User login
A frontline treatment regimen including brentuximab vedotin (Bv) was well tolerated, was highly effective, and significantly reduced radiation exposure in pediatric patients with high-risk Hodgkin lymphoma, according to the results of an open-label, phase 2 trial.
Of 77 patients enrolled in the investigator-initiated, single-arm, multicenter trial, 27 (35%) achieved complete remission (CR) without radiation at the early response assessment (ERA) after two cycles of therapy, reported Monika L. Metzger, MD, of St. Jude Children’s Research Hospital, Memphis, Tenn. and colleagues. The report was published online in the Journal of Clinical Oncology.
The addition of Bv also resulted in superior event-free survival (97.4%) and overall survival (98.7%) at median follow-up of 3.4 years, compared with previously published pediatric trials, such as the HOD99 trial (EFS and OS of 80.8% and 96.5%, respectively), the authors noted.
Bv chemotherapy
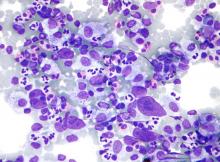
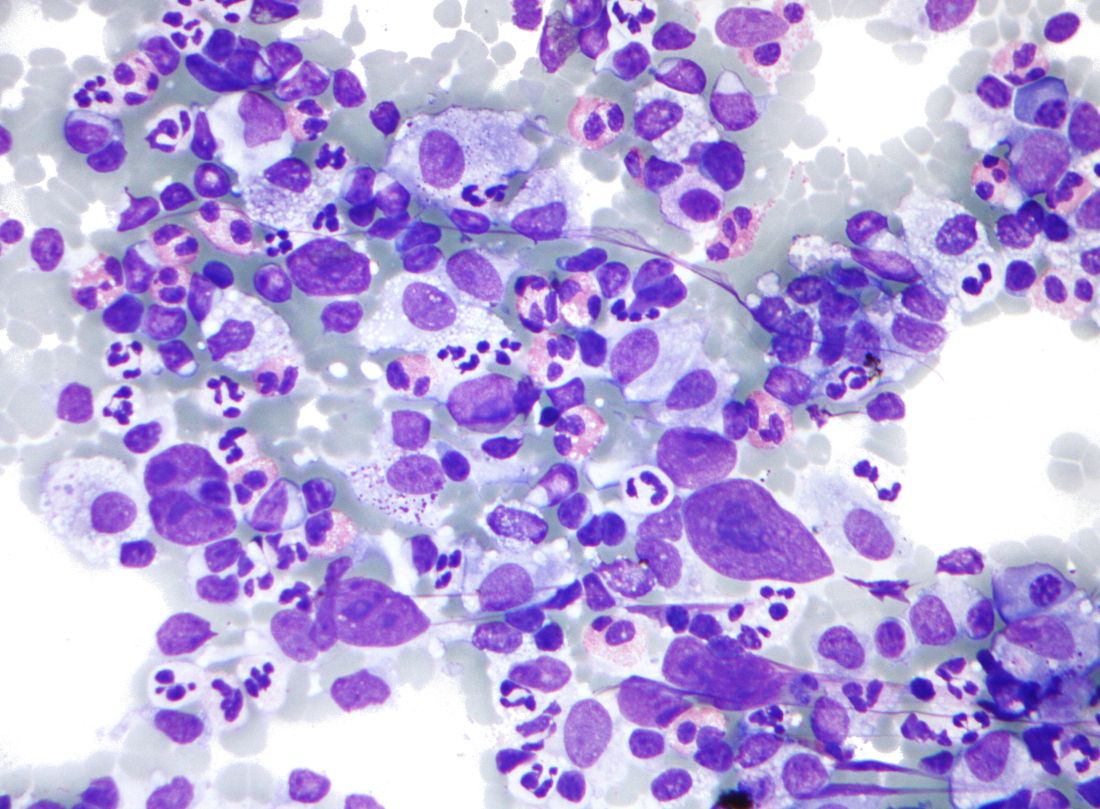
Bv, a targeted anti-CD30 antibody-drug conjugate, received expanded Food and Drug Administration approval in March 2018 for frontline use in combination with chemotherapy in adults with stage III or IV classical Hodgkin lymphoma (HL). The current study is the first to include Bv as part of a chemotherapy regimen in the frontline setting for pediatric classical HL, the authors noted, adding that their primary aim was to reduce prescribed radiation thereby limiting late toxicities associated with radiation in this population.
