User login
Hand‐carried ultrasound (HCU) is a field technique. Originally intended for military triage, the advent of small, portable, ultrasound devices has brought ultrasound imaging to the patient's bedside to guide procedures and evaluate life‐threatening conditions. Although many recently‐trained physicians in emergency or critical care medicine now routinely use HCU to place central lines1 and tap effusions,2, 3 the capability of this technique to augment physical examination by all physicians has far greater potential value in medicine. When applied in acute critical scenarios, HCU techniques can quickly demonstrate findings regarding abdominal aortic aneurysm,4 deep vein thrombosis,5 pericardial fluid, or hemoperitoneum6 in patients with unexplained hypotension, and examine inferior vena cava collapsibility7 or brachial artery velocity variation8 to help determine the need for volume resuscitation in sepsis. In patients with unexplained dyspnea, HCU can search for ultrasound lung comet‐tail artifacts as a sign of pulmonary edema,9 or use the presence of pleural sliding to exclude pneumothorax.10 In addition, numerous less urgent applications for HCU imaging are emerging such as cardiac, lung, vascular, musculoskeletal, nerve, thyroid, gallbladder, liver, spleen, renal, testicular, and bladder imaging.
Medical or surgical subspecialties familiar with ultrasound have developed limited HCU examinations that serve specific purposes within the relatively narrow clinical indications encountered by these specialties. As a consequence, overall expertise in bedside HCU currently requires the mastery of multiple unrelated ultrasound views and diagnostic criteria. Without central leadership within this burgeoning field, HCU has found no consensus on its use or development within general medical practice. No one has yet validated a single ultrasound imaging protocol for augmenting the physical examination on all patients akin to the use of the stethoscope. This review discusses the importance of the internisthospitalist at this critical point in the early development of bedside HCU examination, focusing on the cardiopulmonary component as a prototype that has universal application across medical practice. Involvement by hospitalists in pioneering the overall technique will direct research in clinical outcome, restructure internal medicine education, change perception of the physical examination, and spur industry in device development specific for general medicine.
The role of the hospitalist as the leading in‐house diagnostician is unique in medicine, requiring breadth in medical knowledge and unprecedented communication skills in the seamless care of the most medically ill patients in the community.11 Ideally, the hospitalist quickly recognizes disease, discriminately uses consultation or expensive diagnostic testing, chooses cost‐effective therapies, and shortens length of hospital stay. Early accurate diagnosis afforded by HCU imaging has the potential to improve efficiency of medical care across a wide spectrum of clinical presentations. Although to date there are no outcome studies using a mortality endpoint, small individual studies have demonstrated that specific HCU findings improve diagnostic accuracy and relate to hospital stay length12 and readmission.13 The hospitalist position is in theory well‐suited for learning and applying bedside ultrasound, having both expert resources in the hospital to guide training and a clinical objective to reduce unnecessary hospital costs.
Saving the Bedside Examination: The Laying‐on of Ultrasound
Bedside examination is a vital component of the initial hospitalist‐patient interaction, adding objective data to the patient's history. In this era of physician surrogates and telemedicine, physical examination remains a nonnegotiable reason why physicians must appear in person at the patient's bedside to lay on hands. However, bedside cardiovascular examination skills have greatly diminished over the past decade for a variety of reasons.14 In particular, physical examination is impaired in the environment in which the hospitalist must practice. The admitting physician must oftentimes hurriedly examine the patient on the gurney in the noisy emergency department or in bed in an alarm‐filled intensive care unit (ICU) or hospital room. Ambient noise levels often preclude auscultation of acute aortic and mitral valve regurgitation, splitting of valve sounds, low diastolic rumbles, soft gallops, and fine rales. Patient positioning is limited in ventilated patients or those in respiratory or circulatory distress. Although medical education still honors the value of teaching the traditional cardiac examination, no outcome data exist to justify the application of the various maneuvers and techniques learned in medical school to contemporary, commonly encountered inpatient care scenarios. For example, few physical examination data exist on how to evaluate central venous pressures of an obese patient on the ventilator or assess the severity of aortic stenosis in the elderly hypertensive patient. Furthermore, many important cardiopulmonary abnormalities that are easily detected by ultrasound, such as pericardial fluid, well‐compensated left ventricular systolic dysfunction, small pleural effusion, and left atrial enlargement, make no characteristic sound for auscultation. The effect of undiagnosed cardiac abnormalities on the patient's immediate hospital course is unknown, but is likely related to the clinical presentation and long‐term outcome. Today, the hospitalist's suspicion of cardiovascular abnormalities is more often generated from elements in the patient's initial history, serum biomarkers, chest radiography, or electrocardiogram, and less from auscultation. Accordingly, cardiac physical examination is only adjunctively used in determining the general direction of the ensuing evaluation and when abnormal, often generates additional diagnostic testing for confirmation.
The optimal role of HCU for the internist‐hospitalist is in augmentation of bedside physical diagnosis.15, 16 Unlike x‐ray or even rapid serum biomarkers, ultrasound is a safe, immediate, noninvasive modality and has been particularly effective in delineating cardiac structure and physiology. Accurate HCU estimation of a patient's central venous pressure,17 left atrial size,18 or left ventricular ejection fraction19, 20 is of particular value in those with unexplained respiratory distress or circulatory collapse, or in those in whom referral for echocardiography or cardiac consultation is not obvious. Asymptomatic left ventricular systolic dysfunction has an estimated prevalence of 5% in adult populations,21 and its detection would have immediate implications in regard to etiology, volume management, and drug therapy. Multiple studies have shown the prognostic importance of left atrial enlargement in ischemic cardiac disease, congestive heart failure, atrial arrhythmias, and stroke.22 The inferior vena cava diameter has been related to central venous pressure and prognosis in congestive heart failure. A recent study13 using medical residents employing HCU demonstrated that persistent dilatation of the inferior vena cava at discharge related to a higher readmission rate in patients with congestive heart failure. The potential exists to follow and guide a patient's response to therapy with HCU during daily rounds. Comparative studies2325 confirm that HCU examinations are better than expert auscultation and improve overall exam accuracy when added to traditional physical exam techniques. Entering into the modern‐day emergency room with a pocket‐sized ultrasound device that provides the immediate capability of detecting left ventricular dysfunction, left atrial enlargement, pericardial effusion, or abnormalities in volume status, provides an additional sense of being prepared for battle.
