User login
Delivering patient‐centered care is at the core of ensuring patient engagement and active participation that will lead to positive outcomes. Physician‐patient interaction has become an area of increasing focus in an effort to optimize the patient experience. Positive patient‐provider communication has been shown to increase satisfaction,[1, 2, 3, 4] decrease the likelihood of medical malpractice lawsuits,[5, 6, 7, 8] and improve clinical outcomes.[9, 10, 11, 12, 13] Specifically, a decrease in psychological symptoms such as anxiety and stress, as well as perception of physical symptoms have been correlated with improved communication.[9, 12] Furthermore, objective health outcomes, such as improvement in hypertension and glycosylated hemoglobin, have also been correlated with improved physician‐patient communication.[10, 11, 13] The multifaceted effects of improved communication are impactful to both the patient and the physician; therefore, it is essential that we understand how to optimize this interaction.
Patient‐centered care is a critical objective for many high‐quality healthcare systems.[14] In recent years, the use of electronic health records (EHRs) has been increasingly adopted by healthcare systems nationally in an effort to improve the quality of care delivered. The positive benefits of EHRs on the facilitation of healthcare, including consolidation of information, reduction of medical errors, easily transferable medical records,[15, 16, 17] as well as their impact on healthcare spending,[18] are well‐documented and have been emphasized as reasons for adoption of EHRs by the Patient Protection and Affordable Care Act. However, EHR implementation has encountered some resistance regarding its impact on the patient experience.
As EHR implementation is exponentially increasing in the United States, there is limited literature on the consequences of this technology.[19] Barriers reported during EHR implementation include the limitations of standardization, attitudinal and organizational constraints, behavior of individuals, and resistance to change.[20] Additionally, poor EHR system design and improper use can cause errors that jeopardize the integrity of the information inputted, leading to inaccuracies that endanger patient safety or decrease the quality of care.[21]
One of the limitations of EHRs has been the reported negative impact on patient‐centered care by decreasing communication during the hospital visit.[22] Although the EHR has enhanced internal provider communication,[23] the literature suggests a lack of focus on the patient sitting in front of the provider. Due to perceived physician distraction during the visit, patients report decreased satisfaction when physicians spend a considerable period of time during the visit at the computer.[22] Furthermore, the average hospital length of stay has been increased due to the use of EHRs.[22]
Although some physicians report that EHR use impedes patient workflow and decreases time spent with patients,[23] previous literature suggests that EHRs decrease the time to develop a synopsis and improve communication efficiency.[19] Some studies have also noted an increase in the ability for medical history retrieval and analysis, which will ultimately increase the quality of care provided to the patient.[24] Physicians who use the EHR adopted a more active role in clarifying information, encouraging questions, and ensuring completeness at the end of a visit.[25] Finally, studies show that the EHR has a positive return on investment from savings in drug expenditures, radiology tests, and billing errors.[26] Given the significant financial and time commitment that health systems and physicians must invest to implement EHRs, it is vital that we understand the multifaceted effects of EHRs on the field of medicine.
METHODS
The purpose of this study was to assess the physician‐patient communication patterns associated with the implementation and use of an EHR in a hospital setting.
ARC Medical Program
In 2006, the Office of Patient Experience at University of California, Los Angeles (UCLA) Health, in conjunction with the David Geffen School of Medicine at UCLA, launched the Assessing Residents' CI‐CARE (ARC) Medical Program. CI‐CARE is a protocol that emphasizes for medical staff and providers to Connect with their patients, Introduce themselves, Communicate their purpose, Ask or anticipate patients' needs, Respond to questions with immediacy, and to Exit courteously. CI‐CARE represents the standards for staff and providers in any encounter with patients or their families. The goals of the ARC Medical Program are to monitor housestaff performance and patient satisfaction while improving trainee education through timely and patient‐centered feedback. The ARC Medical Program's survey has served as an important tool to assess and improve physician professionalism and interpersonal skills and communication, 2 of the Accreditation Council for Graduate Medical Education core competencies.[27]
