User login
“A patient I’ve seen for a number of years had been diagnosed in the pervasive developmental disorder spectrum, but she was quite atypical. Her perseverative thinking focused on a fantasy world, and she was so preoccupied that it was very difficult to pull her out of it. Now at age 12, she has a full-blown psychotic disorder, and the fantasy world is enveloping her. She hears people talking to her all day long.”
Jean A. Frazier, MD, who treats this patient and other children with psychotic disorders, was 1 of 4 principal investigators in the Treatment of Early-Onset Schizophrenia Spectrum Disorders (TEOSS) study, a randomized, double-blind, multisite trial funded by the National Institute of Mental Health. The study, published in November 2008,1 compared the efficacy and tolerability of 3 antipsychotics—olanzapine, risperidone, and molindone—in pediatric patients with schizophrenia or schizoaffective disorder (Box 1).
Dr. Frazier discusses the unexpected findings of the TEOSS trial with Current Psychiatry Section Editor Robert A. Kowatch, MD, PhD. Based on the trial findings and her experience, she tells how she makes decisions when prescribing antipsychotics for children and adolescents with schizophrenia and related disorders.
DR. KOWATCH: The TEOSS trial found no significant differences in efficacy between molindone and the atypical antipsychotics (olanzapine and risperidone) included in the study. You’ve prescribed both typical and atypical antipsychotics in research and in your clinical practice. Do you believe there’s any difference between the 2 classes?
DR. FRAZIER: There are some differences. For example, treatment-refractory patients, especially young children, sometimes need more D2 blockade than some atypical antipsychotics provide. I’ve seen more extra pyramidal side effects with the typical antipsychotics than the atypicals, although it’s not uncommon to see some akathisia with aripiprazole or some dystonia and dyskinesia with risperidone.
DR. KOWATCH: What are the benefits and risks of using antipsychotics in young children?
DR. FRAZIER: The benefit is that antipsychotics can decrease children’s suffering and get them more centered in reality so they can enjoy their friends and progress in school. And when that happens, it’s wonderful. What are the risks? With the atypicals my greatest concern is weight gain, and with the typical agents it’s tardive dyskinesia.
DR. KOWATCH: Have you changed the way you prescribe antipsychotics as a result of the TEOSS study?
DR. FRAZIER: Actually, I have. Clinicians have to be very careful about selecting psychotropic agents that can worsen pediatric-onset obesity. Olanzapine is an effective agent for targeting psychosis and mood symptoms, but the weight gain associated with it is a concern. I do not prescribe olanzapine as much as I have in the past, although I keep it in my armamentarium and tend to reserve it for third- or fourth-line therapy.
I have found molindone to be quite effective in children with schizophrenia or schizoaffective disorder, especially in those who have gained a lot of weight on atypical antipsychotics. They usually lose weight on molindone.
DR. KOWATCH: Do you think the TEOSS study had adequate power to demonstrate differences among molindone, olanzapine, and risperidone?
DR. FRAZIER: We enrolled 119 patients—which is large for a study such as this—but we did not reach our target of 168 patients, which might have increased our power to detect differences. Among the children we did enroll, the 3 antipsychotics showed no difference in efficacy, but the meaningful finding of this study to me was the side effect profile of these agents.
DR. KOWATCH: You mean weight gain with olanzapine and extrapyramidal symptoms with molindone?
DR. FRAZIER: Yes.
Managing side effects
DR. KOWATCH: How do you manage antipsychotic side effects?
DR. FRAZIER: For any of the antipsychotics’ side effects, you have to decide whether to continue the agent or switch to another anti psychotic. For example, I’ve had a number of children—many with significant weight problems—whose psychotic symptoms have responded only to risperidone. So we put them back on risperidone, and the decision then becomes what can we do to help with the weight gain while continuing that agent.
For weight gain, I think the best intervention is diet, exercise, and drinking a lot of water, but that can be effective only if you engage the patient’s entire family in the intervention as well. Short of that, a number of pharmacologic interventions have been studied, although not specifically in children.
In an open-label trial our group conducted with 11 children age 10 to 18 years who had gained weight while taking atypical antipsychotics, metformin decreased lipid levels and body mass index but not significantly. I’ve followed these children in my practice, however, and all those who continued taking metformin over a period of months lost weight.
TEOSS study adds to debate about efficacy and tolerability
The 5-year National Institute of Mental Health-funded Treatment of Early-Onset Schizophrenia Spectrum Disorders (TEOSS) trial began with an ambitious goal: to compare the efficacy and safety of 1 typical and 2 atypical antipsychotics in children age 8 to 19 with schizophrenia. The primary hypothesis was that atypical agents would show greater efficacy and tolerability when given for 8 weeks. Instead, the atypical agents showed no greater efficacy, and adverse effects occurred with all 3 antipsychotics. Because the trial was designed for 168 subjects but enrolled 119, it may not have been adequately powered to detect differences among the 3 agents.
Medications: Most of the 116 children who received medications were severely ill with psychotic symptoms when randomly assigned to 1 of the 3 antipsychotics for 8 weeks of double-blind treatment. Administration began at the lowest dose in a set range and usually was increased to midrange within 10 to 14 days. Dosing remained flexible within these ranges:
- molindone, 10 to 140 mg/d (mean endpoint dose 59.9 mg/d)
- olanzapine, 2.5 to 20 mg/d (mean endpoint dose 11.4 mg/d)
- risperidone, 0.5 to 6 mg/d (mean endpoint dose 2.8 mg/d).
Benztropine, ≥1 mg/d, was given to all patients treated with molindone, 14% of those treated with olanzapine, and 34% of those treated with risperidone to prevent or manage akathisia.
Efficacy: Two criteria defined treatment response: a Clinical Global Impression improvement score of 1 or 2 and a ≥20% reduction in baseline Positive and Negative Syndrome Scale (PANSS) score. Tolerability outcomes included neurologic side effects, weight changes, laboratory analyses, vital signs, ECG, serious adverse events, and treatment discontinuation. Extrapyramidal symptoms were monitored with involuntary movement and akathisia scales.
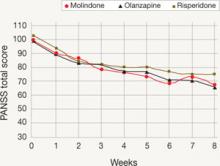
Observed PANSS total score by week of treatment
Mean Positive and Negative Symptom Scale (PANSS) total scores of observed cases during each week of the TEOSS trial. Minimum possible PANSS score is 30; scores >60 typically are viewed as problematic.
Among the 70 patients who completed treatment (25 of 40 with molindone, 17 of 35 olanzapine, and 28 of 41 with risperidone), more than one-half failed to achieve an adequate response. Response rates were 50% with molindone, 34% with olanzapine, and 46% with risperidone. The atypical antipsychotics did not show greater efficacy than molindone, and mean reductions in psychotic symptoms were modest (20% to 34% on the PANSS). Mean medication doses were midrange and considered moderate.
