User login
Ultrasound has been used for decades by radiology, obstetrics-gynecology, and cardiology departments within a comprehensive paradigm in which a physician enters an order, then a trained sonographer performs the study, followed by a physician evaluating and interpreting the images.1 Unlike the traditional comprehensive paradigm, point-of-care ultrasound (POCUS) is a focused study that is both performed and interpreted by the bedside provider.2 POCUS has been demonstrated to improve diagnosis and clinical management in multiple studies.3-15
The scope of practice in POCUS differs by specialty, as POCUS is done to achieve specific procedural aims (eg, direct the needle to the correct location) or answer focused questions (eg, does the patient have a distended bladder?) related to the specialty. POCUS in hospital medicine (HM) provides immediate answers, without the delay and potential risk of transportation to other hospital areas. It may be used to diagnose pleural effusion, pneumonia, hydronephrosis, heart failure, deep vein thrombosis, and many other pathologies.5-15 It is important to understand that POCUS performed by HM is a limited study and is not a substitute for more complete ultrasound examinations conducted in the radiology suite or in the echocardiography lab.
POCUS should not be used exclusively in medical decision making, but rather in conjunction with the greater clinical context of each patient, building on established principles of diagnosis and management.
DEFINITIONS
- Credentialing: An umbrella term, which incorporates licensure, education, and certification.
- Privileging: Used to define the scope authorized for a provider by a healthcare organization based on an evaluation of the individual’s credentials and performance.
- Competency: An observable ability of a provider, integrating multiple components, such as knowledge and skills. Since competencies are observable, they can be measured and assessed to ensure their acquisition.
- Certification: The process by which an association grants recognition to a provider who has met certain predetermined qualifications specified by the association. Competence is distinguished from certification, which is defined as the process by which competence is recognized by an external agency.
All of the above mechanisms work together to provide the highest quality of reliability that a practitioner is providing safe, competent care.16-18
STATEMENTS FROM MAJOR SPECIALTY SOCIETIES
Acknowledging that there are no published guidelines in the realm of HM POCUS, the development of the credentialing process at our institution is consistent with published guidelines by Emergency Medicine societies (the most established physician users of POCUS) and the American Medical Association (AMA).19-21
The use of emergency ultrasound by physicians in the emergency department is endorsed by the American College of Emergency Physicians (ACEP).19 ACEP, along with the Society of Academic Emergency Medicine (SAEM), recommends that training in the performance and interpretation of ultrasound imaging be included during residency.20 ACEP and SAEM add that the availability of equivalent training should be made available to practicing physicians. The American Society of Echocardiography has supported the use of POCUS and sees this modality as part of the continuum of care.23,24
The AMA has also recognized that POCUS is within the scope of practice of trained physicians.22 The AMA further recommended hospital staff create their own criteria for granting ultrasound privileges based on the background and training of the physician and in accordance with the standards set within specific specialties.22,23
LOCAL POLICY AND PROCEDURE
The provision of clinical privileges in HM is governed by the rules and regulations of the department and institution for which privileges are sought. In detailing our policies and procedures above, we intend to provide an example for HM departments at other institutions that are attempting to create a POCUS credentialing program.
An interdisciplinary approach was created by our institution to address training, competency, and ongoing quality assurance (QA) concerns due to the increasing popularity of POCUS and variability in its use. We developed a hospital-wide POCUS committee with, among others, members from HM, emergency medicine, critical care, radiology, and cardiology, with a charter to standardize POCUS across departments. After review of the literature,16-18, 20, 21, 23-74 baseline training requirements were established for credentialing and developing a unified delineation of privileges for hospital-wide POCUS. The data support the use of a variety of assessments to ensure a provider has developed competence (portfolio development, knowledge-based examination, skills-based assessment, ongoing QA process). The POCUS committee identified which exams could be performed at bedside for credentialed providers, delineated imaging requirements for each exam, and set up the information technology infrastructure to support ordering and reporting through electronic health records (EHR). While the POCUS committee delineated this process for all hospital providers, we will focus our discussion on the credentialing policy and procedure in HM.
STEP 1: PATHWAY TO POCUS CREDENTIALING IN HM: COMPLETE MINIMAL FORMAL REQUIREMENTS
The credentialing requirements at our institution include one of the the following basic education pathways and minimal formal training:
Residency/Fellowship Based Pathway
Completed training in an Accreditation Council for Graduate Medical Education–approved program that provided opportunities for 20 hours of POCUS training with at least 6 hours of hands-on ultrasound scanning, 5 proctored limited cardiac ultrasound cases and portfolio development.
Practice Based Pathway
Completed 20 hours of POCUS continuing medical education (CME) with at least 6 hours of hands-on ultrasound scanning and has completed 5 proctored limited cardiac ultrasound cases (as part of CME).
The majority of HM providers had little formal residency training in POCUS, so a training program needed to be developed. Our training program, modeled after the American College of Chest Physicians’ CHEST certificate of completion,86 utilizes didactic training, hands-on instruction, and portfolio development that fulfills the minimal formal requirements in the practice-based pathway.
STEP 2: PATHWAY TO POCUS CREDENTIALING IN HM: COMPLETE PORTFOLIO AND FINAL ASSESSMENTS (KNOWLEDGE AND SKILLS–BASED)
After satisfactory completion of the minimal formal training, applicants need to provide documentation of a set number of cases. To aid this requirement, our HM department developed the portfolio guidelines in the Table. These are minimum requirements, and because of the varying training curves of learning,76-80 1 hospitalist may need to submit 300 files for review to meet the standards, while another may need to submit 500 files. Submissions are not accepted unless they yield high-quality video files with meticulous attention to gain, depth, and appropriate topographic planes. The portfolio development monitors hospitalists’ progression during their deliberate practice, providing objective assessments, feedback, and mentorship.81,82
A final knowledge exam with case-based image interpretation and hands-on examination is also provided. The passing score for the written examination is 85% and was based on the Angoff methodology.75 Providers who meet these requirements are then able to apply for POCUS credentialing in HM. Providers who do not pass the final assessments are required to participate in further training before they reattempt the assessments. There is uniformity in training outcomes but diversity in training time for POCUS providers.
Candidates who complete the portfolio and satisfactorily pass the final assessments are credentialed after review by the POCUS committee. Credentialed physicians are then able to perform POCUS and to integrate the findings into patient care.
MAINTENANCE OF CREDENTIALS
Documentation
After credentialing is obtained, all POCUS studies used in patient care are included in the EHR following a clearly defined workflow. The study is ordered through the EHR and is retrieved wirelessly on the ultrasound machine. After performing the ultrasound, all images are wirelessly transferred to the radiology Picture Archiving and Communication System server. Standardized text reports are used to distinguish focused POCUS from traditional diagnostic ultrasound studies. Documentation is optimized using electronic drop-down menus for documenting ultrasound findings in the EHR.
Minimum Number of Examinations
Maintenance of credentials will require that each hospitalist perform 10 documented ultrasounds per year for each cardiac and noncardiac application for which credentials are requested. If these numbers are not met, then all the studies performed during the previous year will be reviewed by the ultrasound committee, and providers will be provided with opportunities to meet the minimum benchmark (supervised scanning sessions).
Quality Assurance
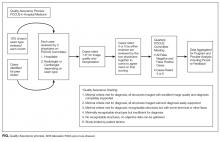
Establishing scope of practice, developing curricula, and credentialing criteria are important steps toward assuring provider competence.16,17,22,74 To be confident that providers are using POCUS appropriately, there must also be a development of standards of periodic assessment that encompass both examination performance and interpretation. The objective of a QA process is to evaluate the POCUS cases for technical competence and the interpretations for clinical accuracy, and to provide feedback to improve performance of providers.
QA is maintained through the interdisciplinary POCUS committee and is described in the Figure.
After initial credentialing, continued QA of HM POCUS is done for a proportion of ongoing exams (10% as per recommendations by ACEP) to document continued competency.2 Credentialed POCUS providers perform and document their exam and interpretations. Ultrasound interpretations are reviewed by the POCUS committee (every case by 2 physicians, 1 hospitalist, and 1 radiologist or cardiologist depending on the study type) at appropriate intervals based on volume (at minimum, quarterly). A standardized review form is used to grade images and interpretations. This is the same general rubric used with the portfolio for initial credentialing. Each case is scored on a scale of 1 to 6, with 1 representing high image quality and support for diagnosis and 6 representing studies limited by patient factors. All scores rated 4 or 5 are reviewed at the larger quarterly POCUS committee meetings. For any provider scoring a 4 or 5, the ultrasound committee will recommend a focused professional practice evaluation as it pertains to POCUS. The committee will also make recommendations on a physician’s continued privileges to the department leaders.83
BILLING
Coding, billing, and reimbursement for focused ultrasound has been supported through the AMA Physicians’ Current Procedural Terminology (CPT) 2011 codes, which includes CPT code modifiers for POCUS.84 There are significant costs associated with building a HM ultrasound program, including the education of hospitalists, ultrasound equipment purchase and maintenance, as well as image archiving and QA. The development of a HM ultrasound billing program can help justify and fund these costs.19,85
To appropriately bill for POCUS, permanently retrievable images and an interpretation document need to be available for review. HM coders are instructed to only bill if both components are available. Because most insurers will not pay for 2 of the same type of study performed within a 24-hour period, coders do not bill for ultrasounds when a comprehensive ultrasound of the same body region is performed within a 24-hour period. The workflow that we have developed, including ordering, performing, and documenting, allows for easy coding and billing.
BARRIERS AND LIMITATIONS
While POCUS has a well-established literature base in other specialties like emergency medicine, it has been a relatively recent addition to the HM specialty. As such, there exists a paucity of evidence-based medicine to support its use of POCUS in HM. While it is tempting to extrapolate from the literature of other specialties, this may not be a valid approach.
Training curves in which novice users of ultrasound become competent in specific applications are incompletely understood. Little research describes the rate of progression of learners in ultrasound towards competency. We have recently started the QA process and hope that the data will further guide feedback to the process.
Additionally, with the portfolios, the raters’ expertise may not be stable (develops through experience). We aim to mitigate this by having a group of raters reviewing each file, particularly if there is a question about if a submission is of high image quality. A notable barrier that groups face is support from their leadership regarding POCUS. Our group has had support from the chief medical officer who helped mandate the development of POCUS standards.
LESSONS LEARNED
We have developed a robust collaborative HM POCUS program. We have noted challenges in motivating all providers to work through this protocol. Development of a POCUS program takes dedicated time, and without a champion, it is at risk for failing. HM departments would be advised to seek out willing collaborators at their institutions. We have seen that it is useful to partner with some experienced emergency medicine providers. Additionally, portfolio development and feedback has been key to demonstrating growth in image acquisition. Deliberate longitudinal practice with feedback and successive refinements with POCUS obtain the highest yield towards competency. We hope our QA data will provide further feedback into the credentialing policy and procedure.
SUMMARY
It is important that POCUS users work together to recognize its potential and limitations, teach current and future care providers’ best practices, and create an infrastructure that maximizes quality of care while minimizing patient risk.
We are hopeful that this document will prove beneficial to other HM departments in the development of successful POCUS programs. We feel that it is important to make available to other HM departments a concise protocol that has successfully passed through the credentialing process at a large tertiary care medical system.