The ARC program is a unique and innovative volunteer program that provides timely and patient‐centered feedback from trainees' daily encounters with hospitalized patients. The ARC Medical Program has an established infrastructure to conduct evaluations on a system‐wide scale, including 9 departments within UCLA Health. ARC volunteers interview patients using a CI‐CARE Questionnaire (ARC survey) to assess their resident physician's communication patterns. The ARC Survey targets specific areas of the residents' care as outlined by the CI‐CARE Program of UCLA Health.
As part of UCLA Health's mission to ensure the highest level of patient‐centered care, the CI‐CARE standards were introduced in 2006, followed by implementation of the EHR system. Given the lack of previous research and conflicting results on the impact of EHRs on the patient experience, this article uses ARC data to assess whether or not there was a significant difference following implementation of the EHR on March 2, 2013.
The materials and methods of this study are largely based on those of a previous study, also published by the ARC Medical Program.[27]
CI‐CARE QuestionnaireARC Survey
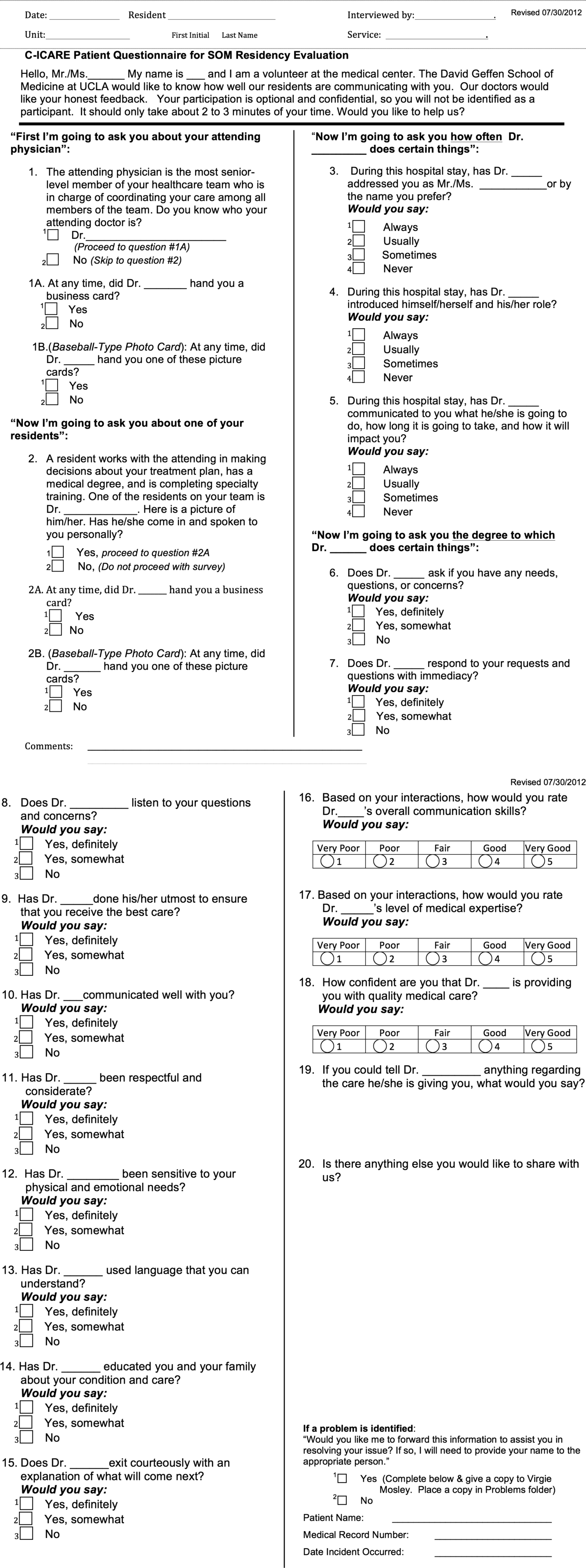
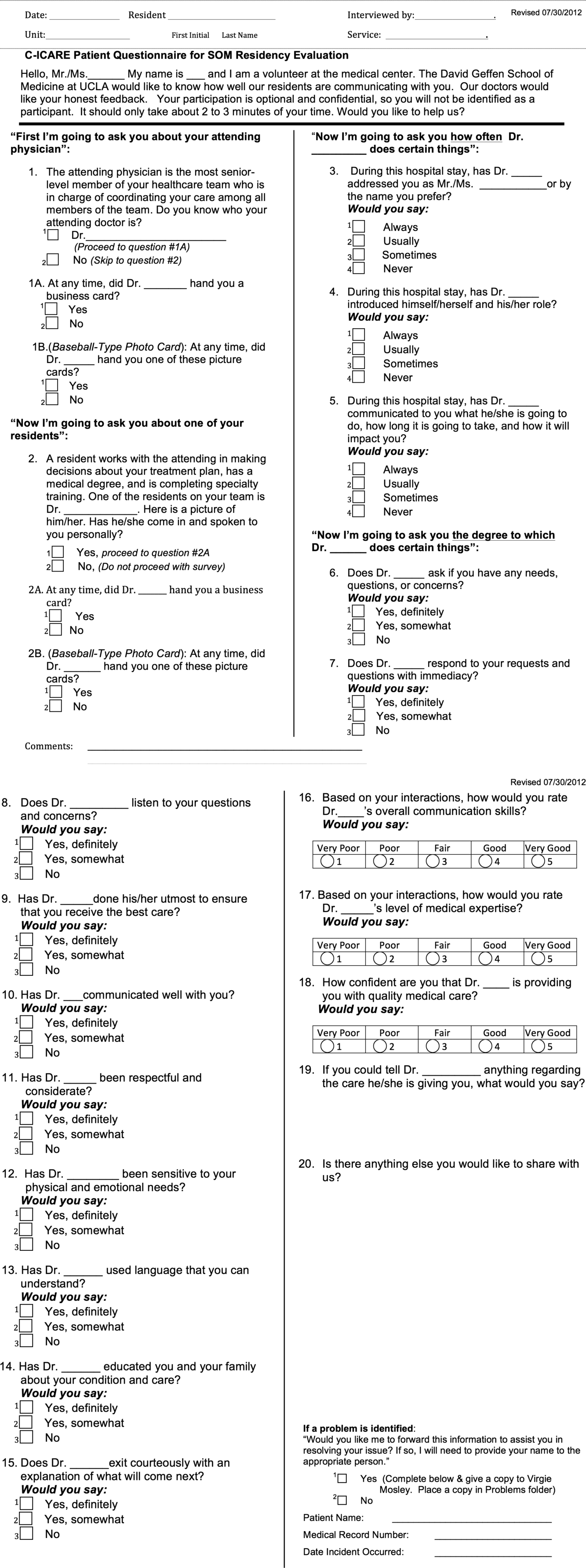
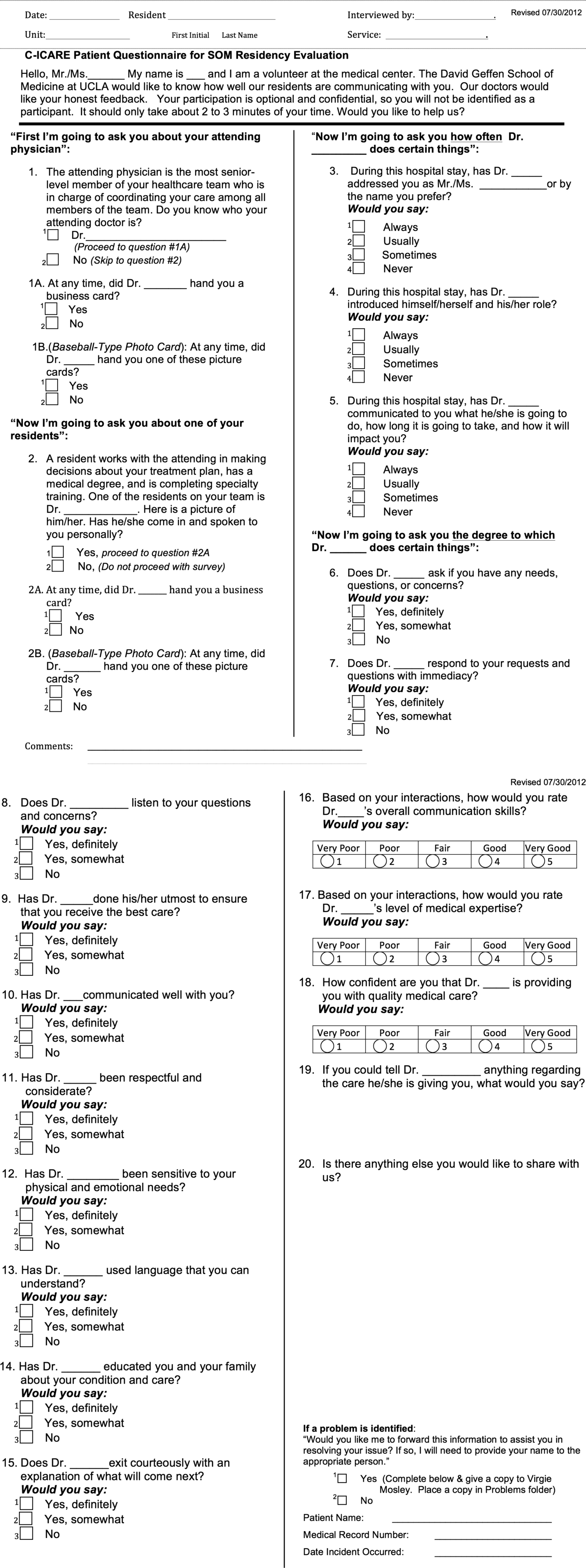
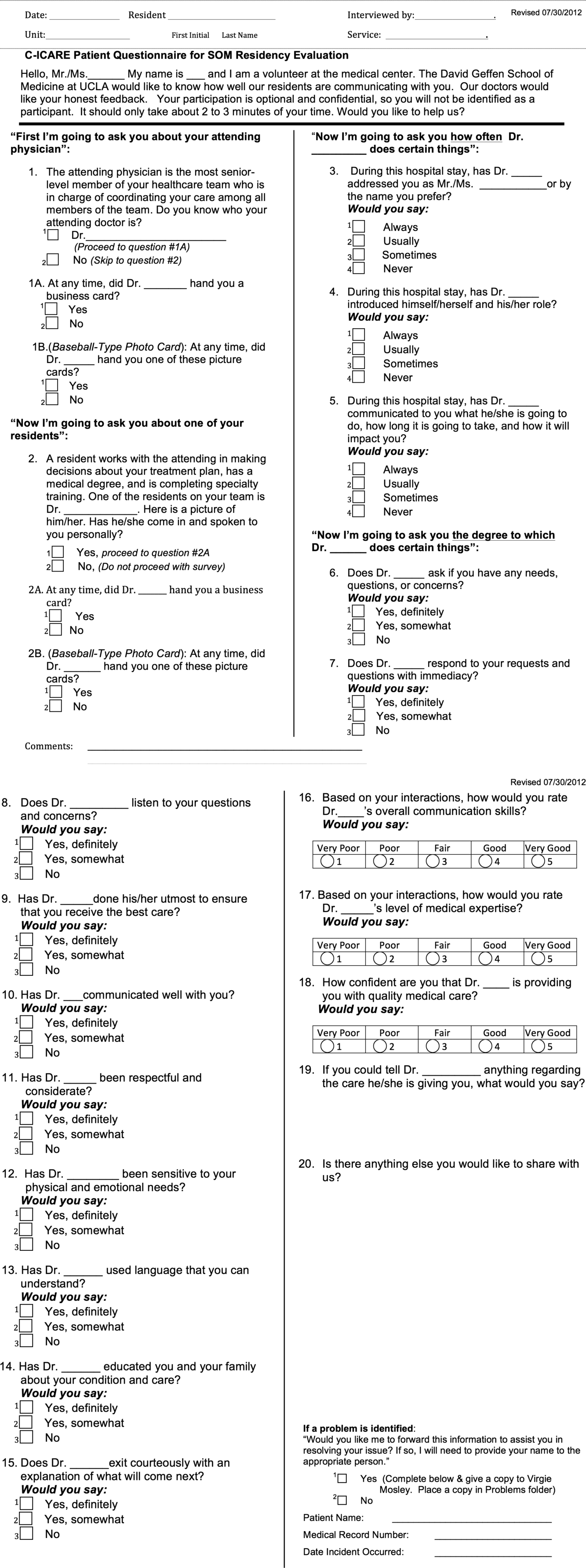
The CI‐CARE Questionnaire is a standardized audit tool consisting of a total of 20 questions used by the facilitators who work with ARC. There are a total of 20 items on the ARC survey, including 18 multiple‐choice, polar, and Likert‐scale questions, and 2 free‐response questions that assess the patients' overall perception of their resident physician and their hospital experience. Questions 1 and 2 pertain to the recognition of attending physicians and resident physicians, respectively. Questions 3, 4, 6, 7, and 8 are Likert‐scalebased questions assessing the residents' professionalism. Questions 9 through 14 are Likert‐scalebased items included to evaluate the quality of communication between patient and provider. We categorized questions 5 and 15 as relating to diagnostics.[27] In 2012, ARC implemented 3 additional questions that assessed residents' communication skills (question 16), level of medical expertise (question 17), and quality of medical care (question 18). We chose to examine the CI‐CARE Questionnaire instead of a standard survey such as the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), because it examines the physician‐patient interaction in more detail. The survey can be reviewed in Figure 1.
Interview Procedure
The ARC Medical Program is comprised of 47 premedical UCLA students who conducted the surveys. New surveyors were trained by the senior surveyors for a minimum of 12 hours before conducting a survey independently. All surveyors were evaluated biyearly by their peers and the program director for quality assurance and to ensure uniform procedures. The volunteers' surveying experience on December 1, 2012 was as follows: (=10 months [237 months], =10 months).
Prior to the interview, the surveyor introduces himself or herself, the purpose and length of the interview, and that the patient's anonymous participation is optional and confidential. Upon receiving verbal consent from the patient, the surveyor presents a picture card to the patient and asks him or her to identify a resident who was on rotation who treated them. If the patient is able to identify the resident who treated them, the surveyor asks each question and records each response verbatim. The surveyors are trained not to probe for responses, and to ensure that the patients answer in accordance with the possible responses. Although it has not been formally studied, the inter‐rater reliability of the survey is likely to be very high due to the verbatim requirements.
Population Interviewed
A total of 3414 surveys were collected from patients seen in the departments of internal medicine, family medicine, pediatrics, general surgery, head and neck surgery, orthopedic surgery, neurosurgery, neurology, and obstetrics and gynecology in this retrospective cohort study. Exclusion criteria included patients who were not awake, were not conscious, could not confidently identify a resident, or stated that they were not able to confidently complete the survey.
Data Analysis
The researchers reviewed and evaluated all data gathered using standard protocols. Statistical comparisons were made using [2] tests. All quantitative analyses were performed in Excel 2010 (Microsoft Corp., Redmond, WA) and SPSS version 21 (IBM Corp., Armonk, NY).
Institutional Review Board
This project received an exemption by the UCLA institutional review board.
