 months of ICD-10-CM use.
This “flexibility” is an opportunity and should not be disregarded. Physician practices can effectively use this time to become accustomed to the ICD-10-CM system, correct coding principles, and payer policy requirements. Internal audit and review processes should increase in order to correct or confirm appropriate coding and claim submission.
Valid Codes
Medicare review contractors are instructed “not to deny physician or other practitioner claims billed under the Part B physician fee schedule through either automated medical review or complex medical review based solely on the specificity of the ICD-10 diagnosis code as long as the physician/practitioner used a valid code from the right family.”2 This “flexibility” will only occur for the first 12 months of ICD-10-CM implementation; the ultimate goal is for providers to assign the correct diagnosis code and the appropriate level of specificity after one year.
The “family code” allowance should not be confused with provision of an incomplete or truncated diagnosis code; these types of codes will always result in claim denial. The ICD-10-CM code presented on the claim form must be carried out to the highest character available for that particular code.
For example, an initial encounter involving an infected peripherally inserted central catheter (PICC) is reported with ICD-10-CM T80.212A (local infection due to central venous catheter). An individual unfamiliar with ICD-10-CM nomenclature may not realize that the seventh extension character of the code is required to carry the code out to its highest level of specificity. If T880.212 is mistakenly reported because the encounter detail (i.e., initial encounter [A], subsequent encounter [D], or sequela [S]) was not documented or provided to the biller, the payers’ claim edit system will identify this as a truncated or invalid diagnosis and reject the claim. Therefore, the code is required to be complete. The “flexibility” refers to reporting the code that best reflects the documented condition. As long as the reported code comes from the same family of codes and is valid, the claim cannot be denied.
Code Families
Code families are “codes within a category [that] are clinically related and provide differences in capturing specific information on the type of condition.”3 Upon review, Medicare will allow ICD-10-CM codes from the same code family to be reported on the claim without penalty if the most accurate code is not selected.
For example, a patient with COPD with acute exacerbation is admitted to the hospital. During the 12-month “flexibility” period, the claim could include J44.9 (COPD, unspecified) without being considered erroneous. The most appropriate code, however, is J44.1 (COPD with acute exacerbation). During the course of the hospitalization, if the physician determines that the COPD exacerbation was caused by an acute lower respiratory infection, J44.0 (COPD with acute lower respiratory infection) is the best option.
The provider goal for this flexibility period is to identify all of the “unspecified codes” used on their claims, review the documentation, and determine the most appropriate code. The practice staff assigned to this task would then provide feedback to the physicians to enhance their future reporting strategies. Although “unspecified” codes are often reported by default, physicians and staff should attempt to reduce usage of this code type unless the patient’s condition is unable to be further specified or categorized at a given point in time.
For example, it would not be acceptable to report R10.8 (unspecified abdominal pain) when a more specific diagnosis code can be easily determined by patient history or exam findings (e.g. right upper quadrant abdominal pain, R10.11).
Affected Claims
As previously stated, “Medicare review contractors will not deny physician or other practitioner claims billed under the Part B physician fee schedule through either automated medical review or complex medical record review.”3 The review contractors included are as follows:
- Medicare Administrative Contractors (MACs) process claims submitted by physicians, hospitals, and other healthcare professionals and submit payment to those providers according to Medicare rules and regulations (including identifying and correcting underpayments and overpayments);
- Recovery Auditors (RACs) review claims to identify potential underpayments and overpayments in Medicare fee-for-service, as part of the Recovery Audit Program;
- Zone Program Integrity Contractors (ZPICs) perform investigations that are unique and tailored to the specific circumstances and occur only in situations where there is potential fraud and take appropriate corrective actions; and
- Supplemental Medical Review Contractor (SMRCs) conduct nationwide medical review as directed by CMS (including identifying underpayments and overpayments).4
This instruction applies to claims that are typically selected for review due to the ICD-10-CM code used on the claim but does not affect claims that are selected for review for other reasons (e.g. modifier 25 [separately identifiable visit performed on the same day as another procedure or service], unbundling, service-specific current procedural terminology code). If a claim is selected for one of these other reasons and does not meet the corresponding criterion, the service will be denied. This instruction also excludes claims for services that correspond to an existing local coverage determination (LCD) or national coverage determination (NCD).
For example, an esophagogastroduodenoscopy (EGD) is not considered “medically necessary” when reported with R10.8 (unspecified abdominal pain) and would be denied. EGD requires a more specific diagnosis (e.g. right upper quadrant abdominal pain, R10.11) per Medicare LCD.
Non-Medicare Payer Considerations
Most payers that are required to convert to ICD-10-CM have also provided some guidance about claim submission. Although most do not address the audit and review process, payers will follow some basic principles:
- Claims submitted with service dates on or after October 1 must use ICD-10-CM codes.
- Claims submitted with service dates prior to October 1 must use ICD-9-CM codes; this includes claims that are initially submitted after October 1 or require correction and resubmission after October 1.
- Physician claims will be held to medical necessity guidelines identified by specific ICD-10-CM codes represented in existing payer policies.
- General equivalence mappings (GEMs) should only be used as a starting point to convert large databases and large code lists from ICD-9 to ICD-10. Many ICD-9-CM codes do not crosswalk directly to an ICD-10-CM code. Physician and staff should continue to use the ICD-10-CM coding books and resources to determine the most accurate code selection.
- “Unspecified” codes are only for use when the information in the medical record is insufficient to assign a more specific code.5,6,7
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. CMS and AMA announce efforts to help providers get ready for ICD-10. July 6, 2015. Accessed October 3, 2015.
- Centers for Medicare and Medicaid Services. CMS and AMA announce efforts to help providers get ready for ICD-10: frequently asked questions. Accessed October 3, 2015.
- Centers for Medicare and Medicaid Services. Clarifying questions and answers related to the July 6, 2015 CMS/AMA joint announcement and guidance regarding ICD-10 flexibilities. Accessed October 3, 2015.
- Centers for Medicare and Medicaid Services. Medicare Learning Network: Medicare claim review programs. May 2015. Accessed October 3, 2015.
- Aetna. Preparation for ICD-10-CM: frequently asked questions. Accessed October 3, 2015.
- Independence Blue Cross. Transition to ICD-10: frequently asked questions. Accessed October 3, 2015.
- Cigna. Ready, Set, Switch: Know Your ICD-10 Codes. Accessed November 16, 2015.
Effective October 1, providers submit claims with ICD-10-CM codes. As they adapt to this new system, physicians, clinical staff, and billers should be relying on feedback from each other to achieve a successful transition. On July 6, the Centers for Medicare and Medicaid Services (CMS), in conjunction with the AMA, issued a letter to the provider community offering ICD-10-CM guidance. The joint announcement and guidance regarding ICD-10 flexibilities minimizes the anxiety that often accompanies change and clarifies a few key points about claim scrutiny.1
According to the correspondence, “CMS is releasing additional guidance that will allow for flexibility in the claims auditing and quality reporting process as the medical community gains experience using the new ICD-10 code set.”1 The guidance specifies the flexibility that will be used during the first 12 months of ICD-10-CM use.
This “flexibility” is an opportunity and should not be disregarded. Physician practices can effectively use this time to become accustomed to the ICD-10-CM system, correct coding principles, and payer policy requirements. Internal audit and review processes should increase in order to correct or confirm appropriate coding and claim submission.
Valid Codes
Medicare review contractors are instructed “not to deny physician or other practitioner claims billed under the Part B physician fee schedule through either automated medical review or complex medical review based solely on the specificity of the ICD-10 diagnosis code as long as the physician/practitioner used a valid code from the right family.”2 This “flexibility” will only occur for the first 12 months of ICD-10-CM implementation; the ultimate goal is for providers to assign the correct diagnosis code and the appropriate level of specificity after one year.
The “family code” allowance should not be confused with provision of an incomplete or truncated diagnosis code; these types of codes will always result in claim denial. The ICD-10-CM code presented on the claim form must be carried out to the highest character available for that particular code.
For example, an initial encounter involving an infected peripherally inserted central catheter (PICC) is reported with ICD-10-CM T80.212A (local infection due to central venous catheter). An individual unfamiliar with ICD-10-CM nomenclature may not realize that the seventh extension character of the code is required to carry the code out to its highest level of specificity. If T880.212 is mistakenly reported because the encounter detail (i.e., initial encounter [A], subsequent encounter [D], or sequela [S]) was not documented or provided to the biller, the payers’ claim edit system will identify this as a truncated or invalid diagnosis and reject the claim. Therefore, the code is required to be complete. The “flexibility” refers to reporting the code that best reflects the documented condition. As long as the reported code comes from the same family of codes and is valid, the claim cannot be denied.
Code Families
Code families are “codes within a category [that] are clinically related and provide differences in capturing specific information on the type of condition.”3 Upon review, Medicare will allow ICD-10-CM codes from the same code family to be reported on the claim without penalty if the most accurate code is not selected.
For example, a patient with COPD with acute exacerbation is admitted to the hospital. During the 12-month “flexibility” period, the claim could include J44.9 (COPD, unspecified) without being considered erroneous. The most appropriate code, however, is J44.1 (COPD with acute exacerbation). During the course of the hospitalization, if the physician determines that the COPD exacerbation was caused by an acute lower respiratory infection, J44.0 (COPD with acute lower respiratory infection) is the best option.
The provider goal for this flexibility period is to identify all of the “unspecified codes” used on their claims, review the documentation, and determine the most appropriate code. The practice staff assigned to this task would then provide feedback to the physicians to enhance their future reporting strategies. Although “unspecified” codes are often reported by default, physicians and staff should attempt to reduce usage of this code type unless the patient’s condition is unable to be further specified or categorized at a given point in time.
For example, it would not be acceptable to report R10.8 (unspecified abdominal pain) when a more specific diagnosis code can be easily determined by patient history or exam findings (e.g. right upper quadrant abdominal pain, R10.11).
Affected Claims
As previously stated, “Medicare review contractors will not deny physician or other practitioner claims billed under the Part B physician fee schedule through either automated medical review or complex medical record review.”3 The review contractors included are as follows:
- Medicare Administrative Contractors (MACs) process claims submitted by physicians, hospitals, and other healthcare professionals and submit payment to those providers according to Medicare rules and regulations (including identifying and correcting underpayments and overpayments);
- Recovery Auditors (RACs) review claims to identify potential underpayments and overpayments in Medicare fee-for-service, as part of the Recovery Audit Program;
- Zone Program Integrity Contractors (ZPICs) perform investigations that are unique and tailored to the specific circumstances and occur only in situations where there is potential fraud and take appropriate corrective actions; and
- Supplemental Medical Review Contractor (SMRCs) conduct nationwide medical review as directed by CMS (including identifying underpayments and overpayments).4
This instruction applies to claims that are typically selected for review due to the ICD-10-CM code used on the claim but does not affect claims that are selected for review for other reasons (e.g. modifier 25 [separately identifiable visit performed on the same day as another procedure or service], unbundling, service-specific current procedural terminology code). If a claim is selected for one of these other reasons and does not meet the corresponding criterion, the service will be denied. This instruction also excludes claims for services that correspond to an existing local coverage determination (LCD) or national coverage determination (NCD).
For example, an esophagogastroduodenoscopy (EGD) is not considered “medically necessary” when reported with R10.8 (unspecified abdominal pain) and would be denied. EGD requires a more specific diagnosis (e.g. right upper quadrant abdominal pain, R10.11) per Medicare LCD.
Non-Medicare Payer Considerations
Most payers that are required to convert to ICD-10-CM have also provided some guidance about claim submission. Although most do not address the audit and review process, payers will follow some basic principles:
- Claims submitted with service dates on or after October 1 must use ICD-10-CM codes.
- Claims submitted with service dates prior to October 1 must use ICD-9-CM codes; this includes claims that are initially submitted after October 1 or require correction and resubmission after October 1.
- Physician claims will be held to medical necessity guidelines identified by specific ICD-10-CM codes represented in existing payer policies.
- General equivalence mappings (GEMs) should only be used as a starting point to convert large databases and large code lists from ICD-9 to ICD-10. Many ICD-9-CM codes do not crosswalk directly to an ICD-10-CM code. Physician and staff should continue to use the ICD-10-CM coding books and resources to determine the most accurate code selection.
- “Unspecified” codes are only for use when the information in the medical record is insufficient to assign a more specific code.5,6,7
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. CMS and AMA announce efforts to help providers get ready for ICD-10. July 6, 2015. Accessed October 3, 2015.
- Centers for Medicare and Medicaid Services. CMS and AMA announce efforts to help providers get ready for ICD-10: frequently asked questions. Accessed October 3, 2015.
- Centers for Medicare and Medicaid Services. Clarifying questions and answers related to the July 6, 2015 CMS/AMA joint announcement and guidance regarding ICD-10 flexibilities. Accessed October 3, 2015.
- Centers for Medicare and Medicaid Services. Medicare Learning Network: Medicare claim review programs. May 2015. Accessed October 3, 2015.
- Aetna. Preparation for ICD-10-CM: frequently asked questions. Accessed October 3, 2015.
- Independence Blue Cross. Transition to ICD-10: frequently asked questions. Accessed October 3, 2015.
- Cigna. Ready, Set, Switch: Know Your ICD-10 Codes. Accessed November 16, 2015.
Effective October 1, providers submit claims with ICD-10-CM codes. As they adapt to this new system, physicians, clinical staff, and billers should be relying on feedback from each other to achieve a successful transition. On July 6, the Centers for Medicare and Medicaid Services (CMS), in conjunction with the AMA, issued a letter to the provider community offering ICD-10-CM guidance. The joint announcement and guidance regarding ICD-10 flexibilities minimizes the anxiety that often accompanies change and clarifies a few key points about claim scrutiny.1
According to the correspondence, “CMS is releasing additional guidance that will allow for flexibility in the claims auditing and quality reporting process as the medical community gains experience using the new ICD-10 code set.”1 The guidance specifies the flexibility that will be used during the first 12 months of ICD-10-CM use.
This “flexibility” is an opportunity and should not be disregarded. Physician practices can effectively use this time to become accustomed to the ICD-10-CM system, correct coding principles, and payer policy requirements. Internal audit and review processes should increase in order to correct or confirm appropriate coding and claim submission.
Valid Codes
Medicare review contractors are instructed “not to deny physician or other practitioner claims billed under the Part B physician fee schedule through either automated medical review or complex medical review based solely on the specificity of the ICD-10 diagnosis code as long as the physician/practitioner used a valid code from the right family.”2 This “flexibility” will only occur for the first 12 months of ICD-10-CM implementation; the ultimate goal is for providers to assign the correct diagnosis code and the appropriate level of specificity after one year.
The “family code” allowance should not be confused with provision of an incomplete or truncated diagnosis code; these types of codes will always result in claim denial. The ICD-10-CM code presented on the claim form must be carried out to the highest character available for that particular code.
For example, an initial encounter involving an infected peripherally inserted central catheter (PICC) is reported with ICD-10-CM T80.212A (local infection due to central venous catheter). An individual unfamiliar with ICD-10-CM nomenclature may not realize that the seventh extension character of the code is required to carry the code out to its highest level of specificity. If T880.212 is mistakenly reported because the encounter detail (i.e., initial encounter [A], subsequent encounter [D], or sequela [S]) was not documented or provided to the biller, the payers’ claim edit system will identify this as a truncated or invalid diagnosis and reject the claim. Therefore, the code is required to be complete. The “flexibility” refers to reporting the code that best reflects the documented condition. As long as the reported code comes from the same family of codes and is valid, the claim cannot be denied.
Code Families
Code families are “codes within a category [that] are clinically related and provide differences in capturing specific information on the type of condition.”3 Upon review, Medicare will allow ICD-10-CM codes from the same code family to be reported on the claim without penalty if the most accurate code is not selected.
For example, a patient with COPD with acute exacerbation is admitted to the hospital. During the 12-month “flexibility” period, the claim could include J44.9 (COPD, unspecified) without being considered erroneous. The most appropriate code, however, is J44.1 (COPD with acute exacerbation). During the course of the hospitalization, if the physician determines that the COPD exacerbation was caused by an acute lower respiratory infection, J44.0 (COPD with acute lower respiratory infection) is the best option.
The provider goal for this flexibility period is to identify all of the “unspecified codes” used on their claims, review the documentation, and determine the most appropriate code. The practice staff assigned to this task would then provide feedback to the physicians to enhance their future reporting strategies. Although “unspecified” codes are often reported by default, physicians and staff should attempt to reduce usage of this code type unless the patient’s condition is unable to be further specified or categorized at a given point in time.
For example, it would not be acceptable to report R10.8 (unspecified abdominal pain) when a more specific diagnosis code can be easily determined by patient history or exam findings (e.g. right upper quadrant abdominal pain, R10.11).
Affected Claims
As previously stated, “Medicare review contractors will not deny physician or other practitioner claims billed under the Part B physician fee schedule through either automated medical review or complex medical record review.”3 The review contractors included are as follows:
- Medicare Administrative Contractors (MACs) process claims submitted by physicians, hospitals, and other healthcare professionals and submit payment to those providers according to Medicare rules and regulations (including identifying and correcting underpayments and overpayments);
- Recovery Auditors (RACs) review claims to identify potential underpayments and overpayments in Medicare fee-for-service, as part of the Recovery Audit Program;
- Zone Program Integrity Contractors (ZPICs) perform investigations that are unique and tailored to the specific circumstances and occur only in situations where there is potential fraud and take appropriate corrective actions; and
- Supplemental Medical Review Contractor (SMRCs) conduct nationwide medical review as directed by CMS (including identifying underpayments and overpayments).4
This instruction applies to claims that are typically selected for review due to the ICD-10-CM code used on the claim but does not affect claims that are selected for review for other reasons (e.g. modifier 25 [separately identifiable visit performed on the same day as another procedure or service], unbundling, service-specific current procedural terminology code). If a claim is selected for one of these other reasons and does not meet the corresponding criterion, the service will be denied. This instruction also excludes claims for services that correspond to an existing local coverage determination (LCD) or national coverage determination (NCD).
For example, an esophagogastroduodenoscopy (EGD) is not considered “medically necessary” when reported with R10.8 (unspecified abdominal pain) and would be denied. EGD requires a more specific diagnosis (e.g. right upper quadrant abdominal pain, R10.11) per Medicare LCD.
Non-Medicare Payer Considerations
Most payers that are required to convert to ICD-10-CM have also provided some guidance about claim submission. Although most do not address the audit and review process, payers will follow some basic principles:
- Claims submitted with service dates on or after October 1 must use ICD-10-CM codes.
- Claims submitted with service dates prior to October 1 must use ICD-9-CM codes; this includes claims that are initially submitted after October 1 or require correction and resubmission after October 1.
- Physician claims will be held to medical necessity guidelines identified by specific ICD-10-CM codes represented in existing payer policies.
- General equivalence mappings (GEMs) should only be used as a starting point to convert large databases and large code lists from ICD-9 to ICD-10. Many ICD-9-CM codes do not crosswalk directly to an ICD-10-CM code. Physician and staff should continue to use the ICD-10-CM coding books and resources to determine the most accurate code selection.
- “Unspecified” codes are only for use when the information in the medical record is insufficient to assign a more specific code.5,6,7
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. CMS and AMA announce efforts to help providers get ready for ICD-10. July 6, 2015. Accessed October 3, 2015.