Acknowledgments
The authors would like to acknowledge Susan Truman, MD, for her contributions to the success of the POCUS committee at Regions Hospital. The authors would like to acknowledge Kreegan Reierson, MD, Ankit Mehta, MBBS, and Khuong Vuong, MD for their contributions to the success of POCUS within hospital medicine at HealthPartners. The authors would like to acknowledge Sandi Wewerka, MPH, for her review and input of this manuscript.
Disclosure
The authors do not have any relevant financial disclosures to report.
1. Soni NJ, Nilam J, Arntfield R, Kory P. Point of Care Ultrasound. Philadelphia:
Elsevier; 2015.
2. Moore CL, Copel JA. Point-of-Care Ultrasonography. N Engl J Med.
2011;364(8):749-757. PubMed
3. Randolph AG, Cook DJ, Gonzales CA, et al. Ultrasound guidance for placement
of central venous catheters: A meta-analysis of the literature. Crit Care Med.
1996;24:2053-2058. PubMed
4. Gordon CE, Feller-Kopman D, Balk EM, et al. Pneumothorax following thoracentesis:
A systematic review and meta-analysis. Arch Intern Med. 2010;170:332-339. PubMed
5. Soni NJ, Nilam J, Franco R, et al. Ultrasound in the diagnosis and management of
pleural effusions. J Hosp Med. 2015;10(12):811-816. PubMed
6. Nazerian P, Volpicelli G, Gigli C, et al. Diagnostic performance of Wells score
combined with point-of-care lung and venous ultrasound in suspected pulmonary
embolism. Acad Emerg Med. 2017;24(3):270-280. PubMed
7. Chatziantoniou A, Nazerian P, Vanni S, et al. A combination of the Wells score
with multiorgan ultrasound to stratify patients with suspected pulmonary embolism.
Eur Respir J. 2015;46:OA493; DOI:10.1183/13993003.congress-2015.
OA493.
8. Boyd JH, Sirounis D, Maizel J, Slama M. Echocardiography as a guide for fluid
management. Crit Care. 2016; DOI:10.1186/s13054-016-1407-1. PubMed
9. Mantuani D, Frazee BW, Fahimi J, Nagdev A. Point-of-Care Multi-Organ Ultrasound
Improves Diagnostic Accuracy in Adults Presenting to the Emergency
Department with Acute Dyspnea. West J Emerg Med. 2016;17(1):46-53. PubMed
10. Glockner E, Christ M, Geier F, et al. Accuracy of Point-of-Care B-Line Lung
Ultrasound in Comparison to NT-ProBNP for Screening Acute Heart Failure.
Ultrasound Int Open. 2016;2(3):e90-e92. PubMed
11. Bhagra A, Tierney DM, Sekiguchi H, Soni NJ. Point-of-Care Ultrasonography
for Primary Care Physicians and General Internists. Mayo Clin Proc.
2016;91(12):1811-1827. PubMed
12. Crisp JG, Lovato LM, and Jang TB. Compression ultrasonography of the lower extremity
with portable vascular ultrasonography can accurately detect deep venous
thrombosis in the emergency department. Ann Emerg Med. 2010;56:601-610. PubMed
13. Squire BT, Fox JC, and Anderson C. ABSCESS: Applied bedside sonography
for convenient. Evaluation of superficial soft tissue infections. Acad Emerg Med.
2005;12:601-606. PubMed
14. Narasimhan M, Koenig SJ, Mayo PH. A Whole-Body Approach to Point of Care
Ultrasound. Chest. 2016;150(4):772-776. PubMed
15. Oks M, Cleven KL, Cardenas-Garcia J, et al. The effect of point-of-care ultrasonography
on imaging studies in the medical ICU: a comparative study. Chest.
2014;146(6):1574-1577. PubMed
16. Mayo PH, Beaulieu Y, Doelken P, et al. American College of Chest Physicians/
La Société de Réanimation de Langue Française Statement on Competence in
Critical Care Ultrasonography. Chest. 2009;135(4):1050-1060. PubMed
17. Frank JR, Snell LS, Ten Cate O, et al. Competency-based medical education:
Theory to practice. Med Teach. 2010;32:638-645. PubMed
18. The Who, What, When, and Where’s of Credentialing and Privileging. The
Joint Commission. http://www.jointcommission.org/assets/1/6/AHC_who_what_
when_and_where_credentialing_booklet.pdf. Accessed December 21, 2016.
19. American College of Emergency Physicians Policy Statement: Emergency Ultrasound
Guidelines. 2016. https://www.acep.org/Clinical---Practice-Management/
ACEP-Ultrasound-Guidelines/. Accessed October 26, 2016.
20. Society for Academic Emergency Medicine. Ultrasound Position Statement. Annual
Meeting 1996.
21. American Medical Association. Privileging for ultrasound imaging. 2001; Policy
H-230.960. www.ama-assn.org. Accessed July 28, 2017 PubMed
22. Stein JC, Nobay F. Emergency Department Ultrasound Credentialing: a sample
policy and procedure. J Emerg Med. 2009;37(2):153-159. PubMed
23. Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ. Focused
Cardiac Ultrasound: Recommendations from the American Society of Echocardiography.
J Am Soc Echocardiogr. 2013;26(6):567-581. PubMed
24. Wiegers S. The Point of Care. J Am Soc Echocardiogr. 2016;29(4):19. PubMed
25. Mandavia D, Aragona J, Chan L, et al. Ultrasound training for emergency physicians—
a prospective study. Acad Emerg Med. 2000;7:1008-1014. PubMed
26. American College of Radiology Practice Parameters and Technical Standards.
https://www.acr.org/quality-safety/standards-guidelines. Accessed December 21, 2016.
27. Blois B. Office-based ultrasound screening for abdominal aortic aneurysm. Can
Fam Physician. 2012;58(3):e172-e178. PubMed
28. Rubano E, Mehta N, Caputo W, Paladino L, Sinert R. Systematic review: emergency
department bedside ultrasonography for diagnosing suspected abdominal
aortic aneurysm. Acad Emerg Med. 2013;20:128-138. PubMed
29. Dijos M, Pucheux Y, Lafitte M, et al. Fast track echo of abdominal aortic aneurysm
using a real pocket-ultrasound device at bedside. Echocardiography. PubMed
2012;29(3):285-290.
30. Cox C, MacDonald S, Henneberry R, Atkinson PR. My patient has abdominal
and flank pain: Identifying renal causes. Ultrasound. 2015;23(4):242-250. PubMed
31. Gaspari R, Horst K. Emergency ultrasound and urinalysis in the evaluation of
patients with flank pain. Acad Emerg Med. 2005;12:1180-1184. PubMed
32. Kartal M, Eray O, Erdogru T, et al. Prospective validation of a current algorithm
including bedside US performed by emergency physicians for patients with acute
flank pain suspected for renal colic. Emerg Med J. 2006;23(5):341-344. PubMed
33. Noble VE, Brown DF. Renal ultrasound. Emerg Med Clin North Am. 2004;22:641-659. PubMed
34. Surange R, Jeygopal NS, Chowdhury SD, et al. Bedside ultrasound: a useful tool
for the on call urologist? Int Urol Nephrol. 2001;32:591-596. PubMed
35. Pomero F, Dentali F, Borretta V, et al. Accuracy of emergency physician-performed
ultrasonography in the diagnosis of deep-vein thrombosis. Thromb Haemost.
2013;109(1):137-145. PubMed
36. Bernardi E, Camporese G, Buller HR, et al. Erasmus Study Group. Serial 2-Point
Ultrasonography Plus D-Dimer vs Whole-Leg Color-Coded Doppler Ultrasonography
for Diagnosing Suspected Symptomatic Deep Vein Thrombosis: A Randomized
Controlled Trial. JAMA. 2008;300(14):1653-1659. PubMed
37. Burnside PR, Brown MD, Kline JA. Systematic Review of Emergency Physician–
performed Ultrasonography for Lower-Extremity Deep Vein Thrombosis. Acad
Emerg Med. 2008;15:493-498. PubMed
38. Magazzini S, Vanni S, Toccafondi S, et al. Duplex ultrasound in the emergency
department for the diagnostic management of clinically suspected deep vein
thrombosis. Acad Emerg Med. 2007;14:216-220. PubMed
39. Jacoby J, Cesta M, Axelband J, Melanson S, Heller M, Reed J. Can emergency
medicine residents detect acute deep venous thrombosis with a limited, two-site
ultrasound examination? J Emerg Med. 2007;32:197-200. PubMed
40. Jang T, Docherty M, Aubin C, Polites G. Resident-performed compression ultrasonography
for the detection of proximal deep vein thrombosis: fast and accurate.
Acad Emerg Med. 2004;11:319-322. PubMed
41. Frazee BW, Snoey ER, Levitt A. Emergency Department compression ultrasound
to diagnose proximal deep vein thrombosis. J Emerg Med. 2001;20:107-112. PubMed
42. Blaivas M, Lambert MJ, Harwood RA, Wood JP, Konicki J. Lower-extremity Doppler
for deep venous thrombosis--can emergency physicians be accurate and fast?
Acad Emerg Med. 2000;7:120-126. PubMed
43. Koenig SJ, Narasimhan M, Mayo PH. Thoracic ultrasonography for the pulmonary
specialist. Chest. 2011;140(5):1332-1341. PubMed
44. Lichtenstein, DA. A bedside ultrasound sign ruling out pneumothorax in the critically
ill. Lung sliding. Chest. 1995;108(5):1345-1348. PubMed
45. Lichtenstein D, Mézière G, Biderman P, Gepner A, Barré O. The comet-tail artifact.
An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care
Med. 1997;156(5):1640-1646. PubMed
46. Copetti R, Soldati G, Copetti P. Chest sonography: a useful tool to differentiate
acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc
Ultrasound. 2008;6:16. PubMed
47. Agricola E, Bove T, Oppizzi M, et al. Ultrasound comet-tail images: a marker
of pulmonary edema: a comparative study with wedge pressure and extravascular
lung water. Chest. 2005;127(5):1690-1695. PubMed
48. Lichtenstein DA, Meziere GA, Laqoueyte JF, Biderman P, Goldstein I, Gepner A.
A-lines and B-lines: lung ultrasound as a bedside tool for predicting pulmonary
artery occlusion pressure in the critically ill. Chest. 2009;136(4):1014-1020. PubMed
49. Lichtenstein DA, Lascols N, Meziere G, Gepner A. Ultrasound diagnosis of alveolar
consolidation in the critically ill. Intensive Care Med. 2004;30(2):276-281. PubMed
50. Lichtenstein D, Mezière G, Seitz J. The dynamic air bronchogram. A lung
ultrasound sign of alveolar consolidation ruling out atelectasis. Chest.
2009;135(6):1421–1425. PubMed
51. Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ. Comparative
diagnostic performances of auscultation, chest radiography, and lung ultrasonography
in acute respiratory distress syndrome. Anesthesiology. 2004;100(1):9-15. PubMed
52. Lichtenstein D, Meziere G. Relevance of lung ultrasound in the diagnosis of acute
respiratory failure: the BLUE protocol. Chest. 2008;134(1):117-125. PubMed
53. Mayo P, Doelken P. Pleural ultrasonography. Clin Chest Med. 2006;27(2):215-227. PubMed
54. Galderisi M, Santoro A, Versiero M, et al. Improved cardiovascular diagnostic accuracy
by pocket size imaging device in non-cardiologic outpatients: the NaUSi-
Ca (Naples Ultrasound Stethoscope in Cardiology) study. Cardiovasc Ultrasound.