Tolerability: Sedation, irritability, and anxiety were frequent adverse events. Patients receiving molindone reported significantly higher rates of akathisia (P < .0008). Those receiving olanzapine reported significantly higher rates of weight gain (P < .0001) and were the only group with increased lipid and insulin serum levels and liver function tests. Patients in the risperidone group reported significantly higher rates of constipation (P < .021) and were the only group that experienced elevated serum prolactin.
Source: Sikich L, Frazier JA, McClellan J, et al. Double-blind comparison of first- and second-generation antipsychotics in early-onset schizophrenia and schizoaffective disorder: findings from the Treatment of Early-Onset Schizophrenia Spectrum disorders (TEOSS) study. Am J Psychiatry. 2008;165:1420-1431
Choosing antipsychotics
DR. KOWATCH: Let’s say you’re seeing psychosis in a 12-year-old whom you think is schizophrenic, and he or she has not yet received an antipsychotic. What are your top 3 treatment choices?
DR. FRAZIER: The first agent I usually select is risperidone. We have the most data on the use of this atypical antipsychotic in children and adolescents, and most psychotic children I see do better with a bit more D2 blockade than some of the other atypicals provide. That said, I remain concerned about risperidone’s side effects—such as weight gain and increased serum prolactin—so my usual second-line agent is aripiprazole.
I became interested in the complicated overlap between pervasive developmental disorders spectrum and psychotic disorders early in my training. More is known about prodromal symptoms in adolescents and adults than in children.
A group in the Netherlands5 compared 32 adolescents with severe early deficits in affect regulation, anxiety, disturbed social relationships, and thought disorder (characterized as “multiple complex developmental disorder” [MCDD]) with 80 adolescents with prodromal psychotic symptoms who met criteria for “at-risk mental state” (ARMS). Three-quarters of the children with MCDD (78%) were found to meet criteria for ARMS, and the 2 groups showed similar schizotypal traits, disorganization, and prodromal symptoms.
Signs of progression to psychosis and schizophrenia in children typically include:
- change in personality
- decrease in functioning or decline in ability to perform at school
- unusual thoughts or behaviors
- crippling anxiety
- supersensitivity to stress.
With experience, the clinician can more clearly differentiate the prodromal signs of psychosis from normal childhood behaviors. Children who are psychotic often don’t make good eye contact. When you try to engage them in discussion about hearing voices, they’re inattentive and internally preoccupied.
Normal vs psychotic children. You want a child in the latency age to have a rich fantasy life. If they do not, that raises concerns. Both normal and psychotic children sometimes say an imaginary friend told them something. Normal children eventually will admit this friend is imaginary. When children are psychotic, especially at an early age, you can’t pull them out of thinking about the imaginary friend, and they can’t distinguish fantasy from reality. Psychotic children also hear imaginary friends talking to them much more often.
Normal children usually are not afraid of their imaginary friends, whereas psychotic children—particularly adolescents—often are afraid of the voices they hear. However, if a psychotic child has heard voices from a young age, the voices aren’t always ego-dystonic. The girl I mentioned at the beginning of this article likes having the voices around. In fact, she gets uncomfortable when the voices are quiet.—Jean A. Frazier, MD
DR. KOWATCH: Why do you like aripiprazole for this patient population?
DR. FRAZIER: Aripiprazole doesn’t tend to be associated with as much weight gain as olanzapine or risperidone, although I’ve had children—especially in the autism spectrum—who have gained quite a bit of weight on aripiprazole. Clinically, I’ve noticed that aripiprazole seems to brighten up children’s affect. It also seems to help many children in my practice with attentional symptoms, although that’s anecdotal.
Although we don’t have a lot of data to inform this discussion about aripiprazole, a placebo-controlled study of 302 adolescents diagnosed with schizophrenia showed that aripiprazole, 10 mg/d, targeted negative symptoms fairly well, based on changes from baseline in PANSS (Positive and Negative Syndrome Scale) total scores. This was a 6-week multicenter, double-blind, randomized, trial.2
Ultimately, cognition in patients with schizophrenia is the strongest predictor of success in the workplace and in school. We need data on what happens to neurocognitive functioning with aripiprazole—and all the other atypical agents.
DR. KOWATCH: What would be your third-line agent?
DR. FRAZIER: Well, that varies for me. I’m trying to match the medication I use with the individual patient, and at this point I prescribe based on the side-effect profile more than anything else. I also consider if the child has a family member who has suffered from a similar condition and what agents the family member responded to.
Let’s say I have a child who has tried 1 or 2 atypical antipsychotics and has not had a good response. Many times I decide to try yet another atypical, and often I will try quetiapine. But after a patient has not responded to 2 atypicals, I might start thinking about a typical agent or clozapine. I use clozapine quite a bit. I find it is the most efficacious agent available, and the data speak to this as well.3,4 It has been truly remarkable for some children in my practice.
Less than 50% chance of efficacy?
DR. KOWATCH: The TEOSS study found 50% or lower response rates across 8 weeks of antipsychotic treatment. Clinically, what kind of response rates do you see with antipsychotics in children and adolescents?
DR. FRAZIER: I probably see about a 50% response rate in my practice as well. It’s variable, and the earlier the onset of the illness, the harder it is to treat.
DR. KOWATCH: Do you ever combine a typical antipsychotic with an atypical?
DR. FRAZIER: I try not to, but a number of children in the schizophrenia spectrum have enduring positive symptoms after 2 or 3 trials of atypical antipsychotics. Sometimes adding a touch of a typical agent can improve the situation. The typicals I usually try are perphenazine (around 8 to 16 mg/d) or molin done (around 20 to 60 mg/d). Sometimes I use a very low dose of haloperidol (such as 0.5 to 2 mg/d) with an atypical agent, and it can be quite effective.
DR. KOWATCH: That has been our experience as well; sometimes combining typical and atypical agents improves response. Besides medications, what do you consider an optimal treatment plan for a child or adolescent with psychosis?
DR. FRAZIER: These children need a multi-modal approach. Pharmacotherapy is the cornerstone because you want to decrease positive symptoms of psychosis, but often these children require therapeutic school placements or residential programs. If they’re old enough, cognitive-behavioral therapy can help by teaching them skills to manage ongoing psychotic symptoms. Older teens often have comorbid substance abuse and may require substance abuse intervention.
Are antipsychotics overused?
DR. KOWATCH: Do you think antipsychotics are overused in pediatric patients with psychosis?
DR. FRAZIER: In pediatric patients with psychosis? No.
DR. KOWATCH: What about in pediatric patients with behavioral disorders?
DR. FRAZIER: We need more studies to inform our practice and to be mindful of the evidence. Most children with schizophrenia have substantial developmental challenges (Box 2).5 In the autism spectrum, often an atypical antipsychotic is the only agent that can help a patient who is aggressive, self-injurious, or agitated.
In terms of bipolar disorder in children and adolescents, it would be ideal if we had more head-to-head comparator studies to inform our prescriptive practice. For example, we need more studies comparing traditional mood stabilizers such as lithium with the atypical agents.
