User login
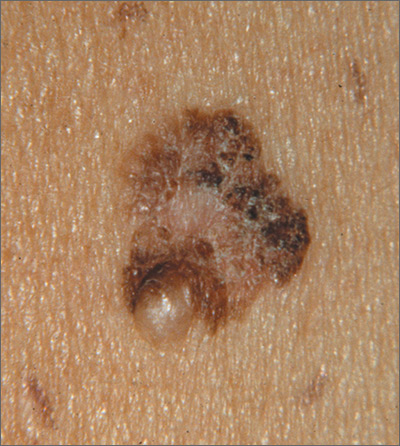
The FP suspected that this was a melanoma.
He thought through the ABCDEs of melanoma and saw that it was Asymmetric, had an irregular Border, had varied Colors, the Diameter was larger than 6 mm, and it was Evolving. The FP also noted that one area was elevated and another area (the center) seemed to be regressing. Using his dermatoscope, he noted strong evidence of regression in the center and an “atypical network.” He told the patient that this was very suspicious for melanoma and recommended a skin biopsy without delay. The patient agreed and after local anesthesia with lidocaine with epinephrine, a saucerization biopsy was performed using a DermaBlade. (See the Watch & Learn video on “Shave biopsy.”) The FP easily removed all of the visible tumor with the saucerization (deep shave). The bleeding was stopped with topical aluminum chloride, and the specimen was sent in formalin to the pathologist. The pathology report came back as a melanoma of 2.1 mm depth arising in a pre-existing nevus.
The patient was referred to a surgical oncologist for sentinel lymph node biopsy and excision with wide margins.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Congenital nevi. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine, 2nd ed. New York, NY: McGraw-Hill; 2013:953-957.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.
The FP suspected that this was a melanoma.
He thought through the ABCDEs of melanoma and saw that it was Asymmetric, had an irregular Border, had varied Colors, the Diameter was larger than 6 mm, and it was Evolving. The FP also noted that one area was elevated and another area (the center) seemed to be regressing. Using his dermatoscope, he noted strong evidence of regression in the center and an “atypical network.” He told the patient that this was very suspicious for melanoma and recommended a skin biopsy without delay. The patient agreed and after local anesthesia with lidocaine with epinephrine, a saucerization biopsy was performed using a DermaBlade. (See the Watch & Learn video on “Shave biopsy.”) The FP easily removed all of the visible tumor with the saucerization (deep shave). The bleeding was stopped with topical aluminum chloride, and the specimen was sent in formalin to the pathologist. The pathology report came back as a melanoma of 2.1 mm depth arising in a pre-existing nevus.
The patient was referred to a surgical oncologist for sentinel lymph node biopsy and excision with wide margins.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Congenital nevi. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine, 2nd ed. New York, NY: McGraw-Hill; 2013:953-957.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.
The FP suspected that this was a melanoma.
He thought through the ABCDEs of melanoma and saw that it was Asymmetric, had an irregular Border, had varied Colors, the Diameter was larger than 6 mm, and it was Evolving. The FP also noted that one area was elevated and another area (the center) seemed to be regressing. Using his dermatoscope, he noted strong evidence of regression in the center and an “atypical network.” He told the patient that this was very suspicious for melanoma and recommended a skin biopsy without delay. The patient agreed and after local anesthesia with lidocaine with epinephrine, a saucerization biopsy was performed using a DermaBlade. (See the Watch & Learn video on “Shave biopsy.”) The FP easily removed all of the visible tumor with the saucerization (deep shave). The bleeding was stopped with topical aluminum chloride, and the specimen was sent in formalin to the pathologist. The pathology report came back as a melanoma of 2.1 mm depth arising in a pre-existing nevus.
The patient was referred to a surgical oncologist for sentinel lymph node biopsy and excision with wide margins.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Congenital nevi. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine, 2nd ed. New York, NY: McGraw-Hill; 2013:953-957.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.