User login
For people who must travel long distances east or west by air or who must work the night shift, some relief is possible for the grogginess and disorientation that often ensue. The problems arise from the body’s internal clock being out of sync with the sun. Part of the solution involves helping reset the internal clock, or sometimes, preventing it from resetting itself.
This review will focus on jet lag sleep disorder and shift work sleep disorder, with an emphasis on the causes, the clinical assessment, and evidence-based treatment options.
WHEN THE INTERNAL CLOCK IS OUT OF SYNC WITH THE SUN
Circadian rhythm sleep disorders are the result of dyssynchrony between the body’s internal clock and the external 24-hour light-dark cycle. Patients typically present with insomnia or excessive somnolence. These disorders may represent an intrinsic disorder, such as delayed or advanced sleep-phase disorder, or may be the result of transmeridian air travel or working nonstandard shifts.1
The intrinsic human circadian period is typically slightly longer than 24 hours,9 but it is synchronized (“entrained”) to the 24-hour day by various environmental inputs, or zeitgebers (German for “time-givers”), the most important of which is light exposure.10
When the internal clock is out of sync with the sun, the misalignment can result in daytime anergia, alternating complaints of insomnia and hypersomnia, and various other symptoms, including emotional disturbances and gastrointestinal distress. In particular, long-distance air travel or a nocturnal work schedule overwhelms the ability of the intrinsic clock to adjust rapidly enough, and the result is jet lag sleep disorder or shift work sleep disorder.1
TOOLS TO EVALUATE CIRCADIAN RHYTHM DISTURBANCES
A thorough history is the cornerstone of the evaluation for all sleep disorders, and if a circadian rhythm disturbance is suspected, the sleep history is supplemented with specific questions to establish a clear diagnosis.
When assessing for jet lag disorder, ask about:
- The patient’s degree of sleep deprivation before and during travel
- His or her innate circadian preference (ie, whether he or she is a “night owl” or “early bird”)
- Patterns of alcohol and caffeine consumption.
When assessing for shift work disorder, include the above questions and also look for differences in the sleep-wake schedule on working days vs nonworking days, as well as external contributors to poor sleep quality (eg, the degree to which daytime sleep is not “protected”).
The following tools help in acquiring this information.
Sleep diary
In a sleep diary or log, patients record the times that they take naps, maintain consolidated sleep, and subsequently arise. The diary also prompts the patient for information about sleep latency, wakefulness after sleep onset, time in bed, medication and caffeine intake, and the restorative quality of sleep.
While the sleep diary by itself may provide insight into counteractive sleep-related behaviors and misperceptions the patient may have, compliance is often limited. Therefore, the sleep diary is best used in conjunction with actigraphy.
Actigraphy
An actigraph is a wristwatch-size motion detector, typically worn continuously for 7 days or longer. The data it gathers and stores serve as a surrogate measure of various sleep-wake variables.11
Either a sleep diary or actigraphy is required to demonstrate the stability of sleep patterns and circadian preference, but the actigraph typically generates more reliable data.11,12 It is also valuable in assessing the response to treatment of circadian rhythm sleep disorders.13
Are you an early bird or a night owl?
The Morningness-Eveningness questionnaire contains 19 items. Night owls tend to score lower on it than early birds do.14 This information may help some people avoid situations in which they may not do well, such as an early bird going on a permanent night-shift schedule.
Other assessment tools
Polysomnography is used primarily to rule out sleep-disordered breathing; it is not indicated for routine evaluation of circadian rhythm sleep disorders.
The minimum core body temperature and the peak melatonin secretion follow a 24-hour cycle. Although these measures are often used in research, they are not routinely used in clinical practice. (The minimum core body temperature is discussed further below.)
JET LAG SLEEP DISORDER
Jet lag results from air travel across multiple time zones, with a resultant discordance between the internal circadian clock and the destination’s light-dark cycle. Most sufferers report sleeping poorly at night and feeling groggy during the day, and some also experience general malaise and gastrointestinal distress.1
The severity depends on a number of variables.
Going west is easier than going east
Westward travel is normally less taxing than eastward travel, as it requires setting one’s internal clock later rather than earlier. Presumably, because the circadian period tends to exceed 24 hours, we can move our internal clock later by about 2 hours per day, but we can move it earlier by only 1 to 1.5 hours.15,16
The more time zones crossed, the longer it takes the circadian pacemaker to re-entrain and the longer-lasting and more severe are the symptoms of jet lag. Travel across one or two time zones is only transiently troublesome.
Does age affect jet lag?
Whether age affects the severity of jet lag is not yet known.
In a study of simulated jet lag (requiring a 6-hour advance), middle-aged people (ages 37 to 52) experienced a greater degree of fragmented sleep on polysomnography than younger ones (ages 18 to 25). The older group also had greater impairment in daytime alertness, suggesting that phase tolerance—ie, the ability to sleep at an abnormal time in the circadian cycle17—decreases with age. However, two field studies involving both eastward and westward travel yielded the opposite results, suggesting that older age may actually protect against jet lag.18–20
Methodologic differences preclude direct comparisons of the studies, as do differences in the age groups studied.
Light exposure can help or hurt, depending on the timing
Our core body temperature dips to its lowest point about 2 to 3 hours before we habitually awake. Exposure to bright light in the hours leading up to this minimum (the inverted triangle in Figure 2) sets our internal clock later (a phase delay)—desirable, say, for someone travelling from New York City to Los Angeles. Conversely, exposure to bright light after this temperature minimum sets the clock earlier.
Inadvertent shifting of circadian phase in the wrong direction (“antidromic re-entrainment”) is common and delays circadian reacclimation and the dissipation of jet lag symptoms.
We discuss ways to reduce antidromic reentrainment in more detail further below.