Of course it would be ideal if we could use monotherapy in children who suffer from bipolar disorder and schizophrenia. But early-onset bipolar disorder—like early-onset schizophrenia—can be very difficult to treat and often requires more than 1 agent.
In a recent study of a pharmacotherapy algorithm for treating pediatric bipolar disorder,3 the children who did the best were on a combination of a mood stabilizer and an atypical antipsychotic. That has been my experience, too. I do my best to manage children on a mood stabilizer alone, but I rarely have been able to do that.
In terms of attention-deficit/hyperactivity disorder (ADHD), it depends on what’s going on with the child. Certain children with an ADHD diagnosis have complicated behavioral issues. First I would wonder if they have a different diagnosis, particularly if it gets to the point that an atypical agent is being considered. But sometimes it becomes a question of treating pronounced aggression. We need more studies to inform what we do. Some studies indicate that stimulants can be quite helpful for the aggressive child with ADHD.7
DR. KOWATCH: I don’t see any child and adolescent psychiatrist in the United States using antipsychotics to treat uncomplicated ADHD. The kids we see [at specialty clinics] have comorbid problems such as conduct disorder, oppositional-defiant disorder, mood instability—whatever you want to call it. And we’re seeing these patients because they haven’t done well on other medications, such as stimulants. Usually the parents are desperate because these children are moody and aggressive. I don’t think anybody wants to treat children with antipsychotics or mood stabilizers, but it’s what keeps these children well.
DR. FRAZIER: Yes, I agree.
Related resources
- Longitudinal assessment and monitoring of clinical status and brain function in adolescents and adults. Boston Center for Intervention Development and Applied Research (CIDAR) study. www.bostoncidar.org.
- Frazier JA, Hodge S, Breeze JL, et al. Diagnostic and sex effects on limbic volumes in early-onset bipolar disorder and schizophrenia. Schizophr Bull. 2008;34(1):37-46.
- Frazier JA, McClellan J, Findling RL, et al. Treatment of Early-Onset Schizophrenia Spectrum disorders (TEOSS): demographic and clinical characteristics. J Am Acad Child Adolesc Psychiatry. 2007;46:979-988.
Drug brand names
- Aripiprazole • Abilify
- Benztropine • Cogentin
- Clozapine • Clozaril
- Haloperidol • Haldol
- Metformin • Glucophage
- Molindone • Moban
- Olanzapine • Zyprexa
- Perphenazine • Trilafon
- Quetiapine • Seroquel
- Risperidone • Risperdal
Disclosures
Dr. Kowatch receives grant/research support from the Stanley Foundation, National Institute of Mental Health, National Institute of Child Health and Human Development, and the National Alliance for Research on Schizophrenia and Depression. He is a consultant to AstraZeneca and Forest Pharmaceuticals and a speaker for AstraZeneca.
Dr. Frazier receives grant/research support from Bristol-Myers Squibb, Eli Lilly and Company, GlaxoSmithKline, Johnson & Johnson, Neuropharm, Otsuka America Pharmaceuticals, and Pfizer Inc.
1. Sikich L, Frazier JA, McClellan J, et al. Double-blind comparison of first- and second-generation antipsychotics in early-onset schizophrenia and schizoaffective disorder: findings from the Treatment of Early-Onset Schizophrenia Spectrum Disorders (TEOSS) study. Am J Psychiatry. 2008;165:1420-1431.
2. Findling RL, Robb A, Nyilas M, et al. A multiple-center, randomized, double-blind, placebo-controlled study of oral aripiprazole for treatment of adolescents with schizophrenia. Am J Psychiatry. 2008;165(11):1432-1441.
3. Findling RL, Frazier JA, Gerbino-Rosen G, et al. Is there a role for clozapine in the treatment of children and adolescents? J Am Acad Child Adolesc Psychiatry. 2007;46(3):423-428.
4. Kim Y, Kim BN, Cho SC, et al. Long-term sustained benefits of clozapine treatment in refractory early onset schizophrenia: a retrospective study in Korean children and adolescents. Hum Psychopharmacol. 2008;23(8):715-722.
5. Sprong M, Becker HE, Schothorst PF, et al. Pathways to psychosis: a comparison of the pervasive developmental disorder subtype multiple complex developmental disorder and the “at risk mental state.” Schizophr Res. 2008;99:38-47.
6. Pavuluri MN, Henry DB, Devineni B, et al. A pharmacotherapy algorithm for stabilization and maintenance of pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2004;43(7):859-867.
7. Sinzig J, Döpfner M, Lehmkuhl G, et al. Long-acting methylphenidate has an effect on aggressive behavior in children with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2007;17(4):421-432.
“A patient I’ve seen for a number of years had been diagnosed in the pervasive developmental disorder spectrum, but she was quite atypical. Her perseverative thinking focused on a fantasy world, and she was so preoccupied that it was very difficult to pull her out of it. Now at age 12, she has a full-blown psychotic disorder, and the fantasy world is enveloping her. She hears people talking to her all day long.”
Jean A. Frazier, MD, who treats this patient and other children with psychotic disorders, was 1 of 4 principal investigators in the Treatment of Early-Onset Schizophrenia Spectrum Disorders (TEOSS) study, a randomized, double-blind, multisite trial funded by the National Institute of Mental Health. The study, published in November 2008,1 compared the efficacy and tolerability of 3 antipsychotics—olanzapine, risperidone, and molindone—in pediatric patients with schizophrenia or schizoaffective disorder (Box 1).
Dr. Frazier discusses the unexpected findings of the TEOSS trial with Current Psychiatry Section Editor Robert A. Kowatch, MD, PhD. Based on the trial findings and her experience, she tells how she makes decisions when prescribing antipsychotics for children and adolescents with schizophrenia and related disorders.
DR. KOWATCH: The TEOSS trial found no significant differences in efficacy between molindone and the atypical antipsychotics (olanzapine and risperidone) included in the study. You’ve prescribed both typical and atypical antipsychotics in research and in your clinical practice. Do you believe there’s any difference between the 2 classes?
DR. FRAZIER: There are some differences. For example, treatment-refractory patients, especially young children, sometimes need more D2 blockade than some atypical antipsychotics provide. I’ve seen more extra pyramidal side effects with the typical antipsychotics than the atypicals, although it’s not uncommon to see some akathisia with aripiprazole or some dystonia and dyskinesia with risperidone.
DR. KOWATCH: What are the benefits and risks of using antipsychotics in young children?
DR. FRAZIER: The benefit is that antipsychotics can decrease children’s suffering and get them more centered in reality so they can enjoy their friends and progress in school. And when that happens, it’s wonderful. What are the risks? With the atypicals my greatest concern is weight gain, and with the typical agents it’s tardive dyskinesia.
DR. KOWATCH: Have you changed the way you prescribe antipsychotics as a result of the TEOSS study?
