User login
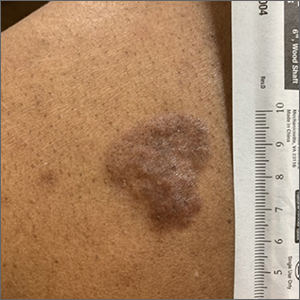
Based on the thickness and size of this irregular lesion, a punch biopsy was performed and confirmed the diagnosis of dermatofibrosarcoma protuberans (DFSP).
DFSPs are usually found on the trunk and proximal extremities; they are most often located on the chest and shoulders. The lesion usually manifests as an asymptomatic, firm, and sometimes nodular plaque that may go undiagnosed for years. DFSP is an uncommon mesenchymal tumor with uncertain etiology. It is thought that prior injury to the affected skin may result in a translocation of chromosomes 17 and 22 in skin cells, as this molecular change characterizes the vast majority of DFSPs.
Black patients are more likely than other ethnic populations to develop DFSP and its variants; there is also a slight female predominance.1 Known variants of DFSP include violaceous plaques with telangiectatic atrophic skin, and plaques with dark brown pigmentation called Bednar tumors.1,2
DFSPs are rarely metastatic, but can be locally invasive, so primary treatment consists of wide local excision or Mohs micrographic surgery (MMS). There is a higher probability for cure when MMS is utilized to treat DFSPs with the added benefit of minimizing surgical margins and preserving healthy surrounding skin. In the rarer cases of advanced local, unresectable, or metastatic disease, inhibitor therapy with imatinib or radiation therapy may be considered.2 Due to the risk of local recurrence, patients with DFSP should have regular clinical follow-up every 6 months for 5 years, followed by annual lifelong surveillance.1
This patient was referred for MMS and has not yet returned for follow-up evaluation.
Photo courtesy of Daniel Stulberg, MD. Text courtesy of Morgan Haynes, BS, University of New Mexico School of Medicine and Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Mendenhall WM, Scarborough MT, Flowers FP. Dermatofibrosarcoma protuberans: epidemiology, pathogenesis, clinical presentation, diagnosis, and staging. UpToDate. Updated March 31, 2021. Accessed February 2, 2022. www.uptodate.com/contents/dermatofibrosarcoma-protuberans-epidemiology-pathogenesis-clinical-presentation-diagnosis-and-staging
2. Brooks J, Ramsey ML. Dermatofibrosarcoma Protuberans. StatPearls. Updated November 14, 2021. Accessed January 27, 2022. www.ncbi.nlm.nih.gov/books/NBK513305
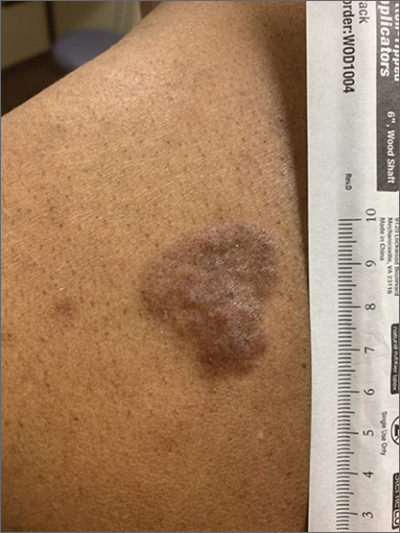
Based on the thickness and size of this irregular lesion, a punch biopsy was performed and confirmed the diagnosis of dermatofibrosarcoma protuberans (DFSP).
DFSPs are usually found on the trunk and proximal extremities; they are most often located on the chest and shoulders. The lesion usually manifests as an asymptomatic, firm, and sometimes nodular plaque that may go undiagnosed for years. DFSP is an uncommon mesenchymal tumor with uncertain etiology. It is thought that prior injury to the affected skin may result in a translocation of chromosomes 17 and 22 in skin cells, as this molecular change characterizes the vast majority of DFSPs.
Black patients are more likely than other ethnic populations to develop DFSP and its variants; there is also a slight female predominance.1 Known variants of DFSP include violaceous plaques with telangiectatic atrophic skin, and plaques with dark brown pigmentation called Bednar tumors.1,2
DFSPs are rarely metastatic, but can be locally invasive, so primary treatment consists of wide local excision or Mohs micrographic surgery (MMS). There is a higher probability for cure when MMS is utilized to treat DFSPs with the added benefit of minimizing surgical margins and preserving healthy surrounding skin. In the rarer cases of advanced local, unresectable, or metastatic disease, inhibitor therapy with imatinib or radiation therapy may be considered.2 Due to the risk of local recurrence, patients with DFSP should have regular clinical follow-up every 6 months for 5 years, followed by annual lifelong surveillance.1
This patient was referred for MMS and has not yet returned for follow-up evaluation.