- Centers for Medicare and Medicaid Services. CMS and AMA announce efforts to help providers get ready for ICD-10: frequently asked questions. Accessed October 3, 2015.
- Centers for Medicare and Medicaid Services. Clarifying questions and answers related to the July 6, 2015 CMS/AMA joint announcement and guidance regarding ICD-10 flexibilities. Accessed October 3, 2015.
- Centers for Medicare and Medicaid Services. Medicare Learning Network: Medicare claim review programs. May 2015. Accessed October 3, 2015.
- Aetna. Preparation for ICD-10-CM: frequently asked questions. Accessed October 3, 2015.
- Independence Blue Cross. Transition to ICD-10: frequently asked questions. Accessed October 3, 2015.
- Cigna. Ready, Set, Switch: Know Your ICD-10 Codes. Accessed November 16, 2015.
Billing, Coding Documentation to Support Services, Minimize Risks
The electronic health record (EHR) has many benefits:
- Improved patient care;
- Improved care coordination;
- Improved diagnostics and patient outcomes;
- Increased patient participation; and
- Increased practice efficiencies and cost savings.1
EHRs also introduce risks, however. Heightened concern about EHR misuse and vulnerability elevates the level of scrutiny placed on provider documentation as it relates to billing and coding. Without clear guidelines from the Centers for Medicare and Medicaid Services (CMS) or other payers, the potential for unintentional misapplication exists. Auditor misinterpretation is also possible. Providers should utilize simple defensive documentation principles to support their services and minimize their risks.
Reason for Encounter
Under section 1862 (a)(1)(A) of the Social Security Act, the Medicare Program may only pay for items and services that are “reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member,” unless there is another statutory authorization for payment (e.g. colorectal cancer screening).2
A payer can determine if a service is “reasonable and necessary” based on the service indication. The reason for the patient encounter, otherwise known as the chief complaint, must be evident. This can be a symptom, problem, condition, diagnosis, physician-recommended return, or another factor that necessitates the encounter.1 It cannot be inferred and must be clearly stated in the documentation. Without it, a payer may question the medical necessity of the service, especially if it involves hospital-based services in the course of which multiple specialists will see the patient on any given date. Payers are likely to deny services that cannot be easily differentiated (e.g. “no c/o”). Furthermore, payers can deny concurrent care services for the following reasons:3
- Services exceed normal frequency or duration for a given condition without documented circumstances requiring additional care; or
- Services by one physician duplicate/overlap those of the other provider without any recognizable distinction.
Providers should be specific in identifying the encounter reason, as in the following examples: “Patient seen for shortness of breath” or “Patient with COPD, feeling improved with 3L O2 NC.”
Assessment and Plan
Accurately representing patient complexity for every visit throughout the hospitalization presents its challenges. Although the problem list may not dramatically change day to day, providers must formulate an assessment of the patient’s condition with a corresponding plan of care for each encounter. Documenting problems without a corresponding plan of care does not substantiate physician participation in the management of that problem. Providing a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) minimizes the complexity and effort put forth in the encounter and could result in auditor downgrading upon documentation review.
Developing shortcuts might falsely minimize the provider’s documentation burden. An electronic documentation system might make it possible to copy previous progress notes into the current encounter to save time; however, the previously entered information could include elements that do not require reassessment during a subsequent encounter or contain information about conditions that are being managed concurrently by another specialist (e.g. CKD being managed by the nephrologist). Leaving the copied information unmodified may not accurately reflect the patient’s current condition or the care provided by the hospitalist during the current encounter. Information that is pulled forward or copied and pasted from a previous entry should be modified to demonstrate updated content and nonoverlapping care relevant to that date.
According to the Office of Inspector General (OIG), “inappropriate copy-pasting could facilitate attempts to inflate claims and duplicate or create fraudulent claims.”4
An equally problematic EHR function involves “overdocumentation,” the practice of inserting false or irrelevant documentation to create the appearance of support for billing higher level services.4 EHR technology has the ability to auto-populate fields using templates built into the system or generate extensive documentation on the basis of a single click. The OIG cautions providers to use these features carefully, because they can produce information suggesting the practitioner performed more comprehensive services than were actually rendered.4
An example is the inclusion of the same lab results more than once. Although clinicians include this information as a reference to avoid having to “find it somewhere in the chart” when it is needed—as a basis for comparison, for example—auditors mistake this as an attempt to gain credit for the daily review of the same “old” information. Including only relevant data will mitigate this concern.
Authorship
Dates and signatures are essential to each encounter. Medicare requires services provided/ordered to be authenticated by the author.5 A reviewer must be able to identify each individual who performs, documents, and bills for a service on a given date. Progress notes that fail to identify the service date or service provider will likely result in denial.
Additionally, a service is questioned when two different sets of handwriting appear on a note, yet only one signature is provided. Since the reviewer cannot confirm the credentials of the unidentified individual and cannot be sure which portion belongs to the identified individual, the entire note is disregarded.
Notes that contain an illegible signature are equally problematic. If the legibility of the signature prevents the reviewer from correctly identifying the rendering provider, the service may be denied.
CMS has instructed Medicare contractors to request a signed provider attestation before issuing a denial.5 The provider should print his/her name beside the signature or include a separate signature sheet with the requested documentation to assist the reviewer in provider identification. Stamped signatures are not acceptable under any circumstance. Medicare accepts only handwritten or electronic signatures.5
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- HealthIT.gov. Benefits of electronic health records (EHRs). Accessed August 1, 2015.
- Social Security Administration. Exclusions from coverage and Medicare as secondary payer. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15—Covered medical and other health services. Chapter 15, Section 30.E. Concurrent care. Accessed August 1, 2015.
- Department of Health and Human Services. Office of Inspector General. CMS and its contractors have adopted few program integrity practices to address vulnerabilities in EHRs. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. Signature guidelines for medical review purposes. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. 1995 documentation guidelines for evaluation and management services. Accessed August 1, 2015.
The electronic health record (EHR) has many benefits:
- Improved patient care;
- Improved care coordination;
- Improved diagnostics and patient outcomes;
- Increased patient participation; and
- Increased practice efficiencies and cost savings.1
EHRs also introduce risks, however. Heightened concern about EHR misuse and vulnerability elevates the level of scrutiny placed on provider documentation as it relates to billing and coding. Without clear guidelines from the Centers for Medicare and Medicaid Services (CMS) or other payers, the potential for unintentional misapplication exists. Auditor misinterpretation is also possible. Providers should utilize simple defensive documentation principles to support their services and minimize their risks.
Reason for Encounter
Under section 1862 (a)(1)(A) of the Social Security Act, the Medicare Program may only pay for items and services that are “reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member,” unless there is another statutory authorization for payment (e.g. colorectal cancer screening).2
A payer can determine if a service is “reasonable and necessary” based on the service indication. The reason for the patient encounter, otherwise known as the chief complaint, must be evident. This can be a symptom, problem, condition, diagnosis, physician-recommended return, or another factor that necessitates the encounter.1 It cannot be inferred and must be clearly stated in the documentation. Without it, a payer may question the medical necessity of the service, especially if it involves hospital-based services in the course of which multiple specialists will see the patient on any given date. Payers are likely to deny services that cannot be easily differentiated (e.g. “no c/o”). Furthermore, payers can deny concurrent care services for the following reasons:3
- Services exceed normal frequency or duration for a given condition without documented circumstances requiring additional care; or
- Services by one physician duplicate/overlap those of the other provider without any recognizable distinction.
Providers should be specific in identifying the encounter reason, as in the following examples: “Patient seen for shortness of breath” or “Patient with COPD, feeling improved with 3L O2 NC.”
Assessment and Plan
Accurately representing patient complexity for every visit throughout the hospitalization presents its challenges. Although the problem list may not dramatically change day to day, providers must formulate an assessment of the patient’s condition with a corresponding plan of care for each encounter. Documenting problems without a corresponding plan of care does not substantiate physician participation in the management of that problem. Providing a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) minimizes the complexity and effort put forth in the encounter and could result in auditor downgrading upon documentation review.
Developing shortcuts might falsely minimize the provider’s documentation burden. An electronic documentation system might make it possible to copy previous progress notes into the current encounter to save time; however, the previously entered information could include elements that do not require reassessment during a subsequent encounter or contain information about conditions that are being managed concurrently by another specialist (e.g. CKD being managed by the nephrologist). Leaving the copied information unmodified may not accurately reflect the patient’s current condition or the care provided by the hospitalist during the current encounter. Information that is pulled forward or copied and pasted from a previous entry should be modified to demonstrate updated content and nonoverlapping care relevant to that date.
According to the Office of Inspector General (OIG), “inappropriate copy-pasting could facilitate attempts to inflate claims and duplicate or create fraudulent claims.”4
An equally problematic EHR function involves “overdocumentation,” the practice of inserting false or irrelevant documentation to create the appearance of support for billing higher level services.4 EHR technology has the ability to auto-populate fields using templates built into the system or generate extensive documentation on the basis of a single click. The OIG cautions providers to use these features carefully, because they can produce information suggesting the practitioner performed more comprehensive services than were actually rendered.4
An example is the inclusion of the same lab results more than once. Although clinicians include this information as a reference to avoid having to “find it somewhere in the chart” when it is needed—as a basis for comparison, for example—auditors mistake this as an attempt to gain credit for the daily review of the same “old” information. Including only relevant data will mitigate this concern.
Authorship
Dates and signatures are essential to each encounter. Medicare requires services provided/ordered to be authenticated by the author.5 A reviewer must be able to identify each individual who performs, documents, and bills for a service on a given date. Progress notes that fail to identify the service date or service provider will likely result in denial.
Additionally, a service is questioned when two different sets of handwriting appear on a note, yet only one signature is provided. Since the reviewer cannot confirm the credentials of the unidentified individual and cannot be sure which portion belongs to the identified individual, the entire note is disregarded.
Notes that contain an illegible signature are equally problematic. If the legibility of the signature prevents the reviewer from correctly identifying the rendering provider, the service may be denied.
CMS has instructed Medicare contractors to request a signed provider attestation before issuing a denial.5 The provider should print his/her name beside the signature or include a separate signature sheet with the requested documentation to assist the reviewer in provider identification. Stamped signatures are not acceptable under any circumstance. Medicare accepts only handwritten or electronic signatures.5
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- HealthIT.gov. Benefits of electronic health records (EHRs). Accessed August 1, 2015.
- Social Security Administration. Exclusions from coverage and Medicare as secondary payer. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15—Covered medical and other health services. Chapter 15, Section 30.E. Concurrent care. Accessed August 1, 2015.
- Department of Health and Human Services. Office of Inspector General. CMS and its contractors have adopted few program integrity practices to address vulnerabilities in EHRs. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. Signature guidelines for medical review purposes. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. 1995 documentation guidelines for evaluation and management services. Accessed August 1, 2015.
The electronic health record (EHR) has many benefits:
- Improved patient care;
- Improved care coordination;
- Improved diagnostics and patient outcomes;
- Increased patient participation; and
- Increased practice efficiencies and cost savings.1
EHRs also introduce risks, however. Heightened concern about EHR misuse and vulnerability elevates the level of scrutiny placed on provider documentation as it relates to billing and coding. Without clear guidelines from the Centers for Medicare and Medicaid Services (CMS) or other payers, the potential for unintentional misapplication exists. Auditor misinterpretation is also possible. Providers should utilize simple defensive documentation principles to support their services and minimize their risks.
Reason for Encounter
Under section 1862 (a)(1)(A) of the Social Security Act, the Medicare Program may only pay for items and services that are “reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member,” unless there is another statutory authorization for payment (e.g. colorectal cancer screening).2
A payer can determine if a service is “reasonable and necessary” based on the service indication. The reason for the patient encounter, otherwise known as the chief complaint, must be evident. This can be a symptom, problem, condition, diagnosis, physician-recommended return, or another factor that necessitates the encounter.1 It cannot be inferred and must be clearly stated in the documentation. Without it, a payer may question the medical necessity of the service, especially if it involves hospital-based services in the course of which multiple specialists will see the patient on any given date. Payers are likely to deny services that cannot be easily differentiated (e.g. “no c/o”). Furthermore, payers can deny concurrent care services for the following reasons:3
- Services exceed normal frequency or duration for a given condition without documented circumstances requiring additional care; or
- Services by one physician duplicate/overlap those of the other provider without any recognizable distinction.
Providers should be specific in identifying the encounter reason, as in the following examples: “Patient seen for shortness of breath” or “Patient with COPD, feeling improved with 3L O2 NC.”
Assessment and Plan
Accurately representing patient complexity for every visit throughout the hospitalization presents its challenges. Although the problem list may not dramatically change day to day, providers must formulate an assessment of the patient’s condition with a corresponding plan of care for each encounter. Documenting problems without a corresponding plan of care does not substantiate physician participation in the management of that problem. Providing a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) minimizes the complexity and effort put forth in the encounter and could result in auditor downgrading upon documentation review.
Developing shortcuts might falsely minimize the provider’s documentation burden. An electronic documentation system might make it possible to copy previous progress notes into the current encounter to save time; however, the previously entered information could include elements that do not require reassessment during a subsequent encounter or contain information about conditions that are being managed concurrently by another specialist (e.g. CKD being managed by the nephrologist). Leaving the copied information unmodified may not accurately reflect the patient’s current condition or the care provided by the hospitalist during the current encounter. Information that is pulled forward or copied and pasted from a previous entry should be modified to demonstrate updated content and nonoverlapping care relevant to that date.
According to the Office of Inspector General (OIG), “inappropriate copy-pasting could facilitate attempts to inflate claims and duplicate or create fraudulent claims.”4
An equally problematic EHR function involves “overdocumentation,” the practice of inserting false or irrelevant documentation to create the appearance of support for billing higher level services.4 EHR technology has the ability to auto-populate fields using templates built into the system or generate extensive documentation on the basis of a single click. The OIG cautions providers to use these features carefully, because they can produce information suggesting the practitioner performed more comprehensive services than were actually rendered.4
An example is the inclusion of the same lab results more than once. Although clinicians include this information as a reference to avoid having to “find it somewhere in the chart” when it is needed—as a basis for comparison, for example—auditors mistake this as an attempt to gain credit for the daily review of the same “old” information. Including only relevant data will mitigate this concern.
Authorship
Dates and signatures are essential to each encounter. Medicare requires services provided/ordered to be authenticated by the author.5 A reviewer must be able to identify each individual who performs, documents, and bills for a service on a given date. Progress notes that fail to identify the service date or service provider will likely result in denial.
Additionally, a service is questioned when two different sets of handwriting appear on a note, yet only one signature is provided. Since the reviewer cannot confirm the credentials of the unidentified individual and cannot be sure which portion belongs to the identified individual, the entire note is disregarded.
Notes that contain an illegible signature are equally problematic. If the legibility of the signature prevents the reviewer from correctly identifying the rendering provider, the service may be denied.
CMS has instructed Medicare contractors to request a signed provider attestation before issuing a denial.5 The provider should print his/her name beside the signature or include a separate signature sheet with the requested documentation to assist the reviewer in provider identification. Stamped signatures are not acceptable under any circumstance. Medicare accepts only handwritten or electronic signatures.5
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- HealthIT.gov. Benefits of electronic health records (EHRs). Accessed August 1, 2015.
- Social Security Administration. Exclusions from coverage and Medicare as secondary payer. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15—Covered medical and other health services. Chapter 15, Section 30.E. Concurrent care. Accessed August 1, 2015.
- Department of Health and Human Services. Office of Inspector General. CMS and its contractors have adopted few program integrity practices to address vulnerabilities in EHRs. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. Signature guidelines for medical review purposes. Accessed August 1, 2015.
- Centers for Medicare and Medicaid Services. 1995 documentation guidelines for evaluation and management services. Accessed August 1, 2015.
ICD-10 Medical Coding System Likely to Improve Documentation, Reimbursement
ICD-10 is the system that will replace ICD-9 for all parties covered by the Health Insurance Portability and Accountability Act (HIPAA). ICD-10 contains a code set used for inpatient procedural reporting and a code set used for diagnosis reporting. Physicians billing for professional services will only be affected when reporting diagnoses codes on their claims, but both physician and hospital selection of ICD-10 codes relies heavily on physician documentation. Therefore, documentation must be scrutinized. The most widely noted impact ICD-10 will have on documentation is increased specificity, with enhanced reporting of the patient’s presenting problem(s). Expanding from a pool of 14,000 3/5-digit codes to 69,000 7-digit codes, and accommodating this change, are daunting tasks. These anticipated burdens make it hard for physicians to recognize the positive effects ICD-10 may create, such as:1
- Better clinical decisions as better data is documented, collected, and evaluated;
- Improved protocol and clinical pathway design for various health conditions;
- Improved public health reporting and tracking of illnesses and severity over time;
- Better definition of patient conditions, providing improved matching of professional resources and care teams and increasing communications between providers;
- Support in practice transition to risk-sharing models with more precise data for patients and populations;
- Provision of clear objective data for credentialing and privileges, and support for professional Maintenance of Certification reporting across specialties;
- Better documentation of patient complexity and level of care, supporting reimbursement and measures for quality and efficiency reporting; and
- Reduction in audit risk exposure by encouraging the use of diagnosis codes with a greater degree of specificity as supported by the clinical documentation.
With the Oct. 1 implementation date rapidly approaching, physicians need to ask themselves, “Am I prepared?”
Getting Started
Everyone has a role and responsibility in transitioning to ICD-10. Active participation by all involved parties guarantees a more successful outcome. Practice administration must ensure that each aspect of implementation is reviewed and appropriately addressed. If not already done, immediate steps should be taken to verify the products and services that affect implementation. These include:
- Payer mix and related contracts: Entities not covered by HIPAA (e.g. workers’ compensation and auto insurance companies) may choose not to implement ICD-10. Since ICD-9 will no longer be maintained post-ICD-10 implementation, it is in the best interest of non-covered entities to use the new coding system.2 For payers who are required to transition to ICD-10, it is important to identify whether patient eligibility, claim processing, and/or payment timelines will be affected, as well as fee schedules or capitated rates.
- Vendor readiness: Physician groups may use a variety of vendors to assist with different aspects of the revenue cycle, including an electronic health record (e.g. documenting services and transmitting physician orders/prescriptions); a practice management system (e.g. scheduling and registering patients); a billing service (e.g. processing patient claims and payments); and a clearinghouse (e.g. verifying patient eligibility and obtaining authorizations). Know when software and/or hardware upgrades are available and if there are additional upgrade fees. Identify vendors that provide support services, training, and tools or templates to ease the transition. Most importantly, inquire about a testing period for products and applications to ensure functionality and adequate feedback on use of the system(s).
- Internal coding and billing resources. Identify physicians and staff who use ICD-9 codes and need to know ICD-10 codes in order to fulfill their responsibilities. Both physicians and staff can assist in identifying common clinical scenarios and the most frequently used ICD-9 codes, in order to develop a list of common ICD-10 specialty codes. Payer coverage policies currently include ICD-10 codes for provider review and comparison. Revise current forms/templates that include diagnosis codes to reflect this updated information. Schedule ICD-10 training for clinicians, office managers, billers, coders, and other key staff. Coding professionals recommend that training take place approximately six months prior to the ICD-10 compliance deadline.3 Training sessions are available from consultants, professional societies, payers, and other entities. Cost varies depending upon the type and length of training. CMS provides some free services, but in-depth training or certification for at least one practice member should be considered.