Other factors
Other factors that contribute to travel fatigue include sleep deprivation (before the flight or en route), acute discomfort as the plane ascends to its cruising altitude,25 and excessive alcohol or caffeine intake during the flight. Although the effects of these factors rapidly diminish once one reaches the travel destination, jet lag will persist until circadian re-entrainment occurs.15
NONDRUG THERAPIES FOR JET LAG SLEEP DISORDER
The goal of treatment is to realign the circadian rhythm in the most rapid and efficient way and to minimize symptoms in the meantime. Frequent shifts to different time zones, often required in business travel, are very difficult to accommodate, and business travelers actually may do better if they remain on their home-based schedule.
One study compared keeping home-based sleep hours as opposed to adopting local sleep hours during a 2-day stay after a 9-hour westward flight.26 Travelers who remained on home-based hours were less sleepy and had lower (ie, better) global jet lag ratings than those who adopted local sleep hours, in part because of better sleep quality and duration. Nevertheless, about one-third of the participants said they preferred to adhere to the local schedule.
Strategic avoidance of, and exposure to, light
If the traveler intends to remain at the destination long enough, he or she can adjust better (and avoid an antidromic process) via strategic avoidance of and exposure to light.24
People travelling east, who want to set their clocks ahead (a phase advance), need to keep to the dark in the 3 hours leading up to the time they reach their minimum core body temperature (depicted as “D” in Figure 3), and then expose themselves to light in the 3 hours immediately after (“L” in Figure 3). Thus, the traveler from Chicago to Paris would do better by avoiding light exposure on arrival, either by remaining in darkness in his or her hotel room, or by wearing dark sunglasses when outdoors. Wearing sunglasses during transit to the hotel would also help avoid light exposure.
When attempting to delay circadian rhythms, the opposite light-dark patterns are sought, as depicted in Figure 4. As flight and layover patterns often do not permit strict adherence to these measures, they represent idealized scenarios.
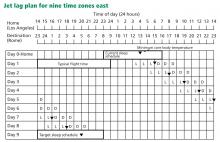
The first step is to make a grid with a concurrent listing of home and destination times. In the example in Figure 3, the person is traveling seven time zones east. On day 0, a rectangle is drawn around the times representing home-based sleep hours.
Next, we mark the time at which we expect the traveler’s core body temperature to reach its minimum (inverted triangle). If the person habitually sleeps no more than 7 hours per night, then we mark this point as 2 hours before his or her habitual wake-up time; if the person sleeps more than 7 hours, then we place it 3 hours before wake-up time.23,29 This process is repeated at the bottom of the grid to represent the desired sleep schedule at the traveler’s destination. The distance between the home and the destination-based minimum core body temperature symbols represents the required degree of circadian realignment.
If a phase advance is required (eg, if travelling from Chicago to Paris), the core body temperature symbol is drawn on day 1 in the same location as day 0. For each subsequent day, the symbol is moved 1 hour earlier (which is about how fast the internal clock can advance),15,27 until a clock time within 1 hour of the desired destination core body temperature time is reached or satisfactory sleep and daytime functioning are achieved (Figure 3). If a phase delay is required (eg, if travelling from New York City to Los Angeles), the symbol is drawn 2 hours later on day 1 than on day 0 (reflecting the greater ease at which delays are achieved),15,27 with subsequent daily shifts in 2-hour increments, again until a clock time within 1 hour of the desired destination minimum core body temperature time is reached or satisfactory sleep and daytime functioning are achieved.
Requirements for darkness can be met with protective eyewear (ie, dark sunglasses), or by remaining in a dark room. Light requirements can be met with outdoor exposure, with a commercial light box, or with a separate apparatus (eg, goggles, visors) portable enough for travel.
DRUGS TO TREAT JET LAG SLEEP DISORDER
Melatonin appears safe
Most field studies have found that nightly doses of melatonin (2–8 mg) improve the quality of sleep30–32 or alleviate daytime symptoms of jet lag, or both.20,30,31,33–36 Immediate-release preparations appear to be more effective than slow-release ones.31 Although most studies looked exclusively at adaptation to eastward travel,30–32,35,36 one studied westward travel,33 and another assessed melatonin’s effects during both departure and return trips that traversed 11 time zones.34
In studies of preflight dosing, melatonin was scheduled for up to 3 days before departure (and en route in two instances),30,34 at clock hours corresponding to the nocturnal sleep period at the travel destination (consistent times daily), and then for a subsequent 3 to 4 days between a destination time of 22:00 and 00:00 hours (ie, at bedtime).30,31,34–36 Several other studies further simplified this regimen, with participants taking nocturnal melatonin only on arrival at the destination, either for eastward31,32 or for westward travel.33
The study involving solely westward travel (Los Angeles to New Zealand) was the only one of the studies with positive findings that allowed for comparisons between participants who received melatonin before departure (3 days at 5-mg doses, taken between 07:00 and 08:00 Los Angeles time) and continuing for 5 days after arrival at 22:00 to 00:00 New Zealand time, and those who received melatonin beginning only on arrival.33 Significantly better jet lag outcomes were found in the latter group.
An important caveat is that melatonin is sold over the counter as a nutritional supplement and is not regulated by the United States Food and Drug Administration (FDA), so verification of purity of the product is difficult.
A comprehensive review by the National Academy of Sciences stated that, given the available data, short-term use of melatonin in total daily doses of 10 mg or less in healthy adults appears to be safe.37
Benzodiazepine receptor agonists improve sleep, but maybe not sleepiness
The use of standard hypnotics during periods of circadian realignment appears to be commonplace but has not been well studied.20 Trials of the newer benzodiazepine receptor agonists—three studies of zolpidem (Ambien) 10 mg30,38,39 and two of zopiclone 5 to 7.5 mg32,40—found consistently favorable subjective30,38 and objective32,39,40 outcomes in counteracting jet-lag-induced insomnia (for both eastward and westward travel). (Note: Zopiclone is not available in the United States, but its enantiomer eszopiclone [Lunesta] is.) However, the evidence is less clear for daytime symptoms of jet lag, with outcomes reported as favorable,30 equivocal,40 or inaccessible.32,38,39
The discrepancy between studies incorporating systematic daytime assessments may be due to differential medication effects (zolpidem vs zopiclone).
