User login
ANSWER
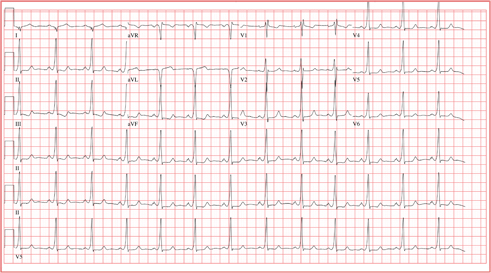
This ECG is diagnostic for Wolff-Parkinson-White (WPW) syndrome. Criteria for WPW syndrome include a normal P wave with a PR interval generally (but not always) of 0.12 sec (120 ms) or greater, initial slurring of the QRS (delta wave), a wide QRS interval > 0.10 sec (100 ms), and secondary ST/T wave changes.
In WPW syndrome, one (or multiple) accessory pathway between the atria and ventricles allows conduction impulses to bypass the atrioventricular node and activate the ventricles prematurely. This premature ventricular activation is responsible for the initial slurring of the QRS complex and produces the characteristic delta wave. The presence of an accessory pathway allows a reentrant tachycardia circuit to occur and is the source of this patient’s palpitations. Subsequent electrophysiology studies identified a single left lateral accessory pathway.
ANSWER
This ECG is diagnostic for Wolff-Parkinson-White (WPW) syndrome. Criteria for WPW syndrome include a normal P wave with a PR interval generally (but not always) of 0.12 sec (120 ms) or greater, initial slurring of the QRS (delta wave), a wide QRS interval > 0.10 sec (100 ms), and secondary ST/T wave changes.
In WPW syndrome, one (or multiple) accessory pathway between the atria and ventricles allows conduction impulses to bypass the atrioventricular node and activate the ventricles prematurely. This premature ventricular activation is responsible for the initial slurring of the QRS complex and produces the characteristic delta wave. The presence of an accessory pathway allows a reentrant tachycardia circuit to occur and is the source of this patient’s palpitations. Subsequent electrophysiology studies identified a single left lateral accessory pathway.
ANSWER
This ECG is diagnostic for Wolff-Parkinson-White (WPW) syndrome. Criteria for WPW syndrome include a normal P wave with a PR interval generally (but not always) of 0.12 sec (120 ms) or greater, initial slurring of the QRS (delta wave), a wide QRS interval > 0.10 sec (100 ms), and secondary ST/T wave changes.
In WPW syndrome, one (or multiple) accessory pathway between the atria and ventricles allows conduction impulses to bypass the atrioventricular node and activate the ventricles prematurely. This premature ventricular activation is responsible for the initial slurring of the QRS complex and produces the characteristic delta wave. The presence of an accessory pathway allows a reentrant tachycardia circuit to occur and is the source of this patient’s palpitations. Subsequent electrophysiology studies identified a single left lateral accessory pathway.

A 20-year-old woman is involved in a motor vehicle accident. Her car was hit from behind while stopped at a light, with the force of impact sufficient to deploy the airbags in both vehicles. When the paramedics arrive, the patient is conscious and responsive but is found to have a rapid pulse (approximately 170 beats/min). During transport to the hospital, her tachycardia abruptly terminates and sinus rhythm returns at rates between 80 and 90 beats/min. In the emergency department, the patient’s physical examination and x-rays reveal no injuries. Review of the rhythm strips from the paramedics in the field shows a narrow complex tachycardia at a rate of 176 beats/min. When interviewed, the patient reveals a history of palpitations, lasting from five minutes up to two hours, over the past several years. When they occur, she says, she gets dizzy and feels a pounding sensation in her chest, but she has never had chest pain or syncope. She cannot identify any specific trigger that initiates her palpitations, but has noticed that if she holds her breath and bears down (Valsalva maneuver), her palpitations will sometimes stop. Her medical history is positive for mild asthma and an allergy to peanuts. She is taking no medications and denies tobacco, alcohol, or recreational drug use. Family history is remarkable for hypertension (father) and type 2 diabetes (mother). She is the oldest of three children, and one of her sisters experiences similar bouts of palpitations. A 14-point review of systems is negative. She denies she could be pregnant; she is currently menstruating. She is 61” tall, weighs 110 lb, and is of small stature and body habitus. She is in no acute distress. Her blood pressure is 110/72 mm Hg; pulse, 80 beats/min and regular; and respiratory rate, 14 breaths/min. The physical exam is unremarkable, with the exception of abrasions on her hands and left forearm. Given the documentation of a tachycardia by the paramedics in the field and a history of recurring palpitations, an ECG is obtained, which reveals the following: a ventricular rate of 77 beats/min; PR interval, 128 ms; QRS duration, 116 ms; QT/QTc interval, 416/470 ms; P axis, 61°; R axis, 98°; and T axis, 5°. What is your interpretation of this ECG?