User login
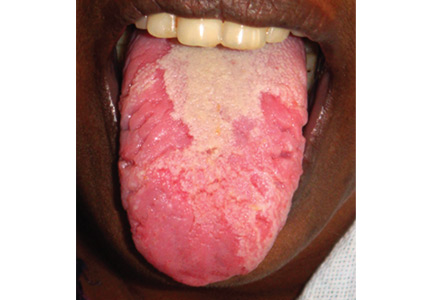
A previously healthy 35-year-old woman presented with reddish discoloration of her tongue for the past 7 days, accompanied by mild soreness over the area when eating spicy foods. The lesion had also changed shape repeatedly. She denied any other local or systemic symptoms.
Lingual examination showed clearly delineated areas of shiny, erythematous mucosa on the dorsal and lateral aspects of the tongue, surrounded by white borders (Figure 1). Examination of the throat and oral cavity were unremarkable. All other systemic examinations were normal. Laboratory testing showed a normal hemogram, blood glucose, and metabolic profile.
These findings were suggestive of geographic tongue, a benign, self-limiting inflammation. The patient was reassured of the benign nature of the condition and was advised to avoid spicy food until resolution of the lesion. A follow-up examination 1 month later showed complete healing of the lesion.
A COMMON, BENIGN, SELF-LIMITING MUCOSAL CONDITION
Geographic tongue—also known as benign migratory glossitis and lingual erythema migrans—is commonly seen in daily practice, with a prevalence of 2% to 3% in the general population.1 In the United States, the condition is more prevalent in whites and blacks than in Hispanics, but has no association with age or sex.
This condition is characterized by circinate, maplike areas of erythema surrounded by well-demarcated scalloped white borders, typically on the dorsum and the lateral borders of the tongue.2 The appearance, which represents loss of filiform papillae (depapillation) from the lingual mucosa, can change in size, shape, or location in a matter of minutes or hours. The name “lingual erythema migrans” reflects the changing clinical picture.3 Rarely, the labial or palatal mucosa is affected.
POSTULATED TO BE AN INTRAORAL FORM OF PSORIASIS
The precise etiology remains obscure.2 Histopathologically, geographic tongue is characterized by hyperparakeratosis and acanthosis resembling psoriasis. Hence, it has been postulated that it represents a form of intraoral psoriasis.2,4 The condition is also associated with allergy, stress, diabetes mellitus, and anemia. Triggers include hot, spicy, and acidic foods and alcohol. Contrary to previous belief, geographic tongue has been found to have an inverse association with smoking.5 Although striking, the lesion rarely warrants further investigation.
REASSURANCE IS THE MAIN TREATMENT
Geographic tongue has a remitting and relapsing course with no complications or permanent sequelae.3 The differential diagnosis includes oral candidiasis, leukoplakia, vitamin deficiency glossitis, lichen planus, systemic lupus erythematosus, drug reaction, and recurrent aphthous stomatitis. The condition is differentiated from oral candidiasis by its presence in an otherwise healthy person and by the changing pattern of the lesions over time. Also, candidal pseudomembranes can be easily removed, leaving a painless red base. Evaluations to rule out anemia, nutritional deficiencies, and diabetes mellitus can be done if these conditions are suspected, as they are associated with geographic tongue.
Reassurance is the main treatment. Topical corticosteroids and local anesthetics may provide symptomatic relief in mild forms of the disease. Topical tacrolimus and systemic cyclosporine have been reported as useful in severe cases.6
- Masferrer E, Jucgla A. Images in clinical medicine. Geographic tongue. N Engl J Med 2009; 361:e44.
- Assimakopoulos D, Patrikakos G, Fotika C, Elisaf M. Benign migratory glossitis or geographic tongue: an enigmatic oral lesion. Am J Med 2002; 113:751–755.
- Scully C, Hegarty A. The oral cavity and lips. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8th ed. West Sussex, UK: Wiley-Blackwell; 2010:69–100.
- Zargari O. The prevalence and significance of fissured tongue and geographical tongue in psoriatic patients. Clin Exp Dermatol 2006; 31:192–195.