In two studies that compared these standard hypnotics to oral melatonin, one found that zopiclone 5 mg and melatonin 2 mg were equally beneficial with respect to sleep variables (other jet lag symptoms were not assessed).32 In another study, zolpidem 10 mg was superior to melatonin 5 mg for sleep and other jet lag symptoms, and the combination of zolpidem and melatonin was no better than zolpidem alone.30
Importantly, however, adverse effects were more frequent in those taking zolpidem and included nausea, vomiting, and confusion.30 Although these effects were not deemed serious, 14 participants (10%) withdrew from the study.
Stimulants
Caffeine is commonly used to combat the sleepiness of jet lag, but only two controlled field studies have assessed its efficacy.41,42 Both used slow-release preparations at a daily dosage of 300 mg.
In one study, after an eastward flight traversing seven time zones, participants took the pill at 08:00 destination time every day for 5 days.41 Curiously, alertness and other jet lag symptoms were not assessed, but circadian rhythms (determined by levels of cortisol in saliva) were re-entrained at a more rapid rate with caffeine than with placebo, and to a degree comparable with that achieved by exogenous melatonin.
In a follow-up study by the same group, those receiving caffeine were objectively less sleepy (as assessed by multiple sleep latency tests) than those taking melatonin or placebo, but subjective differences between groups were not identified.42 Furthermore, those taking caffeine had significantly more nocturnal sleep complaints, as assessed both objectively and subjectively.
A recent randomized, double-blind, placebo-controlled trial of the stimulant armodafinil (Nuvigil) found less sleepiness on multiple sleep latency testing and a decrease in jet leg symptoms with a dosage of 150 mg than with placebo.43
SHIFT WORK SLEEP DISORDER: DEFINITION, PREDISPOSING FACTORS
Shift work refers to nonstandard work schedules, including on-call duty, rotating shifts, and permanent night work. In the United States, one in five workers works a nonstandard shift.20
While shift work presents obvious difficulties, the diagnosis of shift work sleep disorder is reserved for those who have chronic insomnia or sleepiness at times that are not conducive to the externally demanded sleep-wake schedule, despite having the opportunity for sufficient daytime sleep.1 When defined in such a fashion, this disorder may afflict nearly a third of workers,44 with potential adverse effects on safety, health, and quality of life.
Older age is considered a risk factor for intolerance to shift work.20 In a study of physiologic phase shifts in response to night work, older workers were less able to recover after several night shifts.45 A large survey of police officers working the night shift supported the finding of more sleep disruption and on-duty sleepiness in older people.46
TREATMENT OF SHIFT WORK SLEEP DISORDER
Bright light at work, sunglasses on the way home
Various field studies have described hastening of circadian adaptation (and immediate alerting effects) during night shifts with the use of bright light.20
Boivin and James47 found that workers who received 6 hours of intermittent bright light during their shifts experienced significantly greater phase delays than those who received no such intervention. Those receiving bright light also wore sunglasses during the commute home (to protect from an undesired phase advance), and this has demonstrated favorable effects as an independent intervention.48
Drug treatment of shift work sleep disorder
Melatonin: Mixed results. Two field studies found that taking melatonin (5–6 mg) before the daytime sleep period had a favorable impact on subjective sleep quality.49,50 However, two other studies found no such benefit with doses ranging from 6 to 10 mg.51,52 Differences between these studies—eg, shift schedules, dosages, and the time the melatonin was taken—preclude definitive comparisons.
Effects of melatonin on workplace alertness are indeterminate because of inconsistent measurements of this variable. Importantly, a simulated shift work study found no phase-shifting advantages of melatonin in those who concomitantly used bright light during their work shift with or without morning protective eyewear.48
Hypnotic drugs. In simulation studies and field studies, people taking benzodiazepine receptor agonists have consistently said they sleep better.53–58 A simulation study noted additional benefit in the ability to stay alert during the night shift (assessed by maintenance of wakefulness testing),55 but two other studies saw no changes in manifest sleepiness (assessed with multiple sleep latency tests).53,54 These divergent findings may represent different effects on these two dimensions of sleepiness.
The only field study to assess post-sleep psychomotor performance found no impairments after taking 7.5 mg of zopiclone, a relatively long-acting nonbenzodiazepine hypnotic.57
Stimulants. In the largest trial to date of shift work sleep disorder, modafinil 200 mg (the only drug currently FDA-approved for shift work sleep disorder) had significant benefits compared with placebo with respect to objective measurements of workplace sleepiness, reaction time performance testing, and self-rated improvement of symptoms.59 Perhaps because of the low dose studied, both treated and untreated patients continued to manifest sleepiness within the pathologic range on objective testing.
Although the efficacy of caffeine is well documented as a countermeasure for sleepiness during experimentally induced sleep deprivation,20 very few field trials have specifically addressed impairments associated with shift work sleep disorder. In one study, caffeine at a dose of 4 mg/kg taken 30 minutes before starting a night shift provided objective improvement in both performance and alertness.60
Strategic napping is an additional practical intervention to promote alertness during night shifts, and cumulative data indicate that it provides objective and subjective improvements in alertness and performance.61,62 Earlier timed naps (ie, before or during the early portion of a shift) of short duration (ie, 20 minutes or less) are likely to produce maximal benefit, because they avoid sleep inertia (the grogginess or sleepiness that may follow a long nap), and also because they have no effect on the subsequent daytime sleep bout.61,63
Interventions may also be used in combination. For example, napping in conjunction with caffeine results in a greater degree of increased objective alertness than either intervention alone.60
How about days off?
