User login
› Develop a diabetes registry and use it to identify patients in need of intervention. B
› Adopt routine depression screening for patients with diabetes. A
› Individualize HbA1c targets based on the patient’s comorbidities and duration of diabetes, among other patient factors. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
The prevalence of diabetes, particularly type 2 (T2D), continues to grow at an unprecedented rate,1 largely because Americans are eating more than in years past and exercising less. At the same time, improvements in treatment are resulting in lower rates of cardiovascular (CV) comorbidities and increased longevity for those with T2D.2,3
Most patients with diabetes are cared for in a primary care setting. With more than a quarter of those who have diabetes (an estimated 7 million Americans) unaware that they have it,4,5 primary care physicians typically see many patients with undiagnosed T2D, as well.
Diabetes care is extremely costly; approximately 20 cents of every health care dollar is spent on those with the disease.6 As a result of this expenditure and increasing adherence to annually updated evidence-based guidelines,7 control is improving, but slowly: Between 2007 and 2010, only 18.8% of patients with diabetes achieved all 3 American Diabetes Association (ADA) goals—for glycemia, blood pressure, and low-density lipoprotein (LDL) cholesterol.8
Part of the problem, experts agree, is that the US health care system is not well suited to manage chronic conditions. This has prompted efforts to develop enhanced delivery modes like the Chronic Care Model and the Patient-Centered Medical Home,9,10 but none has been widely adopted. While groups that have implemented such changes have had significant success,11,12 practices already operating at full capacity often find the work of practice transformation to be daunting.
Difficult as the task may be, we’ve been able to identify—and follow—a number of strategies that serve us well in caring for patients with diabetes. Whether you have the resources to undertake a major practice transformation or simply wish to sharpen your focus, adopting any (or all) of the strategies detailed here will help you optimize diabetes care.
1. Develop a diabetes registry
To have the greatest possible impact on a particular type of patient, you need a way to reliably identify those with a specific condition or set of symptoms. A diabetes registry—a database that starts with basic demographic information for all the patients in your practice with a diabetes diagnosis and is populated with relevant lab results and dates, immunization status, and date of last visit—serves such a function. Some EHRs have this built-in functionality, but most spreadsheet software packages, such as Excel, have the necessary features, as well.
The ideal registry is accurate and up to date, comprehensive, sortable by any of the parameters, and easily accessed, ideally at the point of care. In addition to being able to generate reports for individual patients, the registry should have the ability to track providers—showing, for example, how many (or what percentage) of a provider’s patients have had a diabetes foot exam within the past 12 months. A registry should also be able to pull such statistics for the practice as a whole.
Population management, in which the same standards are applied to all the patients in your practice with a particular diagnosis, is made possible by a registry. Because the registry can be searched by any of the parameters, office staff can use it to identify patients in need of interventions—eg, because of an HbA1c >8%, LDL cholesterol >100 mg/dL, or no recent visit. Medical assistants can then reach out to such patients to ensure that they receive the interventions they need.
Often the greatest challenge associated with the creation of a useful registry is the ability to populate it with accurate and continuously updated data. Using the presence of diabetes on the problem list is a reasonable place to start. But this can create difficulties if any clinicians in the practice have coded for T2D when they were simply testing for it. To avoid such problems, develop clearly defined inclusion criteria before trying to populate the registry.
2. Analyze (and streamline) workflow
Practices that undertake a critical analysis of their workflow often find, as we did, that some staff members are not working to the full capacity of their license. Medical assistants, for example, could give routine immunizations following protocols and standing orders.
To learn more about the workflow in your practice, consider establishing a “change team,” with at least one Teams that conduct “waste walks” to analyze practice workflow often find that some staff members are not working to the full capacity of their license. representative from each position (eg, front office clerk, medical assistant, RN, physician assistant, and family physician). The team can then conduct “waste walks”—literally walking through the workspace to assess office processes from a fresh perspective.
Typically, such teams identify potentially wasteful activities—duplication of efforts or steps that can be done in a more efficient way, or eliminated completely, without ill effect. Medical assistants could stop reconciling medications, for instance, if the primary care providers in the practice are already doing this, and use the time saved to screen patients for depression or neuropathy.
In our experience, physicians who undertake workflow analyses are often surprised to find that members of their staff have many ideas about practice improvements—and are happy to take on more work if they see that doing so would improve patient care. When our staff was reminded of how important blood pressure control is for patients with diabetes, for example, they started placing a sticky note with out-of-range numbers on the computer monitor in the exam room to ensure that this important finding would not be missed.
3. Build a multidisciplinary team
Properly managing a disorder as complex as diabetes requires a team approach. The team might include diabetes educators, nutritionists, behavioral counselors, diabetologists, ophthalmologists, nephrologists, cardiologists, and podiatrists, as well as primary care physicians and family members. Whenever possible, such team members should be integrated within the practice. When this is not the case, transparent communication is critical. A shared EHR can facilitate this.
And while sharing—and gathering—patient data such as blood glucose levels, carbohydrates consumed, intensity and duration of exercise, and daily medications can be time consuming, it is critical to do so. Data review makes it Office staff can be trained to give patients with diabetes a brief depression screen, such as the Patient Health Questionnaire (PHQ-9), at least once a year. possible to prevent acute complications associated with glucose levels that are too high or too low, for example, or to uncover patterns, such as increasing weight or abnormally low (or high) blood sugar at a particular time of day, and take timely corrective actions.
Whether such data analysis occurs within your practice or in the office of a nutritionist or other specialist, diabetes management in a primary care setting benefits from teamwork, too. Medical assistants can administer monofilament tests for neuropathy at each visit, for example, to ensure that this important screening isn’t missed. Office staff can flag the charts of patients in need of additional screening and review before the end of the visit to ensure that the requisite testing has been done. They can also facilitate previsit labs (see “Previsit labs: A simple but effective practice change” on page 546), eliminating the need to contact patients in the days after the visit to review findings and make recommendations that could have been done during the visit.
4. Screen for depression
Patients with diabetes are more likely than those who do not have diabetes to suffer from depression.13 It has also been shown that those who are depressed are less likely to have their diabetes under control than those who are not depressed,14 in part because depressed patients are not as likely to adhere to a medication regimen.15
In some cases, identifying and treating depression can be the key intervention that leads to improved diabetes management. A recent randomized controlled trial found that an integrated approach to managing diabetes and depression resulted in improvements in both glycemic control and depression.16
Without a good screening program, clinicians typically fail to identify depression in a substantial number of their patients.17 A brief screening tool, such as the Patient Health Questionnaire (PHQ-9), can reliably identify depression. Office staff can be trained to give patients with diabetes a depression screen at least once a year when they check in.