DR. FRAZIER: Actually, I have. Clinicians have to be very careful about selecting psychotropic agents that can worsen pediatric-onset obesity. Olanzapine is an effective agent for targeting psychosis and mood symptoms, but the weight gain associated with it is a concern. I do not prescribe olanzapine as much as I have in the past, although I keep it in my armamentarium and tend to reserve it for third- or fourth-line therapy.
I have found molindone to be quite effective in children with schizophrenia or schizoaffective disorder, especially in those who have gained a lot of weight on atypical antipsychotics. They usually lose weight on molindone.
DR. KOWATCH: Do you think the TEOSS study had adequate power to demonstrate differences among molindone, olanzapine, and risperidone?
DR. FRAZIER: We enrolled 119 patients—which is large for a study such as this—but we did not reach our target of 168 patients, which might have increased our power to detect differences. Among the children we did enroll, the 3 antipsychotics showed no difference in efficacy, but the meaningful finding of this study to me was the side effect profile of these agents.
DR. KOWATCH: You mean weight gain with olanzapine and extrapyramidal symptoms with molindone?
DR. FRAZIER: Yes.
Managing side effects
DR. KOWATCH: How do you manage antipsychotic side effects?
DR. FRAZIER: For any of the antipsychotics’ side effects, you have to decide whether to continue the agent or switch to another anti psychotic. For example, I’ve had a number of children—many with significant weight problems—whose psychotic symptoms have responded only to risperidone. So we put them back on risperidone, and the decision then becomes what can we do to help with the weight gain while continuing that agent.
For weight gain, I think the best intervention is diet, exercise, and drinking a lot of water, but that can be effective only if you engage the patient’s entire family in the intervention as well. Short of that, a number of pharmacologic interventions have been studied, although not specifically in children.
In an open-label trial our group conducted with 11 children age 10 to 18 years who had gained weight while taking atypical antipsychotics, metformin decreased lipid levels and body mass index but not significantly. I’ve followed these children in my practice, however, and all those who continued taking metformin over a period of months lost weight.
TEOSS study adds to debate about efficacy and tolerability
The 5-year National Institute of Mental Health-funded Treatment of Early-Onset Schizophrenia Spectrum Disorders (TEOSS) trial began with an ambitious goal: to compare the efficacy and safety of 1 typical and 2 atypical antipsychotics in children age 8 to 19 with schizophrenia. The primary hypothesis was that atypical agents would show greater efficacy and tolerability when given for 8 weeks. Instead, the atypical agents showed no greater efficacy, and adverse effects occurred with all 3 antipsychotics. Because the trial was designed for 168 subjects but enrolled 119, it may not have been adequately powered to detect differences among the 3 agents.
Medications: Most of the 116 children who received medications were severely ill with psychotic symptoms when randomly assigned to 1 of the 3 antipsychotics for 8 weeks of double-blind treatment. Administration began at the lowest dose in a set range and usually was increased to midrange within 10 to 14 days. Dosing remained flexible within these ranges:
- molindone, 10 to 140 mg/d (mean endpoint dose 59.9 mg/d)
- olanzapine, 2.5 to 20 mg/d (mean endpoint dose 11.4 mg/d)
- risperidone, 0.5 to 6 mg/d (mean endpoint dose 2.8 mg/d).
Benztropine, ≥1 mg/d, was given to all patients treated with molindone, 14% of those treated with olanzapine, and 34% of those treated with risperidone to prevent or manage akathisia.
Efficacy: Two criteria defined treatment response: a Clinical Global Impression improvement score of 1 or 2 and a ≥20% reduction in baseline Positive and Negative Syndrome Scale (PANSS) score. Tolerability outcomes included neurologic side effects, weight changes, laboratory analyses, vital signs, ECG, serious adverse events, and treatment discontinuation. Extrapyramidal symptoms were monitored with involuntary movement and akathisia scales.
Observed PANSS total score by week of treatment
Mean Positive and Negative Symptom Scale (PANSS) total scores of observed cases during each week of the TEOSS trial. Minimum possible PANSS score is 30; scores >60 typically are viewed as problematic.
Among the 70 patients who completed treatment (25 of 40 with molindone, 17 of 35 olanzapine, and 28 of 41 with risperidone), more than one-half failed to achieve an adequate response. Response rates were 50% with molindone, 34% with olanzapine, and 46% with risperidone. The atypical antipsychotics did not show greater efficacy than molindone, and mean reductions in psychotic symptoms were modest (20% to 34% on the PANSS). Mean medication doses were midrange and considered moderate.
Tolerability: Sedation, irritability, and anxiety were frequent adverse events. Patients receiving molindone reported significantly higher rates of akathisia (P < .0008). Those receiving olanzapine reported significantly higher rates of weight gain (P < .0001) and were the only group with increased lipid and insulin serum levels and liver function tests. Patients in the risperidone group reported significantly higher rates of constipation (P < .021) and were the only group that experienced elevated serum prolactin.
Source: Sikich L, Frazier JA, McClellan J, et al. Double-blind comparison of first- and second-generation antipsychotics in early-onset schizophrenia and schizoaffective disorder: findings from the Treatment of Early-Onset Schizophrenia Spectrum disorders (TEOSS) study. Am J Psychiatry. 2008;165:1420-1431
Choosing antipsychotics
DR. KOWATCH: Let’s say you’re seeing psychosis in a 12-year-old whom you think is schizophrenic, and he or she has not yet received an antipsychotic. What are your top 3 treatment choices?
DR. FRAZIER: The first agent I usually select is risperidone. We have the most data on the use of this atypical antipsychotic in children and adolescents, and most psychotic children I see do better with a bit more D2 blockade than some of the other atypicals provide. That said, I remain concerned about risperidone’s side effects—such as weight gain and increased serum prolactin—so my usual second-line agent is aripiprazole.
I became interested in the complicated overlap between pervasive developmental disorders spectrum and psychotic disorders early in my training. More is known about prodromal symptoms in adolescents and adults than in children.
A group in the Netherlands5 compared 32 adolescents with severe early deficits in affect regulation, anxiety, disturbed social relationships, and thought disorder (characterized as “multiple complex developmental disorder” [MCDD]) with 80 adolescents with prodromal psychotic symptoms who met criteria for “at-risk mental state” (ARMS). Three-quarters of the children with MCDD (78%) were found to meet criteria for ARMS, and the 2 groups showed similar schizotypal traits, disorganization, and prodromal symptoms.
Signs of progression to psychosis and schizophrenia in children typically include:
- change in personality
- decrease in functioning or decline in ability to perform at school
- unusual thoughts or behaviors
- crippling anxiety
- supersensitivity to stress.
With experience, the clinician can more clearly differentiate the prodromal signs of psychosis from normal childhood behaviors. Children who are psychotic often don’t make good eye contact. When you try to engage them in discussion about hearing voices, they’re inattentive and internally preoccupied.
