User login
The prevalence of T2DM is on the rise in the United States, and T2DM is currently the 7th leading cause of death.1 In a study of 28,143 participants in the US National Health and Nutrition Examination Survey (NHANES) who were 18 years or older, the prevalence of diabetes increased from 9.8% to 14.3% between 2000 and 2008.2 About 24% of the participants had undiagnosed diabetes prior to the testing they received as a study participant.2 People from minority groups have a higher rate of T2DM than non-Hispanic White people. Using data from 2018, the Centers for Disease Control and Prevention reported that the prevalence of diagnosed diabetes was highest among American Indians/Alaska Natives (14.7%), people of Hispanic origin (12.5%), and non-Hispanic Blacks (11.7%), followed by non-Hispanic Asians (9.2%) and non-Hispanic Whites (7.5%).1 Diabetes is a major risk factor for myocardial infarction, stroke, renal failure, retinopathy, peripheral vascular disease, and neuropathy.1 Early detection and treatment of both prediabetes and diabetes may improve health and reduce these preventable complications, saving lives, preventing heart and renal failure and blindness.
T2DM is caused by a combination of insulin resistance and insufficient pancreatic secretion of insulin to overcome the insulin resistance.3 In young adults with insulin resistance, pancreatic secretion of insulin is often sufficient to overcome the insulin resistance resulting in normal glucose levels and persistently increased insulin concentration. As individuals with insulin resistance age, pancreatic secretion of insulin may decline, resulting in insufficient production of insulin and rising glucose levels. Many individuals experience a prolonged stage of prediabetes that may be present for decades prior to transitioning to T2DM. In 2020, 35% of US adults were reported to have prediabetes.1
Screening for diabetes mellitus
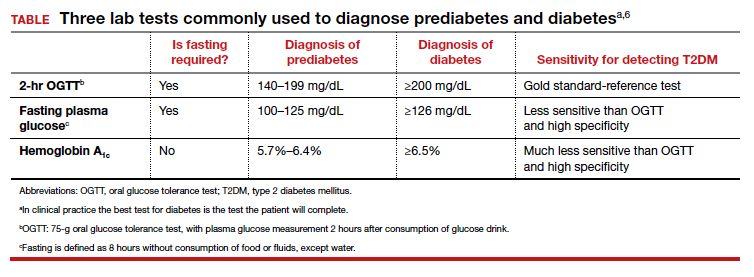
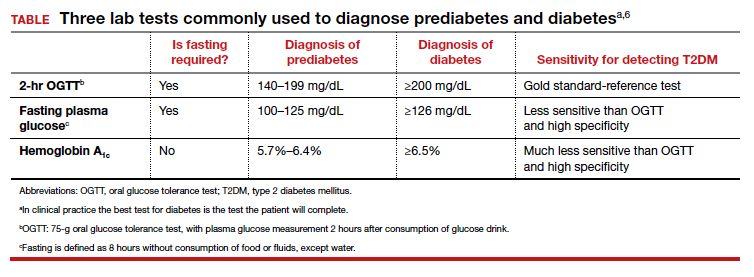
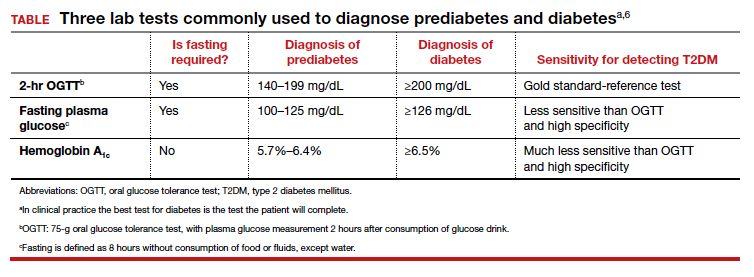
The US Preventive Services Task Force (USPSTF) recently recommended that all adults aged 35 to 70 years who are overweight or obese be screened for T2DM (B recommendation).4 Screening for diabetes will also result in detecting many people with prediabetes. The criteria for diagnosing diabetes and prediabetes are presented in the TABLE. Based on cohort studies, the USPSTF noted that screening every 3 years is a reasonable approach.4 They also recommended that people diagnosed with prediabetes should initiate preventive measures, including optimizing diet, weight loss, exercise, and in some cases, medication treatment such as metformin.5
Approaches to the diagnosis of diabetes and prediabetes
Three laboratory tests are widely utilized for the diagnosis of prediabetes and diabetes: measurement of a plasma glucose 2 hours following consumption of oral glucose 75 g (2-hr oral glucose tolerance test [OGTT]), measurement of a fasting plasma glucose, and measurement of hemoglobin A1c (see Table).6In clinical practice, the best diabetes screening test is the test the patient will complete. Most evidence indicates that, compared with the 2-hr OGTT, a hemoglobin A1c measurement is specific for diagnosing T2DM, but not sensitive. In other words, if the hemoglobin A1c is ≥6.5%, the glucose measurement 2 hours following an OGTT will very likely be ≥200 mg/dL. But if the hemoglobin A1c is between 5.7% and 6.5%, the person might be diagnosed with T2DM if they had a 2-hr OGTT.6
In one study, 1,241 nondiabetic, overweight, or obese participants had all 3 tests to diagnose T2DM.7 The 2-hr OGTT diagnosed T2DM in 148 participants (12%). However, the hemoglobin A1c test only diagnosed T2DM in 78 of the 148 participants who were diagnosed with T2DM based on the 2-hr OGTT, missing 47% of the cases of T2DM. In this study, using the 2-hr OGTT as the “gold standard” reference test, the hemoglobin A1c test had a sensitivity of 53% and specificity of 97%.7
In clinical practice one approach is to explain to the patient the pros and cons of the 3 tests for T2DM and ask them to select the test they prefer to complete. In a high-risk population, including people with obesity, completing any of the 3 tests is better than not testing for diabetes. It also should be noted that, among people who have a normal body mass index (BMI), a “prediabetes” diagnosis is controversial. Compared with obese persons with prediabetes, people with a normal BMI and prediabetes diagnosed by a blood test progress to diabetes at a much lower rate. The value of diagnosing prediabetes after 70 years of age is also controversial because few people in this situation progress to diabetes.8 Clinicians should be cautious about diagnosing prediabetes in lean or elderly people.
