User login
- Standard treadmill exercise testing for diagnosis and risk stratification is suitable for patients with a normal resting electrocardiogram (ECG) and without contraindications to exercise.
- Those with an uninterpretable ECG should undergo either nuclear or echocardiographic imaging in concert with their exercise test.
- Patients in whom exercise is either contraindicated or who have a condition that interferes with exercising to target level are candidates for nuclear or echocardiographic pharmacologic stress testing.
- Patients with suspected coronary heart disease and for whom exercise or pharmacologic testing is contraindicated should be referred to a cardiologist for evaluation.
Most men and women experience symptoms before myocardial infarction (MI).1 Early recognition of these symptoms and prompt treatment are essential for prevention of death and disability related to coronary heart disease (CHD).
Patients with multiple risk factors, chest pain typically suggestive of CHD, or a history of CHD are usually easy to identify and triage. However, many patients do not have obvious risks for CHD but experience occasional symptoms of cardiac ischemia.
Patients can be stratified into low-, intermediate-, and high-risk categories that will help determine appropriate work-up. Those at intermediate risk can be difficult to assess, and may particularly benefit from stress-imaging studies.
The algorithm (Figure 1) is based on current guidelines,2 and indicates how patients with chest pain/symptoms may be identified and treated according to an initial estimate of the probability of obstructive coronary artery disease. The choice of noninvasive diagnostic tests for individuals with stable chest pain and a lower risk for CHD is then outlined.
Case studies
Patient 1
A 64-year-old, nonsmoking, obese woman with degenerative osteoarthritis of the knees occasionally experiences chest discomfort that lasts for a few minutes, sometimes radiating to her back. The discomfort, which started 4 weeks ago, occasionally becomes worse after a brief walk, but is not usually related to exertion, or associated with nausea or diaphoresis. She sometimes becomes short of breath climbing stairs.
Physical examination: In no acute distress; body-mass index 31.2, waist circumference 42 inches, heart rate 70 beats/min, blood pressure 142/88 mm Hg, cardiovascular examination unremarkable.
Laboratory evaluation: resting electrocardiogram (ECG)—sinus rhythm otherwise normal; creatinine 1.2 mg/dL; fasting glucose 122 mg/dL; glycosylated hemoglobin 6.4%. Lipids: total cholesterol 232 mg/dL; triglycerides 230 mg/dL; high-density lipoprotein (HDL) cholesterol 28 mg/dL; low-density lipoprotein (LDL) cholesterol 158 mg/dL.
Patient 2
A 58-year-old, nonsmoking, otherwise healthy man experiences tightness in the chest, usually at night. The pain began 4 to 8 weeks ago; it lasts as long as 1 to 2 hours but is “very mild.” It does not radiate to the arm or jaw and is unrelated to exertion. There is no diaphoresis or nausea. He sometimes feels a bit winded, which “might be due to anxiety.”
Physical examination: slightly overweight man in no acute distress; body-mass index 27.0, waist circumference 36 inches, heart rate 74 beats/min, blood pressure 138/88 mm Hg, cardiovascular examination unremarkable.
Laboratory evaluation: ECG— sinus rhythm, otherwise normal; creatinine 1.0 mg/dL; fasting glucose 98 mg/dL. Lipids: total cholesterol 215 mg/dL; triglycerides 150 mg/dL; HDL 40 mg/dL; LDL 145 mg/dL.
Diagnostic approaches
Standard diagnostic techniques include history, physical examination, laboratory testing as indicated, resting ECG, and assessment of risk factors for CHD.
Evaluation of chest pain
A careful history and physical examination can often quickly exclude many noncardiac causes of chest discomfort or pain. Table 1 contrasts the characteristics of atypical (noncardiac) symptoms with those of typical (cardiac) symptoms. Its quality, location, and the factors that relieve or provoke it, duration, and any associated symptoms should be evaluated. If high-risk or unstable signs or symptoms are present that suggest acute coronary syndrome (unstable angina or MI), evaluation in the emergency department should be performed.
Patients exhibiting stable or atypical (noncardiac) symptoms with some, but not all, of the features of angina described above have a lower probability of coronary artery disease, and should be considered for diagnostic evaluation under the guidance of the primary care physician.3
TABLE 1
Characteristics of atypical (noncardiac) vs typical cardiac symptoms
| Characteristic | Atypical/noncardiac | Typical/cardiac |
|---|---|---|
| Quality | Sharp, stabbing, positional | Squeezing, ache, pressure, fullness, burning, heavy, suffocating, “discomfort” |
| Location | Highly localized, below the epigastrium, above the mandible | Diffuse area—substernal, chest, jaw, back, arms |
| Provoked by | “Nothing,” body movement, cough, deep inspiration, chest palpation | Exertion, emotional stress, cold air |
| Relieved by | “Nothing,” position change, analgesics, heat, antacids | Rest; nitroglycerin |
| Duration | “Seconds” (fleeting), or hours, days | 30 seconds to 5 minutes |
| Associated symptoms | Reflux/heartburn | Dyspnea, diaphoresis, nausea, fatigue |
Evaluating women
In women aged <55 years, noncardiac chest pain is common, but since the prevalence of CHD is increasing among younger women, their symptoms should not be dismissed as “noncardiac” without full evaluation.
Women are also more likely than men to report dyspnea or pain in the jaw or back instead of, or in addition to, chest symptoms. Further, since women are often older and less active when they develop CHD, they may not exhibit typical exertional symptoms. Diagnosis in women is also hampered by lower accuracy of standard stress ECG testing compared with men. False-positive and false-negative tests may occur more frequently in women due to hormonal effects on the ECG, and more frequent comorbidities that limit maximal exercise capacity.
Physical examination
Palpation and auscultation of the chest may detect the presence of a friction rub or significant murmur, and thus identify a nonischemic cause for the chest symptoms. Carotid bruits or reduced pedal pulses indicate the presence of other vascular diseases. Patients with xanthomas, hypertension, or signs of congestive heart failure are more likely to have CHD, while those whose pain can be reproduced by body movement or by palpating the chest are less likely to have CHD.
Risk factor assessment. The assessment of risk factors for CHD allows the identification of many patients at high risk for CHD and can be helpful in guiding the choice of additional tests. As evident in the Framingham Heart Study,4 independent risk factors such as cigarette smoking, hypertension, diabetes mellitus, and hyperlipidemia are direct causes of CHD.
Laboratory tests
In the patient at low risk of CHD, blood testing for cardiac markers is not indicated. A lipid profile and blood glucose level help to establish the risk level associated with hyperlipidemia and diabetes. A complete blood count (eg, for anemia), thyroid hormone studies (eg, for hyperthyroidism), arterial blood gases (eg, PCO2 for chronic obstructive pulmonary disease), and other tests may help in diagnosing contributory conditions.
Resting electrocardiogram
A routine resting 12-lead ECG is an inexpensive but critical test that can provide important diagnostic and prognostic information. Evidence of infarction, ischemia, hypertrophy arrhythmias, and conduction disturbances can be detected and, if present, substantially increase the likelihood of a cardiac cause of symptoms.
Even the presence of mild or nonspecific ST-T wave changes, while not diagnostic, can aid the clinician by suggesting a higher probability of a nondiagnostic stress ECG and the need for an imaging stress test.3 An abnormal resting ECG with ST-T wave changes associated with digoxin use, left bundle branch block, left ventricular hypertrophy, and so on, limit interpretation of an exercise ECG, and points to a need for exercise testing with imaging.
It is important to note that a normal ECG obtained when the patient is asymptomatic does not exclude CHD, and additional risk stratification with noninvasive diagnostic stress testing may be indicated.5
Chest x-ray
A chest x-ray is often appropriate for patients with cardiac or pulmonary signs/symptoms. It may show cardiac enlargement, ventricular aneurysm, or evidence of heart failure, which may support the diagnosis of CHD and help to assess the extent of cardiopulmonary involvement.