2010;8:51. PubMed
55. DeCara JM, Lang RM, Koch R, Bala R, Penzotti J, Spencer KT. The use of small
personal ultrasound devices by internists without formal training in echocardiography.
Eur J Echocardiography. 2002;4:141-147. PubMed
56. Martin LD, Howell EE, Ziegelstein RC, Martire C, Shapiro EP, Hellmann DB.
Hospitalist performance of cardiac hand-carried ultrasound after focused training.
Am J Med. 2007;120:1000-1004. PubMed
57. Martin LD, Howell EE, Ziegelstein RC, et al. Hand-carried ultrasound performed
by hospitalists: does it improve the cardiac physical examination? Am J Med.
2009;122:35-41. PubMed
58. Perez-Avraham G, Kobal SL, Etzion O, et al. Left ventricular geometric abnormality
screening in hypertensive patients using a hand-carried ultrasound device.
J Clin Hypertens. 2010;12:181-186. PubMed
59. Lucas BP, Candotti C, Margeta B, et al. Diagnostic accuracy of hospitalist-performed
hand-carried ultrasound echocardiography after a brief training program. J
Hosp Med. 2009;4:340-349. PubMed
60. Kimura BJ, Fowler SJ, Fergus TS, et al. Detection of left atrial enlargement using
hand-carried ultrasound devices to screen for cardiac abnormalities. Am J Med.
2005;118:912-916. PubMed
61. Brennan JM, Blair JE, Goonewardena S, et al. A comparison by medicine residents of physical examination versus hand-carried ultrasound for estimation of
right atrial pressure. Am J Cardiol. 2007;99:1614-1616. PubMed
62. Blair JE, Brennan JM, Goonewardena SN, Shah D, Vasaiwala S, Spencer KT.
Usefulness of hand-carried ultrasound to predict elevated left ventricular filling
pressure. Am J Cardiol. 2009;103:246-247. PubMed
63. Stawicki SP, Braslow BM, Panebianco NL, et al. Intensivist use of hand-carried
ultrasonography to measure IVC collapsibility in estimating intravascular volume
status: correlations with CVP. J Am Coll Surg. 2009;209:55-61. PubMed
64. Gunst M, Ghaemmaghami V, Sperry J, et al. Accuracy of cardiac function and volume
status estimates using the bedside echocardiographic assessment in trauma/
critical care. J Trauma. 2008;65:509-515. PubMed
65. Razi R, Estrada JR, Doll J, Spencer KT. Bedside hand-carried ultrasound by internal
medicine residents versus traditional clinical assessment for the identification
of systolic dysfunction in patients admitted with decompensated heart failure. J
Am Soc Echocardiogr. 2011;24:1319-1324. PubMed
66. Croft LB, Duvall WL, Goldman ME. A pilot study of the clinical impact
of hand-carried cardiac ultrasound in the medical clinic. Echocardiography.
2006;23:439-446. PubMed
67. Vignon P, Dugard A, Abraham J, et al. Focused training for goal-oriented handheld
echocardiography performed by noncardiologist residents in the intensive
care unit. Intensive Care Med. 2007;33:1795-1799. PubMed
68. Melamed R, Sprenkle MD, Ulstad VK, Herzog CA, Leatherman JW. Assessment
of left ventricular function by intensivists using hand-held echocardiography.
Chest. 2009;135:1416-1420. PubMed
69. Mark DG, Hayden GE, Ky B, et al. Hand-carried echocardiography for assessment
of left ventricular filling and ejection fraction in the surgical intensive care unit. J
Crit Care. 2009;24(3):470.e1-470.e7. PubMed
70. Kirkpatrick JN, Davis A, Decara JM, et al. Hand-carried cardiac ultrasound as a
tool to screen for important cardiovascular disease in an underserved minority
health care clinic. J Am Soc Echocardiogr. 2004;17:399-403. PubMed
71. Fedson S, Neithardt G, Thomas P, et al. Unsuspected clinically important findings
detected with a small portable ultrasound device in patients admitted to a general
medicine service. J Am Soc Echocardiogr. 2003;16:901-905. PubMed
72. Ghani SN, Kirkpatrick JN, Spencer, KT, et al. Rapid assessment of left ventricular
systolic function in a pacemaker clinic using a hand-carried ultrasound device.
J Interv Card Electrophysiol. 2006;16:39-43. PubMed
73. Kirkpatrick JN, Ghani SN, Spencer KT. Hand carried echocardiography
screening for LV systolic dysfunction in a pulmonary function laboratory.
Eur J Echocardiogr. 2008;9:381-383. PubMed
74. Alexander JH, Peterson ED, Chen AY, Harding TM, Adams DB, Kisslo JA Jr.
Feasibility of point-of-care echocardiography by internal medicine house staff. Am
Heart J. 2004;147:476-481. PubMed
75. Angoff WH. Scales, norms and equivalent Scores. Washington, DC: American
Council on Education; 1971.
76. Hellmann DB, Whiting-O’Keefe Q, Shapiro EP, Martin LD, Martire C, Ziegelstein
RC. The rate at which residents learn to use hand-held echocardiography at
the bedside. Am J Med. 2005;118:1010-1018. PubMed
77. Kimura BJ, Amundson SA, Phan JN, Agan DL, Shaw DJ. Observations during
development of an internal medicine residency training program in cardiovascular
limited ultrasound examination. J Hosp Med. 2012;7:537-542. PubMed
78. Akhtar S, Theodoro D, Gaspari R, et al. Resident training in emergency ultrasound:
consensus recommendations from the 2008 Council of Emergency Medicine
Residency Directors Conference. Acad Emerg Med. 2009;16(s2):S32-S36. PubMed
79. Ma OJ, Gaddis G, Norvell JG, Subramanian S. How fast is the focused assessment
with sonography for trauma examination learning curve? Emerg Med Australas.
2008;20(1):32-37. PubMed
80. Gaspari RJ, Dickman E, Blehar D. Learning curve of bedside ultrasound of the gallbladder. J Emerg Med. 2009;37(1):51-56. DOI:10.1016/j.jemermed.2007.10.070. PubMed
81. Ericsson KA, Lehmann AC. Expert and exceptional performance: Evidence of
maximal adaptation to task constraints. Ann Rev Psychol. 1996;47:273-305. PubMed
82. Ericcson KA, Krampe RT, Tesch-Romer C. The role of deliberate practice in the
acquisition of expert performance. Psychol Rev. 1993;100:363-406.
83. OPPE and FPPE: Tools to help make privileging decisions. The Joint Commission.
2013. http://www.jointcommission.org/jc_physician_blog/oppe_fppe_tools_privileging_
decisions/ Accessed October 26, 2016.
84. American Medical Association. Physicians’ Current Procedural Terminology (CPT)
2011. American Medical Association, Chicago; 2011.
85. Moore CL, Gregg S, Lambert M. Performance, training, quality assurance, and
reimbursement of emergency physician-performed ultrasonography at academic
medical centers. J Ultrasound Med. 2004;23(4):459-466. PubMed
86. Critical Care Ultrasonography Certificate of Completion Program. CHEST.
American College of Chest Physicians. http://www.chestnet.org/Education/Advanced-
Clinical-Training/Certificate-of-Completion-Program/Critical-Care-Ultrasonography.
Accessed July 28, 2017.
Ultrasound has been used for decades by radiology, obstetrics-gynecology, and cardiology departments within a comprehensive paradigm in which a physician enters an order, then a trained sonographer performs the study, followed by a physician evaluating and interpreting the images.1 Unlike the traditional comprehensive paradigm, point-of-care ultrasound (POCUS) is a focused study that is both performed and interpreted by the bedside provider.2 POCUS has been demonstrated to improve diagnosis and clinical management in multiple studies.3-15
The scope of practice in POCUS differs by specialty, as POCUS is done to achieve specific procedural aims (eg, direct the needle to the correct location) or answer focused questions (eg, does the patient have a distended bladder?) related to the specialty. POCUS in hospital medicine (HM) provides immediate answers, without the delay and potential risk of transportation to other hospital areas. It may be used to diagnose pleural effusion, pneumonia, hydronephrosis, heart failure, deep vein thrombosis, and many other pathologies.5-15 It is important to understand that POCUS performed by HM is a limited study and is not a substitute for more complete ultrasound examinations conducted in the radiology suite or in the echocardiography lab.
POCUS should not be used exclusively in medical decision making, but rather in conjunction with the greater clinical context of each patient, building on established principles of diagnosis and management.
DEFINITIONS
- Credentialing: An umbrella term, which incorporates licensure, education, and certification.
- Privileging: Used to define the scope authorized for a provider by a healthcare organization based on an evaluation of the individual’s credentials and performance.
- Competency: An observable ability of a provider, integrating multiple components, such as knowledge and skills. Since competencies are observable, they can be measured and assessed to ensure their acquisition.
- Certification: The process by which an association grants recognition to a provider who has met certain predetermined qualifications specified by the association. Competence is distinguished from certification, which is defined as the process by which competence is recognized by an external agency.
All of the above mechanisms work together to provide the highest quality of reliability that a practitioner is providing safe, competent care.16-18
STATEMENTS FROM MAJOR SPECIALTY SOCIETIES
Acknowledging that there are no published guidelines in the realm of HM POCUS, the development of the credentialing process at our institution is consistent with published guidelines by Emergency Medicine societies (the most established physician users of POCUS) and the American Medical Association (AMA).19-21
The use of emergency ultrasound by physicians in the emergency department is endorsed by the American College of Emergency Physicians (ACEP).19 ACEP, along with the Society of Academic Emergency Medicine (SAEM), recommends that training in the performance and interpretation of ultrasound imaging be included during residency.20 ACEP and SAEM add that the availability of equivalent training should be made available to practicing physicians. The American Society of Echocardiography has supported the use of POCUS and sees this modality as part of the continuum of care.23,24
The AMA has also recognized that POCUS is within the scope of practice of trained physicians.22 The AMA further recommended hospital staff create their own criteria for granting ultrasound privileges based on the background and training of the physician and in accordance with the standards set within specific specialties.22,23
LOCAL POLICY AND PROCEDURE
The provision of clinical privileges in HM is governed by the rules and regulations of the department and institution for which privileges are sought. In detailing our policies and procedures above, we intend to provide an example for HM departments at other institutions that are attempting to create a POCUS credentialing program.
An interdisciplinary approach was created by our institution to address training, competency, and ongoing quality assurance (QA) concerns due to the increasing popularity of POCUS and variability in its use. We developed a hospital-wide POCUS committee with, among others, members from HM, emergency medicine, critical care, radiology, and cardiology, with a charter to standardize POCUS across departments. After review of the literature,16-18, 20, 21, 23-74 baseline training requirements were established for credentialing and developing a unified delineation of privileges for hospital-wide POCUS. The data support the use of a variety of assessments to ensure a provider has developed competence (portfolio development, knowledge-based examination, skills-based assessment, ongoing QA process). The POCUS committee identified which exams could be performed at bedside for credentialed providers, delineated imaging requirements for each exam, and set up the information technology infrastructure to support ordering and reporting through electronic health records (EHR). While the POCUS committee delineated this process for all hospital providers, we will focus our discussion on the credentialing policy and procedure in HM.