The reliability of the hemoglobin A1c test is reduced in conditions associated with increased red blood cell turnover, including sickle cell disease, pregnancy (second and third trimesters), hemodialysis, recent blood transfusions or erythropoietin therapy. In these clinical situations, only blood glucose measurements should be used to diagnose prediabetes and T2DM.6 It should be noted that concordance among any of the 3 tests is not perfect.6
Continue to: A 2-step approach to diagnosing T2DM...
A 2-step approach to diagnosing T2DM
An alternative to relying on a single test for T2DM is to use a 2-step approach for screening. The first step is a hemoglobin A1c measurement, which neither requires fasting nor waiting for 2 hours for post–glucose load blood draw. If the hemoglobin A1c result is ≥6.5%, a T2DM diagnosis can be made, with no additional testing. If the hemoglobin A1c result is 5.7% to 6.4%, the person probably has either prediabetes or diabetes and can be offered a 2-hr OGTT to definitively determine if T2DM is the proper diagnosis. If the hemoglobin A1c test is <5.7%, it is unlikely that the person has T2DM or prediabetes at the time of the test. In this situation, the testing could be repeated in 3 years. Using a 2-step approach reduces the number of people who are tested with a 2-hr OGTT and detects more cases of T2DM than a 1-step approach that relies on a hemoglobin A1c measurement alone.
Treatment of prediabetes is warranted in people at high risk for developing diabetes
It is better to prevent diabetes among people with a high risk of diabetes than to treat diabetes once it is established. People with prediabetes who are overweight or obese are at high risk for developing diabetes. Prediabetes is diagnosed by a fasting plasma glucose level of 100 to 125 mg/dL or a hemoglobin A1c measurement of 5.7% to 6.4%.
High-quality randomized clinical trials have definitively demonstrated that, among people at high risk for developing diabetes, lifestyle modification and metformin treatment reduce the risk of developing diabetes. In the Diabetes Prevention Program (DPP) 3,234 people with a high risk of diabetes, mean BMI 34 kg/m2, were randomly assigned to 1 of 3 groups9:
- a control group
- metformin (850 mg twice daily) or
- lifestyle modification that included exercise (moderate intensity exercise for 150 minutes per week and weight loss (7% of body weight using a low-calorie, low-fat diet).
At 2.8 years of follow-up the incidence of diabetes was 11%, 7.8%, and 4.8% per 100 person-years in the people assigned to the control, metformin, and lifestyle modification groups, respectively.9 In the DPP study, compared with the control group, metformin was most effective in decreasing the risk of transitioning to diabetes in people who had a BMI ≥35 kg/m2 (53% reduction in risk) or a BMI from 30 to 35 kg/m2 (16% reduction in risk).9 Metformin was not as effective at preventing the transition to diabetes in people who had a normal BMI or who were overweight (3% reduction).9
In the Finnish Diabetes Prevention Study, 522 obese people with impaired glucose tolerance were randomly assigned to lifestyle modification or a control group. After 4 years, the cumulative incidence of diabetes was 11% and 23% in the lifestyle modification and control groups, respectively.10 A meta-analysis of 23 randomized clinical trials reported that, among people with a high risk of developing diabetes, compared with no intervention (control group), lifestyle modification, including dieting, exercising, and weight loss significantly reduced the risk of developing diabetes (pooled relative risk [RR], 0.78; 95% confidence interval [CI], 0.69‒0.88).5
In clinical practice, offering a patient at high risk for diabetes a suite of options, including5,9,10:
- a formal nutrition consult with the goal of targeting a 7% reduction in weight
- recommending moderate intensity exercise, 150 minutes weekly
- metformin treatment, if the patient is obese
would reduce the patient’s risk of developing diabetes.
