User login
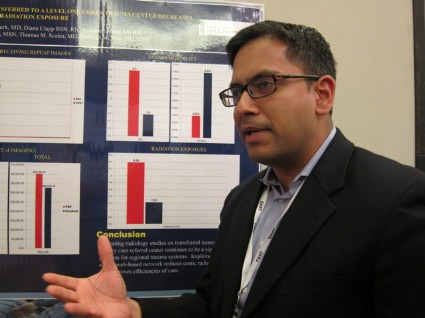
NAPLES, FLA. – Implementing a cloud-based network for sharing radiological images reduced radiation exposure and costs at a Level 1 tertiary care trauma center.
The number of trauma patients who underwent the exact same imaging study decreased significantly from 62% to 47% in the 6 months after the network was available (P less than .01).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This resulted in a significant 19.2% decline in radiation exposure (mean 8.39 mSv vs. 7.23 mSv; P less than .01), Dr. Mayur Narayan reported at the annual meeting of the Eastern Association for the Surgery of Trauma.
"I think it’s a potential game changer," he said. "... The concept is important. The way we’re doing business currently is not sustainable."
Patients transferred within a regional trauma system to a tertiary care referral center frequently have prior radiology studies, but often undergo repeat imaging because of poor image quality, incompatible imaging software, or misplaced imaging discs. This can delay patient management, bring unwelcome radiation, and raise health care costs, explained Dr. Narayan, with the R Adams Cowley Shock Trauma Center at the University of Maryland Medical Center in Baltimore.
To reverse this trend, the center set up a secure, electronic (lifeIMAGE) network that uses a single platform for all medical image exchanges. Physicians can retrieve outside exams via the cloud or merge any or all picture archiving and communication system (PACS) data into their own PACS.
Ten hospitals are now on board and prospective data have been analyzed for 1,950 patients transferred to the trauma center between Jan. 1 and June 30, 2011, (pre-network) and between Jan. 1 and June 30, 2012, (post-network). About 8,500 patients are transferred to the trauma center annually from across the state. Patients in both time periods had similar demographics and Injury Severity Scores (mean 12).
In the 6 months after the network was implemented, the cost of imaging per patient dropped 18.7% ($413 vs. $333; P less than .01), while total imaging costs declined from $401,765 to $326,756 during the same period, Dr. Narayan said.
The most common repeat study in the analysis was an abdominal pelvic CT scan.
Inexplicably, hospital length of stay also declined from 4.4 days to 3.8 days (P = .07), he said. In-hospital mortality was unchanged (3.8% vs. 4.4%; P = .52).
The network cost Cowley Shock Trauma about $30,000 to set up, but other hospital groups are working to provide similar software for free, Dr. Narayan noted.
"The upfront costs should go away," he said.
During a discussion of the poster, one attendee said they set up a similar cloud-based system for their region, but no one used it. "I think it’s because small hospitals don’t see a lot of trauma. They have one or two patients maybe a month that would require transfer and with different people at the CT scanner every night, there’s no uniformity on how to do it," he said.
Others, however, noted that image sharing between hospitals has been fully integrated into their transfer algorithm, prompting calls between hospital radiology units, so that PAC files and patient record numbers have already been merged before the patient ever arrives in the trauma bay.
The Radiological Society of North America has also harnessed cloud-based computing to allow consumers to share their images and interpretations with any provider, regardless of institutional affiliation. According to 20-month follow-up data reported in late 2013, four out of five patients and 9 out of 10 physicians were satisfied with the RSNA Image Share network. A full 90% of patients were comfortable with the amount of privacy provided by the network, though some criticized the site for being "clunky" to navigate.
Dr. Narayan reported having no financial disclosures.
NAPLES, FLA. – Implementing a cloud-based network for sharing radiological images reduced radiation exposure and costs at a Level 1 tertiary care trauma center.
The number of trauma patients who underwent the exact same imaging study decreased significantly from 62% to 47% in the 6 months after the network was available (P less than .01).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This resulted in a significant 19.2% decline in radiation exposure (mean 8.39 mSv vs. 7.23 mSv; P less than .01), Dr. Mayur Narayan reported at the annual meeting of the Eastern Association for the Surgery of Trauma.
"I think it’s a potential game changer," he said. "... The concept is important. The way we’re doing business currently is not sustainable."
Patients transferred within a regional trauma system to a tertiary care referral center frequently have prior radiology studies, but often undergo repeat imaging because of poor image quality, incompatible imaging software, or misplaced imaging discs. This can delay patient management, bring unwelcome radiation, and raise health care costs, explained Dr. Narayan, with the R Adams Cowley Shock Trauma Center at the University of Maryland Medical Center in Baltimore.
To reverse this trend, the center set up a secure, electronic (lifeIMAGE) network that uses a single platform for all medical image exchanges. Physicians can retrieve outside exams via the cloud or merge any or all picture archiving and communication system (PACS) data into their own PACS.
Ten hospitals are now on board and prospective data have been analyzed for 1,950 patients transferred to the trauma center between Jan. 1 and June 30, 2011, (pre-network) and between Jan. 1 and June 30, 2012, (post-network). About 8,500 patients are transferred to the trauma center annually from across the state. Patients in both time periods had similar demographics and Injury Severity Scores (mean 12).