Once training is completed, dual coding is an option. Dual coding is the process by which both ICD-9 codes and ICD-10 codes are selected during the coding process. Some practices rely on independent selection of each code, while others rely on the General Equivalence Mappings (GEMs). GEMs were developed to assist industry migration to ICD-10. They are intended to be used primarily for translations of code lists or code tables used by an application or other coded data when codes in one code set are the only source of information; they are not intended as a substitution for direct use of ICD-9-CM and ICD-10-CM/PCS.4 Manual coding enhances coding efficiency and also identifies physician documentation deficiencies. Dual coding should begin as soon as possible, prior to October 1.
End-to-end testing is an opportunity to submit test claims to CMS with ICD-10 codes; providers will receive a remittance advice that explains the adjudication of the claims.5 This testing is limited to a small group of providers who were required to register in April, and its final week is July 20-24.
Provide Feedback
The importance of feedback is often understated. Many physician practices do not have the time to plan ahead and, as a result, find themselves in a reactive rather than proactive role. Over the next couple of months, find the time and resources to audit physician documentation based on ICD-10 criteria. Ask yourself whether or not the information contains enough specificity to select the best possible code, or does code selection default to an “unspecified” code?
Avoid “unspecified” codes when possible in preparation for payer policy revisions that are aimed at reducing or eliminating these types of codes. If the documentation lacks detail, educate physicians on the missing elements.
Review ICD-10 code sets with physicians to improve their understanding of the new system. For example, diabetes mellitus is identified in ICD-9 as one category (250.xx), with digits to specify Type I or Type II, controlled vs. uncontrolled, with or without complications. ICD-10 separates diabetes into categories of Type I (E10) or Type II (E11), with subcategories to identify complications and affected body systems, thereby expanding the volume of codes and corresponding documentation criteria.6
Post-implementation feedback will become even more important. Monitor claim denials for invalid codes and medical necessity issues (i.e., valid codes not included for coverage). If the medical necessity denials are a result of inaccurate code selection related to insufficient documentation details, provider education will be crucial in resolving these errors. Continuing education to strengthen and update staff skills is imperative.
CMS has developed many tools and resources to promote a successful transition and assess your ICD-10 preparedness. Physician practices can develop an “action plan,” learn basic ICD-10 concepts, and much more.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Road to 10: the small physician practice’s route to ICD-10? Accessed June 6, 2015.
- Department of Health and Human Services. Centers for Medicare and Medicaid Services. Medicare Learning Network: ICD-10-CM/PCS Myths and Facts. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10: ICD-10 Basics for Medical Practices. Accessed June 6, 2015.
- American Health Information Management Association (AHIMA). Putting the ICD-10-CM/PCS GEMs into practice. Accessed June 6, 2015.
- Novitas Solutions. Medicare JL, Part B. ICD-10 Implementation. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10 Coding and Diabetes. Accessed June 6, 2015.
ICD-10 is the system that will replace ICD-9 for all parties covered by the Health Insurance Portability and Accountability Act (HIPAA). ICD-10 contains a code set used for inpatient procedural reporting and a code set used for diagnosis reporting. Physicians billing for professional services will only be affected when reporting diagnoses codes on their claims, but both physician and hospital selection of ICD-10 codes relies heavily on physician documentation. Therefore, documentation must be scrutinized. The most widely noted impact ICD-10 will have on documentation is increased specificity, with enhanced reporting of the patient’s presenting problem(s). Expanding from a pool of 14,000 3/5-digit codes to 69,000 7-digit codes, and accommodating this change, are daunting tasks. These anticipated burdens make it hard for physicians to recognize the positive effects ICD-10 may create, such as:1
- Better clinical decisions as better data is documented, collected, and evaluated;
- Improved protocol and clinical pathway design for various health conditions;
- Improved public health reporting and tracking of illnesses and severity over time;
- Better definition of patient conditions, providing improved matching of professional resources and care teams and increasing communications between providers;
- Support in practice transition to risk-sharing models with more precise data for patients and populations;
- Provision of clear objective data for credentialing and privileges, and support for professional Maintenance of Certification reporting across specialties;
- Better documentation of patient complexity and level of care, supporting reimbursement and measures for quality and efficiency reporting; and
- Reduction in audit risk exposure by encouraging the use of diagnosis codes with a greater degree of specificity as supported by the clinical documentation.
With the Oct. 1 implementation date rapidly approaching, physicians need to ask themselves, “Am I prepared?”
Getting Started
Everyone has a role and responsibility in transitioning to ICD-10. Active participation by all involved parties guarantees a more successful outcome. Practice administration must ensure that each aspect of implementation is reviewed and appropriately addressed. If not already done, immediate steps should be taken to verify the products and services that affect implementation. These include:
- Payer mix and related contracts: Entities not covered by HIPAA (e.g. workers’ compensation and auto insurance companies) may choose not to implement ICD-10. Since ICD-9 will no longer be maintained post-ICD-10 implementation, it is in the best interest of non-covered entities to use the new coding system.2 For payers who are required to transition to ICD-10, it is important to identify whether patient eligibility, claim processing, and/or payment timelines will be affected, as well as fee schedules or capitated rates.
- Vendor readiness: Physician groups may use a variety of vendors to assist with different aspects of the revenue cycle, including an electronic health record (e.g. documenting services and transmitting physician orders/prescriptions); a practice management system (e.g. scheduling and registering patients); a billing service (e.g. processing patient claims and payments); and a clearinghouse (e.g. verifying patient eligibility and obtaining authorizations). Know when software and/or hardware upgrades are available and if there are additional upgrade fees. Identify vendors that provide support services, training, and tools or templates to ease the transition. Most importantly, inquire about a testing period for products and applications to ensure functionality and adequate feedback on use of the system(s).
- Internal coding and billing resources. Identify physicians and staff who use ICD-9 codes and need to know ICD-10 codes in order to fulfill their responsibilities. Both physicians and staff can assist in identifying common clinical scenarios and the most frequently used ICD-9 codes, in order to develop a list of common ICD-10 specialty codes. Payer coverage policies currently include ICD-10 codes for provider review and comparison. Revise current forms/templates that include diagnosis codes to reflect this updated information. Schedule ICD-10 training for clinicians, office managers, billers, coders, and other key staff. Coding professionals recommend that training take place approximately six months prior to the ICD-10 compliance deadline.3 Training sessions are available from consultants, professional societies, payers, and other entities. Cost varies depending upon the type and length of training. CMS provides some free services, but in-depth training or certification for at least one practice member should be considered.
Once training is completed, dual coding is an option. Dual coding is the process by which both ICD-9 codes and ICD-10 codes are selected during the coding process. Some practices rely on independent selection of each code, while others rely on the General Equivalence Mappings (GEMs). GEMs were developed to assist industry migration to ICD-10. They are intended to be used primarily for translations of code lists or code tables used by an application or other coded data when codes in one code set are the only source of information; they are not intended as a substitution for direct use of ICD-9-CM and ICD-10-CM/PCS.4 Manual coding enhances coding efficiency and also identifies physician documentation deficiencies. Dual coding should begin as soon as possible, prior to October 1.
End-to-end testing is an opportunity to submit test claims to CMS with ICD-10 codes; providers will receive a remittance advice that explains the adjudication of the claims.5 This testing is limited to a small group of providers who were required to register in April, and its final week is July 20-24.
Provide Feedback
The importance of feedback is often understated. Many physician practices do not have the time to plan ahead and, as a result, find themselves in a reactive rather than proactive role. Over the next couple of months, find the time and resources to audit physician documentation based on ICD-10 criteria. Ask yourself whether or not the information contains enough specificity to select the best possible code, or does code selection default to an “unspecified” code?
Avoid “unspecified” codes when possible in preparation for payer policy revisions that are aimed at reducing or eliminating these types of codes. If the documentation lacks detail, educate physicians on the missing elements.
Review ICD-10 code sets with physicians to improve their understanding of the new system. For example, diabetes mellitus is identified in ICD-9 as one category (250.xx), with digits to specify Type I or Type II, controlled vs. uncontrolled, with or without complications. ICD-10 separates diabetes into categories of Type I (E10) or Type II (E11), with subcategories to identify complications and affected body systems, thereby expanding the volume of codes and corresponding documentation criteria.6
Post-implementation feedback will become even more important. Monitor claim denials for invalid codes and medical necessity issues (i.e., valid codes not included for coverage). If the medical necessity denials are a result of inaccurate code selection related to insufficient documentation details, provider education will be crucial in resolving these errors. Continuing education to strengthen and update staff skills is imperative.
CMS has developed many tools and resources to promote a successful transition and assess your ICD-10 preparedness. Physician practices can develop an “action plan,” learn basic ICD-10 concepts, and much more.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Road to 10: the small physician practice’s route to ICD-10? Accessed June 6, 2015.
- Department of Health and Human Services. Centers for Medicare and Medicaid Services. Medicare Learning Network: ICD-10-CM/PCS Myths and Facts. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10: ICD-10 Basics for Medical Practices. Accessed June 6, 2015.
- American Health Information Management Association (AHIMA). Putting the ICD-10-CM/PCS GEMs into practice. Accessed June 6, 2015.
- Novitas Solutions. Medicare JL, Part B. ICD-10 Implementation. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10 Coding and Diabetes. Accessed June 6, 2015.
ICD-10 is the system that will replace ICD-9 for all parties covered by the Health Insurance Portability and Accountability Act (HIPAA). ICD-10 contains a code set used for inpatient procedural reporting and a code set used for diagnosis reporting. Physicians billing for professional services will only be affected when reporting diagnoses codes on their claims, but both physician and hospital selection of ICD-10 codes relies heavily on physician documentation. Therefore, documentation must be scrutinized. The most widely noted impact ICD-10 will have on documentation is increased specificity, with enhanced reporting of the patient’s presenting problem(s). Expanding from a pool of 14,000 3/5-digit codes to 69,000 7-digit codes, and accommodating this change, are daunting tasks. These anticipated burdens make it hard for physicians to recognize the positive effects ICD-10 may create, such as:1
- Better clinical decisions as better data is documented, collected, and evaluated;
- Improved protocol and clinical pathway design for various health conditions;
- Improved public health reporting and tracking of illnesses and severity over time;
- Better definition of patient conditions, providing improved matching of professional resources and care teams and increasing communications between providers;
- Support in practice transition to risk-sharing models with more precise data for patients and populations;
- Provision of clear objective data for credentialing and privileges, and support for professional Maintenance of Certification reporting across specialties;
- Better documentation of patient complexity and level of care, supporting reimbursement and measures for quality and efficiency reporting; and
- Reduction in audit risk exposure by encouraging the use of diagnosis codes with a greater degree of specificity as supported by the clinical documentation.
With the Oct. 1 implementation date rapidly approaching, physicians need to ask themselves, “Am I prepared?”
Getting Started
Everyone has a role and responsibility in transitioning to ICD-10. Active participation by all involved parties guarantees a more successful outcome. Practice administration must ensure that each aspect of implementation is reviewed and appropriately addressed. If not already done, immediate steps should be taken to verify the products and services that affect implementation. These include:
- Payer mix and related contracts: Entities not covered by HIPAA (e.g. workers’ compensation and auto insurance companies) may choose not to implement ICD-10. Since ICD-9 will no longer be maintained post-ICD-10 implementation, it is in the best interest of non-covered entities to use the new coding system.2 For payers who are required to transition to ICD-10, it is important to identify whether patient eligibility, claim processing, and/or payment timelines will be affected, as well as fee schedules or capitated rates.
- Vendor readiness: Physician groups may use a variety of vendors to assist with different aspects of the revenue cycle, including an electronic health record (e.g. documenting services and transmitting physician orders/prescriptions); a practice management system (e.g. scheduling and registering patients); a billing service (e.g. processing patient claims and payments); and a clearinghouse (e.g. verifying patient eligibility and obtaining authorizations). Know when software and/or hardware upgrades are available and if there are additional upgrade fees. Identify vendors that provide support services, training, and tools or templates to ease the transition. Most importantly, inquire about a testing period for products and applications to ensure functionality and adequate feedback on use of the system(s).
- Internal coding and billing resources. Identify physicians and staff who use ICD-9 codes and need to know ICD-10 codes in order to fulfill their responsibilities. Both physicians and staff can assist in identifying common clinical scenarios and the most frequently used ICD-9 codes, in order to develop a list of common ICD-10 specialty codes. Payer coverage policies currently include ICD-10 codes for provider review and comparison. Revise current forms/templates that include diagnosis codes to reflect this updated information. Schedule ICD-10 training for clinicians, office managers, billers, coders, and other key staff. Coding professionals recommend that training take place approximately six months prior to the ICD-10 compliance deadline.3 Training sessions are available from consultants, professional societies, payers, and other entities. Cost varies depending upon the type and length of training. CMS provides some free services, but in-depth training or certification for at least one practice member should be considered.
Once training is completed, dual coding is an option. Dual coding is the process by which both ICD-9 codes and ICD-10 codes are selected during the coding process. Some practices rely on independent selection of each code, while others rely on the General Equivalence Mappings (GEMs). GEMs were developed to assist industry migration to ICD-10. They are intended to be used primarily for translations of code lists or code tables used by an application or other coded data when codes in one code set are the only source of information; they are not intended as a substitution for direct use of ICD-9-CM and ICD-10-CM/PCS.4 Manual coding enhances coding efficiency and also identifies physician documentation deficiencies. Dual coding should begin as soon as possible, prior to October 1.
End-to-end testing is an opportunity to submit test claims to CMS with ICD-10 codes; providers will receive a remittance advice that explains the adjudication of the claims.5 This testing is limited to a small group of providers who were required to register in April, and its final week is July 20-24.
Provide Feedback
The importance of feedback is often understated. Many physician practices do not have the time to plan ahead and, as a result, find themselves in a reactive rather than proactive role. Over the next couple of months, find the time and resources to audit physician documentation based on ICD-10 criteria. Ask yourself whether or not the information contains enough specificity to select the best possible code, or does code selection default to an “unspecified” code?
Avoid “unspecified” codes when possible in preparation for payer policy revisions that are aimed at reducing or eliminating these types of codes. If the documentation lacks detail, educate physicians on the missing elements.
Review ICD-10 code sets with physicians to improve their understanding of the new system. For example, diabetes mellitus is identified in ICD-9 as one category (250.xx), with digits to specify Type I or Type II, controlled vs. uncontrolled, with or without complications. ICD-10 separates diabetes into categories of Type I (E10) or Type II (E11), with subcategories to identify complications and affected body systems, thereby expanding the volume of codes and corresponding documentation criteria.6
Post-implementation feedback will become even more important. Monitor claim denials for invalid codes and medical necessity issues (i.e., valid codes not included for coverage). If the medical necessity denials are a result of inaccurate code selection related to insufficient documentation details, provider education will be crucial in resolving these errors. Continuing education to strengthen and update staff skills is imperative.
CMS has developed many tools and resources to promote a successful transition and assess your ICD-10 preparedness. Physician practices can develop an “action plan,” learn basic ICD-10 concepts, and much more.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Road to 10: the small physician practice’s route to ICD-10? Accessed June 6, 2015.
- Department of Health and Human Services. Centers for Medicare and Medicaid Services. Medicare Learning Network: ICD-10-CM/PCS Myths and Facts. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10: ICD-10 Basics for Medical Practices. Accessed June 6, 2015.
- American Health Information Management Association (AHIMA). Putting the ICD-10-CM/PCS GEMs into practice. Accessed June 6, 2015.
- Novitas Solutions. Medicare JL, Part B. ICD-10 Implementation. Accessed June 6, 2015.
- Centers for Medicare and Medicaid Services. ICD-10 Coding and Diabetes. Accessed June 6, 2015.
Medicare Standard Practical Solution to Medical Coding Complexity
In the article “Common Coding Mistakes Hospitalists Should Avoid” in the August 2014 issue of The Hospitalist, the author states:
“For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization.”
This definition contradicts what I have been told in other coding courses regarding new vs. established problems relative to the examiner. It has been my understanding that when [I am] rotating on service and I have not seen that particular patient during the current admission, all of the current problems are new to me, even if previously identified by another member of my group. This [situation] results in a higher complexity of medical decision-making, which is reflective of the increased time spent learning a new patient when coming on service. I would appreciate clarification from the author.
–Matt George, MD,
medical director, MBHS Hospitalists
Billing and coding expert Carol Pohlig, BSN, RN, CPC, ACS, explains:
Be mindful when attending coding courses that are not contractor sponsored, as they may not validate the geographical interpretations of the rules for providers. There are several factors to consider when crediting the physician with “new” or “established” problems.
CMS documentation guidelines state: “Decision making with respect to a diagnosed problem is easier than that for an identified but undiagnosed problem.1
- For a presenting problem with an established diagnosis, the record should reflect whether the problem is:
- Improved, well-controlled, resolving, or resolved or
- Inadequately controlled, worsening, or failing to change as expected.
- For a presenting problem without an established diagnosis, the assessment or clinical impression may be stated in the form of differential diagnoses or as a “possible,” “probable,” or “rule out” diagnosis.
Although Medicare contractors utilize the Marshfield Clinic Scoring Tool when reviewing evaluation and management (E/M) services, a tool that historically refers to the “examiner” when considering the patient’s diagnoses, not all accept this tool-inspired standard, particularly in the advent of electronic health record accessibility and the idea that same-specialty physicians in a group practice are viewed as an individual physician.2,3
Reviewing information and familiarization of patients is often considered pre-service work and factored into the payment for E/M services. More importantly, the feasibility of an auditor being able to distinguish new vs. established problems at the level of the “examiner” is decreased when auditing a single date of service. Non-Medicare payers who audit E/M services do not necessarily follow contractor-specific guidelines but, rather, general CMS guidelines.
Therefore, without knowing the insurer or their interpretation at the time of service or visit level selection, the CMS-developed standard is the most practical application when considering the complexity of the encounter.
References
- Centers for Medicare and Medicaid Services. Department of Health and Human Services. Evaluation and management services guide. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads//eval_mgmt_serv_guide-ICN006764.pdf. Accessed November 13, 2014.
- National Government Services. Evaluation and management documentation training too. Available at: http://www.ngsmedicare.com/ngs/wcm/connect/3632a905-b697-4266-8fc0-2aa2a84fedb2/1074_0514_EM_Documentation_Training_Tool_508.pdf?MOD=AJPERES. Accessed November 13, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual. Chapter 12 – Physicians/nonphysician practitioners. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed November 13, 2014.
In the article “Common Coding Mistakes Hospitalists Should Avoid” in the August 2014 issue of The Hospitalist, the author states:
“For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization.”
This definition contradicts what I have been told in other coding courses regarding new vs. established problems relative to the examiner. It has been my understanding that when [I am] rotating on service and I have not seen that particular patient during the current admission, all of the current problems are new to me, even if previously identified by another member of my group. This [situation] results in a higher complexity of medical decision-making, which is reflective of the increased time spent learning a new patient when coming on service. I would appreciate clarification from the author.
–Matt George, MD,
medical director, MBHS Hospitalists
Billing and coding expert Carol Pohlig, BSN, RN, CPC, ACS, explains:
Be mindful when attending coding courses that are not contractor sponsored, as they may not validate the geographical interpretations of the rules for providers. There are several factors to consider when crediting the physician with “new” or “established” problems.