Noninvasive stress testing
Considering our 2 patients with occasional episodes of unexplained chest discomfort: Based on the ECG and clinical findings, their risk for CHD is considered low to intermediate.
Test selection
Diagnostic tests should be selected based on the clinician’s estimate of probability of CHD.2
Low probability. If the likelihood of CHD is low, stress testing is generally not indicated, as its specificity is extremely low, and test results do not improve diagnostic accuracy over the clinical impression alone.
Intermediate probability. If the patient is able to exercise to capacity, the choice is exercise testing. Patients who can exercise and have an interpretable ECG, with no evidence of left ventricular dysfunction and no prior revascularization procedure, should usually undergo standard stress ECG testing. If the ECG is not interpretable, (due to repolarization abnormalities, left bundle branch block, left ventricular hypertrophy, digoxin use, etc) an exercise test with imaging (nuclear or echocardiographic) is indicated.
For patients unable to exercise, pharmacologic stress testing with imaging is indicated.
High probability. If the probability of CHD is high, it is reasonable to proceed directly to coronary angiography.
Exercise stress test
Exercise testing is a cardiovascular stress that uses treadmill or bicycle exercise with ECG and blood pressure monitoring. Such testing is widely available and relatively inexpensive.2 It allows assessment of exercise capacity and correlation of symptoms with ECG changes typical of myocardial ischemia.
Exercise testing provides the highest level of incremental diagnostic and prognostic information for patients with an intermediate probability of CHD.2 An important objective of stress testing is to identify individuals with a high risk for severe (left main or 3-vessel) CHD. More invasive procedures, such as percutaneous cutaneous angioplasty (PCTA), are recommended for these high-risk individuals to improve their survival.
Candidates for exercise treadmill testing include patients with stable symptoms who can be expected to exercise to an adequate workload. Patients with repolarization abnormalities on the resting ECG, such as left bundle branch block, left ventricular hypertrophy, or digoxin use, frequently have noninterpretable stress ECGs and may benefit from imaging techniques.
Limitations. Some patients referred for exercise treadmill testing are unable to achieve either adequate exercise levels or the target heart rate due to comorbid conditions,6 such as degenerative joint disease, obesity, pulmonary disease, peripheral vascular disease, central nervous system disorders, physical deconditioning, chronotropic incompetence, and medications such as beta blockers. More subtle factors, such as an unwillingness to exercise, may also affect a patient’s suitability for stress testing. These patients should be considered for pharmacologic stress testing.
Additionally, stress-induced ST-T wave changes do not accurately localize the site of myocardial ischemia and provide no direct information on left ventricular function and other clinically important variables. The sensitivity and specificity of exercise ECG testing ranges from approximately 67% to 72%, which is below that of stress imaging techniques, whose average sensitivity ranges from 80% to 85%.7-9
Stress imaging modalities
For a patient with an abnormal resting ECG, evidence of left ventricular dysfunction, or a prior coronary revascularization, stress imaging with either echocardiography or nuclear perfusion scanning is appropriate. Both techniques show higher specificity than the stress ECG alone.
Nuclear imaging. Nuclear imaging uses radiotracers (thallium-201, technetium-99m tetrofosmin [Myoview], or technetium-99m sestamibi [Cardiolite]) to evaluate myocardial perfusion and function, and has greatly advanced the ability to detect and assess the extent of CHD. Stress myocardial perfusion imaging has a sensitivity of >90% for detecting patients at risk of cardiac death or MI.6
To detect ischemia or infarction, a radioisotope is injected at rest and after stress to produce images of myocardial regional uptake, which is proportional to regional blood flow. Normally, with maximal exercise or pharmacologic stress, myocardial blood flow is greatly increased above the resting condition. If a fixed coronary stenosis is present, myocardial perfusion in the territory supplied by the stenosis cannot be increased, which will create a flow differential and uneven distribution of the tracer.
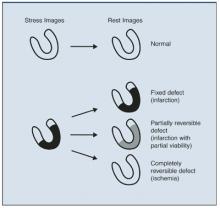
As illustrated in Figure 2, a normal myocardial perfusion image shows homogenous accumulation of radiotracer on both the stress and rest images. A perfusion defect appears as an area of reduced tracer uptake.
Nuclear perfusion studies can also provide a measure of left ventricular function and wall motion utilizing a bolus injection of radiotracer. While images can be obtained in most patients utilizing current techniques, artifacts due to breast and diaphragmatic tissue attenuation can lead to false-positive interpretation, particularly when examining women and when using thallium.
Echocardiography. Echocardiography visualizes the heart directly in real time using ultrasound, providing convenient assessment of the cardiac chambers, myocardium, valves, pericardium, and great vessels. The test can also identify mechanical complications of acute myocardial infarction, differentiate causes of reduced cardiac output and blood pressure, and help guide therapy. Stress echocardiography (exercise or pharmacologic stress) can be used to detect the presence, location, and severity of inducible myocardial ischemia as well as for risk stratification and prognosis.
During stress-induced ischemia, decrements in contractile function are directly related to decreases in regional subendocardial blood flow. Wall-motion changes precede ischemic ECG changes, accounting for the increased sensitivity of echocardiography versus ECG stress testing.
Interpretation of stress echocardiograms is based on analysis of segmental wall motion before and soon after stress. Normally, with exercise, or dobutamine infusion, left ventricular wall motion becomes hyperdynamic. The hallmark of ischemia is the development with stress of new, or the worsening of preexisting, wall motion abnormalities. The lack of improvement with stress in an already hypokinetic segment indicates infarction. Stress-induced left ventricular cavity enlargement, systolic dysfunction, or mitral regurgitation may also suggest CHD. Accuracy of stress echocardiography is similar to that of nuclear stress testing.
Considerable expertise in echocardiography is needed to rapidly acquire diagnostic images, so that its selection is limited by the skill of the technician. Image quality can be compromised by obesity and other factors, but the widespread use of intravenous contrast agents has significantly reduced the proportion of patients with uninterpretable images.
FIGURE 2
Accumulation of radiotracer in nuclear imaging (stress and rest images)
Patients who are not expected to achieve an adequate exercise capacity (as in our patient with osteoarthritis) should undergo pharmacologic stress testing with adenosine, dipyridamole, or dobutamine. Atrial pacing utilizing a swallowed esophageal electrode is also used in some cases. These agents, combined with echocardiographic or nuclear imaging, are particularly useful in patients who are unable to exercise adequately.
Pharmacologic stress agents are sometimes combined with low-level exercise protocols which may reduce the noncardiac side effects and improve image quality.10
Adenosine is the pharmacologic agent used most commonly in nuclear perfusion stress testing. An intravenous infusion of adenosine produces coronary vasodilation which is quickly attenuated when the infusion is terminated. Side effects, which are short-lived, include flushing, palpitations, and chest pain.
Dipyridamole is used less commonly due to its prolonged side effects and reports of lower specificity.11 Dobutamine, a beta-adrenergic agonist, increases heart rate and contractility in a dose-related fashion when infused intravenously. This agent is most commonly used in echocardiographic imaging. It can also be utilized with nuclear imaging when adenosine is contraindicated due to severe pulmonary or cerebrovascular disease. Side effects include transient arrhythmias, hypertension or hypotension, tremor, and chest pain.
Referral to a cardiologist
Referral to a cardiologist should be considered when the suspicion for cardiac disease is high, there is substantial diagnostic uncertainty after initial evaluation, or if symptoms persist, despite treatment of a noncardiac cause. Further evaluation and treatment often includes coronary angiography.
Coronary angiography
Most outpatients, such as the 2 presented, can be diagnosed with clinical and noninvasive measures. Coronary angiography is most commonly used to determine the presence and extent of obstructive CHD, and to guide decisions about revascularization in high-risk patients, or in patients with an abnormal stress test.
Cardiac catheterization presents a small but real risk to the patient, involves discomfort and substantial cost, and can challenge effective resource utilization. Risks and benefits to individual patients should be discussed between primary care physician and cardiologist.