Treatment of T2DM is complex
For people with T2DM, a widely recommended treatment goal is to reduce the hemoglobin A1c measurement to ≤7%. Initial treatment includes a comprehensive diabetes self-management education program, weight loss using diet and exercise, and metformin treatment. Metformin may be associated with an increased risk of lactic acidosis, especially in people with renal insufficiency. The US Food and Drug Administration (FDA) recommends against initiating metformin therapy for people with an estimated glomerular filtration rate (eGFR) of 30 to 45 mL/min/1.73 m2. The FDA determined that metformin is contraindicated in people with an eGFR of <30 mL/min/1.73 m2.11 Many people with T2DM will require treatment with multiple pharmacologic agents to achieve a hemoglobin A1c ≤7%. In addition to metformin, pharmacologic agents used to treat T2DM include insulin, sulfonylureas, glucagon-like peptide-1(GLP-1) receptor agonists, a sodium glucose cotransporter (SGLT2) inhibitor, dipeptidyl peptidase-4 (DPP-4) inhibitors, or an alpha-glucosidase inhibitor. Given the complexity of managing T2DM over a lifetime, most individuals with T2DM receive their diabetes care from a primary care clinician or subspecialist in endocrinology.
Experts predict that, within the next 8 years, the prevalence of obesity among adults in the United States will be approximately 50%.12 The US health care system has not been effective in controlling the obesity epidemic. Our failure to control the obesity epidemic will result in an increase in the prevalence of prediabetes and T2DM, leading to a rise in cardiovascular, renal, and eye disease. The diagnosis of prediabetes and diabetes is within the scope of practice of obstetrics and gynecology. The treatment of prediabetes is also within the scope of ObGyns, who have both expertise and familiarity in the diagnosis of gestational diabetes, a form of prediabetes. ●
- Centers for Disease Control and Prevention. National Diabetes Statistics Report. 2020. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed October 26, 2021.
- Wang L, Li X, Wang Z, et al. Trends in prevalence of diabetes and control of risk factors in diabetes among U.S. adults, 1999-2018. JAMA. 2021;326:1-13. doi: 10.1001/jama.2021.9883.
- Type 2 diabetes. Centers for Disease Control and Prevention website. . Last reviewed August 10, 2021 Accessed October 27, 2021.
- US Preventive Services Task Force. Screening for prediabetes and diabetes. US Preventive Services Task Force Recommendation Statement. JAMA. 2021;326:736-743. doi: 10.1001/jama.2021.12531.
- Jonas D, Crotty K, Yun JD, et al. Screening for prediabetes and type 2 diabetes mellitus: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2021;326:744-760. doi: 10.1001/jama.2021.10403.
- American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes‒2020. Diabetes Care. 2020;43(suppl 1):S14-S31. doi: 10.2337/dc20-S002.
- Meijnikman AS, De Block CE, Dirinck E, et al. Not performing an OGTT results in significant under diagnosis of (pre)diabetes in a high-risk adult Caucasian population. Int J Obes. 2017;41:1615-1620. doi: 10.1038/ijo.2017.165.
- Rooney MR, Rawlings AM, Pankow JS, et al. Risk of progression to diabetes among older adults with prediabetes. JAMA Intern Med. 2021;181:511-519. doi: 10.1001/jamainternmed.2020.8774.
- Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403. doi: 10.1056/NEJMoa012512.
- Tuomilehto J, Lindström J, Eriksson JG, et al; Finnish Diabetes Prevention Study Group. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343-1350. doi: 10.1056/NEJM200105033441801.
- Glucophage [package insert]. Princeton, NJ: Bristol Meyers Squibb; April 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017020357s037s039,021202s021s023lbl.pdf. Accessed October 27, 2021.
- Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381;2440-2450. doi: 10.1056/NEJMc1917339.