CMS documentation guidelines state: “Decision making with respect to a diagnosed problem is easier than that for an identified but undiagnosed problem.1
- For a presenting problem with an established diagnosis, the record should reflect whether the problem is:
- Improved, well-controlled, resolving, or resolved or
- Inadequately controlled, worsening, or failing to change as expected.
- For a presenting problem without an established diagnosis, the assessment or clinical impression may be stated in the form of differential diagnoses or as a “possible,” “probable,” or “rule out” diagnosis.
Although Medicare contractors utilize the Marshfield Clinic Scoring Tool when reviewing evaluation and management (E/M) services, a tool that historically refers to the “examiner” when considering the patient’s diagnoses, not all accept this tool-inspired standard, particularly in the advent of electronic health record accessibility and the idea that same-specialty physicians in a group practice are viewed as an individual physician.2,3
Reviewing information and familiarization of patients is often considered pre-service work and factored into the payment for E/M services. More importantly, the feasibility of an auditor being able to distinguish new vs. established problems at the level of the “examiner” is decreased when auditing a single date of service. Non-Medicare payers who audit E/M services do not necessarily follow contractor-specific guidelines but, rather, general CMS guidelines.
Therefore, without knowing the insurer or their interpretation at the time of service or visit level selection, the CMS-developed standard is the most practical application when considering the complexity of the encounter.
References
- Centers for Medicare and Medicaid Services. Department of Health and Human Services. Evaluation and management services guide. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads//eval_mgmt_serv_guide-ICN006764.pdf. Accessed November 13, 2014.
- National Government Services. Evaluation and management documentation training too. Available at: http://www.ngsmedicare.com/ngs/wcm/connect/3632a905-b697-4266-8fc0-2aa2a84fedb2/1074_0514_EM_Documentation_Training_Tool_508.pdf?MOD=AJPERES. Accessed November 13, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual. Chapter 12 – Physicians/nonphysician practitioners. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed November 13, 2014.
In the article “Common Coding Mistakes Hospitalists Should Avoid” in the August 2014 issue of The Hospitalist, the author states:
“For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization.”
This definition contradicts what I have been told in other coding courses regarding new vs. established problems relative to the examiner. It has been my understanding that when [I am] rotating on service and I have not seen that particular patient during the current admission, all of the current problems are new to me, even if previously identified by another member of my group. This [situation] results in a higher complexity of medical decision-making, which is reflective of the increased time spent learning a new patient when coming on service. I would appreciate clarification from the author.
–Matt George, MD,
medical director, MBHS Hospitalists
Billing and coding expert Carol Pohlig, BSN, RN, CPC, ACS, explains:
Be mindful when attending coding courses that are not contractor sponsored, as they may not validate the geographical interpretations of the rules for providers. There are several factors to consider when crediting the physician with “new” or “established” problems.
CMS documentation guidelines state: “Decision making with respect to a diagnosed problem is easier than that for an identified but undiagnosed problem.1
- For a presenting problem with an established diagnosis, the record should reflect whether the problem is:
- Improved, well-controlled, resolving, or resolved or
- Inadequately controlled, worsening, or failing to change as expected.
- For a presenting problem without an established diagnosis, the assessment or clinical impression may be stated in the form of differential diagnoses or as a “possible,” “probable,” or “rule out” diagnosis.
Although Medicare contractors utilize the Marshfield Clinic Scoring Tool when reviewing evaluation and management (E/M) services, a tool that historically refers to the “examiner” when considering the patient’s diagnoses, not all accept this tool-inspired standard, particularly in the advent of electronic health record accessibility and the idea that same-specialty physicians in a group practice are viewed as an individual physician.2,3
Reviewing information and familiarization of patients is often considered pre-service work and factored into the payment for E/M services. More importantly, the feasibility of an auditor being able to distinguish new vs. established problems at the level of the “examiner” is decreased when auditing a single date of service. Non-Medicare payers who audit E/M services do not necessarily follow contractor-specific guidelines but, rather, general CMS guidelines.
Therefore, without knowing the insurer or their interpretation at the time of service or visit level selection, the CMS-developed standard is the most practical application when considering the complexity of the encounter.
References
- Centers for Medicare and Medicaid Services. Department of Health and Human Services. Evaluation and management services guide. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads//eval_mgmt_serv_guide-ICN006764.pdf. Accessed November 13, 2014.
- National Government Services. Evaluation and management documentation training too. Available at: http://www.ngsmedicare.com/ngs/wcm/connect/3632a905-b697-4266-8fc0-2aa2a84fedb2/1074_0514_EM_Documentation_Training_Tool_508.pdf?MOD=AJPERES. Accessed November 13, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual. Chapter 12 – Physicians/nonphysician practitioners. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed November 13, 2014.
Service Distinction Crucial for Medical Claim Submissions
Hospitalists often are tasked with coordinating and overseeing patient care throughout a hospitalization. Depending on the care model and the availability of varying specialists, a patient could see several specialists throughout the stay, and even during a single day. A recurring issue for many hospitalists is justifying the medical necessity of their services, because payers do not want to reimburse overlapping care (i.e., multiple providers caring for the same patient problem) when more than one physician provides care on the same service date.
Payers often consider two key principles before reimbursing multiple visits on the same date:1
- Does the patient’s condition warrant the services of more than one physician?
- Are the individual services provided by each physician reasonable and necessary?
Consider the following example: A 65-year-old female patient is admitted with a hip fracture (820.8) after slipping on the ice outside her home. The patient also has hypertension (401.1) and type II diabetes (250.00). The surgeon manages the patient’s peri-operative course for the fracture, while the hospitalist manages the patient’s medical issues.
Payers must be sure that the services of one physician do not duplicate those provided by another.1 For the above scenario, it is imperative that the hospitalist understand which services are considered the surgeon’s responsibility. The global surgical package includes payment for the surgical procedure and the completion of its corresponding facility-required paperwork (e.g. pre-operative history and physical exam, operative consent forms, pre-operative orders), in addition to the following services:2
- Pre-operative visits after making the decision for surgery beginning one day prior to surgery;
- All additional post-operative medical or surgical services provided by the surgeon related to complications but not requiring additional trips to the operating room;
- Post-operative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes, local incisional care, removal of cutaneous sutures and staples, line removals, changes and removal of tracheostomy tubes, and discharge services; and
- Post-operative pain management provided by the surgeon.
Another physician who performs any component of the global package will not receive separate payment unless the surgeon is willing to forego a portion of the payment. For example, a hospitalist admits a patient who has no other identifiable medical conditions aside from the problem prompting surgery. The hospitalist’s role may be dictated by facility policy—quality of care or risk reduction, for example—and administrative requirements (history and physical exam, discharge services, coordination of care) rather than what a payer would perceive as necessary “medical” management. Similarly, if the hospitalist’s post-op care is limited to ordering routine post-op labs or maintaining appropriate pain management, the hospitalist’s service will likely be denied as incidental to the surgical package.
Remember, if the hospitalist’s claim is submitted and paid, it doesn’t mean that the payer won’t retract the payment upon review if an erroneous payment is suspected. A payer review may be triggered when the diagnosis listed on the hospitalist’s claim matches the diagnosis listed on the surgeon’s claim (e.g. 820.8). If too many claims are considered “not medically necessary” due to overlapping care, hospitalists may need to negotiate other terms of payment with the facility to recoup unpaid time and effort when involved in this type of care.
When more than one medical condition exists and several physicians participate in the patient’s care, medical necessity is easily established for each physician. Each physician manages the condition related to his/her expertise. In the above example, the surgeon cares for the patient’s fracture, while the hospitalist oversees diabetes and hypertension management. Service distinction is crucial during the claim submission process. The hospitalist should report a subsequent hospital care code (99231-99233) with a primary diagnosis corresponding to his/her specialty-related care (i.e., 9923x with 250.00, 401.1).3
When more specialists are involved, claim submission becomes more complex. A cardiologist who was also involved in patient management would report his or her service using 401.1. When a different primary diagnosis is assigned to the visit code to indicate the reason for each physician’s involvement, all claims are more likely to be paid.4 As long as the hospitalist maintains care over one of the patients’ conditions, concurrent care is justified.
Because these physicians are in different specialties and different provider groups, most payers do not require the modifier 25 (separately identifiable evaluation/management [E/M] service on the same day as a procedure or other service) with the visit code; however, some managed care payers may have a general claim edit that pays the first claim and denies the second unless modifier 25 is appended to the concurrent E/M visit code (i.e., 99232-25) as an attestation that the service is distinct from any other provider’s service that day, despite claim submission under different tax identification numbers. This may not be identified until the claim is rejected or denied. If appropriate modifier use does not yield payment, appeal the denied concurrent care claims with supporting documentation from each physician visit, if possible. This demonstrates each physician’s contribution to care.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15—Covered Medical and Other Health Services. Section 30.E. Available at: www.cms.gov/manuals/Downloads/bp102c15.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 40.A. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed March 5, 2015.
- American Medical Association. Current Procedural Terminology 2015 Professional Edition. Chicago: American Medical Association Press; 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 30.6.9.C. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 30.6.5. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 26—Completing and Processing Form CMS-1500 Data Set. Section 10.8.2. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf. Accessed March 5, 2015.
Hospitalists often are tasked with coordinating and overseeing patient care throughout a hospitalization. Depending on the care model and the availability of varying specialists, a patient could see several specialists throughout the stay, and even during a single day. A recurring issue for many hospitalists is justifying the medical necessity of their services, because payers do not want to reimburse overlapping care (i.e., multiple providers caring for the same patient problem) when more than one physician provides care on the same service date.
Payers often consider two key principles before reimbursing multiple visits on the same date:1
- Does the patient’s condition warrant the services of more than one physician?
- Are the individual services provided by each physician reasonable and necessary?
Consider the following example: A 65-year-old female patient is admitted with a hip fracture (820.8) after slipping on the ice outside her home. The patient also has hypertension (401.1) and type II diabetes (250.00). The surgeon manages the patient’s peri-operative course for the fracture, while the hospitalist manages the patient’s medical issues.
Payers must be sure that the services of one physician do not duplicate those provided by another.1 For the above scenario, it is imperative that the hospitalist understand which services are considered the surgeon’s responsibility. The global surgical package includes payment for the surgical procedure and the completion of its corresponding facility-required paperwork (e.g. pre-operative history and physical exam, operative consent forms, pre-operative orders), in addition to the following services:2
- Pre-operative visits after making the decision for surgery beginning one day prior to surgery;
- All additional post-operative medical or surgical services provided by the surgeon related to complications but not requiring additional trips to the operating room;
- Post-operative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes, local incisional care, removal of cutaneous sutures and staples, line removals, changes and removal of tracheostomy tubes, and discharge services; and
- Post-operative pain management provided by the surgeon.
Another physician who performs any component of the global package will not receive separate payment unless the surgeon is willing to forego a portion of the payment. For example, a hospitalist admits a patient who has no other identifiable medical conditions aside from the problem prompting surgery. The hospitalist’s role may be dictated by facility policy—quality of care or risk reduction, for example—and administrative requirements (history and physical exam, discharge services, coordination of care) rather than what a payer would perceive as necessary “medical” management. Similarly, if the hospitalist’s post-op care is limited to ordering routine post-op labs or maintaining appropriate pain management, the hospitalist’s service will likely be denied as incidental to the surgical package.
Remember, if the hospitalist’s claim is submitted and paid, it doesn’t mean that the payer won’t retract the payment upon review if an erroneous payment is suspected. A payer review may be triggered when the diagnosis listed on the hospitalist’s claim matches the diagnosis listed on the surgeon’s claim (e.g. 820.8). If too many claims are considered “not medically necessary” due to overlapping care, hospitalists may need to negotiate other terms of payment with the facility to recoup unpaid time and effort when involved in this type of care.
When more than one medical condition exists and several physicians participate in the patient’s care, medical necessity is easily established for each physician. Each physician manages the condition related to his/her expertise. In the above example, the surgeon cares for the patient’s fracture, while the hospitalist oversees diabetes and hypertension management. Service distinction is crucial during the claim submission process. The hospitalist should report a subsequent hospital care code (99231-99233) with a primary diagnosis corresponding to his/her specialty-related care (i.e., 9923x with 250.00, 401.1).3
When more specialists are involved, claim submission becomes more complex. A cardiologist who was also involved in patient management would report his or her service using 401.1. When a different primary diagnosis is assigned to the visit code to indicate the reason for each physician’s involvement, all claims are more likely to be paid.4 As long as the hospitalist maintains care over one of the patients’ conditions, concurrent care is justified.
Because these physicians are in different specialties and different provider groups, most payers do not require the modifier 25 (separately identifiable evaluation/management [E/M] service on the same day as a procedure or other service) with the visit code; however, some managed care payers may have a general claim edit that pays the first claim and denies the second unless modifier 25 is appended to the concurrent E/M visit code (i.e., 99232-25) as an attestation that the service is distinct from any other provider’s service that day, despite claim submission under different tax identification numbers. This may not be identified until the claim is rejected or denied. If appropriate modifier use does not yield payment, appeal the denied concurrent care claims with supporting documentation from each physician visit, if possible. This demonstrates each physician’s contribution to care.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15—Covered Medical and Other Health Services. Section 30.E. Available at: www.cms.gov/manuals/Downloads/bp102c15.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 40.A. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed March 5, 2015.
- American Medical Association. Current Procedural Terminology 2015 Professional Edition. Chicago: American Medical Association Press; 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 30.6.9.C. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 30.6.5. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 26—Completing and Processing Form CMS-1500 Data Set. Section 10.8.2. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf. Accessed March 5, 2015.
Hospitalists often are tasked with coordinating and overseeing patient care throughout a hospitalization. Depending on the care model and the availability of varying specialists, a patient could see several specialists throughout the stay, and even during a single day. A recurring issue for many hospitalists is justifying the medical necessity of their services, because payers do not want to reimburse overlapping care (i.e., multiple providers caring for the same patient problem) when more than one physician provides care on the same service date.
Payers often consider two key principles before reimbursing multiple visits on the same date:1
- Does the patient’s condition warrant the services of more than one physician?
- Are the individual services provided by each physician reasonable and necessary?
Consider the following example: A 65-year-old female patient is admitted with a hip fracture (820.8) after slipping on the ice outside her home. The patient also has hypertension (401.1) and type II diabetes (250.00). The surgeon manages the patient’s peri-operative course for the fracture, while the hospitalist manages the patient’s medical issues.
Payers must be sure that the services of one physician do not duplicate those provided by another.1 For the above scenario, it is imperative that the hospitalist understand which services are considered the surgeon’s responsibility. The global surgical package includes payment for the surgical procedure and the completion of its corresponding facility-required paperwork (e.g. pre-operative history and physical exam, operative consent forms, pre-operative orders), in addition to the following services:2
- Pre-operative visits after making the decision for surgery beginning one day prior to surgery;
- All additional post-operative medical or surgical services provided by the surgeon related to complications but not requiring additional trips to the operating room;
- Post-operative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes, local incisional care, removal of cutaneous sutures and staples, line removals, changes and removal of tracheostomy tubes, and discharge services; and
- Post-operative pain management provided by the surgeon.
Another physician who performs any component of the global package will not receive separate payment unless the surgeon is willing to forego a portion of the payment. For example, a hospitalist admits a patient who has no other identifiable medical conditions aside from the problem prompting surgery. The hospitalist’s role may be dictated by facility policy—quality of care or risk reduction, for example—and administrative requirements (history and physical exam, discharge services, coordination of care) rather than what a payer would perceive as necessary “medical” management. Similarly, if the hospitalist’s post-op care is limited to ordering routine post-op labs or maintaining appropriate pain management, the hospitalist’s service will likely be denied as incidental to the surgical package.
Remember, if the hospitalist’s claim is submitted and paid, it doesn’t mean that the payer won’t retract the payment upon review if an erroneous payment is suspected. A payer review may be triggered when the diagnosis listed on the hospitalist’s claim matches the diagnosis listed on the surgeon’s claim (e.g. 820.8). If too many claims are considered “not medically necessary” due to overlapping care, hospitalists may need to negotiate other terms of payment with the facility to recoup unpaid time and effort when involved in this type of care.
When more than one medical condition exists and several physicians participate in the patient’s care, medical necessity is easily established for each physician. Each physician manages the condition related to his/her expertise. In the above example, the surgeon cares for the patient’s fracture, while the hospitalist oversees diabetes and hypertension management. Service distinction is crucial during the claim submission process. The hospitalist should report a subsequent hospital care code (99231-99233) with a primary diagnosis corresponding to his/her specialty-related care (i.e., 9923x with 250.00, 401.1).3
When more specialists are involved, claim submission becomes more complex. A cardiologist who was also involved in patient management would report his or her service using 401.1. When a different primary diagnosis is assigned to the visit code to indicate the reason for each physician’s involvement, all claims are more likely to be paid.4 As long as the hospitalist maintains care over one of the patients’ conditions, concurrent care is justified.
Because these physicians are in different specialties and different provider groups, most payers do not require the modifier 25 (separately identifiable evaluation/management [E/M] service on the same day as a procedure or other service) with the visit code; however, some managed care payers may have a general claim edit that pays the first claim and denies the second unless modifier 25 is appended to the concurrent E/M visit code (i.e., 99232-25) as an attestation that the service is distinct from any other provider’s service that day, despite claim submission under different tax identification numbers. This may not be identified until the claim is rejected or denied. If appropriate modifier use does not yield payment, appeal the denied concurrent care claims with supporting documentation from each physician visit, if possible. This demonstrates each physician’s contribution to care.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15—Covered Medical and Other Health Services. Section 30.E. Available at: www.cms.gov/manuals/Downloads/bp102c15.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 40.A. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed March 5, 2015.
- American Medical Association. Current Procedural Terminology 2015 Professional Edition. Chicago: American Medical Association Press; 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 30.6.9.C. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12—Physicians/Nonphysician Practitioners. Section 30.6.5. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2015.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 26—Completing and Processing Form CMS-1500 Data Set. Section 10.8.2. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf. Accessed March 5, 2015.
Time-Based Physician Services Require Proper Documentation
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record, and they often misunderstand the use of time when selecting visit levels. Sometimes providers may report a lower service level than warranted because they didn’t feel that they spent the required amount of time with the patient; however, the duration of the visit is an ancillary factor and does not control the level of service to be billed unless more than 50% of the face-to-face time (for non-inpatient services) or more than 50% of the floor time (for inpatient services) is spent providing counseling or coordination of care (C/CC).1 In these instances, providers may choose to document only a brief history and exam, or none at all. They should update the medical decision-making based on the discussion.
Consider the hospitalization of an elderly patient who is newly diagnosed with diabetes. In addition to stabilizing the patient’s glucose levels and devising the appropriate care plan, the patient and/or caregivers also require extensive counseling regarding disease management, lifestyle modification, and medication regime. Coordination of care for outpatient programs and resources is also crucial. To make sure that this qualifies as a time-based service, ensure that the documentation contains the duration, the issues addressed, and the signature of the service provider.
Duration of Counseling and/or Coordination of Care
Time is not used for visit level selection if C/CC is minimal (<50%) or absent from the patient encounter. For inpatient services, total visit time is identified as provider face-to-face time (i.e., at the bedside) combined with time spent on the patient’s unit/floor performing services that are directly related to that patient, such as reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers.