Deriving Limited Ultrasound Applications: Time Well Spent
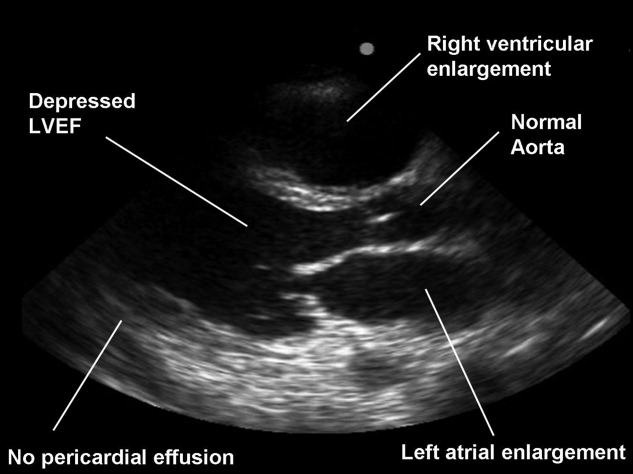
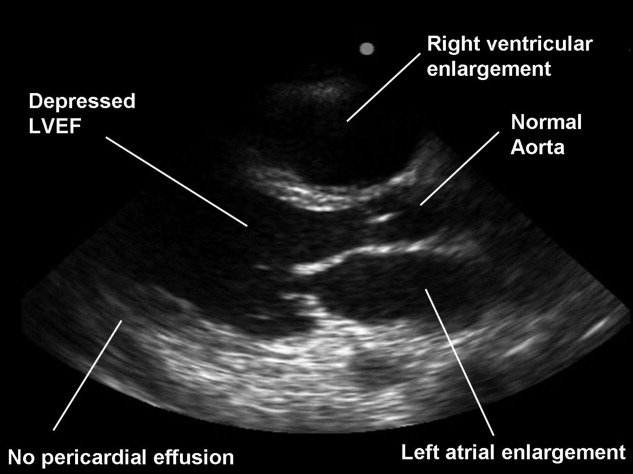
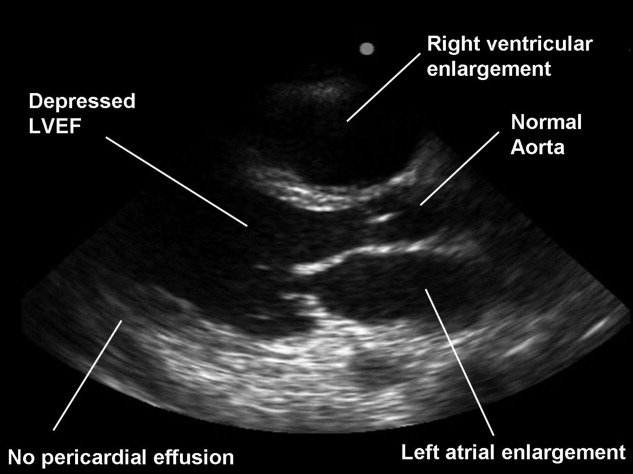
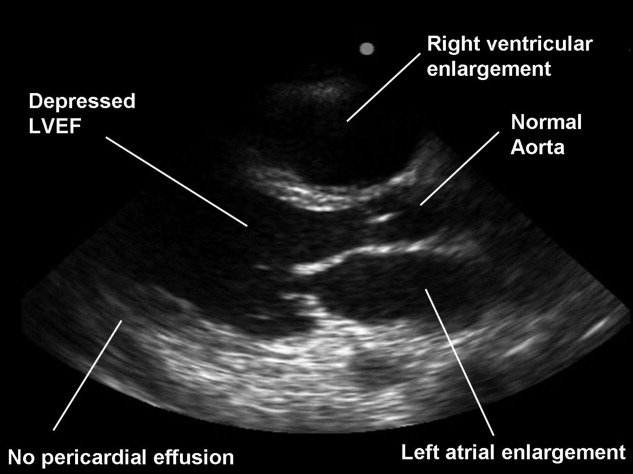
However, in order for a hospitalist to use HCU, easily applied limited imaging protocols must be derived from standard ultrasound examination techniques for each organ. For the heart, studies from our laboratory have shown that it is feasible to distill the comprehensive echocardiogram down to simple cardiac screening examinations for rapid bedside HCU use.2628 We found that a limited cardiac ultrasound study consisting of a single parasternal long‐axis (PLAX) view (Figure 1) requires only seconds to perform and can identify those patients who have significant cardiac abnormalities. In an outpatient population (n = 196) followed in an internal medicine clinic, the PLAX component of an HCU cardiac screening protocol uncovered left atrial enlargement in 4 patients and left ventricular systolic dysfunction in 4 patients that had not been suspected by the patients' primary physicians.29 In a study of 124 patients in the emergency department with suspected cardiac disease,12 abnormal cardiac findings were noted 3 times more frequently by PLAX than by clinical evaluation, and an abnormal PLAX was significantly associated with a longer hospital length of stay. In other preliminary studies using cardiologists, limited imaging has been shown to reduce costs of unnecessary echo referral.28, 3032 Cost analysis has yet to be performed in nonexpert HCU users, but benefit is likely related to the difference between the user's own accuracy with the stethoscope and the HCU device.
Although experts in ultrasound exist in radiology and cardiology, it is unlikely these subspecialists will spontaneously create and optimize a full‐body HCU imaging protocol for hospitalists. Similar to the use of ultrasound in emergency medicine, anesthesiology, and critical care medicine, the derivation of a bedside ultrasound exam appropriate for the in‐hospital physical examination should be developed within the specialty itself, by those acquainted with the clinical scenarios in which HCU would be deployed. For example, the question of whether the gallbladder should be routinely imaged by a quick HCU exam in the evaluation of chest pain is similar to the question of whether the Valsalva maneuver should be performed in the evaluation of every murmurboth require Bayesian knowledge of disease prevalence, exam difficulty, and test accuracy. With the collaboration of experts in ultrasound, internists can derive brief, easily learned, limited ultrasound exams for left ventricular dysfunction, left atrial enlargement, carotid atherosclerosis, interstitial lung disease, hepatosplenomegaly, cholelithiasis, hydronephrosis, renal atrophy, pleural or pericardial effusion, ascites, deep vein thrombosis, and abdominal aortic aneurysm. The discovery of these disease states has clinical value for long‐term care, even if incidental to the patient's acute presentation. The lasting implications of a more comprehensive general examination will likely differentiate the use of HCU in internal medicine practice from that of emergency medicine.
Basic Training in HCU
A significant challenge to medical education will be in physician training in HCU. Over 15 studies12, 13, 15, 1720, 22, 23, 3343 have now shown the ability of briefly trained medical students, residents, and physicians in internal medicine to perform a limited cardiovascular ultrasound examination. Not surprisingly, these studies show variable degrees of training proficiency, apparently dependent upon the complexity of the imaging protocol. In a recent pair of studies from 1 institution,42, 43 10 hospitalists were trained to perform an extensive HCU echocardiogram including 4 views, color and spectral Doppler, and interpret severity of valvular disease, ventricular function, pericardial effusion. In 345 patients already referred for formal echocardiography, which later served as the gold standard, HCU improved the hospitalists' physical examination for left ventricular dysfunction, cardiomegaly, and pericardial effusion, but not for valvular disease. Notably, despite a focused training program including didactic teaching, self‐study cases, 5 training studies, and the imaging of 35 patients with assistance as needed, image acquisition was inferior to standard examination and image interpretation was inferior to that of cardiology fellows. Such data reemphasize the fact that the scope of each body‐system imaging protocol must be narrow in order to make the learning of a full‐body HCU exam feasible and to incorporate training into time already allocated to the bedside physical examination curriculum or continuing medical education activities.
At our institution, internal medical residents are trained in bedside cardiovascular ultrasound to blend results with their auscultative findings during bedside examination. We have developed 2 cardiovascular limited ultrasound examinations (CLUEs) that can be performed in 5 minutes and have evidence‐basis for their clinical use through pilot training studies.18, 19, 29, 35 Our basic CLUE, designed for general cardiovascular examination, includes screening the carotid bulb for subclinical atherosclerosis, PLAX imaging for left atrial enlargement and systolic dysfunction of the left ventricle, and abdominal scanning for abdominal aortic aneurysm. In this imaging protocol consisting of only 4 targets, atherosclerotic risk increases from top to bottom (cephalad to caudal), making the exam easy to remember. The CLUEparasternal, lung, and subcostal (CLUE‐PLUS), designed for the urgent evaluation of unexplained dyspnea or hypotension, uses a work backward imaging format (from left ventricle to right atrium) and a single cardiac transducer for simplicity. The PLAX view screens for left ventricular systolic dysfunction and then left atrial enlargement. Next, a brief 4‐point lung exam screens for ultrasonic lung comets and pleural effusion. A subcostal view of the heart is used to evaluate right ventricular size and pericardial effusion, and finally the inferior vena cava is evaluated for central venous pressures. CLUEs are taught in bedside and didactic formats over the 3 years of residency with formal competency testing after lecture attendance, practice imaging in our echo‐vascular laboratories, participation in rounds, and completion of at least 30 supervised examinations.
Reaffirming the Role of the Internist
Although emergency44 and critical care45 medical subspecialties have begun to train their constituencies in HCU, general diagnostic techniques that have wide‐ranging application in medical illness should be the evidence‐based tools of the internist. The rejuvenation of bedside examination using HCU on multiple organ systems should be orchestrated within internal medicine and not simply evolve as an unedited collection of all subspecialty organ ultrasound examinations. Device development can then be customized and made affordable for use in general internal medicine, perhaps limiting the unnecessary production costs and training requirements for advanced Doppler or multiple transducers.
Concern has been raised about the medical and economic impact of training internists in HCU. Although training costs can be incorporated in residency or hospital‐based continuing medical education, discussions regarding reimbursement for cardiac imaging require a distinction between the brief application of ultrasound using a small device by a nontraditional user and a limited echocardiogram as defined by payers and professional societies.46 To date, no procedural code or reimbursement has yet been approved for ultrasound‐assisted physical examination using HCU devices and likely awaits outcome data. There is also concern about the possibility of errors being made by HCU use by briefly trained physicians. Patient care and cost‐savings depend on HCU accuracy, being liable both for unnecessary referrals due to false‐positive screening HCU exams and delays in diagnosis due to false‐negative examinations. However, such errors are commonplace and accepted with standard physical examination techniques and the current use of the stethoscope, both of which lack sensitivity when compared to HCU.