Summary
Findings in our 2 patients are summarized below. Diagnostic decisions reflect the algorithm in Figure 1and are based on current guidelines.2
Patient 1. After initial assessment, our 64-year-old asymptomatic woman still falls into “intermediate probability of CHD” due to her multiple CHD risks. Stress testing was therefore indicated. Due to her inability to exercise because of an orthopedic limitation, she underwent pharmacologic stress testing with an adenosine sestamibi study. A small inferior reversible defect was identified, suggestive of myocardial ischemia.
Aggressive medical therapy aimed at minimizing symptoms and reducing risk was selected: aspirin, a beta-blocker for ischemia and hypertension, and a statin for hyperlipidemia. Longacting nitrates or calcium-channel blockers would have been reasonable alternatives. Consideration of an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker is also indicated in light of her new CHD diagnosis and glucose intolerance. She was advised to initiate a low-fat, low-carbohydrate diet and to exercise (swim) regularly to lower risk. She will be seen in 6 weeks to reevaluate her symptoms, blood pressure, and lipid and glycemic control.
Patient 2. Our male patient also warranted stress testing. He was referred for a standard stress ECG due to his normal resting ECG, and the expectation that he would be able to exercise adequately. He satisfactorily completed 10.5 minutes (10 METS) of a Bruce protocol on a treadmill exercise stress test, which was entirely normal.
This admittedly anxious individual was reassured that his chest symptoms are not due to heart disease. An empiric trial with a proton pump inhibitor could be initiated if gastro-esophageal reflux is suspected.
Conclusions
Standard treadmill exercise testing for diagnosis and risk stratification is suitable for patients with a normal resting ECG and without contraindications to exercise, as in our male patient. Those with an uninterpretable ECG should undergo either nuclear or echocardiographic imaging in concert with their exercise test. Patients in whom exercise is either contraindicated or who have a condition that interferes with exercising to the target level are candidates for nuclear or echocardiographic pharmacologic stress testing, as was indicated for our female patient. Patients with suspected CHD and for whom exercise or pharmacologic testing is contraindicated should be referred to a cardiologist for evaluation.
Finally, when selecting a specific stress imaging technique, physicians should consider the local expertise with the various techniques available, together with their strengths and limitations in the individual patient.19
1. Spertus JA, Radford MJ, Every NR, et al. Challenges and opportunities in quantifying the quality of care for acute myocardial infarction. Summary from the Acute Myocardial Infarction Working Group of the American Heart Association/American College of Cardiology First Scientific Forum on Quality of Care and Outcomes Research in Cardiovascular Disease and Stroke. Circulation 2003;107:1681-1691.
2. Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to update the 1997 exercise testing guidelines). Circulation 2002;106:1883-1892.
3. Gibbons RJ, Chatterjee K, Daley J, et al. ACC/AHA/ACP-ASIM guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients With Chronic Stable Angina). J Am Coll Cardiol 1999;33:2092-2197.
4. Grundy SM, Balady GJ, Criqui MH, et al. Primary prevention of coronary heart disease: guidance from Framingham: a statement for healthcare professionals from the American Heart Association Task Force on Risk Reduction. Circulation 1998;97:1876-1887.
5. Zanger DR, Solomon AJ, Gersh BJ. Contemporary management of angina: part I: risk assessment. Am Fam Physician 1999;60:2543-2552.
6. Bar Harbor Invitation Meeting 2000. Panel 9: Nuclear imaging in coronary artery disease. J Nucl Cardiol 2001;8:305-316.
7. Kotler TS, Diamond GA. Exercise thallium-201 scintigraphy in the diagnosis and prognosis of coronary artery disease. Ann Intern Med 1990;113:684-702.
8. Gibbons RJ. Rest and exercise radionuclide angiography for diagnosis in chronic ischemic heart disease. Circulation 1991;84 (3 Suppl):I93-I99.
9. Roger VL, Pellikka PA, Oh JK, Miller FA, Seward JB, Tajik AJ. Stress echocardiography. Part I. Exercise echocardiography: techniques, implementation, clinical applications, and correlations. Mayo Clin Proc 1995;70:5-15.
10. Thomas GS, Prill NV, Majmundar H, et al. Treadmill exercise during adenosine infusion is safe, results in fewer adverse reactions, and improves myocardial perfusion image quality. J Nucl Cardiol 2000;7:439-446.
11. Li T, Ahlberg A, Hachamovitch R, et al. Comparison of adenosine and dipyridamole in detecting coronary artery disease using Tc-99m sestamibi single-photon emission computed tomography imaging: a randomized, prospective clinical study. J Am Coll Cardiol 2003;41(suppl A):461A. Abstract 858-3.
12. American Heart Association. Heart disease and stroke statistics—2003 update. Dallas, Tex: American Heart Association; 2003.
This special section of The Journal of Family Practiceis provided by an unrestricted grant fromFujisawa Healthcare, Inc. Disclosures: Dr McBride has served on the speakers’ bureau for the following: Abbott Laboratories, Astra-Zeneca, Bristol-Myers Squibb, Glaxo SmithKline, KOS Pharmaceuticals, Merck & Co Inc, Pfizer Inc, Reliant Pharmaceuticals, and Sankyo. He has served as consultant to KOS Pharmaceuticals, Merck & Co Inc, and Pfizer Inc. He has received grant/research support from Merck & Co Inc and Pfizer Inc. Dr Hayes had no commercial interests to report. Corresponding author: Sharonne N. Hayes, MD, Mayo Clinic Women’s Heart Clinic, Rochester MN, 55905. E-mail: [email protected].
- Standard treadmill exercise testing for diagnosis and risk stratification is suitable for patients with a normal resting electrocardiogram (ECG) and without contraindications to exercise.
- Those with an uninterpretable ECG should undergo either nuclear or echocardiographic imaging in concert with their exercise test.
- Patients in whom exercise is either contraindicated or who have a condition that interferes with exercising to target level are candidates for nuclear or echocardiographic pharmacologic stress testing.
- Patients with suspected coronary heart disease and for whom exercise or pharmacologic testing is contraindicated should be referred to a cardiologist for evaluation.
Most men and women experience symptoms before myocardial infarction (MI).1 Early recognition of these symptoms and prompt treatment are essential for prevention of death and disability related to coronary heart disease (CHD).
Patients with multiple risk factors, chest pain typically suggestive of CHD, or a history of CHD are usually easy to identify and triage. However, many patients do not have obvious risks for CHD but experience occasional symptoms of cardiac ischemia.
Patients can be stratified into low-, intermediate-, and high-risk categories that will help determine appropriate work-up. Those at intermediate risk can be difficult to assess, and may particularly benefit from stress-imaging studies.
The algorithm (Figure 1) is based on current guidelines,2 and indicates how patients with chest pain/symptoms may be identified and treated according to an initial estimate of the probability of obstructive coronary artery disease. The choice of noninvasive diagnostic tests for individuals with stable chest pain and a lower risk for CHD is then outlined.
Case studies
Patient 1
A 64-year-old, nonsmoking, obese woman with degenerative osteoarthritis of the knees occasionally experiences chest discomfort that lasts for a few minutes, sometimes radiating to her back. The discomfort, which started 4 weeks ago, occasionally becomes worse after a brief walk, but is not usually related to exertion, or associated with nausea or diaphoresis. She sometimes becomes short of breath climbing stairs.
Physical examination: In no acute distress; body-mass index 31.2, waist circumference 42 inches, heart rate 70 beats/min, blood pressure 142/88 mm Hg, cardiovascular examination unremarkable.
Laboratory evaluation: resting electrocardiogram (ECG)—sinus rhythm otherwise normal; creatinine 1.2 mg/dL; fasting glucose 122 mg/dL; glycosylated hemoglobin 6.4%. Lipids: total cholesterol 232 mg/dL; triglycerides 230 mg/dL; high-density lipoprotein (HDL) cholesterol 28 mg/dL; low-density lipoprotein (LDL) cholesterol 158 mg/dL.