RESULTS
There were a total of 3414 interviews conducted and completed from December 1, 2012 to May 30, 2013. Altogether, 1567 surveys were collected 3 months prior to EHR implementation (DecemberFebruary), and 1847 surveys were collected 3 months following implementation (MarchMay). The survey breakdown is summarized in Table 1.
| Department | Pre (N) | Post (N) | Total (N) |
|---|---|---|---|
| |||
| Family medicine | 65 | 128 | 193 |
| General surgery | 226 | 246 | 472 |
| Head and neck surgery | 43 | 65 | 108 |
| Internal medicine | 439 | 369 | 808 |
| Neurology | 81 | 98 | 179 |
| Neurosurgery | 99 | 54 | 153 |
| OB/GYN | 173 | 199 | 372 |
| Orthopedic surgery | 117 | 128 | 245 |
| Pediatrics | 324 | 563 | 887 |
| Totals | 1,567 | 1,850 | 3,417 |
2 analysis revealed that the residents received significantly better feedback in the 3 months following EHR implementation, compared to the 3 months prior to implementation on questions 3, addressing the patient by their preferred name; 4, introducing themselves and their role; 5, communicating what they will do, how long it will take, and how it will impact the patient; 7, responding to the patient's requests and questions with immediacy; 8, listening to the patient's questions and concerns; 9, doing their utmost to ensure the patient receives the best care; 10, communicating well with the patient; 11, being respectful and considerate; and 12, being sensitive to the patient's physical and emotional needs (P<0.05) (Table 2).
| Question | Pre‐EHR % Responses (n=1,567) | Post‐EHR % Responses (n=1,850) | 2 Significance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| ||||||||||||
| 3 | Address you by preferred name? | 90.1 | 3.8 | 2.7 | 3.4 | 91.5 | 3.6 | 1.3 | 3.6 | 0.032* | ||
| 4 | Introduce himself/herself? | 88.3 | 6.4 | 3.2 | 2.1 | 93.1 | 3.6 | 1.8 | 1.5 | 0.000* | ||
| 5 | Communicate what he/she will do? | 83.1 | 9.3 | 4.5 | 3.2 | 86.9 | 6.4 | 3.5 | 3.3 | 0.006* | ||
| 6 | Ask if you have any questions? | 90.9 | 6.2 | 2.9 | 92.4 | 4.9 | 2.7 | 0.230 | ||||
| 7 | Respond with immediacy? | 92.5 | 5.4 | 2.2 | 94.6 | 3.4 | 2.1 | 0.015* | ||||
| 8 | Listens to your questions and concerns? | 94.8 | 4.0 | 1.1 | 96.6 | 2.4 | 1.0 | 0.022* | ||||
| 9 | Ensure you received the best care? | 92.4 | 6.3 | 1.3 | 95.2 | 3.9 | 1.0 | 0.003* | ||||
| 10 | Communicates well with you? | 92.3 | 6.3 | 1.5 | 94.8 | 4.2 | 0.9 | 0.009* | ||||
| 11 | Is respectful and considerate? | 96.5 | 2.7 | 0.8 | 98.0 | 1.6 | 0.4 | 0.025* | ||||
| 12 | Sensitive to your physical and emotional needs? | 90.4 | 6.9 | 2.7 | 94.5 | 3.9 | 1.6 | 0.000* | ||||
| 13 | Uses language that you can understand? | 96.5 | 2.8 | 0.7 | 96.9 | 2.8 | 0.4 | 0.431 | ||||
| 14 | Educated you/family about condition/care? | 84.0 | 8.6 | 7.4 | 86.6 | 7.4 | 6.0 | 0.111 | ||||
| 15 | Exit courteously? | 89.7 | 6.6 | 3.6 | 91.7 | 5.2 | 3.1 | 0.130 | ||||
| 16 | Communication skills? | 75.6 | 19.5 | 3.6 | 0.7 | 0.7 | 78.6 | 16.9 | 3.9 | 0.4 | 0.3 | 0.077 |
| 17 | Medical expertise? | 79.5 | 15.9 | 3.5 | 0.7 | 0.4 | 80.0 | 16.5 | 2.7 | 0.5 | 0.2 | 0.398 |
| 18 | Quality medical care? | 82.5 | 13.0 | 2.8 | 0.8 | 0.9 | 82.6 | 13.6 | 2.7 | 0.7 | 0.5 | 0.754 |
ARC surveyed for 10 weeks prior to our reported sample (OctoberDecember) and 22 weeks prior to EHR implementation total (OctoberMarch). To rule out resident improvement due to the confounding effects of time and experience, we compared the data from the first 11 weeks (OctoberDecember) to the second 11 weeks (DecemberMarch) prior to EHR implementation. [2] analysis revealed that only 6 of the 16 questions showed improvement in this period, and just 1 of these improvements (question 3) was significant. Furthermore, 10 of the 16 questions actually received worse responses in this period, and 2 of these declines (questions 9 and 12) were significant (Table 3).
| Question | First 11 Weeks' Responses (n=897) | Second 11 Weeks' Responses (n=1,338) | 2 Significance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| ||||||||||||
| 3 | Address you by preferred name? | 87.1 | 6.4 | 4.6 | 2.0 | 90.7 | 3.7 | 2.3 | 3.4 | 0.000* | ||
| 4 | Introduce himself/herself? | 87.7 | 6.9 | 4.1 | 1.2 | 88.3 | 6.1 | 3.3 | 2.3 | 0.174 | ||
| 5 | Communicate what he/she will do? | 82.9 | 8.2 | 5.1 | 3.7 | 83.2 | 9.1 | 4.3 | 3.4 | 0.698 | ||
| 6 | Ask if you have any questions? | 92.0 | 5.9 | 2.1 | 90.7 | 6.1 | 3.1 | 0.336 | ||||
| 7 | Respond with immediacy? | 91.2 | 6.6 | 2.2 | 92.8 | 5.2 | 2.1 | 0.353 | ||||
| 8 | Listens to your questions and concerns? | 94.6 | 3.9 | 1.4 | 95.0 | 3.8 | 1.2 | 0.868 | ||||
| 9 | Ensure you received the best care? | 94.4 | 5.0 | 0.6 | 92.1 | 6.5 | 1.4 | 0.049* | ||||
| 10 | Communicates well with you? | 93.3 | 5.9 | 0.8 | 92.4 | 5.9 | 1.7 | 0.167 | ||||
| 11 | Is respectful and considerate? | 97.3 | 2.1 | 0.6 | 96.4 | 2.7 | 0.9 | 0.455 | ||||
| 12 | Sensitive to your physical and emotional needs? | 93.2 | 5.5 | 1.3 | 90.3 | 6.9 | 2.8 | 0.022* | ||||
| 13 | Uses language that you can understand? | 96.2 | 3.5 | 0.3 | 96.4 | 2.8 | 0.7 | 0.327 | ||||
| 14 | Educated you/family about condition/care? | 85.7 | 8.9 | 5.4 | 83.8 | 8.7 | 7.5 | 0.141 | ||||
| 15 | Exit courteously? | 89.7 | 7.8 | 2.5 | 89.6 | 6.6 | 3.8 | 0.124 | ||||
| 16 | Communication skills? | 78.7 | 17.1 | 2.9 | 0.7 | 0.7 | 75.9 | 19 | 3.6 | 0.7 | 0.8 | 0.633 |
| 17 | Medical expertise? | 82.3 | 13.3 | 3.9 | 0.1 | 0.4 | 78.9 | 16.1 | 3.6 | 0.8 | 0.5 | 0.062 |
| 18 | Quality medical care? | 82.7 | 13.5 | 2.6 | 0.8 | 0.4 | 82.1 | 13.0 | 3.0 | 0.9 | 1.0 | 0.456 |
DISCUSSION
The adoption of EHRs has been fueled by their suggested improvement on healthcare quality and spending.[15, 16, 17, 18] Few studies have investigated the patient experience and its relation to EHR implementation. Furthermore, these studies have not yielded consistent results,[19, 20, 21, 22, 23, 25] raising uncertainty about the effects of EHRs on the patient experience. Possible barriers that may contribute to the scarcity of literature include the relatively recent large‐scale implementation of EHRs and a lack of programs in place to collect extensive data on the physician‐patient relationship.
In a field with increasing demands on patient‐centered care, we need to find ways to preserve and foster the patient‐physician relationship. Given that improvements in the delivery of compassionate care can positively impact clinical outcomes, the likelihood of medical malpractice lawsuits, and patient satisfaction,[1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13] the need to improve the patient‐provider relationship is tremendously important. Following EHR implementation, residents were perceived to provide more frequent diagnostics information including the nature, impact, and treatment of conditions. Furthermore, they were perceived to provide significantly better communication quality following implementation, through care monitoring, respectful and sensitive communication, and enhanced patient and family education. Residents were also perceived as being more professional following implementation, as indicated by positive assessments of several interpersonal communication questions. These results suggest that implementing an EHR may be an effective way to meet these increasing demands on patient‐centered care.
Limitations to this study should be considered. The ARC Medical Program is primarily used as an education tool for resident physicians, so all of our data are specific to resident physicians. It would be interesting and important to observe if EHRs affect nurse or attending‐patient interactions. Furthermore, we did not have access to any patient demographic or clinical data. However, we did not anticipate a significant change in the patient population that would alter the survey responses during this 6‐month period. Patients were required to recognize their resident on a photo card presented to them by the surveyor, which likely favored patients with strong feelings toward their residents. Due to this, our population sampled may not be indicative of the entire patient population. All findings were simply correlational. Due to the nature of our data collection, we were unable to control for many confounding variables, thus causal conclusions are difficult to draw from these results.
There are a few important trends to note. No question on the ARC survey received lower scores following implementation of the EHR. Furthermore, 9 of the 16 questions under investigation received significantly higher scores following implementation. The residents largely received positive responses both before and after EHR implementation, so despite the statistically significant improvements, the absolute differences are relatively small. These significant differences were likely not due to the residents improving through time and experience. We observed relatively insignificant and nonuniform changes in responses between the two 11‐week periods prior to implementation.
One possible reason for the observed significant improvements is that EHRs may increase patient involvement in the healthcare setting,[28] and this collaboration might improve resident‐patient communication.[29] Providing patients with an interactive tablet that details their care has been suggested to increase patient satisfaction and comfort in an inpatient setting.[30] In this light, the EHR can be used as a tool to increase these interactions by inviting patients to view the computer screen and electronic charts during data entry, which allows them to have a participatory role in their care and decision‐making process.[31] Although the reasons for our observed improvements are unclear, they are noteworthy and warrant further study. The notion that implementing an EHR might enhance provider‐patient communication is a powerful concept.
This study not only suggests the improvement of resident‐patient communication due to the implementation of an EHR, but it also reveals the value of the ARC Medical Program for studying the patient experience. The controlled, prolonged, and efficient nature of the ARC Medical Program's data collection was ideal for comparing a change in resident‐patient communication before and after EHR implementation at UCLA Health. ARC and UCLA Health's EHR can serve as a model for residency programs nationwide. Future studies can assess the changes of the patient‐provider interaction for any significant event, as demonstrated by this study and its investigation of the implementation of UCLA Health's EHR.
