User login
In the past, observation services typically did not exceed 24 hours or two calendar days. However, changes in healthcare policy coupled with the impetus to reduce wasteful spending have spurred an atmosphere of scrutiny over hospital admissions. Sometimes there are discrepancies between a hospital’s utilization review committee and a payor’s utilization review committee in determining the appropriateness of healthcare services and supplies, in accordance with each party’s definition of medical necessity. This situation has caused an increase in both the number and cost of observation stays.
In response, subsequent observation-care codes (99224-99226) were developed and published in the 2011 edition of Current Procedural Terminology (CPT).1
Codes and Their Uses
CPT outlines three subsequent observation care codes:
- 99224: Subsequent observation care, per day, for the evaluation and management (E/M) of a patient, which requires at least two of these three key components: problem-focused interval history; problem-focused examination; and medical decision-making that is straightforward or of low complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is stable, recovering, or improving. Physicians typically spend 15 minutes at the bedside and on the patient’s hospital floor or unit.
- 99225: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: expanded problem focused interval history; expanded problem focused examination; and medical decision-making of moderate complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is responding inadequately to therapy or has developed a minor complication. Physicians typically spend 25 minutes at the bedside and on the patient’s hospital floor or unit.
- 99226: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: detailed interval history; detailed examination; and medical decision-making of high complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is unstable or has developed a significant complication or a significant new problem. Physicians typically spend 35 minutes at the bedside and on the patient’s hospital floor or unit.
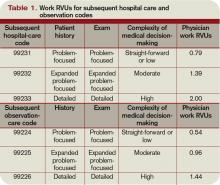
Subsequent observation-care codes replicate the key components and time requirements established for subsequent hospital care services (99231-99233). However, the relative value units (RVUs) of physician work associated with subsequent observation care are not weighted equally (see Table 1, below). Subsequent observation care is a less-intense service, and therefore is valued at a lesser rate.
The attending of record writes the orders to admit the patient to observation (OBS); indicates the reason for the stay; outlines the plan of care; and manages the patient during the stay. Specialists typically are called onto an OBS case for their opinion/advice (i.e. consultants) but do not function as the attending of record.
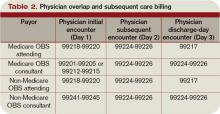
According to CPT 2011, subsequent OBS care codes can be reported by both the attending physician of record and specialists who provide medically necessary, nonoverlapping care to patients on any day other than the admission or discharge day (see Table 2, above). At press time, CMS and private payors had not provided written clarification on the use of subsequent observation-care codes. Therefore, it is imperative to monitor payments, denials, and policy clarifications providing further billing instruction.
On the Horizon
Prior reporting guidelines required the reporting of subsequent observation-care days with established outpatient codes (99212-99215). Some member plans insisted on referrals for all outpatient visits regardless nature of the service. Without the mandated referral for established patient visits performed in the observation setting, physician services were denied for coverage.
The creation of subsequent observation codes might play a role in decreasing these denials. Be sure to review the private payors’ fee schedules for inclusion of 99224-99226 codes. If missing, contact the payor or include it as an agenda item during your contract negotiations.
For more information on observation care services, check out “Observation Care” in the July 2010 issue of The Hospitalist. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology: Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.8. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 16, 2011.
In the past, observation services typically did not exceed 24 hours or two calendar days. However, changes in healthcare policy coupled with the impetus to reduce wasteful spending have spurred an atmosphere of scrutiny over hospital admissions. Sometimes there are discrepancies between a hospital’s utilization review committee and a payor’s utilization review committee in determining the appropriateness of healthcare services and supplies, in accordance with each party’s definition of medical necessity. This situation has caused an increase in both the number and cost of observation stays.
In response, subsequent observation-care codes (99224-99226) were developed and published in the 2011 edition of Current Procedural Terminology (CPT).1
Codes and Their Uses
CPT outlines three subsequent observation care codes:
- 99224: Subsequent observation care, per day, for the evaluation and management (E/M) of a patient, which requires at least two of these three key components: problem-focused interval history; problem-focused examination; and medical decision-making that is straightforward or of low complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is stable, recovering, or improving. Physicians typically spend 15 minutes at the bedside and on the patient’s hospital floor or unit.
- 99225: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: expanded problem focused interval history; expanded problem focused examination; and medical decision-making of moderate complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is responding inadequately to therapy or has developed a minor complication. Physicians typically spend 25 minutes at the bedside and on the patient’s hospital floor or unit.
- 99226: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: detailed interval history; detailed examination; and medical decision-making of high complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is unstable or has developed a significant complication or a significant new problem. Physicians typically spend 35 minutes at the bedside and on the patient’s hospital floor or unit.