5. Screen for undiagnosed diabetes and prediabetes
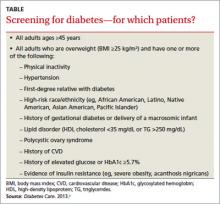
The ADA recommends screening all patients ages 45 years or older for diabetes, as well as overweight adults (BMI ≥25 kg/m2) with one or more additional risk factors (TABLE).7
Screening for diabetes is effective because:
- Diabetes is prevalent (affecting nearly 26 million US residents).5
- The disease is often asymptomatic and many patients do not recognize or acknowledge their symptoms (more than a quarter of those with diabetes are undiagnosed).5
- Accurate, reliable, and inexpensive screening tests are available.
- Early identification provides opportunities for useful interventions.
Traditionally, diabetes was diagnosed by fasting plasma glucose, oral glucose tolerance tests, or—in symptomatic individuals—random glucose elevations. HbA1c was added as a recommended diagnostic test in 2009 and endorsed by the ADA in 2010, with a threshold for diagnosis of ≥6.5%.18
Patients with an HbA1c between 5.7% and 6.4% are considered to have prediabetes, according to the ADA, and have a greater risk for developing both diabetes and CV complications at the higher end of this range. Such patients should be counseled regarding diet, exercise, and other lifestyle issues; metformin should be considered, as well, for those at particularly high risk.7
6. Individualize HbA1c targets
Recent large clinical trials have indicated that no single A1c target is appropriate for all patients.19 Generally speaking, more aggressive, lower targets (eg, <7%) are appropriate for younger patients; recently diagnosed patients who do not have significant CV disease; and those who are highly motivated and have adequate resources and support.20
Higher targets (8% or even higher for some patients) may be appropriate for those who do not fit the above profile. The ADA suggests a fundamentally patient-centered approach to determine an individual’s A1c target, noting that “the desires and values of the patient should be considered, since the achievement of any degree of glucose control requires active participation and commitment.”21
7. Do more to engage patients
Achieving glycemic control and optimizing CV risk factors requires tremendous effort on the part of patients, and sometimes by their families, as well. Unilateral efforts by a physician, no matter how robust and determinedly implemented, nearly always fall short.
Given the complexities associated with managing diabetes, nearly all patients diagnosed with T2D will benefit from education. While some physicians and other health care team members have become very adept at this, there is almost always a role for certified diabetes educators. The ADA recommends that patients receive diabetes self-management education (DSME) according to national standards when their diabetes is diagnosed and as needed thereafter.7
While education is necessary, it is not sufficient. Success occurs only when the patient is educated, engaged, and activated—having the knowledge, skills, and confidence to play the key role in his or her own health care. A recent study with more than 5000 participants found that among those seeing the same physician, patients at higher levels of activation had better health care experiences than those who were less activated.22
Recommendations to patients with diabetes typically require that they carefully obtain, prepare, and consume a particular diet; exercise regularly; manage multiple medications; keep their health care appointments; and engage in regular monitoring of glucose levels and other parameters. Although the health care team may be the source of these recommendations, in every case, it is the patient who must carry them out.
For most patients, the greatest challenge lies in getting and staying motivated to implement all the recommended interventions. Motivational interviewing can be a powerful technique (http://www.motivationalinterview.org/ to learn more). But most patients require a multifaceted approach. Evidence-based principles for promoting and supporting optimal self-management in primary care—including the use of a collaborative, nonjudgmental approach and the support of diverse providers—were identified in a recent publication.23
Many practices have adopted protocols that make it possible for patients with diabetes to have laboratory testing done prior to each visit—a change that benefits both patients and clinicians. office staff can be trained to do the work that this entails, which includes:
- following a protocol to determine which lab tests are indicated
- ensuring that patients have the appropriate lab order for testing before they leave
- contacting patients before their next appointment to ensure that the tests are done and the results available at the time of the visit.
In practices that have adopted such protocols, most visits conclude with the physician giving the patient the requisite lab order. Previsit lab results make an office visit more productive, as they allow for more targeted patient education and counseling, as well as any medication adjustment that is indicated.
This practice also increases efficiency, reducing the time and effort spent trying to communicate with patients after their visit regarding test results and new recommendations. more importantly, it makes it possible for physician and patient to negotiate and reach a consensus about any new interventions during a face-to-face encounter. even accounting for the extra effort of a separate visit for lab testing, we’ve found that most patients appreciate the added value of this approach and are happy to make the effort.
At our facility (UMass Memorial Health Care), primary care providers and diabetes specialists are working together to develop ways to more fully engage patients with diabetes. One such initiative, the Diabetes Scorecard, is delivered to each patient during check-in. Featuring patient-friendly language and simple graphics, the scorecard is automatically populated by data from our EHR, providing an at-a-glance summary that is useful to clinicians and patients alike.
To promote patient self-management and the ability of patients and clinicians to access and carefully review various parameters, several manufacturers of blood glucose meters have developed systems that allow patients to upload the data to a secure, Web-based database that both patients and providers can access and review. We have found, however, that only a few patients—and even fewer clinicians—consistently use them.
Presuming that simple inconvenience is at least part of the reason for such limited use, UMass Memorial has implemented a new system (MyCareTeam™), which works with our EHR provider, Allscripts. This system, which has been shown to improve patient outcomes in other clinical settings, can be launched with a single mouse click from within our EHR. It works with most commercially available glucometers used by our patients, has a user-friendly interface, and provides access to educational resources designed to promote patient engagement. Our goal is to make it easy for patients to upload their own data from a desktop computer, or eventually from mobile devices. Like other systems that electronically capture glucose readings, it prevents patients from excluding any of the results.
At some facilities, physicians “prescribe” apps that patients can use to track chronic diseases on their smartphone or tablet and transmit data, such as glucose readings, to their clinician. Highly rated diabetes apps include Glooko Logbook, Glucose Buddy, and OnTrack Diabetes, to name a few.24
8. Learn more about b-cell function
As the medications available to manage glucose levels have increased in number, it has become more important for clinicians to understand T2D pathophysiology and how various pharmaceutical agents affect it. Central to this understanding are the individual’s sensitivity to insulin’s action and the status of his or her pancreatic b-cell function.
The b-cell dysfunction underlying T2D appears to respond, often dramatically, to even modest weight loss or increased physical activity. Thus, all patients with T2D should be encouraged to pursue daily physical activity and adhere to a diet designed to promote moderate weight loss; any discussion of pharmaceutical approaches should begin with mention of exercise and diet.
For patients whose diabetes is inadequately controlled by lifestyle interventions, medication should be chosen based on an understanding of the pathophysiology and disease state, and particularly, on the patient’s remaining b-cell function. Other considerations include comorbidities, anticipated efficacy, cost, mode of administration, and patient preferences.