Time associated with activities performed in locations other than the patient’s unit/floor (e.g. reviewing current results or images from the physician’s office) is not allowable in calculating the total visit time. Time associated with teaching students/interns is also excluded, because this doesn’t reflect patient care activities. Once the provider documents all services rendered on a given calendar date, the provider selects the visit level that corresponds with the cumulative visit time documented in the chart (see Tables 1 and 2).
Issues Addressed
When counseling and/or coordination of care dominate more than 50% of the time a physician spends with a patient during an evaluation and management (E/M) service, then time may be considered as the controlling factor to qualify the E/M service for a particular level of care.2 The following must be documented in the patient’s medical record in order to report an E/M service based on time:
- The total length of time of the E/M visit;
- Evidence that more than half of the total length of time of the E/M visit was spent in counseling and coordinating of care; and
- The content of the counseling and coordination of care provided during the E/M visit.
History and exam, if performed or updated, should also be documented, along with the patient response or comprehension of information. An acceptable C/CC time entry may be noted as, “Total visit time = 35 minutes; > 50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payer may prefer one documentation style over another. It is always best to query payer policy and review local documentation standards to ensure compliance. Please remember that while this example constitutes the required elements for the notation of time, documentation must also include the details of counseling, care plan revisions, and any information that is pertinent to patient care and communication with other healthcare professionals.
Family Discussions
Family discussions are a typical event involved in taking care of patients and are appropriate to count as C/CC time. Special circumstances are considered when discussions must take place without the patient present. This type of counseling time is recognized but only counts towards C/CC time if the following criteria are met and documented:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.3
Time cannot be counted if the discussion takes place in an area outside of the patient’s unit/floor (e.g. in the physician’s office) or if the time is spent counseling the family members through their grieving process.
It is fairly common for the family discussion to take place later in the day, after the physician has completed morning rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient assessment incorporating the components of an evaluation (i.e., history update and physical) and management (i.e., care plan review/revision) service, the meeting time may qualify for prolonged care services.
Service Provider
Be sure to count only the physician’s time spent in C/CC. Counseling time by the nursing staff, the social worker, or the resident cannot contribute toward the physician’s total visit time. When more than one physician is involved in services throughout the day, the physicians should select a level of service representative of the combined visits and submit the appropriate code for that level under one physician’s name.4
Consider the following example: The hospitalist takes a brief history about overnight events and reviews some of the pertinent information with the patient. He/she then leaves the room to coordinate the patient’s ongoing care in anticipation that the patient will be discharged over the next few days (25 minutes). The resident is asked to continue the assessment and counsel the patient on the patient’s current disease process (20 minutes).
In the above scenario, the hospitalist is only able to report 99232, because the time spent by the resident is “nonbillable time.”
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1B. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Novitas Solutions, Inc. Frequently Asked Questions: Evaluation and Management Services (Part B). Available at: http://www.novitas-solutions.com/webcenter/faces/oracle/webcenter/page/scopedMD/sad78b265_6797_4ed0_a02f_81627913bc78/Page57.jspx?wc.contextURL=%2Fspaces%2FMedicareJH&wc.originURL=%2Fspaces%2FMedicareJH%2Fpage%2Fpagebyid&contentId=00005056&_afrLoop=1728453012371000#%40%3F_afrLoop%3D1728453012371000%26wc.originURL%3D%252Fspaces%252FMedicareJH%252Fpage%252Fpagebyid%26contentId%3D00005056%26wc.contextURL%3D%252Fspaces%252FMedicareJH%26_adf.ctrl-state%3D610bhasa4_134. Accessed on December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare National Coverage Determinations Manual: Chapter 1, Part 1: Coverage Determinations, Section 70.1. Available at: www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.5. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Abraham M, Ahlman JT, Boudreau AJ, Connelly J, Levreau-Davis L. Current Procedural Terminology 2014 Professional Edition. Chicago: American Medical Association Press; 2013:1-32.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1C. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.15.1G. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf.
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record, and they often misunderstand the use of time when selecting visit levels. Sometimes providers may report a lower service level than warranted because they didn’t feel that they spent the required amount of time with the patient; however, the duration of the visit is an ancillary factor and does not control the level of service to be billed unless more than 50% of the face-to-face time (for non-inpatient services) or more than 50% of the floor time (for inpatient services) is spent providing counseling or coordination of care (C/CC).1 In these instances, providers may choose to document only a brief history and exam, or none at all. They should update the medical decision-making based on the discussion.
Consider the hospitalization of an elderly patient who is newly diagnosed with diabetes. In addition to stabilizing the patient’s glucose levels and devising the appropriate care plan, the patient and/or caregivers also require extensive counseling regarding disease management, lifestyle modification, and medication regime. Coordination of care for outpatient programs and resources is also crucial. To make sure that this qualifies as a time-based service, ensure that the documentation contains the duration, the issues addressed, and the signature of the service provider.
Duration of Counseling and/or Coordination of Care
Time is not used for visit level selection if C/CC is minimal (<50%) or absent from the patient encounter. For inpatient services, total visit time is identified as provider face-to-face time (i.e., at the bedside) combined with time spent on the patient’s unit/floor performing services that are directly related to that patient, such as reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers.
Time associated with activities performed in locations other than the patient’s unit/floor (e.g. reviewing current results or images from the physician’s office) is not allowable in calculating the total visit time. Time associated with teaching students/interns is also excluded, because this doesn’t reflect patient care activities. Once the provider documents all services rendered on a given calendar date, the provider selects the visit level that corresponds with the cumulative visit time documented in the chart (see Tables 1 and 2).
Issues Addressed
When counseling and/or coordination of care dominate more than 50% of the time a physician spends with a patient during an evaluation and management (E/M) service, then time may be considered as the controlling factor to qualify the E/M service for a particular level of care.2 The following must be documented in the patient’s medical record in order to report an E/M service based on time:
- The total length of time of the E/M visit;
- Evidence that more than half of the total length of time of the E/M visit was spent in counseling and coordinating of care; and
- The content of the counseling and coordination of care provided during the E/M visit.
History and exam, if performed or updated, should also be documented, along with the patient response or comprehension of information. An acceptable C/CC time entry may be noted as, “Total visit time = 35 minutes; > 50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payer may prefer one documentation style over another. It is always best to query payer policy and review local documentation standards to ensure compliance. Please remember that while this example constitutes the required elements for the notation of time, documentation must also include the details of counseling, care plan revisions, and any information that is pertinent to patient care and communication with other healthcare professionals.
Family Discussions
Family discussions are a typical event involved in taking care of patients and are appropriate to count as C/CC time. Special circumstances are considered when discussions must take place without the patient present. This type of counseling time is recognized but only counts towards C/CC time if the following criteria are met and documented:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.3
Time cannot be counted if the discussion takes place in an area outside of the patient’s unit/floor (e.g. in the physician’s office) or if the time is spent counseling the family members through their grieving process.
It is fairly common for the family discussion to take place later in the day, after the physician has completed morning rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient assessment incorporating the components of an evaluation (i.e., history update and physical) and management (i.e., care plan review/revision) service, the meeting time may qualify for prolonged care services.
Service Provider
Be sure to count only the physician’s time spent in C/CC. Counseling time by the nursing staff, the social worker, or the resident cannot contribute toward the physician’s total visit time. When more than one physician is involved in services throughout the day, the physicians should select a level of service representative of the combined visits and submit the appropriate code for that level under one physician’s name.4
Consider the following example: The hospitalist takes a brief history about overnight events and reviews some of the pertinent information with the patient. He/she then leaves the room to coordinate the patient’s ongoing care in anticipation that the patient will be discharged over the next few days (25 minutes). The resident is asked to continue the assessment and counsel the patient on the patient’s current disease process (20 minutes).
In the above scenario, the hospitalist is only able to report 99232, because the time spent by the resident is “nonbillable time.”
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1B. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Novitas Solutions, Inc. Frequently Asked Questions: Evaluation and Management Services (Part B). Available at: http://www.novitas-solutions.com/webcenter/faces/oracle/webcenter/page/scopedMD/sad78b265_6797_4ed0_a02f_81627913bc78/Page57.jspx?wc.contextURL=%2Fspaces%2FMedicareJH&wc.originURL=%2Fspaces%2FMedicareJH%2Fpage%2Fpagebyid&contentId=00005056&_afrLoop=1728453012371000#%40%3F_afrLoop%3D1728453012371000%26wc.originURL%3D%252Fspaces%252FMedicareJH%252Fpage%252Fpagebyid%26contentId%3D00005056%26wc.contextURL%3D%252Fspaces%252FMedicareJH%26_adf.ctrl-state%3D610bhasa4_134. Accessed on December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare National Coverage Determinations Manual: Chapter 1, Part 1: Coverage Determinations, Section 70.1. Available at: www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.5. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Abraham M, Ahlman JT, Boudreau AJ, Connelly J, Levreau-Davis L. Current Procedural Terminology 2014 Professional Edition. Chicago: American Medical Association Press; 2013:1-32.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1C. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.15.1G. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf.
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record, and they often misunderstand the use of time when selecting visit levels. Sometimes providers may report a lower service level than warranted because they didn’t feel that they spent the required amount of time with the patient; however, the duration of the visit is an ancillary factor and does not control the level of service to be billed unless more than 50% of the face-to-face time (for non-inpatient services) or more than 50% of the floor time (for inpatient services) is spent providing counseling or coordination of care (C/CC).1 In these instances, providers may choose to document only a brief history and exam, or none at all. They should update the medical decision-making based on the discussion.
Consider the hospitalization of an elderly patient who is newly diagnosed with diabetes. In addition to stabilizing the patient’s glucose levels and devising the appropriate care plan, the patient and/or caregivers also require extensive counseling regarding disease management, lifestyle modification, and medication regime. Coordination of care for outpatient programs and resources is also crucial. To make sure that this qualifies as a time-based service, ensure that the documentation contains the duration, the issues addressed, and the signature of the service provider.
Duration of Counseling and/or Coordination of Care
Time is not used for visit level selection if C/CC is minimal (<50%) or absent from the patient encounter. For inpatient services, total visit time is identified as provider face-to-face time (i.e., at the bedside) combined with time spent on the patient’s unit/floor performing services that are directly related to that patient, such as reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers.
Time associated with activities performed in locations other than the patient’s unit/floor (e.g. reviewing current results or images from the physician’s office) is not allowable in calculating the total visit time. Time associated with teaching students/interns is also excluded, because this doesn’t reflect patient care activities. Once the provider documents all services rendered on a given calendar date, the provider selects the visit level that corresponds with the cumulative visit time documented in the chart (see Tables 1 and 2).
Issues Addressed
When counseling and/or coordination of care dominate more than 50% of the time a physician spends with a patient during an evaluation and management (E/M) service, then time may be considered as the controlling factor to qualify the E/M service for a particular level of care.2 The following must be documented in the patient’s medical record in order to report an E/M service based on time:
- The total length of time of the E/M visit;
- Evidence that more than half of the total length of time of the E/M visit was spent in counseling and coordinating of care; and
- The content of the counseling and coordination of care provided during the E/M visit.
History and exam, if performed or updated, should also be documented, along with the patient response or comprehension of information. An acceptable C/CC time entry may be noted as, “Total visit time = 35 minutes; > 50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payer may prefer one documentation style over another. It is always best to query payer policy and review local documentation standards to ensure compliance. Please remember that while this example constitutes the required elements for the notation of time, documentation must also include the details of counseling, care plan revisions, and any information that is pertinent to patient care and communication with other healthcare professionals.
Family Discussions
Family discussions are a typical event involved in taking care of patients and are appropriate to count as C/CC time. Special circumstances are considered when discussions must take place without the patient present. This type of counseling time is recognized but only counts towards C/CC time if the following criteria are met and documented:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.3
Time cannot be counted if the discussion takes place in an area outside of the patient’s unit/floor (e.g. in the physician’s office) or if the time is spent counseling the family members through their grieving process.
It is fairly common for the family discussion to take place later in the day, after the physician has completed morning rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient assessment incorporating the components of an evaluation (i.e., history update and physical) and management (i.e., care plan review/revision) service, the meeting time may qualify for prolonged care services.
Service Provider
Be sure to count only the physician’s time spent in C/CC. Counseling time by the nursing staff, the social worker, or the resident cannot contribute toward the physician’s total visit time. When more than one physician is involved in services throughout the day, the physicians should select a level of service representative of the combined visits and submit the appropriate code for that level under one physician’s name.4
Consider the following example: The hospitalist takes a brief history about overnight events and reviews some of the pertinent information with the patient. He/she then leaves the room to coordinate the patient’s ongoing care in anticipation that the patient will be discharged over the next few days (25 minutes). The resident is asked to continue the assessment and counsel the patient on the patient’s current disease process (20 minutes).
In the above scenario, the hospitalist is only able to report 99232, because the time spent by the resident is “nonbillable time.”
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1B. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Novitas Solutions, Inc. Frequently Asked Questions: Evaluation and Management Services (Part B). Available at: http://www.novitas-solutions.com/webcenter/faces/oracle/webcenter/page/scopedMD/sad78b265_6797_4ed0_a02f_81627913bc78/Page57.jspx?wc.contextURL=%2Fspaces%2FMedicareJH&wc.originURL=%2Fspaces%2FMedicareJH%2Fpage%2Fpagebyid&contentId=00005056&_afrLoop=1728453012371000#%40%3F_afrLoop%3D1728453012371000%26wc.originURL%3D%252Fspaces%252FMedicareJH%252Fpage%252Fpagebyid%26contentId%3D00005056%26wc.contextURL%3D%252Fspaces%252FMedicareJH%26_adf.ctrl-state%3D610bhasa4_134. Accessed on December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare National Coverage Determinations Manual: Chapter 1, Part 1: Coverage Determinations, Section 70.1. Available at: www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.5. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Abraham M, Ahlman JT, Boudreau AJ, Connelly J, Levreau-Davis L. Current Procedural Terminology 2014 Professional Edition. Chicago: American Medical Association Press; 2013:1-32.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1C. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.15.1G. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf.
Avoid Billing, Coding Discrepancies When Documenting Patient History
- Continue to educate physicians on proper billing for E/M services;
- Encourage its contractors to review physicians’ billing for E/M services; and
- Review physicians who bill higher level E/M codes for appropriate action.1
When documenting patient history, physicians must be aware of the common discrepancies that occur. Although the physician becomes familiar with the patient as he/she provides care throughout the hospitalization, the auditor must acquaint himself or herself with the patient using only the limited information provided in the progress note.
When documentation is requested by the payer for a specific service date, only the documentation from that service date is considered. Be sure that the information is adequate to support both clinical care and the reported service level.
Patient History Requirements
Chief complaint. The chief complaint (CC) is the reason for the visit as stated in the patient’s own words. Every encounter, regardless of visit type, must include a CC. The physician must personally document and/or validate the CC with reference to a specific condition or symptom (e.g. patient complains of abdominal pain).
- Incomplete CC example: “Follow-up”;
- Better CC example: “Follow-up for severe abdominal cramping.”
History of present illness. The history of present illness (HPI) describes the development or progression of the patient’s current problem(s). The traditional HPI elements recognized in the 1995 documentation guidelines are location, quality, severity, duration, timing, context, modifying factors, and associated signs/symptoms.2,3
The physician must obtain and personally document the HPI. He/she also has the option to link to the HPI documented by residents (i.e., residents, fellows, interns) in compliance with the teaching physician rules or nonphysician practitioners (i.e., nurse practitioners and physician assistants) as defined by the split-shared billing rules. An auditor will not accept HPI information if the physician attempts to link to any other individual, even if that person may be qualified to obtain this (e.g. registered nurse, medical assistant) or is a student (e.g. medical students, nurse practitioner students).
Because auditors recognize both 1995 and 1997 documentation guidelines, they must also recognize the HPI differences. The 1997 HPI format promotes the status of the patient’s chronic or inactive conditions.4 The physician receives one credit for each chronic condition that is noted, along with documentation of what has occurred since the last physician encounter as it relates to the chronic condition (e.g. “patient has a history of chronic obstructive bronchitis without acute exacerbation in past six months”).
Physicians may utilize either style of HPI documentation, and auditors must review provider records against each set of guidelines. The final audited result reflects the highest visit level supported by either set of guidelines. For example, if physician documentation yields an “extended” HPI when 1995 guidelines are used but only a “brief” HPI (see Table 2) when 1997 guidelines are reviewed, the auditor awards the physician credit for the “extended” HPI.
- 1995 example: “The patient has intermittent (duration), sharp (quality) pain in the right upper quadrant (location) without associated nausea, vomiting, or diarrhea (associated signs/symptoms).”
- 1997 example: “Diabetes controlled by oral medication; hyperlipidemia stable on simvastatin with increased dietary efforts; hypertension stable with pressures ranging from 130-140/80-90 overnight” (status of three chronic conditions).
Review of systems. A review of systems (ROS) is a series of questions inquiring about additional signs, symptoms, or problems currently or previously experienced by the patient as related to the CC or presenting problem. The recognized systems are constitutional; eyes; ears, nose, mouth, throat; cardiovascular; respiratory; gastrointestinal; genitourinary; musculoskeletal; integumentary (including skin and/or breast); neurological; psychiatric; endocrine; hematologic/lymphatic; and allergic/immunologic.2,3
The physician may choose to document the ROS by making a notation for individual systems: “no fever/chills (constitutional) or blurred vision (eyes); no chest pain (cardiovascular) or shortness of breath (respiratory); intermittent nausea (gastrointestinal) and occasional runny nose (ears, nose, mouth, throat).” Alternatively, the physician may inquire about all of the systems but only document the positive and pertinent negative findings related to the CC, along with an additional comment that “all other systems are negative.” Most Medicare audit contractors currently accept this method as long as all systems were reviewed.5,6,7,8,9
Be advised that ROS information can be documented by anyone, including the patient. The physician must remember to reference ROS information that is completed by individuals other than residents or nonphysician practitioners (the physician is already required to reference the documentation of the latter individuals under the Teaching Physician Rules or Split-Shared Billing Rules).
Past, family, and social histories. Documentation of past, family, and social histories (PFSH) involves data obtained about the patient’s previous illness or medical conditions/therapies, family occurrences with illness, and relevant patient activities. An auditor credits the physician for a single comment correlated to each history for the PFSH. Using the term “noncontributory” (N/C) with any of the histories can result in downcoding. Many contractors do not allow this statement due to previous misunderstandings over its use.
- Incomplete PFSH example: “Patient is status-post cholecystectomy in August 2013; family history N/C; patient is former smoker” (Note: “family history N/C” is not accepted by most contractors).
- Better PFSH example: “Patient currently on Prilosec 20 mg daily; family history of Barrett’s Esophagus; no tobacco or alcohol use.”
PFSH data can also be documented by anyone, including the patient, and the physician must reference the PFSH information in his own progress note. Re-documenting the PFSH is not necessary unless a revision is required. PFSH documentation is only required for initial care services (i.e., initial hospital care, initial observation care, consultations). It is not required for subsequent care services, unless additional pertinent information that impacts care is obtained during the hospital stay.
Common Problems to Avoid
Information cannot be obtained. Some contractors will not penalize the physician for the inability to ascertain complete historical information as long as there is evidenced documentation of an attempt to obtain the information. When the physician cannot extract historical information from the patient directly and no other source is available, the physician documents that he is “unable to obtain” the history. Additionally, the physician must provide a comment to explain why the information is unobtainable (e.g. patient confused, no caregiver present) along with the available information from the limited resources (e.g. emergency medical technicians, records from previous hospitalizations at the same facility).