The recommendations described here presume that shift workers maintain the workday sleep-wake schedule continuously, including when they are not at work. This is likely not a real-world scenario.
Smith et al64 developed a “compromise” phase position, whereby internal rhythms are optimized to facilitate alertness during work and sleepiness during the day, while allowing one to adopt a non-workday sleep schedule that maintains accessibility to family and social activities. In brief, non-workday sleep starts about 5.5 hours earlier than workday sleep; all sleep bouts are followed by brief exposure to bright light (to avoid excessive phase delay); and, as described previously, both workplace bright light and protection from morning light are implemented.
Although further studies are needed to determine whether this regimen is practical in real life, study participants who achieved desired partial phase shifts had performance ratings on a par with baseline levels, and comparable to those in a group that achieved complete re-entrainment.64
Finally, all shift workers need to be encouraged to protect the daytime bedroom environment just as daytime workers protect their nighttime environment. Sleep should be sought in an appropriately darkened and quiet environment, phones and doorbells silenced, and appointments scheduled accordingly.
- International Classification of Sleep Disorders: Diagnostic and Coding Manual/American Academy of Sleep Medicine. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005.
- Borbély AA, Achermann P. Concepts and models of sleep regulation: an overview. J Sleep Res 1992; 1:63–79.
- Carskadon MA, Dement WC. Effects of total sleep loss on sleep tendency. Percept Mot Skills 1979; 48:495–506.
- Beersma DG, Gordijn MC. Circadian control of the sleep-wake cycle. Physiol Behav 2007; 90:190–195.
- Moore RY, Eichler VB. Loss of a circadian adrenal corticosterone rhythm following suprachiasmatic lesions in the rat. Brain Res 1972; 42:201–206.
- Stephan FK, Zucker I. Circadian rhythms in drinking behavior and locomotor activity of rats are eliminated by hypothalamic lesions. Proc Natl Acad Sci U S A 1972; 69:1583–1586.
- Welsh DK, Logothetis DE, Meister M, Reppert SM. Individual neurons dissociated from rat suprachiasmatic nucleus express independently phased circadian firing rhythms. Neuron 1995; 14:697–706.
- Ralph MR, Foster RG, Davis FC, Menaker M. Transplanted suprachiasmatic nucleus determines circadian period. Science 1990; 247:975–978.
- Czeisler CA, Duffy JF, Shanahan TL, et al. Stability, precision, and near-24-hour period of the human circadian pacemaker. Science 1999; 284:2177–2181.
- Waterhouse JM, DeCoursey PJ. Human circadian organization. In:Dunlap JC, Loros JJ, DeCoursey PJ, editors. Chronobiology: Biological Timekeeping. Sunderland, MA: Sinauer Associates; 2004:291–324.
- Morgenthaler T, Alessi C, Friedman L, et al; Standards of Practice Committee; American Academy of Sleep Medicine. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007. Sleep 2007; 30:519–529.
- Bradshaw DA, Yanagi MA, Pak ES, Peery TS, Ruff GA. Nightly sleep duration in the 2-week period preceding multiple sleep latency testing. J Clin Sleep Med 2007; 3:613–619.
- Morgenthaler TI, Lee-Chiong T, Alessi C, et al; Standards of Practice Committee of the American Academy of Sleep Medicine. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report. Sleep 2007; 30:1445–1459.
- Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol 1976; 4:97–110.
- Waterhouse J, Reilly T, Atkinson G, Edwards B. Jet lag: trends and coping strategies. Lancet 2007; 369:1117–1129.
- Eastman CI, Gazda CJ, Burgess HJ, Crowley SJ, Fogg LF. Advancing circadian rhythms before eastward flight: a strategy to prevent or reduce jet lag. Sleep 2005; 28:33–44.
- Moline ML, Pollak CP, Monk TH, et al. Age-related differences in recovery from simulated jet lag. Sleep 1992; 15:28–40.
- Waterhouse J, Edwards B, Nevill A, et al. Identifying some determinants of “jet lag” and its symptoms: a study of athletes and other travellers. Br J Sports Med 2002; 36:54–60.
- Tresguerres JA, Ariznavarreta C, Granados B, et al. Circadian urinary 6-sulphatoxymelatonin, cortisol excretion and locomotor activity in airline pilots during transmeridian flights. J Pineal Res 2001; 31:16–22.
- Sack RL, Auckley D, Auger RR, et al; American Academy of Sleep Medicine. Circadian rhythm sleep disorders: part I, basic principles, shift work and jet lag disorders. An American Academy of Sleep Medicine review. Sleep 2007; 30:1460–1483.
- Burgess HJ, Sharkey KM, Eastman CI. Bright light, dark and melatonin can promote circadian adaptation in night shift workers. Sleep Med Rev 2002; 6:407–420.
- Lewy AJ, Bauer VK, Saeeduddin A, et al. The human phase response curve (PRC) to melatonin is about 12 hours out of phase with the PRC to light. Chronobiol Int 1998; 15:71–83.
- Burgess HJ, Eastman CT. Prevention of Jet Lag. 2010. http://pier.acponline.org/physicians/screening/prev1015/prev1015.html. Accessed June 25, 2010.
- Daan S, Lewy AJ. Scheduled exposure to daylight: a potential strategy to reduce “jet lag” following transmeridian flight. Psychopharmacol Bull 1984; 20:566–568.
- Muhm JM, Rock PB, McMullin DL, et al. Effect of aircraft-cabin altitude on passenger discomfort. N Engl J Med 2007; 357:18–27.
