User login
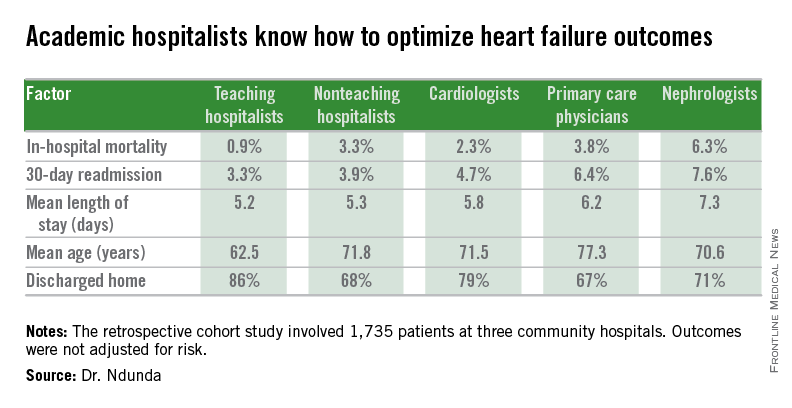
LAS VEGAS – When it comes to managing patients hospitalized for heart failure, academic hospitalists are the experts – and cardiologists, primary care physicians, and nephrologists are the students.
That’s the lesson Dr. Paul M. Ndunda drew from his retrospective cohort study of 1,735 patients hospitalized for heart failure at three community hospitals. The patients admitted by members of the three teaching hospitalist groups had the lowest inpatient mortality, mean length of stay, and 30-day readmission rates compared to the other admitting physicians.
Although these data aren’t risk adjusted and its certainly possible that the academic hospitalists culled patients with a more favorable risk profile, it’s also likely that the explanation for the outcome differences is multifactorial and that specialty-specific differences in the care delivery process played a role. Indeed, it would appear that the hospitalist model of management of heart failure patients holds lessons of value for other types of physicians, Dr. Ndunda asserted at the annual meeting of the Heart Failure Society of America.
It’s also noteworthy that the teaching hospitalist groups achieved patient outcomes that were by and large better than the nonteaching hospitalist groups, added Dr. Ndunda of the University of Kansas, Wichita.
The major caveat, he conceded, is that outcomes weren’t risk adjusted. This takes on added weight in light of the fact that the teaching hospitalists’ patients were significantly younger than other physicians’ patients were. They were also more likely to be discharged home.
Dr. Ndunda reported having no financial conflicts with regard to this study.
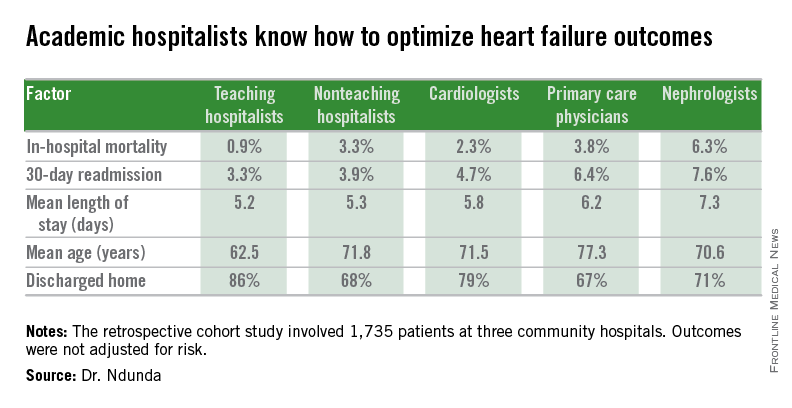
LAS VEGAS – When it comes to managing patients hospitalized for heart failure, academic hospitalists are the experts – and cardiologists, primary care physicians, and nephrologists are the students.
That’s the lesson Dr. Paul M. Ndunda drew from his retrospective cohort study of 1,735 patients hospitalized for heart failure at three community hospitals. The patients admitted by members of the three teaching hospitalist groups had the lowest inpatient mortality, mean length of stay, and 30-day readmission rates compared to the other admitting physicians.
Although these data aren’t risk adjusted and its certainly possible that the academic hospitalists culled patients with a more favorable risk profile, it’s also likely that the explanation for the outcome differences is multifactorial and that specialty-specific differences in the care delivery process played a role. Indeed, it would appear that the hospitalist model of management of heart failure patients holds lessons of value for other types of physicians, Dr. Ndunda asserted at the annual meeting of the Heart Failure Society of America.
