User login
MANCHESTER, U.K. – Multiple joint and skin benefits can be achieved by intensively treating patients with psoriatic arthritis until they achieve a set of minimal disease activity criteria, an expert said at the British Society for Rheumatology annual conference.
While data are mounting on the value of treating to target (otherwise known as tight control) in psoriatic arthritis (PsA), these data lag significantly behind that for inducing and maintaining remission in rheumatoid arthritis (RA), noted Dr. Philip Helliwell of the University of Leeds (England).
“There is half as much evidence in PsA as there is in rheumatoid arthritis,” he observed. “But we’ve also got a heterogeneous disease and what we are going to have to do moving forward is to find out how to treat different phenotypic expressions of psoriatic disease, and we’re beginning to work towards that now,” he said during a Special Interest Group on Spondyloarthropathies.
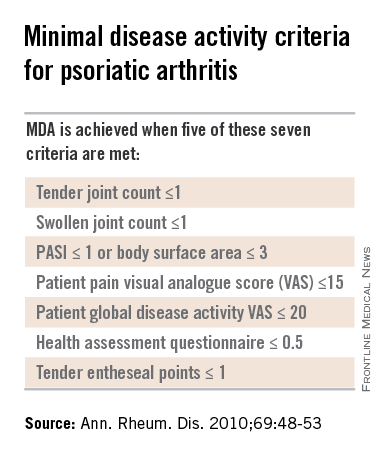
Dr. Helliwell is the principal investigator of the Tight Control of Psoriatic Arthritis (TICOPA) study, which he highlighted as an example of how targeting treatment to achieve minimal disease activity (MDA) criteria (Ann. Rheum. Dis. 2010;69:48-53) could be beneficial versus standard care.
A total of 206 patients with newly-diagnosed PsA were enrolled into the study and were randomized to receive either ‘tight control’ – meaning an intensive management strategy – or to standard care for 48 weeks.
Intensive treatment involved starting with methotrexate at a dose of 15 mg/kg per week and rapidly escalating to 25 mg/kg per week at 6 weeks if needed. If patients did not achieve five out of a set of seven MDA criteria for PsA, then methotrexate was continued and sulfasalazine was added and dose escalated after 4-8 weeks.
If MDA was still not achieved and criteria for biologics were not met according to NICE guidance, then alternatives were swapping out sulfasalazine for cyclosporine or leflunomide, again increasing the doses. Patients who did get put onto a biologic could switch to another anti-TNF if they did not respond after 12 weeks.
The primary endpoint data from the trial have been reported previously and showed that a higher proportion of patients in the intensive management group achieved ACR20 at 48 weeks, compared with those in the standard care group (62% vs. 45%, respectively; P = .02). A higher percentage of intensively managed patients also achieved ACR50 (51% vs. 25%; P = .0004) and ACR70 (38% vs. 17%, P = .002).
Skin symptoms, measured via the Psoriasis Area and Severity Index (PASI) showed significant improvement favoring intensive therapy over standard care. PASI20 was achieved by 72% of intensively managed patients versus 52% of those who received standard care. PASI75 was achieved by 59% versus 33%, respectively, and PASI90 by 40% versus 20%, respectively.
The full results of the study will be published soon in The Lancet and will include details of a variety of secondary outcomes and the cost-effectiveness of the intensive management strategy versus the standard care approach.
One of the key secondary outcomes of the trial was to look at the effects of the two treatment strategies on other PsA symptoms, such as enthesitis, dactylitis, and nail symptoms. No differences between the groups were observed, however, with similar decreases seen in the tight control and standard care groups.
There were no statistically significant differences in radiologic outcomes, which included baseline and end-of-treatment changes in the total modified Sharp van der Heijde (SVdH) score, the erosion score, and joint-space narrowing (JSN) score.
While this might seem somewhat disappointing, “there wasn’t a lot of radiologic progression going on anyway,” Dr. Helliwell pointed out. Overall, there was a difference of about 5% in the percentage of patients with at least one joint erosion at baseline and after 48 weeks of treatment.
The majority of radiographic change that did occur was JSN of the hands, Dr. Helliwell said, adding that patients with JSN tended to be slightly older than those without, although this observation did not reach statistical significance.