Patient 2
A 58-year-old, nonsmoking, otherwise healthy man experiences tightness in the chest, usually at night. The pain began 4 to 8 weeks ago; it lasts as long as 1 to 2 hours but is “very mild.” It does not radiate to the arm or jaw and is unrelated to exertion. There is no diaphoresis or nausea. He sometimes feels a bit winded, which “might be due to anxiety.”
Physical examination: slightly overweight man in no acute distress; body-mass index 27.0, waist circumference 36 inches, heart rate 74 beats/min, blood pressure 138/88 mm Hg, cardiovascular examination unremarkable.
Laboratory evaluation: ECG— sinus rhythm, otherwise normal; creatinine 1.0 mg/dL; fasting glucose 98 mg/dL. Lipids: total cholesterol 215 mg/dL; triglycerides 150 mg/dL; HDL 40 mg/dL; LDL 145 mg/dL.
Diagnostic approaches
Standard diagnostic techniques include history, physical examination, laboratory testing as indicated, resting ECG, and assessment of risk factors for CHD.
Evaluation of chest pain
A careful history and physical examination can often quickly exclude many noncardiac causes of chest discomfort or pain. Table 1 contrasts the characteristics of atypical (noncardiac) symptoms with those of typical (cardiac) symptoms. Its quality, location, and the factors that relieve or provoke it, duration, and any associated symptoms should be evaluated. If high-risk or unstable signs or symptoms are present that suggest acute coronary syndrome (unstable angina or MI), evaluation in the emergency department should be performed.
Patients exhibiting stable or atypical (noncardiac) symptoms with some, but not all, of the features of angina described above have a lower probability of coronary artery disease, and should be considered for diagnostic evaluation under the guidance of the primary care physician.3
TABLE 1
Characteristics of atypical (noncardiac) vs typical cardiac symptoms
| Characteristic | Atypical/noncardiac | Typical/cardiac |
|---|---|---|
| Quality | Sharp, stabbing, positional | Squeezing, ache, pressure, fullness, burning, heavy, suffocating, “discomfort” |
| Location | Highly localized, below the epigastrium, above the mandible | Diffuse area—substernal, chest, jaw, back, arms |
| Provoked by | “Nothing,” body movement, cough, deep inspiration, chest palpation | Exertion, emotional stress, cold air |
| Relieved by | “Nothing,” position change, analgesics, heat, antacids | Rest; nitroglycerin |
| Duration | “Seconds” (fleeting), or hours, days | 30 seconds to 5 minutes |
| Associated symptoms | Reflux/heartburn | Dyspnea, diaphoresis, nausea, fatigue |
Evaluating women
In women aged <55 years, noncardiac chest pain is common, but since the prevalence of CHD is increasing among younger women, their symptoms should not be dismissed as “noncardiac” without full evaluation.
Women are also more likely than men to report dyspnea or pain in the jaw or back instead of, or in addition to, chest symptoms. Further, since women are often older and less active when they develop CHD, they may not exhibit typical exertional symptoms. Diagnosis in women is also hampered by lower accuracy of standard stress ECG testing compared with men. False-positive and false-negative tests may occur more frequently in women due to hormonal effects on the ECG, and more frequent comorbidities that limit maximal exercise capacity.
Physical examination
Palpation and auscultation of the chest may detect the presence of a friction rub or significant murmur, and thus identify a nonischemic cause for the chest symptoms. Carotid bruits or reduced pedal pulses indicate the presence of other vascular diseases. Patients with xanthomas, hypertension, or signs of congestive heart failure are more likely to have CHD, while those whose pain can be reproduced by body movement or by palpating the chest are less likely to have CHD.
Risk factor assessment. The assessment of risk factors for CHD allows the identification of many patients at high risk for CHD and can be helpful in guiding the choice of additional tests. As evident in the Framingham Heart Study,4 independent risk factors such as cigarette smoking, hypertension, diabetes mellitus, and hyperlipidemia are direct causes of CHD.
Laboratory tests
In the patient at low risk of CHD, blood testing for cardiac markers is not indicated. A lipid profile and blood glucose level help to establish the risk level associated with hyperlipidemia and diabetes. A complete blood count (eg, for anemia), thyroid hormone studies (eg, for hyperthyroidism), arterial blood gases (eg, PCO2 for chronic obstructive pulmonary disease), and other tests may help in diagnosing contributory conditions.
Resting electrocardiogram
A routine resting 12-lead ECG is an inexpensive but critical test that can provide important diagnostic and prognostic information. Evidence of infarction, ischemia, hypertrophy arrhythmias, and conduction disturbances can be detected and, if present, substantially increase the likelihood of a cardiac cause of symptoms.
Even the presence of mild or nonspecific ST-T wave changes, while not diagnostic, can aid the clinician by suggesting a higher probability of a nondiagnostic stress ECG and the need for an imaging stress test.3 An abnormal resting ECG with ST-T wave changes associated with digoxin use, left bundle branch block, left ventricular hypertrophy, and so on, limit interpretation of an exercise ECG, and points to a need for exercise testing with imaging.
It is important to note that a normal ECG obtained when the patient is asymptomatic does not exclude CHD, and additional risk stratification with noninvasive diagnostic stress testing may be indicated.5
Chest x-ray
A chest x-ray is often appropriate for patients with cardiac or pulmonary signs/symptoms. It may show cardiac enlargement, ventricular aneurysm, or evidence of heart failure, which may support the diagnosis of CHD and help to assess the extent of cardiopulmonary involvement.
Noninvasive stress testing
Considering our 2 patients with occasional episodes of unexplained chest discomfort: Based on the ECG and clinical findings, their risk for CHD is considered low to intermediate.
Test selection
Diagnostic tests should be selected based on the clinician’s estimate of probability of CHD.2
Low probability. If the likelihood of CHD is low, stress testing is generally not indicated, as its specificity is extremely low, and test results do not improve diagnostic accuracy over the clinical impression alone.
Intermediate probability. If the patient is able to exercise to capacity, the choice is exercise testing. Patients who can exercise and have an interpretable ECG, with no evidence of left ventricular dysfunction and no prior revascularization procedure, should usually undergo standard stress ECG testing. If the ECG is not interpretable, (due to repolarization abnormalities, left bundle branch block, left ventricular hypertrophy, digoxin use, etc) an exercise test with imaging (nuclear or echocardiographic) is indicated.
For patients unable to exercise, pharmacologic stress testing with imaging is indicated.
High probability. If the probability of CHD is high, it is reasonable to proceed directly to coronary angiography.
Exercise stress test
Exercise testing is a cardiovascular stress that uses treadmill or bicycle exercise with ECG and blood pressure monitoring. Such testing is widely available and relatively inexpensive.2 It allows assessment of exercise capacity and correlation of symptoms with ECG changes typical of myocardial ischemia.
Exercise testing provides the highest level of incremental diagnostic and prognostic information for patients with an intermediate probability of CHD.2 An important objective of stress testing is to identify individuals with a high risk for severe (left main or 3-vessel) CHD. More invasive procedures, such as percutaneous cutaneous angioplasty (PCTA), are recommended for these high-risk individuals to improve their survival.
Candidates for exercise treadmill testing include patients with stable symptoms who can be expected to exercise to an adequate workload. Patients with repolarization abnormalities on the resting ECG, such as left bundle branch block, left ventricular hypertrophy, or digoxin use, frequently have noninterpretable stress ECGs and may benefit from imaging techniques.
Limitations. Some patients referred for exercise treadmill testing are unable to achieve either adequate exercise levels or the target heart rate due to comorbid conditions,6 such as degenerative joint disease, obesity, pulmonary disease, peripheral vascular disease, central nervous system disorders, physical deconditioning, chronotropic incompetence, and medications such as beta blockers. More subtle factors, such as an unwillingness to exercise, may also affect a patient’s suitability for stress testing. These patients should be considered for pharmacologic stress testing.