HCU is a disruptive technology.47 However, unlike the successful disruption that small desktop computers had on their mainframe counterparts, HCU devices appeared before the operating system of their clinical application had been formulated, making dissemination to new users nearly impossible. Furthermore, placing ultrasound transducers into the hands of nontraditional users often alienates or displaces established users of ultrasound as well as established untrained members within the profession. Competency requirements will have to be derived, preferably from studies performed within the profession for specific uses in internal medicine. Perhaps championed by hospitalists and driven by hospital‐based outcome studies, the use of HCU by internists as a physical exam technique will require advocacy by internists themselves. The alternative, having the hospitalist ask the emergency department physician for help in examining the patient, is difficult to imagine. The answer to whether the hospitalist should use HCU should be a resounding yesbased upon the benefit of earlier, more accurate examination and the value of preserving the diagnostic role of the internist at the bedside. In regard to the latter, it is a concept worth fighting for.
- ,,,.Ultrasound guidance for placement of central venous catheters: a meta‐analysis of the literature.Crit Care Med.1996;24(12):2053–2058.
- .Ultrasound‐guided thoracentesis.Chest.2006;129(6):1709–1714.
- ,,, et al.Hand‐carried ultrasound‐guided pericardiocentesis and thoracentesis.J Am Soc Echocardogr.2003;16(5):480–484.
- ,,, et al.A prospective study of a hand‐held ultrasound device in abdominal aortic aneurysm evaluation.Am J Surg.2003;186(5):455–459.
- ,,.Emergency department compression ultrasound to diagnose proximal deep vein thrombosis.J Emerg Med.2001;20(2):107–112.
- ,,,,.The hand‐held FAST: experience with hand‐held trauma sonography in a level‐I urban trauma center.Injury.2002;33(4):303–308.
- ,,, et al.Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients.Intensive Care Med.2004;30(9):1740–1746.
- ,,, et al.Radial artery pulse pressure variation correlates with brachial artery peak velocity variation in ventilated subjects when measured by internal medicine residents using hand‐carried ultrasound devices.Chest.2007;131(5):1301–1307.
- ,,,,,.Evaluation of ultrasound lung comets by hand‐held echocardiography.Cardiovasc Ultrasound.2006;4:34.
- ,.A bedside ultrasound sign ruling out pneumothorax in the critically ill. Lung sliding.Chest.1995;108(5):1345–1348.
- ,The hospitalist movement 5 years later.JAMA.2002;287(4):487–494.
- ,,,.Screening cardiac ultrasound examination in patients with suspected cardiac disease in the emergency room setting.Am Heart J.2001;142:324–330.
- ,,, et al.Comparison of hand‐carried ultrasound assessment of the inferior vena cava and N‐terminal pro‐brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure.J Am Coll Cardiol Img.2008;1:595–601.
- ,.Cardiac auscultatory skills of internal medicine and family practice trainees. A comparison of diagnostic proficiency.JAMA.1997;278(9):717–722.
- ,.Technology insight: hand‐carried ultrasound cardiac assessment—evolution, not revolution.Nat Clin Pract Cardiovasc Med.2005;2(4):217–223.
- ,,.Hand‐carried ultrasound improves the bedside cardiovascular examination.Chest.2004;126(3):693–701.
- ,,, et al.A comparison of medicine residents of physical examination versus hand‐carried ultrasound for estimation of right atrial pressure.Am J Cardiol.2007;99(11):1614–1616.
- ,,, et al.Detection of left atrial enlargement using hand‐carried ultrasound devices to screen for cardiac abnormalities.Am J Med.2005;118(8):912–916.
- ,,,,.Usefulness of a hand‐held ultrasound device for the bedside examination of left ventricular function.Am J Cardiol.2002;90(9):1038–1039.
- ,,,.A hand‐carried personal ultrasound device for rapid evaluation of left ventricular function: use after limited echo training.Echocardiography.2003;20(4):309–312.
- ,.Stage B heart failure: management of asymptomatic left ventricular systolic dysfunction.Circulation.2006;113:2851–2860.
- .The left atrium. A biomarker of chronic diastolic dysfunction and cardiovascular disease risk.J Am Coll Cardiol.2003;42:1206–1207.
- ,,, et al.Physician‐performed point‐of‐care echocardiography using a laptop platform compared with physical examination in the cardiovascular patient.J Am Coll Cardiol.2001;3(8):2013–2018.
- ,,.The hand‐carried echocardiographic device as an aid to the physical examination.Echocardiography.2003;20(5):477–485.
- ,,, et al.Comparison of effectiveness of hand‐carried ultrasound to bedside cardiovascular physical examination.Am J Cardiol.2005;96(7):1002–1006.
- ,,,.Feasibility of “limited” echo imaging: characterization of incidental findings.J Am Soc Echocardiogr.1998;11:746–750.
- ,.Indications for limited echocardiographic imaging: a mathematical model.J Am Soc Echocardiogr.2000;13(9):855–861.
- ,,,.Limited cardiac ultrasound examination for cost‐effective echo referral.J Am Soc Echocardiogr.2002;15:640–646.
- ,,,,,.Value of a cardiovascular limited ultrasound examination using a hand‐carried ultrasound device on clinical management in an outpatient medical clinic.Am J Cardiol.2007;100(2):321–325.
- ,,,.Diagnostic accuracy and cost‐effective implications of an ultrasound screening strategy in suspected mitral valve prolapse.Am J Medicine.2000;108:331–333.
- ,,, et al.The use of hand‐carried ultrasound in the hospital setting—a cost‐effective analysis.J Am Soc Echocardiogr.2005;18(6):620–625.
- ,,, et al.A hand‐carried cardiac ultrasound device in the outpatient cardiology clinic reduces the need for standard echocardiography.Heart.2007;93(4):470–475.
- ,,, et al.Teaching cardiovascular anatomy to medical students by using a handheld ultrasound device.JAMA.2002;288(9):1062–1063.
- ,,,,.The use of small personal ultrasound devices by internists without formal training in echocardiography.Eur J Echocardiogr.2003;4:141–147.
- ,,,,.Briefly‐trained physicians can screen for early atherosclerosis at the bedside using hand‐held ultrasound.Am J Cardiol.2003;92:239–240.
- ,,,,,.Feasibility of point‐of‐care echocardiography by internal medicine house staff.Am Heart J.2004;147(3):476–481.
- ,,, et al.Hand‐carried cardiac ultrasound as a tool to screen for important cardiovascular disease in an underserved minority health care clinic.J Am Soc Echocardiogr.2004;17(5):339–403.
- ,,,,,.The rate at which residents learn to use hand‐held echocardiography at the bedside.Am J Med.2005;118(9):1010–1018.
- ,,, et al.Use of hand‐carried ultrasound devices to augment the accuracy of medical student bedside cardiac diagnoses.J Am Soc Echocardiogr.2005;18(3):257–263.
- ,,, et al.Focused training for goal‐oriented hand‐held echocardiography performed by noncardiologist residents in the intensive care unit.Intensive Care Med.2007;33(10):1795–1799.
- ,,.A pilot study of the clinical impact of hand‐carried cardiac ultrasound in the medical clinic.Echocardiography.2006;23(6):439–446.
- ,,,,,.Hospitalist performance of cardiac hand‐carried ultrasound after focused training.Am J Med.2007;120(11):1000–1004.
- ,,, et al.Hand‐carried ultrasound performed by hospitalist: does it improve the cardiac physical examination?Am J Med.2009;122(1):35–41.
- ,,, et al.Usefulness of hand‐held ultrasound devices in out‐of‐hospital diagnosis performed by emergency physicians.Am J Emerg Med.2006;24(2):237–242.
- ,,, et al.Feasibility and potential clinical utility of goal‐directed transthoracic echocardiography performed by noncardiologist intensivists using a small hand‐carried device (SonoHeart) in critically ill patients.J Cardiothorac Vasc Anesth.2005;19(2):155–159.
- ,,, et al.Hand‐carried cardiac ultrasound (HCU) device: recommendations regarding new technology. A report from the Echocardiography Task Force on New Technology of the Nomenclature and Standards Committee of the American Society of Echocardiography.J Am Soc of Echocardiogr.2002;15(4):369–373.
- ,,.Will disruptive innovations cure health care?Harv Bus Rev.2000;78(5):102–112,199.