Acknowledgements
The authors acknowledge the UCLA Health Office of the Patient Experience and UCLA Health for allowing for this unique partnership with the David Geffen School of Medicine to improve physician‐patient communication. Furthermore, the authors thank the student volunteers and interns of the ARC Medical program for their commitment and effort to optimize the patient experience. Additionally, the authors thank the program directors of the David Geffen School of Medicine residency physician training programs for their outstanding support of the ARC Medical Program.
Disclosures: C.W.M. and A.A.N. contributed equally to this manuscript. C.W.M. and A.A.N. collected data, performed statistical analyses, and drafted and revised the manuscript. A.A.N. and V.N.M. oversaw the program. N.A. provided faculty support and revised the manuscript. The authors report no conflicts of interest.
- , , . Doctor‐patient communication and patient satisfaction: a review. Fam Pract. 1998;15(5):480–492.
- . Patient satisfaction in primary health care: a literature review and analysis. Eval Program Plann. 1983;6:185–210.
- , . The significance of patients' perceptions of physician conduct. J Community Health. 1980;6(1):18–34.
- , , , . Predicting patient satisfaction from physicians' nonverbal communication skills. Med Care. 1980;18(4):376–387.
- , , . Why do people sue doctors? A study of patients and relatives. Lancet. 1994;343:1609–1613.
- , , . Reducing legal risk by practicing patient‐centered medicine. Arch Intern Med. 2002;162(11):1217–1219.
- , . Listening and talking. West J Med. 1993;158:268–272.
- , , . Medical malpractice: the effect of doctor‐patient relations on medical patient perceptions and malpractice intentions. West J Med. 2000;173(4):244–250.
- . Effective physician‐patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–1433.
- , , , , . Patients' participation in medical care: effects on blood sugar control and quality of life in diabetes. J Intern Med. 1988;3:448–457.
- , , . Assessing the effects of physician‐patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 suppl):S110–S127.
- , , . Expanding patient involvement in care. Ann Intern Med. 1985;102:520–528.
- , , , , . Patient exposition and provider explanation in routine interviews and hypertensive patients' blood control. Health Psychol. 1987;6(1):29–42.
- , , . A framework for making patient‐centered care front and center. Perm J. 2012;16(3):49–53.
- . Interoperability: the key to the future health care system. Health Aff. 2005;5(21):19–21.
- , . Physicians' use of electronic medical records: barriers and solutions. Health Aff. 2004;23(2):116–126.
- , . Do hospitals with electronic medical records (EMRs) provide higher quality care?: an examination of three clinical conditions. Med Care Res Rev. 2008;65(4):496–513.
- , , , et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff. 2005;24(5):1103–1117.
- , , , . An electronic medical record in primary care: impact on satisfaction, work efficiency and clinic processes. AMIA Annu Symp.2006:394–398.
- , . Barriers to implement electronic health records (EHRs). Mater Sociomed. 2013;25(3):213–215.
- . Impact of electronic health record systems on information integrity: quality and safety implications. Perspect Health Inf Manag. 2013;10:1c.eCollection 2013.
- , , , , . Electronic medical record use and physician–patient communication: an observational study of Israeli primary care encounters. Patient Educ Couns. 2006;61:134–141.
- , , , et al. EHR implementation in a new clinic: a case study of clinician perceptions. J Med Syst. 2013;37(9955):1–6.
- , , . Accuracy and speed of electronic health record versus paper‐based ophthalmic documentation strategies. Am J Ophthalmol. 2013;156(1):165–172.
- , , . The use of electronic medical records communication patterns in outpatient encounters. J Am Informatics Assoc. 2001:610–616.
- , , . Cost‐benefit analysis of electronic medical record system at a tertiary care hospital. Healthc Inform Res. 2013;19(3):205–214.
- , , , . Promoting patient‐centred care through trainee feedback: assessing residents' C‐I‐CARE (ARC) program. BMJ Qual Saf. 2012;21(3):225–233.
- . Electronic health records?: can we maximize their benefits and minimize their risks? Acad Med. 2012;87(11):1456–1457.
- , . Let the left hand know what the right is doing: a vision for care coordination and electronic health records. J Am Med Inform Assoc. 2014;21(1):13–16.
- , , , et al. A tablet computer application for patients to participate in their hospital care. AMIA Annu Symp Proc. 2011;2011:1428–1435.
- , . Enhancing patient‐centered communication and collaboration by using the electronic health record in the examination room. J Am Med Assoc. 2013;309(22):2327–2328.
Delivering patient‐centered care is at the core of ensuring patient engagement and active participation that will lead to positive outcomes. Physician‐patient interaction has become an area of increasing focus in an effort to optimize the patient experience. Positive patient‐provider communication has been shown to increase satisfaction,[1, 2, 3, 4] decrease the likelihood of medical malpractice lawsuits,[5, 6, 7, 8] and improve clinical outcomes.[9, 10, 11, 12, 13] Specifically, a decrease in psychological symptoms such as anxiety and stress, as well as perception of physical symptoms have been correlated with improved communication.[9, 12] Furthermore, objective health outcomes, such as improvement in hypertension and glycosylated hemoglobin, have also been correlated with improved physician‐patient communication.[10, 11, 13] The multifaceted effects of improved communication are impactful to both the patient and the physician; therefore, it is essential that we understand how to optimize this interaction.
Patient‐centered care is a critical objective for many high‐quality healthcare systems.[14] In recent years, the use of electronic health records (EHRs) has been increasingly adopted by healthcare systems nationally in an effort to improve the quality of care delivered. The positive benefits of EHRs on the facilitation of healthcare, including consolidation of information, reduction of medical errors, easily transferable medical records,[15, 16, 17] as well as their impact on healthcare spending,[18] are well‐documented and have been emphasized as reasons for adoption of EHRs by the Patient Protection and Affordable Care Act. However, EHR implementation has encountered some resistance regarding its impact on the patient experience.
As EHR implementation is exponentially increasing in the United States, there is limited literature on the consequences of this technology.[19] Barriers reported during EHR implementation include the limitations of standardization, attitudinal and organizational constraints, behavior of individuals, and resistance to change.[20] Additionally, poor EHR system design and improper use can cause errors that jeopardize the integrity of the information inputted, leading to inaccuracies that endanger patient safety or decrease the quality of care.[21]
One of the limitations of EHRs has been the reported negative impact on patient‐centered care by decreasing communication during the hospital visit.[22] Although the EHR has enhanced internal provider communication,[23] the literature suggests a lack of focus on the patient sitting in front of the provider. Due to perceived physician distraction during the visit, patients report decreased satisfaction when physicians spend a considerable period of time during the visit at the computer.[22] Furthermore, the average hospital length of stay has been increased due to the use of EHRs.[22]
Although some physicians report that EHR use impedes patient workflow and decreases time spent with patients,[23] previous literature suggests that EHRs decrease the time to develop a synopsis and improve communication efficiency.[19] Some studies have also noted an increase in the ability for medical history retrieval and analysis, which will ultimately increase the quality of care provided to the patient.[24] Physicians who use the EHR adopted a more active role in clarifying information, encouraging questions, and ensuring completeness at the end of a visit.[25] Finally, studies show that the EHR has a positive return on investment from savings in drug expenditures, radiology tests, and billing errors.[26] Given the significant financial and time commitment that health systems and physicians must invest to implement EHRs, it is vital that we understand the multifaceted effects of EHRs on the field of medicine.
METHODS
The purpose of this study was to assess the physician‐patient communication patterns associated with the implementation and use of an EHR in a hospital setting.
ARC Medical Program
In 2006, the Office of Patient Experience at University of California, Los Angeles (UCLA) Health, in conjunction with the David Geffen School of Medicine at UCLA, launched the Assessing Residents' CI‐CARE (ARC) Medical Program. CI‐CARE is a protocol that emphasizes for medical staff and providers to Connect with their patients, Introduce themselves, Communicate their purpose, Ask or anticipate patients' needs, Respond to questions with immediacy, and to Exit courteously. CI‐CARE represents the standards for staff and providers in any encounter with patients or their families. The goals of the ARC Medical Program are to monitor housestaff performance and patient satisfaction while improving trainee education through timely and patient‐centered feedback. The ARC Medical Program's survey has served as an important tool to assess and improve physician professionalism and interpersonal skills and communication, 2 of the Accreditation Council for Graduate Medical Education core competencies.[27]
The ARC program is a unique and innovative volunteer program that provides timely and patient‐centered feedback from trainees' daily encounters with hospitalized patients. The ARC Medical Program has an established infrastructure to conduct evaluations on a system‐wide scale, including 9 departments within UCLA Health. ARC volunteers interview patients using a CI‐CARE Questionnaire (ARC survey) to assess their resident physician's communication patterns. The ARC Survey targets specific areas of the residents' care as outlined by the CI‐CARE Program of UCLA Health.
As part of UCLA Health's mission to ensure the highest level of patient‐centered care, the CI‐CARE standards were introduced in 2006, followed by implementation of the EHR system. Given the lack of previous research and conflicting results on the impact of EHRs on the patient experience, this article uses ARC data to assess whether or not there was a significant difference following implementation of the EHR on March 2, 2013.
The materials and methods of this study are largely based on those of a previous study, also published by the ARC Medical Program.[27]
CI‐CARE QuestionnaireARC Survey
The CI‐CARE Questionnaire is a standardized audit tool consisting of a total of 20 questions used by the facilitators who work with ARC. There are a total of 20 items on the ARC survey, including 18 multiple‐choice, polar, and Likert‐scale questions, and 2 free‐response questions that assess the patients' overall perception of their resident physician and their hospital experience. Questions 1 and 2 pertain to the recognition of attending physicians and resident physicians, respectively. Questions 3, 4, 6, 7, and 8 are Likert‐scalebased questions assessing the residents' professionalism. Questions 9 through 14 are Likert‐scalebased items included to evaluate the quality of communication between patient and provider. We categorized questions 5 and 15 as relating to diagnostics.[27] In 2012, ARC implemented 3 additional questions that assessed residents' communication skills (question 16), level of medical expertise (question 17), and quality of medical care (question 18). We chose to examine the CI‐CARE Questionnaire instead of a standard survey such as the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), because it examines the physician‐patient interaction in more detail. The survey can be reviewed in Figure 1.