Previous information referenced. When referencing items from a previous encounter, be sure to include the referenced information when documentation is requested by the payer. Per CMS guidelines, the ROS and/or PFSH obtained during an earlier encounter does not need to be re-recorded if there is evidence that the physician reviewed and updated the previous information. The review and update may be documented by either describing any new ROS and/or PFSH information or noting that there has been no change in the information and noting the date and location of the earlier ROS and/or PFSH.2
Pre-op clearance and HPI deficiencies. HPI is typically not as deficient as the ROS or family history elements; however, HPI underdocumentation is mostly associated with encounters for pre-op clearance. The physician may state that “patient requires pre-op clearance for left knee repair.” In the absence of any comorbidities or acute illness, HPI documentation may be missing. The physician should remember to identify the details of the presenting problem: “Patient runs five miles daily. Knee felt unstable after running two weeks ago. Swelling and intermittent sharp pain 7/10. Patient has been taking ibuprofen daily without relief.”
Not medically necessary. Remember not to document any elements for the purpose of “getting paid.” Only document information that is clinically relevant, lends to the quality of care provided, or demonstrates the delivery of healthcare services. This prevents accusations of fraud and abuse, promotes billing compliance, and supports medical necessity for the services provided.
Varying levels of history. E/M services are selected based on the content of the three “key” components: history, exam, and decision-making (or visit time). If counseling and/or coordination of care does not encompass >50% of the physician’s total visit time or the service is not exclusively designated as a time-based service (e.g. critical care and discharge day management), the physician’s service time is not considered.
Documentation for each of the three key components must support the reported visit level when reporting initial hospital care and consultations (for those payers who still recognize consultation codes). Subsequent hospital care (e.g. 99233) only requires supportive documentation from two key components. Medical decision-making should be one of the two supporting components in order to demonstrate the medical necessity and nature of the presenting problem; the other supporting component can be history or exam.
Each visit category (e.g. initial hospital care or subsequent hospital care) and service level (e.g. 99221-99233) identifies corresponding documentation requirements. Failure to document any essential element in a given visit level (e.g. family history required for a comprehensive history when billing for 99222 and 99223) may result in service denial or downcoding (e.g. 99221). Be aware of what an auditor expects when reviewing patient history (see Table 1).
There are four levels of history: problem-focused, expanded problem-focused, detailed, and comprehensive. An auditor determines the number of history elements documented in the progress note (see Table 2). The history level corresponds to the lowest documented element. For example, if physician documentation includes four HPI elements, eight ROS, and a comment in each of the PFSHs, the history level is equivalent to “detailed.” The history would support initial hospital care 99221 or subsequent hospital care 99233.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Levinson DR. Department of Health and Human Services, Office of Inspector General: Coding Trends of Medicare Evaluation and Management Services. May 2012. Available at: oig.hhs.gov/oei/reports/oei-04-10-00180.pdf. Accessed October 4, 2014.
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/95Docguidelines.pdf. Accessed October 4, 2014.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis L. CPT 2013 Professional Edition (Current Procedural Terminology). Chicago: American Medical Association Press; 2012:4-10.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf. Accessed October 4, 2014.
- Noridian Healthcare Solutions. Medicare Part B: Evaluation and Management Workshop Questions and Answers. Available at: www.noridianmedicare.com/cgi-bin/coranto/viewnews.cgi?id=EkZpEVAyylqZyOfqel&tmpl=part_b_viewnews&style=part_ab_viewnews Accessed on October 4, 2014.
- WPS Medicare Health Insurance. J5 MAC Part B: Documentation (Q&As). Available at: www.wpsmedicare.com/j5macpartb/resources/provider_types/evalmngmntqa.shtml. Accessed October 4, 2014.
- NHIC, Corp. Building Your Medicare Knowledge: Advanced Building Blocks. Available at: www.medicarenhic.com/providers/pubs/AdvdBuildBlocks061212.pdf.
- Palmetto GBA. Jurisdiction 11 Part B: History Component. Available at: www.palmettogba.com/Palmetto/Providers.nsf/docsCat/Jurisdiction%2011%20Part%20B~EM%20Help%20Center~General%20Articles~History%20Component?open&Expand=1. Accessed October 4, 2014.
- Novitas Solutions. Frequently Asked Questions: Evaluation and Management Services (Part B). Available at: https://www.novitas-solutions.com/faq/partb/pet/lpet-evaluation_management_services.html. Accessed October 4, 2014.
- Continue to educate physicians on proper billing for E/M services;
- Encourage its contractors to review physicians’ billing for E/M services; and
- Review physicians who bill higher level E/M codes for appropriate action.1
When documenting patient history, physicians must be aware of the common discrepancies that occur. Although the physician becomes familiar with the patient as he/she provides care throughout the hospitalization, the auditor must acquaint himself or herself with the patient using only the limited information provided in the progress note.
When documentation is requested by the payer for a specific service date, only the documentation from that service date is considered. Be sure that the information is adequate to support both clinical care and the reported service level.
Patient History Requirements
Chief complaint. The chief complaint (CC) is the reason for the visit as stated in the patient’s own words. Every encounter, regardless of visit type, must include a CC. The physician must personally document and/or validate the CC with reference to a specific condition or symptom (e.g. patient complains of abdominal pain).
- Incomplete CC example: “Follow-up”;
- Better CC example: “Follow-up for severe abdominal cramping.”
History of present illness. The history of present illness (HPI) describes the development or progression of the patient’s current problem(s). The traditional HPI elements recognized in the 1995 documentation guidelines are location, quality, severity, duration, timing, context, modifying factors, and associated signs/symptoms.2,3
The physician must obtain and personally document the HPI. He/she also has the option to link to the HPI documented by residents (i.e., residents, fellows, interns) in compliance with the teaching physician rules or nonphysician practitioners (i.e., nurse practitioners and physician assistants) as defined by the split-shared billing rules. An auditor will not accept HPI information if the physician attempts to link to any other individual, even if that person may be qualified to obtain this (e.g. registered nurse, medical assistant) or is a student (e.g. medical students, nurse practitioner students).
Because auditors recognize both 1995 and 1997 documentation guidelines, they must also recognize the HPI differences. The 1997 HPI format promotes the status of the patient’s chronic or inactive conditions.4 The physician receives one credit for each chronic condition that is noted, along with documentation of what has occurred since the last physician encounter as it relates to the chronic condition (e.g. “patient has a history of chronic obstructive bronchitis without acute exacerbation in past six months”).
Physicians may utilize either style of HPI documentation, and auditors must review provider records against each set of guidelines. The final audited result reflects the highest visit level supported by either set of guidelines. For example, if physician documentation yields an “extended” HPI when 1995 guidelines are used but only a “brief” HPI (see Table 2) when 1997 guidelines are reviewed, the auditor awards the physician credit for the “extended” HPI.
- 1995 example: “The patient has intermittent (duration), sharp (quality) pain in the right upper quadrant (location) without associated nausea, vomiting, or diarrhea (associated signs/symptoms).”
- 1997 example: “Diabetes controlled by oral medication; hyperlipidemia stable on simvastatin with increased dietary efforts; hypertension stable with pressures ranging from 130-140/80-90 overnight” (status of three chronic conditions).
Review of systems. A review of systems (ROS) is a series of questions inquiring about additional signs, symptoms, or problems currently or previously experienced by the patient as related to the CC or presenting problem. The recognized systems are constitutional; eyes; ears, nose, mouth, throat; cardiovascular; respiratory; gastrointestinal; genitourinary; musculoskeletal; integumentary (including skin and/or breast); neurological; psychiatric; endocrine; hematologic/lymphatic; and allergic/immunologic.2,3
The physician may choose to document the ROS by making a notation for individual systems: “no fever/chills (constitutional) or blurred vision (eyes); no chest pain (cardiovascular) or shortness of breath (respiratory); intermittent nausea (gastrointestinal) and occasional runny nose (ears, nose, mouth, throat).” Alternatively, the physician may inquire about all of the systems but only document the positive and pertinent negative findings related to the CC, along with an additional comment that “all other systems are negative.” Most Medicare audit contractors currently accept this method as long as all systems were reviewed.5,6,7,8,9
Be advised that ROS information can be documented by anyone, including the patient. The physician must remember to reference ROS information that is completed by individuals other than residents or nonphysician practitioners (the physician is already required to reference the documentation of the latter individuals under the Teaching Physician Rules or Split-Shared Billing Rules).
Past, family, and social histories. Documentation of past, family, and social histories (PFSH) involves data obtained about the patient’s previous illness or medical conditions/therapies, family occurrences with illness, and relevant patient activities. An auditor credits the physician for a single comment correlated to each history for the PFSH. Using the term “noncontributory” (N/C) with any of the histories can result in downcoding. Many contractors do not allow this statement due to previous misunderstandings over its use.
- Incomplete PFSH example: “Patient is status-post cholecystectomy in August 2013; family history N/C; patient is former smoker” (Note: “family history N/C” is not accepted by most contractors).
- Better PFSH example: “Patient currently on Prilosec 20 mg daily; family history of Barrett’s Esophagus; no tobacco or alcohol use.”
PFSH data can also be documented by anyone, including the patient, and the physician must reference the PFSH information in his own progress note. Re-documenting the PFSH is not necessary unless a revision is required. PFSH documentation is only required for initial care services (i.e., initial hospital care, initial observation care, consultations). It is not required for subsequent care services, unless additional pertinent information that impacts care is obtained during the hospital stay.
Common Problems to Avoid
Information cannot be obtained. Some contractors will not penalize the physician for the inability to ascertain complete historical information as long as there is evidenced documentation of an attempt to obtain the information. When the physician cannot extract historical information from the patient directly and no other source is available, the physician documents that he is “unable to obtain” the history. Additionally, the physician must provide a comment to explain why the information is unobtainable (e.g. patient confused, no caregiver present) along with the available information from the limited resources (e.g. emergency medical technicians, records from previous hospitalizations at the same facility).
Previous information referenced. When referencing items from a previous encounter, be sure to include the referenced information when documentation is requested by the payer. Per CMS guidelines, the ROS and/or PFSH obtained during an earlier encounter does not need to be re-recorded if there is evidence that the physician reviewed and updated the previous information. The review and update may be documented by either describing any new ROS and/or PFSH information or noting that there has been no change in the information and noting the date and location of the earlier ROS and/or PFSH.2
Pre-op clearance and HPI deficiencies. HPI is typically not as deficient as the ROS or family history elements; however, HPI underdocumentation is mostly associated with encounters for pre-op clearance. The physician may state that “patient requires pre-op clearance for left knee repair.” In the absence of any comorbidities or acute illness, HPI documentation may be missing. The physician should remember to identify the details of the presenting problem: “Patient runs five miles daily. Knee felt unstable after running two weeks ago. Swelling and intermittent sharp pain 7/10. Patient has been taking ibuprofen daily without relief.”
Not medically necessary. Remember not to document any elements for the purpose of “getting paid.” Only document information that is clinically relevant, lends to the quality of care provided, or demonstrates the delivery of healthcare services. This prevents accusations of fraud and abuse, promotes billing compliance, and supports medical necessity for the services provided.
Varying levels of history. E/M services are selected based on the content of the three “key” components: history, exam, and decision-making (or visit time). If counseling and/or coordination of care does not encompass >50% of the physician’s total visit time or the service is not exclusively designated as a time-based service (e.g. critical care and discharge day management), the physician’s service time is not considered.
Documentation for each of the three key components must support the reported visit level when reporting initial hospital care and consultations (for those payers who still recognize consultation codes). Subsequent hospital care (e.g. 99233) only requires supportive documentation from two key components. Medical decision-making should be one of the two supporting components in order to demonstrate the medical necessity and nature of the presenting problem; the other supporting component can be history or exam.
Each visit category (e.g. initial hospital care or subsequent hospital care) and service level (e.g. 99221-99233) identifies corresponding documentation requirements. Failure to document any essential element in a given visit level (e.g. family history required for a comprehensive history when billing for 99222 and 99223) may result in service denial or downcoding (e.g. 99221). Be aware of what an auditor expects when reviewing patient history (see Table 1).
There are four levels of history: problem-focused, expanded problem-focused, detailed, and comprehensive. An auditor determines the number of history elements documented in the progress note (see Table 2). The history level corresponds to the lowest documented element. For example, if physician documentation includes four HPI elements, eight ROS, and a comment in each of the PFSHs, the history level is equivalent to “detailed.” The history would support initial hospital care 99221 or subsequent hospital care 99233.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Levinson DR. Department of Health and Human Services, Office of Inspector General: Coding Trends of Medicare Evaluation and Management Services. May 2012. Available at: oig.hhs.gov/oei/reports/oei-04-10-00180.pdf. Accessed October 4, 2014.
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/95Docguidelines.pdf. Accessed October 4, 2014.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis L. CPT 2013 Professional Edition (Current Procedural Terminology). Chicago: American Medical Association Press; 2012:4-10.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf. Accessed October 4, 2014.
- Noridian Healthcare Solutions. Medicare Part B: Evaluation and Management Workshop Questions and Answers. Available at: www.noridianmedicare.com/cgi-bin/coranto/viewnews.cgi?id=EkZpEVAyylqZyOfqel&tmpl=part_b_viewnews&style=part_ab_viewnews Accessed on October 4, 2014.
- WPS Medicare Health Insurance. J5 MAC Part B: Documentation (Q&As). Available at: www.wpsmedicare.com/j5macpartb/resources/provider_types/evalmngmntqa.shtml. Accessed October 4, 2014.
- NHIC, Corp. Building Your Medicare Knowledge: Advanced Building Blocks. Available at: www.medicarenhic.com/providers/pubs/AdvdBuildBlocks061212.pdf.
- Palmetto GBA. Jurisdiction 11 Part B: History Component. Available at: www.palmettogba.com/Palmetto/Providers.nsf/docsCat/Jurisdiction%2011%20Part%20B~EM%20Help%20Center~General%20Articles~History%20Component?open&Expand=1. Accessed October 4, 2014.
- Novitas Solutions. Frequently Asked Questions: Evaluation and Management Services (Part B). Available at: https://www.novitas-solutions.com/faq/partb/pet/lpet-evaluation_management_services.html. Accessed October 4, 2014.
- Continue to educate physicians on proper billing for E/M services;
- Encourage its contractors to review physicians’ billing for E/M services; and
- Review physicians who bill higher level E/M codes for appropriate action.1
When documenting patient history, physicians must be aware of the common discrepancies that occur. Although the physician becomes familiar with the patient as he/she provides care throughout the hospitalization, the auditor must acquaint himself or herself with the patient using only the limited information provided in the progress note.
When documentation is requested by the payer for a specific service date, only the documentation from that service date is considered. Be sure that the information is adequate to support both clinical care and the reported service level.
Patient History Requirements
Chief complaint. The chief complaint (CC) is the reason for the visit as stated in the patient’s own words. Every encounter, regardless of visit type, must include a CC. The physician must personally document and/or validate the CC with reference to a specific condition or symptom (e.g. patient complains of abdominal pain).
- Incomplete CC example: “Follow-up”;
- Better CC example: “Follow-up for severe abdominal cramping.”
History of present illness. The history of present illness (HPI) describes the development or progression of the patient’s current problem(s). The traditional HPI elements recognized in the 1995 documentation guidelines are location, quality, severity, duration, timing, context, modifying factors, and associated signs/symptoms.2,3
The physician must obtain and personally document the HPI. He/she also has the option to link to the HPI documented by residents (i.e., residents, fellows, interns) in compliance with the teaching physician rules or nonphysician practitioners (i.e., nurse practitioners and physician assistants) as defined by the split-shared billing rules. An auditor will not accept HPI information if the physician attempts to link to any other individual, even if that person may be qualified to obtain this (e.g. registered nurse, medical assistant) or is a student (e.g. medical students, nurse practitioner students).
Because auditors recognize both 1995 and 1997 documentation guidelines, they must also recognize the HPI differences. The 1997 HPI format promotes the status of the patient’s chronic or inactive conditions.4 The physician receives one credit for each chronic condition that is noted, along with documentation of what has occurred since the last physician encounter as it relates to the chronic condition (e.g. “patient has a history of chronic obstructive bronchitis without acute exacerbation in past six months”).
Physicians may utilize either style of HPI documentation, and auditors must review provider records against each set of guidelines. The final audited result reflects the highest visit level supported by either set of guidelines. For example, if physician documentation yields an “extended” HPI when 1995 guidelines are used but only a “brief” HPI (see Table 2) when 1997 guidelines are reviewed, the auditor awards the physician credit for the “extended” HPI.
- 1995 example: “The patient has intermittent (duration), sharp (quality) pain in the right upper quadrant (location) without associated nausea, vomiting, or diarrhea (associated signs/symptoms).”
- 1997 example: “Diabetes controlled by oral medication; hyperlipidemia stable on simvastatin with increased dietary efforts; hypertension stable with pressures ranging from 130-140/80-90 overnight” (status of three chronic conditions).
Review of systems. A review of systems (ROS) is a series of questions inquiring about additional signs, symptoms, or problems currently or previously experienced by the patient as related to the CC or presenting problem. The recognized systems are constitutional; eyes; ears, nose, mouth, throat; cardiovascular; respiratory; gastrointestinal; genitourinary; musculoskeletal; integumentary (including skin and/or breast); neurological; psychiatric; endocrine; hematologic/lymphatic; and allergic/immunologic.2,3
The physician may choose to document the ROS by making a notation for individual systems: “no fever/chills (constitutional) or blurred vision (eyes); no chest pain (cardiovascular) or shortness of breath (respiratory); intermittent nausea (gastrointestinal) and occasional runny nose (ears, nose, mouth, throat).” Alternatively, the physician may inquire about all of the systems but only document the positive and pertinent negative findings related to the CC, along with an additional comment that “all other systems are negative.” Most Medicare audit contractors currently accept this method as long as all systems were reviewed.5,6,7,8,9
Be advised that ROS information can be documented by anyone, including the patient. The physician must remember to reference ROS information that is completed by individuals other than residents or nonphysician practitioners (the physician is already required to reference the documentation of the latter individuals under the Teaching Physician Rules or Split-Shared Billing Rules).
Past, family, and social histories. Documentation of past, family, and social histories (PFSH) involves data obtained about the patient’s previous illness or medical conditions/therapies, family occurrences with illness, and relevant patient activities. An auditor credits the physician for a single comment correlated to each history for the PFSH. Using the term “noncontributory” (N/C) with any of the histories can result in downcoding. Many contractors do not allow this statement due to previous misunderstandings over its use.
- Incomplete PFSH example: “Patient is status-post cholecystectomy in August 2013; family history N/C; patient is former smoker” (Note: “family history N/C” is not accepted by most contractors).
- Better PFSH example: “Patient currently on Prilosec 20 mg daily; family history of Barrett’s Esophagus; no tobacco or alcohol use.”
PFSH data can also be documented by anyone, including the patient, and the physician must reference the PFSH information in his own progress note. Re-documenting the PFSH is not necessary unless a revision is required. PFSH documentation is only required for initial care services (i.e., initial hospital care, initial observation care, consultations). It is not required for subsequent care services, unless additional pertinent information that impacts care is obtained during the hospital stay.