“We’ve since looked for associations with ACPA [anticitrullinated protein antibodies] – about 7% of our patients were ACPA positive – but there is no relationship,” he added. There was also no significant association between levels of C-reactive protein levels and erosive disease.
There was a trend suggesting that patients with erosions may be more likely to have polyarticular disease than oligoarticular disease, so a next step would be to look at radiologic progression in these two groups of patients in more detail.
More adverse events were seen in the tight control arm, compared with the standard care arm, including more serious adverse events, but not all of these were related to study treatment and many adverse events were those to be expected with methotrexate treatment, Dr. Helliwell observed.
But is the intensive approach cost-effective when compared to standard care? Data suggest that it is. Although the incremental cost-effectiveness ratio (ICER) initially exceeded the £20,000–£30,000 (about $31,000-$47,000) threshold used by the U.K. National Institute for Health and Care Excellence to judge if a new treatment is cost effective, allowing for certain factors enabled the ICER to be brought down to about £28,000 ($44,000), making it a cost-effective strategy.
PsA consists of five classical subtypes. The most common of these subtypes is polyarthritis (60% of patients), followed by oligoarthritis (30%). The remaining 10% of patients comprise those with arthritis mutilans, distal interphalangeal predominant disease, or spinal predominant disease. The clinical features of dactylitis and enthesitis are prevalent in about 40% and 50% of patients, respectively, and can occur in any subgroup.
Considering such heterogeneity in its presentation, the challenge now will be to determine if all clinical subgroups of PsA could benefit from treating to an MDA target with intensive management, or if one or other subgroups benefit more than another.
The TICOPA study was funded by Arthritis Research UK with support from Pfizer. Dr. Helliwell has received consulting fees from Pfizer.
Results of this study were published in the Lancet Sept. 30, 2015.
This article was updated October 6, 2015.
MANCHESTER, U.K. – Multiple joint and skin benefits can be achieved by intensively treating patients with psoriatic arthritis until they achieve a set of minimal disease activity criteria, an expert said at the British Society for Rheumatology annual conference.
While data are mounting on the value of treating to target (otherwise known as tight control) in psoriatic arthritis (PsA), these data lag significantly behind that for inducing and maintaining remission in rheumatoid arthritis (RA), noted Dr. Philip Helliwell of the University of Leeds (England).
“There is half as much evidence in PsA as there is in rheumatoid arthritis,” he observed. “But we’ve also got a heterogeneous disease and what we are going to have to do moving forward is to find out how to treat different phenotypic expressions of psoriatic disease, and we’re beginning to work towards that now,” he said during a Special Interest Group on Spondyloarthropathies.
Dr. Helliwell is the principal investigator of the Tight Control of Psoriatic Arthritis (TICOPA) study, which he highlighted as an example of how targeting treatment to achieve minimal disease activity (MDA) criteria (Ann. Rheum. Dis. 2010;69:48-53) could be beneficial versus standard care.
A total of 206 patients with newly-diagnosed PsA were enrolled into the study and were randomized to receive either ‘tight control’ – meaning an intensive management strategy – or to standard care for 48 weeks.
Intensive treatment involved starting with methotrexate at a dose of 15 mg/kg per week and rapidly escalating to 25 mg/kg per week at 6 weeks if needed. If patients did not achieve five out of a set of seven MDA criteria for PsA, then methotrexate was continued and sulfasalazine was added and dose escalated after 4-8 weeks.
If MDA was still not achieved and criteria for biologics were not met according to NICE guidance, then alternatives were swapping out sulfasalazine for cyclosporine or leflunomide, again increasing the doses. Patients who did get put onto a biologic could switch to another anti-TNF if they did not respond after 12 weeks.
The primary endpoint data from the trial have been reported previously and showed that a higher proportion of patients in the intensive management group achieved ACR20 at 48 weeks, compared with those in the standard care group (62% vs. 45%, respectively; P = .02). A higher percentage of intensively managed patients also achieved ACR50 (51% vs. 25%; P = .0004) and ACR70 (38% vs. 17%, P = .002).
Skin symptoms, measured via the Psoriasis Area and Severity Index (PASI) showed significant improvement favoring intensive therapy over standard care. PASI20 was achieved by 72% of intensively managed patients versus 52% of those who received standard care. PASI75 was achieved by 59% versus 33%, respectively, and PASI90 by 40% versus 20%, respectively.