Subsequent observation-care codes replicate the key components and time requirements established for subsequent hospital care services (99231-99233). However, the relative value units (RVUs) of physician work associated with subsequent observation care are not weighted equally (see Table 1, below). Subsequent observation care is a less-intense service, and therefore is valued at a lesser rate.
The attending of record writes the orders to admit the patient to observation (OBS); indicates the reason for the stay; outlines the plan of care; and manages the patient during the stay. Specialists typically are called onto an OBS case for their opinion/advice (i.e. consultants) but do not function as the attending of record.
According to CPT 2011, subsequent OBS care codes can be reported by both the attending physician of record and specialists who provide medically necessary, nonoverlapping care to patients on any day other than the admission or discharge day (see Table 2, above). At press time, CMS and private payors had not provided written clarification on the use of subsequent observation-care codes. Therefore, it is imperative to monitor payments, denials, and policy clarifications providing further billing instruction.
On the Horizon
Prior reporting guidelines required the reporting of subsequent observation-care days with established outpatient codes (99212-99215). Some member plans insisted on referrals for all outpatient visits regardless nature of the service. Without the mandated referral for established patient visits performed in the observation setting, physician services were denied for coverage.
The creation of subsequent observation codes might play a role in decreasing these denials. Be sure to review the private payors’ fee schedules for inclusion of 99224-99226 codes. If missing, contact the payor or include it as an agenda item during your contract negotiations.
For more information on observation care services, check out “Observation Care” in the July 2010 issue of The Hospitalist. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology: Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.8. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 16, 2011.
In the past, observation services typically did not exceed 24 hours or two calendar days. However, changes in healthcare policy coupled with the impetus to reduce wasteful spending have spurred an atmosphere of scrutiny over hospital admissions. Sometimes there are discrepancies between a hospital’s utilization review committee and a payor’s utilization review committee in determining the appropriateness of healthcare services and supplies, in accordance with each party’s definition of medical necessity. This situation has caused an increase in both the number and cost of observation stays.
In response, subsequent observation-care codes (99224-99226) were developed and published in the 2011 edition of Current Procedural Terminology (CPT).1
Codes and Their Uses
CPT outlines three subsequent observation care codes:
- 99224: Subsequent observation care, per day, for the evaluation and management (E/M) of a patient, which requires at least two of these three key components: problem-focused interval history; problem-focused examination; and medical decision-making that is straightforward or of low complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is stable, recovering, or improving. Physicians typically spend 15 minutes at the bedside and on the patient’s hospital floor or unit.
- 99225: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: expanded problem focused interval history; expanded problem focused examination; and medical decision-making of moderate complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is responding inadequately to therapy or has developed a minor complication. Physicians typically spend 25 minutes at the bedside and on the patient’s hospital floor or unit.
- 99226: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: detailed interval history; detailed examination; and medical decision-making of high complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is unstable or has developed a significant complication or a significant new problem. Physicians typically spend 35 minutes at the bedside and on the patient’s hospital floor or unit.
Subsequent observation-care codes replicate the key components and time requirements established for subsequent hospital care services (99231-99233). However, the relative value units (RVUs) of physician work associated with subsequent observation care are not weighted equally (see Table 1, below). Subsequent observation care is a less-intense service, and therefore is valued at a lesser rate.
The attending of record writes the orders to admit the patient to observation (OBS); indicates the reason for the stay; outlines the plan of care; and manages the patient during the stay. Specialists typically are called onto an OBS case for their opinion/advice (i.e. consultants) but do not function as the attending of record.
According to CPT 2011, subsequent OBS care codes can be reported by both the attending physician of record and specialists who provide medically necessary, nonoverlapping care to patients on any day other than the admission or discharge day (see Table 2, above). At press time, CMS and private payors had not provided written clarification on the use of subsequent observation-care codes. Therefore, it is imperative to monitor payments, denials, and policy clarifications providing further billing instruction.
On the Horizon
Prior reporting guidelines required the reporting of subsequent observation-care days with established outpatient codes (99212-99215). Some member plans insisted on referrals for all outpatient visits regardless nature of the service. Without the mandated referral for established patient visits performed in the observation setting, physician services were denied for coverage.
The creation of subsequent observation codes might play a role in decreasing these denials. Be sure to review the private payors’ fee schedules for inclusion of 99224-99226 codes. If missing, contact the payor or include it as an agenda item during your contract negotiations.
For more information on observation care services, check out “Observation Care” in the July 2010 issue of The Hospitalist. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology: Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.8. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 16, 2011.