Normal vs psychotic children. You want a child in the latency age to have a rich fantasy life. If they do not, that raises concerns. Both normal and psychotic children sometimes say an imaginary friend told them something. Normal children eventually will admit this friend is imaginary. When children are psychotic, especially at an early age, you can’t pull them out of thinking about the imaginary friend, and they can’t distinguish fantasy from reality. Psychotic children also hear imaginary friends talking to them much more often.
Normal children usually are not afraid of their imaginary friends, whereas psychotic children—particularly adolescents—often are afraid of the voices they hear. However, if a psychotic child has heard voices from a young age, the voices aren’t always ego-dystonic. The girl I mentioned at the beginning of this article likes having the voices around. In fact, she gets uncomfortable when the voices are quiet.—Jean A. Frazier, MD
DR. KOWATCH: Why do you like aripiprazole for this patient population?
DR. FRAZIER: Aripiprazole doesn’t tend to be associated with as much weight gain as olanzapine or risperidone, although I’ve had children—especially in the autism spectrum—who have gained quite a bit of weight on aripiprazole. Clinically, I’ve noticed that aripiprazole seems to brighten up children’s affect. It also seems to help many children in my practice with attentional symptoms, although that’s anecdotal.
Although we don’t have a lot of data to inform this discussion about aripiprazole, a placebo-controlled study of 302 adolescents diagnosed with schizophrenia showed that aripiprazole, 10 mg/d, targeted negative symptoms fairly well, based on changes from baseline in PANSS (Positive and Negative Syndrome Scale) total scores. This was a 6-week multicenter, double-blind, randomized, trial.2
Ultimately, cognition in patients with schizophrenia is the strongest predictor of success in the workplace and in school. We need data on what happens to neurocognitive functioning with aripiprazole—and all the other atypical agents.
DR. KOWATCH: What would be your third-line agent?
DR. FRAZIER: Well, that varies for me. I’m trying to match the medication I use with the individual patient, and at this point I prescribe based on the side-effect profile more than anything else. I also consider if the child has a family member who has suffered from a similar condition and what agents the family member responded to.
Let’s say I have a child who has tried 1 or 2 atypical antipsychotics and has not had a good response. Many times I decide to try yet another atypical, and often I will try quetiapine. But after a patient has not responded to 2 atypicals, I might start thinking about a typical agent or clozapine. I use clozapine quite a bit. I find it is the most efficacious agent available, and the data speak to this as well.3,4 It has been truly remarkable for some children in my practice.
Less than 50% chance of efficacy?
DR. KOWATCH: The TEOSS study found 50% or lower response rates across 8 weeks of antipsychotic treatment. Clinically, what kind of response rates do you see with antipsychotics in children and adolescents?
DR. FRAZIER: I probably see about a 50% response rate in my practice as well. It’s variable, and the earlier the onset of the illness, the harder it is to treat.
DR. KOWATCH: Do you ever combine a typical antipsychotic with an atypical?
DR. FRAZIER: I try not to, but a number of children in the schizophrenia spectrum have enduring positive symptoms after 2 or 3 trials of atypical antipsychotics. Sometimes adding a touch of a typical agent can improve the situation. The typicals I usually try are perphenazine (around 8 to 16 mg/d) or molin done (around 20 to 60 mg/d). Sometimes I use a very low dose of haloperidol (such as 0.5 to 2 mg/d) with an atypical agent, and it can be quite effective.
DR. KOWATCH: That has been our experience as well; sometimes combining typical and atypical agents improves response. Besides medications, what do you consider an optimal treatment plan for a child or adolescent with psychosis?
DR. FRAZIER: These children need a multi-modal approach. Pharmacotherapy is the cornerstone because you want to decrease positive symptoms of psychosis, but often these children require therapeutic school placements or residential programs. If they’re old enough, cognitive-behavioral therapy can help by teaching them skills to manage ongoing psychotic symptoms. Older teens often have comorbid substance abuse and may require substance abuse intervention.
Are antipsychotics overused?
DR. KOWATCH: Do you think antipsychotics are overused in pediatric patients with psychosis?
DR. FRAZIER: In pediatric patients with psychosis? No.
DR. KOWATCH: What about in pediatric patients with behavioral disorders?
DR. FRAZIER: We need more studies to inform our practice and to be mindful of the evidence. Most children with schizophrenia have substantial developmental challenges (Box 2).5 In the autism spectrum, often an atypical antipsychotic is the only agent that can help a patient who is aggressive, self-injurious, or agitated.
In terms of bipolar disorder in children and adolescents, it would be ideal if we had more head-to-head comparator studies to inform our prescriptive practice. For example, we need more studies comparing traditional mood stabilizers such as lithium with the atypical agents.
Of course it would be ideal if we could use monotherapy in children who suffer from bipolar disorder and schizophrenia. But early-onset bipolar disorder—like early-onset schizophrenia—can be very difficult to treat and often requires more than 1 agent.
In a recent study of a pharmacotherapy algorithm for treating pediatric bipolar disorder,3 the children who did the best were on a combination of a mood stabilizer and an atypical antipsychotic. That has been my experience, too. I do my best to manage children on a mood stabilizer alone, but I rarely have been able to do that.
In terms of attention-deficit/hyperactivity disorder (ADHD), it depends on what’s going on with the child. Certain children with an ADHD diagnosis have complicated behavioral issues. First I would wonder if they have a different diagnosis, particularly if it gets to the point that an atypical agent is being considered. But sometimes it becomes a question of treating pronounced aggression. We need more studies to inform what we do. Some studies indicate that stimulants can be quite helpful for the aggressive child with ADHD.7
DR. KOWATCH: I don’t see any child and adolescent psychiatrist in the United States using antipsychotics to treat uncomplicated ADHD. The kids we see [at specialty clinics] have comorbid problems such as conduct disorder, oppositional-defiant disorder, mood instability—whatever you want to call it. And we’re seeing these patients because they haven’t done well on other medications, such as stimulants. Usually the parents are desperate because these children are moody and aggressive. I don’t think anybody wants to treat children with antipsychotics or mood stabilizers, but it’s what keeps these children well.
DR. FRAZIER: Yes, I agree.
Related resources
- Longitudinal assessment and monitoring of clinical status and brain function in adolescents and adults. Boston Center for Intervention Development and Applied Research (CIDAR) study. www.bostoncidar.org.
- Frazier JA, Hodge S, Breeze JL, et al. Diagnostic and sex effects on limbic volumes in early-onset bipolar disorder and schizophrenia. Schizophr Bull. 2008;34(1):37-46.
- Frazier JA, McClellan J, Findling RL, et al. Treatment of Early-Onset Schizophrenia Spectrum disorders (TEOSS): demographic and clinical characteristics. J Am Acad Child Adolesc Psychiatry. 2007;46:979-988.