It’s also noteworthy that the teaching hospitalist groups achieved patient outcomes that were by and large better than the nonteaching hospitalist groups, added Dr. Ndunda of the University of Kansas, Wichita.
The major caveat, he conceded, is that outcomes weren’t risk adjusted. This takes on added weight in light of the fact that the teaching hospitalists’ patients were significantly younger than other physicians’ patients were. They were also more likely to be discharged home.
Dr. Ndunda reported having no financial conflicts with regard to this study.
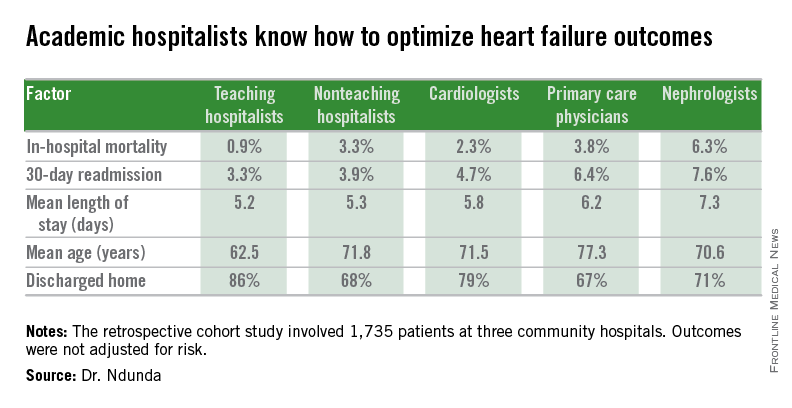
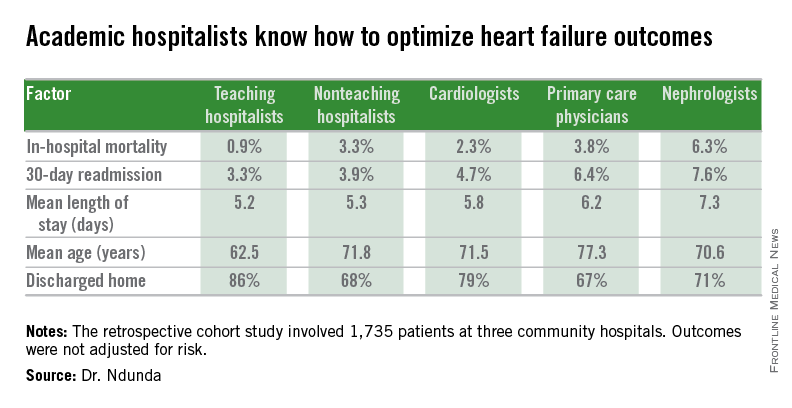
LAS VEGAS – When it comes to managing patients hospitalized for heart failure, academic hospitalists are the experts – and cardiologists, primary care physicians, and nephrologists are the students.
That’s the lesson Dr. Paul M. Ndunda drew from his retrospective cohort study of 1,735 patients hospitalized for heart failure at three community hospitals. The patients admitted by members of the three teaching hospitalist groups had the lowest inpatient mortality, mean length of stay, and 30-day readmission rates compared to the other admitting physicians.
Although these data aren’t risk adjusted and its certainly possible that the academic hospitalists culled patients with a more favorable risk profile, it’s also likely that the explanation for the outcome differences is multifactorial and that specialty-specific differences in the care delivery process played a role. Indeed, it would appear that the hospitalist model of management of heart failure patients holds lessons of value for other types of physicians, Dr. Ndunda asserted at the annual meeting of the Heart Failure Society of America.
It’s also noteworthy that the teaching hospitalist groups achieved patient outcomes that were by and large better than the nonteaching hospitalist groups, added Dr. Ndunda of the University of Kansas, Wichita.
The major caveat, he conceded, is that outcomes weren’t risk adjusted. This takes on added weight in light of the fact that the teaching hospitalists’ patients were significantly younger than other physicians’ patients were. They were also more likely to be discharged home.
Dr. Ndunda reported having no financial conflicts with regard to this study.
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point: Outcomes were significantly better among patients admitted for heart failure by academic hospitalists than in those admitted by primary care physicians, cardiologists, nonteaching hospitalists, or nephrologists.
Major finding: The unadjusted 30-day heart failure–specific readmission rate for patients admitted by academic hospitalists was 3.3% – significantly lower than other physicians’ rates.
Data source: This retrospective cohort study included 1,735 patients admitted for heart failure to three community hospitals.
Disclosures: The presenter reported having no financial conflicts with regard to this study.