The prevalence of T2DM is on the rise in the United States, and T2DM is currently the 7th leading cause of death.1 In a study of 28,143 participants in the US National Health and Nutrition Examination Survey (NHANES) who were 18 years or older, the prevalence of diabetes increased from 9.8% to 14.3% between 2000 and 2008.2 About 24% of the participants had undiagnosed diabetes prior to the testing they received as a study participant.2 People from minority groups have a higher rate of T2DM than non-Hispanic White people. Using data from 2018, the Centers for Disease Control and Prevention reported that the prevalence of diagnosed diabetes was highest among American Indians/Alaska Natives (14.7%), people of Hispanic origin (12.5%), and non-Hispanic Blacks (11.7%), followed by non-Hispanic Asians (9.2%) and non-Hispanic Whites (7.5%).1 Diabetes is a major risk factor for myocardial infarction, stroke, renal failure, retinopathy, peripheral vascular disease, and neuropathy.1 Early detection and treatment of both prediabetes and diabetes may improve health and reduce these preventable complications, saving lives, preventing heart and renal failure and blindness.
T2DM is caused by a combination of insulin resistance and insufficient pancreatic secretion of insulin to overcome the insulin resistance.3 In young adults with insulin resistance, pancreatic secretion of insulin is often sufficient to overcome the insulin resistance resulting in normal glucose levels and persistently increased insulin concentration. As individuals with insulin resistance age, pancreatic secretion of insulin may decline, resulting in insufficient production of insulin and rising glucose levels. Many individuals experience a prolonged stage of prediabetes that may be present for decades prior to transitioning to T2DM. In 2020, 35% of US adults were reported to have prediabetes.1
Screening for diabetes mellitus
The US Preventive Services Task Force (USPSTF) recently recommended that all adults aged 35 to 70 years who are overweight or obese be screened for T2DM (B recommendation).4 Screening for diabetes will also result in detecting many people with prediabetes. The criteria for diagnosing diabetes and prediabetes are presented in the TABLE. Based on cohort studies, the USPSTF noted that screening every 3 years is a reasonable approach.4 They also recommended that people diagnosed with prediabetes should initiate preventive measures, including optimizing diet, weight loss, exercise, and in some cases, medication treatment such as metformin.5
Approaches to the diagnosis of diabetes and prediabetes
Three laboratory tests are widely utilized for the diagnosis of prediabetes and diabetes: measurement of a plasma glucose 2 hours following consumption of oral glucose 75 g (2-hr oral glucose tolerance test [OGTT]), measurement of a fasting plasma glucose, and measurement of hemoglobin A1c (see Table).6In clinical practice, the best diabetes screening test is the test the patient will complete. Most evidence indicates that, compared with the 2-hr OGTT, a hemoglobin A1c measurement is specific for diagnosing T2DM, but not sensitive. In other words, if the hemoglobin A1c is ≥6.5%, the glucose measurement 2 hours following an OGTT will very likely be ≥200 mg/dL. But if the hemoglobin A1c is between 5.7% and 6.5%, the person might be diagnosed with T2DM if they had a 2-hr OGTT.6
In one study, 1,241 nondiabetic, overweight, or obese participants had all 3 tests to diagnose T2DM.7 The 2-hr OGTT diagnosed T2DM in 148 participants (12%). However, the hemoglobin A1c test only diagnosed T2DM in 78 of the 148 participants who were diagnosed with T2DM based on the 2-hr OGTT, missing 47% of the cases of T2DM. In this study, using the 2-hr OGTT as the “gold standard” reference test, the hemoglobin A1c test had a sensitivity of 53% and specificity of 97%.7
In clinical practice one approach is to explain to the patient the pros and cons of the 3 tests for T2DM and ask them to select the test they prefer to complete. In a high-risk population, including people with obesity, completing any of the 3 tests is better than not testing for diabetes. It also should be noted that, among people who have a normal body mass index (BMI), a “prediabetes” diagnosis is controversial. Compared with obese persons with prediabetes, people with a normal BMI and prediabetes diagnosed by a blood test progress to diabetes at a much lower rate. The value of diagnosing prediabetes after 70 years of age is also controversial because few people in this situation progress to diabetes.8 Clinicians should be cautious about diagnosing prediabetes in lean or elderly people.
The reliability of the hemoglobin A1c test is reduced in conditions associated with increased red blood cell turnover, including sickle cell disease, pregnancy (second and third trimesters), hemodialysis, recent blood transfusions or erythropoietin therapy. In these clinical situations, only blood glucose measurements should be used to diagnose prediabetes and T2DM.6 It should be noted that concordance among any of the 3 tests is not perfect.6
Continue to: A 2-step approach to diagnosing T2DM...