Patients enrolled were children and adolescents aged 18 years and under with stage IIB, IIIB, or IV classical HL. Bv was used in place of vincristine in the standard OEPA/COPDac (vincristine, etoposide, prednisone, and doxorubicin/cyclophosphamide, vincristine, prednisone, and dacarbazine) frontline regimen for pediatric HL.
The Bv-based chemotherapy regimen was well tolerated and mostly limited to low-grade nausea, vomiting, and constipation, and the most common adverse events were hematologic events occurring mainly during the first two cycles of chemotherapy.
“Notably, we observed a very low incidence of neuropathy (4%) by both clinician and patient report, and no participants required Bv dose reduction or discontinuation,” they wrote, explaining that neuropathy is more common with vincristine.
Radiation exposure
Residual node radiotherapy (RNRT) was delivered at a prescribed dose of 25.5 Gy in 17 fractions of 1.5 Gy, 2-4 weeks after completion of chemotherapy only to nodal sites that did not achieve a CR at the early response assessment (ERA) after two cycles of therapy.
“Patients treated with RNRT had significantly lower integral radiation dose compared with patients treated on HOD99 with [involved-field radiation therapy] (78.1 J vs. 249.6 J),” the authors wrote. “Doses to specific organs were also compared ... [t]he mean heart dose was reduced to 5.29 Gy from 16.9 Gy, and the mean thyroid dose was reduced to 4.46 Gy from 25.9 Gy.”
Women also had significantly less breast radiation exposure (mean of 3.21 Gy vs. 6.85 Gy in HOD99).
One irradiated patient experienced disease progression at the end of therapy, but remained disease free more than 6 years following salvage therapy, and one unexpected death occurred, the authors said.
“We have already reduced the use of radiation for low-risk Hodgkin lymphoma patients. In this study we’ve shown that it is also possible to either omit or reduce the extent of radiation for high-risk patients, using highly focal methods such as proton beam radiation or intensity modulated radiation,” co–senior author Matthew Krasin, MD, of St. Jude’s department of radiation oncology, stated in a press release.
Next steps
Co–senior author Melissa Hudson, MD, the St. Jude cancer survivorship division director, added that “[b]eing able to offer Hodgkin lymphoma patients a targeted therapy in the frontline setting is an exciting development.
“The favorable safety and toxicity profile of Bv in combination with chemotherapy for high-risk pediatric patients supports its prospective evaluation in a randomized trial,” the authors concluded, noting that “[l]onger follow-up is required to establish if this approach reduces risk of late-occurring toxicities such as second malignant neoplasms in this cohort of minimally irradiated patients.”
The study was sponsored by Seattle Genetics. The research at St. Jude was funded in part by grants from the National Cancer Institute and ALSAC (American Lebanese Syrian Associated Charities), St. Jude’s fundraising and awareness organization. Dr. Metzger reported research funding from Seattle Genetics. Dr. Krasin reported a consulting or advisory role for Debiopharm Group. Dr. Hudson reported a consulting or advisory role for Oncology Research Information Exchange Network, Princess Máxima Center.
A frontline treatment regimen including brentuximab vedotin (Bv) was well tolerated, was highly effective, and significantly reduced radiation exposure in pediatric patients with high-risk Hodgkin lymphoma, according to the results of an open-label, phase 2 trial.
Of 77 patients enrolled in the investigator-initiated, single-arm, multicenter trial, 27 (35%) achieved complete remission (CR) without radiation at the early response assessment (ERA) after two cycles of therapy, reported Monika L. Metzger, MD, of St. Jude Children’s Research Hospital, Memphis, Tenn. and colleagues. The report was published online in the Journal of Clinical Oncology.