Additionally, stress-induced ST-T wave changes do not accurately localize the site of myocardial ischemia and provide no direct information on left ventricular function and other clinically important variables. The sensitivity and specificity of exercise ECG testing ranges from approximately 67% to 72%, which is below that of stress imaging techniques, whose average sensitivity ranges from 80% to 85%.7-9
Stress imaging modalities
For a patient with an abnormal resting ECG, evidence of left ventricular dysfunction, or a prior coronary revascularization, stress imaging with either echocardiography or nuclear perfusion scanning is appropriate. Both techniques show higher specificity than the stress ECG alone.
Nuclear imaging. Nuclear imaging uses radiotracers (thallium-201, technetium-99m tetrofosmin [Myoview], or technetium-99m sestamibi [Cardiolite]) to evaluate myocardial perfusion and function, and has greatly advanced the ability to detect and assess the extent of CHD. Stress myocardial perfusion imaging has a sensitivity of >90% for detecting patients at risk of cardiac death or MI.6
To detect ischemia or infarction, a radioisotope is injected at rest and after stress to produce images of myocardial regional uptake, which is proportional to regional blood flow. Normally, with maximal exercise or pharmacologic stress, myocardial blood flow is greatly increased above the resting condition. If a fixed coronary stenosis is present, myocardial perfusion in the territory supplied by the stenosis cannot be increased, which will create a flow differential and uneven distribution of the tracer.
As illustrated in Figure 2, a normal myocardial perfusion image shows homogenous accumulation of radiotracer on both the stress and rest images. A perfusion defect appears as an area of reduced tracer uptake.
Nuclear perfusion studies can also provide a measure of left ventricular function and wall motion utilizing a bolus injection of radiotracer. While images can be obtained in most patients utilizing current techniques, artifacts due to breast and diaphragmatic tissue attenuation can lead to false-positive interpretation, particularly when examining women and when using thallium.
Echocardiography. Echocardiography visualizes the heart directly in real time using ultrasound, providing convenient assessment of the cardiac chambers, myocardium, valves, pericardium, and great vessels. The test can also identify mechanical complications of acute myocardial infarction, differentiate causes of reduced cardiac output and blood pressure, and help guide therapy. Stress echocardiography (exercise or pharmacologic stress) can be used to detect the presence, location, and severity of inducible myocardial ischemia as well as for risk stratification and prognosis.
During stress-induced ischemia, decrements in contractile function are directly related to decreases in regional subendocardial blood flow. Wall-motion changes precede ischemic ECG changes, accounting for the increased sensitivity of echocardiography versus ECG stress testing.
Interpretation of stress echocardiograms is based on analysis of segmental wall motion before and soon after stress. Normally, with exercise, or dobutamine infusion, left ventricular wall motion becomes hyperdynamic. The hallmark of ischemia is the development with stress of new, or the worsening of preexisting, wall motion abnormalities. The lack of improvement with stress in an already hypokinetic segment indicates infarction. Stress-induced left ventricular cavity enlargement, systolic dysfunction, or mitral regurgitation may also suggest CHD. Accuracy of stress echocardiography is similar to that of nuclear stress testing.
Considerable expertise in echocardiography is needed to rapidly acquire diagnostic images, so that its selection is limited by the skill of the technician. Image quality can be compromised by obesity and other factors, but the widespread use of intravenous contrast agents has significantly reduced the proportion of patients with uninterpretable images.
FIGURE 2
Accumulation of radiotracer in nuclear imaging (stress and rest images)
Patients who are not expected to achieve an adequate exercise capacity (as in our patient with osteoarthritis) should undergo pharmacologic stress testing with adenosine, dipyridamole, or dobutamine. Atrial pacing utilizing a swallowed esophageal electrode is also used in some cases. These agents, combined with echocardiographic or nuclear imaging, are particularly useful in patients who are unable to exercise adequately.
Pharmacologic stress agents are sometimes combined with low-level exercise protocols which may reduce the noncardiac side effects and improve image quality.10
Adenosine is the pharmacologic agent used most commonly in nuclear perfusion stress testing. An intravenous infusion of adenosine produces coronary vasodilation which is quickly attenuated when the infusion is terminated. Side effects, which are short-lived, include flushing, palpitations, and chest pain.
Dipyridamole is used less commonly due to its prolonged side effects and reports of lower specificity.11 Dobutamine, a beta-adrenergic agonist, increases heart rate and contractility in a dose-related fashion when infused intravenously. This agent is most commonly used in echocardiographic imaging. It can also be utilized with nuclear imaging when adenosine is contraindicated due to severe pulmonary or cerebrovascular disease. Side effects include transient arrhythmias, hypertension or hypotension, tremor, and chest pain.
Referral to a cardiologist
Referral to a cardiologist should be considered when the suspicion for cardiac disease is high, there is substantial diagnostic uncertainty after initial evaluation, or if symptoms persist, despite treatment of a noncardiac cause. Further evaluation and treatment often includes coronary angiography.
Coronary angiography
Most outpatients, such as the 2 presented, can be diagnosed with clinical and noninvasive measures. Coronary angiography is most commonly used to determine the presence and extent of obstructive CHD, and to guide decisions about revascularization in high-risk patients, or in patients with an abnormal stress test.
Cardiac catheterization presents a small but real risk to the patient, involves discomfort and substantial cost, and can challenge effective resource utilization. Risks and benefits to individual patients should be discussed between primary care physician and cardiologist.
Summary
Findings in our 2 patients are summarized below. Diagnostic decisions reflect the algorithm in Figure 1and are based on current guidelines.2
Patient 1. After initial assessment, our 64-year-old asymptomatic woman still falls into “intermediate probability of CHD” due to her multiple CHD risks. Stress testing was therefore indicated. Due to her inability to exercise because of an orthopedic limitation, she underwent pharmacologic stress testing with an adenosine sestamibi study. A small inferior reversible defect was identified, suggestive of myocardial ischemia.
Aggressive medical therapy aimed at minimizing symptoms and reducing risk was selected: aspirin, a beta-blocker for ischemia and hypertension, and a statin for hyperlipidemia. Longacting nitrates or calcium-channel blockers would have been reasonable alternatives. Consideration of an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker is also indicated in light of her new CHD diagnosis and glucose intolerance. She was advised to initiate a low-fat, low-carbohydrate diet and to exercise (swim) regularly to lower risk. She will be seen in 6 weeks to reevaluate her symptoms, blood pressure, and lipid and glycemic control.
Patient 2. Our male patient also warranted stress testing. He was referred for a standard stress ECG due to his normal resting ECG, and the expectation that he would be able to exercise adequately. He satisfactorily completed 10.5 minutes (10 METS) of a Bruce protocol on a treadmill exercise stress test, which was entirely normal.
This admittedly anxious individual was reassured that his chest symptoms are not due to heart disease. An empiric trial with a proton pump inhibitor could be initiated if gastro-esophageal reflux is suspected.
Conclusions
Standard treadmill exercise testing for diagnosis and risk stratification is suitable for patients with a normal resting ECG and without contraindications to exercise, as in our male patient. Those with an uninterpretable ECG should undergo either nuclear or echocardiographic imaging in concert with their exercise test. Patients in whom exercise is either contraindicated or who have a condition that interferes with exercising to the target level are candidates for nuclear or echocardiographic pharmacologic stress testing, as was indicated for our female patient. Patients with suspected CHD and for whom exercise or pharmacologic testing is contraindicated should be referred to a cardiologist for evaluation.
Finally, when selecting a specific stress imaging technique, physicians should consider the local expertise with the various techniques available, together with their strengths and limitations in the individual patient.19
- Standard treadmill exercise testing for diagnosis and risk stratification is suitable for patients with a normal resting electrocardiogram (ECG) and without contraindications to exercise.
- Those with an uninterpretable ECG should undergo either nuclear or echocardiographic imaging in concert with their exercise test.
- Patients in whom exercise is either contraindicated or who have a condition that interferes with exercising to target level are candidates for nuclear or echocardiographic pharmacologic stress testing.
- Patients with suspected coronary heart disease and for whom exercise or pharmacologic testing is contraindicated should be referred to a cardiologist for evaluation.