A 2-step approach to diagnosing T2DM
An alternative to relying on a single test for T2DM is to use a 2-step approach for screening. The first step is a hemoglobin A1c measurement, which neither requires fasting nor waiting for 2 hours for post–glucose load blood draw. If the hemoglobin A1c result is ≥6.5%, a T2DM diagnosis can be made, with no additional testing. If the hemoglobin A1c result is 5.7% to 6.4%, the person probably has either prediabetes or diabetes and can be offered a 2-hr OGTT to definitively determine if T2DM is the proper diagnosis. If the hemoglobin A1c test is <5.7%, it is unlikely that the person has T2DM or prediabetes at the time of the test. In this situation, the testing could be repeated in 3 years. Using a 2-step approach reduces the number of people who are tested with a 2-hr OGTT and detects more cases of T2DM than a 1-step approach that relies on a hemoglobin A1c measurement alone.
Treatment of prediabetes is warranted in people at high risk for developing diabetes
It is better to prevent diabetes among people with a high risk of diabetes than to treat diabetes once it is established. People with prediabetes who are overweight or obese are at high risk for developing diabetes. Prediabetes is diagnosed by a fasting plasma glucose level of 100 to 125 mg/dL or a hemoglobin A1c measurement of 5.7% to 6.4%.
High-quality randomized clinical trials have definitively demonstrated that, among people at high risk for developing diabetes, lifestyle modification and metformin treatment reduce the risk of developing diabetes. In the Diabetes Prevention Program (DPP) 3,234 people with a high risk of diabetes, mean BMI 34 kg/m2, were randomly assigned to 1 of 3 groups9:
- a control group
- metformin (850 mg twice daily) or
- lifestyle modification that included exercise (moderate intensity exercise for 150 minutes per week and weight loss (7% of body weight using a low-calorie, low-fat diet).
At 2.8 years of follow-up the incidence of diabetes was 11%, 7.8%, and 4.8% per 100 person-years in the people assigned to the control, metformin, and lifestyle modification groups, respectively.9 In the DPP study, compared with the control group, metformin was most effective in decreasing the risk of transitioning to diabetes in people who had a BMI ≥35 kg/m2 (53% reduction in risk) or a BMI from 30 to 35 kg/m2 (16% reduction in risk).9 Metformin was not as effective at preventing the transition to diabetes in people who had a normal BMI or who were overweight (3% reduction).9
In the Finnish Diabetes Prevention Study, 522 obese people with impaired glucose tolerance were randomly assigned to lifestyle modification or a control group. After 4 years, the cumulative incidence of diabetes was 11% and 23% in the lifestyle modification and control groups, respectively.10 A meta-analysis of 23 randomized clinical trials reported that, among people with a high risk of developing diabetes, compared with no intervention (control group), lifestyle modification, including dieting, exercising, and weight loss significantly reduced the risk of developing diabetes (pooled relative risk [RR], 0.78; 95% confidence interval [CI], 0.69‒0.88).5
In clinical practice, offering a patient at high risk for diabetes a suite of options, including5,9,10:
- a formal nutrition consult with the goal of targeting a 7% reduction in weight
- recommending moderate intensity exercise, 150 minutes weekly
- metformin treatment, if the patient is obese
would reduce the patient’s risk of developing diabetes.
Treatment of T2DM is complex
For people with T2DM, a widely recommended treatment goal is to reduce the hemoglobin A1c measurement to ≤7%. Initial treatment includes a comprehensive diabetes self-management education program, weight loss using diet and exercise, and metformin treatment. Metformin may be associated with an increased risk of lactic acidosis, especially in people with renal insufficiency. The US Food and Drug Administration (FDA) recommends against initiating metformin therapy for people with an estimated glomerular filtration rate (eGFR) of 30 to 45 mL/min/1.73 m2. The FDA determined that metformin is contraindicated in people with an eGFR of <30 mL/min/1.73 m2.11 Many people with T2DM will require treatment with multiple pharmacologic agents to achieve a hemoglobin A1c ≤7%. In addition to metformin, pharmacologic agents used to treat T2DM include insulin, sulfonylureas, glucagon-like peptide-1(GLP-1) receptor agonists, a sodium glucose cotransporter (SGLT2) inhibitor, dipeptidyl peptidase-4 (DPP-4) inhibitors, or an alpha-glucosidase inhibitor. Given the complexity of managing T2DM over a lifetime, most individuals with T2DM receive their diabetes care from a primary care clinician or subspecialist in endocrinology.