- Shulman JD, Carpenter WM. Prevalence and risk factors associated with geographic tongue among US adults. Oral Dis 2006; 12:381–386.
- Ishibashi M, Tojo G, Watanabe M, Tamabuchi T, Masu T, Aiba S. Geographic tongue treated with topical tacrolimus. J Dermatol Case Rep 2010; 4:57–59.
A previously healthy 35-year-old woman presented with reddish discoloration of her tongue for the past 7 days, accompanied by mild soreness over the area when eating spicy foods. The lesion had also changed shape repeatedly. She denied any other local or systemic symptoms.
Lingual examination showed clearly delineated areas of shiny, erythematous mucosa on the dorsal and lateral aspects of the tongue, surrounded by white borders (Figure 1). Examination of the throat and oral cavity were unremarkable. All other systemic examinations were normal. Laboratory testing showed a normal hemogram, blood glucose, and metabolic profile.
These findings were suggestive of geographic tongue, a benign, self-limiting inflammation. The patient was reassured of the benign nature of the condition and was advised to avoid spicy food until resolution of the lesion. A follow-up examination 1 month later showed complete healing of the lesion.
A COMMON, BENIGN, SELF-LIMITING MUCOSAL CONDITION
Geographic tongue—also known as benign migratory glossitis and lingual erythema migrans—is commonly seen in daily practice, with a prevalence of 2% to 3% in the general population.1 In the United States, the condition is more prevalent in whites and blacks than in Hispanics, but has no association with age or sex.
This condition is characterized by circinate, maplike areas of erythema surrounded by well-demarcated scalloped white borders, typically on the dorsum and the lateral borders of the tongue.2 The appearance, which represents loss of filiform papillae (depapillation) from the lingual mucosa, can change in size, shape, or location in a matter of minutes or hours. The name “lingual erythema migrans” reflects the changing clinical picture.3 Rarely, the labial or palatal mucosa is affected.
POSTULATED TO BE AN INTRAORAL FORM OF PSORIASIS
The precise etiology remains obscure.2 Histopathologically, geographic tongue is characterized by hyperparakeratosis and acanthosis resembling psoriasis. Hence, it has been postulated that it represents a form of intraoral psoriasis.2,4 The condition is also associated with allergy, stress, diabetes mellitus, and anemia. Triggers include hot, spicy, and acidic foods and alcohol. Contrary to previous belief, geographic tongue has been found to have an inverse association with smoking.5 Although striking, the lesion rarely warrants further investigation.
REASSURANCE IS THE MAIN TREATMENT
Geographic tongue has a remitting and relapsing course with no complications or permanent sequelae.3 The differential diagnosis includes oral candidiasis, leukoplakia, vitamin deficiency glossitis, lichen planus, systemic lupus erythematosus, drug reaction, and recurrent aphthous stomatitis. The condition is differentiated from oral candidiasis by its presence in an otherwise healthy person and by the changing pattern of the lesions over time. Also, candidal pseudomembranes can be easily removed, leaving a painless red base. Evaluations to rule out anemia, nutritional deficiencies, and diabetes mellitus can be done if these conditions are suspected, as they are associated with geographic tongue.
Reassurance is the main treatment. Topical corticosteroids and local anesthetics may provide symptomatic relief in mild forms of the disease. Topical tacrolimus and systemic cyclosporine have been reported as useful in severe cases.6
A previously healthy 35-year-old woman presented with reddish discoloration of her tongue for the past 7 days, accompanied by mild soreness over the area when eating spicy foods. The lesion had also changed shape repeatedly. She denied any other local or systemic symptoms.
Lingual examination showed clearly delineated areas of shiny, erythematous mucosa on the dorsal and lateral aspects of the tongue, surrounded by white borders (Figure 1). Examination of the throat and oral cavity were unremarkable. All other systemic examinations were normal. Laboratory testing showed a normal hemogram, blood glucose, and metabolic profile.
These findings were suggestive of geographic tongue, a benign, self-limiting inflammation. The patient was reassured of the benign nature of the condition and was advised to avoid spicy food until resolution of the lesion. A follow-up examination 1 month later showed complete healing of the lesion.