The full results of the study will be published soon in The Lancet and will include details of a variety of secondary outcomes and the cost-effectiveness of the intensive management strategy versus the standard care approach.
One of the key secondary outcomes of the trial was to look at the effects of the two treatment strategies on other PsA symptoms, such as enthesitis, dactylitis, and nail symptoms. No differences between the groups were observed, however, with similar decreases seen in the tight control and standard care groups.
There were no statistically significant differences in radiologic outcomes, which included baseline and end-of-treatment changes in the total modified Sharp van der Heijde (SVdH) score, the erosion score, and joint-space narrowing (JSN) score.
While this might seem somewhat disappointing, “there wasn’t a lot of radiologic progression going on anyway,” Dr. Helliwell pointed out. Overall, there was a difference of about 5% in the percentage of patients with at least one joint erosion at baseline and after 48 weeks of treatment.
The majority of radiographic change that did occur was JSN of the hands, Dr. Helliwell said, adding that patients with JSN tended to be slightly older than those without, although this observation did not reach statistical significance.
“We’ve since looked for associations with ACPA [anticitrullinated protein antibodies] – about 7% of our patients were ACPA positive – but there is no relationship,” he added. There was also no significant association between levels of C-reactive protein levels and erosive disease.
There was a trend suggesting that patients with erosions may be more likely to have polyarticular disease than oligoarticular disease, so a next step would be to look at radiologic progression in these two groups of patients in more detail.
More adverse events were seen in the tight control arm, compared with the standard care arm, including more serious adverse events, but not all of these were related to study treatment and many adverse events were those to be expected with methotrexate treatment, Dr. Helliwell observed.
But is the intensive approach cost-effective when compared to standard care? Data suggest that it is. Although the incremental cost-effectiveness ratio (ICER) initially exceeded the £20,000–£30,000 (about $31,000-$47,000) threshold used by the U.K. National Institute for Health and Care Excellence to judge if a new treatment is cost effective, allowing for certain factors enabled the ICER to be brought down to about £28,000 ($44,000), making it a cost-effective strategy.
PsA consists of five classical subtypes. The most common of these subtypes is polyarthritis (60% of patients), followed by oligoarthritis (30%). The remaining 10% of patients comprise those with arthritis mutilans, distal interphalangeal predominant disease, or spinal predominant disease. The clinical features of dactylitis and enthesitis are prevalent in about 40% and 50% of patients, respectively, and can occur in any subgroup.
Considering such heterogeneity in its presentation, the challenge now will be to determine if all clinical subgroups of PsA could benefit from treating to an MDA target with intensive management, or if one or other subgroups benefit more than another.
The TICOPA study was funded by Arthritis Research UK with support from Pfizer. Dr. Helliwell has received consulting fees from Pfizer.
Results of this study were published in the Lancet Sept. 30, 2015.
This article was updated October 6, 2015.
MANCHESTER, U.K. – Multiple joint and skin benefits can be achieved by intensively treating patients with psoriatic arthritis until they achieve a set of minimal disease activity criteria, an expert said at the British Society for Rheumatology annual conference.
While data are mounting on the value of treating to target (otherwise known as tight control) in psoriatic arthritis (PsA), these data lag significantly behind that for inducing and maintaining remission in rheumatoid arthritis (RA), noted Dr. Philip Helliwell of the University of Leeds (England).
“There is half as much evidence in PsA as there is in rheumatoid arthritis,” he observed. “But we’ve also got a heterogeneous disease and what we are going to have to do moving forward is to find out how to treat different phenotypic expressions of psoriatic disease, and we’re beginning to work towards that now,” he said during a Special Interest Group on Spondyloarthropathies.
Dr. Helliwell is the principal investigator of the Tight Control of Psoriatic Arthritis (TICOPA) study, which he highlighted as an example of how targeting treatment to achieve minimal disease activity (MDA) criteria (Ann. Rheum. Dis. 2010;69:48-53) could be beneficial versus standard care.
A total of 206 patients with newly-diagnosed PsA were enrolled into the study and were randomized to receive either ‘tight control’ – meaning an intensive management strategy – or to standard care for 48 weeks.
