User login
ANSWER
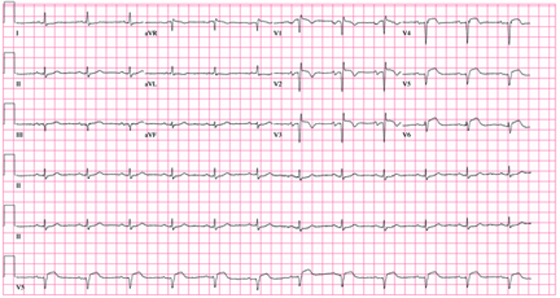
The correct interpretation of this ECG includes normal sinus rhythm, left atrial enlargement, and an anteroseptal myocardial infarction.
The diagnostic criteria for left atrial enlargement include a P-wave duration of ≥ 120 ms in lead II and/or a terminal negative component of a biphasic P wave in lead V1. In this example, the biphasic P wave is better seen in lead V2, while a large negative P wave is present in V1.
The diagnostic criteria for anteroseptal myocardial infarction include Q, QS, or QRS complexes in leads V1 through V4 along with evolving ST-T changes. In this example, leads V1 through V3 have large Q waves, while lead V4 has a large QS complex. All precordial leads contain ST-T wave elevations.
ANSWER
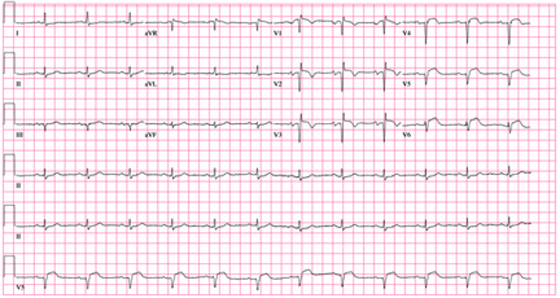
The correct interpretation of this ECG includes normal sinus rhythm, left atrial enlargement, and an anteroseptal myocardial infarction.
The diagnostic criteria for left atrial enlargement include a P-wave duration of ≥ 120 ms in lead II and/or a terminal negative component of a biphasic P wave in lead V1. In this example, the biphasic P wave is better seen in lead V2, while a large negative P wave is present in V1.
The diagnostic criteria for anteroseptal myocardial infarction include Q, QS, or QRS complexes in leads V1 through V4 along with evolving ST-T changes. In this example, leads V1 through V3 have large Q waves, while lead V4 has a large QS complex. All precordial leads contain ST-T wave elevations.
ANSWER
The correct interpretation of this ECG includes normal sinus rhythm, left atrial enlargement, and an anteroseptal myocardial infarction.
The diagnostic criteria for left atrial enlargement include a P-wave duration of ≥ 120 ms in lead II and/or a terminal negative component of a biphasic P wave in lead V1. In this example, the biphasic P wave is better seen in lead V2, while a large negative P wave is present in V1.
The diagnostic criteria for anteroseptal myocardial infarction include Q, QS, or QRS complexes in leads V1 through V4 along with evolving ST-T changes. In this example, leads V1 through V3 have large Q waves, while lead V4 has a large QS complex. All precordial leads contain ST-T wave elevations.
A 62-year-old African-American man presents to the urgent care center with a six-hour history of chest pain. He describes the pain as a “burning, achy” sensation with radiation to his left neck and shoulder. The pain started while the man was at rest but did not increase with activity. The patient denies symptoms such as shortness of breath, orthopnea, nausea, or vomiting. He says he had hoped the pain would resolve, but he now thinks it has “gone on long enough.” The patient has a history of similar chest pain four years ago. At that time, cardiac catheterization showed an 80% proximal stenosis of the left anterior descending (LAD) coronary artery. A drug-eluting stent was placed from the origin to the mid vessel of the LAD. Although the patient has a prescription for nitroglycerin, he hasn’t filled it in three months because he hasn’t experienced chest pain in more than a year and wanted to save money. Medical history is remarkable for type 1 diabetes, hypertension, hyperlipidemia, COPD, migraine, and diverticulitis. Surgical history is remarkable for an appendectomy during childhood. The patient is allergic to penicillin and cephalosporins. His current medication list includes insulin glargine, carvedilol, clopidogrel, ezetimibe, fenofibrate, hydrochlorothiazide, and aspirin (in addition to the nitroglycerin), but he has not taken any of these for two weeks due to financial constraints. The patient smokes 1½ packs of cigarettes daily and drinks an average of one case of beer per week. He does not know any details of his family history. The review of systems is remarkable for increased fatigue and weakness during the past week and for a migraine that the patient says is starting now. The physical exam reveals a blood pressure of 188/105 mm Hg; pulse, 70 beats/min; respiratory rate, 20 min-1; and temperature, 99°F. His weight is 119 lb, and his height is 68”. He is anxious, uncomfortable, and chronically ill appearing. Pertinent physical findings include pulmonary crackles in both bases, jugular venous distention to the angle of the jaw, a regular rate and rhythm with an S3 gallop, and a soft early systolic murmur at the left sternal border. He has no lower extremity edema, and his neurologic exam is intact. Abnormal laboratory data include: serum glucose of 318 mg/dL; creatinine, 2.6 mg/dL; troponin, 72 ng/mL; and B-type natriuretic peptide (BNP), 2,499 pg/mL. A stat ECG shows the following: a ventricular rate of 73 beats/min; PR interval, 160 ms; QRS duration, 88 ms; QT/QTc interval, 358/394; P axis, 39°; R axis, -3°; and T axis, 88°. What is your interpretation of this ECG?