Early in the T2D disease process, insulin resistance typically predominates, and b-cell dysfunction is mild. At our facility, we emphasize agents that help restore insulin sensitivity, especially metformin. Patients who are not achieving their glycemic target with lifestyle changes and metformin will benefit from the addition of a secretagogue, which provides a complementary mechanism of action.
Sulfonylureas are inexpensive and effective but potentially problematic because they may cause hypoglycemia and contribute to b-cell exhaustion. This is because they stimulate insulin secretion independent of circulating glucose levels. Glinides work in a similar manner, but have a more rapid onset and a shorter duration of action than sulfonylureas. Thus, they can be effective at mitigating prandial hyperglycemia, but require dosing with meals.
Newer secretagogues such as GLP-1 agonists and DPP-4 inhibitors stimulate secretion of insulin in response to hyperglycemia, reducing the risk of hypoglycemia and ultimately preserving some b-cell function. These newer agents, as well as glinides, are significantly more expensive than sulfony-lureas. GLP-1 agonists have the additional disadvantage of requiring injection. Patients who are Our Diabetes Scorecard, which is automatically populated by data from our EHR, provides an at-a-glance summary that is useful to clinicians and patients alike. far from their glycemic target will benefit from the addition of insulin.
CORRESPONDENCE
Ronald N. Adler, MD, UMass Memorial Medical Center, 279 Lincoln Street, Worcester, MA 01605; [email protected]
1. Danaei G, Finucane MM, Lu Y, et al. National, regional, and global trends in fasting plasma glucose and diabetes preva- lence since 1980. Lancet. 2011;378:31-40.
2. Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643-2653.
3. Ford ES. Trends in the risk for coronary heart disease among adults with diagnosed diabetes in the U.S.: findings from the National Health and Nutrition Examination Survey, 1999- 2008. Diabetes Care. 2011;34:1337-1343.
4. Golden SH. Emerging therapeutic approaches for the manage- ment of diabetes mellitus and macrovascular complications. Am J Cardiol. 2011;108(3 suppl):59B-67B.
5. American Diabetes Association. Diabetes statistics. Edited Au- gust 20, 2013. Available at: http://www.diabetes.org/diabetes- basics/diabetes-statistics/. Accessed September 11, 2013.
6. Economic costs of diabetes in the U.S. in 2007. Diabetes Care. 2008;31:596-615.
7. Standards of medical care in diabetes—2013. Diabetes Care. 2013;36(suppl 1):S11-S66.
8. Stark Casagrande S, Fradkin JE, Saydah SH, et al. The preva- lence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988-2010. Diabetes Care. 2013;36:2271- 2279.
9. Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1:2-4.
10. Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff (Millwood). 2001;20:64-78.
11. Coleman K, Austin BT, Brach C, et al. Evidence on the chronic care model in the new millennium. Health Aff (Millwood). 2009;28:75-85.
12. Bojadzievski T, Gabbay RA. Patient-centered medical home and diabetes. Diabetes Care. 2011;34:1047-1053.
13. Anderson RJ, Freedland KE, Clouse RE, et al. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24:1069-1078.
14. Katon W, Von KM, Ciechanowski P, et al. Behavioral and clini- cal factors associated with depression among individuals with diabetes. Diabetes Care. 2004;27:914-920.
15. Katon W, Russo J, Lin EH, et al. Diabetes and poor disease control: is comorbid depression associated with poor medica- tion adherence or lack of treatment intensification? Psychosom Med. 2009;71:965-972.
16. Bogner HR, Morales KH, de Vries HF, et al. Integrated manage- ment of type 2 diabetes mellitus and depression treatment to improve medication adherence: a randomized controlled trial. Ann Fam Med. 2012;10:15-22.
17. Pignone MP, Gaynes BN, Rushton JL, et al. Screening for de- pression in adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;136:765- 776.
18. Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(suppl 1):S11-S61.
19. Executive summary: standards of medical care in diabe- tes—2013. Diabetes Care. 2013;36(suppl 1):S4-S10.
20. Ismail-Beigi F. Clinical practice. Glycemic management of type 2 diabetes mellitus. N Engl J Med. 2012;366:1319-1327.
21. Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hy- perglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35:1364-1379.
22. Greene J, Hibbard JH, Sacks R, et al. When seeing the same physician, highly activated patients have better experi- ences than less activated patients. Health Aff (Millwood). 2013;32:1299-1305.
23. Battersby M, Von KM, Schaefer J, et al. Twelve evidence-based principles for implementing self-management support in pri- mary care. Jt Comm J Qual Patient Saf. 2010;36:561-570.
24. Watson S. The 13 best diabetes iPhone & Android apps of 2013. Healthline Web site. Available at: http://www.healthline.com/ health-slideshow/top-iphone-android-apps-diabetes. Published August 8, 2013. Accessed September 16, 2013.
› Develop a diabetes registry and use it to identify patients in need of intervention. B
› Adopt routine depression screening for patients with diabetes. A
› Individualize HbA1c targets based on the patient’s comorbidities and duration of diabetes, among other patient factors. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
The prevalence of diabetes, particularly type 2 (T2D), continues to grow at an unprecedented rate,1 largely because Americans are eating more than in years past and exercising less. At the same time, improvements in treatment are resulting in lower rates of cardiovascular (CV) comorbidities and increased longevity for those with T2D.2,3
Most patients with diabetes are cared for in a primary care setting. With more than a quarter of those who have diabetes (an estimated 7 million Americans) unaware that they have it,4,5 primary care physicians typically see many patients with undiagnosed T2D, as well.
Diabetes care is extremely costly; approximately 20 cents of every health care dollar is spent on those with the disease.6 As a result of this expenditure and increasing adherence to annually updated evidence-based guidelines,7 control is improving, but slowly: Between 2007 and 2010, only 18.8% of patients with diabetes achieved all 3 American Diabetes Association (ADA) goals—for glycemia, blood pressure, and low-density lipoprotein (LDL) cholesterol.8
Part of the problem, experts agree, is that the US health care system is not well suited to manage chronic conditions. This has prompted efforts to develop enhanced delivery modes like the Chronic Care Model and the Patient-Centered Medical Home,9,10 but none has been widely adopted. While groups that have implemented such changes have had significant success,11,12 practices already operating at full capacity often find the work of practice transformation to be daunting.
Difficult as the task may be, we’ve been able to identify—and follow—a number of strategies that serve us well in caring for patients with diabetes. Whether you have the resources to undertake a major practice transformation or simply wish to sharpen your focus, adopting any (or all) of the strategies detailed here will help you optimize diabetes care.
1. Develop a diabetes registry
To have the greatest possible impact on a particular type of patient, you need a way to reliably identify those with a specific condition or set of symptoms. A diabetes registry—a database that starts with basic demographic information for all the patients in your practice with a diabetes diagnosis and is populated with relevant lab results and dates, immunization status, and date of last visit—serves such a function. Some EHRs have this built-in functionality, but most spreadsheet software packages, such as Excel, have the necessary features, as well.