Experts predict that, within the next 8 years, the prevalence of obesity among adults in the United States will be approximately 50%.12 The US health care system has not been effective in controlling the obesity epidemic. Our failure to control the obesity epidemic will result in an increase in the prevalence of prediabetes and T2DM, leading to a rise in cardiovascular, renal, and eye disease. The diagnosis of prediabetes and diabetes is within the scope of practice of obstetrics and gynecology. The treatment of prediabetes is also within the scope of ObGyns, who have both expertise and familiarity in the diagnosis of gestational diabetes, a form of prediabetes. ●
The prevalence of T2DM is on the rise in the United States, and T2DM is currently the 7th leading cause of death.1 In a study of 28,143 participants in the US National Health and Nutrition Examination Survey (NHANES) who were 18 years or older, the prevalence of diabetes increased from 9.8% to 14.3% between 2000 and 2008.2 About 24% of the participants had undiagnosed diabetes prior to the testing they received as a study participant.2 People from minority groups have a higher rate of T2DM than non-Hispanic White people. Using data from 2018, the Centers for Disease Control and Prevention reported that the prevalence of diagnosed diabetes was highest among American Indians/Alaska Natives (14.7%), people of Hispanic origin (12.5%), and non-Hispanic Blacks (11.7%), followed by non-Hispanic Asians (9.2%) and non-Hispanic Whites (7.5%).1 Diabetes is a major risk factor for myocardial infarction, stroke, renal failure, retinopathy, peripheral vascular disease, and neuropathy.1 Early detection and treatment of both prediabetes and diabetes may improve health and reduce these preventable complications, saving lives, preventing heart and renal failure and blindness.
T2DM is caused by a combination of insulin resistance and insufficient pancreatic secretion of insulin to overcome the insulin resistance.3 In young adults with insulin resistance, pancreatic secretion of insulin is often sufficient to overcome the insulin resistance resulting in normal glucose levels and persistently increased insulin concentration. As individuals with insulin resistance age, pancreatic secretion of insulin may decline, resulting in insufficient production of insulin and rising glucose levels. Many individuals experience a prolonged stage of prediabetes that may be present for decades prior to transitioning to T2DM. In 2020, 35% of US adults were reported to have prediabetes.1
Screening for diabetes mellitus
The US Preventive Services Task Force (USPSTF) recently recommended that all adults aged 35 to 70 years who are overweight or obese be screened for T2DM (B recommendation).4 Screening for diabetes will also result in detecting many people with prediabetes. The criteria for diagnosing diabetes and prediabetes are presented in the TABLE. Based on cohort studies, the USPSTF noted that screening every 3 years is a reasonable approach.4 They also recommended that people diagnosed with prediabetes should initiate preventive measures, including optimizing diet, weight loss, exercise, and in some cases, medication treatment such as metformin.5
Approaches to the diagnosis of diabetes and prediabetes
Three laboratory tests are widely utilized for the diagnosis of prediabetes and diabetes: measurement of a plasma glucose 2 hours following consumption of oral glucose 75 g (2-hr oral glucose tolerance test [OGTT]), measurement of a fasting plasma glucose, and measurement of hemoglobin A1c (see Table).6In clinical practice, the best diabetes screening test is the test the patient will complete. Most evidence indicates that, compared with the 2-hr OGTT, a hemoglobin A1c measurement is specific for diagnosing T2DM, but not sensitive. In other words, if the hemoglobin A1c is ≥6.5%, the glucose measurement 2 hours following an OGTT will very likely be ≥200 mg/dL. But if the hemoglobin A1c is between 5.7% and 6.5%, the person might be diagnosed with T2DM if they had a 2-hr OGTT.6
In one study, 1,241 nondiabetic, overweight, or obese participants had all 3 tests to diagnose T2DM.7 The 2-hr OGTT diagnosed T2DM in 148 participants (12%). However, the hemoglobin A1c test only diagnosed T2DM in 78 of the 148 participants who were diagnosed with T2DM based on the 2-hr OGTT, missing 47% of the cases of T2DM. In this study, using the 2-hr OGTT as the “gold standard” reference test, the hemoglobin A1c test had a sensitivity of 53% and specificity of 97%.7
In clinical practice one approach is to explain to the patient the pros and cons of the 3 tests for T2DM and ask them to select the test they prefer to complete. In a high-risk population, including people with obesity, completing any of the 3 tests is better than not testing for diabetes. It also should be noted that, among people who have a normal body mass index (BMI), a “prediabetes” diagnosis is controversial. Compared with obese persons with prediabetes, people with a normal BMI and prediabetes diagnosed by a blood test progress to diabetes at a much lower rate. The value of diagnosing prediabetes after 70 years of age is also controversial because few people in this situation progress to diabetes.8 Clinicians should be cautious about diagnosing prediabetes in lean or elderly people.