STEP 1: PATHWAY TO POCUS CREDENTIALING IN HM: COMPLETE MINIMAL FORMAL REQUIREMENTS
The credentialing requirements at our institution include one of the the following basic education pathways and minimal formal training:
Residency/Fellowship Based Pathway
Completed training in an Accreditation Council for Graduate Medical Education–approved program that provided opportunities for 20 hours of POCUS training with at least 6 hours of hands-on ultrasound scanning, 5 proctored limited cardiac ultrasound cases and portfolio development.
Practice Based Pathway
Completed 20 hours of POCUS continuing medical education (CME) with at least 6 hours of hands-on ultrasound scanning and has completed 5 proctored limited cardiac ultrasound cases (as part of CME).
The majority of HM providers had little formal residency training in POCUS, so a training program needed to be developed. Our training program, modeled after the American College of Chest Physicians’ CHEST certificate of completion,86 utilizes didactic training, hands-on instruction, and portfolio development that fulfills the minimal formal requirements in the practice-based pathway.
STEP 2: PATHWAY TO POCUS CREDENTIALING IN HM: COMPLETE PORTFOLIO AND FINAL ASSESSMENTS (KNOWLEDGE AND SKILLS–BASED)
After satisfactory completion of the minimal formal training, applicants need to provide documentation of a set number of cases. To aid this requirement, our HM department developed the portfolio guidelines in the Table. These are minimum requirements, and because of the varying training curves of learning,76-80 1 hospitalist may need to submit 300 files for review to meet the standards, while another may need to submit 500 files. Submissions are not accepted unless they yield high-quality video files with meticulous attention to gain, depth, and appropriate topographic planes. The portfolio development monitors hospitalists’ progression during their deliberate practice, providing objective assessments, feedback, and mentorship.81,82
A final knowledge exam with case-based image interpretation and hands-on examination is also provided. The passing score for the written examination is 85% and was based on the Angoff methodology.75 Providers who meet these requirements are then able to apply for POCUS credentialing in HM. Providers who do not pass the final assessments are required to participate in further training before they reattempt the assessments. There is uniformity in training outcomes but diversity in training time for POCUS providers.
Candidates who complete the portfolio and satisfactorily pass the final assessments are credentialed after review by the POCUS committee. Credentialed physicians are then able to perform POCUS and to integrate the findings into patient care.
MAINTENANCE OF CREDENTIALS
Documentation
After credentialing is obtained, all POCUS studies used in patient care are included in the EHR following a clearly defined workflow. The study is ordered through the EHR and is retrieved wirelessly on the ultrasound machine. After performing the ultrasound, all images are wirelessly transferred to the radiology Picture Archiving and Communication System server. Standardized text reports are used to distinguish focused POCUS from traditional diagnostic ultrasound studies. Documentation is optimized using electronic drop-down menus for documenting ultrasound findings in the EHR.
Minimum Number of Examinations
Maintenance of credentials will require that each hospitalist perform 10 documented ultrasounds per year for each cardiac and noncardiac application for which credentials are requested. If these numbers are not met, then all the studies performed during the previous year will be reviewed by the ultrasound committee, and providers will be provided with opportunities to meet the minimum benchmark (supervised scanning sessions).
Quality Assurance
Establishing scope of practice, developing curricula, and credentialing criteria are important steps toward assuring provider competence.16,17,22,74 To be confident that providers are using POCUS appropriately, there must also be a development of standards of periodic assessment that encompass both examination performance and interpretation. The objective of a QA process is to evaluate the POCUS cases for technical competence and the interpretations for clinical accuracy, and to provide feedback to improve performance of providers.
QA is maintained through the interdisciplinary POCUS committee and is described in the Figure.
After initial credentialing, continued QA of HM POCUS is done for a proportion of ongoing exams (10% as per recommendations by ACEP) to document continued competency.2 Credentialed POCUS providers perform and document their exam and interpretations. Ultrasound interpretations are reviewed by the POCUS committee (every case by 2 physicians, 1 hospitalist, and 1 radiologist or cardiologist depending on the study type) at appropriate intervals based on volume (at minimum, quarterly). A standardized review form is used to grade images and interpretations. This is the same general rubric used with the portfolio for initial credentialing. Each case is scored on a scale of 1 to 6, with 1 representing high image quality and support for diagnosis and 6 representing studies limited by patient factors. All scores rated 4 or 5 are reviewed at the larger quarterly POCUS committee meetings. For any provider scoring a 4 or 5, the ultrasound committee will recommend a focused professional practice evaluation as it pertains to POCUS. The committee will also make recommendations on a physician’s continued privileges to the department leaders.83
BILLING
Coding, billing, and reimbursement for focused ultrasound has been supported through the AMA Physicians’ Current Procedural Terminology (CPT) 2011 codes, which includes CPT code modifiers for POCUS.84 There are significant costs associated with building a HM ultrasound program, including the education of hospitalists, ultrasound equipment purchase and maintenance, as well as image archiving and QA. The development of a HM ultrasound billing program can help justify and fund these costs.19,85
To appropriately bill for POCUS, permanently retrievable images and an interpretation document need to be available for review. HM coders are instructed to only bill if both components are available. Because most insurers will not pay for 2 of the same type of study performed within a 24-hour period, coders do not bill for ultrasounds when a comprehensive ultrasound of the same body region is performed within a 24-hour period. The workflow that we have developed, including ordering, performing, and documenting, allows for easy coding and billing.
BARRIERS AND LIMITATIONS
While POCUS has a well-established literature base in other specialties like emergency medicine, it has been a relatively recent addition to the HM specialty. As such, there exists a paucity of evidence-based medicine to support its use of POCUS in HM. While it is tempting to extrapolate from the literature of other specialties, this may not be a valid approach.
Training curves in which novice users of ultrasound become competent in specific applications are incompletely understood. Little research describes the rate of progression of learners in ultrasound towards competency. We have recently started the QA process and hope that the data will further guide feedback to the process.
Additionally, with the portfolios, the raters’ expertise may not be stable (develops through experience). We aim to mitigate this by having a group of raters reviewing each file, particularly if there is a question about if a submission is of high image quality. A notable barrier that groups face is support from their leadership regarding POCUS. Our group has had support from the chief medical officer who helped mandate the development of POCUS standards.
LESSONS LEARNED
We have developed a robust collaborative HM POCUS program. We have noted challenges in motivating all providers to work through this protocol. Development of a POCUS program takes dedicated time, and without a champion, it is at risk for failing. HM departments would be advised to seek out willing collaborators at their institutions. We have seen that it is useful to partner with some experienced emergency medicine providers. Additionally, portfolio development and feedback has been key to demonstrating growth in image acquisition. Deliberate longitudinal practice with feedback and successive refinements with POCUS obtain the highest yield towards competency. We hope our QA data will provide further feedback into the credentialing policy and procedure.
SUMMARY
It is important that POCUS users work together to recognize its potential and limitations, teach current and future care providers’ best practices, and create an infrastructure that maximizes quality of care while minimizing patient risk.
We are hopeful that this document will prove beneficial to other HM departments in the development of successful POCUS programs. We feel that it is important to make available to other HM departments a concise protocol that has successfully passed through the credentialing process at a large tertiary care medical system.
Acknowledgments
The authors would like to acknowledge Susan Truman, MD, for her contributions to the success of the POCUS committee at Regions Hospital. The authors would like to acknowledge Kreegan Reierson, MD, Ankit Mehta, MBBS, and Khuong Vuong, MD for their contributions to the success of POCUS within hospital medicine at HealthPartners. The authors would like to acknowledge Sandi Wewerka, MPH, for her review and input of this manuscript.
Disclosure
The authors do not have any relevant financial disclosures to report.
Ultrasound has been used for decades by radiology, obstetrics-gynecology, and cardiology departments within a comprehensive paradigm in which a physician enters an order, then a trained sonographer performs the study, followed by a physician evaluating and interpreting the images.1 Unlike the traditional comprehensive paradigm, point-of-care ultrasound (POCUS) is a focused study that is both performed and interpreted by the bedside provider.2 POCUS has been demonstrated to improve diagnosis and clinical management in multiple studies.3-15
The scope of practice in POCUS differs by specialty, as POCUS is done to achieve specific procedural aims (eg, direct the needle to the correct location) or answer focused questions (eg, does the patient have a distended bladder?) related to the specialty. POCUS in hospital medicine (HM) provides immediate answers, without the delay and potential risk of transportation to other hospital areas. It may be used to diagnose pleural effusion, pneumonia, hydronephrosis, heart failure, deep vein thrombosis, and many other pathologies.5-15 It is important to understand that POCUS performed by HM is a limited study and is not a substitute for more complete ultrasound examinations conducted in the radiology suite or in the echocardiography lab.
POCUS should not be used exclusively in medical decision making, but rather in conjunction with the greater clinical context of each patient, building on established principles of diagnosis and management.
DEFINITIONS
- Credentialing: An umbrella term, which incorporates licensure, education, and certification.
- Privileging: Used to define the scope authorized for a provider by a healthcare organization based on an evaluation of the individual’s credentials and performance.
- Competency: An observable ability of a provider, integrating multiple components, such as knowledge and skills. Since competencies are observable, they can be measured and assessed to ensure their acquisition.
- Certification: The process by which an association grants recognition to a provider who has met certain predetermined qualifications specified by the association. Competence is distinguished from certification, which is defined as the process by which competence is recognized by an external agency.
All of the above mechanisms work together to provide the highest quality of reliability that a practitioner is providing safe, competent care.16-18
STATEMENTS FROM MAJOR SPECIALTY SOCIETIES
Acknowledging that there are no published guidelines in the realm of HM POCUS, the development of the credentialing process at our institution is consistent with published guidelines by Emergency Medicine societies (the most established physician users of POCUS) and the American Medical Association (AMA).19-21
The use of emergency ultrasound by physicians in the emergency department is endorsed by the American College of Emergency Physicians (ACEP).19 ACEP, along with the Society of Academic Emergency Medicine (SAEM), recommends that training in the performance and interpretation of ultrasound imaging be included during residency.20 ACEP and SAEM add that the availability of equivalent training should be made available to practicing physicians. The American Society of Echocardiography has supported the use of POCUS and sees this modality as part of the continuum of care.23,24
The AMA has also recognized that POCUS is within the scope of practice of trained physicians.22 The AMA further recommended hospital staff create their own criteria for granting ultrasound privileges based on the background and training of the physician and in accordance with the standards set within specific specialties.22,23
LOCAL POLICY AND PROCEDURE
The provision of clinical privileges in HM is governed by the rules and regulations of the department and institution for which privileges are sought. In detailing our policies and procedures above, we intend to provide an example for HM departments at other institutions that are attempting to create a POCUS credentialing program.