Interview Procedure
The ARC Medical Program is comprised of 47 premedical UCLA students who conducted the surveys. New surveyors were trained by the senior surveyors for a minimum of 12 hours before conducting a survey independently. All surveyors were evaluated biyearly by their peers and the program director for quality assurance and to ensure uniform procedures. The volunteers' surveying experience on December 1, 2012 was as follows: (=10 months [237 months], =10 months).
Prior to the interview, the surveyor introduces himself or herself, the purpose and length of the interview, and that the patient's anonymous participation is optional and confidential. Upon receiving verbal consent from the patient, the surveyor presents a picture card to the patient and asks him or her to identify a resident who was on rotation who treated them. If the patient is able to identify the resident who treated them, the surveyor asks each question and records each response verbatim. The surveyors are trained not to probe for responses, and to ensure that the patients answer in accordance with the possible responses. Although it has not been formally studied, the inter‐rater reliability of the survey is likely to be very high due to the verbatim requirements.
Population Interviewed
A total of 3414 surveys were collected from patients seen in the departments of internal medicine, family medicine, pediatrics, general surgery, head and neck surgery, orthopedic surgery, neurosurgery, neurology, and obstetrics and gynecology in this retrospective cohort study. Exclusion criteria included patients who were not awake, were not conscious, could not confidently identify a resident, or stated that they were not able to confidently complete the survey.
Data Analysis
The researchers reviewed and evaluated all data gathered using standard protocols. Statistical comparisons were made using [2] tests. All quantitative analyses were performed in Excel 2010 (Microsoft Corp., Redmond, WA) and SPSS version 21 (IBM Corp., Armonk, NY).
Institutional Review Board
This project received an exemption by the UCLA institutional review board.
RESULTS
There were a total of 3414 interviews conducted and completed from December 1, 2012 to May 30, 2013. Altogether, 1567 surveys were collected 3 months prior to EHR implementation (DecemberFebruary), and 1847 surveys were collected 3 months following implementation (MarchMay). The survey breakdown is summarized in Table 1.
| Department | Pre (N) | Post (N) | Total (N) |
|---|---|---|---|
| |||
| Family medicine | 65 | 128 | 193 |
| General surgery | 226 | 246 | 472 |
| Head and neck surgery | 43 | 65 | 108 |
| Internal medicine | 439 | 369 | 808 |
| Neurology | 81 | 98 | 179 |
| Neurosurgery | 99 | 54 | 153 |
| OB/GYN | 173 | 199 | 372 |
| Orthopedic surgery | 117 | 128 | 245 |
| Pediatrics | 324 | 563 | 887 |
| Totals | 1,567 | 1,850 | 3,417 |
2 analysis revealed that the residents received significantly better feedback in the 3 months following EHR implementation, compared to the 3 months prior to implementation on questions 3, addressing the patient by their preferred name; 4, introducing themselves and their role; 5, communicating what they will do, how long it will take, and how it will impact the patient; 7, responding to the patient's requests and questions with immediacy; 8, listening to the patient's questions and concerns; 9, doing their utmost to ensure the patient receives the best care; 10, communicating well with the patient; 11, being respectful and considerate; and 12, being sensitive to the patient's physical and emotional needs (P<0.05) (Table 2).
| Question | Pre‐EHR % Responses (n=1,567) | Post‐EHR % Responses (n=1,850) | 2 Significance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| ||||||||||||
| 3 | Address you by preferred name? | 90.1 | 3.8 | 2.7 | 3.4 | 91.5 | 3.6 | 1.3 | 3.6 | 0.032* | ||
| 4 | Introduce himself/herself? | 88.3 | 6.4 | 3.2 | 2.1 | 93.1 | 3.6 | 1.8 | 1.5 | 0.000* | ||
| 5 | Communicate what he/she will do? | 83.1 | 9.3 | 4.5 | 3.2 | 86.9 | 6.4 | 3.5 | 3.3 | 0.006* | ||
| 6 | Ask if you have any questions? | 90.9 | 6.2 | 2.9 | 92.4 | 4.9 | 2.7 | 0.230 | ||||
| 7 | Respond with immediacy? | 92.5 | 5.4 | 2.2 | 94.6 | 3.4 | 2.1 | 0.015* | ||||
| 8 | Listens to your questions and concerns? | 94.8 | 4.0 | 1.1 | 96.6 | 2.4 | 1.0 | 0.022* | ||||
| 9 | Ensure you received the best care? | 92.4 | 6.3 | 1.3 | 95.2 | 3.9 | 1.0 | 0.003* | ||||
| 10 | Communicates well with you? | 92.3 | 6.3 | 1.5 | 94.8 | 4.2 | 0.9 | 0.009* | ||||
| 11 | Is respectful and considerate? | 96.5 | 2.7 | 0.8 | 98.0 | 1.6 | 0.4 | 0.025* | ||||
| 12 | Sensitive to your physical and emotional needs? | 90.4 | 6.9 | 2.7 | 94.5 | 3.9 | 1.6 | 0.000* | ||||
| 13 | Uses language that you can understand? | 96.5 | 2.8 | 0.7 | 96.9 | 2.8 | 0.4 | 0.431 | ||||
| 14 | Educated you/family about condition/care? | 84.0 | 8.6 | 7.4 | 86.6 | 7.4 | 6.0 | 0.111 | ||||
| 15 | Exit courteously? | 89.7 | 6.6 | 3.6 | 91.7 | 5.2 | 3.1 | 0.130 | ||||
| 16 | Communication skills? | 75.6 | 19.5 | 3.6 | 0.7 | 0.7 | 78.6 | 16.9 | 3.9 | 0.4 | 0.3 | 0.077 |
| 17 | Medical expertise? | 79.5 | 15.9 | 3.5 | 0.7 | 0.4 | 80.0 | 16.5 | 2.7 | 0.5 | 0.2 | 0.398 |
| 18 | Quality medical care? | 82.5 | 13.0 | 2.8 | 0.8 | 0.9 | 82.6 | 13.6 | 2.7 | 0.7 | 0.5 | 0.754 |
ARC surveyed for 10 weeks prior to our reported sample (OctoberDecember) and 22 weeks prior to EHR implementation total (OctoberMarch). To rule out resident improvement due to the confounding effects of time and experience, we compared the data from the first 11 weeks (OctoberDecember) to the second 11 weeks (DecemberMarch) prior to EHR implementation. [2] analysis revealed that only 6 of the 16 questions showed improvement in this period, and just 1 of these improvements (question 3) was significant. Furthermore, 10 of the 16 questions actually received worse responses in this period, and 2 of these declines (questions 9 and 12) were significant (Table 3).
| Question | First 11 Weeks' Responses (n=897) | Second 11 Weeks' Responses (n=1,338) | 2 Significance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| ||||||||||||
| 3 | Address you by preferred name? | 87.1 | 6.4 | 4.6 | 2.0 | 90.7 | 3.7 | 2.3 | 3.4 | 0.000* | ||
| 4 | Introduce himself/herself? | 87.7 | 6.9 | 4.1 | 1.2 | 88.3 | 6.1 | 3.3 | 2.3 | 0.174 | ||
| 5 | Communicate what he/she will do? | 82.9 | 8.2 | 5.1 | 3.7 | 83.2 | 9.1 | 4.3 | 3.4 | 0.698 | ||
| 6 | Ask if you have any questions? | 92.0 | 5.9 | 2.1 | 90.7 | 6.1 | 3.1 | 0.336 | ||||
| 7 | Respond with immediacy? | 91.2 | 6.6 | 2.2 | 92.8 | 5.2 | 2.1 | 0.353 | ||||
| 8 | Listens to your questions and concerns? | 94.6 | 3.9 | 1.4 | 95.0 | 3.8 | 1.2 | 0.868 | ||||
| 9 | Ensure you received the best care? | 94.4 | 5.0 | 0.6 | 92.1 | 6.5 | 1.4 | 0.049* | ||||
| 10 | Communicates well with you? | 93.3 | 5.9 | 0.8 | 92.4 | 5.9 | 1.7 | 0.167 | ||||
| 11 | Is respectful and considerate? | 97.3 | 2.1 | 0.6 | 96.4 | 2.7 | 0.9 | 0.455 | ||||
| 12 | Sensitive to your physical and emotional needs? | 93.2 | 5.5 | 1.3 | 90.3 | 6.9 | 2.8 | 0.022* | ||||
| 13 | Uses language that you can understand? | 96.2 | 3.5 | 0.3 | 96.4 | 2.8 | 0.7 | 0.327 | ||||
| 14 | Educated you/family about condition/care? | 85.7 | 8.9 | 5.4 | 83.8 | 8.7 | 7.5 | 0.141 | ||||
| 15 | Exit courteously? | 89.7 | 7.8 | 2.5 | 89.6 | 6.6 | 3.8 | 0.124 | ||||
| 16 | Communication skills? | 78.7 | 17.1 | 2.9 | 0.7 | 0.7 | 75.9 | 19 | 3.6 | 0.7 | 0.8 | 0.633 |
| 17 | Medical expertise? | 82.3 | 13.3 | 3.9 | 0.1 | 0.4 | 78.9 | 16.1 | 3.6 | 0.8 | 0.5 | 0.062 |
| 18 | Quality medical care? | 82.7 | 13.5 | 2.6 | 0.8 | 0.4 | 82.1 | 13.0 | 3.0 | 0.9 | 1.0 | 0.456 |
DISCUSSION
The adoption of EHRs has been fueled by their suggested improvement on healthcare quality and spending.[15, 16, 17, 18] Few studies have investigated the patient experience and its relation to EHR implementation. Furthermore, these studies have not yielded consistent results,[19, 20, 21, 22, 23, 25] raising uncertainty about the effects of EHRs on the patient experience. Possible barriers that may contribute to the scarcity of literature include the relatively recent large‐scale implementation of EHRs and a lack of programs in place to collect extensive data on the physician‐patient relationship.