The addition of Bv also resulted in superior event-free survival (97.4%) and overall survival (98.7%) at median follow-up of 3.4 years, compared with previously published pediatric trials, such as the HOD99 trial (EFS and OS of 80.8% and 96.5%, respectively), the authors noted.
Bv chemotherapy
Bv, a targeted anti-CD30 antibody-drug conjugate, received expanded Food and Drug Administration approval in March 2018 for frontline use in combination with chemotherapy in adults with stage III or IV classical Hodgkin lymphoma (HL). The current study is the first to include Bv as part of a chemotherapy regimen in the frontline setting for pediatric classical HL, the authors noted, adding that their primary aim was to reduce prescribed radiation thereby limiting late toxicities associated with radiation in this population.
Patients enrolled were children and adolescents aged 18 years and under with stage IIB, IIIB, or IV classical HL. Bv was used in place of vincristine in the standard OEPA/COPDac (vincristine, etoposide, prednisone, and doxorubicin/cyclophosphamide, vincristine, prednisone, and dacarbazine) frontline regimen for pediatric HL.
The Bv-based chemotherapy regimen was well tolerated and mostly limited to low-grade nausea, vomiting, and constipation, and the most common adverse events were hematologic events occurring mainly during the first two cycles of chemotherapy.
“Notably, we observed a very low incidence of neuropathy (4%) by both clinician and patient report, and no participants required Bv dose reduction or discontinuation,” they wrote, explaining that neuropathy is more common with vincristine.
Radiation exposure
Residual node radiotherapy (RNRT) was delivered at a prescribed dose of 25.5 Gy in 17 fractions of 1.5 Gy, 2-4 weeks after completion of chemotherapy only to nodal sites that did not achieve a CR at the early response assessment (ERA) after two cycles of therapy.
“Patients treated with RNRT had significantly lower integral radiation dose compared with patients treated on HOD99 with [involved-field radiation therapy] (78.1 J vs. 249.6 J),” the authors wrote. “Doses to specific organs were also compared ... [t]he mean heart dose was reduced to 5.29 Gy from 16.9 Gy, and the mean thyroid dose was reduced to 4.46 Gy from 25.9 Gy.”
Women also had significantly less breast radiation exposure (mean of 3.21 Gy vs. 6.85 Gy in HOD99).
One irradiated patient experienced disease progression at the end of therapy, but remained disease free more than 6 years following salvage therapy, and one unexpected death occurred, the authors said.
“We have already reduced the use of radiation for low-risk Hodgkin lymphoma patients. In this study we’ve shown that it is also possible to either omit or reduce the extent of radiation for high-risk patients, using highly focal methods such as proton beam radiation or intensity modulated radiation,” co–senior author Matthew Krasin, MD, of St. Jude’s department of radiation oncology, stated in a press release.
Next steps
Co–senior author Melissa Hudson, MD, the St. Jude cancer survivorship division director, added that “[b]eing able to offer Hodgkin lymphoma patients a targeted therapy in the frontline setting is an exciting development.
“The favorable safety and toxicity profile of Bv in combination with chemotherapy for high-risk pediatric patients supports its prospective evaluation in a randomized trial,” the authors concluded, noting that “[l]onger follow-up is required to establish if this approach reduces risk of late-occurring toxicities such as second malignant neoplasms in this cohort of minimally irradiated patients.”
The study was sponsored by Seattle Genetics. The research at St. Jude was funded in part by grants from the National Cancer Institute and ALSAC (American Lebanese Syrian Associated Charities), St. Jude’s fundraising and awareness organization. Dr. Metzger reported research funding from Seattle Genetics. Dr. Krasin reported a consulting or advisory role for Debiopharm Group. Dr. Hudson reported a consulting or advisory role for Oncology Research Information Exchange Network, Princess Máxima Center.
A frontline treatment regimen including brentuximab vedotin (Bv) was well tolerated, was highly effective, and significantly reduced radiation exposure in pediatric patients with high-risk Hodgkin lymphoma, according to the results of an open-label, phase 2 trial.