Most men and women experience symptoms before myocardial infarction (MI).1 Early recognition of these symptoms and prompt treatment are essential for prevention of death and disability related to coronary heart disease (CHD).
Patients with multiple risk factors, chest pain typically suggestive of CHD, or a history of CHD are usually easy to identify and triage. However, many patients do not have obvious risks for CHD but experience occasional symptoms of cardiac ischemia.
Patients can be stratified into low-, intermediate-, and high-risk categories that will help determine appropriate work-up. Those at intermediate risk can be difficult to assess, and may particularly benefit from stress-imaging studies.
The algorithm (Figure 1) is based on current guidelines,2 and indicates how patients with chest pain/symptoms may be identified and treated according to an initial estimate of the probability of obstructive coronary artery disease. The choice of noninvasive diagnostic tests for individuals with stable chest pain and a lower risk for CHD is then outlined.
Case studies
Patient 1
A 64-year-old, nonsmoking, obese woman with degenerative osteoarthritis of the knees occasionally experiences chest discomfort that lasts for a few minutes, sometimes radiating to her back. The discomfort, which started 4 weeks ago, occasionally becomes worse after a brief walk, but is not usually related to exertion, or associated with nausea or diaphoresis. She sometimes becomes short of breath climbing stairs.
Physical examination: In no acute distress; body-mass index 31.2, waist circumference 42 inches, heart rate 70 beats/min, blood pressure 142/88 mm Hg, cardiovascular examination unremarkable.
Laboratory evaluation: resting electrocardiogram (ECG)—sinus rhythm otherwise normal; creatinine 1.2 mg/dL; fasting glucose 122 mg/dL; glycosylated hemoglobin 6.4%. Lipids: total cholesterol 232 mg/dL; triglycerides 230 mg/dL; high-density lipoprotein (HDL) cholesterol 28 mg/dL; low-density lipoprotein (LDL) cholesterol 158 mg/dL.
Patient 2
A 58-year-old, nonsmoking, otherwise healthy man experiences tightness in the chest, usually at night. The pain began 4 to 8 weeks ago; it lasts as long as 1 to 2 hours but is “very mild.” It does not radiate to the arm or jaw and is unrelated to exertion. There is no diaphoresis or nausea. He sometimes feels a bit winded, which “might be due to anxiety.”
Physical examination: slightly overweight man in no acute distress; body-mass index 27.0, waist circumference 36 inches, heart rate 74 beats/min, blood pressure 138/88 mm Hg, cardiovascular examination unremarkable.
Laboratory evaluation: ECG— sinus rhythm, otherwise normal; creatinine 1.0 mg/dL; fasting glucose 98 mg/dL. Lipids: total cholesterol 215 mg/dL; triglycerides 150 mg/dL; HDL 40 mg/dL; LDL 145 mg/dL.
Diagnostic approaches
Standard diagnostic techniques include history, physical examination, laboratory testing as indicated, resting ECG, and assessment of risk factors for CHD.
Evaluation of chest pain
A careful history and physical examination can often quickly exclude many noncardiac causes of chest discomfort or pain. Table 1 contrasts the characteristics of atypical (noncardiac) symptoms with those of typical (cardiac) symptoms. Its quality, location, and the factors that relieve or provoke it, duration, and any associated symptoms should be evaluated. If high-risk or unstable signs or symptoms are present that suggest acute coronary syndrome (unstable angina or MI), evaluation in the emergency department should be performed.
Patients exhibiting stable or atypical (noncardiac) symptoms with some, but not all, of the features of angina described above have a lower probability of coronary artery disease, and should be considered for diagnostic evaluation under the guidance of the primary care physician.3
TABLE 1
Characteristics of atypical (noncardiac) vs typical cardiac symptoms
| Characteristic | Atypical/noncardiac | Typical/cardiac |
|---|---|---|
| Quality | Sharp, stabbing, positional | Squeezing, ache, pressure, fullness, burning, heavy, suffocating, “discomfort” |
| Location | Highly localized, below the epigastrium, above the mandible | Diffuse area—substernal, chest, jaw, back, arms |
| Provoked by | “Nothing,” body movement, cough, deep inspiration, chest palpation | Exertion, emotional stress, cold air |
| Relieved by | “Nothing,” position change, analgesics, heat, antacids | Rest; nitroglycerin |
| Duration | “Seconds” (fleeting), or hours, days | 30 seconds to 5 minutes |
| Associated symptoms | Reflux/heartburn | Dyspnea, diaphoresis, nausea, fatigue |
Evaluating women
In women aged <55 years, noncardiac chest pain is common, but since the prevalence of CHD is increasing among younger women, their symptoms should not be dismissed as “noncardiac” without full evaluation.
Women are also more likely than men to report dyspnea or pain in the jaw or back instead of, or in addition to, chest symptoms. Further, since women are often older and less active when they develop CHD, they may not exhibit typical exertional symptoms. Diagnosis in women is also hampered by lower accuracy of standard stress ECG testing compared with men. False-positive and false-negative tests may occur more frequently in women due to hormonal effects on the ECG, and more frequent comorbidities that limit maximal exercise capacity.
Physical examination
Palpation and auscultation of the chest may detect the presence of a friction rub or significant murmur, and thus identify a nonischemic cause for the chest symptoms. Carotid bruits or reduced pedal pulses indicate the presence of other vascular diseases. Patients with xanthomas, hypertension, or signs of congestive heart failure are more likely to have CHD, while those whose pain can be reproduced by body movement or by palpating the chest are less likely to have CHD.
Risk factor assessment. The assessment of risk factors for CHD allows the identification of many patients at high risk for CHD and can be helpful in guiding the choice of additional tests. As evident in the Framingham Heart Study,4 independent risk factors such as cigarette smoking, hypertension, diabetes mellitus, and hyperlipidemia are direct causes of CHD.
Laboratory tests
In the patient at low risk of CHD, blood testing for cardiac markers is not indicated. A lipid profile and blood glucose level help to establish the risk level associated with hyperlipidemia and diabetes. A complete blood count (eg, for anemia), thyroid hormone studies (eg, for hyperthyroidism), arterial blood gases (eg, PCO2 for chronic obstructive pulmonary disease), and other tests may help in diagnosing contributory conditions.
Resting electrocardiogram
A routine resting 12-lead ECG is an inexpensive but critical test that can provide important diagnostic and prognostic information. Evidence of infarction, ischemia, hypertrophy arrhythmias, and conduction disturbances can be detected and, if present, substantially increase the likelihood of a cardiac cause of symptoms.
Even the presence of mild or nonspecific ST-T wave changes, while not diagnostic, can aid the clinician by suggesting a higher probability of a nondiagnostic stress ECG and the need for an imaging stress test.3 An abnormal resting ECG with ST-T wave changes associated with digoxin use, left bundle branch block, left ventricular hypertrophy, and so on, limit interpretation of an exercise ECG, and points to a need for exercise testing with imaging.
It is important to note that a normal ECG obtained when the patient is asymptomatic does not exclude CHD, and additional risk stratification with noninvasive diagnostic stress testing may be indicated.5
Chest x-ray
A chest x-ray is often appropriate for patients with cardiac or pulmonary signs/symptoms. It may show cardiac enlargement, ventricular aneurysm, or evidence of heart failure, which may support the diagnosis of CHD and help to assess the extent of cardiopulmonary involvement.
Noninvasive stress testing
Considering our 2 patients with occasional episodes of unexplained chest discomfort: Based on the ECG and clinical findings, their risk for CHD is considered low to intermediate.
Test selection
Diagnostic tests should be selected based on the clinician’s estimate of probability of CHD.2
Low probability. If the likelihood of CHD is low, stress testing is generally not indicated, as its specificity is extremely low, and test results do not improve diagnostic accuracy over the clinical impression alone.
Intermediate probability. If the patient is able to exercise to capacity, the choice is exercise testing. Patients who can exercise and have an interpretable ECG, with no evidence of left ventricular dysfunction and no prior revascularization procedure, should usually undergo standard stress ECG testing. If the ECG is not interpretable, (due to repolarization abnormalities, left bundle branch block, left ventricular hypertrophy, digoxin use, etc) an exercise test with imaging (nuclear or echocardiographic) is indicated.