Photo courtesy of Daniel Stulberg, MD. Text courtesy of Morgan Haynes, BS, University of New Mexico School of Medicine and Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
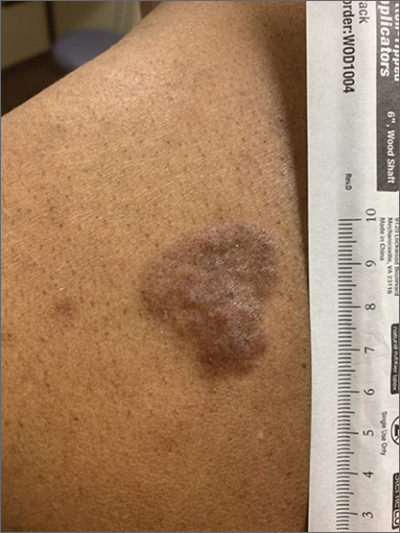
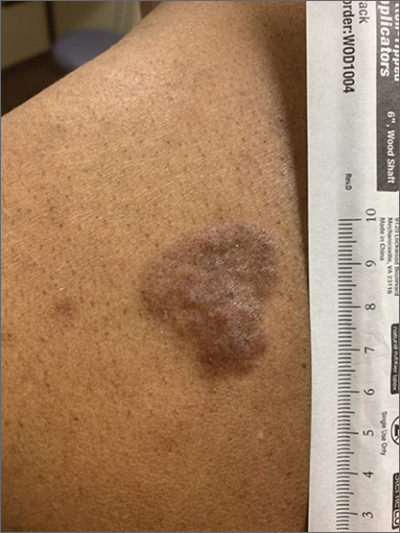
Based on the thickness and size of this irregular lesion, a punch biopsy was performed and confirmed the diagnosis of dermatofibrosarcoma protuberans (DFSP).
DFSPs are usually found on the trunk and proximal extremities; they are most often located on the chest and shoulders. The lesion usually manifests as an asymptomatic, firm, and sometimes nodular plaque that may go undiagnosed for years. DFSP is an uncommon mesenchymal tumor with uncertain etiology. It is thought that prior injury to the affected skin may result in a translocation of chromosomes 17 and 22 in skin cells, as this molecular change characterizes the vast majority of DFSPs.
Black patients are more likely than other ethnic populations to develop DFSP and its variants; there is also a slight female predominance.1 Known variants of DFSP include violaceous plaques with telangiectatic atrophic skin, and plaques with dark brown pigmentation called Bednar tumors.1,2
DFSPs are rarely metastatic, but can be locally invasive, so primary treatment consists of wide local excision or Mohs micrographic surgery (MMS). There is a higher probability for cure when MMS is utilized to treat DFSPs with the added benefit of minimizing surgical margins and preserving healthy surrounding skin. In the rarer cases of advanced local, unresectable, or metastatic disease, inhibitor therapy with imatinib or radiation therapy may be considered.2 Due to the risk of local recurrence, patients with DFSP should have regular clinical follow-up every 6 months for 5 years, followed by annual lifelong surveillance.1
This patient was referred for MMS and has not yet returned for follow-up evaluation.
Photo courtesy of Daniel Stulberg, MD. Text courtesy of Morgan Haynes, BS, University of New Mexico School of Medicine and Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Mendenhall WM, Scarborough MT, Flowers FP. Dermatofibrosarcoma protuberans: epidemiology, pathogenesis, clinical presentation, diagnosis, and staging. UpToDate. Updated March 31, 2021. Accessed February 2, 2022. www.uptodate.com/contents/dermatofibrosarcoma-protuberans-epidemiology-pathogenesis-clinical-presentation-diagnosis-and-staging
2. Brooks J, Ramsey ML. Dermatofibrosarcoma Protuberans. StatPearls. Updated November 14, 2021. Accessed January 27, 2022. www.ncbi.nlm.nih.gov/books/NBK513305
1. Mendenhall WM, Scarborough MT, Flowers FP. Dermatofibrosarcoma protuberans: epidemiology, pathogenesis, clinical presentation, diagnosis, and staging. UpToDate. Updated March 31, 2021. Accessed February 2, 2022. www.uptodate.com/contents/dermatofibrosarcoma-protuberans-epidemiology-pathogenesis-clinical-presentation-diagnosis-and-staging
2. Brooks J, Ramsey ML. Dermatofibrosarcoma Protuberans. StatPearls. Updated November 14, 2021. Accessed January 27, 2022. www.ncbi.nlm.nih.gov/books/NBK513305