Intensive treatment involved starting with methotrexate at a dose of 15 mg/kg per week and rapidly escalating to 25 mg/kg per week at 6 weeks if needed. If patients did not achieve five out of a set of seven MDA criteria for PsA, then methotrexate was continued and sulfasalazine was added and dose escalated after 4-8 weeks.
If MDA was still not achieved and criteria for biologics were not met according to NICE guidance, then alternatives were swapping out sulfasalazine for cyclosporine or leflunomide, again increasing the doses. Patients who did get put onto a biologic could switch to another anti-TNF if they did not respond after 12 weeks.
The primary endpoint data from the trial have been reported previously and showed that a higher proportion of patients in the intensive management group achieved ACR20 at 48 weeks, compared with those in the standard care group (62% vs. 45%, respectively; P = .02). A higher percentage of intensively managed patients also achieved ACR50 (51% vs. 25%; P = .0004) and ACR70 (38% vs. 17%, P = .002).
Skin symptoms, measured via the Psoriasis Area and Severity Index (PASI) showed significant improvement favoring intensive therapy over standard care. PASI20 was achieved by 72% of intensively managed patients versus 52% of those who received standard care. PASI75 was achieved by 59% versus 33%, respectively, and PASI90 by 40% versus 20%, respectively.
The full results of the study will be published soon in The Lancet and will include details of a variety of secondary outcomes and the cost-effectiveness of the intensive management strategy versus the standard care approach.
One of the key secondary outcomes of the trial was to look at the effects of the two treatment strategies on other PsA symptoms, such as enthesitis, dactylitis, and nail symptoms. No differences between the groups were observed, however, with similar decreases seen in the tight control and standard care groups.
There were no statistically significant differences in radiologic outcomes, which included baseline and end-of-treatment changes in the total modified Sharp van der Heijde (SVdH) score, the erosion score, and joint-space narrowing (JSN) score.
While this might seem somewhat disappointing, “there wasn’t a lot of radiologic progression going on anyway,” Dr. Helliwell pointed out. Overall, there was a difference of about 5% in the percentage of patients with at least one joint erosion at baseline and after 48 weeks of treatment.
The majority of radiographic change that did occur was JSN of the hands, Dr. Helliwell said, adding that patients with JSN tended to be slightly older than those without, although this observation did not reach statistical significance.
“We’ve since looked for associations with ACPA [anticitrullinated protein antibodies] – about 7% of our patients were ACPA positive – but there is no relationship,” he added. There was also no significant association between levels of C-reactive protein levels and erosive disease.
There was a trend suggesting that patients with erosions may be more likely to have polyarticular disease than oligoarticular disease, so a next step would be to look at radiologic progression in these two groups of patients in more detail.
More adverse events were seen in the tight control arm, compared with the standard care arm, including more serious adverse events, but not all of these were related to study treatment and many adverse events were those to be expected with methotrexate treatment, Dr. Helliwell observed.
But is the intensive approach cost-effective when compared to standard care? Data suggest that it is. Although the incremental cost-effectiveness ratio (ICER) initially exceeded the £20,000–£30,000 (about $31,000-$47,000) threshold used by the U.K. National Institute for Health and Care Excellence to judge if a new treatment is cost effective, allowing for certain factors enabled the ICER to be brought down to about £28,000 ($44,000), making it a cost-effective strategy.
PsA consists of five classical subtypes. The most common of these subtypes is polyarthritis (60% of patients), followed by oligoarthritis (30%). The remaining 10% of patients comprise those with arthritis mutilans, distal interphalangeal predominant disease, or spinal predominant disease. The clinical features of dactylitis and enthesitis are prevalent in about 40% and 50% of patients, respectively, and can occur in any subgroup.
Considering such heterogeneity in its presentation, the challenge now will be to determine if all clinical subgroups of PsA could benefit from treating to an MDA target with intensive management, or if one or other subgroups benefit more than another.
The TICOPA study was funded by Arthritis Research UK with support from Pfizer. Dr. Helliwell has received consulting fees from Pfizer.
Results of this study were published in the Lancet Sept. 30, 2015.
This article was updated October 6, 2015.
EXPERT ANALYSIS AT RHEUMATOLOGY 2015