The ideal registry is accurate and up to date, comprehensive, sortable by any of the parameters, and easily accessed, ideally at the point of care. In addition to being able to generate reports for individual patients, the registry should have the ability to track providers—showing, for example, how many (or what percentage) of a provider’s patients have had a diabetes foot exam within the past 12 months. A registry should also be able to pull such statistics for the practice as a whole.
Population management, in which the same standards are applied to all the patients in your practice with a particular diagnosis, is made possible by a registry. Because the registry can be searched by any of the parameters, office staff can use it to identify patients in need of interventions—eg, because of an HbA1c >8%, LDL cholesterol >100 mg/dL, or no recent visit. Medical assistants can then reach out to such patients to ensure that they receive the interventions they need.
Often the greatest challenge associated with the creation of a useful registry is the ability to populate it with accurate and continuously updated data. Using the presence of diabetes on the problem list is a reasonable place to start. But this can create difficulties if any clinicians in the practice have coded for T2D when they were simply testing for it. To avoid such problems, develop clearly defined inclusion criteria before trying to populate the registry.
2. Analyze (and streamline) workflow
Practices that undertake a critical analysis of their workflow often find, as we did, that some staff members are not working to the full capacity of their license. Medical assistants, for example, could give routine immunizations following protocols and standing orders.
To learn more about the workflow in your practice, consider establishing a “change team,” with at least one Teams that conduct “waste walks” to analyze practice workflow often find that some staff members are not working to the full capacity of their license. representative from each position (eg, front office clerk, medical assistant, RN, physician assistant, and family physician). The team can then conduct “waste walks”—literally walking through the workspace to assess office processes from a fresh perspective.
Typically, such teams identify potentially wasteful activities—duplication of efforts or steps that can be done in a more efficient way, or eliminated completely, without ill effect. Medical assistants could stop reconciling medications, for instance, if the primary care providers in the practice are already doing this, and use the time saved to screen patients for depression or neuropathy.
In our experience, physicians who undertake workflow analyses are often surprised to find that members of their staff have many ideas about practice improvements—and are happy to take on more work if they see that doing so would improve patient care. When our staff was reminded of how important blood pressure control is for patients with diabetes, for example, they started placing a sticky note with out-of-range numbers on the computer monitor in the exam room to ensure that this important finding would not be missed.
3. Build a multidisciplinary team
Properly managing a disorder as complex as diabetes requires a team approach. The team might include diabetes educators, nutritionists, behavioral counselors, diabetologists, ophthalmologists, nephrologists, cardiologists, and podiatrists, as well as primary care physicians and family members. Whenever possible, such team members should be integrated within the practice. When this is not the case, transparent communication is critical. A shared EHR can facilitate this.
And while sharing—and gathering—patient data such as blood glucose levels, carbohydrates consumed, intensity and duration of exercise, and daily medications can be time consuming, it is critical to do so. Data review makes it Office staff can be trained to give patients with diabetes a brief depression screen, such as the Patient Health Questionnaire (PHQ-9), at least once a year. possible to prevent acute complications associated with glucose levels that are too high or too low, for example, or to uncover patterns, such as increasing weight or abnormally low (or high) blood sugar at a particular time of day, and take timely corrective actions.
Whether such data analysis occurs within your practice or in the office of a nutritionist or other specialist, diabetes management in a primary care setting benefits from teamwork, too. Medical assistants can administer monofilament tests for neuropathy at each visit, for example, to ensure that this important screening isn’t missed. Office staff can flag the charts of patients in need of additional screening and review before the end of the visit to ensure that the requisite testing has been done. They can also facilitate previsit labs (see “Previsit labs: A simple but effective practice change” on page 546), eliminating the need to contact patients in the days after the visit to review findings and make recommendations that could have been done during the visit.
4. Screen for depression
Patients with diabetes are more likely than those who do not have diabetes to suffer from depression.13 It has also been shown that those who are depressed are less likely to have their diabetes under control than those who are not depressed,14 in part because depressed patients are not as likely to adhere to a medication regimen.15
In some cases, identifying and treating depression can be the key intervention that leads to improved diabetes management. A recent randomized controlled trial found that an integrated approach to managing diabetes and depression resulted in improvements in both glycemic control and depression.16
Without a good screening program, clinicians typically fail to identify depression in a substantial number of their patients.17 A brief screening tool, such as the Patient Health Questionnaire (PHQ-9), can reliably identify depression. Office staff can be trained to give patients with diabetes a depression screen at least once a year when they check in.
5. Screen for undiagnosed diabetes and prediabetes
The ADA recommends screening all patients ages 45 years or older for diabetes, as well as overweight adults (BMI ≥25 kg/m2) with one or more additional risk factors (TABLE).7
Screening for diabetes is effective because:
- Diabetes is prevalent (affecting nearly 26 million US residents).5
- The disease is often asymptomatic and many patients do not recognize or acknowledge their symptoms (more than a quarter of those with diabetes are undiagnosed).5
- Accurate, reliable, and inexpensive screening tests are available.
- Early identification provides opportunities for useful interventions.
Traditionally, diabetes was diagnosed by fasting plasma glucose, oral glucose tolerance tests, or—in symptomatic individuals—random glucose elevations. HbA1c was added as a recommended diagnostic test in 2009 and endorsed by the ADA in 2010, with a threshold for diagnosis of ≥6.5%.18
Patients with an HbA1c between 5.7% and 6.4% are considered to have prediabetes, according to the ADA, and have a greater risk for developing both diabetes and CV complications at the higher end of this range. Such patients should be counseled regarding diet, exercise, and other lifestyle issues; metformin should be considered, as well, for those at particularly high risk.7
6. Individualize HbA1c targets
Recent large clinical trials have indicated that no single A1c target is appropriate for all patients.19 Generally speaking, more aggressive, lower targets (eg, <7%) are appropriate for younger patients; recently diagnosed patients who do not have significant CV disease; and those who are highly motivated and have adequate resources and support.20
Higher targets (8% or even higher for some patients) may be appropriate for those who do not fit the above profile. The ADA suggests a fundamentally patient-centered approach to determine an individual’s A1c target, noting that “the desires and values of the patient should be considered, since the achievement of any degree of glucose control requires active participation and commitment.”21
7. Do more to engage patients
Achieving glycemic control and optimizing CV risk factors requires tremendous effort on the part of patients, and sometimes by their families, as well. Unilateral efforts by a physician, no matter how robust and determinedly implemented, nearly always fall short.
