User login
SAN DIEGO – Elevated leptin may play a role in the relationship between excess adiposity and depressive symptoms in older adults, judging from the results of a cross-sectional survey.
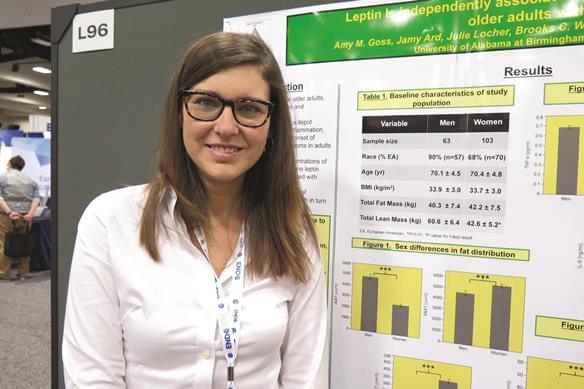
While depression is common among older adults, particularly among those who are obese, “what’s not known is the underlying physiological mechanisms of what’s linking depression with excess fat mass,” Amy M. Goss, Ph.D., a postdoctoral research fellow in the department of nutrition sciences at the University of Alabama at Birmingham, said in an interview at the meeting of the Endocrine Society. “There’s a lot of work showing that visceral fat in particular is linked to depression. It’s thought that inflammation that emanates from visceral fat can lead to depressive symptoms. This is a particular problem in older adults, because they tend to have a lot of visceral adiposity.”
In an effort to investigate the independent relationships among depressive symptoms, total fat mass, intra-abdominal adipose tissue, markers of inflammation, and leptin in aging men and women, Dr. Goss and her associates evaluated 164 obese adults older than 65 years. The researchers used the Center for Epidemiologic Studies Depression (CES-D) 20-item scale to assess depressive symptoms, DXA to assess body composition, MRI to assess fat distribution, and a fasting blood sample to assess leptin, high-sensitivity C-reactive protein (hsCRP), interleukin-6, and tumor necrosis factor–alpha.
Compared with men, women had significantly greater levels of leptin (+100%; P less than .001), hsCRP (+63.9%; P less than .01), and CES-D scores (+52.7%; P less than .001). At the same time, men had significantly greater intra-abdominal adipose tissue (+82%; P less than .001) and lean mass (+42%; P less than .001), compared with women.
Multiple linear regression analysis revealed that only leptin was positively associated with CES-D scores, independent of gender and of all other markers studied (P less than .05).
In their abstract, the researchers concluded that elevated leptin “may, in part, mediate the observed relationship between excess adiposity and onset of depressive symptoms in aging, obese adults. Higher leptin and hsCRP concentration in women, compared to men may indicate greater proinflammatory state and explain sex differences in depressive symptoms in this population.”
Dr. Goss said that a key limitation of the study is its cross-sectional design. “We can’t determine the cause and effect based on this study, but it does lead the way to design randomized, clinical trials to test how we can improve depression in older adults with obesity,” she said.
She reported having no relevant financial conflicts.
On Twitter @dougbrunk
SAN DIEGO – Elevated leptin may play a role in the relationship between excess adiposity and depressive symptoms in older adults, judging from the results of a cross-sectional survey.
While depression is common among older adults, particularly among those who are obese, “what’s not known is the underlying physiological mechanisms of what’s linking depression with excess fat mass,” Amy M. Goss, Ph.D., a postdoctoral research fellow in the department of nutrition sciences at the University of Alabama at Birmingham, said in an interview at the meeting of the Endocrine Society. “There’s a lot of work showing that visceral fat in particular is linked to depression. It’s thought that inflammation that emanates from visceral fat can lead to depressive symptoms. This is a particular problem in older adults, because they tend to have a lot of visceral adiposity.”