Hand‐carried ultrasound (HCU) is a field technique. Originally intended for military triage, the advent of small, portable, ultrasound devices has brought ultrasound imaging to the patient's bedside to guide procedures and evaluate life‐threatening conditions. Although many recently‐trained physicians in emergency or critical care medicine now routinely use HCU to place central lines1 and tap effusions,2, 3 the capability of this technique to augment physical examination by all physicians has far greater potential value in medicine. When applied in acute critical scenarios, HCU techniques can quickly demonstrate findings regarding abdominal aortic aneurysm,4 deep vein thrombosis,5 pericardial fluid, or hemoperitoneum6 in patients with unexplained hypotension, and examine inferior vena cava collapsibility7 or brachial artery velocity variation8 to help determine the need for volume resuscitation in sepsis. In patients with unexplained dyspnea, HCU can search for ultrasound lung comet‐tail artifacts as a sign of pulmonary edema,9 or use the presence of pleural sliding to exclude pneumothorax.10 In addition, numerous less urgent applications for HCU imaging are emerging such as cardiac, lung, vascular, musculoskeletal, nerve, thyroid, gallbladder, liver, spleen, renal, testicular, and bladder imaging.
Medical or surgical subspecialties familiar with ultrasound have developed limited HCU examinations that serve specific purposes within the relatively narrow clinical indications encountered by these specialties. As a consequence, overall expertise in bedside HCU currently requires the mastery of multiple unrelated ultrasound views and diagnostic criteria. Without central leadership within this burgeoning field, HCU has found no consensus on its use or development within general medical practice. No one has yet validated a single ultrasound imaging protocol for augmenting the physical examination on all patients akin to the use of the stethoscope. This review discusses the importance of the internisthospitalist at this critical point in the early development of bedside HCU examination, focusing on the cardiopulmonary component as a prototype that has universal application across medical practice. Involvement by hospitalists in pioneering the overall technique will direct research in clinical outcome, restructure internal medicine education, change perception of the physical examination, and spur industry in device development specific for general medicine.
The role of the hospitalist as the leading in‐house diagnostician is unique in medicine, requiring breadth in medical knowledge and unprecedented communication skills in the seamless care of the most medically ill patients in the community.11 Ideally, the hospitalist quickly recognizes disease, discriminately uses consultation or expensive diagnostic testing, chooses cost‐effective therapies, and shortens length of hospital stay. Early accurate diagnosis afforded by HCU imaging has the potential to improve efficiency of medical care across a wide spectrum of clinical presentations. Although to date there are no outcome studies using a mortality endpoint, small individual studies have demonstrated that specific HCU findings improve diagnostic accuracy and relate to hospital stay length12 and readmission.13 The hospitalist position is in theory well‐suited for learning and applying bedside ultrasound, having both expert resources in the hospital to guide training and a clinical objective to reduce unnecessary hospital costs.
Saving the Bedside Examination: The Laying‐on of Ultrasound
Bedside examination is a vital component of the initial hospitalist‐patient interaction, adding objective data to the patient's history. In this era of physician surrogates and telemedicine, physical examination remains a nonnegotiable reason why physicians must appear in person at the patient's bedside to lay on hands. However, bedside cardiovascular examination skills have greatly diminished over the past decade for a variety of reasons.14 In particular, physical examination is impaired in the environment in which the hospitalist must practice. The admitting physician must oftentimes hurriedly examine the patient on the gurney in the noisy emergency department or in bed in an alarm‐filled intensive care unit (ICU) or hospital room. Ambient noise levels often preclude auscultation of acute aortic and mitral valve regurgitation, splitting of valve sounds, low diastolic rumbles, soft gallops, and fine rales. Patient positioning is limited in ventilated patients or those in respiratory or circulatory distress. Although medical education still honors the value of teaching the traditional cardiac examination, no outcome data exist to justify the application of the various maneuvers and techniques learned in medical school to contemporary, commonly encountered inpatient care scenarios. For example, few physical examination data exist on how to evaluate central venous pressures of an obese patient on the ventilator or assess the severity of aortic stenosis in the elderly hypertensive patient. Furthermore, many important cardiopulmonary abnormalities that are easily detected by ultrasound, such as pericardial fluid, well‐compensated left ventricular systolic dysfunction, small pleural effusion, and left atrial enlargement, make no characteristic sound for auscultation. The effect of undiagnosed cardiac abnormalities on the patient's immediate hospital course is unknown, but is likely related to the clinical presentation and long‐term outcome. Today, the hospitalist's suspicion of cardiovascular abnormalities is more often generated from elements in the patient's initial history, serum biomarkers, chest radiography, or electrocardiogram, and less from auscultation. Accordingly, cardiac physical examination is only adjunctively used in determining the general direction of the ensuing evaluation and when abnormal, often generates additional diagnostic testing for confirmation.
The optimal role of HCU for the internist‐hospitalist is in augmentation of bedside physical diagnosis.15, 16 Unlike x‐ray or even rapid serum biomarkers, ultrasound is a safe, immediate, noninvasive modality and has been particularly effective in delineating cardiac structure and physiology. Accurate HCU estimation of a patient's central venous pressure,17 left atrial size,18 or left ventricular ejection fraction19, 20 is of particular value in those with unexplained respiratory distress or circulatory collapse, or in those in whom referral for echocardiography or cardiac consultation is not obvious. Asymptomatic left ventricular systolic dysfunction has an estimated prevalence of 5% in adult populations,21 and its detection would have immediate implications in regard to etiology, volume management, and drug therapy. Multiple studies have shown the prognostic importance of left atrial enlargement in ischemic cardiac disease, congestive heart failure, atrial arrhythmias, and stroke.22 The inferior vena cava diameter has been related to central venous pressure and prognosis in congestive heart failure. A recent study13 using medical residents employing HCU demonstrated that persistent dilatation of the inferior vena cava at discharge related to a higher readmission rate in patients with congestive heart failure. The potential exists to follow and guide a patient's response to therapy with HCU during daily rounds. Comparative studies2325 confirm that HCU examinations are better than expert auscultation and improve overall exam accuracy when added to traditional physical exam techniques. Entering into the modern‐day emergency room with a pocket‐sized ultrasound device that provides the immediate capability of detecting left ventricular dysfunction, left atrial enlargement, pericardial effusion, or abnormalities in volume status, provides an additional sense of being prepared for battle.
Deriving Limited Ultrasound Applications: Time Well Spent
However, in order for a hospitalist to use HCU, easily applied limited imaging protocols must be derived from standard ultrasound examination techniques for each organ. For the heart, studies from our laboratory have shown that it is feasible to distill the comprehensive echocardiogram down to simple cardiac screening examinations for rapid bedside HCU use.2628 We found that a limited cardiac ultrasound study consisting of a single parasternal long‐axis (PLAX) view (Figure 1) requires only seconds to perform and can identify those patients who have significant cardiac abnormalities. In an outpatient population (n = 196) followed in an internal medicine clinic, the PLAX component of an HCU cardiac screening protocol uncovered left atrial enlargement in 4 patients and left ventricular systolic dysfunction in 4 patients that had not been suspected by the patients' primary physicians.29 In a study of 124 patients in the emergency department with suspected cardiac disease,12 abnormal cardiac findings were noted 3 times more frequently by PLAX than by clinical evaluation, and an abnormal PLAX was significantly associated with a longer hospital length of stay. In other preliminary studies using cardiologists, limited imaging has been shown to reduce costs of unnecessary echo referral.28, 3032 Cost analysis has yet to be performed in nonexpert HCU users, but benefit is likely related to the difference between the user's own accuracy with the stethoscope and the HCU device.
Although experts in ultrasound exist in radiology and cardiology, it is unlikely these subspecialists will spontaneously create and optimize a full‐body HCU imaging protocol for hospitalists. Similar to the use of ultrasound in emergency medicine, anesthesiology, and critical care medicine, the derivation of a bedside ultrasound exam appropriate for the in‐hospital physical examination should be developed within the specialty itself, by those acquainted with the clinical scenarios in which HCU would be deployed. For example, the question of whether the gallbladder should be routinely imaged by a quick HCU exam in the evaluation of chest pain is similar to the question of whether the Valsalva maneuver should be performed in the evaluation of every murmurboth require Bayesian knowledge of disease prevalence, exam difficulty, and test accuracy. With the collaboration of experts in ultrasound, internists can derive brief, easily learned, limited ultrasound exams for left ventricular dysfunction, left atrial enlargement, carotid atherosclerosis, interstitial lung disease, hepatosplenomegaly, cholelithiasis, hydronephrosis, renal atrophy, pleural or pericardial effusion, ascites, deep vein thrombosis, and abdominal aortic aneurysm. The discovery of these disease states has clinical value for long‐term care, even if incidental to the patient's acute presentation. The lasting implications of a more comprehensive general examination will likely differentiate the use of HCU in internal medicine practice from that of emergency medicine.