- Lowden A, Akerstedt T. Retaining home-base sleep hours to prevent jet lag in connection with a westward flight across nine time zones. Chronobiol Int 1998; 15:365–376.
- Eastman CI, Burgess HJ. How to travel the world without jet lag. Sleep Med Clin 2009; 4:241–255.
- Revell VL, Eastman CI. How to trick mother nature into letting you fly around or stay up all night. J Biol Rhythms 2005; 20:353–365.
- Cagnacci A, Elliott JA, Yen SS. Melatonin: a major regulator of the circadian rhythm of core temperature in humans. J Clin Endocrinol Metab 1992; 75:447–452.
- Suhner A, Schlagenhauf P, Höfer I, Johnson R, Tschopp A, Steffen R. Effectiveness and tolerability of melatonin and zolpidem for the alleviation of jet lag. Aviat Space Environ Med 2001; 72:638–646.
- Suhner A, Schlagenhauf P, Johnson R, Tschopp A, Steffen R. Comparative study to determine the optimal melatonin dosage form for the alleviation of jet lag. Chronobiol Int 1998; 15:655–666.
- Paul MA, Gray G, Sardana TM, Pigeau RA. Melatonin and zopiclone as facilitators of early circadian sleep in operational air transport crews. Aviat Space Environ Med 2004; 75:439–443.
- Petrie K, Dawson AG, Thompson L, Brook R. A double-blind trial of melatonin as a treatment for jet lag in international cabin crew. Biol Psychiatry 1993; 33:526–530.
- Petrie K, Conaglen JV, Thompson L, Chamberlain K. Effect of melatonin on jet lag after long haul flights. BMJ 1989; 298:705–707.
- Arendt J, Aldhous M, Marks V. Alleviation of jet lag by melatonin: preliminary results of controlled double blind trial. Br Med J (Clin Res Ed) 1986; 292:1170.
- Claustrat B, Brun J, David M, Sassolas G, Chazot G. Melatonin and jet lag: confirmatory result using a simplified protocol. Biol Psychiatry 1992; 32:705–711.
- Committee on the Framework for Evaluating the Safety of Dietary Supplements, Food and Nutrition Board, Board on Life Sciences, Institute of Medicine and National Research Council of the National Academies. Dietary supplements: a framework for evaluating safety. Washington, DC: The National Academies Press; 2005.
- Jamieson AO, Zammit GK, Rosenberg RS, Davis JR, Walsh JK. Zolpidem reduces the sleep disturbance of jet lag. Sleep Med 2001; 2:423–430.
- Hirschfeld U, Moreno-Reyes R, Akseki E, et al. Progressive elevation of plasma thyrotropin during adaptation to simulated jet lag: effects of treatment with bright light or zolpidem. J Clin Endocrinol Metab 1996; 81:3270–3277.
- Daurat A, Benoit O, Buguet A. Effects of zopiclone on the rest/activity rhythm after a westward flight across five time zones. Psychopharmacology (Berl) 2000; 149:241–245.
- Piérard C, Beaumont M, Enslen M, et al. Resynchronization of hormonal rhythms after an eastbound flight in humans: effects of slow-release caffeine and melatonin. Eur J Appl Physiol 2001; 85:144–150.
- Beaumont M, Batéjat D, Piérard C, et al. Caffeine or melatonin effects on sleep and sleepiness after rapid eastward transmeridian travel. J Appl Physiol 2004; 96:50–58.
- Rosenberg RP, Bogan RK, Tiller JM, et al. A phase 3, double-blind, randomized, placebo-controlled study of armodafinil for excessive sleepiness associated with jet lag disorder. Mayo Clin Proc 2010; 85:630–638.
- Drake CL, Roehrs T, Richardson G, Walsh JK, Roth T. Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep 2004; 27:1453–1462.
- Härmä MI, Hakola T, Akerstedt T, Laitinen JT. Age and adjustment to night work. Occup Environ Med 1994; 51:568–573.
- Smith L, Mason C. Reducing night shift exposure: a pilot study of rota, night shift and age effects on sleepiness and fatigue. J Hum Ergol (Tokyo) 2001; 30:83–87.
- Boivin DB, James FO. Circadian adaptation to night-shift work by judicious light and darkness exposure. J Biol Rhythms 2002; 17:556–567.
- Crowley SJ, Lee C, Tseng CY, Fogg LF, Eastman CI. Combinations of bright light, scheduled dark, sunglasses, and melatonin to facilitate circadian entrainment to night shift work. J Biol Rhythms 2003; 18:513–523.
- Folkard S, Arendt J, Clark M. Can melatonin improve shift workers’ tolerance of the night shift? Some preliminary findings. Chronobiol Int 1993; 10:315–320.
- Yoon IY, Song BG. Role of morning melatonin administration and attenuation of sunlight exposure in improving adaptation of nightshift workers. Chronobiol Int 2002; 19:903–913.
- James M, Tremea MO, Jones JS, Krohmer JR. Can melatonin improve adaptation to night shift? Am J Emerg Med 1998; 16:367–370.
- Jorgensen KM, Witting MD. Does exogenous melatonin improve day sleep or night alertness in emergency physicians working night shifts? Ann Emerg Med 1998; 31:699–704.
- Walsh JK, Schweitzer PK, Anch AM, Muehlbach MJ, Jenkins NA, Dickins QS. Sleepiness/alertness on a simulated night shift following sleep at home with triazolam. Sleep 1991; 14:140–146.
- Walsh JK, Sugerman JL, Muehlbach MJ, Schweitzer PK. Physiological sleep tendency on a simulated night shift: adaptation and effects of triazolam. Sleep 1988; 11:251–264.