Drug brand names
- Aripiprazole • Abilify
- Benztropine • Cogentin
- Clozapine • Clozaril
- Haloperidol • Haldol
- Metformin • Glucophage
- Molindone • Moban
- Olanzapine • Zyprexa
- Perphenazine • Trilafon
- Quetiapine • Seroquel
- Risperidone • Risperdal
Disclosures
Dr. Kowatch receives grant/research support from the Stanley Foundation, National Institute of Mental Health, National Institute of Child Health and Human Development, and the National Alliance for Research on Schizophrenia and Depression. He is a consultant to AstraZeneca and Forest Pharmaceuticals and a speaker for AstraZeneca.
Dr. Frazier receives grant/research support from Bristol-Myers Squibb, Eli Lilly and Company, GlaxoSmithKline, Johnson & Johnson, Neuropharm, Otsuka America Pharmaceuticals, and Pfizer Inc.
“A patient I’ve seen for a number of years had been diagnosed in the pervasive developmental disorder spectrum, but she was quite atypical. Her perseverative thinking focused on a fantasy world, and she was so preoccupied that it was very difficult to pull her out of it. Now at age 12, she has a full-blown psychotic disorder, and the fantasy world is enveloping her. She hears people talking to her all day long.”
Jean A. Frazier, MD, who treats this patient and other children with psychotic disorders, was 1 of 4 principal investigators in the Treatment of Early-Onset Schizophrenia Spectrum Disorders (TEOSS) study, a randomized, double-blind, multisite trial funded by the National Institute of Mental Health. The study, published in November 2008,1 compared the efficacy and tolerability of 3 antipsychotics—olanzapine, risperidone, and molindone—in pediatric patients with schizophrenia or schizoaffective disorder (Box 1).
Dr. Frazier discusses the unexpected findings of the TEOSS trial with Current Psychiatry Section Editor Robert A. Kowatch, MD, PhD. Based on the trial findings and her experience, she tells how she makes decisions when prescribing antipsychotics for children and adolescents with schizophrenia and related disorders.
DR. KOWATCH: The TEOSS trial found no significant differences in efficacy between molindone and the atypical antipsychotics (olanzapine and risperidone) included in the study. You’ve prescribed both typical and atypical antipsychotics in research and in your clinical practice. Do you believe there’s any difference between the 2 classes?
DR. FRAZIER: There are some differences. For example, treatment-refractory patients, especially young children, sometimes need more D2 blockade than some atypical antipsychotics provide. I’ve seen more extra pyramidal side effects with the typical antipsychotics than the atypicals, although it’s not uncommon to see some akathisia with aripiprazole or some dystonia and dyskinesia with risperidone.
DR. KOWATCH: What are the benefits and risks of using antipsychotics in young children?
DR. FRAZIER: The benefit is that antipsychotics can decrease children’s suffering and get them more centered in reality so they can enjoy their friends and progress in school. And when that happens, it’s wonderful. What are the risks? With the atypicals my greatest concern is weight gain, and with the typical agents it’s tardive dyskinesia.
DR. KOWATCH: Have you changed the way you prescribe antipsychotics as a result of the TEOSS study?
DR. FRAZIER: Actually, I have. Clinicians have to be very careful about selecting psychotropic agents that can worsen pediatric-onset obesity. Olanzapine is an effective agent for targeting psychosis and mood symptoms, but the weight gain associated with it is a concern. I do not prescribe olanzapine as much as I have in the past, although I keep it in my armamentarium and tend to reserve it for third- or fourth-line therapy.
I have found molindone to be quite effective in children with schizophrenia or schizoaffective disorder, especially in those who have gained a lot of weight on atypical antipsychotics. They usually lose weight on molindone.
DR. KOWATCH: Do you think the TEOSS study had adequate power to demonstrate differences among molindone, olanzapine, and risperidone?
DR. FRAZIER: We enrolled 119 patients—which is large for a study such as this—but we did not reach our target of 168 patients, which might have increased our power to detect differences. Among the children we did enroll, the 3 antipsychotics showed no difference in efficacy, but the meaningful finding of this study to me was the side effect profile of these agents.
DR. KOWATCH: You mean weight gain with olanzapine and extrapyramidal symptoms with molindone?
DR. FRAZIER: Yes.
Managing side effects
DR. KOWATCH: How do you manage antipsychotic side effects?
DR. FRAZIER: For any of the antipsychotics’ side effects, you have to decide whether to continue the agent or switch to another anti psychotic. For example, I’ve had a number of children—many with significant weight problems—whose psychotic symptoms have responded only to risperidone. So we put them back on risperidone, and the decision then becomes what can we do to help with the weight gain while continuing that agent.
For weight gain, I think the best intervention is diet, exercise, and drinking a lot of water, but that can be effective only if you engage the patient’s entire family in the intervention as well. Short of that, a number of pharmacologic interventions have been studied, although not specifically in children.
In an open-label trial our group conducted with 11 children age 10 to 18 years who had gained weight while taking atypical antipsychotics, metformin decreased lipid levels and body mass index but not significantly. I’ve followed these children in my practice, however, and all those who continued taking metformin over a period of months lost weight.
TEOSS study adds to debate about efficacy and tolerability
The 5-year National Institute of Mental Health-funded Treatment of Early-Onset Schizophrenia Spectrum Disorders (TEOSS) trial began with an ambitious goal: to compare the efficacy and safety of 1 typical and 2 atypical antipsychotics in children age 8 to 19 with schizophrenia. The primary hypothesis was that atypical agents would show greater efficacy and tolerability when given for 8 weeks. Instead, the atypical agents showed no greater efficacy, and adverse effects occurred with all 3 antipsychotics. Because the trial was designed for 168 subjects but enrolled 119, it may not have been adequately powered to detect differences among the 3 agents.
Medications: Most of the 116 children who received medications were severely ill with psychotic symptoms when randomly assigned to 1 of the 3 antipsychotics for 8 weeks of double-blind treatment. Administration began at the lowest dose in a set range and usually was increased to midrange within 10 to 14 days. Dosing remained flexible within these ranges:
- molindone, 10 to 140 mg/d (mean endpoint dose 59.9 mg/d)
- olanzapine, 2.5 to 20 mg/d (mean endpoint dose 11.4 mg/d)
- risperidone, 0.5 to 6 mg/d (mean endpoint dose 2.8 mg/d).
Benztropine, ≥1 mg/d, was given to all patients treated with molindone, 14% of those treated with olanzapine, and 34% of those treated with risperidone to prevent or manage akathisia.
Efficacy: Two criteria defined treatment response: a Clinical Global Impression improvement score of 1 or 2 and a ≥20% reduction in baseline Positive and Negative Syndrome Scale (PANSS) score. Tolerability outcomes included neurologic side effects, weight changes, laboratory analyses, vital signs, ECG, serious adverse events, and treatment discontinuation. Extrapyramidal symptoms were monitored with involuntary movement and akathisia scales.