Basic Training in HCU
A significant challenge to medical education will be in physician training in HCU. Over 15 studies12, 13, 15, 1720, 22, 23, 3343 have now shown the ability of briefly trained medical students, residents, and physicians in internal medicine to perform a limited cardiovascular ultrasound examination. Not surprisingly, these studies show variable degrees of training proficiency, apparently dependent upon the complexity of the imaging protocol. In a recent pair of studies from 1 institution,42, 43 10 hospitalists were trained to perform an extensive HCU echocardiogram including 4 views, color and spectral Doppler, and interpret severity of valvular disease, ventricular function, pericardial effusion. In 345 patients already referred for formal echocardiography, which later served as the gold standard, HCU improved the hospitalists' physical examination for left ventricular dysfunction, cardiomegaly, and pericardial effusion, but not for valvular disease. Notably, despite a focused training program including didactic teaching, self‐study cases, 5 training studies, and the imaging of 35 patients with assistance as needed, image acquisition was inferior to standard examination and image interpretation was inferior to that of cardiology fellows. Such data reemphasize the fact that the scope of each body‐system imaging protocol must be narrow in order to make the learning of a full‐body HCU exam feasible and to incorporate training into time already allocated to the bedside physical examination curriculum or continuing medical education activities.
At our institution, internal medical residents are trained in bedside cardiovascular ultrasound to blend results with their auscultative findings during bedside examination. We have developed 2 cardiovascular limited ultrasound examinations (CLUEs) that can be performed in 5 minutes and have evidence‐basis for their clinical use through pilot training studies.18, 19, 29, 35 Our basic CLUE, designed for general cardiovascular examination, includes screening the carotid bulb for subclinical atherosclerosis, PLAX imaging for left atrial enlargement and systolic dysfunction of the left ventricle, and abdominal scanning for abdominal aortic aneurysm. In this imaging protocol consisting of only 4 targets, atherosclerotic risk increases from top to bottom (cephalad to caudal), making the exam easy to remember. The CLUEparasternal, lung, and subcostal (CLUE‐PLUS), designed for the urgent evaluation of unexplained dyspnea or hypotension, uses a work backward imaging format (from left ventricle to right atrium) and a single cardiac transducer for simplicity. The PLAX view screens for left ventricular systolic dysfunction and then left atrial enlargement. Next, a brief 4‐point lung exam screens for ultrasonic lung comets and pleural effusion. A subcostal view of the heart is used to evaluate right ventricular size and pericardial effusion, and finally the inferior vena cava is evaluated for central venous pressures. CLUEs are taught in bedside and didactic formats over the 3 years of residency with formal competency testing after lecture attendance, practice imaging in our echo‐vascular laboratories, participation in rounds, and completion of at least 30 supervised examinations.
Reaffirming the Role of the Internist
Although emergency44 and critical care45 medical subspecialties have begun to train their constituencies in HCU, general diagnostic techniques that have wide‐ranging application in medical illness should be the evidence‐based tools of the internist. The rejuvenation of bedside examination using HCU on multiple organ systems should be orchestrated within internal medicine and not simply evolve as an unedited collection of all subspecialty organ ultrasound examinations. Device development can then be customized and made affordable for use in general internal medicine, perhaps limiting the unnecessary production costs and training requirements for advanced Doppler or multiple transducers.
Concern has been raised about the medical and economic impact of training internists in HCU. Although training costs can be incorporated in residency or hospital‐based continuing medical education, discussions regarding reimbursement for cardiac imaging require a distinction between the brief application of ultrasound using a small device by a nontraditional user and a limited echocardiogram as defined by payers and professional societies.46 To date, no procedural code or reimbursement has yet been approved for ultrasound‐assisted physical examination using HCU devices and likely awaits outcome data. There is also concern about the possibility of errors being made by HCU use by briefly trained physicians. Patient care and cost‐savings depend on HCU accuracy, being liable both for unnecessary referrals due to false‐positive screening HCU exams and delays in diagnosis due to false‐negative examinations. However, such errors are commonplace and accepted with standard physical examination techniques and the current use of the stethoscope, both of which lack sensitivity when compared to HCU.
HCU is a disruptive technology.47 However, unlike the successful disruption that small desktop computers had on their mainframe counterparts, HCU devices appeared before the operating system of their clinical application had been formulated, making dissemination to new users nearly impossible. Furthermore, placing ultrasound transducers into the hands of nontraditional users often alienates or displaces established users of ultrasound as well as established untrained members within the profession. Competency requirements will have to be derived, preferably from studies performed within the profession for specific uses in internal medicine. Perhaps championed by hospitalists and driven by hospital‐based outcome studies, the use of HCU by internists as a physical exam technique will require advocacy by internists themselves. The alternative, having the hospitalist ask the emergency department physician for help in examining the patient, is difficult to imagine. The answer to whether the hospitalist should use HCU should be a resounding yesbased upon the benefit of earlier, more accurate examination and the value of preserving the diagnostic role of the internist at the bedside. In regard to the latter, it is a concept worth fighting for.
Hand‐carried ultrasound (HCU) is a field technique. Originally intended for military triage, the advent of small, portable, ultrasound devices has brought ultrasound imaging to the patient's bedside to guide procedures and evaluate life‐threatening conditions. Although many recently‐trained physicians in emergency or critical care medicine now routinely use HCU to place central lines1 and tap effusions,2, 3 the capability of this technique to augment physical examination by all physicians has far greater potential value in medicine. When applied in acute critical scenarios, HCU techniques can quickly demonstrate findings regarding abdominal aortic aneurysm,4 deep vein thrombosis,5 pericardial fluid, or hemoperitoneum6 in patients with unexplained hypotension, and examine inferior vena cava collapsibility7 or brachial artery velocity variation8 to help determine the need for volume resuscitation in sepsis. In patients with unexplained dyspnea, HCU can search for ultrasound lung comet‐tail artifacts as a sign of pulmonary edema,9 or use the presence of pleural sliding to exclude pneumothorax.10 In addition, numerous less urgent applications for HCU imaging are emerging such as cardiac, lung, vascular, musculoskeletal, nerve, thyroid, gallbladder, liver, spleen, renal, testicular, and bladder imaging.
Medical or surgical subspecialties familiar with ultrasound have developed limited HCU examinations that serve specific purposes within the relatively narrow clinical indications encountered by these specialties. As a consequence, overall expertise in bedside HCU currently requires the mastery of multiple unrelated ultrasound views and diagnostic criteria. Without central leadership within this burgeoning field, HCU has found no consensus on its use or development within general medical practice. No one has yet validated a single ultrasound imaging protocol for augmenting the physical examination on all patients akin to the use of the stethoscope. This review discusses the importance of the internisthospitalist at this critical point in the early development of bedside HCU examination, focusing on the cardiopulmonary component as a prototype that has universal application across medical practice. Involvement by hospitalists in pioneering the overall technique will direct research in clinical outcome, restructure internal medicine education, change perception of the physical examination, and spur industry in device development specific for general medicine.
The role of the hospitalist as the leading in‐house diagnostician is unique in medicine, requiring breadth in medical knowledge and unprecedented communication skills in the seamless care of the most medically ill patients in the community.11 Ideally, the hospitalist quickly recognizes disease, discriminately uses consultation or expensive diagnostic testing, chooses cost‐effective therapies, and shortens length of hospital stay. Early accurate diagnosis afforded by HCU imaging has the potential to improve efficiency of medical care across a wide spectrum of clinical presentations. Although to date there are no outcome studies using a mortality endpoint, small individual studies have demonstrated that specific HCU findings improve diagnostic accuracy and relate to hospital stay length12 and readmission.13 The hospitalist position is in theory well‐suited for learning and applying bedside ultrasound, having both expert resources in the hospital to guide training and a clinical objective to reduce unnecessary hospital costs.