Given the complexities associated with managing diabetes, nearly all patients diagnosed with T2D will benefit from education. While some physicians and other health care team members have become very adept at this, there is almost always a role for certified diabetes educators. The ADA recommends that patients receive diabetes self-management education (DSME) according to national standards when their diabetes is diagnosed and as needed thereafter.7
While education is necessary, it is not sufficient. Success occurs only when the patient is educated, engaged, and activated—having the knowledge, skills, and confidence to play the key role in his or her own health care. A recent study with more than 5000 participants found that among those seeing the same physician, patients at higher levels of activation had better health care experiences than those who were less activated.22
Recommendations to patients with diabetes typically require that they carefully obtain, prepare, and consume a particular diet; exercise regularly; manage multiple medications; keep their health care appointments; and engage in regular monitoring of glucose levels and other parameters. Although the health care team may be the source of these recommendations, in every case, it is the patient who must carry them out.
For most patients, the greatest challenge lies in getting and staying motivated to implement all the recommended interventions. Motivational interviewing can be a powerful technique (http://www.motivationalinterview.org/ to learn more). But most patients require a multifaceted approach. Evidence-based principles for promoting and supporting optimal self-management in primary care—including the use of a collaborative, nonjudgmental approach and the support of diverse providers—were identified in a recent publication.23
Many practices have adopted protocols that make it possible for patients with diabetes to have laboratory testing done prior to each visit—a change that benefits both patients and clinicians. office staff can be trained to do the work that this entails, which includes:
- following a protocol to determine which lab tests are indicated
- ensuring that patients have the appropriate lab order for testing before they leave
- contacting patients before their next appointment to ensure that the tests are done and the results available at the time of the visit.
In practices that have adopted such protocols, most visits conclude with the physician giving the patient the requisite lab order. Previsit lab results make an office visit more productive, as they allow for more targeted patient education and counseling, as well as any medication adjustment that is indicated.
This practice also increases efficiency, reducing the time and effort spent trying to communicate with patients after their visit regarding test results and new recommendations. more importantly, it makes it possible for physician and patient to negotiate and reach a consensus about any new interventions during a face-to-face encounter. even accounting for the extra effort of a separate visit for lab testing, we’ve found that most patients appreciate the added value of this approach and are happy to make the effort.
At our facility (UMass Memorial Health Care), primary care providers and diabetes specialists are working together to develop ways to more fully engage patients with diabetes. One such initiative, the Diabetes Scorecard, is delivered to each patient during check-in. Featuring patient-friendly language and simple graphics, the scorecard is automatically populated by data from our EHR, providing an at-a-glance summary that is useful to clinicians and patients alike.
To promote patient self-management and the ability of patients and clinicians to access and carefully review various parameters, several manufacturers of blood glucose meters have developed systems that allow patients to upload the data to a secure, Web-based database that both patients and providers can access and review. We have found, however, that only a few patients—and even fewer clinicians—consistently use them.
Presuming that simple inconvenience is at least part of the reason for such limited use, UMass Memorial has implemented a new system (MyCareTeam™), which works with our EHR provider, Allscripts. This system, which has been shown to improve patient outcomes in other clinical settings, can be launched with a single mouse click from within our EHR. It works with most commercially available glucometers used by our patients, has a user-friendly interface, and provides access to educational resources designed to promote patient engagement. Our goal is to make it easy for patients to upload their own data from a desktop computer, or eventually from mobile devices. Like other systems that electronically capture glucose readings, it prevents patients from excluding any of the results.
At some facilities, physicians “prescribe” apps that patients can use to track chronic diseases on their smartphone or tablet and transmit data, such as glucose readings, to their clinician. Highly rated diabetes apps include Glooko Logbook, Glucose Buddy, and OnTrack Diabetes, to name a few.24
8. Learn more about b-cell function
As the medications available to manage glucose levels have increased in number, it has become more important for clinicians to understand T2D pathophysiology and how various pharmaceutical agents affect it. Central to this understanding are the individual’s sensitivity to insulin’s action and the status of his or her pancreatic b-cell function.
The b-cell dysfunction underlying T2D appears to respond, often dramatically, to even modest weight loss or increased physical activity. Thus, all patients with T2D should be encouraged to pursue daily physical activity and adhere to a diet designed to promote moderate weight loss; any discussion of pharmaceutical approaches should begin with mention of exercise and diet.
For patients whose diabetes is inadequately controlled by lifestyle interventions, medication should be chosen based on an understanding of the pathophysiology and disease state, and particularly, on the patient’s remaining b-cell function. Other considerations include comorbidities, anticipated efficacy, cost, mode of administration, and patient preferences.
Early in the T2D disease process, insulin resistance typically predominates, and b-cell dysfunction is mild. At our facility, we emphasize agents that help restore insulin sensitivity, especially metformin. Patients who are not achieving their glycemic target with lifestyle changes and metformin will benefit from the addition of a secretagogue, which provides a complementary mechanism of action.
Sulfonylureas are inexpensive and effective but potentially problematic because they may cause hypoglycemia and contribute to b-cell exhaustion. This is because they stimulate insulin secretion independent of circulating glucose levels. Glinides work in a similar manner, but have a more rapid onset and a shorter duration of action than sulfonylureas. Thus, they can be effective at mitigating prandial hyperglycemia, but require dosing with meals.
Newer secretagogues such as GLP-1 agonists and DPP-4 inhibitors stimulate secretion of insulin in response to hyperglycemia, reducing the risk of hypoglycemia and ultimately preserving some b-cell function. These newer agents, as well as glinides, are significantly more expensive than sulfony-lureas. GLP-1 agonists have the additional disadvantage of requiring injection. Patients who are Our Diabetes Scorecard, which is automatically populated by data from our EHR, provides an at-a-glance summary that is useful to clinicians and patients alike. far from their glycemic target will benefit from the addition of insulin.
CORRESPONDENCE
Ronald N. Adler, MD, UMass Memorial Medical Center, 279 Lincoln Street, Worcester, MA 01605; [email protected]
› Develop a diabetes registry and use it to identify patients in need of intervention. B
› Adopt routine depression screening for patients with diabetes. A
› Individualize HbA1c targets based on the patient’s comorbidities and duration of diabetes, among other patient factors. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
The prevalence of diabetes, particularly type 2 (T2D), continues to grow at an unprecedented rate,1 largely because Americans are eating more than in years past and exercising less. At the same time, improvements in treatment are resulting in lower rates of cardiovascular (CV) comorbidities and increased longevity for those with T2D.2,3
Most patients with diabetes are cared for in a primary care setting. With more than a quarter of those who have diabetes (an estimated 7 million Americans) unaware that they have it,4,5 primary care physicians typically see many patients with undiagnosed T2D, as well.