An interdisciplinary approach was created by our institution to address training, competency, and ongoing quality assurance (QA) concerns due to the increasing popularity of POCUS and variability in its use. We developed a hospital-wide POCUS committee with, among others, members from HM, emergency medicine, critical care, radiology, and cardiology, with a charter to standardize POCUS across departments. After review of the literature,16-18, 20, 21, 23-74 baseline training requirements were established for credentialing and developing a unified delineation of privileges for hospital-wide POCUS. The data support the use of a variety of assessments to ensure a provider has developed competence (portfolio development, knowledge-based examination, skills-based assessment, ongoing QA process). The POCUS committee identified which exams could be performed at bedside for credentialed providers, delineated imaging requirements for each exam, and set up the information technology infrastructure to support ordering and reporting through electronic health records (EHR). While the POCUS committee delineated this process for all hospital providers, we will focus our discussion on the credentialing policy and procedure in HM.
STEP 1: PATHWAY TO POCUS CREDENTIALING IN HM: COMPLETE MINIMAL FORMAL REQUIREMENTS
The credentialing requirements at our institution include one of the the following basic education pathways and minimal formal training:
Residency/Fellowship Based Pathway
Completed training in an Accreditation Council for Graduate Medical Education–approved program that provided opportunities for 20 hours of POCUS training with at least 6 hours of hands-on ultrasound scanning, 5 proctored limited cardiac ultrasound cases and portfolio development.
Practice Based Pathway
Completed 20 hours of POCUS continuing medical education (CME) with at least 6 hours of hands-on ultrasound scanning and has completed 5 proctored limited cardiac ultrasound cases (as part of CME).
The majority of HM providers had little formal residency training in POCUS, so a training program needed to be developed. Our training program, modeled after the American College of Chest Physicians’ CHEST certificate of completion,86 utilizes didactic training, hands-on instruction, and portfolio development that fulfills the minimal formal requirements in the practice-based pathway.
STEP 2: PATHWAY TO POCUS CREDENTIALING IN HM: COMPLETE PORTFOLIO AND FINAL ASSESSMENTS (KNOWLEDGE AND SKILLS–BASED)
After satisfactory completion of the minimal formal training, applicants need to provide documentation of a set number of cases. To aid this requirement, our HM department developed the portfolio guidelines in the Table. These are minimum requirements, and because of the varying training curves of learning,76-80 1 hospitalist may need to submit 300 files for review to meet the standards, while another may need to submit 500 files. Submissions are not accepted unless they yield high-quality video files with meticulous attention to gain, depth, and appropriate topographic planes. The portfolio development monitors hospitalists’ progression during their deliberate practice, providing objective assessments, feedback, and mentorship.81,82
A final knowledge exam with case-based image interpretation and hands-on examination is also provided. The passing score for the written examination is 85% and was based on the Angoff methodology.75 Providers who meet these requirements are then able to apply for POCUS credentialing in HM. Providers who do not pass the final assessments are required to participate in further training before they reattempt the assessments. There is uniformity in training outcomes but diversity in training time for POCUS providers.
Candidates who complete the portfolio and satisfactorily pass the final assessments are credentialed after review by the POCUS committee. Credentialed physicians are then able to perform POCUS and to integrate the findings into patient care.
MAINTENANCE OF CREDENTIALS
Documentation
After credentialing is obtained, all POCUS studies used in patient care are included in the EHR following a clearly defined workflow. The study is ordered through the EHR and is retrieved wirelessly on the ultrasound machine. After performing the ultrasound, all images are wirelessly transferred to the radiology Picture Archiving and Communication System server. Standardized text reports are used to distinguish focused POCUS from traditional diagnostic ultrasound studies. Documentation is optimized using electronic drop-down menus for documenting ultrasound findings in the EHR.
Minimum Number of Examinations
Maintenance of credentials will require that each hospitalist perform 10 documented ultrasounds per year for each cardiac and noncardiac application for which credentials are requested. If these numbers are not met, then all the studies performed during the previous year will be reviewed by the ultrasound committee, and providers will be provided with opportunities to meet the minimum benchmark (supervised scanning sessions).
Quality Assurance
Establishing scope of practice, developing curricula, and credentialing criteria are important steps toward assuring provider competence.16,17,22,74 To be confident that providers are using POCUS appropriately, there must also be a development of standards of periodic assessment that encompass both examination performance and interpretation. The objective of a QA process is to evaluate the POCUS cases for technical competence and the interpretations for clinical accuracy, and to provide feedback to improve performance of providers.
QA is maintained through the interdisciplinary POCUS committee and is described in the Figure.
After initial credentialing, continued QA of HM POCUS is done for a proportion of ongoing exams (10% as per recommendations by ACEP) to document continued competency.2 Credentialed POCUS providers perform and document their exam and interpretations. Ultrasound interpretations are reviewed by the POCUS committee (every case by 2 physicians, 1 hospitalist, and 1 radiologist or cardiologist depending on the study type) at appropriate intervals based on volume (at minimum, quarterly). A standardized review form is used to grade images and interpretations. This is the same general rubric used with the portfolio for initial credentialing. Each case is scored on a scale of 1 to 6, with 1 representing high image quality and support for diagnosis and 6 representing studies limited by patient factors. All scores rated 4 or 5 are reviewed at the larger quarterly POCUS committee meetings. For any provider scoring a 4 or 5, the ultrasound committee will recommend a focused professional practice evaluation as it pertains to POCUS. The committee will also make recommendations on a physician’s continued privileges to the department leaders.83
BILLING
Coding, billing, and reimbursement for focused ultrasound has been supported through the AMA Physicians’ Current Procedural Terminology (CPT) 2011 codes, which includes CPT code modifiers for POCUS.84 There are significant costs associated with building a HM ultrasound program, including the education of hospitalists, ultrasound equipment purchase and maintenance, as well as image archiving and QA. The development of a HM ultrasound billing program can help justify and fund these costs.19,85
To appropriately bill for POCUS, permanently retrievable images and an interpretation document need to be available for review. HM coders are instructed to only bill if both components are available. Because most insurers will not pay for 2 of the same type of study performed within a 24-hour period, coders do not bill for ultrasounds when a comprehensive ultrasound of the same body region is performed within a 24-hour period. The workflow that we have developed, including ordering, performing, and documenting, allows for easy coding and billing.
BARRIERS AND LIMITATIONS
While POCUS has a well-established literature base in other specialties like emergency medicine, it has been a relatively recent addition to the HM specialty. As such, there exists a paucity of evidence-based medicine to support its use of POCUS in HM. While it is tempting to extrapolate from the literature of other specialties, this may not be a valid approach.
Training curves in which novice users of ultrasound become competent in specific applications are incompletely understood. Little research describes the rate of progression of learners in ultrasound towards competency. We have recently started the QA process and hope that the data will further guide feedback to the process.
Additionally, with the portfolios, the raters’ expertise may not be stable (develops through experience). We aim to mitigate this by having a group of raters reviewing each file, particularly if there is a question about if a submission is of high image quality. A notable barrier that groups face is support from their leadership regarding POCUS. Our group has had support from the chief medical officer who helped mandate the development of POCUS standards.
LESSONS LEARNED
We have developed a robust collaborative HM POCUS program. We have noted challenges in motivating all providers to work through this protocol. Development of a POCUS program takes dedicated time, and without a champion, it is at risk for failing. HM departments would be advised to seek out willing collaborators at their institutions. We have seen that it is useful to partner with some experienced emergency medicine providers. Additionally, portfolio development and feedback has been key to demonstrating growth in image acquisition. Deliberate longitudinal practice with feedback and successive refinements with POCUS obtain the highest yield towards competency. We hope our QA data will provide further feedback into the credentialing policy and procedure.
SUMMARY
It is important that POCUS users work together to recognize its potential and limitations, teach current and future care providers’ best practices, and create an infrastructure that maximizes quality of care while minimizing patient risk.
We are hopeful that this document will prove beneficial to other HM departments in the development of successful POCUS programs. We feel that it is important to make available to other HM departments a concise protocol that has successfully passed through the credentialing process at a large tertiary care medical system.
Acknowledgments
The authors would like to acknowledge Susan Truman, MD, for her contributions to the success of the POCUS committee at Regions Hospital. The authors would like to acknowledge Kreegan Reierson, MD, Ankit Mehta, MBBS, and Khuong Vuong, MD for their contributions to the success of POCUS within hospital medicine at HealthPartners. The authors would like to acknowledge Sandi Wewerka, MPH, for her review and input of this manuscript.
Disclosure
The authors do not have any relevant financial disclosures to report.
1. Soni NJ, Nilam J, Arntfield R, Kory P. Point of Care Ultrasound. Philadelphia:
Elsevier; 2015.
2. Moore CL, Copel JA. Point-of-Care Ultrasonography. N Engl J Med.
2011;364(8):749-757. PubMed
3. Randolph AG, Cook DJ, Gonzales CA, et al. Ultrasound guidance for placement
of central venous catheters: A meta-analysis of the literature. Crit Care Med.
1996;24:2053-2058. PubMed
4. Gordon CE, Feller-Kopman D, Balk EM, et al. Pneumothorax following thoracentesis:
A systematic review and meta-analysis. Arch Intern Med. 2010;170:332-339. PubMed
5. Soni NJ, Nilam J, Franco R, et al. Ultrasound in the diagnosis and management of
pleural effusions. J Hosp Med. 2015;10(12):811-816. PubMed
6. Nazerian P, Volpicelli G, Gigli C, et al. Diagnostic performance of Wells score
combined with point-of-care lung and venous ultrasound in suspected pulmonary
embolism. Acad Emerg Med. 2017;24(3):270-280. PubMed
7. Chatziantoniou A, Nazerian P, Vanni S, et al. A combination of the Wells score
with multiorgan ultrasound to stratify patients with suspected pulmonary embolism.
Eur Respir J. 2015;46:OA493; DOI:10.1183/13993003.congress-2015.
OA493.
8. Boyd JH, Sirounis D, Maizel J, Slama M. Echocardiography as a guide for fluid
management. Crit Care. 2016; DOI:10.1186/s13054-016-1407-1. PubMed
9. Mantuani D, Frazee BW, Fahimi J, Nagdev A. Point-of-Care Multi-Organ Ultrasound
Improves Diagnostic Accuracy in Adults Presenting to the Emergency
Department with Acute Dyspnea. West J Emerg Med. 2016;17(1):46-53. PubMed
10. Glockner E, Christ M, Geier F, et al. Accuracy of Point-of-Care B-Line Lung
Ultrasound in Comparison to NT-ProBNP for Screening Acute Heart Failure.
Ultrasound Int Open. 2016;2(3):e90-e92. PubMed
11. Bhagra A, Tierney DM, Sekiguchi H, Soni NJ. Point-of-Care Ultrasonography
for Primary Care Physicians and General Internists. Mayo Clin Proc.
2016;91(12):1811-1827. PubMed
12. Crisp JG, Lovato LM, and Jang TB. Compression ultrasonography of the lower extremity
with portable vascular ultrasonography can accurately detect deep venous
thrombosis in the emergency department. Ann Emerg Med. 2010;56:601-610. PubMed
13. Squire BT, Fox JC, and Anderson C. ABSCESS: Applied bedside sonography
for convenient. Evaluation of superficial soft tissue infections. Acad Emerg Med.