Observed PANSS total score by week of treatment
Mean Positive and Negative Symptom Scale (PANSS) total scores of observed cases during each week of the TEOSS trial. Minimum possible PANSS score is 30; scores >60 typically are viewed as problematic.
Among the 70 patients who completed treatment (25 of 40 with molindone, 17 of 35 olanzapine, and 28 of 41 with risperidone), more than one-half failed to achieve an adequate response. Response rates were 50% with molindone, 34% with olanzapine, and 46% with risperidone. The atypical antipsychotics did not show greater efficacy than molindone, and mean reductions in psychotic symptoms were modest (20% to 34% on the PANSS). Mean medication doses were midrange and considered moderate.
Tolerability: Sedation, irritability, and anxiety were frequent adverse events. Patients receiving molindone reported significantly higher rates of akathisia (P < .0008). Those receiving olanzapine reported significantly higher rates of weight gain (P < .0001) and were the only group with increased lipid and insulin serum levels and liver function tests. Patients in the risperidone group reported significantly higher rates of constipation (P < .021) and were the only group that experienced elevated serum prolactin.
Source: Sikich L, Frazier JA, McClellan J, et al. Double-blind comparison of first- and second-generation antipsychotics in early-onset schizophrenia and schizoaffective disorder: findings from the Treatment of Early-Onset Schizophrenia Spectrum disorders (TEOSS) study. Am J Psychiatry. 2008;165:1420-1431
Choosing antipsychotics
DR. KOWATCH: Let’s say you’re seeing psychosis in a 12-year-old whom you think is schizophrenic, and he or she has not yet received an antipsychotic. What are your top 3 treatment choices?
DR. FRAZIER: The first agent I usually select is risperidone. We have the most data on the use of this atypical antipsychotic in children and adolescents, and most psychotic children I see do better with a bit more D2 blockade than some of the other atypicals provide. That said, I remain concerned about risperidone’s side effects—such as weight gain and increased serum prolactin—so my usual second-line agent is aripiprazole.
I became interested in the complicated overlap between pervasive developmental disorders spectrum and psychotic disorders early in my training. More is known about prodromal symptoms in adolescents and adults than in children.
A group in the Netherlands5 compared 32 adolescents with severe early deficits in affect regulation, anxiety, disturbed social relationships, and thought disorder (characterized as “multiple complex developmental disorder” [MCDD]) with 80 adolescents with prodromal psychotic symptoms who met criteria for “at-risk mental state” (ARMS). Three-quarters of the children with MCDD (78%) were found to meet criteria for ARMS, and the 2 groups showed similar schizotypal traits, disorganization, and prodromal symptoms.
Signs of progression to psychosis and schizophrenia in children typically include:
- change in personality
- decrease in functioning or decline in ability to perform at school
- unusual thoughts or behaviors
- crippling anxiety
- supersensitivity to stress.
With experience, the clinician can more clearly differentiate the prodromal signs of psychosis from normal childhood behaviors. Children who are psychotic often don’t make good eye contact. When you try to engage them in discussion about hearing voices, they’re inattentive and internally preoccupied.
Normal vs psychotic children. You want a child in the latency age to have a rich fantasy life. If they do not, that raises concerns. Both normal and psychotic children sometimes say an imaginary friend told them something. Normal children eventually will admit this friend is imaginary. When children are psychotic, especially at an early age, you can’t pull them out of thinking about the imaginary friend, and they can’t distinguish fantasy from reality. Psychotic children also hear imaginary friends talking to them much more often.
Normal children usually are not afraid of their imaginary friends, whereas psychotic children—particularly adolescents—often are afraid of the voices they hear. However, if a psychotic child has heard voices from a young age, the voices aren’t always ego-dystonic. The girl I mentioned at the beginning of this article likes having the voices around. In fact, she gets uncomfortable when the voices are quiet.—Jean A. Frazier, MD
DR. KOWATCH: Why do you like aripiprazole for this patient population?
DR. FRAZIER: Aripiprazole doesn’t tend to be associated with as much weight gain as olanzapine or risperidone, although I’ve had children—especially in the autism spectrum—who have gained quite a bit of weight on aripiprazole. Clinically, I’ve noticed that aripiprazole seems to brighten up children’s affect. It also seems to help many children in my practice with attentional symptoms, although that’s anecdotal.
Although we don’t have a lot of data to inform this discussion about aripiprazole, a placebo-controlled study of 302 adolescents diagnosed with schizophrenia showed that aripiprazole, 10 mg/d, targeted negative symptoms fairly well, based on changes from baseline in PANSS (Positive and Negative Syndrome Scale) total scores. This was a 6-week multicenter, double-blind, randomized, trial.2
Ultimately, cognition in patients with schizophrenia is the strongest predictor of success in the workplace and in school. We need data on what happens to neurocognitive functioning with aripiprazole—and all the other atypical agents.
DR. KOWATCH: What would be your third-line agent?
DR. FRAZIER: Well, that varies for me. I’m trying to match the medication I use with the individual patient, and at this point I prescribe based on the side-effect profile more than anything else. I also consider if the child has a family member who has suffered from a similar condition and what agents the family member responded to.
Let’s say I have a child who has tried 1 or 2 atypical antipsychotics and has not had a good response. Many times I decide to try yet another atypical, and often I will try quetiapine. But after a patient has not responded to 2 atypicals, I might start thinking about a typical agent or clozapine. I use clozapine quite a bit. I find it is the most efficacious agent available, and the data speak to this as well.3,4 It has been truly remarkable for some children in my practice.
Less than 50% chance of efficacy?
DR. KOWATCH: The TEOSS study found 50% or lower response rates across 8 weeks of antipsychotic treatment. Clinically, what kind of response rates do you see with antipsychotics in children and adolescents?
DR. FRAZIER: I probably see about a 50% response rate in my practice as well. It’s variable, and the earlier the onset of the illness, the harder it is to treat.
DR. KOWATCH: Do you ever combine a typical antipsychotic with an atypical?
DR. FRAZIER: I try not to, but a number of children in the schizophrenia spectrum have enduring positive symptoms after 2 or 3 trials of atypical antipsychotics. Sometimes adding a touch of a typical agent can improve the situation. The typicals I usually try are perphenazine (around 8 to 16 mg/d) or molin done (around 20 to 60 mg/d). Sometimes I use a very low dose of haloperidol (such as 0.5 to 2 mg/d) with an atypical agent, and it can be quite effective.
DR. KOWATCH: That has been our experience as well; sometimes combining typical and atypical agents improves response. Besides medications, what do you consider an optimal treatment plan for a child or adolescent with psychosis?
DR. FRAZIER: These children need a multi-modal approach. Pharmacotherapy is the cornerstone because you want to decrease positive symptoms of psychosis, but often these children require therapeutic school placements or residential programs. If they’re old enough, cognitive-behavioral therapy can help by teaching them skills to manage ongoing psychotic symptoms. Older teens often have comorbid substance abuse and may require substance abuse intervention.
Are antipsychotics overused?