A COMMON, BENIGN, SELF-LIMITING MUCOSAL CONDITION
Geographic tongue—also known as benign migratory glossitis and lingual erythema migrans—is commonly seen in daily practice, with a prevalence of 2% to 3% in the general population.1 In the United States, the condition is more prevalent in whites and blacks than in Hispanics, but has no association with age or sex.
This condition is characterized by circinate, maplike areas of erythema surrounded by well-demarcated scalloped white borders, typically on the dorsum and the lateral borders of the tongue.2 The appearance, which represents loss of filiform papillae (depapillation) from the lingual mucosa, can change in size, shape, or location in a matter of minutes or hours. The name “lingual erythema migrans” reflects the changing clinical picture.3 Rarely, the labial or palatal mucosa is affected.
POSTULATED TO BE AN INTRAORAL FORM OF PSORIASIS
The precise etiology remains obscure.2 Histopathologically, geographic tongue is characterized by hyperparakeratosis and acanthosis resembling psoriasis. Hence, it has been postulated that it represents a form of intraoral psoriasis.2,4 The condition is also associated with allergy, stress, diabetes mellitus, and anemia. Triggers include hot, spicy, and acidic foods and alcohol. Contrary to previous belief, geographic tongue has been found to have an inverse association with smoking.5 Although striking, the lesion rarely warrants further investigation.
REASSURANCE IS THE MAIN TREATMENT
Geographic tongue has a remitting and relapsing course with no complications or permanent sequelae.3 The differential diagnosis includes oral candidiasis, leukoplakia, vitamin deficiency glossitis, lichen planus, systemic lupus erythematosus, drug reaction, and recurrent aphthous stomatitis. The condition is differentiated from oral candidiasis by its presence in an otherwise healthy person and by the changing pattern of the lesions over time. Also, candidal pseudomembranes can be easily removed, leaving a painless red base. Evaluations to rule out anemia, nutritional deficiencies, and diabetes mellitus can be done if these conditions are suspected, as they are associated with geographic tongue.
Reassurance is the main treatment. Topical corticosteroids and local anesthetics may provide symptomatic relief in mild forms of the disease. Topical tacrolimus and systemic cyclosporine have been reported as useful in severe cases.6
- Masferrer E, Jucgla A. Images in clinical medicine. Geographic tongue. N Engl J Med 2009; 361:e44.
- Assimakopoulos D, Patrikakos G, Fotika C, Elisaf M. Benign migratory glossitis or geographic tongue: an enigmatic oral lesion. Am J Med 2002; 113:751–755.
- Scully C, Hegarty A. The oral cavity and lips. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8th ed. West Sussex, UK: Wiley-Blackwell; 2010:69–100.
- Zargari O. The prevalence and significance of fissured tongue and geographical tongue in psoriatic patients. Clin Exp Dermatol 2006; 31:192–195.
- Shulman JD, Carpenter WM. Prevalence and risk factors associated with geographic tongue among US adults. Oral Dis 2006; 12:381–386.
- Ishibashi M, Tojo G, Watanabe M, Tamabuchi T, Masu T, Aiba S. Geographic tongue treated with topical tacrolimus. J Dermatol Case Rep 2010; 4:57–59.
- Masferrer E, Jucgla A. Images in clinical medicine. Geographic tongue. N Engl J Med 2009; 361:e44.
- Assimakopoulos D, Patrikakos G, Fotika C, Elisaf M. Benign migratory glossitis or geographic tongue: an enigmatic oral lesion. Am J Med 2002; 113:751–755.
- Scully C, Hegarty A. The oral cavity and lips. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8th ed. West Sussex, UK: Wiley-Blackwell; 2010:69–100.
- Zargari O. The prevalence and significance of fissured tongue and geographical tongue in psoriatic patients. Clin Exp Dermatol 2006; 31:192–195.
- Shulman JD, Carpenter WM. Prevalence and risk factors associated with geographic tongue among US adults. Oral Dis 2006; 12:381–386.
- Ishibashi M, Tojo G, Watanabe M, Tamabuchi T, Masu T, Aiba S. Geographic tongue treated with topical tacrolimus. J Dermatol Case Rep 2010; 4:57–59.