Saving the Bedside Examination: The Laying‐on of Ultrasound
Bedside examination is a vital component of the initial hospitalist‐patient interaction, adding objective data to the patient's history. In this era of physician surrogates and telemedicine, physical examination remains a nonnegotiable reason why physicians must appear in person at the patient's bedside to lay on hands. However, bedside cardiovascular examination skills have greatly diminished over the past decade for a variety of reasons.14 In particular, physical examination is impaired in the environment in which the hospitalist must practice. The admitting physician must oftentimes hurriedly examine the patient on the gurney in the noisy emergency department or in bed in an alarm‐filled intensive care unit (ICU) or hospital room. Ambient noise levels often preclude auscultation of acute aortic and mitral valve regurgitation, splitting of valve sounds, low diastolic rumbles, soft gallops, and fine rales. Patient positioning is limited in ventilated patients or those in respiratory or circulatory distress. Although medical education still honors the value of teaching the traditional cardiac examination, no outcome data exist to justify the application of the various maneuvers and techniques learned in medical school to contemporary, commonly encountered inpatient care scenarios. For example, few physical examination data exist on how to evaluate central venous pressures of an obese patient on the ventilator or assess the severity of aortic stenosis in the elderly hypertensive patient. Furthermore, many important cardiopulmonary abnormalities that are easily detected by ultrasound, such as pericardial fluid, well‐compensated left ventricular systolic dysfunction, small pleural effusion, and left atrial enlargement, make no characteristic sound for auscultation. The effect of undiagnosed cardiac abnormalities on the patient's immediate hospital course is unknown, but is likely related to the clinical presentation and long‐term outcome. Today, the hospitalist's suspicion of cardiovascular abnormalities is more often generated from elements in the patient's initial history, serum biomarkers, chest radiography, or electrocardiogram, and less from auscultation. Accordingly, cardiac physical examination is only adjunctively used in determining the general direction of the ensuing evaluation and when abnormal, often generates additional diagnostic testing for confirmation.
The optimal role of HCU for the internist‐hospitalist is in augmentation of bedside physical diagnosis.15, 16 Unlike x‐ray or even rapid serum biomarkers, ultrasound is a safe, immediate, noninvasive modality and has been particularly effective in delineating cardiac structure and physiology. Accurate HCU estimation of a patient's central venous pressure,17 left atrial size,18 or left ventricular ejection fraction19, 20 is of particular value in those with unexplained respiratory distress or circulatory collapse, or in those in whom referral for echocardiography or cardiac consultation is not obvious. Asymptomatic left ventricular systolic dysfunction has an estimated prevalence of 5% in adult populations,21 and its detection would have immediate implications in regard to etiology, volume management, and drug therapy. Multiple studies have shown the prognostic importance of left atrial enlargement in ischemic cardiac disease, congestive heart failure, atrial arrhythmias, and stroke.22 The inferior vena cava diameter has been related to central venous pressure and prognosis in congestive heart failure. A recent study13 using medical residents employing HCU demonstrated that persistent dilatation of the inferior vena cava at discharge related to a higher readmission rate in patients with congestive heart failure. The potential exists to follow and guide a patient's response to therapy with HCU during daily rounds. Comparative studies2325 confirm that HCU examinations are better than expert auscultation and improve overall exam accuracy when added to traditional physical exam techniques. Entering into the modern‐day emergency room with a pocket‐sized ultrasound device that provides the immediate capability of detecting left ventricular dysfunction, left atrial enlargement, pericardial effusion, or abnormalities in volume status, provides an additional sense of being prepared for battle.
Deriving Limited Ultrasound Applications: Time Well Spent
However, in order for a hospitalist to use HCU, easily applied limited imaging protocols must be derived from standard ultrasound examination techniques for each organ. For the heart, studies from our laboratory have shown that it is feasible to distill the comprehensive echocardiogram down to simple cardiac screening examinations for rapid bedside HCU use.2628 We found that a limited cardiac ultrasound study consisting of a single parasternal long‐axis (PLAX) view (Figure 1) requires only seconds to perform and can identify those patients who have significant cardiac abnormalities. In an outpatient population (n = 196) followed in an internal medicine clinic, the PLAX component of an HCU cardiac screening protocol uncovered left atrial enlargement in 4 patients and left ventricular systolic dysfunction in 4 patients that had not been suspected by the patients' primary physicians.29 In a study of 124 patients in the emergency department with suspected cardiac disease,12 abnormal cardiac findings were noted 3 times more frequently by PLAX than by clinical evaluation, and an abnormal PLAX was significantly associated with a longer hospital length of stay. In other preliminary studies using cardiologists, limited imaging has been shown to reduce costs of unnecessary echo referral.28, 3032 Cost analysis has yet to be performed in nonexpert HCU users, but benefit is likely related to the difference between the user's own accuracy with the stethoscope and the HCU device.
Although experts in ultrasound exist in radiology and cardiology, it is unlikely these subspecialists will spontaneously create and optimize a full‐body HCU imaging protocol for hospitalists. Similar to the use of ultrasound in emergency medicine, anesthesiology, and critical care medicine, the derivation of a bedside ultrasound exam appropriate for the in‐hospital physical examination should be developed within the specialty itself, by those acquainted with the clinical scenarios in which HCU would be deployed. For example, the question of whether the gallbladder should be routinely imaged by a quick HCU exam in the evaluation of chest pain is similar to the question of whether the Valsalva maneuver should be performed in the evaluation of every murmurboth require Bayesian knowledge of disease prevalence, exam difficulty, and test accuracy. With the collaboration of experts in ultrasound, internists can derive brief, easily learned, limited ultrasound exams for left ventricular dysfunction, left atrial enlargement, carotid atherosclerosis, interstitial lung disease, hepatosplenomegaly, cholelithiasis, hydronephrosis, renal atrophy, pleural or pericardial effusion, ascites, deep vein thrombosis, and abdominal aortic aneurysm. The discovery of these disease states has clinical value for long‐term care, even if incidental to the patient's acute presentation. The lasting implications of a more comprehensive general examination will likely differentiate the use of HCU in internal medicine practice from that of emergency medicine.
Basic Training in HCU
A significant challenge to medical education will be in physician training in HCU. Over 15 studies12, 13, 15, 1720, 22, 23, 3343 have now shown the ability of briefly trained medical students, residents, and physicians in internal medicine to perform a limited cardiovascular ultrasound examination. Not surprisingly, these studies show variable degrees of training proficiency, apparently dependent upon the complexity of the imaging protocol. In a recent pair of studies from 1 institution,42, 43 10 hospitalists were trained to perform an extensive HCU echocardiogram including 4 views, color and spectral Doppler, and interpret severity of valvular disease, ventricular function, pericardial effusion. In 345 patients already referred for formal echocardiography, which later served as the gold standard, HCU improved the hospitalists' physical examination for left ventricular dysfunction, cardiomegaly, and pericardial effusion, but not for valvular disease. Notably, despite a focused training program including didactic teaching, self‐study cases, 5 training studies, and the imaging of 35 patients with assistance as needed, image acquisition was inferior to standard examination and image interpretation was inferior to that of cardiology fellows. Such data reemphasize the fact that the scope of each body‐system imaging protocol must be narrow in order to make the learning of a full‐body HCU exam feasible and to incorporate training into time already allocated to the bedside physical examination curriculum or continuing medical education activities.
At our institution, internal medical residents are trained in bedside cardiovascular ultrasound to blend results with their auscultative findings during bedside examination. We have developed 2 cardiovascular limited ultrasound examinations (CLUEs) that can be performed in 5 minutes and have evidence‐basis for their clinical use through pilot training studies.18, 19, 29, 35 Our basic CLUE, designed for general cardiovascular examination, includes screening the carotid bulb for subclinical atherosclerosis, PLAX imaging for left atrial enlargement and systolic dysfunction of the left ventricle, and abdominal scanning for abdominal aortic aneurysm. In this imaging protocol consisting of only 4 targets, atherosclerotic risk increases from top to bottom (cephalad to caudal), making the exam easy to remember. The CLUEparasternal, lung, and subcostal (CLUE‐PLUS), designed for the urgent evaluation of unexplained dyspnea or hypotension, uses a work backward imaging format (from left ventricle to right atrium) and a single cardiac transducer for simplicity. The PLAX view screens for left ventricular systolic dysfunction and then left atrial enlargement. Next, a brief 4‐point lung exam screens for ultrasonic lung comets and pleural effusion. A subcostal view of the heart is used to evaluate right ventricular size and pericardial effusion, and finally the inferior vena cava is evaluated for central venous pressures. CLUEs are taught in bedside and didactic formats over the 3 years of residency with formal competency testing after lecture attendance, practice imaging in our echo‐vascular laboratories, participation in rounds, and completion of at least 30 supervised examinations.