DR. KOWATCH: Do you think antipsychotics are overused in pediatric patients with psychosis?
DR. FRAZIER: In pediatric patients with psychosis? No.
DR. KOWATCH: What about in pediatric patients with behavioral disorders?
DR. FRAZIER: We need more studies to inform our practice and to be mindful of the evidence. Most children with schizophrenia have substantial developmental challenges (Box 2).5 In the autism spectrum, often an atypical antipsychotic is the only agent that can help a patient who is aggressive, self-injurious, or agitated.
In terms of bipolar disorder in children and adolescents, it would be ideal if we had more head-to-head comparator studies to inform our prescriptive practice. For example, we need more studies comparing traditional mood stabilizers such as lithium with the atypical agents.
Of course it would be ideal if we could use monotherapy in children who suffer from bipolar disorder and schizophrenia. But early-onset bipolar disorder—like early-onset schizophrenia—can be very difficult to treat and often requires more than 1 agent.
In a recent study of a pharmacotherapy algorithm for treating pediatric bipolar disorder,3 the children who did the best were on a combination of a mood stabilizer and an atypical antipsychotic. That has been my experience, too. I do my best to manage children on a mood stabilizer alone, but I rarely have been able to do that.
In terms of attention-deficit/hyperactivity disorder (ADHD), it depends on what’s going on with the child. Certain children with an ADHD diagnosis have complicated behavioral issues. First I would wonder if they have a different diagnosis, particularly if it gets to the point that an atypical agent is being considered. But sometimes it becomes a question of treating pronounced aggression. We need more studies to inform what we do. Some studies indicate that stimulants can be quite helpful for the aggressive child with ADHD.7
DR. KOWATCH: I don’t see any child and adolescent psychiatrist in the United States using antipsychotics to treat uncomplicated ADHD. The kids we see [at specialty clinics] have comorbid problems such as conduct disorder, oppositional-defiant disorder, mood instability—whatever you want to call it. And we’re seeing these patients because they haven’t done well on other medications, such as stimulants. Usually the parents are desperate because these children are moody and aggressive. I don’t think anybody wants to treat children with antipsychotics or mood stabilizers, but it’s what keeps these children well.
DR. FRAZIER: Yes, I agree.
Related resources
- Longitudinal assessment and monitoring of clinical status and brain function in adolescents and adults. Boston Center for Intervention Development and Applied Research (CIDAR) study. www.bostoncidar.org.
- Frazier JA, Hodge S, Breeze JL, et al. Diagnostic and sex effects on limbic volumes in early-onset bipolar disorder and schizophrenia. Schizophr Bull. 2008;34(1):37-46.
- Frazier JA, McClellan J, Findling RL, et al. Treatment of Early-Onset Schizophrenia Spectrum disorders (TEOSS): demographic and clinical characteristics. J Am Acad Child Adolesc Psychiatry. 2007;46:979-988.
Drug brand names
- Aripiprazole • Abilify
- Benztropine • Cogentin
- Clozapine • Clozaril
- Haloperidol • Haldol
- Metformin • Glucophage
- Molindone • Moban
- Olanzapine • Zyprexa
- Perphenazine • Trilafon
- Quetiapine • Seroquel
- Risperidone • Risperdal
Disclosures
Dr. Kowatch receives grant/research support from the Stanley Foundation, National Institute of Mental Health, National Institute of Child Health and Human Development, and the National Alliance for Research on Schizophrenia and Depression. He is a consultant to AstraZeneca and Forest Pharmaceuticals and a speaker for AstraZeneca.
Dr. Frazier receives grant/research support from Bristol-Myers Squibb, Eli Lilly and Company, GlaxoSmithKline, Johnson & Johnson, Neuropharm, Otsuka America Pharmaceuticals, and Pfizer Inc.
1. Sikich L, Frazier JA, McClellan J, et al. Double-blind comparison of first- and second-generation antipsychotics in early-onset schizophrenia and schizoaffective disorder: findings from the Treatment of Early-Onset Schizophrenia Spectrum Disorders (TEOSS) study. Am J Psychiatry. 2008;165:1420-1431.
2. Findling RL, Robb A, Nyilas M, et al. A multiple-center, randomized, double-blind, placebo-controlled study of oral aripiprazole for treatment of adolescents with schizophrenia. Am J Psychiatry. 2008;165(11):1432-1441.
3. Findling RL, Frazier JA, Gerbino-Rosen G, et al. Is there a role for clozapine in the treatment of children and adolescents? J Am Acad Child Adolesc Psychiatry. 2007;46(3):423-428.
4. Kim Y, Kim BN, Cho SC, et al. Long-term sustained benefits of clozapine treatment in refractory early onset schizophrenia: a retrospective study in Korean children and adolescents. Hum Psychopharmacol. 2008;23(8):715-722.
5. Sprong M, Becker HE, Schothorst PF, et al. Pathways to psychosis: a comparison of the pervasive developmental disorder subtype multiple complex developmental disorder and the “at risk mental state.” Schizophr Res. 2008;99:38-47.
6. Pavuluri MN, Henry DB, Devineni B, et al. A pharmacotherapy algorithm for stabilization and maintenance of pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2004;43(7):859-867.
7. Sinzig J, Döpfner M, Lehmkuhl G, et al. Long-acting methylphenidate has an effect on aggressive behavior in children with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2007;17(4):421-432.
1. Sikich L, Frazier JA, McClellan J, et al. Double-blind comparison of first- and second-generation antipsychotics in early-onset schizophrenia and schizoaffective disorder: findings from the Treatment of Early-Onset Schizophrenia Spectrum Disorders (TEOSS) study. Am J Psychiatry. 2008;165:1420-1431.
2. Findling RL, Robb A, Nyilas M, et al. A multiple-center, randomized, double-blind, placebo-controlled study of oral aripiprazole for treatment of adolescents with schizophrenia. Am J Psychiatry. 2008;165(11):1432-1441.
3. Findling RL, Frazier JA, Gerbino-Rosen G, et al. Is there a role for clozapine in the treatment of children and adolescents? J Am Acad Child Adolesc Psychiatry. 2007;46(3):423-428.
4. Kim Y, Kim BN, Cho SC, et al. Long-term sustained benefits of clozapine treatment in refractory early onset schizophrenia: a retrospective study in Korean children and adolescents. Hum Psychopharmacol. 2008;23(8):715-722.
5. Sprong M, Becker HE, Schothorst PF, et al. Pathways to psychosis: a comparison of the pervasive developmental disorder subtype multiple complex developmental disorder and the “at risk mental state.” Schizophr Res. 2008;99:38-47.
6. Pavuluri MN, Henry DB, Devineni B, et al. A pharmacotherapy algorithm for stabilization and maintenance of pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2004;43(7):859-867.
7. Sinzig J, Döpfner M, Lehmkuhl G, et al. Long-acting methylphenidate has an effect on aggressive behavior in children with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2007;17(4):421-432.