For patients unable to exercise, pharmacologic stress testing with imaging is indicated.
High probability. If the probability of CHD is high, it is reasonable to proceed directly to coronary angiography.
Exercise stress test
Exercise testing is a cardiovascular stress that uses treadmill or bicycle exercise with ECG and blood pressure monitoring. Such testing is widely available and relatively inexpensive.2 It allows assessment of exercise capacity and correlation of symptoms with ECG changes typical of myocardial ischemia.
Exercise testing provides the highest level of incremental diagnostic and prognostic information for patients with an intermediate probability of CHD.2 An important objective of stress testing is to identify individuals with a high risk for severe (left main or 3-vessel) CHD. More invasive procedures, such as percutaneous cutaneous angioplasty (PCTA), are recommended for these high-risk individuals to improve their survival.
Candidates for exercise treadmill testing include patients with stable symptoms who can be expected to exercise to an adequate workload. Patients with repolarization abnormalities on the resting ECG, such as left bundle branch block, left ventricular hypertrophy, or digoxin use, frequently have noninterpretable stress ECGs and may benefit from imaging techniques.
Limitations. Some patients referred for exercise treadmill testing are unable to achieve either adequate exercise levels or the target heart rate due to comorbid conditions,6 such as degenerative joint disease, obesity, pulmonary disease, peripheral vascular disease, central nervous system disorders, physical deconditioning, chronotropic incompetence, and medications such as beta blockers. More subtle factors, such as an unwillingness to exercise, may also affect a patient’s suitability for stress testing. These patients should be considered for pharmacologic stress testing.
Additionally, stress-induced ST-T wave changes do not accurately localize the site of myocardial ischemia and provide no direct information on left ventricular function and other clinically important variables. The sensitivity and specificity of exercise ECG testing ranges from approximately 67% to 72%, which is below that of stress imaging techniques, whose average sensitivity ranges from 80% to 85%.7-9
Stress imaging modalities
For a patient with an abnormal resting ECG, evidence of left ventricular dysfunction, or a prior coronary revascularization, stress imaging with either echocardiography or nuclear perfusion scanning is appropriate. Both techniques show higher specificity than the stress ECG alone.
Nuclear imaging. Nuclear imaging uses radiotracers (thallium-201, technetium-99m tetrofosmin [Myoview], or technetium-99m sestamibi [Cardiolite]) to evaluate myocardial perfusion and function, and has greatly advanced the ability to detect and assess the extent of CHD. Stress myocardial perfusion imaging has a sensitivity of >90% for detecting patients at risk of cardiac death or MI.6
To detect ischemia or infarction, a radioisotope is injected at rest and after stress to produce images of myocardial regional uptake, which is proportional to regional blood flow. Normally, with maximal exercise or pharmacologic stress, myocardial blood flow is greatly increased above the resting condition. If a fixed coronary stenosis is present, myocardial perfusion in the territory supplied by the stenosis cannot be increased, which will create a flow differential and uneven distribution of the tracer.
As illustrated in Figure 2, a normal myocardial perfusion image shows homogenous accumulation of radiotracer on both the stress and rest images. A perfusion defect appears as an area of reduced tracer uptake.
Nuclear perfusion studies can also provide a measure of left ventricular function and wall motion utilizing a bolus injection of radiotracer. While images can be obtained in most patients utilizing current techniques, artifacts due to breast and diaphragmatic tissue attenuation can lead to false-positive interpretation, particularly when examining women and when using thallium.
Echocardiography. Echocardiography visualizes the heart directly in real time using ultrasound, providing convenient assessment of the cardiac chambers, myocardium, valves, pericardium, and great vessels. The test can also identify mechanical complications of acute myocardial infarction, differentiate causes of reduced cardiac output and blood pressure, and help guide therapy. Stress echocardiography (exercise or pharmacologic stress) can be used to detect the presence, location, and severity of inducible myocardial ischemia as well as for risk stratification and prognosis.
During stress-induced ischemia, decrements in contractile function are directly related to decreases in regional subendocardial blood flow. Wall-motion changes precede ischemic ECG changes, accounting for the increased sensitivity of echocardiography versus ECG stress testing.
Interpretation of stress echocardiograms is based on analysis of segmental wall motion before and soon after stress. Normally, with exercise, or dobutamine infusion, left ventricular wall motion becomes hyperdynamic. The hallmark of ischemia is the development with stress of new, or the worsening of preexisting, wall motion abnormalities. The lack of improvement with stress in an already hypokinetic segment indicates infarction. Stress-induced left ventricular cavity enlargement, systolic dysfunction, or mitral regurgitation may also suggest CHD. Accuracy of stress echocardiography is similar to that of nuclear stress testing.
Considerable expertise in echocardiography is needed to rapidly acquire diagnostic images, so that its selection is limited by the skill of the technician. Image quality can be compromised by obesity and other factors, but the widespread use of intravenous contrast agents has significantly reduced the proportion of patients with uninterpretable images.
FIGURE 2
Accumulation of radiotracer in nuclear imaging (stress and rest images)
Patients who are not expected to achieve an adequate exercise capacity (as in our patient with osteoarthritis) should undergo pharmacologic stress testing with adenosine, dipyridamole, or dobutamine. Atrial pacing utilizing a swallowed esophageal electrode is also used in some cases. These agents, combined with echocardiographic or nuclear imaging, are particularly useful in patients who are unable to exercise adequately.
Pharmacologic stress agents are sometimes combined with low-level exercise protocols which may reduce the noncardiac side effects and improve image quality.10
Adenosine is the pharmacologic agent used most commonly in nuclear perfusion stress testing. An intravenous infusion of adenosine produces coronary vasodilation which is quickly attenuated when the infusion is terminated. Side effects, which are short-lived, include flushing, palpitations, and chest pain.
Dipyridamole is used less commonly due to its prolonged side effects and reports of lower specificity.11 Dobutamine, a beta-adrenergic agonist, increases heart rate and contractility in a dose-related fashion when infused intravenously. This agent is most commonly used in echocardiographic imaging. It can also be utilized with nuclear imaging when adenosine is contraindicated due to severe pulmonary or cerebrovascular disease. Side effects include transient arrhythmias, hypertension or hypotension, tremor, and chest pain.
Referral to a cardiologist
Referral to a cardiologist should be considered when the suspicion for cardiac disease is high, there is substantial diagnostic uncertainty after initial evaluation, or if symptoms persist, despite treatment of a noncardiac cause. Further evaluation and treatment often includes coronary angiography.
Coronary angiography
Most outpatients, such as the 2 presented, can be diagnosed with clinical and noninvasive measures. Coronary angiography is most commonly used to determine the presence and extent of obstructive CHD, and to guide decisions about revascularization in high-risk patients, or in patients with an abnormal stress test.
Cardiac catheterization presents a small but real risk to the patient, involves discomfort and substantial cost, and can challenge effective resource utilization. Risks and benefits to individual patients should be discussed between primary care physician and cardiologist.
Summary
Findings in our 2 patients are summarized below. Diagnostic decisions reflect the algorithm in Figure 1and are based on current guidelines.2
Patient 1. After initial assessment, our 64-year-old asymptomatic woman still falls into “intermediate probability of CHD” due to her multiple CHD risks. Stress testing was therefore indicated. Due to her inability to exercise because of an orthopedic limitation, she underwent pharmacologic stress testing with an adenosine sestamibi study. A small inferior reversible defect was identified, suggestive of myocardial ischemia.
Aggressive medical therapy aimed at minimizing symptoms and reducing risk was selected: aspirin, a beta-blocker for ischemia and hypertension, and a statin for hyperlipidemia. Longacting nitrates or calcium-channel blockers would have been reasonable alternatives. Consideration of an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker is also indicated in light of her new CHD diagnosis and glucose intolerance. She was advised to initiate a low-fat, low-carbohydrate diet and to exercise (swim) regularly to lower risk. She will be seen in 6 weeks to reevaluate her symptoms, blood pressure, and lipid and glycemic control.