Diabetes care is extremely costly; approximately 20 cents of every health care dollar is spent on those with the disease.6 As a result of this expenditure and increasing adherence to annually updated evidence-based guidelines,7 control is improving, but slowly: Between 2007 and 2010, only 18.8% of patients with diabetes achieved all 3 American Diabetes Association (ADA) goals—for glycemia, blood pressure, and low-density lipoprotein (LDL) cholesterol.8
Part of the problem, experts agree, is that the US health care system is not well suited to manage chronic conditions. This has prompted efforts to develop enhanced delivery modes like the Chronic Care Model and the Patient-Centered Medical Home,9,10 but none has been widely adopted. While groups that have implemented such changes have had significant success,11,12 practices already operating at full capacity often find the work of practice transformation to be daunting.
Difficult as the task may be, we’ve been able to identify—and follow—a number of strategies that serve us well in caring for patients with diabetes. Whether you have the resources to undertake a major practice transformation or simply wish to sharpen your focus, adopting any (or all) of the strategies detailed here will help you optimize diabetes care.
1. Develop a diabetes registry
To have the greatest possible impact on a particular type of patient, you need a way to reliably identify those with a specific condition or set of symptoms. A diabetes registry—a database that starts with basic demographic information for all the patients in your practice with a diabetes diagnosis and is populated with relevant lab results and dates, immunization status, and date of last visit—serves such a function. Some EHRs have this built-in functionality, but most spreadsheet software packages, such as Excel, have the necessary features, as well.
The ideal registry is accurate and up to date, comprehensive, sortable by any of the parameters, and easily accessed, ideally at the point of care. In addition to being able to generate reports for individual patients, the registry should have the ability to track providers—showing, for example, how many (or what percentage) of a provider’s patients have had a diabetes foot exam within the past 12 months. A registry should also be able to pull such statistics for the practice as a whole.
Population management, in which the same standards are applied to all the patients in your practice with a particular diagnosis, is made possible by a registry. Because the registry can be searched by any of the parameters, office staff can use it to identify patients in need of interventions—eg, because of an HbA1c >8%, LDL cholesterol >100 mg/dL, or no recent visit. Medical assistants can then reach out to such patients to ensure that they receive the interventions they need.
Often the greatest challenge associated with the creation of a useful registry is the ability to populate it with accurate and continuously updated data. Using the presence of diabetes on the problem list is a reasonable place to start. But this can create difficulties if any clinicians in the practice have coded for T2D when they were simply testing for it. To avoid such problems, develop clearly defined inclusion criteria before trying to populate the registry.
2. Analyze (and streamline) workflow
Practices that undertake a critical analysis of their workflow often find, as we did, that some staff members are not working to the full capacity of their license. Medical assistants, for example, could give routine immunizations following protocols and standing orders.
To learn more about the workflow in your practice, consider establishing a “change team,” with at least one Teams that conduct “waste walks” to analyze practice workflow often find that some staff members are not working to the full capacity of their license. representative from each position (eg, front office clerk, medical assistant, RN, physician assistant, and family physician). The team can then conduct “waste walks”—literally walking through the workspace to assess office processes from a fresh perspective.
Typically, such teams identify potentially wasteful activities—duplication of efforts or steps that can be done in a more efficient way, or eliminated completely, without ill effect. Medical assistants could stop reconciling medications, for instance, if the primary care providers in the practice are already doing this, and use the time saved to screen patients for depression or neuropathy.
In our experience, physicians who undertake workflow analyses are often surprised to find that members of their staff have many ideas about practice improvements—and are happy to take on more work if they see that doing so would improve patient care. When our staff was reminded of how important blood pressure control is for patients with diabetes, for example, they started placing a sticky note with out-of-range numbers on the computer monitor in the exam room to ensure that this important finding would not be missed.
3. Build a multidisciplinary team
Properly managing a disorder as complex as diabetes requires a team approach. The team might include diabetes educators, nutritionists, behavioral counselors, diabetologists, ophthalmologists, nephrologists, cardiologists, and podiatrists, as well as primary care physicians and family members. Whenever possible, such team members should be integrated within the practice. When this is not the case, transparent communication is critical. A shared EHR can facilitate this.
And while sharing—and gathering—patient data such as blood glucose levels, carbohydrates consumed, intensity and duration of exercise, and daily medications can be time consuming, it is critical to do so. Data review makes it Office staff can be trained to give patients with diabetes a brief depression screen, such as the Patient Health Questionnaire (PHQ-9), at least once a year. possible to prevent acute complications associated with glucose levels that are too high or too low, for example, or to uncover patterns, such as increasing weight or abnormally low (or high) blood sugar at a particular time of day, and take timely corrective actions.
Whether such data analysis occurs within your practice or in the office of a nutritionist or other specialist, diabetes management in a primary care setting benefits from teamwork, too. Medical assistants can administer monofilament tests for neuropathy at each visit, for example, to ensure that this important screening isn’t missed. Office staff can flag the charts of patients in need of additional screening and review before the end of the visit to ensure that the requisite testing has been done. They can also facilitate previsit labs (see “Previsit labs: A simple but effective practice change” on page 546), eliminating the need to contact patients in the days after the visit to review findings and make recommendations that could have been done during the visit.
4. Screen for depression
Patients with diabetes are more likely than those who do not have diabetes to suffer from depression.13 It has also been shown that those who are depressed are less likely to have their diabetes under control than those who are not depressed,14 in part because depressed patients are not as likely to adhere to a medication regimen.15
In some cases, identifying and treating depression can be the key intervention that leads to improved diabetes management. A recent randomized controlled trial found that an integrated approach to managing diabetes and depression resulted in improvements in both glycemic control and depression.16
Without a good screening program, clinicians typically fail to identify depression in a substantial number of their patients.17 A brief screening tool, such as the Patient Health Questionnaire (PHQ-9), can reliably identify depression. Office staff can be trained to give patients with diabetes a depression screen at least once a year when they check in.
5. Screen for undiagnosed diabetes and prediabetes
The ADA recommends screening all patients ages 45 years or older for diabetes, as well as overweight adults (BMI ≥25 kg/m2) with one or more additional risk factors (TABLE).7
Screening for diabetes is effective because:
- Diabetes is prevalent (affecting nearly 26 million US residents).5
- The disease is often asymptomatic and many patients do not recognize or acknowledge their symptoms (more than a quarter of those with diabetes are undiagnosed).5
- Accurate, reliable, and inexpensive screening tests are available.
- Early identification provides opportunities for useful interventions.