In the 6 months after the network was implemented, the cost of imaging per patient dropped 18.7% ($413 vs. $333; P less than .01), while total imaging costs declined from $401,765 to $326,756 during the same period, Dr. Narayan said.
The most common repeat study in the analysis was an abdominal pelvic CT scan.
Inexplicably, hospital length of stay also declined from 4.4 days to 3.8 days (P = .07), he said. In-hospital mortality was unchanged (3.8% vs. 4.4%; P = .52).
The network cost Cowley Shock Trauma about $30,000 to set up, but other hospital groups are working to provide similar software for free, Dr. Narayan noted.
"The upfront costs should go away," he said.
During a discussion of the poster, one attendee said they set up a similar cloud-based system for their region, but no one used it. "I think it’s because small hospitals don’t see a lot of trauma. They have one or two patients maybe a month that would require transfer and with different people at the CT scanner every night, there’s no uniformity on how to do it," he said.
Others, however, noted that image sharing between hospitals has been fully integrated into their transfer algorithm, prompting calls between hospital radiology units, so that PAC files and patient record numbers have already been merged before the patient ever arrives in the trauma bay.
The Radiological Society of North America has also harnessed cloud-based computing to allow consumers to share their images and interpretations with any provider, regardless of institutional affiliation. According to 20-month follow-up data reported in late 2013, four out of five patients and 9 out of 10 physicians were satisfied with the RSNA Image Share network. A full 90% of patients were comfortable with the amount of privacy provided by the network, though some criticized the site for being "clunky" to navigate.
Dr. Narayan reported having no financial disclosures.
NAPLES, FLA. – Implementing a cloud-based network for sharing radiological images reduced radiation exposure and costs at a Level 1 tertiary care trauma center.
The number of trauma patients who underwent the exact same imaging study decreased significantly from 62% to 47% in the 6 months after the network was available (P less than .01).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This resulted in a significant 19.2% decline in radiation exposure (mean 8.39 mSv vs. 7.23 mSv; P less than .01), Dr. Mayur Narayan reported at the annual meeting of the Eastern Association for the Surgery of Trauma.
"I think it’s a potential game changer," he said. "... The concept is important. The way we’re doing business currently is not sustainable."
Patients transferred within a regional trauma system to a tertiary care referral center frequently have prior radiology studies, but often undergo repeat imaging because of poor image quality, incompatible imaging software, or misplaced imaging discs. This can delay patient management, bring unwelcome radiation, and raise health care costs, explained Dr. Narayan, with the R Adams Cowley Shock Trauma Center at the University of Maryland Medical Center in Baltimore.
To reverse this trend, the center set up a secure, electronic (lifeIMAGE) network that uses a single platform for all medical image exchanges. Physicians can retrieve outside exams via the cloud or merge any or all picture archiving and communication system (PACS) data into their own PACS.
Ten hospitals are now on board and prospective data have been analyzed for 1,950 patients transferred to the trauma center between Jan. 1 and June 30, 2011, (pre-network) and between Jan. 1 and June 30, 2012, (post-network). About 8,500 patients are transferred to the trauma center annually from across the state. Patients in both time periods had similar demographics and Injury Severity Scores (mean 12).
In the 6 months after the network was implemented, the cost of imaging per patient dropped 18.7% ($413 vs. $333; P less than .01), while total imaging costs declined from $401,765 to $326,756 during the same period, Dr. Narayan said.
The most common repeat study in the analysis was an abdominal pelvic CT scan.
Inexplicably, hospital length of stay also declined from 4.4 days to 3.8 days (P = .07), he said. In-hospital mortality was unchanged (3.8% vs. 4.4%; P = .52).
The network cost Cowley Shock Trauma about $30,000 to set up, but other hospital groups are working to provide similar software for free, Dr. Narayan noted.
"The upfront costs should go away," he said.
During a discussion of the poster, one attendee said they set up a similar cloud-based system for their region, but no one used it. "I think it’s because small hospitals don’t see a lot of trauma. They have one or two patients maybe a month that would require transfer and with different people at the CT scanner every night, there’s no uniformity on how to do it," he said.
Others, however, noted that image sharing between hospitals has been fully integrated into their transfer algorithm, prompting calls between hospital radiology units, so that PAC files and patient record numbers have already been merged before the patient ever arrives in the trauma bay.
The Radiological Society of North America has also harnessed cloud-based computing to allow consumers to share their images and interpretations with any provider, regardless of institutional affiliation. According to 20-month follow-up data reported in late 2013, four out of five patients and 9 out of 10 physicians were satisfied with the RSNA Image Share network. A full 90% of patients were comfortable with the amount of privacy provided by the network, though some criticized the site for being "clunky" to navigate.
Dr. Narayan reported having no financial disclosures.
AT EAST 2014
Major finding: The number of patients who underwent repeat imaging declined from 62% to 47% in the 6 months after the network was implemented (P less than .01).
Data source: Prospective data review of 1,950 trauma patients.
Disclosures: Dr. Narayan reported having no financial disclosures.