- Porcù S, Bellatreccia A, Ferrara M, Casagrande M. Performance, ability to stay awake, and tendency to fall asleep during the night after a diurnal sleep with temazepam or placebo. Sleep 1997; 20:535–541.
- Monchesky TC, Billings BJ, Phillips R, Bourgouin J. Zopiclone in insomniac shiftworkers. Evaluation of its hypnotic properties and its effects on mood and work performance. Int Arch Occup Environ Health 1989; 61:255–259.
- Moon CA, Hindmarch I, Holland RL. The effect of zopiclone 7.5 mg on the sleep, mood and performance of shift workers. Int Clin Psychopharmacol 1990; 5(suppl 2):79–83.
- Puca FM, Perrucci S, Prudenzano MP, et al. Quality of life in shift work syndrome. Funct Neurol 1996; 11:261–268.
- Czeisler CA, Walsh JK, Roth T, et al; US Modafinil in Shift Work Sleep Disorder Study Group. Modafinil for excessive sleepiness associated with shift-work sleep disorder. N Engl J Med 2005; 353:476–486.
- Schweitzer PK, Randazzo AC, Stone K, Erman M, Walsh JK. Laboratory and field studies of naps and caffeine as practical countermeasures for sleep-wake problems associated with night work. Sleep 2006; 29:39–50.
- Sallinen M, Härmä M, Akerstedt T, Rosa R, Lillqvist O. Promoting alertness with a short nap during a night shift. J Sleep Res 1998; 7:240–247.
- Garbarino S, Mascialino B, Penco MA, et al. Professional shift-work drivers who adopt prophylactic naps can reduce the risk of car accidents during night work. Sleep 2004; 27:1295–1302.
- Purnell MT, Feyer AM, Herbison GP. The impact of a nap opportunity during the night shift on the performance and alertness of 12-h shift workers. J Sleep Res 2002; 11:219–227.
- Smith MR, Fogg LF, Eastman CI. A compromise circadian phase position for permanent night work improves mood, fatigue, and performance. Sleep 2009; 32:1481–1489.
For people who must travel long distances east or west by air or who must work the night shift, some relief is possible for the grogginess and disorientation that often ensue. The problems arise from the body’s internal clock being out of sync with the sun. Part of the solution involves helping reset the internal clock, or sometimes, preventing it from resetting itself.
This review will focus on jet lag sleep disorder and shift work sleep disorder, with an emphasis on the causes, the clinical assessment, and evidence-based treatment options.
WHEN THE INTERNAL CLOCK IS OUT OF SYNC WITH THE SUN
Circadian rhythm sleep disorders are the result of dyssynchrony between the body’s internal clock and the external 24-hour light-dark cycle. Patients typically present with insomnia or excessive somnolence. These disorders may represent an intrinsic disorder, such as delayed or advanced sleep-phase disorder, or may be the result of transmeridian air travel or working nonstandard shifts.1
The intrinsic human circadian period is typically slightly longer than 24 hours,9 but it is synchronized (“entrained”) to the 24-hour day by various environmental inputs, or zeitgebers (German for “time-givers”), the most important of which is light exposure.10
When the internal clock is out of sync with the sun, the misalignment can result in daytime anergia, alternating complaints of insomnia and hypersomnia, and various other symptoms, including emotional disturbances and gastrointestinal distress. In particular, long-distance air travel or a nocturnal work schedule overwhelms the ability of the intrinsic clock to adjust rapidly enough, and the result is jet lag sleep disorder or shift work sleep disorder.1
TOOLS TO EVALUATE CIRCADIAN RHYTHM DISTURBANCES
A thorough history is the cornerstone of the evaluation for all sleep disorders, and if a circadian rhythm disturbance is suspected, the sleep history is supplemented with specific questions to establish a clear diagnosis.
When assessing for jet lag disorder, ask about:
- The patient’s degree of sleep deprivation before and during travel
- His or her innate circadian preference (ie, whether he or she is a “night owl” or “early bird”)
- Patterns of alcohol and caffeine consumption.
When assessing for shift work disorder, include the above questions and also look for differences in the sleep-wake schedule on working days vs nonworking days, as well as external contributors to poor sleep quality (eg, the degree to which daytime sleep is not “protected”).
The following tools help in acquiring this information.
Sleep diary
In a sleep diary or log, patients record the times that they take naps, maintain consolidated sleep, and subsequently arise. The diary also prompts the patient for information about sleep latency, wakefulness after sleep onset, time in bed, medication and caffeine intake, and the restorative quality of sleep.
While the sleep diary by itself may provide insight into counteractive sleep-related behaviors and misperceptions the patient may have, compliance is often limited. Therefore, the sleep diary is best used in conjunction with actigraphy.
Actigraphy
An actigraph is a wristwatch-size motion detector, typically worn continuously for 7 days or longer. The data it gathers and stores serve as a surrogate measure of various sleep-wake variables.11
Either a sleep diary or actigraphy is required to demonstrate the stability of sleep patterns and circadian preference, but the actigraph typically generates more reliable data.11,12 It is also valuable in assessing the response to treatment of circadian rhythm sleep disorders.13
Are you an early bird or a night owl?
The Morningness-Eveningness questionnaire contains 19 items. Night owls tend to score lower on it than early birds do.14 This information may help some people avoid situations in which they may not do well, such as an early bird going on a permanent night-shift schedule.
Other assessment tools
Polysomnography is used primarily to rule out sleep-disordered breathing; it is not indicated for routine evaluation of circadian rhythm sleep disorders.
The minimum core body temperature and the peak melatonin secretion follow a 24-hour cycle. Although these measures are often used in research, they are not routinely used in clinical practice. (The minimum core body temperature is discussed further below.)