In a field with increasing demands on patient‐centered care, we need to find ways to preserve and foster the patient‐physician relationship. Given that improvements in the delivery of compassionate care can positively impact clinical outcomes, the likelihood of medical malpractice lawsuits, and patient satisfaction,[1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13] the need to improve the patient‐provider relationship is tremendously important. Following EHR implementation, residents were perceived to provide more frequent diagnostics information including the nature, impact, and treatment of conditions. Furthermore, they were perceived to provide significantly better communication quality following implementation, through care monitoring, respectful and sensitive communication, and enhanced patient and family education. Residents were also perceived as being more professional following implementation, as indicated by positive assessments of several interpersonal communication questions. These results suggest that implementing an EHR may be an effective way to meet these increasing demands on patient‐centered care.
Limitations to this study should be considered. The ARC Medical Program is primarily used as an education tool for resident physicians, so all of our data are specific to resident physicians. It would be interesting and important to observe if EHRs affect nurse or attending‐patient interactions. Furthermore, we did not have access to any patient demographic or clinical data. However, we did not anticipate a significant change in the patient population that would alter the survey responses during this 6‐month period. Patients were required to recognize their resident on a photo card presented to them by the surveyor, which likely favored patients with strong feelings toward their residents. Due to this, our population sampled may not be indicative of the entire patient population. All findings were simply correlational. Due to the nature of our data collection, we were unable to control for many confounding variables, thus causal conclusions are difficult to draw from these results.
There are a few important trends to note. No question on the ARC survey received lower scores following implementation of the EHR. Furthermore, 9 of the 16 questions under investigation received significantly higher scores following implementation. The residents largely received positive responses both before and after EHR implementation, so despite the statistically significant improvements, the absolute differences are relatively small. These significant differences were likely not due to the residents improving through time and experience. We observed relatively insignificant and nonuniform changes in responses between the two 11‐week periods prior to implementation.
One possible reason for the observed significant improvements is that EHRs may increase patient involvement in the healthcare setting,[28] and this collaboration might improve resident‐patient communication.[29] Providing patients with an interactive tablet that details their care has been suggested to increase patient satisfaction and comfort in an inpatient setting.[30] In this light, the EHR can be used as a tool to increase these interactions by inviting patients to view the computer screen and electronic charts during data entry, which allows them to have a participatory role in their care and decision‐making process.[31] Although the reasons for our observed improvements are unclear, they are noteworthy and warrant further study. The notion that implementing an EHR might enhance provider‐patient communication is a powerful concept.
This study not only suggests the improvement of resident‐patient communication due to the implementation of an EHR, but it also reveals the value of the ARC Medical Program for studying the patient experience. The controlled, prolonged, and efficient nature of the ARC Medical Program's data collection was ideal for comparing a change in resident‐patient communication before and after EHR implementation at UCLA Health. ARC and UCLA Health's EHR can serve as a model for residency programs nationwide. Future studies can assess the changes of the patient‐provider interaction for any significant event, as demonstrated by this study and its investigation of the implementation of UCLA Health's EHR.
Acknowledgements
The authors acknowledge the UCLA Health Office of the Patient Experience and UCLA Health for allowing for this unique partnership with the David Geffen School of Medicine to improve physician‐patient communication. Furthermore, the authors thank the student volunteers and interns of the ARC Medical program for their commitment and effort to optimize the patient experience. Additionally, the authors thank the program directors of the David Geffen School of Medicine residency physician training programs for their outstanding support of the ARC Medical Program.
Disclosures: C.W.M. and A.A.N. contributed equally to this manuscript. C.W.M. and A.A.N. collected data, performed statistical analyses, and drafted and revised the manuscript. A.A.N. and V.N.M. oversaw the program. N.A. provided faculty support and revised the manuscript. The authors report no conflicts of interest.
Delivering patient‐centered care is at the core of ensuring patient engagement and active participation that will lead to positive outcomes. Physician‐patient interaction has become an area of increasing focus in an effort to optimize the patient experience. Positive patient‐provider communication has been shown to increase satisfaction,[1, 2, 3, 4] decrease the likelihood of medical malpractice lawsuits,[5, 6, 7, 8] and improve clinical outcomes.[9, 10, 11, 12, 13] Specifically, a decrease in psychological symptoms such as anxiety and stress, as well as perception of physical symptoms have been correlated with improved communication.[9, 12] Furthermore, objective health outcomes, such as improvement in hypertension and glycosylated hemoglobin, have also been correlated with improved physician‐patient communication.[10, 11, 13] The multifaceted effects of improved communication are impactful to both the patient and the physician; therefore, it is essential that we understand how to optimize this interaction.
Patient‐centered care is a critical objective for many high‐quality healthcare systems.[14] In recent years, the use of electronic health records (EHRs) has been increasingly adopted by healthcare systems nationally in an effort to improve the quality of care delivered. The positive benefits of EHRs on the facilitation of healthcare, including consolidation of information, reduction of medical errors, easily transferable medical records,[15, 16, 17] as well as their impact on healthcare spending,[18] are well‐documented and have been emphasized as reasons for adoption of EHRs by the Patient Protection and Affordable Care Act. However, EHR implementation has encountered some resistance regarding its impact on the patient experience.
As EHR implementation is exponentially increasing in the United States, there is limited literature on the consequences of this technology.[19] Barriers reported during EHR implementation include the limitations of standardization, attitudinal and organizational constraints, behavior of individuals, and resistance to change.[20] Additionally, poor EHR system design and improper use can cause errors that jeopardize the integrity of the information inputted, leading to inaccuracies that endanger patient safety or decrease the quality of care.[21]
One of the limitations of EHRs has been the reported negative impact on patient‐centered care by decreasing communication during the hospital visit.[22] Although the EHR has enhanced internal provider communication,[23] the literature suggests a lack of focus on the patient sitting in front of the provider. Due to perceived physician distraction during the visit, patients report decreased satisfaction when physicians spend a considerable period of time during the visit at the computer.[22] Furthermore, the average hospital length of stay has been increased due to the use of EHRs.[22]
Although some physicians report that EHR use impedes patient workflow and decreases time spent with patients,[23] previous literature suggests that EHRs decrease the time to develop a synopsis and improve communication efficiency.[19] Some studies have also noted an increase in the ability for medical history retrieval and analysis, which will ultimately increase the quality of care provided to the patient.[24] Physicians who use the EHR adopted a more active role in clarifying information, encouraging questions, and ensuring completeness at the end of a visit.[25] Finally, studies show that the EHR has a positive return on investment from savings in drug expenditures, radiology tests, and billing errors.[26] Given the significant financial and time commitment that health systems and physicians must invest to implement EHRs, it is vital that we understand the multifaceted effects of EHRs on the field of medicine.
METHODS
The purpose of this study was to assess the physician‐patient communication patterns associated with the implementation and use of an EHR in a hospital setting.
ARC Medical Program
In 2006, the Office of Patient Experience at University of California, Los Angeles (UCLA) Health, in conjunction with the David Geffen School of Medicine at UCLA, launched the Assessing Residents' CI‐CARE (ARC) Medical Program. CI‐CARE is a protocol that emphasizes for medical staff and providers to Connect with their patients, Introduce themselves, Communicate their purpose, Ask or anticipate patients' needs, Respond to questions with immediacy, and to Exit courteously. CI‐CARE represents the standards for staff and providers in any encounter with patients or their families. The goals of the ARC Medical Program are to monitor housestaff performance and patient satisfaction while improving trainee education through timely and patient‐centered feedback. The ARC Medical Program's survey has served as an important tool to assess and improve physician professionalism and interpersonal skills and communication, 2 of the Accreditation Council for Graduate Medical Education core competencies.[27]
The ARC program is a unique and innovative volunteer program that provides timely and patient‐centered feedback from trainees' daily encounters with hospitalized patients. The ARC Medical Program has an established infrastructure to conduct evaluations on a system‐wide scale, including 9 departments within UCLA Health. ARC volunteers interview patients using a CI‐CARE Questionnaire (ARC survey) to assess their resident physician's communication patterns. The ARC Survey targets specific areas of the residents' care as outlined by the CI‐CARE Program of UCLA Health.
As part of UCLA Health's mission to ensure the highest level of patient‐centered care, the CI‐CARE standards were introduced in 2006, followed by implementation of the EHR system. Given the lack of previous research and conflicting results on the impact of EHRs on the patient experience, this article uses ARC data to assess whether or not there was a significant difference following implementation of the EHR on March 2, 2013.
The materials and methods of this study are largely based on those of a previous study, also published by the ARC Medical Program.[27]
CI‐CARE QuestionnaireARC Survey
The CI‐CARE Questionnaire is a standardized audit tool consisting of a total of 20 questions used by the facilitators who work with ARC. There are a total of 20 items on the ARC survey, including 18 multiple‐choice, polar, and Likert‐scale questions, and 2 free‐response questions that assess the patients' overall perception of their resident physician and their hospital experience. Questions 1 and 2 pertain to the recognition of attending physicians and resident physicians, respectively. Questions 3, 4, 6, 7, and 8 are Likert‐scalebased questions assessing the residents' professionalism. Questions 9 through 14 are Likert‐scalebased items included to evaluate the quality of communication between patient and provider. We categorized questions 5 and 15 as relating to diagnostics.[27] In 2012, ARC implemented 3 additional questions that assessed residents' communication skills (question 16), level of medical expertise (question 17), and quality of medical care (question 18). We chose to examine the CI‐CARE Questionnaire instead of a standard survey such as the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), because it examines the physician‐patient interaction in more detail. The survey can be reviewed in Figure 1.
Interview Procedure
The ARC Medical Program is comprised of 47 premedical UCLA students who conducted the surveys. New surveyors were trained by the senior surveyors for a minimum of 12 hours before conducting a survey independently. All surveyors were evaluated biyearly by their peers and the program director for quality assurance and to ensure uniform procedures. The volunteers' surveying experience on December 1, 2012 was as follows: (=10 months [237 months], =10 months).
Prior to the interview, the surveyor introduces himself or herself, the purpose and length of the interview, and that the patient's anonymous participation is optional and confidential. Upon receiving verbal consent from the patient, the surveyor presents a picture card to the patient and asks him or her to identify a resident who was on rotation who treated them. If the patient is able to identify the resident who treated them, the surveyor asks each question and records each response verbatim. The surveyors are trained not to probe for responses, and to ensure that the patients answer in accordance with the possible responses. Although it has not been formally studied, the inter‐rater reliability of the survey is likely to be very high due to the verbatim requirements.