In an effort to investigate the independent relationships among depressive symptoms, total fat mass, intra-abdominal adipose tissue, markers of inflammation, and leptin in aging men and women, Dr. Goss and her associates evaluated 164 obese adults older than 65 years. The researchers used the Center for Epidemiologic Studies Depression (CES-D) 20-item scale to assess depressive symptoms, DXA to assess body composition, MRI to assess fat distribution, and a fasting blood sample to assess leptin, high-sensitivity C-reactive protein (hsCRP), interleukin-6, and tumor necrosis factor–alpha.
Compared with men, women had significantly greater levels of leptin (+100%; P less than .001), hsCRP (+63.9%; P less than .01), and CES-D scores (+52.7%; P less than .001). At the same time, men had significantly greater intra-abdominal adipose tissue (+82%; P less than .001) and lean mass (+42%; P less than .001), compared with women.
Multiple linear regression analysis revealed that only leptin was positively associated with CES-D scores, independent of gender and of all other markers studied (P less than .05).
In their abstract, the researchers concluded that elevated leptin “may, in part, mediate the observed relationship between excess adiposity and onset of depressive symptoms in aging, obese adults. Higher leptin and hsCRP concentration in women, compared to men may indicate greater proinflammatory state and explain sex differences in depressive symptoms in this population.”
Dr. Goss said that a key limitation of the study is its cross-sectional design. “We can’t determine the cause and effect based on this study, but it does lead the way to design randomized, clinical trials to test how we can improve depression in older adults with obesity,” she said.
She reported having no relevant financial conflicts.
On Twitter @dougbrunk
SAN DIEGO – Elevated leptin may play a role in the relationship between excess adiposity and depressive symptoms in older adults, judging from the results of a cross-sectional survey.
While depression is common among older adults, particularly among those who are obese, “what’s not known is the underlying physiological mechanisms of what’s linking depression with excess fat mass,” Amy M. Goss, Ph.D., a postdoctoral research fellow in the department of nutrition sciences at the University of Alabama at Birmingham, said in an interview at the meeting of the Endocrine Society. “There’s a lot of work showing that visceral fat in particular is linked to depression. It’s thought that inflammation that emanates from visceral fat can lead to depressive symptoms. This is a particular problem in older adults, because they tend to have a lot of visceral adiposity.”
In an effort to investigate the independent relationships among depressive symptoms, total fat mass, intra-abdominal adipose tissue, markers of inflammation, and leptin in aging men and women, Dr. Goss and her associates evaluated 164 obese adults older than 65 years. The researchers used the Center for Epidemiologic Studies Depression (CES-D) 20-item scale to assess depressive symptoms, DXA to assess body composition, MRI to assess fat distribution, and a fasting blood sample to assess leptin, high-sensitivity C-reactive protein (hsCRP), interleukin-6, and tumor necrosis factor–alpha.
Compared with men, women had significantly greater levels of leptin (+100%; P less than .001), hsCRP (+63.9%; P less than .01), and CES-D scores (+52.7%; P less than .001). At the same time, men had significantly greater intra-abdominal adipose tissue (+82%; P less than .001) and lean mass (+42%; P less than .001), compared with women.
Multiple linear regression analysis revealed that only leptin was positively associated with CES-D scores, independent of gender and of all other markers studied (P less than .05).
In their abstract, the researchers concluded that elevated leptin “may, in part, mediate the observed relationship between excess adiposity and onset of depressive symptoms in aging, obese adults. Higher leptin and hsCRP concentration in women, compared to men may indicate greater proinflammatory state and explain sex differences in depressive symptoms in this population.”
Dr. Goss said that a key limitation of the study is its cross-sectional design. “We can’t determine the cause and effect based on this study, but it does lead the way to design randomized, clinical trials to test how we can improve depression in older adults with obesity,” she said.
She reported having no relevant financial conflicts.
On Twitter @dougbrunk
AT ENDO 2015
Key clinical point: Leptin may play a role in the onset of depressive symptoms in aging, obese adults.
Major finding: Only leptin was positively associated with Center for Epidemiologic Studies Depression (CES-D) scores, independent of gender and of all other markers studied (P less than .05).
Data source: A cross-sectional study of 164 obese adults over the age of 65 years.
Disclosures: Dr. Goss reported having no relevant financial conflicts.