2005;12:601-606. PubMed
14. Narasimhan M, Koenig SJ, Mayo PH. A Whole-Body Approach to Point of Care
Ultrasound. Chest. 2016;150(4):772-776. PubMed
15. Oks M, Cleven KL, Cardenas-Garcia J, et al. The effect of point-of-care ultrasonography
on imaging studies in the medical ICU: a comparative study. Chest.
2014;146(6):1574-1577. PubMed
16. Mayo PH, Beaulieu Y, Doelken P, et al. American College of Chest Physicians/
La Société de Réanimation de Langue Française Statement on Competence in
Critical Care Ultrasonography. Chest. 2009;135(4):1050-1060. PubMed
17. Frank JR, Snell LS, Ten Cate O, et al. Competency-based medical education:
Theory to practice. Med Teach. 2010;32:638-645. PubMed
18. The Who, What, When, and Where’s of Credentialing and Privileging. The
Joint Commission. http://www.jointcommission.org/assets/1/6/AHC_who_what_
when_and_where_credentialing_booklet.pdf. Accessed December 21, 2016.
19. American College of Emergency Physicians Policy Statement: Emergency Ultrasound
Guidelines. 2016. https://www.acep.org/Clinical---Practice-Management/
ACEP-Ultrasound-Guidelines/. Accessed October 26, 2016.
20. Society for Academic Emergency Medicine. Ultrasound Position Statement. Annual
Meeting 1996.
21. American Medical Association. Privileging for ultrasound imaging. 2001; Policy
H-230.960. www.ama-assn.org. Accessed July 28, 2017 PubMed
22. Stein JC, Nobay F. Emergency Department Ultrasound Credentialing: a sample
policy and procedure. J Emerg Med. 2009;37(2):153-159. PubMed
23. Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ. Focused
Cardiac Ultrasound: Recommendations from the American Society of Echocardiography.
J Am Soc Echocardiogr. 2013;26(6):567-581. PubMed
24. Wiegers S. The Point of Care. J Am Soc Echocardiogr. 2016;29(4):19. PubMed
25. Mandavia D, Aragona J, Chan L, et al. Ultrasound training for emergency physicians—
a prospective study. Acad Emerg Med. 2000;7:1008-1014. PubMed
26. American College of Radiology Practice Parameters and Technical Standards.
https://www.acr.org/quality-safety/standards-guidelines. Accessed December 21, 2016.
27. Blois B. Office-based ultrasound screening for abdominal aortic aneurysm. Can
Fam Physician. 2012;58(3):e172-e178. PubMed
28. Rubano E, Mehta N, Caputo W, Paladino L, Sinert R. Systematic review: emergency
department bedside ultrasonography for diagnosing suspected abdominal
aortic aneurysm. Acad Emerg Med. 2013;20:128-138. PubMed
29. Dijos M, Pucheux Y, Lafitte M, et al. Fast track echo of abdominal aortic aneurysm
using a real pocket-ultrasound device at bedside. Echocardiography. PubMed
2012;29(3):285-290.
30. Cox C, MacDonald S, Henneberry R, Atkinson PR. My patient has abdominal
and flank pain: Identifying renal causes. Ultrasound. 2015;23(4):242-250. PubMed
31. Gaspari R, Horst K. Emergency ultrasound and urinalysis in the evaluation of
patients with flank pain. Acad Emerg Med. 2005;12:1180-1184. PubMed
32. Kartal M, Eray O, Erdogru T, et al. Prospective validation of a current algorithm
including bedside US performed by emergency physicians for patients with acute
flank pain suspected for renal colic. Emerg Med J. 2006;23(5):341-344. PubMed
33. Noble VE, Brown DF. Renal ultrasound. Emerg Med Clin North Am. 2004;22:641-659. PubMed
34. Surange R, Jeygopal NS, Chowdhury SD, et al. Bedside ultrasound: a useful tool
for the on call urologist? Int Urol Nephrol. 2001;32:591-596. PubMed
35. Pomero F, Dentali F, Borretta V, et al. Accuracy of emergency physician-performed
ultrasonography in the diagnosis of deep-vein thrombosis. Thromb Haemost.
2013;109(1):137-145. PubMed
36. Bernardi E, Camporese G, Buller HR, et al. Erasmus Study Group. Serial 2-Point
Ultrasonography Plus D-Dimer vs Whole-Leg Color-Coded Doppler Ultrasonography
for Diagnosing Suspected Symptomatic Deep Vein Thrombosis: A Randomized
Controlled Trial. JAMA. 2008;300(14):1653-1659. PubMed
37. Burnside PR, Brown MD, Kline JA. Systematic Review of Emergency Physician–
performed Ultrasonography for Lower-Extremity Deep Vein Thrombosis. Acad
Emerg Med. 2008;15:493-498. PubMed
38. Magazzini S, Vanni S, Toccafondi S, et al. Duplex ultrasound in the emergency
department for the diagnostic management of clinically suspected deep vein
thrombosis. Acad Emerg Med. 2007;14:216-220. PubMed
39. Jacoby J, Cesta M, Axelband J, Melanson S, Heller M, Reed J. Can emergency
medicine residents detect acute deep venous thrombosis with a limited, two-site
ultrasound examination? J Emerg Med. 2007;32:197-200. PubMed
40. Jang T, Docherty M, Aubin C, Polites G. Resident-performed compression ultrasonography
for the detection of proximal deep vein thrombosis: fast and accurate.
Acad Emerg Med. 2004;11:319-322. PubMed
41. Frazee BW, Snoey ER, Levitt A. Emergency Department compression ultrasound
to diagnose proximal deep vein thrombosis. J Emerg Med. 2001;20:107-112. PubMed
42. Blaivas M, Lambert MJ, Harwood RA, Wood JP, Konicki J. Lower-extremity Doppler
for deep venous thrombosis--can emergency physicians be accurate and fast?
Acad Emerg Med. 2000;7:120-126. PubMed
43. Koenig SJ, Narasimhan M, Mayo PH. Thoracic ultrasonography for the pulmonary
specialist. Chest. 2011;140(5):1332-1341. PubMed
44. Lichtenstein, DA. A bedside ultrasound sign ruling out pneumothorax in the critically
ill. Lung sliding. Chest. 1995;108(5):1345-1348. PubMed
45. Lichtenstein D, Mézière G, Biderman P, Gepner A, Barré O. The comet-tail artifact.
An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care
Med. 1997;156(5):1640-1646. PubMed
46. Copetti R, Soldati G, Copetti P. Chest sonography: a useful tool to differentiate
acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc
Ultrasound. 2008;6:16. PubMed
47. Agricola E, Bove T, Oppizzi M, et al. Ultrasound comet-tail images: a marker
of pulmonary edema: a comparative study with wedge pressure and extravascular
lung water. Chest. 2005;127(5):1690-1695. PubMed
48. Lichtenstein DA, Meziere GA, Laqoueyte JF, Biderman P, Goldstein I, Gepner A.
A-lines and B-lines: lung ultrasound as a bedside tool for predicting pulmonary
artery occlusion pressure in the critically ill. Chest. 2009;136(4):1014-1020. PubMed
49. Lichtenstein DA, Lascols N, Meziere G, Gepner A. Ultrasound diagnosis of alveolar
consolidation in the critically ill. Intensive Care Med. 2004;30(2):276-281. PubMed
50. Lichtenstein D, Mezière G, Seitz J. The dynamic air bronchogram. A lung
ultrasound sign of alveolar consolidation ruling out atelectasis. Chest.
2009;135(6):1421–1425. PubMed
51. Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ. Comparative
diagnostic performances of auscultation, chest radiography, and lung ultrasonography
in acute respiratory distress syndrome. Anesthesiology. 2004;100(1):9-15. PubMed
52. Lichtenstein D, Meziere G. Relevance of lung ultrasound in the diagnosis of acute
respiratory failure: the BLUE protocol. Chest. 2008;134(1):117-125. PubMed
53. Mayo P, Doelken P. Pleural ultrasonography. Clin Chest Med. 2006;27(2):215-227. PubMed
54. Galderisi M, Santoro A, Versiero M, et al. Improved cardiovascular diagnostic accuracy
by pocket size imaging device in non-cardiologic outpatients: the NaUSi-
Ca (Naples Ultrasound Stethoscope in Cardiology) study. Cardiovasc Ultrasound.
2010;8:51. PubMed
55. DeCara JM, Lang RM, Koch R, Bala R, Penzotti J, Spencer KT. The use of small
personal ultrasound devices by internists without formal training in echocardiography.
Eur J Echocardiography. 2002;4:141-147. PubMed
56. Martin LD, Howell EE, Ziegelstein RC, Martire C, Shapiro EP, Hellmann DB.
Hospitalist performance of cardiac hand-carried ultrasound after focused training.
Am J Med. 2007;120:1000-1004. PubMed
57. Martin LD, Howell EE, Ziegelstein RC, et al. Hand-carried ultrasound performed
by hospitalists: does it improve the cardiac physical examination? Am J Med.
2009;122:35-41. PubMed
58. Perez-Avraham G, Kobal SL, Etzion O, et al. Left ventricular geometric abnormality
screening in hypertensive patients using a hand-carried ultrasound device.
J Clin Hypertens. 2010;12:181-186. PubMed
59. Lucas BP, Candotti C, Margeta B, et al. Diagnostic accuracy of hospitalist-performed
hand-carried ultrasound echocardiography after a brief training program. J
Hosp Med. 2009;4:340-349. PubMed
60. Kimura BJ, Fowler SJ, Fergus TS, et al. Detection of left atrial enlargement using
hand-carried ultrasound devices to screen for cardiac abnormalities. Am J Med.
2005;118:912-916. PubMed
61. Brennan JM, Blair JE, Goonewardena S, et al. A comparison by medicine residents of physical examination versus hand-carried ultrasound for estimation of
right atrial pressure. Am J Cardiol. 2007;99:1614-1616. PubMed
62. Blair JE, Brennan JM, Goonewardena SN, Shah D, Vasaiwala S, Spencer KT.
Usefulness of hand-carried ultrasound to predict elevated left ventricular filling
pressure. Am J Cardiol. 2009;103:246-247. PubMed
63. Stawicki SP, Braslow BM, Panebianco NL, et al. Intensivist use of hand-carried
ultrasonography to measure IVC collapsibility in estimating intravascular volume
status: correlations with CVP. J Am Coll Surg. 2009;209:55-61. PubMed
64. Gunst M, Ghaemmaghami V, Sperry J, et al. Accuracy of cardiac function and volume
status estimates using the bedside echocardiographic assessment in trauma/
critical care. J Trauma. 2008;65:509-515. PubMed
65. Razi R, Estrada JR, Doll J, Spencer KT. Bedside hand-carried ultrasound by internal
medicine residents versus traditional clinical assessment for the identification
of systolic dysfunction in patients admitted with decompensated heart failure. J
Am Soc Echocardiogr. 2011;24:1319-1324. PubMed
66. Croft LB, Duvall WL, Goldman ME. A pilot study of the clinical impact
of hand-carried cardiac ultrasound in the medical clinic. Echocardiography.
2006;23:439-446. PubMed
67. Vignon P, Dugard A, Abraham J, et al. Focused training for goal-oriented handheld
echocardiography performed by noncardiologist residents in the intensive
care unit. Intensive Care Med. 2007;33:1795-1799. PubMed
68. Melamed R, Sprenkle MD, Ulstad VK, Herzog CA, Leatherman JW. Assessment
of left ventricular function by intensivists using hand-held echocardiography.