Population Interviewed
A total of 3414 surveys were collected from patients seen in the departments of internal medicine, family medicine, pediatrics, general surgery, head and neck surgery, orthopedic surgery, neurosurgery, neurology, and obstetrics and gynecology in this retrospective cohort study. Exclusion criteria included patients who were not awake, were not conscious, could not confidently identify a resident, or stated that they were not able to confidently complete the survey.
Data Analysis
The researchers reviewed and evaluated all data gathered using standard protocols. Statistical comparisons were made using [2] tests. All quantitative analyses were performed in Excel 2010 (Microsoft Corp., Redmond, WA) and SPSS version 21 (IBM Corp., Armonk, NY).
Institutional Review Board
This project received an exemption by the UCLA institutional review board.
RESULTS
There were a total of 3414 interviews conducted and completed from December 1, 2012 to May 30, 2013. Altogether, 1567 surveys were collected 3 months prior to EHR implementation (DecemberFebruary), and 1847 surveys were collected 3 months following implementation (MarchMay). The survey breakdown is summarized in Table 1.
| Department | Pre (N) | Post (N) | Total (N) |
|---|---|---|---|
| |||
| Family medicine | 65 | 128 | 193 |
| General surgery | 226 | 246 | 472 |
| Head and neck surgery | 43 | 65 | 108 |
| Internal medicine | 439 | 369 | 808 |
| Neurology | 81 | 98 | 179 |
| Neurosurgery | 99 | 54 | 153 |
| OB/GYN | 173 | 199 | 372 |
| Orthopedic surgery | 117 | 128 | 245 |
| Pediatrics | 324 | 563 | 887 |
| Totals | 1,567 | 1,850 | 3,417 |
2 analysis revealed that the residents received significantly better feedback in the 3 months following EHR implementation, compared to the 3 months prior to implementation on questions 3, addressing the patient by their preferred name; 4, introducing themselves and their role; 5, communicating what they will do, how long it will take, and how it will impact the patient; 7, responding to the patient's requests and questions with immediacy; 8, listening to the patient's questions and concerns; 9, doing their utmost to ensure the patient receives the best care; 10, communicating well with the patient; 11, being respectful and considerate; and 12, being sensitive to the patient's physical and emotional needs (P<0.05) (Table 2).
| Question | Pre‐EHR % Responses (n=1,567) | Post‐EHR % Responses (n=1,850) | 2 Significance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| ||||||||||||
| 3 | Address you by preferred name? | 90.1 | 3.8 | 2.7 | 3.4 | 91.5 | 3.6 | 1.3 | 3.6 | 0.032* | ||
| 4 | Introduce himself/herself? | 88.3 | 6.4 | 3.2 | 2.1 | 93.1 | 3.6 | 1.8 | 1.5 | 0.000* | ||
| 5 | Communicate what he/she will do? | 83.1 | 9.3 | 4.5 | 3.2 | 86.9 | 6.4 | 3.5 | 3.3 | 0.006* | ||
| 6 | Ask if you have any questions? | 90.9 | 6.2 | 2.9 | 92.4 | 4.9 | 2.7 | 0.230 | ||||
| 7 | Respond with immediacy? | 92.5 | 5.4 | 2.2 | 94.6 | 3.4 | 2.1 | 0.015* | ||||
| 8 | Listens to your questions and concerns? | 94.8 | 4.0 | 1.1 | 96.6 | 2.4 | 1.0 | 0.022* | ||||
| 9 | Ensure you received the best care? | 92.4 | 6.3 | 1.3 | 95.2 | 3.9 | 1.0 | 0.003* | ||||
| 10 | Communicates well with you? | 92.3 | 6.3 | 1.5 | 94.8 | 4.2 | 0.9 | 0.009* | ||||
| 11 | Is respectful and considerate? | 96.5 | 2.7 | 0.8 | 98.0 | 1.6 | 0.4 | 0.025* | ||||
| 12 | Sensitive to your physical and emotional needs? | 90.4 | 6.9 | 2.7 | 94.5 | 3.9 | 1.6 | 0.000* | ||||
| 13 | Uses language that you can understand? | 96.5 | 2.8 | 0.7 | 96.9 | 2.8 | 0.4 | 0.431 | ||||
| 14 | Educated you/family about condition/care? | 84.0 | 8.6 | 7.4 | 86.6 | 7.4 | 6.0 | 0.111 | ||||
| 15 | Exit courteously? | 89.7 | 6.6 | 3.6 | 91.7 | 5.2 | 3.1 | 0.130 | ||||
| 16 | Communication skills? | 75.6 | 19.5 | 3.6 | 0.7 | 0.7 | 78.6 | 16.9 | 3.9 | 0.4 | 0.3 | 0.077 |
| 17 | Medical expertise? | 79.5 | 15.9 | 3.5 | 0.7 | 0.4 | 80.0 | 16.5 | 2.7 | 0.5 | 0.2 | 0.398 |
| 18 | Quality medical care? | 82.5 | 13.0 | 2.8 | 0.8 | 0.9 | 82.6 | 13.6 | 2.7 | 0.7 | 0.5 | 0.754 |
ARC surveyed for 10 weeks prior to our reported sample (OctoberDecember) and 22 weeks prior to EHR implementation total (OctoberMarch). To rule out resident improvement due to the confounding effects of time and experience, we compared the data from the first 11 weeks (OctoberDecember) to the second 11 weeks (DecemberMarch) prior to EHR implementation. [2] analysis revealed that only 6 of the 16 questions showed improvement in this period, and just 1 of these improvements (question 3) was significant. Furthermore, 10 of the 16 questions actually received worse responses in this period, and 2 of these declines (questions 9 and 12) were significant (Table 3).
| Question | First 11 Weeks' Responses (n=897) | Second 11 Weeks' Responses (n=1,338) | 2 Significance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| ||||||||||||
| 3 | Address you by preferred name? | 87.1 | 6.4 | 4.6 | 2.0 | 90.7 | 3.7 | 2.3 | 3.4 | 0.000* | ||
| 4 | Introduce himself/herself? | 87.7 | 6.9 | 4.1 | 1.2 | 88.3 | 6.1 | 3.3 | 2.3 | 0.174 | ||
| 5 | Communicate what he/she will do? | 82.9 | 8.2 | 5.1 | 3.7 | 83.2 | 9.1 | 4.3 | 3.4 | 0.698 | ||
| 6 | Ask if you have any questions? | 92.0 | 5.9 | 2.1 | 90.7 | 6.1 | 3.1 | 0.336 | ||||
| 7 | Respond with immediacy? | 91.2 | 6.6 | 2.2 | 92.8 | 5.2 | 2.1 | 0.353 | ||||
| 8 | Listens to your questions and concerns? | 94.6 | 3.9 | 1.4 | 95.0 | 3.8 | 1.2 | 0.868 | ||||
| 9 | Ensure you received the best care? | 94.4 | 5.0 | 0.6 | 92.1 | 6.5 | 1.4 | 0.049* | ||||
| 10 | Communicates well with you? | 93.3 | 5.9 | 0.8 | 92.4 | 5.9 | 1.7 | 0.167 | ||||
| 11 | Is respectful and considerate? | 97.3 | 2.1 | 0.6 | 96.4 | 2.7 | 0.9 | 0.455 | ||||
| 12 | Sensitive to your physical and emotional needs? | 93.2 | 5.5 | 1.3 | 90.3 | 6.9 | 2.8 | 0.022* | ||||
| 13 | Uses language that you can understand? | 96.2 | 3.5 | 0.3 | 96.4 | 2.8 | 0.7 | 0.327 | ||||
| 14 | Educated you/family about condition/care? | 85.7 | 8.9 | 5.4 | 83.8 | 8.7 | 7.5 | 0.141 | ||||
| 15 | Exit courteously? | 89.7 | 7.8 | 2.5 | 89.6 | 6.6 | 3.8 | 0.124 | ||||
| 16 | Communication skills? | 78.7 | 17.1 | 2.9 | 0.7 | 0.7 | 75.9 | 19 | 3.6 | 0.7 | 0.8 | 0.633 |
| 17 | Medical expertise? | 82.3 | 13.3 | 3.9 | 0.1 | 0.4 | 78.9 | 16.1 | 3.6 | 0.8 | 0.5 | 0.062 |
| 18 | Quality medical care? | 82.7 | 13.5 | 2.6 | 0.8 | 0.4 | 82.1 | 13.0 | 3.0 | 0.9 | 1.0 | 0.456 |
DISCUSSION
The adoption of EHRs has been fueled by their suggested improvement on healthcare quality and spending.[15, 16, 17, 18] Few studies have investigated the patient experience and its relation to EHR implementation. Furthermore, these studies have not yielded consistent results,[19, 20, 21, 22, 23, 25] raising uncertainty about the effects of EHRs on the patient experience. Possible barriers that may contribute to the scarcity of literature include the relatively recent large‐scale implementation of EHRs and a lack of programs in place to collect extensive data on the physician‐patient relationship.
In a field with increasing demands on patient‐centered care, we need to find ways to preserve and foster the patient‐physician relationship. Given that improvements in the delivery of compassionate care can positively impact clinical outcomes, the likelihood of medical malpractice lawsuits, and patient satisfaction,[1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13] the need to improve the patient‐provider relationship is tremendously important. Following EHR implementation, residents were perceived to provide more frequent diagnostics information including the nature, impact, and treatment of conditions. Furthermore, they were perceived to provide significantly better communication quality following implementation, through care monitoring, respectful and sensitive communication, and enhanced patient and family education. Residents were also perceived as being more professional following implementation, as indicated by positive assessments of several interpersonal communication questions. These results suggest that implementing an EHR may be an effective way to meet these increasing demands on patient‐centered care.