Traditionally, diabetes was diagnosed by fasting plasma glucose, oral glucose tolerance tests, or—in symptomatic individuals—random glucose elevations. HbA1c was added as a recommended diagnostic test in 2009 and endorsed by the ADA in 2010, with a threshold for diagnosis of ≥6.5%.18
Patients with an HbA1c between 5.7% and 6.4% are considered to have prediabetes, according to the ADA, and have a greater risk for developing both diabetes and CV complications at the higher end of this range. Such patients should be counseled regarding diet, exercise, and other lifestyle issues; metformin should be considered, as well, for those at particularly high risk.7
6. Individualize HbA1c targets
Recent large clinical trials have indicated that no single A1c target is appropriate for all patients.19 Generally speaking, more aggressive, lower targets (eg, <7%) are appropriate for younger patients; recently diagnosed patients who do not have significant CV disease; and those who are highly motivated and have adequate resources and support.20
Higher targets (8% or even higher for some patients) may be appropriate for those who do not fit the above profile. The ADA suggests a fundamentally patient-centered approach to determine an individual’s A1c target, noting that “the desires and values of the patient should be considered, since the achievement of any degree of glucose control requires active participation and commitment.”21
7. Do more to engage patients
Achieving glycemic control and optimizing CV risk factors requires tremendous effort on the part of patients, and sometimes by their families, as well. Unilateral efforts by a physician, no matter how robust and determinedly implemented, nearly always fall short.
Given the complexities associated with managing diabetes, nearly all patients diagnosed with T2D will benefit from education. While some physicians and other health care team members have become very adept at this, there is almost always a role for certified diabetes educators. The ADA recommends that patients receive diabetes self-management education (DSME) according to national standards when their diabetes is diagnosed and as needed thereafter.7
While education is necessary, it is not sufficient. Success occurs only when the patient is educated, engaged, and activated—having the knowledge, skills, and confidence to play the key role in his or her own health care. A recent study with more than 5000 participants found that among those seeing the same physician, patients at higher levels of activation had better health care experiences than those who were less activated.22
Recommendations to patients with diabetes typically require that they carefully obtain, prepare, and consume a particular diet; exercise regularly; manage multiple medications; keep their health care appointments; and engage in regular monitoring of glucose levels and other parameters. Although the health care team may be the source of these recommendations, in every case, it is the patient who must carry them out.
For most patients, the greatest challenge lies in getting and staying motivated to implement all the recommended interventions. Motivational interviewing can be a powerful technique (http://www.motivationalinterview.org/ to learn more). But most patients require a multifaceted approach. Evidence-based principles for promoting and supporting optimal self-management in primary care—including the use of a collaborative, nonjudgmental approach and the support of diverse providers—were identified in a recent publication.23
Many practices have adopted protocols that make it possible for patients with diabetes to have laboratory testing done prior to each visit—a change that benefits both patients and clinicians. office staff can be trained to do the work that this entails, which includes:
- following a protocol to determine which lab tests are indicated
- ensuring that patients have the appropriate lab order for testing before they leave
- contacting patients before their next appointment to ensure that the tests are done and the results available at the time of the visit.
In practices that have adopted such protocols, most visits conclude with the physician giving the patient the requisite lab order. Previsit lab results make an office visit more productive, as they allow for more targeted patient education and counseling, as well as any medication adjustment that is indicated.
This practice also increases efficiency, reducing the time and effort spent trying to communicate with patients after their visit regarding test results and new recommendations. more importantly, it makes it possible for physician and patient to negotiate and reach a consensus about any new interventions during a face-to-face encounter. even accounting for the extra effort of a separate visit for lab testing, we’ve found that most patients appreciate the added value of this approach and are happy to make the effort.
At our facility (UMass Memorial Health Care), primary care providers and diabetes specialists are working together to develop ways to more fully engage patients with diabetes. One such initiative, the Diabetes Scorecard, is delivered to each patient during check-in. Featuring patient-friendly language and simple graphics, the scorecard is automatically populated by data from our EHR, providing an at-a-glance summary that is useful to clinicians and patients alike.
To promote patient self-management and the ability of patients and clinicians to access and carefully review various parameters, several manufacturers of blood glucose meters have developed systems that allow patients to upload the data to a secure, Web-based database that both patients and providers can access and review. We have found, however, that only a few patients—and even fewer clinicians—consistently use them.
Presuming that simple inconvenience is at least part of the reason for such limited use, UMass Memorial has implemented a new system (MyCareTeam™), which works with our EHR provider, Allscripts. This system, which has been shown to improve patient outcomes in other clinical settings, can be launched with a single mouse click from within our EHR. It works with most commercially available glucometers used by our patients, has a user-friendly interface, and provides access to educational resources designed to promote patient engagement. Our goal is to make it easy for patients to upload their own data from a desktop computer, or eventually from mobile devices. Like other systems that electronically capture glucose readings, it prevents patients from excluding any of the results.
At some facilities, physicians “prescribe” apps that patients can use to track chronic diseases on their smartphone or tablet and transmit data, such as glucose readings, to their clinician. Highly rated diabetes apps include Glooko Logbook, Glucose Buddy, and OnTrack Diabetes, to name a few.24
8. Learn more about b-cell function
As the medications available to manage glucose levels have increased in number, it has become more important for clinicians to understand T2D pathophysiology and how various pharmaceutical agents affect it. Central to this understanding are the individual’s sensitivity to insulin’s action and the status of his or her pancreatic b-cell function.
The b-cell dysfunction underlying T2D appears to respond, often dramatically, to even modest weight loss or increased physical activity. Thus, all patients with T2D should be encouraged to pursue daily physical activity and adhere to a diet designed to promote moderate weight loss; any discussion of pharmaceutical approaches should begin with mention of exercise and diet.
For patients whose diabetes is inadequately controlled by lifestyle interventions, medication should be chosen based on an understanding of the pathophysiology and disease state, and particularly, on the patient’s remaining b-cell function. Other considerations include comorbidities, anticipated efficacy, cost, mode of administration, and patient preferences.
Early in the T2D disease process, insulin resistance typically predominates, and b-cell dysfunction is mild. At our facility, we emphasize agents that help restore insulin sensitivity, especially metformin. Patients who are not achieving their glycemic target with lifestyle changes and metformin will benefit from the addition of a secretagogue, which provides a complementary mechanism of action.
Sulfonylureas are inexpensive and effective but potentially problematic because they may cause hypoglycemia and contribute to b-cell exhaustion. This is because they stimulate insulin secretion independent of circulating glucose levels. Glinides work in a similar manner, but have a more rapid onset and a shorter duration of action than sulfonylureas. Thus, they can be effective at mitigating prandial hyperglycemia, but require dosing with meals.
Newer secretagogues such as GLP-1 agonists and DPP-4 inhibitors stimulate secretion of insulin in response to hyperglycemia, reducing the risk of hypoglycemia and ultimately preserving some b-cell function. These newer agents, as well as glinides, are significantly more expensive than sulfony-lureas. GLP-1 agonists have the additional disadvantage of requiring injection. Patients who are Our Diabetes Scorecard, which is automatically populated by data from our EHR, provides an at-a-glance summary that is useful to clinicians and patients alike. far from their glycemic target will benefit from the addition of insulin.