Chest. 2009;135:1416-1420. PubMed
69. Mark DG, Hayden GE, Ky B, et al. Hand-carried echocardiography for assessment
of left ventricular filling and ejection fraction in the surgical intensive care unit. J
Crit Care. 2009;24(3):470.e1-470.e7. PubMed
70. Kirkpatrick JN, Davis A, Decara JM, et al. Hand-carried cardiac ultrasound as a
tool to screen for important cardiovascular disease in an underserved minority
health care clinic. J Am Soc Echocardiogr. 2004;17:399-403. PubMed
71. Fedson S, Neithardt G, Thomas P, et al. Unsuspected clinically important findings
detected with a small portable ultrasound device in patients admitted to a general
medicine service. J Am Soc Echocardiogr. 2003;16:901-905. PubMed
72. Ghani SN, Kirkpatrick JN, Spencer, KT, et al. Rapid assessment of left ventricular
systolic function in a pacemaker clinic using a hand-carried ultrasound device.
J Interv Card Electrophysiol. 2006;16:39-43. PubMed
73. Kirkpatrick JN, Ghani SN, Spencer KT. Hand carried echocardiography
screening for LV systolic dysfunction in a pulmonary function laboratory.
Eur J Echocardiogr. 2008;9:381-383. PubMed
74. Alexander JH, Peterson ED, Chen AY, Harding TM, Adams DB, Kisslo JA Jr.
Feasibility of point-of-care echocardiography by internal medicine house staff. Am
Heart J. 2004;147:476-481. PubMed
75. Angoff WH. Scales, norms and equivalent Scores. Washington, DC: American
Council on Education; 1971.
76. Hellmann DB, Whiting-O’Keefe Q, Shapiro EP, Martin LD, Martire C, Ziegelstein
RC. The rate at which residents learn to use hand-held echocardiography at
the bedside. Am J Med. 2005;118:1010-1018. PubMed
77. Kimura BJ, Amundson SA, Phan JN, Agan DL, Shaw DJ. Observations during
development of an internal medicine residency training program in cardiovascular
limited ultrasound examination. J Hosp Med. 2012;7:537-542. PubMed
78. Akhtar S, Theodoro D, Gaspari R, et al. Resident training in emergency ultrasound:
consensus recommendations from the 2008 Council of Emergency Medicine
Residency Directors Conference. Acad Emerg Med. 2009;16(s2):S32-S36. PubMed
79. Ma OJ, Gaddis G, Norvell JG, Subramanian S. How fast is the focused assessment
with sonography for trauma examination learning curve? Emerg Med Australas.
2008;20(1):32-37. PubMed
80. Gaspari RJ, Dickman E, Blehar D. Learning curve of bedside ultrasound of the gallbladder. J Emerg Med. 2009;37(1):51-56. DOI:10.1016/j.jemermed.2007.10.070. PubMed
81. Ericsson KA, Lehmann AC. Expert and exceptional performance: Evidence of
maximal adaptation to task constraints. Ann Rev Psychol. 1996;47:273-305. PubMed
82. Ericcson KA, Krampe RT, Tesch-Romer C. The role of deliberate practice in the
acquisition of expert performance. Psychol Rev. 1993;100:363-406.
83. OPPE and FPPE: Tools to help make privileging decisions. The Joint Commission.
2013. http://www.jointcommission.org/jc_physician_blog/oppe_fppe_tools_privileging_
decisions/ Accessed October 26, 2016.
84. American Medical Association. Physicians’ Current Procedural Terminology (CPT)
2011. American Medical Association, Chicago; 2011.
85. Moore CL, Gregg S, Lambert M. Performance, training, quality assurance, and
reimbursement of emergency physician-performed ultrasonography at academic
medical centers. J Ultrasound Med. 2004;23(4):459-466. PubMed
86. Critical Care Ultrasonography Certificate of Completion Program. CHEST.
American College of Chest Physicians. http://www.chestnet.org/Education/Advanced-
Clinical-Training/Certificate-of-Completion-Program/Critical-Care-Ultrasonography.
Accessed July 28, 2017.
1. Soni NJ, Nilam J, Arntfield R, Kory P. Point of Care Ultrasound. Philadelphia:
Elsevier; 2015.
2. Moore CL, Copel JA. Point-of-Care Ultrasonography. N Engl J Med.
2011;364(8):749-757. PubMed
3. Randolph AG, Cook DJ, Gonzales CA, et al. Ultrasound guidance for placement
of central venous catheters: A meta-analysis of the literature. Crit Care Med.
1996;24:2053-2058. PubMed
4. Gordon CE, Feller-Kopman D, Balk EM, et al. Pneumothorax following thoracentesis:
A systematic review and meta-analysis. Arch Intern Med. 2010;170:332-339. PubMed
5. Soni NJ, Nilam J, Franco R, et al. Ultrasound in the diagnosis and management of
pleural effusions. J Hosp Med. 2015;10(12):811-816. PubMed
6. Nazerian P, Volpicelli G, Gigli C, et al. Diagnostic performance of Wells score
combined with point-of-care lung and venous ultrasound in suspected pulmonary
embolism. Acad Emerg Med. 2017;24(3):270-280. PubMed
7. Chatziantoniou A, Nazerian P, Vanni S, et al. A combination of the Wells score
with multiorgan ultrasound to stratify patients with suspected pulmonary embolism.
Eur Respir J. 2015;46:OA493; DOI:10.1183/13993003.congress-2015.
OA493.
8. Boyd JH, Sirounis D, Maizel J, Slama M. Echocardiography as a guide for fluid
management. Crit Care. 2016; DOI:10.1186/s13054-016-1407-1. PubMed
9. Mantuani D, Frazee BW, Fahimi J, Nagdev A. Point-of-Care Multi-Organ Ultrasound
Improves Diagnostic Accuracy in Adults Presenting to the Emergency
Department with Acute Dyspnea. West J Emerg Med. 2016;17(1):46-53. PubMed
10. Glockner E, Christ M, Geier F, et al. Accuracy of Point-of-Care B-Line Lung
Ultrasound in Comparison to NT-ProBNP for Screening Acute Heart Failure.
Ultrasound Int Open. 2016;2(3):e90-e92. PubMed
11. Bhagra A, Tierney DM, Sekiguchi H, Soni NJ. Point-of-Care Ultrasonography
for Primary Care Physicians and General Internists. Mayo Clin Proc.
2016;91(12):1811-1827. PubMed
12. Crisp JG, Lovato LM, and Jang TB. Compression ultrasonography of the lower extremity
with portable vascular ultrasonography can accurately detect deep venous
thrombosis in the emergency department. Ann Emerg Med. 2010;56:601-610. PubMed
13. Squire BT, Fox JC, and Anderson C. ABSCESS: Applied bedside sonography
for convenient. Evaluation of superficial soft tissue infections. Acad Emerg Med.
2005;12:601-606. PubMed
14. Narasimhan M, Koenig SJ, Mayo PH. A Whole-Body Approach to Point of Care
Ultrasound. Chest. 2016;150(4):772-776. PubMed
15. Oks M, Cleven KL, Cardenas-Garcia J, et al. The effect of point-of-care ultrasonography
on imaging studies in the medical ICU: a comparative study. Chest.
2014;146(6):1574-1577. PubMed
16. Mayo PH, Beaulieu Y, Doelken P, et al. American College of Chest Physicians/
La Société de Réanimation de Langue Française Statement on Competence in
Critical Care Ultrasonography. Chest. 2009;135(4):1050-1060. PubMed
17. Frank JR, Snell LS, Ten Cate O, et al. Competency-based medical education:
Theory to practice. Med Teach. 2010;32:638-645. PubMed
18. The Who, What, When, and Where’s of Credentialing and Privileging. The
Joint Commission. http://www.jointcommission.org/assets/1/6/AHC_who_what_
when_and_where_credentialing_booklet.pdf. Accessed December 21, 2016.
19. American College of Emergency Physicians Policy Statement: Emergency Ultrasound
Guidelines. 2016. https://www.acep.org/Clinical---Practice-Management/
ACEP-Ultrasound-Guidelines/. Accessed October 26, 2016.
20. Society for Academic Emergency Medicine. Ultrasound Position Statement. Annual
Meeting 1996.
21. American Medical Association. Privileging for ultrasound imaging. 2001; Policy
H-230.960. www.ama-assn.org. Accessed July 28, 2017 PubMed
22. Stein JC, Nobay F. Emergency Department Ultrasound Credentialing: a sample
policy and procedure. J Emerg Med. 2009;37(2):153-159. PubMed
23. Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ. Focused
Cardiac Ultrasound: Recommendations from the American Society of Echocardiography.
J Am Soc Echocardiogr. 2013;26(6):567-581. PubMed
24. Wiegers S. The Point of Care. J Am Soc Echocardiogr. 2016;29(4):19. PubMed
25. Mandavia D, Aragona J, Chan L, et al. Ultrasound training for emergency physicians—
a prospective study. Acad Emerg Med. 2000;7:1008-1014. PubMed
26. American College of Radiology Practice Parameters and Technical Standards.
https://www.acr.org/quality-safety/standards-guidelines. Accessed December 21, 2016.
27. Blois B. Office-based ultrasound screening for abdominal aortic aneurysm. Can
Fam Physician. 2012;58(3):e172-e178. PubMed
28. Rubano E, Mehta N, Caputo W, Paladino L, Sinert R. Systematic review: emergency
department bedside ultrasonography for diagnosing suspected abdominal
aortic aneurysm. Acad Emerg Med. 2013;20:128-138. PubMed
29. Dijos M, Pucheux Y, Lafitte M, et al. Fast track echo of abdominal aortic aneurysm
using a real pocket-ultrasound device at bedside. Echocardiography. PubMed
2012;29(3):285-290.
30. Cox C, MacDonald S, Henneberry R, Atkinson PR. My patient has abdominal
and flank pain: Identifying renal causes. Ultrasound. 2015;23(4):242-250. PubMed
31. Gaspari R, Horst K. Emergency ultrasound and urinalysis in the evaluation of
patients with flank pain. Acad Emerg Med. 2005;12:1180-1184. PubMed
32. Kartal M, Eray O, Erdogru T, et al. Prospective validation of a current algorithm
including bedside US performed by emergency physicians for patients with acute
flank pain suspected for renal colic. Emerg Med J. 2006;23(5):341-344. PubMed
33. Noble VE, Brown DF. Renal ultrasound. Emerg Med Clin North Am. 2004;22:641-659. PubMed
34. Surange R, Jeygopal NS, Chowdhury SD, et al. Bedside ultrasound: a useful tool
for the on call urologist? Int Urol Nephrol. 2001;32:591-596. PubMed
35. Pomero F, Dentali F, Borretta V, et al. Accuracy of emergency physician-performed
ultrasonography in the diagnosis of deep-vein thrombosis. Thromb Haemost.