Limitations to this study should be considered. The ARC Medical Program is primarily used as an education tool for resident physicians, so all of our data are specific to resident physicians. It would be interesting and important to observe if EHRs affect nurse or attending‐patient interactions. Furthermore, we did not have access to any patient demographic or clinical data. However, we did not anticipate a significant change in the patient population that would alter the survey responses during this 6‐month period. Patients were required to recognize their resident on a photo card presented to them by the surveyor, which likely favored patients with strong feelings toward their residents. Due to this, our population sampled may not be indicative of the entire patient population. All findings were simply correlational. Due to the nature of our data collection, we were unable to control for many confounding variables, thus causal conclusions are difficult to draw from these results.
There are a few important trends to note. No question on the ARC survey received lower scores following implementation of the EHR. Furthermore, 9 of the 16 questions under investigation received significantly higher scores following implementation. The residents largely received positive responses both before and after EHR implementation, so despite the statistically significant improvements, the absolute differences are relatively small. These significant differences were likely not due to the residents improving through time and experience. We observed relatively insignificant and nonuniform changes in responses between the two 11‐week periods prior to implementation.
One possible reason for the observed significant improvements is that EHRs may increase patient involvement in the healthcare setting,[28] and this collaboration might improve resident‐patient communication.[29] Providing patients with an interactive tablet that details their care has been suggested to increase patient satisfaction and comfort in an inpatient setting.[30] In this light, the EHR can be used as a tool to increase these interactions by inviting patients to view the computer screen and electronic charts during data entry, which allows them to have a participatory role in their care and decision‐making process.[31] Although the reasons for our observed improvements are unclear, they are noteworthy and warrant further study. The notion that implementing an EHR might enhance provider‐patient communication is a powerful concept.
This study not only suggests the improvement of resident‐patient communication due to the implementation of an EHR, but it also reveals the value of the ARC Medical Program for studying the patient experience. The controlled, prolonged, and efficient nature of the ARC Medical Program's data collection was ideal for comparing a change in resident‐patient communication before and after EHR implementation at UCLA Health. ARC and UCLA Health's EHR can serve as a model for residency programs nationwide. Future studies can assess the changes of the patient‐provider interaction for any significant event, as demonstrated by this study and its investigation of the implementation of UCLA Health's EHR.
Acknowledgements
The authors acknowledge the UCLA Health Office of the Patient Experience and UCLA Health for allowing for this unique partnership with the David Geffen School of Medicine to improve physician‐patient communication. Furthermore, the authors thank the student volunteers and interns of the ARC Medical program for their commitment and effort to optimize the patient experience. Additionally, the authors thank the program directors of the David Geffen School of Medicine residency physician training programs for their outstanding support of the ARC Medical Program.
Disclosures: C.W.M. and A.A.N. contributed equally to this manuscript. C.W.M. and A.A.N. collected data, performed statistical analyses, and drafted and revised the manuscript. A.A.N. and V.N.M. oversaw the program. N.A. provided faculty support and revised the manuscript. The authors report no conflicts of interest.
- , , . Doctor‐patient communication and patient satisfaction: a review. Fam Pract. 1998;15(5):480–492.
- . Patient satisfaction in primary health care: a literature review and analysis. Eval Program Plann. 1983;6:185–210.
- , . The significance of patients' perceptions of physician conduct. J Community Health. 1980;6(1):18–34.
- , , , . Predicting patient satisfaction from physicians' nonverbal communication skills. Med Care. 1980;18(4):376–387.
- , , . Why do people sue doctors? A study of patients and relatives. Lancet. 1994;343:1609–1613.
- , , . Reducing legal risk by practicing patient‐centered medicine. Arch Intern Med. 2002;162(11):1217–1219.
- , . Listening and talking. West J Med. 1993;158:268–272.
- , , . Medical malpractice: the effect of doctor‐patient relations on medical patient perceptions and malpractice intentions. West J Med. 2000;173(4):244–250.
- . Effective physician‐patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–1433.
- , , , , . Patients' participation in medical care: effects on blood sugar control and quality of life in diabetes. J Intern Med. 1988;3:448–457.
- , , . Assessing the effects of physician‐patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 suppl):S110–S127.
- , , . Expanding patient involvement in care. Ann Intern Med. 1985;102:520–528.
- , , , , . Patient exposition and provider explanation in routine interviews and hypertensive patients' blood control. Health Psychol. 1987;6(1):29–42.
- , , . A framework for making patient‐centered care front and center. Perm J. 2012;16(3):49–53.
- . Interoperability: the key to the future health care system. Health Aff. 2005;5(21):19–21.
- , . Physicians' use of electronic medical records: barriers and solutions. Health Aff. 2004;23(2):116–126.
- , . Do hospitals with electronic medical records (EMRs) provide higher quality care?: an examination of three clinical conditions. Med Care Res Rev. 2008;65(4):496–513.
- , , , et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff. 2005;24(5):1103–1117.
- , , , . An electronic medical record in primary care: impact on satisfaction, work efficiency and clinic processes. AMIA Annu Symp.2006:394–398.
- , . Barriers to implement electronic health records (EHRs). Mater Sociomed. 2013;25(3):213–215.
- . Impact of electronic health record systems on information integrity: quality and safety implications. Perspect Health Inf Manag. 2013;10:1c.eCollection 2013.
- , , , , . Electronic medical record use and physician–patient communication: an observational study of Israeli primary care encounters. Patient Educ Couns. 2006;61:134–141.
- , , , et al. EHR implementation in a new clinic: a case study of clinician perceptions. J Med Syst. 2013;37(9955):1–6.
- , , . Accuracy and speed of electronic health record versus paper‐based ophthalmic documentation strategies. Am J Ophthalmol. 2013;156(1):165–172.
- , , . The use of electronic medical records communication patterns in outpatient encounters. J Am Informatics Assoc. 2001:610–616.
- , , . Cost‐benefit analysis of electronic medical record system at a tertiary care hospital. Healthc Inform Res. 2013;19(3):205–214.
- , , , . Promoting patient‐centred care through trainee feedback: assessing residents' C‐I‐CARE (ARC) program. BMJ Qual Saf. 2012;21(3):225–233.
- . Electronic health records?: can we maximize their benefits and minimize their risks? Acad Med. 2012;87(11):1456–1457.
- , . Let the left hand know what the right is doing: a vision for care coordination and electronic health records. J Am Med Inform Assoc. 2014;21(1):13–16.
- , , , et al. A tablet computer application for patients to participate in their hospital care. AMIA Annu Symp Proc. 2011;2011:1428–1435.
- , . Enhancing patient‐centered communication and collaboration by using the electronic health record in the examination room. J Am Med Assoc. 2013;309(22):2327–2328.
- , , . Doctor‐patient communication and patient satisfaction: a review. Fam Pract. 1998;15(5):480–492.
- . Patient satisfaction in primary health care: a literature review and analysis. Eval Program Plann. 1983;6:185–210.
- , . The significance of patients' perceptions of physician conduct. J Community Health. 1980;6(1):18–34.
- , , , . Predicting patient satisfaction from physicians' nonverbal communication skills. Med Care. 1980;18(4):376–387.
- , , . Why do people sue doctors? A study of patients and relatives. Lancet. 1994;343:1609–1613.
- , , . Reducing legal risk by practicing patient‐centered medicine. Arch Intern Med. 2002;162(11):1217–1219.
- , . Listening and talking. West J Med. 1993;158:268–272.
- , , . Medical malpractice: the effect of doctor‐patient relations on medical patient perceptions and malpractice intentions. West J Med. 2000;173(4):244–250.
- . Effective physician‐patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–1433.
- , , , , . Patients' participation in medical care: effects on blood sugar control and quality of life in diabetes. J Intern Med. 1988;3:448–457.
- , , . Assessing the effects of physician‐patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 suppl):S110–S127.
- , , . Expanding patient involvement in care. Ann Intern Med. 1985;102:520–528.
- , , , , . Patient exposition and provider explanation in routine interviews and hypertensive patients' blood control. Health Psychol. 1987;6(1):29–42.
- , , . A framework for making patient‐centered care front and center. Perm J. 2012;16(3):49–53.
- . Interoperability: the key to the future health care system. Health Aff. 2005;5(21):19–21.
- , . Physicians' use of electronic medical records: barriers and solutions. Health Aff. 2004;23(2):116–126.
- , . Do hospitals with electronic medical records (EMRs) provide higher quality care?: an examination of three clinical conditions. Med Care Res Rev. 2008;65(4):496–513.
- , , , et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff. 2005;24(5):1103–1117.
- , , , . An electronic medical record in primary care: impact on satisfaction, work efficiency and clinic processes. AMIA Annu Symp.2006:394–398.
- , . Barriers to implement electronic health records (EHRs). Mater Sociomed. 2013;25(3):213–215.
- . Impact of electronic health record systems on information integrity: quality and safety implications. Perspect Health Inf Manag. 2013;10:1c.eCollection 2013.
- , , , , . Electronic medical record use and physician–patient communication: an observational study of Israeli primary care encounters. Patient Educ Couns. 2006;61:134–141.
- , , , et al. EHR implementation in a new clinic: a case study of clinician perceptions. J Med Syst. 2013;37(9955):1–6.
- , , . Accuracy and speed of electronic health record versus paper‐based ophthalmic documentation strategies. Am J Ophthalmol. 2013;156(1):165–172.
- , , . The use of electronic medical records communication patterns in outpatient encounters. J Am Informatics Assoc. 2001:610–616.
- , , . Cost‐benefit analysis of electronic medical record system at a tertiary care hospital. Healthc Inform Res. 2013;19(3):205–214.
- , , , . Promoting patient‐centred care through trainee feedback: assessing residents' C‐I‐CARE (ARC) program. BMJ Qual Saf. 2012;21(3):225–233.
- . Electronic health records?: can we maximize their benefits and minimize their risks? Acad Med. 2012;87(11):1456–1457.
- , . Let the left hand know what the right is doing: a vision for care coordination and electronic health records. J Am Med Inform Assoc. 2014;21(1):13–16.
- , , , et al. A tablet computer application for patients to participate in their hospital care. AMIA Annu Symp Proc. 2011;2011:1428–1435.
- , . Enhancing patient‐centered communication and collaboration by using the electronic health record in the examination room. J Am Med Assoc. 2013;309(22):2327–2328.
© 2014 Society of Hospital Medicine