Reaffirming the Role of the Internist
Although emergency44 and critical care45 medical subspecialties have begun to train their constituencies in HCU, general diagnostic techniques that have wide‐ranging application in medical illness should be the evidence‐based tools of the internist. The rejuvenation of bedside examination using HCU on multiple organ systems should be orchestrated within internal medicine and not simply evolve as an unedited collection of all subspecialty organ ultrasound examinations. Device development can then be customized and made affordable for use in general internal medicine, perhaps limiting the unnecessary production costs and training requirements for advanced Doppler or multiple transducers.
Concern has been raised about the medical and economic impact of training internists in HCU. Although training costs can be incorporated in residency or hospital‐based continuing medical education, discussions regarding reimbursement for cardiac imaging require a distinction between the brief application of ultrasound using a small device by a nontraditional user and a limited echocardiogram as defined by payers and professional societies.46 To date, no procedural code or reimbursement has yet been approved for ultrasound‐assisted physical examination using HCU devices and likely awaits outcome data. There is also concern about the possibility of errors being made by HCU use by briefly trained physicians. Patient care and cost‐savings depend on HCU accuracy, being liable both for unnecessary referrals due to false‐positive screening HCU exams and delays in diagnosis due to false‐negative examinations. However, such errors are commonplace and accepted with standard physical examination techniques and the current use of the stethoscope, both of which lack sensitivity when compared to HCU.
HCU is a disruptive technology.47 However, unlike the successful disruption that small desktop computers had on their mainframe counterparts, HCU devices appeared before the operating system of their clinical application had been formulated, making dissemination to new users nearly impossible. Furthermore, placing ultrasound transducers into the hands of nontraditional users often alienates or displaces established users of ultrasound as well as established untrained members within the profession. Competency requirements will have to be derived, preferably from studies performed within the profession for specific uses in internal medicine. Perhaps championed by hospitalists and driven by hospital‐based outcome studies, the use of HCU by internists as a physical exam technique will require advocacy by internists themselves. The alternative, having the hospitalist ask the emergency department physician for help in examining the patient, is difficult to imagine. The answer to whether the hospitalist should use HCU should be a resounding yesbased upon the benefit of earlier, more accurate examination and the value of preserving the diagnostic role of the internist at the bedside. In regard to the latter, it is a concept worth fighting for.
- ,,,.Ultrasound guidance for placement of central venous catheters: a meta‐analysis of the literature.Crit Care Med.1996;24(12):2053–2058.
- .Ultrasound‐guided thoracentesis.Chest.2006;129(6):1709–1714.
- ,,, et al.Hand‐carried ultrasound‐guided pericardiocentesis and thoracentesis.J Am Soc Echocardogr.2003;16(5):480–484.
- ,,, et al.A prospective study of a hand‐held ultrasound device in abdominal aortic aneurysm evaluation.Am J Surg.2003;186(5):455–459.
- ,,.Emergency department compression ultrasound to diagnose proximal deep vein thrombosis.J Emerg Med.2001;20(2):107–112.
- ,,,,.The hand‐held FAST: experience with hand‐held trauma sonography in a level‐I urban trauma center.Injury.2002;33(4):303–308.
- ,,, et al.Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients.Intensive Care Med.2004;30(9):1740–1746.
- ,,, et al.Radial artery pulse pressure variation correlates with brachial artery peak velocity variation in ventilated subjects when measured by internal medicine residents using hand‐carried ultrasound devices.Chest.2007;131(5):1301–1307.
- ,,,,,.Evaluation of ultrasound lung comets by hand‐held echocardiography.Cardiovasc Ultrasound.2006;4:34.
- ,.A bedside ultrasound sign ruling out pneumothorax in the critically ill. Lung sliding.Chest.1995;108(5):1345–1348.
- ,The hospitalist movement 5 years later.JAMA.2002;287(4):487–494.
- ,,,.Screening cardiac ultrasound examination in patients with suspected cardiac disease in the emergency room setting.Am Heart J.2001;142:324–330.
- ,,, et al.Comparison of hand‐carried ultrasound assessment of the inferior vena cava and N‐terminal pro‐brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure.J Am Coll Cardiol Img.2008;1:595–601.
- ,.Cardiac auscultatory skills of internal medicine and family practice trainees. A comparison of diagnostic proficiency.JAMA.1997;278(9):717–722.
- ,.Technology insight: hand‐carried ultrasound cardiac assessment—evolution, not revolution.Nat Clin Pract Cardiovasc Med.2005;2(4):217–223.
- ,,.Hand‐carried ultrasound improves the bedside cardiovascular examination.Chest.2004;126(3):693–701.
- ,,, et al.A comparison of medicine residents of physical examination versus hand‐carried ultrasound for estimation of right atrial pressure.Am J Cardiol.2007;99(11):1614–1616.
- ,,, et al.Detection of left atrial enlargement using hand‐carried ultrasound devices to screen for cardiac abnormalities.Am J Med.2005;118(8):912–916.
- ,,,,.Usefulness of a hand‐held ultrasound device for the bedside examination of left ventricular function.Am J Cardiol.2002;90(9):1038–1039.
- ,,,.A hand‐carried personal ultrasound device for rapid evaluation of left ventricular function: use after limited echo training.Echocardiography.2003;20(4):309–312.
- ,.Stage B heart failure: management of asymptomatic left ventricular systolic dysfunction.Circulation.2006;113:2851–2860.
- .The left atrium. A biomarker of chronic diastolic dysfunction and cardiovascular disease risk.J Am Coll Cardiol.2003;42:1206–1207.
- ,,, et al.Physician‐performed point‐of‐care echocardiography using a laptop platform compared with physical examination in the cardiovascular patient.J Am Coll Cardiol.2001;3(8):2013–2018.
- ,,.The hand‐carried echocardiographic device as an aid to the physical examination.Echocardiography.2003;20(5):477–485.
- ,,, et al.Comparison of effectiveness of hand‐carried ultrasound to bedside cardiovascular physical examination.Am J Cardiol.2005;96(7):1002–1006.
- ,,,.Feasibility of “limited” echo imaging: characterization of incidental findings.J Am Soc Echocardiogr.1998;11:746–750.
- ,.Indications for limited echocardiographic imaging: a mathematical model.J Am Soc Echocardiogr.2000;13(9):855–861.
- ,,,.Limited cardiac ultrasound examination for cost‐effective echo referral.J Am Soc Echocardiogr.2002;15:640–646.
- ,,,,,.Value of a cardiovascular limited ultrasound examination using a hand‐carried ultrasound device on clinical management in an outpatient medical clinic.Am J Cardiol.2007;100(2):321–325.
- ,,,.Diagnostic accuracy and cost‐effective implications of an ultrasound screening strategy in suspected mitral valve prolapse.Am J Medicine.2000;108:331–333.
- ,,, et al.The use of hand‐carried ultrasound in the hospital setting—a cost‐effective analysis.J Am Soc Echocardiogr.2005;18(6):620–625.
- ,,, et al.A hand‐carried cardiac ultrasound device in the outpatient cardiology clinic reduces the need for standard echocardiography.Heart.2007;93(4):470–475.
- ,,, et al.Teaching cardiovascular anatomy to medical students by using a handheld ultrasound device.JAMA.2002;288(9):1062–1063.
- ,,,,.The use of small personal ultrasound devices by internists without formal training in echocardiography.Eur J Echocardiogr.2003;4:141–147.
- ,,,,.Briefly‐trained physicians can screen for early atherosclerosis at the bedside using hand‐held ultrasound.Am J Cardiol.2003;92:239–240.
- ,,,,,.Feasibility of point‐of‐care echocardiography by internal medicine house staff.Am Heart J.2004;147(3):476–481.
- ,,, et al.Hand‐carried cardiac ultrasound as a tool to screen for important cardiovascular disease in an underserved minority health care clinic.J Am Soc Echocardiogr.2004;17(5):339–403.
- ,,,,,.The rate at which residents learn to use hand‐held echocardiography at the bedside.Am J Med.2005;118(9):1010–1018.
- ,,, et al.Use of hand‐carried ultrasound devices to augment the accuracy of medical student bedside cardiac diagnoses.J Am Soc Echocardiogr.2005;18(3):257–263.
- ,,, et al.Focused training for goal‐oriented hand‐held echocardiography performed by noncardiologist residents in the intensive care unit.Intensive Care Med.2007;33(10):1795–1799.
- ,,.A pilot study of the clinical impact of hand‐carried cardiac ultrasound in the medical clinic.Echocardiography.2006;23(6):439–446.