CORRESPONDENCE
Ronald N. Adler, MD, UMass Memorial Medical Center, 279 Lincoln Street, Worcester, MA 01605; [email protected]
1. Danaei G, Finucane MM, Lu Y, et al. National, regional, and global trends in fasting plasma glucose and diabetes preva- lence since 1980. Lancet. 2011;378:31-40.
2. Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643-2653.
3. Ford ES. Trends in the risk for coronary heart disease among adults with diagnosed diabetes in the U.S.: findings from the National Health and Nutrition Examination Survey, 1999- 2008. Diabetes Care. 2011;34:1337-1343.
4. Golden SH. Emerging therapeutic approaches for the manage- ment of diabetes mellitus and macrovascular complications. Am J Cardiol. 2011;108(3 suppl):59B-67B.
5. American Diabetes Association. Diabetes statistics. Edited Au- gust 20, 2013. Available at: http://www.diabetes.org/diabetes- basics/diabetes-statistics/. Accessed September 11, 2013.
6. Economic costs of diabetes in the U.S. in 2007. Diabetes Care. 2008;31:596-615.
7. Standards of medical care in diabetes—2013. Diabetes Care. 2013;36(suppl 1):S11-S66.
8. Stark Casagrande S, Fradkin JE, Saydah SH, et al. The preva- lence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988-2010. Diabetes Care. 2013;36:2271- 2279.
9. Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1:2-4.
10. Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff (Millwood). 2001;20:64-78.
11. Coleman K, Austin BT, Brach C, et al. Evidence on the chronic care model in the new millennium. Health Aff (Millwood). 2009;28:75-85.
12. Bojadzievski T, Gabbay RA. Patient-centered medical home and diabetes. Diabetes Care. 2011;34:1047-1053.
13. Anderson RJ, Freedland KE, Clouse RE, et al. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24:1069-1078.
14. Katon W, Von KM, Ciechanowski P, et al. Behavioral and clini- cal factors associated with depression among individuals with diabetes. Diabetes Care. 2004;27:914-920.
15. Katon W, Russo J, Lin EH, et al. Diabetes and poor disease control: is comorbid depression associated with poor medica- tion adherence or lack of treatment intensification? Psychosom Med. 2009;71:965-972.
16. Bogner HR, Morales KH, de Vries HF, et al. Integrated manage- ment of type 2 diabetes mellitus and depression treatment to improve medication adherence: a randomized controlled trial. Ann Fam Med. 2012;10:15-22.
17. Pignone MP, Gaynes BN, Rushton JL, et al. Screening for de- pression in adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;136:765- 776.
18. Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(suppl 1):S11-S61.
19. Executive summary: standards of medical care in diabe- tes—2013. Diabetes Care. 2013;36(suppl 1):S4-S10.
20. Ismail-Beigi F. Clinical practice. Glycemic management of type 2 diabetes mellitus. N Engl J Med. 2012;366:1319-1327.
21. Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hy- perglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35:1364-1379.
22. Greene J, Hibbard JH, Sacks R, et al. When seeing the same physician, highly activated patients have better experi- ences than less activated patients. Health Aff (Millwood). 2013;32:1299-1305.
23. Battersby M, Von KM, Schaefer J, et al. Twelve evidence-based principles for implementing self-management support in pri- mary care. Jt Comm J Qual Patient Saf. 2010;36:561-570.
24. Watson S. The 13 best diabetes iPhone & Android apps of 2013. Healthline Web site. Available at: http://www.healthline.com/ health-slideshow/top-iphone-android-apps-diabetes. Published August 8, 2013. Accessed September 16, 2013.
1. Danaei G, Finucane MM, Lu Y, et al. National, regional, and global trends in fasting plasma glucose and diabetes preva- lence since 1980. Lancet. 2011;378:31-40.
2. Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643-2653.
3. Ford ES. Trends in the risk for coronary heart disease among adults with diagnosed diabetes in the U.S.: findings from the National Health and Nutrition Examination Survey, 1999- 2008. Diabetes Care. 2011;34:1337-1343.
4. Golden SH. Emerging therapeutic approaches for the manage- ment of diabetes mellitus and macrovascular complications. Am J Cardiol. 2011;108(3 suppl):59B-67B.
5. American Diabetes Association. Diabetes statistics. Edited Au- gust 20, 2013. Available at: http://www.diabetes.org/diabetes- basics/diabetes-statistics/. Accessed September 11, 2013.
6. Economic costs of diabetes in the U.S. in 2007. Diabetes Care. 2008;31:596-615.
7. Standards of medical care in diabetes—2013. Diabetes Care. 2013;36(suppl 1):S11-S66.
8. Stark Casagrande S, Fradkin JE, Saydah SH, et al. The preva- lence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988-2010. Diabetes Care. 2013;36:2271- 2279.
9. Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1:2-4.
10. Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff (Millwood). 2001;20:64-78.
11. Coleman K, Austin BT, Brach C, et al. Evidence on the chronic care model in the new millennium. Health Aff (Millwood). 2009;28:75-85.
12. Bojadzievski T, Gabbay RA. Patient-centered medical home and diabetes. Diabetes Care. 2011;34:1047-1053.
13. Anderson RJ, Freedland KE, Clouse RE, et al. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24:1069-1078.
14. Katon W, Von KM, Ciechanowski P, et al. Behavioral and clini- cal factors associated with depression among individuals with diabetes. Diabetes Care. 2004;27:914-920.
15. Katon W, Russo J, Lin EH, et al. Diabetes and poor disease control: is comorbid depression associated with poor medica- tion adherence or lack of treatment intensification? Psychosom Med. 2009;71:965-972.
16. Bogner HR, Morales KH, de Vries HF, et al. Integrated manage- ment of type 2 diabetes mellitus and depression treatment to improve medication adherence: a randomized controlled trial. Ann Fam Med. 2012;10:15-22.
17. Pignone MP, Gaynes BN, Rushton JL, et al. Screening for de- pression in adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;136:765- 776.
18. Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(suppl 1):S11-S61.
19. Executive summary: standards of medical care in diabe- tes—2013. Diabetes Care. 2013;36(suppl 1):S4-S10.
20. Ismail-Beigi F. Clinical practice. Glycemic management of type 2 diabetes mellitus. N Engl J Med. 2012;366:1319-1327.
21. Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hy- perglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35:1364-1379.
22. Greene J, Hibbard JH, Sacks R, et al. When seeing the same physician, highly activated patients have better experi- ences than less activated patients. Health Aff (Millwood). 2013;32:1299-1305.
23. Battersby M, Von KM, Schaefer J, et al. Twelve evidence-based principles for implementing self-management support in pri- mary care. Jt Comm J Qual Patient Saf. 2010;36:561-570.
24. Watson S. The 13 best diabetes iPhone & Android apps of 2013. Healthline Web site. Available at: http://www.healthline.com/ health-slideshow/top-iphone-android-apps-diabetes. Published August 8, 2013. Accessed September 16, 2013.