Common Problems to Avoid
Information cannot be obtained. Some contractors will not penalize the physician for the inability to ascertain complete historical information as long as there is evidenced documentation of an attempt to obtain the information. When the physician cannot extract historical information from the patient directly and no other source is available, the physician documents that he is “unable to obtain” the history. Additionally, the physician must provide a comment to explain why the information is unobtainable (e.g. patient confused, no caregiver present) along with the available information from the limited resources (e.g. emergency medical technicians, records from previous hospitalizations at the same facility).
Previous information referenced. When referencing items from a previous encounter, be sure to include the referenced information when documentation is requested by the payer. Per CMS guidelines, the ROS and/or PFSH obtained during an earlier encounter does not need to be re-recorded if there is evidence that the physician reviewed and updated the previous information. The review and update may be documented by either describing any new ROS and/or PFSH information or noting that there has been no change in the information and noting the date and location of the earlier ROS and/or PFSH.2
Pre-op clearance and HPI deficiencies. HPI is typically not as deficient as the ROS or family history elements; however, HPI underdocumentation is mostly associated with encounters for pre-op clearance. The physician may state that “patient requires pre-op clearance for left knee repair.” In the absence of any comorbidities or acute illness, HPI documentation may be missing. The physician should remember to identify the details of the presenting problem: “Patient runs five miles daily. Knee felt unstable after running two weeks ago. Swelling and intermittent sharp pain 7/10. Patient has been taking ibuprofen daily without relief.”
Not medically necessary. Remember not to document any elements for the purpose of “getting paid.” Only document information that is clinically relevant, lends to the quality of care provided, or demonstrates the delivery of healthcare services. This prevents accusations of fraud and abuse, promotes billing compliance, and supports medical necessity for the services provided.
Varying levels of history. E/M services are selected based on the content of the three “key” components: history, exam, and decision-making (or visit time). If counseling and/or coordination of care does not encompass >50% of the physician’s total visit time or the service is not exclusively designated as a time-based service (e.g. critical care and discharge day management), the physician’s service time is not considered.
Documentation for each of the three key components must support the reported visit level when reporting initial hospital care and consultations (for those payers who still recognize consultation codes). Subsequent hospital care (e.g. 99233) only requires supportive documentation from two key components. Medical decision-making should be one of the two supporting components in order to demonstrate the medical necessity and nature of the presenting problem; the other supporting component can be history or exam.
Each visit category (e.g. initial hospital care or subsequent hospital care) and service level (e.g. 99221-99233) identifies corresponding documentation requirements. Failure to document any essential element in a given visit level (e.g. family history required for a comprehensive history when billing for 99222 and 99223) may result in service denial or downcoding (e.g. 99221). Be aware of what an auditor expects when reviewing patient history (see Table 1).
There are four levels of history: problem-focused, expanded problem-focused, detailed, and comprehensive. An auditor determines the number of history elements documented in the progress note (see Table 2). The history level corresponds to the lowest documented element. For example, if physician documentation includes four HPI elements, eight ROS, and a comment in each of the PFSHs, the history level is equivalent to “detailed.” The history would support initial hospital care 99221 or subsequent hospital care 99233.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Levinson DR. Department of Health and Human Services, Office of Inspector General: Coding Trends of Medicare Evaluation and Management Services. May 2012. Available at: oig.hhs.gov/oei/reports/oei-04-10-00180.pdf. Accessed October 4, 2014.
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/95Docguidelines.pdf. Accessed October 4, 2014.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis L. CPT 2013 Professional Edition (Current Procedural Terminology). Chicago: American Medical Association Press; 2012:4-10.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf. Accessed October 4, 2014.
- Noridian Healthcare Solutions. Medicare Part B: Evaluation and Management Workshop Questions and Answers. Available at: www.noridianmedicare.com/cgi-bin/coranto/viewnews.cgi?id=EkZpEVAyylqZyOfqel&tmpl=part_b_viewnews&style=part_ab_viewnews Accessed on October 4, 2014.
- WPS Medicare Health Insurance. J5 MAC Part B: Documentation (Q&As). Available at: www.wpsmedicare.com/j5macpartb/resources/provider_types/evalmngmntqa.shtml. Accessed October 4, 2014.
- NHIC, Corp. Building Your Medicare Knowledge: Advanced Building Blocks. Available at: www.medicarenhic.com/providers/pubs/AdvdBuildBlocks061212.pdf.
- Palmetto GBA. Jurisdiction 11 Part B: History Component. Available at: www.palmettogba.com/Palmetto/Providers.nsf/docsCat/Jurisdiction%2011%20Part%20B~EM%20Help%20Center~General%20Articles~History%20Component?open&Expand=1. Accessed October 4, 2014.
- Novitas Solutions. Frequently Asked Questions: Evaluation and Management Services (Part B). Available at: https://www.novitas-solutions.com/faq/partb/pet/lpet-evaluation_management_services.html. Accessed October 4, 2014.
Common Coding Mistakes Hospitalists Should Avoid
Medical decision-making (MDM) mistakes are common. Here are the coding and documentation mistakes hospitalists make most often, along with some tips on how to avoid them.
Listing the problem without a plan. Healthcare professionals are able to infer the acuity and severity of a case without superfluous or redundant documentation, but auditors may not have this ability. Adequate documentation for every service date helps to convey patient complexity during a medical record review. Although the problem list may not change dramatically from day to day during a hospitalization, the auditor only reviews the service date in question, not the entire medical record.
Hospitalists should be sure to formulate a complete and accurate description of the patient’s condition with an analogous plan of care for each encounter. Listing problems without a corresponding plan of care does not corroborate physician management of that problem and could cause a downgrade of complexity. Listing problems with a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) equally diminishes the complexity and effort put forth by the physician.
Clearly document the plan. The care plan represents problems the physician personally manages, along with those that must also be considered when he or she formulates the management options, even if another physician is primarily managing the problem. For example, the hospitalist can monitor the patient’s diabetic management while the nephrologist oversees the chronic kidney disease (CKD). Since the CKD impacts the hospitalist’s diabetic care plan, the hospitalist may also receive credit for any CKD consideration if the documentation supports a hospitalist-related care plan, or comment about CKD that does not overlap or replicate the nephrologist’s plan. In other words, there must be some “value-added” input by the hospitalist.
Credit is given for the quantity of problems addressed as well as the quality. For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization. Established problems are less complex than new problems, for which a diagnosis, prognosis, or care plan has not been developed. Severity of the problem also influences complexity. A “worsening” problem is considered more complex than an “improving” problem, since the worsening problem likely requires revisions to the current care plan and, thus, more physician effort. Physician documentation should always:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- Note management options to be continued somewhere in the progress note for that encounter (e.g. medication list) when documentation indicates a continuation of current management options (e.g. “continue meds”).
Considering relevant data. “Data” is organized as pathology/laboratory testing, radiology, and medicine-based diagnostic testing that contributes to diagnosing or managing patient problems. Pertinent orders or results may appear in the medical record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note, or make an entry that refers to another auditor-accessible location for ordered tests and studies; however, this latter option jeopardizes a medical record review due to potential lack of awareness of the need to submit this extraneous information during a payer record request or appeal.
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”); credit is not given for entries lacking a comment on the findings (e.g. “CXR reviewed”).
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary; be sure to identify the increased efforts of reviewing the considerable number of old records by stating, “OSH (outside hospital) records reviewed and shows…” or “Records from previous hospitalization(s) reveal….”
- Indicate when images, tracings, or specimens are “personally reviewed,” or the auditor will assume the physician merely reviewed the written report; be sure to include a comment on the findings.
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Data credit may be more substantial during the initial investigative phase of the hospitalization, before diagnoses or treatment options have been confirmed. Routine monitoring of the stabilized patient may not yield as many “points.”
Undervaluing the patient’s complexity. A general lack of understanding of the MDM component of the documentation guidelines often results in physicians undervaluing their services. Some physicians may consider a case “low complexity” simply because of the frequency with which they encounter the case type. The speed with which the care plan is developed should have no bearing on how complex the patient’s condition really is. Hospitalists need to better identify the risk involved for the patient.
Patient risk is categorized as minimal, low, moderate, or high based on pre-assigned items pertaining to the presenting problem, diagnostic procedures ordered, and management options selected. The single highest-rated item detected on the Table of Risk determines the overall patient risk for an encounter.1 Chronic conditions with exacerbations and invasive procedures offer more patient risk than acute, uncomplicated illnesses or noninvasive procedures. Stable or improving problems are considered “less risky” than progressing problems; conditions that pose a threat to life/bodily function outweigh undiagnosed problems where it is difficult to determine the patient’s prognosis; and medication risk varies with the administration (e.g. oral vs. parenteral), type, and potential for adverse effects. Medication risk for a particular drug is invariable whether the dosage is increased, decreased, or continued without change. Physicians should:
- Provide status for all problems in the plan of care and identify them as stable, worsening, or progressing (mild or severe), when applicable; don’t assume that the auditor can infer this from the documentation details.
- Document all diagnostic or therapeutic procedures considered.
- Identify surgical risk factors involving co-morbid conditions that place the patient at greater risk than the average patient, when appropriate.
- Associate the labs ordered to monitor for medication toxicity with the corresponding medication; don’t assume that the auditor knows which labs are used to check for toxicity.
Varying levels of complexity. Remember that decision-making is just one of three components in evaluation and management (E&M) services, along with history and exam. MDM is identical for both the 1995 and 1997 guidelines, rooted in the complexity of the patient’s problem(s) addressed during a given encounter.1,2 Complexity is categorized as straightforward, low, moderate, or high, and directly correlates to the content of physician documentation.
Each visit level represents a particular level of complexity (see Table 1). Auditors only consider the care plan for a given service date when reviewing MDM. More specifically, the auditor reviews three areas of MDM for each encounter (see Table 2), and the physician receives credit for: a) the number of diagnoses and/or treatment options; b) the amount and/or complexity of data ordered/reviewed; c) the risk of complications/morbidity/mortality.
To determine MDM complexity, each MDM category is assigned a point level. Complexity correlates to the second-highest MDM category. For example, if the auditor assigns “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician attains moderate complexity decision-making (see Table 3).
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/95Docguidelines.pdf. Accessed July 7, 2014.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation and Management Services. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf. Accessed July 7, 2014.
- American Medical Association. Current Procedural Terminology: 2014 Professional Edition. Chicago: American Medical Association; 2013:14-21.
- Novitas Solutions. Novitas Solutions documentation worksheet. Available at: www.novitas-solutions.com/webcenter/content/conn/UCM_Repository/uuid/dDocName:00004966. Accessed July 7, 2014.
Medical decision-making (MDM) mistakes are common. Here are the coding and documentation mistakes hospitalists make most often, along with some tips on how to avoid them.
Listing the problem without a plan. Healthcare professionals are able to infer the acuity and severity of a case without superfluous or redundant documentation, but auditors may not have this ability. Adequate documentation for every service date helps to convey patient complexity during a medical record review. Although the problem list may not change dramatically from day to day during a hospitalization, the auditor only reviews the service date in question, not the entire medical record.
Hospitalists should be sure to formulate a complete and accurate description of the patient’s condition with an analogous plan of care for each encounter. Listing problems without a corresponding plan of care does not corroborate physician management of that problem and could cause a downgrade of complexity. Listing problems with a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) equally diminishes the complexity and effort put forth by the physician.
Clearly document the plan. The care plan represents problems the physician personally manages, along with those that must also be considered when he or she formulates the management options, even if another physician is primarily managing the problem. For example, the hospitalist can monitor the patient’s diabetic management while the nephrologist oversees the chronic kidney disease (CKD). Since the CKD impacts the hospitalist’s diabetic care plan, the hospitalist may also receive credit for any CKD consideration if the documentation supports a hospitalist-related care plan, or comment about CKD that does not overlap or replicate the nephrologist’s plan. In other words, there must be some “value-added” input by the hospitalist.
Credit is given for the quantity of problems addressed as well as the quality. For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization. Established problems are less complex than new problems, for which a diagnosis, prognosis, or care plan has not been developed. Severity of the problem also influences complexity. A “worsening” problem is considered more complex than an “improving” problem, since the worsening problem likely requires revisions to the current care plan and, thus, more physician effort. Physician documentation should always:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- Note management options to be continued somewhere in the progress note for that encounter (e.g. medication list) when documentation indicates a continuation of current management options (e.g. “continue meds”).
Considering relevant data. “Data” is organized as pathology/laboratory testing, radiology, and medicine-based diagnostic testing that contributes to diagnosing or managing patient problems. Pertinent orders or results may appear in the medical record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note, or make an entry that refers to another auditor-accessible location for ordered tests and studies; however, this latter option jeopardizes a medical record review due to potential lack of awareness of the need to submit this extraneous information during a payer record request or appeal.
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”); credit is not given for entries lacking a comment on the findings (e.g. “CXR reviewed”).
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary; be sure to identify the increased efforts of reviewing the considerable number of old records by stating, “OSH (outside hospital) records reviewed and shows…” or “Records from previous hospitalization(s) reveal….”
- Indicate when images, tracings, or specimens are “personally reviewed,” or the auditor will assume the physician merely reviewed the written report; be sure to include a comment on the findings.
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Data credit may be more substantial during the initial investigative phase of the hospitalization, before diagnoses or treatment options have been confirmed. Routine monitoring of the stabilized patient may not yield as many “points.”
Undervaluing the patient’s complexity. A general lack of understanding of the MDM component of the documentation guidelines often results in physicians undervaluing their services. Some physicians may consider a case “low complexity” simply because of the frequency with which they encounter the case type. The speed with which the care plan is developed should have no bearing on how complex the patient’s condition really is. Hospitalists need to better identify the risk involved for the patient.
Patient risk is categorized as minimal, low, moderate, or high based on pre-assigned items pertaining to the presenting problem, diagnostic procedures ordered, and management options selected. The single highest-rated item detected on the Table of Risk determines the overall patient risk for an encounter.1 Chronic conditions with exacerbations and invasive procedures offer more patient risk than acute, uncomplicated illnesses or noninvasive procedures. Stable or improving problems are considered “less risky” than progressing problems; conditions that pose a threat to life/bodily function outweigh undiagnosed problems where it is difficult to determine the patient’s prognosis; and medication risk varies with the administration (e.g. oral vs. parenteral), type, and potential for adverse effects. Medication risk for a particular drug is invariable whether the dosage is increased, decreased, or continued without change. Physicians should:
- Provide status for all problems in the plan of care and identify them as stable, worsening, or progressing (mild or severe), when applicable; don’t assume that the auditor can infer this from the documentation details.
- Document all diagnostic or therapeutic procedures considered.
- Identify surgical risk factors involving co-morbid conditions that place the patient at greater risk than the average patient, when appropriate.
- Associate the labs ordered to monitor for medication toxicity with the corresponding medication; don’t assume that the auditor knows which labs are used to check for toxicity.
Varying levels of complexity. Remember that decision-making is just one of three components in evaluation and management (E&M) services, along with history and exam. MDM is identical for both the 1995 and 1997 guidelines, rooted in the complexity of the patient’s problem(s) addressed during a given encounter.1,2 Complexity is categorized as straightforward, low, moderate, or high, and directly correlates to the content of physician documentation.
Each visit level represents a particular level of complexity (see Table 1). Auditors only consider the care plan for a given service date when reviewing MDM. More specifically, the auditor reviews three areas of MDM for each encounter (see Table 2), and the physician receives credit for: a) the number of diagnoses and/or treatment options; b) the amount and/or complexity of data ordered/reviewed; c) the risk of complications/morbidity/mortality.
To determine MDM complexity, each MDM category is assigned a point level. Complexity correlates to the second-highest MDM category. For example, if the auditor assigns “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician attains moderate complexity decision-making (see Table 3).
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/95Docguidelines.pdf. Accessed July 7, 2014.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation and Management Services. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf. Accessed July 7, 2014.
- American Medical Association. Current Procedural Terminology: 2014 Professional Edition. Chicago: American Medical Association; 2013:14-21.
- Novitas Solutions. Novitas Solutions documentation worksheet. Available at: www.novitas-solutions.com/webcenter/content/conn/UCM_Repository/uuid/dDocName:00004966. Accessed July 7, 2014.
Medical decision-making (MDM) mistakes are common. Here are the coding and documentation mistakes hospitalists make most often, along with some tips on how to avoid them.
Listing the problem without a plan. Healthcare professionals are able to infer the acuity and severity of a case without superfluous or redundant documentation, but auditors may not have this ability. Adequate documentation for every service date helps to convey patient complexity during a medical record review. Although the problem list may not change dramatically from day to day during a hospitalization, the auditor only reviews the service date in question, not the entire medical record.
Hospitalists should be sure to formulate a complete and accurate description of the patient’s condition with an analogous plan of care for each encounter. Listing problems without a corresponding plan of care does not corroborate physician management of that problem and could cause a downgrade of complexity. Listing problems with a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) equally diminishes the complexity and effort put forth by the physician.
Clearly document the plan. The care plan represents problems the physician personally manages, along with those that must also be considered when he or she formulates the management options, even if another physician is primarily managing the problem. For example, the hospitalist can monitor the patient’s diabetic management while the nephrologist oversees the chronic kidney disease (CKD). Since the CKD impacts the hospitalist’s diabetic care plan, the hospitalist may also receive credit for any CKD consideration if the documentation supports a hospitalist-related care plan, or comment about CKD that does not overlap or replicate the nephrologist’s plan. In other words, there must be some “value-added” input by the hospitalist.
Credit is given for the quantity of problems addressed as well as the quality. For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization. Established problems are less complex than new problems, for which a diagnosis, prognosis, or care plan has not been developed. Severity of the problem also influences complexity. A “worsening” problem is considered more complex than an “improving” problem, since the worsening problem likely requires revisions to the current care plan and, thus, more physician effort. Physician documentation should always:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- Note management options to be continued somewhere in the progress note for that encounter (e.g. medication list) when documentation indicates a continuation of current management options (e.g. “continue meds”).
Considering relevant data. “Data” is organized as pathology/laboratory testing, radiology, and medicine-based diagnostic testing that contributes to diagnosing or managing patient problems. Pertinent orders or results may appear in the medical record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note, or make an entry that refers to another auditor-accessible location for ordered tests and studies; however, this latter option jeopardizes a medical record review due to potential lack of awareness of the need to submit this extraneous information during a payer record request or appeal.
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”); credit is not given for entries lacking a comment on the findings (e.g. “CXR reviewed”).
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary; be sure to identify the increased efforts of reviewing the considerable number of old records by stating, “OSH (outside hospital) records reviewed and shows…” or “Records from previous hospitalization(s) reveal….”
- Indicate when images, tracings, or specimens are “personally reviewed,” or the auditor will assume the physician merely reviewed the written report; be sure to include a comment on the findings.
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Data credit may be more substantial during the initial investigative phase of the hospitalization, before diagnoses or treatment options have been confirmed. Routine monitoring of the stabilized patient may not yield as many “points.”
Undervaluing the patient’s complexity. A general lack of understanding of the MDM component of the documentation guidelines often results in physicians undervaluing their services. Some physicians may consider a case “low complexity” simply because of the frequency with which they encounter the case type. The speed with which the care plan is developed should have no bearing on how complex the patient’s condition really is. Hospitalists need to better identify the risk involved for the patient.
