User login

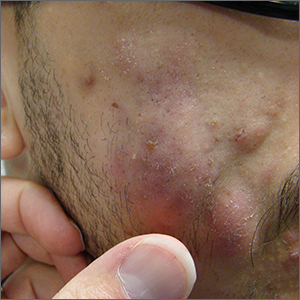
This patient had more than cystic acne; he had acne conglobata. AC is a severe form of inflammatory acne leading to coalescing lesions with purulent sinus tracts under the skin. It can be seen as part of the follicular tetrad syndrome of cystic acne, hidradenitis suppurativa, dissecting cellulitis, and pilonidal disease. AC is thought to be an elevated tumor necrosis factor (TNF)-alpha response to Propionibacterium acnes (now known as Cutibacterium acnes) that leads to excessive inflammation and sterile abscesses.1 Acne fulminans (AF) can also manifest as a purulent form of acne, but AF has associated systemic signs and symptoms that include fevers, chills, and malaise.
Due to the depth of the inflammation, AC is treated with systemic medications, most commonly isotretinoin. Isotretinoin can be started at 0.5 mg/kg (divided twice daily to enhance tolerability) and then increased to 1 mg/kg (divided twice daily) for 5 months. There is some variation in dosing regimens in practice; the target goal is 120 to 150 mg/kg over the course of treatment. In AF, the patient is pretreated with systemic steroids, and in AC, some clinicians will even prescribe systemic steroids (prednisone 0.5 mg/kg daily for the first month) along with isotretinoin.
Second-line medications include dapsone (50-150 mg/d).2 Case reports describe the successful use of the TNF-alpha antagonist adalimumab, although this is not a usual practice in AC treatment.1 Note that all of these medications have the potential for severe adverse effects and require laboratory evaluation prior to initiation.
This patient was counseled, prescribed isotretinoin (dose as above), and enrolled in the IPledge prescribing and monitoring system for isotretinoin. At 20 weeks of use, the purulent drainage ceased. The pus-filled sinus tracts and redness had resolved, although he still had thickened tissue and scarring where the tracts had been. In time, the scars will usually get flatter and softer.
If the patient’s AC were to flare, another 20-week course of isotretinoin could be prescribed after a 2-month hiatus or he could be switched to a second-line medication. Referral for any cosmetic therapy is typically delayed for another 6 months in case there is a need to treat a recurrence.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.
1. Yiu ZZ, Madan V, Griffiths CE. Acne conglobata and adalimumab: use of tumour necrosis factor-α antagonists in treatment-resistant acne conglobata, and review of the literature. Clin Exp Dermatol. 2015;40:383-386. doi: 10.1111/ced.12540
2. Hafsi W, Arnold DL, Kassardjian M. Acne Conglobata. StatPearls Publishing; 2023.

This patient had more than cystic acne; he had acne conglobata. AC is a severe form of inflammatory acne leading to coalescing lesions with purulent sinus tracts under the skin. It can be seen as part of the follicular tetrad syndrome of cystic acne, hidradenitis suppurativa, dissecting cellulitis, and pilonidal disease. AC is thought to be an elevated tumor necrosis factor (TNF)-alpha response to Propionibacterium acnes (now known as Cutibacterium acnes) that leads to excessive inflammation and sterile abscesses.1 Acne fulminans (AF) can also manifest as a purulent form of acne, but AF has associated systemic signs and symptoms that include fevers, chills, and malaise.
Due to the depth of the inflammation, AC is treated with systemic medications, most commonly isotretinoin. Isotretinoin can be started at 0.5 mg/kg (divided twice daily to enhance tolerability) and then increased to 1 mg/kg (divided twice daily) for 5 months. There is some variation in dosing regimens in practice; the target goal is 120 to 150 mg/kg over the course of treatment. In AF, the patient is pretreated with systemic steroids, and in AC, some clinicians will even prescribe systemic steroids (prednisone 0.5 mg/kg daily for the first month) along with isotretinoin.
Second-line medications include dapsone (50-150 mg/d).2 Case reports describe the successful use of the TNF-alpha antagonist adalimumab, although this is not a usual practice in AC treatment.1 Note that all of these medications have the potential for severe adverse effects and require laboratory evaluation prior to initiation.
This patient was counseled, prescribed isotretinoin (dose as above), and enrolled in the IPledge prescribing and monitoring system for isotretinoin. At 20 weeks of use, the purulent drainage ceased. The pus-filled sinus tracts and redness had resolved, although he still had thickened tissue and scarring where the tracts had been. In time, the scars will usually get flatter and softer.
If the patient’s AC were to flare, another 20-week course of isotretinoin could be prescribed after a 2-month hiatus or he could be switched to a second-line medication. Referral for any cosmetic therapy is typically delayed for another 6 months in case there is a need to treat a recurrence.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.

This patient had more than cystic acne; he had acne conglobata. AC is a severe form of inflammatory acne leading to coalescing lesions with purulent sinus tracts under the skin. It can be seen as part of the follicular tetrad syndrome of cystic acne, hidradenitis suppurativa, dissecting cellulitis, and pilonidal disease. AC is thought to be an elevated tumor necrosis factor (TNF)-alpha response to Propionibacterium acnes (now known as Cutibacterium acnes) that leads to excessive inflammation and sterile abscesses.1 Acne fulminans (AF) can also manifest as a purulent form of acne, but AF has associated systemic signs and symptoms that include fevers, chills, and malaise.
Due to the depth of the inflammation, AC is treated with systemic medications, most commonly isotretinoin. Isotretinoin can be started at 0.5 mg/kg (divided twice daily to enhance tolerability) and then increased to 1 mg/kg (divided twice daily) for 5 months. There is some variation in dosing regimens in practice; the target goal is 120 to 150 mg/kg over the course of treatment. In AF, the patient is pretreated with systemic steroids, and in AC, some clinicians will even prescribe systemic steroids (prednisone 0.5 mg/kg daily for the first month) along with isotretinoin.
Second-line medications include dapsone (50-150 mg/d).2 Case reports describe the successful use of the TNF-alpha antagonist adalimumab, although this is not a usual practice in AC treatment.1 Note that all of these medications have the potential for severe adverse effects and require laboratory evaluation prior to initiation.
This patient was counseled, prescribed isotretinoin (dose as above), and enrolled in the IPledge prescribing and monitoring system for isotretinoin. At 20 weeks of use, the purulent drainage ceased. The pus-filled sinus tracts and redness had resolved, although he still had thickened tissue and scarring where the tracts had been. In time, the scars will usually get flatter and softer.
If the patient’s AC were to flare, another 20-week course of isotretinoin could be prescribed after a 2-month hiatus or he could be switched to a second-line medication. Referral for any cosmetic therapy is typically delayed for another 6 months in case there is a need to treat a recurrence.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.
1. Yiu ZZ, Madan V, Griffiths CE. Acne conglobata and adalimumab: use of tumour necrosis factor-α antagonists in treatment-resistant acne conglobata, and review of the literature. Clin Exp Dermatol. 2015;40:383-386. doi: 10.1111/ced.12540
2. Hafsi W, Arnold DL, Kassardjian M. Acne Conglobata. StatPearls Publishing; 2023.
1. Yiu ZZ, Madan V, Griffiths CE. Acne conglobata and adalimumab: use of tumour necrosis factor-α antagonists in treatment-resistant acne conglobata, and review of the literature. Clin Exp Dermatol. 2015;40:383-386. doi: 10.1111/ced.12540
2. Hafsi W, Arnold DL, Kassardjian M. Acne Conglobata. StatPearls Publishing; 2023.