2013;109(1):137-145. PubMed
36. Bernardi E, Camporese G, Buller HR, et al. Erasmus Study Group. Serial 2-Point
Ultrasonography Plus D-Dimer vs Whole-Leg Color-Coded Doppler Ultrasonography
for Diagnosing Suspected Symptomatic Deep Vein Thrombosis: A Randomized
Controlled Trial. JAMA. 2008;300(14):1653-1659. PubMed
37. Burnside PR, Brown MD, Kline JA. Systematic Review of Emergency Physician–
performed Ultrasonography for Lower-Extremity Deep Vein Thrombosis. Acad
Emerg Med. 2008;15:493-498. PubMed
38. Magazzini S, Vanni S, Toccafondi S, et al. Duplex ultrasound in the emergency
department for the diagnostic management of clinically suspected deep vein
thrombosis. Acad Emerg Med. 2007;14:216-220. PubMed
39. Jacoby J, Cesta M, Axelband J, Melanson S, Heller M, Reed J. Can emergency
medicine residents detect acute deep venous thrombosis with a limited, two-site
ultrasound examination? J Emerg Med. 2007;32:197-200. PubMed
40. Jang T, Docherty M, Aubin C, Polites G. Resident-performed compression ultrasonography
for the detection of proximal deep vein thrombosis: fast and accurate.
Acad Emerg Med. 2004;11:319-322. PubMed
41. Frazee BW, Snoey ER, Levitt A. Emergency Department compression ultrasound
to diagnose proximal deep vein thrombosis. J Emerg Med. 2001;20:107-112. PubMed
42. Blaivas M, Lambert MJ, Harwood RA, Wood JP, Konicki J. Lower-extremity Doppler
for deep venous thrombosis--can emergency physicians be accurate and fast?
Acad Emerg Med. 2000;7:120-126. PubMed
43. Koenig SJ, Narasimhan M, Mayo PH. Thoracic ultrasonography for the pulmonary
specialist. Chest. 2011;140(5):1332-1341. PubMed
44. Lichtenstein, DA. A bedside ultrasound sign ruling out pneumothorax in the critically
ill. Lung sliding. Chest. 1995;108(5):1345-1348. PubMed
45. Lichtenstein D, Mézière G, Biderman P, Gepner A, Barré O. The comet-tail artifact.
An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care
Med. 1997;156(5):1640-1646. PubMed
46. Copetti R, Soldati G, Copetti P. Chest sonography: a useful tool to differentiate
acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc
Ultrasound. 2008;6:16. PubMed
47. Agricola E, Bove T, Oppizzi M, et al. Ultrasound comet-tail images: a marker
of pulmonary edema: a comparative study with wedge pressure and extravascular
lung water. Chest. 2005;127(5):1690-1695. PubMed
48. Lichtenstein DA, Meziere GA, Laqoueyte JF, Biderman P, Goldstein I, Gepner A.
A-lines and B-lines: lung ultrasound as a bedside tool for predicting pulmonary
artery occlusion pressure in the critically ill. Chest. 2009;136(4):1014-1020. PubMed
49. Lichtenstein DA, Lascols N, Meziere G, Gepner A. Ultrasound diagnosis of alveolar
consolidation in the critically ill. Intensive Care Med. 2004;30(2):276-281. PubMed
50. Lichtenstein D, Mezière G, Seitz J. The dynamic air bronchogram. A lung
ultrasound sign of alveolar consolidation ruling out atelectasis. Chest.
2009;135(6):1421–1425. PubMed
51. Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ. Comparative
diagnostic performances of auscultation, chest radiography, and lung ultrasonography
in acute respiratory distress syndrome. Anesthesiology. 2004;100(1):9-15. PubMed
52. Lichtenstein D, Meziere G. Relevance of lung ultrasound in the diagnosis of acute
respiratory failure: the BLUE protocol. Chest. 2008;134(1):117-125. PubMed
53. Mayo P, Doelken P. Pleural ultrasonography. Clin Chest Med. 2006;27(2):215-227. PubMed
54. Galderisi M, Santoro A, Versiero M, et al. Improved cardiovascular diagnostic accuracy
by pocket size imaging device in non-cardiologic outpatients: the NaUSi-
Ca (Naples Ultrasound Stethoscope in Cardiology) study. Cardiovasc Ultrasound.
2010;8:51. PubMed
55. DeCara JM, Lang RM, Koch R, Bala R, Penzotti J, Spencer KT. The use of small
personal ultrasound devices by internists without formal training in echocardiography.
Eur J Echocardiography. 2002;4:141-147. PubMed
56. Martin LD, Howell EE, Ziegelstein RC, Martire C, Shapiro EP, Hellmann DB.
Hospitalist performance of cardiac hand-carried ultrasound after focused training.
Am J Med. 2007;120:1000-1004. PubMed
57. Martin LD, Howell EE, Ziegelstein RC, et al. Hand-carried ultrasound performed
by hospitalists: does it improve the cardiac physical examination? Am J Med.
2009;122:35-41. PubMed
58. Perez-Avraham G, Kobal SL, Etzion O, et al. Left ventricular geometric abnormality
screening in hypertensive patients using a hand-carried ultrasound device.
J Clin Hypertens. 2010;12:181-186. PubMed
59. Lucas BP, Candotti C, Margeta B, et al. Diagnostic accuracy of hospitalist-performed
hand-carried ultrasound echocardiography after a brief training program. J
Hosp Med. 2009;4:340-349. PubMed
60. Kimura BJ, Fowler SJ, Fergus TS, et al. Detection of left atrial enlargement using
hand-carried ultrasound devices to screen for cardiac abnormalities. Am J Med.
2005;118:912-916. PubMed
61. Brennan JM, Blair JE, Goonewardena S, et al. A comparison by medicine residents of physical examination versus hand-carried ultrasound for estimation of
right atrial pressure. Am J Cardiol. 2007;99:1614-1616. PubMed
62. Blair JE, Brennan JM, Goonewardena SN, Shah D, Vasaiwala S, Spencer KT.
Usefulness of hand-carried ultrasound to predict elevated left ventricular filling
pressure. Am J Cardiol. 2009;103:246-247. PubMed
63. Stawicki SP, Braslow BM, Panebianco NL, et al. Intensivist use of hand-carried
ultrasonography to measure IVC collapsibility in estimating intravascular volume
status: correlations with CVP. J Am Coll Surg. 2009;209:55-61. PubMed
64. Gunst M, Ghaemmaghami V, Sperry J, et al. Accuracy of cardiac function and volume
status estimates using the bedside echocardiographic assessment in trauma/
critical care. J Trauma. 2008;65:509-515. PubMed
65. Razi R, Estrada JR, Doll J, Spencer KT. Bedside hand-carried ultrasound by internal
medicine residents versus traditional clinical assessment for the identification
of systolic dysfunction in patients admitted with decompensated heart failure. J
Am Soc Echocardiogr. 2011;24:1319-1324. PubMed
66. Croft LB, Duvall WL, Goldman ME. A pilot study of the clinical impact
of hand-carried cardiac ultrasound in the medical clinic. Echocardiography.
2006;23:439-446. PubMed
67. Vignon P, Dugard A, Abraham J, et al. Focused training for goal-oriented handheld
echocardiography performed by noncardiologist residents in the intensive
care unit. Intensive Care Med. 2007;33:1795-1799. PubMed
68. Melamed R, Sprenkle MD, Ulstad VK, Herzog CA, Leatherman JW. Assessment
of left ventricular function by intensivists using hand-held echocardiography.
Chest. 2009;135:1416-1420. PubMed
69. Mark DG, Hayden GE, Ky B, et al. Hand-carried echocardiography for assessment
of left ventricular filling and ejection fraction in the surgical intensive care unit. J
Crit Care. 2009;24(3):470.e1-470.e7. PubMed
70. Kirkpatrick JN, Davis A, Decara JM, et al. Hand-carried cardiac ultrasound as a
tool to screen for important cardiovascular disease in an underserved minority
health care clinic. J Am Soc Echocardiogr. 2004;17:399-403. PubMed
71. Fedson S, Neithardt G, Thomas P, et al. Unsuspected clinically important findings
detected with a small portable ultrasound device in patients admitted to a general
medicine service. J Am Soc Echocardiogr. 2003;16:901-905. PubMed
72. Ghani SN, Kirkpatrick JN, Spencer, KT, et al. Rapid assessment of left ventricular
systolic function in a pacemaker clinic using a hand-carried ultrasound device.
J Interv Card Electrophysiol. 2006;16:39-43. PubMed
73. Kirkpatrick JN, Ghani SN, Spencer KT. Hand carried echocardiography
screening for LV systolic dysfunction in a pulmonary function laboratory.
Eur J Echocardiogr. 2008;9:381-383. PubMed
74. Alexander JH, Peterson ED, Chen AY, Harding TM, Adams DB, Kisslo JA Jr.
Feasibility of point-of-care echocardiography by internal medicine house staff. Am
Heart J. 2004;147:476-481. PubMed
75. Angoff WH. Scales, norms and equivalent Scores. Washington, DC: American
Council on Education; 1971.
76. Hellmann DB, Whiting-O’Keefe Q, Shapiro EP, Martin LD, Martire C, Ziegelstein
RC. The rate at which residents learn to use hand-held echocardiography at
the bedside. Am J Med. 2005;118:1010-1018. PubMed
77. Kimura BJ, Amundson SA, Phan JN, Agan DL, Shaw DJ. Observations during
development of an internal medicine residency training program in cardiovascular
limited ultrasound examination. J Hosp Med. 2012;7:537-542. PubMed
78. Akhtar S, Theodoro D, Gaspari R, et al. Resident training in emergency ultrasound:
consensus recommendations from the 2008 Council of Emergency Medicine
Residency Directors Conference. Acad Emerg Med. 2009;16(s2):S32-S36. PubMed
79. Ma OJ, Gaddis G, Norvell JG, Subramanian S. How fast is the focused assessment
with sonography for trauma examination learning curve? Emerg Med Australas.
2008;20(1):32-37. PubMed
80. Gaspari RJ, Dickman E, Blehar D. Learning curve of bedside ultrasound of the gallbladder. J Emerg Med. 2009;37(1):51-56. DOI:10.1016/j.jemermed.2007.10.070. PubMed
81. Ericsson KA, Lehmann AC. Expert and exceptional performance: Evidence of
maximal adaptation to task constraints. Ann Rev Psychol. 1996;47:273-305. PubMed
82. Ericcson KA, Krampe RT, Tesch-Romer C. The role of deliberate practice in the
acquisition of expert performance. Psychol Rev. 1993;100:363-406.
83. OPPE and FPPE: Tools to help make privileging decisions. The Joint Commission.
2013. http://www.jointcommission.org/jc_physician_blog/oppe_fppe_tools_privileging_
decisions/ Accessed October 26, 2016.
84. American Medical Association. Physicians’ Current Procedural Terminology (CPT)
2011. American Medical Association, Chicago; 2011.
85. Moore CL, Gregg S, Lambert M. Performance, training, quality assurance, and
reimbursement of emergency physician-performed ultrasonography at academic
medical centers. J Ultrasound Med. 2004;23(4):459-466. PubMed
86. Critical Care Ultrasonography Certificate of Completion Program. CHEST.
American College of Chest Physicians. http://www.chestnet.org/Education/Advanced-
Clinical-Training/Certificate-of-Completion-Program/Critical-Care-Ultrasonography.
Accessed July 28, 2017.
© 2017 Society of Hospital Medicine