The reliability of the hemoglobin A1c test is reduced in conditions associated with increased red blood cell turnover, including sickle cell disease, pregnancy (second and third trimesters), hemodialysis, recent blood transfusions or erythropoietin therapy. In these clinical situations, only blood glucose measurements should be used to diagnose prediabetes and T2DM.6 It should be noted that concordance among any of the 3 tests is not perfect.6
Continue to: A 2-step approach to diagnosing T2DM...
A 2-step approach to diagnosing T2DM
An alternative to relying on a single test for T2DM is to use a 2-step approach for screening. The first step is a hemoglobin A1c measurement, which neither requires fasting nor waiting for 2 hours for post–glucose load blood draw. If the hemoglobin A1c result is ≥6.5%, a T2DM diagnosis can be made, with no additional testing. If the hemoglobin A1c result is 5.7% to 6.4%, the person probably has either prediabetes or diabetes and can be offered a 2-hr OGTT to definitively determine if T2DM is the proper diagnosis. If the hemoglobin A1c test is <5.7%, it is unlikely that the person has T2DM or prediabetes at the time of the test. In this situation, the testing could be repeated in 3 years. Using a 2-step approach reduces the number of people who are tested with a 2-hr OGTT and detects more cases of T2DM than a 1-step approach that relies on a hemoglobin A1c measurement alone.
Treatment of prediabetes is warranted in people at high risk for developing diabetes
It is better to prevent diabetes among people with a high risk of diabetes than to treat diabetes once it is established. People with prediabetes who are overweight or obese are at high risk for developing diabetes. Prediabetes is diagnosed by a fasting plasma glucose level of 100 to 125 mg/dL or a hemoglobin A1c measurement of 5.7% to 6.4%.
High-quality randomized clinical trials have definitively demonstrated that, among people at high risk for developing diabetes, lifestyle modification and metformin treatment reduce the risk of developing diabetes. In the Diabetes Prevention Program (DPP) 3,234 people with a high risk of diabetes, mean BMI 34 kg/m2, were randomly assigned to 1 of 3 groups9:
- a control group
- metformin (850 mg twice daily) or
- lifestyle modification that included exercise (moderate intensity exercise for 150 minutes per week and weight loss (7% of body weight using a low-calorie, low-fat diet).
At 2.8 years of follow-up the incidence of diabetes was 11%, 7.8%, and 4.8% per 100 person-years in the people assigned to the control, metformin, and lifestyle modification groups, respectively.9 In the DPP study, compared with the control group, metformin was most effective in decreasing the risk of transitioning to diabetes in people who had a BMI ≥35 kg/m2 (53% reduction in risk) or a BMI from 30 to 35 kg/m2 (16% reduction in risk).9 Metformin was not as effective at preventing the transition to diabetes in people who had a normal BMI or who were overweight (3% reduction).9
In the Finnish Diabetes Prevention Study, 522 obese people with impaired glucose tolerance were randomly assigned to lifestyle modification or a control group. After 4 years, the cumulative incidence of diabetes was 11% and 23% in the lifestyle modification and control groups, respectively.10 A meta-analysis of 23 randomized clinical trials reported that, among people with a high risk of developing diabetes, compared with no intervention (control group), lifestyle modification, including dieting, exercising, and weight loss significantly reduced the risk of developing diabetes (pooled relative risk [RR], 0.78; 95% confidence interval [CI], 0.69‒0.88).5
In clinical practice, offering a patient at high risk for diabetes a suite of options, including5,9,10:
- a formal nutrition consult with the goal of targeting a 7% reduction in weight
- recommending moderate intensity exercise, 150 minutes weekly
- metformin treatment, if the patient is obese
would reduce the patient’s risk of developing diabetes.
Treatment of T2DM is complex
For people with T2DM, a widely recommended treatment goal is to reduce the hemoglobin A1c measurement to ≤7%. Initial treatment includes a comprehensive diabetes self-management education program, weight loss using diet and exercise, and metformin treatment. Metformin may be associated with an increased risk of lactic acidosis, especially in people with renal insufficiency. The US Food and Drug Administration (FDA) recommends against initiating metformin therapy for people with an estimated glomerular filtration rate (eGFR) of 30 to 45 mL/min/1.73 m2. The FDA determined that metformin is contraindicated in people with an eGFR of <30 mL/min/1.73 m2.11 Many people with T2DM will require treatment with multiple pharmacologic agents to achieve a hemoglobin A1c ≤7%. In addition to metformin, pharmacologic agents used to treat T2DM include insulin, sulfonylureas, glucagon-like peptide-1(GLP-1) receptor agonists, a sodium glucose cotransporter (SGLT2) inhibitor, dipeptidyl peptidase-4 (DPP-4) inhibitors, or an alpha-glucosidase inhibitor. Given the complexity of managing T2DM over a lifetime, most individuals with T2DM receive their diabetes care from a primary care clinician or subspecialist in endocrinology.