Patient 2. Our male patient also warranted stress testing. He was referred for a standard stress ECG due to his normal resting ECG, and the expectation that he would be able to exercise adequately. He satisfactorily completed 10.5 minutes (10 METS) of a Bruce protocol on a treadmill exercise stress test, which was entirely normal.
This admittedly anxious individual was reassured that his chest symptoms are not due to heart disease. An empiric trial with a proton pump inhibitor could be initiated if gastro-esophageal reflux is suspected.
Conclusions
Standard treadmill exercise testing for diagnosis and risk stratification is suitable for patients with a normal resting ECG and without contraindications to exercise, as in our male patient. Those with an uninterpretable ECG should undergo either nuclear or echocardiographic imaging in concert with their exercise test. Patients in whom exercise is either contraindicated or who have a condition that interferes with exercising to the target level are candidates for nuclear or echocardiographic pharmacologic stress testing, as was indicated for our female patient. Patients with suspected CHD and for whom exercise or pharmacologic testing is contraindicated should be referred to a cardiologist for evaluation.
Finally, when selecting a specific stress imaging technique, physicians should consider the local expertise with the various techniques available, together with their strengths and limitations in the individual patient.19
1. Spertus JA, Radford MJ, Every NR, et al. Challenges and opportunities in quantifying the quality of care for acute myocardial infarction. Summary from the Acute Myocardial Infarction Working Group of the American Heart Association/American College of Cardiology First Scientific Forum on Quality of Care and Outcomes Research in Cardiovascular Disease and Stroke. Circulation 2003;107:1681-1691.
2. Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to update the 1997 exercise testing guidelines). Circulation 2002;106:1883-1892.
3. Gibbons RJ, Chatterjee K, Daley J, et al. ACC/AHA/ACP-ASIM guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients With Chronic Stable Angina). J Am Coll Cardiol 1999;33:2092-2197.
4. Grundy SM, Balady GJ, Criqui MH, et al. Primary prevention of coronary heart disease: guidance from Framingham: a statement for healthcare professionals from the American Heart Association Task Force on Risk Reduction. Circulation 1998;97:1876-1887.
5. Zanger DR, Solomon AJ, Gersh BJ. Contemporary management of angina: part I: risk assessment. Am Fam Physician 1999;60:2543-2552.
6. Bar Harbor Invitation Meeting 2000. Panel 9: Nuclear imaging in coronary artery disease. J Nucl Cardiol 2001;8:305-316.
7. Kotler TS, Diamond GA. Exercise thallium-201 scintigraphy in the diagnosis and prognosis of coronary artery disease. Ann Intern Med 1990;113:684-702.
8. Gibbons RJ. Rest and exercise radionuclide angiography for diagnosis in chronic ischemic heart disease. Circulation 1991;84 (3 Suppl):I93-I99.
9. Roger VL, Pellikka PA, Oh JK, Miller FA, Seward JB, Tajik AJ. Stress echocardiography. Part I. Exercise echocardiography: techniques, implementation, clinical applications, and correlations. Mayo Clin Proc 1995;70:5-15.
10. Thomas GS, Prill NV, Majmundar H, et al. Treadmill exercise during adenosine infusion is safe, results in fewer adverse reactions, and improves myocardial perfusion image quality. J Nucl Cardiol 2000;7:439-446.
11. Li T, Ahlberg A, Hachamovitch R, et al. Comparison of adenosine and dipyridamole in detecting coronary artery disease using Tc-99m sestamibi single-photon emission computed tomography imaging: a randomized, prospective clinical study. J Am Coll Cardiol 2003;41(suppl A):461A. Abstract 858-3.
12. American Heart Association. Heart disease and stroke statistics—2003 update. Dallas, Tex: American Heart Association; 2003.
This special section of The Journal of Family Practiceis provided by an unrestricted grant fromFujisawa Healthcare, Inc. Disclosures: Dr McBride has served on the speakers’ bureau for the following: Abbott Laboratories, Astra-Zeneca, Bristol-Myers Squibb, Glaxo SmithKline, KOS Pharmaceuticals, Merck & Co Inc, Pfizer Inc, Reliant Pharmaceuticals, and Sankyo. He has served as consultant to KOS Pharmaceuticals, Merck & Co Inc, and Pfizer Inc. He has received grant/research support from Merck & Co Inc and Pfizer Inc. Dr Hayes had no commercial interests to report. Corresponding author: Sharonne N. Hayes, MD, Mayo Clinic Women’s Heart Clinic, Rochester MN, 55905. E-mail: [email protected].
1. Spertus JA, Radford MJ, Every NR, et al. Challenges and opportunities in quantifying the quality of care for acute myocardial infarction. Summary from the Acute Myocardial Infarction Working Group of the American Heart Association/American College of Cardiology First Scientific Forum on Quality of Care and Outcomes Research in Cardiovascular Disease and Stroke. Circulation 2003;107:1681-1691.
2. Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to update the 1997 exercise testing guidelines). Circulation 2002;106:1883-1892.
3. Gibbons RJ, Chatterjee K, Daley J, et al. ACC/AHA/ACP-ASIM guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients With Chronic Stable Angina). J Am Coll Cardiol 1999;33:2092-2197.
4. Grundy SM, Balady GJ, Criqui MH, et al. Primary prevention of coronary heart disease: guidance from Framingham: a statement for healthcare professionals from the American Heart Association Task Force on Risk Reduction. Circulation 1998;97:1876-1887.
5. Zanger DR, Solomon AJ, Gersh BJ. Contemporary management of angina: part I: risk assessment. Am Fam Physician 1999;60:2543-2552.
6. Bar Harbor Invitation Meeting 2000. Panel 9: Nuclear imaging in coronary artery disease. J Nucl Cardiol 2001;8:305-316.
7. Kotler TS, Diamond GA. Exercise thallium-201 scintigraphy in the diagnosis and prognosis of coronary artery disease. Ann Intern Med 1990;113:684-702.
8. Gibbons RJ. Rest and exercise radionuclide angiography for diagnosis in chronic ischemic heart disease. Circulation 1991;84 (3 Suppl):I93-I99.
9. Roger VL, Pellikka PA, Oh JK, Miller FA, Seward JB, Tajik AJ. Stress echocardiography. Part I. Exercise echocardiography: techniques, implementation, clinical applications, and correlations. Mayo Clin Proc 1995;70:5-15.
10. Thomas GS, Prill NV, Majmundar H, et al. Treadmill exercise during adenosine infusion is safe, results in fewer adverse reactions, and improves myocardial perfusion image quality. J Nucl Cardiol 2000;7:439-446.
11. Li T, Ahlberg A, Hachamovitch R, et al. Comparison of adenosine and dipyridamole in detecting coronary artery disease using Tc-99m sestamibi single-photon emission computed tomography imaging: a randomized, prospective clinical study. J Am Coll Cardiol 2003;41(suppl A):461A. Abstract 858-3.
12. American Heart Association. Heart disease and stroke statistics—2003 update. Dallas, Tex: American Heart Association; 2003.
This special section of The Journal of Family Practiceis provided by an unrestricted grant fromFujisawa Healthcare, Inc. Disclosures: Dr McBride has served on the speakers’ bureau for the following: Abbott Laboratories, Astra-Zeneca, Bristol-Myers Squibb, Glaxo SmithKline, KOS Pharmaceuticals, Merck & Co Inc, Pfizer Inc, Reliant Pharmaceuticals, and Sankyo. He has served as consultant to KOS Pharmaceuticals, Merck & Co Inc, and Pfizer Inc. He has received grant/research support from Merck & Co Inc and Pfizer Inc. Dr Hayes had no commercial interests to report. Corresponding author: Sharonne N. Hayes, MD, Mayo Clinic Women’s Heart Clinic, Rochester MN, 55905. E-mail: [email protected].