Patient risk is categorized as minimal, low, moderate, or high based on pre-assigned items pertaining to the presenting problem, diagnostic procedures ordered, and management options selected. The single highest-rated item detected on the Table of Risk determines the overall patient risk for an encounter.1 Chronic conditions with exacerbations and invasive procedures offer more patient risk than acute, uncomplicated illnesses or noninvasive procedures. Stable or improving problems are considered “less risky” than progressing problems; conditions that pose a threat to life/bodily function outweigh undiagnosed problems where it is difficult to determine the patient’s prognosis; and medication risk varies with the administration (e.g. oral vs. parenteral), type, and potential for adverse effects. Medication risk for a particular drug is invariable whether the dosage is increased, decreased, or continued without change. Physicians should:
- Provide status for all problems in the plan of care and identify them as stable, worsening, or progressing (mild or severe), when applicable; don’t assume that the auditor can infer this from the documentation details.
- Document all diagnostic or therapeutic procedures considered.
- Identify surgical risk factors involving co-morbid conditions that place the patient at greater risk than the average patient, when appropriate.
- Associate the labs ordered to monitor for medication toxicity with the corresponding medication; don’t assume that the auditor knows which labs are used to check for toxicity.
Varying levels of complexity. Remember that decision-making is just one of three components in evaluation and management (E&M) services, along with history and exam. MDM is identical for both the 1995 and 1997 guidelines, rooted in the complexity of the patient’s problem(s) addressed during a given encounter.1,2 Complexity is categorized as straightforward, low, moderate, or high, and directly correlates to the content of physician documentation.
Each visit level represents a particular level of complexity (see Table 1). Auditors only consider the care plan for a given service date when reviewing MDM. More specifically, the auditor reviews three areas of MDM for each encounter (see Table 2), and the physician receives credit for: a) the number of diagnoses and/or treatment options; b) the amount and/or complexity of data ordered/reviewed; c) the risk of complications/morbidity/mortality.
To determine MDM complexity, each MDM category is assigned a point level. Complexity correlates to the second-highest MDM category. For example, if the auditor assigns “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician attains moderate complexity decision-making (see Table 3).
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/95Docguidelines.pdf. Accessed July 7, 2014.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation and Management Services. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf. Accessed July 7, 2014.
- American Medical Association. Current Procedural Terminology: 2014 Professional Edition. Chicago: American Medical Association; 2013:14-21.
- Novitas Solutions. Novitas Solutions documentation worksheet. Available at: www.novitas-solutions.com/webcenter/content/conn/UCM_Repository/uuid/dDocName:00004966. Accessed July 7, 2014.
Medical Decision-Making: Avoid These Common Coding & Documentation Mistakes
Medical decision-making (MDM) mistakes are common. Here are the coding and documentation mistakes hospitalists make most often, along with some tips on how to avoid them.
Listing the problem without a plan. Healthcare professionals are able to infer the acuity and severity of a case without superfluous or redundant documentation, but auditors may not have this ability. Adequate documentation for every service date helps to convey patient complexity during a medical record review. Although the problem list may not change dramatically from day to day during a hospitalization, the auditor only reviews the service date in question, not the entire medical record.
Hospitalists should be sure to formulate a complete and accurate description of the patient’s condition with an analogous plan of care for each encounter. Listing problems without a corresponding plan of care does not corroborate physician management of that problem and could cause a downgrade of complexity. Listing problems with a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) equally diminishes the complexity and effort put forth by the physician.
Clearly document the plan. The care plan represents problems the physician personally manages, along with those that must also be considered when he or she formulates the management options, even if another physician is primarily managing the problem. For example, the hospitalist can monitor the patient’s diabetic management while the nephrologist oversees the chronic kidney disease (CKD). Since the CKD impacts the hospitalist’s diabetic care plan, the hospitalist may also receive credit for any CKD consideration if the documentation supports a hospitalist-related care plan, or comment about CKD that does not overlap or replicate the nephrologist’s plan. In other words, there must be some “value-added” input by the hospitalist.
Credit is given for the quantity of problems addressed as well as the quality. For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization. Established problems are less complex than new problems, for which a diagnosis, prognosis, or care plan has not been developed. Severity of the problem also influences complexity. A “worsening” problem is considered more complex than an “improving” problem, since the worsening problem likely requires revisions to the current care plan and, thus, more physician effort. Physician documentation should always:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- Note management options to be continued somewhere in the progress note for that encounter (e.g. medication list) when documentation indicates a continuation of current management options (e.g. “continue meds”).
Considering relevant data. “Data” is organized as pathology/laboratory testing, radiology, and medicine-based diagnostic testing that contributes to diagnosing or managing patient problems. Pertinent orders or results may appear in the medical record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note, or make an entry that refers to another auditor-accessible location for ordered tests and studies; however, this latter option jeopardizes a medical record review due to potential lack of awareness of the need to submit this extraneous information during a payer record request or appeal.
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”); credit is not given for entries lacking a comment on the findings (e.g. “CXR reviewed”).
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary; be sure to identify the increased efforts of reviewing the considerable number of old records by stating, “OSH (outside hospital) records reviewed and shows…” or “Records from previous hospitalization(s) reveal….”
- Indicate when images, tracings, or specimens are “personally reviewed,” or the auditor will assume the physician merely reviewed the written report; be sure to include a comment on the findings.
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Data credit may be more substantial during the initial investigative phase of the hospitalization, before diagnoses or treatment options have been confirmed. Routine monitoring of the stabilized patient may not yield as many “points.”
Undervaluing the patient’s complexity. A general lack of understanding of the MDM component of the documentation guidelines often results in physicians undervaluing their services. Some physicians may consider a case “low complexity” simply because of the frequency with which they encounter the case type. The speed with which the care plan is developed should have no bearing on how complex the patient’s condition really is. Hospitalists need to better identify the risk involved for the patient.
Patient risk is categorized as minimal, low, moderate, or high based on pre-assigned items pertaining to the presenting problem, diagnostic procedures ordered, and management options selected. The single highest-rated item detected on the Table of Risk determines the overall patient risk for an encounter.1 Chronic conditions with exacerbations and invasive procedures offer more patient risk than acute, uncomplicated illnesses or noninvasive procedures. Stable or improving problems are considered “less risky” than progressing problems; conditions that pose a threat to life/bodily function outweigh undiagnosed problems where it is difficult to determine the patient’s prognosis; and medication risk varies with the administration (e.g. oral vs. parenteral), type, and potential for adverse effects. Medication risk for a particular drug is invariable whether the dosage is increased, decreased, or continued without change. Physicians should:
- Provide status for all problems in the plan of care and identify them as stable, worsening, or progressing (mild or severe), when applicable; don’t assume that the auditor can infer this from the documentation details.
- Document all diagnostic or therapeutic procedures considered.
- Identify surgical risk factors involving co-morbid conditions that place the patient at greater risk than the average patient, when appropriate.
- Associate the labs ordered to monitor for medication toxicity with the corresponding medication; don’t assume that the auditor knows which labs are used to check for toxicity.
Varying levels of complexity. Remember that decision-making is just one of three components in evaluation and management (E&M) services, along with history and exam. MDM is identical for both the 1995 and 1997 guidelines, rooted in the complexity of the patient’s problem(s) addressed during a given encounter.1,2 Complexity is categorized as straightforward, low, moderate, or high, and directly correlates to the content of physician documentation.
Each visit level represents a particular level of complexity (see Table 1). Auditors only consider the care plan for a given service date when reviewing MDM. More specifically, the auditor reviews three areas of MDM for each encounter (see Table 2), and the physician receives credit for: a) the number of diagnoses and/or treatment options; b) the amount and/or complexity of data ordered/reviewed; c) the risk of complications/morbidity/mortality.
To determine MDM complexity, each MDM category is assigned a point level. Complexity correlates to the second-highest MDM category. For example, if the auditor assigns “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician attains moderate complexity decision-making (see Table 3).
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/95Docguidelines.pdf. Accessed July 7, 2014.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation and Management Services. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf. Accessed July 7, 2014.
- American Medical Association. Current Procedural Terminology: 2014 Professional Edition. Chicago: American Medical Association; 2013:14-21.
- Novitas Solutions. Novitas Solutions documentation worksheet. Available at: www.novitas-solutions.com/webcenter/content/conn/UCM_Repository/uuid/dDocName:00004966. Accessed July 7, 2014.
Medical decision-making (MDM) mistakes are common. Here are the coding and documentation mistakes hospitalists make most often, along with some tips on how to avoid them.
Listing the problem without a plan. Healthcare professionals are able to infer the acuity and severity of a case without superfluous or redundant documentation, but auditors may not have this ability. Adequate documentation for every service date helps to convey patient complexity during a medical record review. Although the problem list may not change dramatically from day to day during a hospitalization, the auditor only reviews the service date in question, not the entire medical record.
Hospitalists should be sure to formulate a complete and accurate description of the patient’s condition with an analogous plan of care for each encounter. Listing problems without a corresponding plan of care does not corroborate physician management of that problem and could cause a downgrade of complexity. Listing problems with a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) equally diminishes the complexity and effort put forth by the physician.
Clearly document the plan. The care plan represents problems the physician personally manages, along with those that must also be considered when he or she formulates the management options, even if another physician is primarily managing the problem. For example, the hospitalist can monitor the patient’s diabetic management while the nephrologist oversees the chronic kidney disease (CKD). Since the CKD impacts the hospitalist’s diabetic care plan, the hospitalist may also receive credit for any CKD consideration if the documentation supports a hospitalist-related care plan, or comment about CKD that does not overlap or replicate the nephrologist’s plan. In other words, there must be some “value-added” input by the hospitalist.
Credit is given for the quantity of problems addressed as well as the quality. For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization. Established problems are less complex than new problems, for which a diagnosis, prognosis, or care plan has not been developed. Severity of the problem also influences complexity. A “worsening” problem is considered more complex than an “improving” problem, since the worsening problem likely requires revisions to the current care plan and, thus, more physician effort. Physician documentation should always:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- Note management options to be continued somewhere in the progress note for that encounter (e.g. medication list) when documentation indicates a continuation of current management options (e.g. “continue meds”).
Considering relevant data. “Data” is organized as pathology/laboratory testing, radiology, and medicine-based diagnostic testing that contributes to diagnosing or managing patient problems. Pertinent orders or results may appear in the medical record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note, or make an entry that refers to another auditor-accessible location for ordered tests and studies; however, this latter option jeopardizes a medical record review due to potential lack of awareness of the need to submit this extraneous information during a payer record request or appeal.
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”); credit is not given for entries lacking a comment on the findings (e.g. “CXR reviewed”).
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary; be sure to identify the increased efforts of reviewing the considerable number of old records by stating, “OSH (outside hospital) records reviewed and shows…” or “Records from previous hospitalization(s) reveal….”
- Indicate when images, tracings, or specimens are “personally reviewed,” or the auditor will assume the physician merely reviewed the written report; be sure to include a comment on the findings.
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Data credit may be more substantial during the initial investigative phase of the hospitalization, before diagnoses or treatment options have been confirmed. Routine monitoring of the stabilized patient may not yield as many “points.”
Undervaluing the patient’s complexity. A general lack of understanding of the MDM component of the documentation guidelines often results in physicians undervaluing their services. Some physicians may consider a case “low complexity” simply because of the frequency with which they encounter the case type. The speed with which the care plan is developed should have no bearing on how complex the patient’s condition really is. Hospitalists need to better identify the risk involved for the patient.
Patient risk is categorized as minimal, low, moderate, or high based on pre-assigned items pertaining to the presenting problem, diagnostic procedures ordered, and management options selected. The single highest-rated item detected on the Table of Risk determines the overall patient risk for an encounter.1 Chronic conditions with exacerbations and invasive procedures offer more patient risk than acute, uncomplicated illnesses or noninvasive procedures. Stable or improving problems are considered “less risky” than progressing problems; conditions that pose a threat to life/bodily function outweigh undiagnosed problems where it is difficult to determine the patient’s prognosis; and medication risk varies with the administration (e.g. oral vs. parenteral), type, and potential for adverse effects. Medication risk for a particular drug is invariable whether the dosage is increased, decreased, or continued without change. Physicians should:
- Provide status for all problems in the plan of care and identify them as stable, worsening, or progressing (mild or severe), when applicable; don’t assume that the auditor can infer this from the documentation details.
- Document all diagnostic or therapeutic procedures considered.
- Identify surgical risk factors involving co-morbid conditions that place the patient at greater risk than the average patient, when appropriate.
- Associate the labs ordered to monitor for medication toxicity with the corresponding medication; don’t assume that the auditor knows which labs are used to check for toxicity.
Varying levels of complexity. Remember that decision-making is just one of three components in evaluation and management (E&M) services, along with history and exam. MDM is identical for both the 1995 and 1997 guidelines, rooted in the complexity of the patient’s problem(s) addressed during a given encounter.1,2 Complexity is categorized as straightforward, low, moderate, or high, and directly correlates to the content of physician documentation.
Each visit level represents a particular level of complexity (see Table 1). Auditors only consider the care plan for a given service date when reviewing MDM. More specifically, the auditor reviews three areas of MDM for each encounter (see Table 2), and the physician receives credit for: a) the number of diagnoses and/or treatment options; b) the amount and/or complexity of data ordered/reviewed; c) the risk of complications/morbidity/mortality.
To determine MDM complexity, each MDM category is assigned a point level. Complexity correlates to the second-highest MDM category. For example, if the auditor assigns “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician attains moderate complexity decision-making (see Table 3).
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/95Docguidelines.pdf. Accessed July 7, 2014.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation and Management Services. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf. Accessed July 7, 2014.
- American Medical Association. Current Procedural Terminology: 2014 Professional Edition. Chicago: American Medical Association; 2013:14-21.
- Novitas Solutions. Novitas Solutions documentation worksheet. Available at: www.novitas-solutions.com/webcenter/content/conn/UCM_Repository/uuid/dDocName:00004966. Accessed July 7, 2014.
Medical decision-making (MDM) mistakes are common. Here are the coding and documentation mistakes hospitalists make most often, along with some tips on how to avoid them.
Listing the problem without a plan. Healthcare professionals are able to infer the acuity and severity of a case without superfluous or redundant documentation, but auditors may not have this ability. Adequate documentation for every service date helps to convey patient complexity during a medical record review. Although the problem list may not change dramatically from day to day during a hospitalization, the auditor only reviews the service date in question, not the entire medical record.
Hospitalists should be sure to formulate a complete and accurate description of the patient’s condition with an analogous plan of care for each encounter. Listing problems without a corresponding plan of care does not corroborate physician management of that problem and could cause a downgrade of complexity. Listing problems with a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) equally diminishes the complexity and effort put forth by the physician.
Clearly document the plan. The care plan represents problems the physician personally manages, along with those that must also be considered when he or she formulates the management options, even if another physician is primarily managing the problem. For example, the hospitalist can monitor the patient’s diabetic management while the nephrologist oversees the chronic kidney disease (CKD). Since the CKD impacts the hospitalist’s diabetic care plan, the hospitalist may also receive credit for any CKD consideration if the documentation supports a hospitalist-related care plan, or comment about CKD that does not overlap or replicate the nephrologist’s plan. In other words, there must be some “value-added” input by the hospitalist.
Credit is given for the quantity of problems addressed as well as the quality. For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization. Established problems are less complex than new problems, for which a diagnosis, prognosis, or care plan has not been developed. Severity of the problem also influences complexity. A “worsening” problem is considered more complex than an “improving” problem, since the worsening problem likely requires revisions to the current care plan and, thus, more physician effort. Physician documentation should always:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- Note management options to be continued somewhere in the progress note for that encounter (e.g. medication list) when documentation indicates a continuation of current management options (e.g. “continue meds”).
Considering relevant data. “Data” is organized as pathology/laboratory testing, radiology, and medicine-based diagnostic testing that contributes to diagnosing or managing patient problems. Pertinent orders or results may appear in the medical record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note, or make an entry that refers to another auditor-accessible location for ordered tests and studies; however, this latter option jeopardizes a medical record review due to potential lack of awareness of the need to submit this extraneous information during a payer record request or appeal.
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”); credit is not given for entries lacking a comment on the findings (e.g. “CXR reviewed”).
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary; be sure to identify the increased efforts of reviewing the considerable number of old records by stating, “OSH (outside hospital) records reviewed and shows…” or “Records from previous hospitalization(s) reveal….”
- Indicate when images, tracings, or specimens are “personally reviewed,” or the auditor will assume the physician merely reviewed the written report; be sure to include a comment on the findings.
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Data credit may be more substantial during the initial investigative phase of the hospitalization, before diagnoses or treatment options have been confirmed. Routine monitoring of the stabilized patient may not yield as many “points.”
Undervaluing the patient’s complexity. A general lack of understanding of the MDM component of the documentation guidelines often results in physicians undervaluing their services. Some physicians may consider a case “low complexity” simply because of the frequency with which they encounter the case type. The speed with which the care plan is developed should have no bearing on how complex the patient’s condition really is. Hospitalists need to better identify the risk involved for the patient.
Patient risk is categorized as minimal, low, moderate, or high based on pre-assigned items pertaining to the presenting problem, diagnostic procedures ordered, and management options selected. The single highest-rated item detected on the Table of Risk determines the overall patient risk for an encounter.1 Chronic conditions with exacerbations and invasive procedures offer more patient risk than acute, uncomplicated illnesses or noninvasive procedures. Stable or improving problems are considered “less risky” than progressing problems; conditions that pose a threat to life/bodily function outweigh undiagnosed problems where it is difficult to determine the patient’s prognosis; and medication risk varies with the administration (e.g. oral vs. parenteral), type, and potential for adverse effects. Medication risk for a particular drug is invariable whether the dosage is increased, decreased, or continued without change. Physicians should:
- Provide status for all problems in the plan of care and identify them as stable, worsening, or progressing (mild or severe), when applicable; don’t assume that the auditor can infer this from the documentation details.
- Document all diagnostic or therapeutic procedures considered.
- Identify surgical risk factors involving co-morbid conditions that place the patient at greater risk than the average patient, when appropriate.
- Associate the labs ordered to monitor for medication toxicity with the corresponding medication; don’t assume that the auditor knows which labs are used to check for toxicity.
Varying levels of complexity. Remember that decision-making is just one of three components in evaluation and management (E&M) services, along with history and exam. MDM is identical for both the 1995 and 1997 guidelines, rooted in the complexity of the patient’s problem(s) addressed during a given encounter.1,2 Complexity is categorized as straightforward, low, moderate, or high, and directly correlates to the content of physician documentation.
Each visit level represents a particular level of complexity (see Table 1). Auditors only consider the care plan for a given service date when reviewing MDM. More specifically, the auditor reviews three areas of MDM for each encounter (see Table 2), and the physician receives credit for: a) the number of diagnoses and/or treatment options; b) the amount and/or complexity of data ordered/reviewed; c) the risk of complications/morbidity/mortality.
To determine MDM complexity, each MDM category is assigned a point level. Complexity correlates to the second-highest MDM category. For example, if the auditor assigns “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician attains moderate complexity decision-making (see Table 3).
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/95Docguidelines.pdf. Accessed July 7, 2014.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation and Management Services. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf. Accessed July 7, 2014.
- American Medical Association. Current Procedural Terminology: 2014 Professional Edition. Chicago: American Medical Association; 2013:14-21.
- Novitas Solutions. Novitas Solutions documentation worksheet. Available at: www.novitas-solutions.com/webcenter/content/conn/UCM_Repository/uuid/dDocName:00004966. Accessed July 7, 2014.