Experts predict that, within the next 8 years, the prevalence of obesity among adults in the United States will be approximately 50%.12 The US health care system has not been effective in controlling the obesity epidemic. Our failure to control the obesity epidemic will result in an increase in the prevalence of prediabetes and T2DM, leading to a rise in cardiovascular, renal, and eye disease. The diagnosis of prediabetes and diabetes is within the scope of practice of obstetrics and gynecology. The treatment of prediabetes is also within the scope of ObGyns, who have both expertise and familiarity in the diagnosis of gestational diabetes, a form of prediabetes. ●
- Centers for Disease Control and Prevention. National Diabetes Statistics Report. 2020. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed October 26, 2021.
- Wang L, Li X, Wang Z, et al. Trends in prevalence of diabetes and control of risk factors in diabetes among U.S. adults, 1999-2018. JAMA. 2021;326:1-13. doi: 10.1001/jama.2021.9883.
- Type 2 diabetes. Centers for Disease Control and Prevention website. . Last reviewed August 10, 2021 Accessed October 27, 2021.
- US Preventive Services Task Force. Screening for prediabetes and diabetes. US Preventive Services Task Force Recommendation Statement. JAMA. 2021;326:736-743. doi: 10.1001/jama.2021.12531.
- Jonas D, Crotty K, Yun JD, et al. Screening for prediabetes and type 2 diabetes mellitus: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2021;326:744-760. doi: 10.1001/jama.2021.10403.
- American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes‒2020. Diabetes Care. 2020;43(suppl 1):S14-S31. doi: 10.2337/dc20-S002.
- Meijnikman AS, De Block CE, Dirinck E, et al. Not performing an OGTT results in significant under diagnosis of (pre)diabetes in a high-risk adult Caucasian population. Int J Obes. 2017;41:1615-1620. doi: 10.1038/ijo.2017.165.
- Rooney MR, Rawlings AM, Pankow JS, et al. Risk of progression to diabetes among older adults with prediabetes. JAMA Intern Med. 2021;181:511-519. doi: 10.1001/jamainternmed.2020.8774.
- Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403. doi: 10.1056/NEJMoa012512.
- Tuomilehto J, Lindström J, Eriksson JG, et al; Finnish Diabetes Prevention Study Group. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343-1350. doi: 10.1056/NEJM200105033441801.
- Glucophage [package insert]. Princeton, NJ: Bristol Meyers Squibb; April 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017020357s037s039,021202s021s023lbl.pdf. Accessed October 27, 2021.
- Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381;2440-2450. doi: 10.1056/NEJMc1917339.
- Centers for Disease Control and Prevention. National Diabetes Statistics Report. 2020. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed October 26, 2021.
- Wang L, Li X, Wang Z, et al. Trends in prevalence of diabetes and control of risk factors in diabetes among U.S. adults, 1999-2018. JAMA. 2021;326:1-13. doi: 10.1001/jama.2021.9883.
- Type 2 diabetes. Centers for Disease Control and Prevention website. . Last reviewed August 10, 2021 Accessed October 27, 2021.
- US Preventive Services Task Force. Screening for prediabetes and diabetes. US Preventive Services Task Force Recommendation Statement. JAMA. 2021;326:736-743. doi: 10.1001/jama.2021.12531.
- Jonas D, Crotty K, Yun JD, et al. Screening for prediabetes and type 2 diabetes mellitus: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2021;326:744-760. doi: 10.1001/jama.2021.10403.
- American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes‒2020. Diabetes Care. 2020;43(suppl 1):S14-S31. doi: 10.2337/dc20-S002.
- Meijnikman AS, De Block CE, Dirinck E, et al. Not performing an OGTT results in significant under diagnosis of (pre)diabetes in a high-risk adult Caucasian population. Int J Obes. 2017;41:1615-1620. doi: 10.1038/ijo.2017.165.
- Rooney MR, Rawlings AM, Pankow JS, et al. Risk of progression to diabetes among older adults with prediabetes. JAMA Intern Med. 2021;181:511-519. doi: 10.1001/jamainternmed.2020.8774.
- Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403. doi: 10.1056/NEJMoa012512.
- Tuomilehto J, Lindström J, Eriksson JG, et al; Finnish Diabetes Prevention Study Group. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343-1350. doi: 10.1056/NEJM200105033441801.
- Glucophage [package insert]. Princeton, NJ: Bristol Meyers Squibb; April 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017020357s037s039,021202s021s023lbl.pdf. Accessed October 27, 2021.
- Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381;2440-2450. doi: 10.1056/NEJMc1917339.