- ,,,,,.Hospitalist performance of cardiac hand‐carried ultrasound after focused training.Am J Med.2007;120(11):1000–1004.
- ,,, et al.Hand‐carried ultrasound performed by hospitalist: does it improve the cardiac physical examination?Am J Med.2009;122(1):35–41.
- ,,, et al.Usefulness of hand‐held ultrasound devices in out‐of‐hospital diagnosis performed by emergency physicians.Am J Emerg Med.2006;24(2):237–242.
- ,,, et al.Feasibility and potential clinical utility of goal‐directed transthoracic echocardiography performed by noncardiologist intensivists using a small hand‐carried device (SonoHeart) in critically ill patients.J Cardiothorac Vasc Anesth.2005;19(2):155–159.
- ,,, et al.Hand‐carried cardiac ultrasound (HCU) device: recommendations regarding new technology. A report from the Echocardiography Task Force on New Technology of the Nomenclature and Standards Committee of the American Society of Echocardiography.J Am Soc of Echocardiogr.2002;15(4):369–373.
- ,,.Will disruptive innovations cure health care?Harv Bus Rev.2000;78(5):102–112,199.
- ,,,.Ultrasound guidance for placement of central venous catheters: a meta‐analysis of the literature.Crit Care Med.1996;24(12):2053–2058.
- .Ultrasound‐guided thoracentesis.Chest.2006;129(6):1709–1714.
- ,,, et al.Hand‐carried ultrasound‐guided pericardiocentesis and thoracentesis.J Am Soc Echocardogr.2003;16(5):480–484.
- ,,, et al.A prospective study of a hand‐held ultrasound device in abdominal aortic aneurysm evaluation.Am J Surg.2003;186(5):455–459.
- ,,.Emergency department compression ultrasound to diagnose proximal deep vein thrombosis.J Emerg Med.2001;20(2):107–112.
- ,,,,.The hand‐held FAST: experience with hand‐held trauma sonography in a level‐I urban trauma center.Injury.2002;33(4):303–308.
- ,,, et al.Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients.Intensive Care Med.2004;30(9):1740–1746.
- ,,, et al.Radial artery pulse pressure variation correlates with brachial artery peak velocity variation in ventilated subjects when measured by internal medicine residents using hand‐carried ultrasound devices.Chest.2007;131(5):1301–1307.
- ,,,,,.Evaluation of ultrasound lung comets by hand‐held echocardiography.Cardiovasc Ultrasound.2006;4:34.
- ,.A bedside ultrasound sign ruling out pneumothorax in the critically ill. Lung sliding.Chest.1995;108(5):1345–1348.
- ,The hospitalist movement 5 years later.JAMA.2002;287(4):487–494.
- ,,,.Screening cardiac ultrasound examination in patients with suspected cardiac disease in the emergency room setting.Am Heart J.2001;142:324–330.
- ,,, et al.Comparison of hand‐carried ultrasound assessment of the inferior vena cava and N‐terminal pro‐brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure.J Am Coll Cardiol Img.2008;1:595–601.
- ,.Cardiac auscultatory skills of internal medicine and family practice trainees. A comparison of diagnostic proficiency.JAMA.1997;278(9):717–722.
- ,.Technology insight: hand‐carried ultrasound cardiac assessment—evolution, not revolution.Nat Clin Pract Cardiovasc Med.2005;2(4):217–223.
- ,,.Hand‐carried ultrasound improves the bedside cardiovascular examination.Chest.2004;126(3):693–701.
- ,,, et al.A comparison of medicine residents of physical examination versus hand‐carried ultrasound for estimation of right atrial pressure.Am J Cardiol.2007;99(11):1614–1616.
- ,,, et al.Detection of left atrial enlargement using hand‐carried ultrasound devices to screen for cardiac abnormalities.Am J Med.2005;118(8):912–916.
- ,,,,.Usefulness of a hand‐held ultrasound device for the bedside examination of left ventricular function.Am J Cardiol.2002;90(9):1038–1039.
- ,,,.A hand‐carried personal ultrasound device for rapid evaluation of left ventricular function: use after limited echo training.Echocardiography.2003;20(4):309–312.
- ,.Stage B heart failure: management of asymptomatic left ventricular systolic dysfunction.Circulation.2006;113:2851–2860.
- .The left atrium. A biomarker of chronic diastolic dysfunction and cardiovascular disease risk.J Am Coll Cardiol.2003;42:1206–1207.
- ,,, et al.Physician‐performed point‐of‐care echocardiography using a laptop platform compared with physical examination in the cardiovascular patient.J Am Coll Cardiol.2001;3(8):2013–2018.
- ,,.The hand‐carried echocardiographic device as an aid to the physical examination.Echocardiography.2003;20(5):477–485.
- ,,, et al.Comparison of effectiveness of hand‐carried ultrasound to bedside cardiovascular physical examination.Am J Cardiol.2005;96(7):1002–1006.
- ,,,.Feasibility of “limited” echo imaging: characterization of incidental findings.J Am Soc Echocardiogr.1998;11:746–750.
- ,.Indications for limited echocardiographic imaging: a mathematical model.J Am Soc Echocardiogr.2000;13(9):855–861.
- ,,,.Limited cardiac ultrasound examination for cost‐effective echo referral.J Am Soc Echocardiogr.2002;15:640–646.
- ,,,,,.Value of a cardiovascular limited ultrasound examination using a hand‐carried ultrasound device on clinical management in an outpatient medical clinic.Am J Cardiol.2007;100(2):321–325.
- ,,,.Diagnostic accuracy and cost‐effective implications of an ultrasound screening strategy in suspected mitral valve prolapse.Am J Medicine.2000;108:331–333.
- ,,, et al.The use of hand‐carried ultrasound in the hospital setting—a cost‐effective analysis.J Am Soc Echocardiogr.2005;18(6):620–625.
- ,,, et al.A hand‐carried cardiac ultrasound device in the outpatient cardiology clinic reduces the need for standard echocardiography.Heart.2007;93(4):470–475.
- ,,, et al.Teaching cardiovascular anatomy to medical students by using a handheld ultrasound device.JAMA.2002;288(9):1062–1063.
- ,,,,.The use of small personal ultrasound devices by internists without formal training in echocardiography.Eur J Echocardiogr.2003;4:141–147.
- ,,,,.Briefly‐trained physicians can screen for early atherosclerosis at the bedside using hand‐held ultrasound.Am J Cardiol.2003;92:239–240.
- ,,,,,.Feasibility of point‐of‐care echocardiography by internal medicine house staff.Am Heart J.2004;147(3):476–481.
- ,,, et al.Hand‐carried cardiac ultrasound as a tool to screen for important cardiovascular disease in an underserved minority health care clinic.J Am Soc Echocardiogr.2004;17(5):339–403.
- ,,,,,.The rate at which residents learn to use hand‐held echocardiography at the bedside.Am J Med.2005;118(9):1010–1018.
- ,,, et al.Use of hand‐carried ultrasound devices to augment the accuracy of medical student bedside cardiac diagnoses.J Am Soc Echocardiogr.2005;18(3):257–263.
- ,,, et al.Focused training for goal‐oriented hand‐held echocardiography performed by noncardiologist residents in the intensive care unit.Intensive Care Med.2007;33(10):1795–1799.
- ,,.A pilot study of the clinical impact of hand‐carried cardiac ultrasound in the medical clinic.Echocardiography.2006;23(6):439–446.
- ,,,,,.Hospitalist performance of cardiac hand‐carried ultrasound after focused training.Am J Med.2007;120(11):1000–1004.
- ,,, et al.Hand‐carried ultrasound performed by hospitalist: does it improve the cardiac physical examination?Am J Med.2009;122(1):35–41.
- ,,, et al.Usefulness of hand‐held ultrasound devices in out‐of‐hospital diagnosis performed by emergency physicians.Am J Emerg Med.2006;24(2):237–242.
- ,,, et al.Feasibility and potential clinical utility of goal‐directed transthoracic echocardiography performed by noncardiologist intensivists using a small hand‐carried device (SonoHeart) in critically ill patients.J Cardiothorac Vasc Anesth.2005;19(2):155–159.
- ,,, et al.Hand‐carried cardiac ultrasound (HCU) device: recommendations regarding new technology. A report from the Echocardiography Task Force on New Technology of the Nomenclature and Standards Committee of the American Society of Echocardiography.J Am Soc of Echocardiogr.2002;15(4):369–373.
- ,,.Will disruptive innovations cure health care?Harv Bus Rev.2000;78(5):102–112,199.