JET LAG SLEEP DISORDER
Jet lag results from air travel across multiple time zones, with a resultant discordance between the internal circadian clock and the destination’s light-dark cycle. Most sufferers report sleeping poorly at night and feeling groggy during the day, and some also experience general malaise and gastrointestinal distress.1
The severity depends on a number of variables.
Going west is easier than going east
Westward travel is normally less taxing than eastward travel, as it requires setting one’s internal clock later rather than earlier. Presumably, because the circadian period tends to exceed 24 hours, we can move our internal clock later by about 2 hours per day, but we can move it earlier by only 1 to 1.5 hours.15,16
The more time zones crossed, the longer it takes the circadian pacemaker to re-entrain and the longer-lasting and more severe are the symptoms of jet lag. Travel across one or two time zones is only transiently troublesome.
Does age affect jet lag?
Whether age affects the severity of jet lag is not yet known.
In a study of simulated jet lag (requiring a 6-hour advance), middle-aged people (ages 37 to 52) experienced a greater degree of fragmented sleep on polysomnography than younger ones (ages 18 to 25). The older group also had greater impairment in daytime alertness, suggesting that phase tolerance—ie, the ability to sleep at an abnormal time in the circadian cycle17—decreases with age. However, two field studies involving both eastward and westward travel yielded the opposite results, suggesting that older age may actually protect against jet lag.18–20
Methodologic differences preclude direct comparisons of the studies, as do differences in the age groups studied.
Light exposure can help or hurt, depending on the timing
Our core body temperature dips to its lowest point about 2 to 3 hours before we habitually awake. Exposure to bright light in the hours leading up to this minimum (the inverted triangle in Figure 2) sets our internal clock later (a phase delay)—desirable, say, for someone travelling from New York City to Los Angeles. Conversely, exposure to bright light after this temperature minimum sets the clock earlier.
Inadvertent shifting of circadian phase in the wrong direction (“antidromic re-entrainment”) is common and delays circadian reacclimation and the dissipation of jet lag symptoms.
We discuss ways to reduce antidromic reentrainment in more detail further below.
Other factors
Other factors that contribute to travel fatigue include sleep deprivation (before the flight or en route), acute discomfort as the plane ascends to its cruising altitude,25 and excessive alcohol or caffeine intake during the flight. Although the effects of these factors rapidly diminish once one reaches the travel destination, jet lag will persist until circadian re-entrainment occurs.15
NONDRUG THERAPIES FOR JET LAG SLEEP DISORDER
The goal of treatment is to realign the circadian rhythm in the most rapid and efficient way and to minimize symptoms in the meantime. Frequent shifts to different time zones, often required in business travel, are very difficult to accommodate, and business travelers actually may do better if they remain on their home-based schedule.
One study compared keeping home-based sleep hours as opposed to adopting local sleep hours during a 2-day stay after a 9-hour westward flight.26 Travelers who remained on home-based hours were less sleepy and had lower (ie, better) global jet lag ratings than those who adopted local sleep hours, in part because of better sleep quality and duration. Nevertheless, about one-third of the participants said they preferred to adhere to the local schedule.
Strategic avoidance of, and exposure to, light
If the traveler intends to remain at the destination long enough, he or she can adjust better (and avoid an antidromic process) via strategic avoidance of and exposure to light.24
People travelling east, who want to set their clocks ahead (a phase advance), need to keep to the dark in the 3 hours leading up to the time they reach their minimum core body temperature (depicted as “D” in Figure 3), and then expose themselves to light in the 3 hours immediately after (“L” in Figure 3). Thus, the traveler from Chicago to Paris would do better by avoiding light exposure on arrival, either by remaining in darkness in his or her hotel room, or by wearing dark sunglasses when outdoors. Wearing sunglasses during transit to the hotel would also help avoid light exposure.
When attempting to delay circadian rhythms, the opposite light-dark patterns are sought, as depicted in Figure 4. As flight and layover patterns often do not permit strict adherence to these measures, they represent idealized scenarios.
The first step is to make a grid with a concurrent listing of home and destination times. In the example in Figure 3, the person is traveling seven time zones east. On day 0, a rectangle is drawn around the times representing home-based sleep hours.
Next, we mark the time at which we expect the traveler’s core body temperature to reach its minimum (inverted triangle). If the person habitually sleeps no more than 7 hours per night, then we mark this point as 2 hours before his or her habitual wake-up time; if the person sleeps more than 7 hours, then we place it 3 hours before wake-up time.23,29 This process is repeated at the bottom of the grid to represent the desired sleep schedule at the traveler’s destination. The distance between the home and the destination-based minimum core body temperature symbols represents the required degree of circadian realignment.
If a phase advance is required (eg, if travelling from Chicago to Paris), the core body temperature symbol is drawn on day 1 in the same location as day 0. For each subsequent day, the symbol is moved 1 hour earlier (which is about how fast the internal clock can advance),15,27 until a clock time within 1 hour of the desired destination core body temperature time is reached or satisfactory sleep and daytime functioning are achieved (Figure 3). If a phase delay is required (eg, if travelling from New York City to Los Angeles), the symbol is drawn 2 hours later on day 1 than on day 0 (reflecting the greater ease at which delays are achieved),15,27 with subsequent daily shifts in 2-hour increments, again until a clock time within 1 hour of the desired destination minimum core body temperature time is reached or satisfactory sleep and daytime functioning are achieved.
Requirements for darkness can be met with protective eyewear (ie, dark sunglasses), or by remaining in a dark room. Light requirements can be met with outdoor exposure, with a commercial light box, or with a separate apparatus (eg, goggles, visors) portable enough for travel.