Of 77 patients enrolled in the investigator-initiated, single-arm, multicenter trial, 27 (35%) achieved complete remission (CR) without radiation at the early response assessment (ERA) after two cycles of therapy, reported Monika L. Metzger, MD, of St. Jude Children’s Research Hospital, Memphis, Tenn. and colleagues. The report was published online in the Journal of Clinical Oncology.
The addition of Bv also resulted in superior event-free survival (97.4%) and overall survival (98.7%) at median follow-up of 3.4 years, compared with previously published pediatric trials, such as the HOD99 trial (EFS and OS of 80.8% and 96.5%, respectively), the authors noted.
Bv chemotherapy
Bv, a targeted anti-CD30 antibody-drug conjugate, received expanded Food and Drug Administration approval in March 2018 for frontline use in combination with chemotherapy in adults with stage III or IV classical Hodgkin lymphoma (HL). The current study is the first to include Bv as part of a chemotherapy regimen in the frontline setting for pediatric classical HL, the authors noted, adding that their primary aim was to reduce prescribed radiation thereby limiting late toxicities associated with radiation in this population.
Patients enrolled were children and adolescents aged 18 years and under with stage IIB, IIIB, or IV classical HL. Bv was used in place of vincristine in the standard OEPA/COPDac (vincristine, etoposide, prednisone, and doxorubicin/cyclophosphamide, vincristine, prednisone, and dacarbazine) frontline regimen for pediatric HL.
The Bv-based chemotherapy regimen was well tolerated and mostly limited to low-grade nausea, vomiting, and constipation, and the most common adverse events were hematologic events occurring mainly during the first two cycles of chemotherapy.
“Notably, we observed a very low incidence of neuropathy (4%) by both clinician and patient report, and no participants required Bv dose reduction or discontinuation,” they wrote, explaining that neuropathy is more common with vincristine.
Radiation exposure
Residual node radiotherapy (RNRT) was delivered at a prescribed dose of 25.5 Gy in 17 fractions of 1.5 Gy, 2-4 weeks after completion of chemotherapy only to nodal sites that did not achieve a CR at the early response assessment (ERA) after two cycles of therapy.
“Patients treated with RNRT had significantly lower integral radiation dose compared with patients treated on HOD99 with [involved-field radiation therapy] (78.1 J vs. 249.6 J),” the authors wrote. “Doses to specific organs were also compared ... [t]he mean heart dose was reduced to 5.29 Gy from 16.9 Gy, and the mean thyroid dose was reduced to 4.46 Gy from 25.9 Gy.”
Women also had significantly less breast radiation exposure (mean of 3.21 Gy vs. 6.85 Gy in HOD99).
One irradiated patient experienced disease progression at the end of therapy, but remained disease free more than 6 years following salvage therapy, and one unexpected death occurred, the authors said.
“We have already reduced the use of radiation for low-risk Hodgkin lymphoma patients. In this study we’ve shown that it is also possible to either omit or reduce the extent of radiation for high-risk patients, using highly focal methods such as proton beam radiation or intensity modulated radiation,” co–senior author Matthew Krasin, MD, of St. Jude’s department of radiation oncology, stated in a press release.
Next steps
Co–senior author Melissa Hudson, MD, the St. Jude cancer survivorship division director, added that “[b]eing able to offer Hodgkin lymphoma patients a targeted therapy in the frontline setting is an exciting development.
“The favorable safety and toxicity profile of Bv in combination with chemotherapy for high-risk pediatric patients supports its prospective evaluation in a randomized trial,” the authors concluded, noting that “[l]onger follow-up is required to establish if this approach reduces risk of late-occurring toxicities such as second malignant neoplasms in this cohort of minimally irradiated patients.”
The study was sponsored by Seattle Genetics. The research at St. Jude was funded in part by grants from the National Cancer Institute and ALSAC (American Lebanese Syrian Associated Charities), St. Jude’s fundraising and awareness organization. Dr. Metzger reported research funding from Seattle Genetics. Dr. Krasin reported a consulting or advisory role for Debiopharm Group. Dr. Hudson reported a consulting or advisory role for Oncology Research Information Exchange Network, Princess Máxima Center.
FROM THE JOURNAL OF CLINICAL ONCOLOGY