DRUGS TO TREAT JET LAG SLEEP DISORDER
Melatonin appears safe
Most field studies have found that nightly doses of melatonin (2–8 mg) improve the quality of sleep30–32 or alleviate daytime symptoms of jet lag, or both.20,30,31,33–36 Immediate-release preparations appear to be more effective than slow-release ones.31 Although most studies looked exclusively at adaptation to eastward travel,30–32,35,36 one studied westward travel,33 and another assessed melatonin’s effects during both departure and return trips that traversed 11 time zones.34
In studies of preflight dosing, melatonin was scheduled for up to 3 days before departure (and en route in two instances),30,34 at clock hours corresponding to the nocturnal sleep period at the travel destination (consistent times daily), and then for a subsequent 3 to 4 days between a destination time of 22:00 and 00:00 hours (ie, at bedtime).30,31,34–36 Several other studies further simplified this regimen, with participants taking nocturnal melatonin only on arrival at the destination, either for eastward31,32 or for westward travel.33
The study involving solely westward travel (Los Angeles to New Zealand) was the only one of the studies with positive findings that allowed for comparisons between participants who received melatonin before departure (3 days at 5-mg doses, taken between 07:00 and 08:00 Los Angeles time) and continuing for 5 days after arrival at 22:00 to 00:00 New Zealand time, and those who received melatonin beginning only on arrival.33 Significantly better jet lag outcomes were found in the latter group.
An important caveat is that melatonin is sold over the counter as a nutritional supplement and is not regulated by the United States Food and Drug Administration (FDA), so verification of purity of the product is difficult.
A comprehensive review by the National Academy of Sciences stated that, given the available data, short-term use of melatonin in total daily doses of 10 mg or less in healthy adults appears to be safe.37
Benzodiazepine receptor agonists improve sleep, but maybe not sleepiness
The use of standard hypnotics during periods of circadian realignment appears to be commonplace but has not been well studied.20 Trials of the newer benzodiazepine receptor agonists—three studies of zolpidem (Ambien) 10 mg30,38,39 and two of zopiclone 5 to 7.5 mg32,40—found consistently favorable subjective30,38 and objective32,39,40 outcomes in counteracting jet-lag-induced insomnia (for both eastward and westward travel). (Note: Zopiclone is not available in the United States, but its enantiomer eszopiclone [Lunesta] is.) However, the evidence is less clear for daytime symptoms of jet lag, with outcomes reported as favorable,30 equivocal,40 or inaccessible.32,38,39
The discrepancy between studies incorporating systematic daytime assessments may be due to differential medication effects (zolpidem vs zopiclone).
In two studies that compared these standard hypnotics to oral melatonin, one found that zopiclone 5 mg and melatonin 2 mg were equally beneficial with respect to sleep variables (other jet lag symptoms were not assessed).32 In another study, zolpidem 10 mg was superior to melatonin 5 mg for sleep and other jet lag symptoms, and the combination of zolpidem and melatonin was no better than zolpidem alone.30
Importantly, however, adverse effects were more frequent in those taking zolpidem and included nausea, vomiting, and confusion.30 Although these effects were not deemed serious, 14 participants (10%) withdrew from the study.
Stimulants
Caffeine is commonly used to combat the sleepiness of jet lag, but only two controlled field studies have assessed its efficacy.41,42 Both used slow-release preparations at a daily dosage of 300 mg.
In one study, after an eastward flight traversing seven time zones, participants took the pill at 08:00 destination time every day for 5 days.41 Curiously, alertness and other jet lag symptoms were not assessed, but circadian rhythms (determined by levels of cortisol in saliva) were re-entrained at a more rapid rate with caffeine than with placebo, and to a degree comparable with that achieved by exogenous melatonin.
In a follow-up study by the same group, those receiving caffeine were objectively less sleepy (as assessed by multiple sleep latency tests) than those taking melatonin or placebo, but subjective differences between groups were not identified.42 Furthermore, those taking caffeine had significantly more nocturnal sleep complaints, as assessed both objectively and subjectively.
A recent randomized, double-blind, placebo-controlled trial of the stimulant armodafinil (Nuvigil) found less sleepiness on multiple sleep latency testing and a decrease in jet leg symptoms with a dosage of 150 mg than with placebo.43
SHIFT WORK SLEEP DISORDER: DEFINITION, PREDISPOSING FACTORS
Shift work refers to nonstandard work schedules, including on-call duty, rotating shifts, and permanent night work. In the United States, one in five workers works a nonstandard shift.20
While shift work presents obvious difficulties, the diagnosis of shift work sleep disorder is reserved for those who have chronic insomnia or sleepiness at times that are not conducive to the externally demanded sleep-wake schedule, despite having the opportunity for sufficient daytime sleep.1 When defined in such a fashion, this disorder may afflict nearly a third of workers,44 with potential adverse effects on safety, health, and quality of life.
Older age is considered a risk factor for intolerance to shift work.20 In a study of physiologic phase shifts in response to night work, older workers were less able to recover after several night shifts.45 A large survey of police officers working the night shift supported the finding of more sleep disruption and on-duty sleepiness in older people.46
TREATMENT OF SHIFT WORK SLEEP DISORDER
Bright light at work, sunglasses on the way home
Various field studies have described hastening of circadian adaptation (and immediate alerting effects) during night shifts with the use of bright light.20
Boivin and James47 found that workers who received 6 hours of intermittent bright light during their shifts experienced significantly greater phase delays than those who received no such intervention. Those receiving bright light also wore sunglasses during the commute home (to protect from an undesired phase advance), and this has demonstrated favorable effects as an independent intervention.48
Drug treatment of shift work sleep disorder
Melatonin: Mixed results. Two field studies found that taking melatonin (5–6 mg) before the daytime sleep period had a favorable impact on subjective sleep quality.49,50 However, two other studies found no such benefit with doses ranging from 6 to 10 mg.51,52 Differences between these studies—eg, shift schedules, dosages, and the time the melatonin was taken—preclude definitive comparisons.
Effects of melatonin on workplace alertness are indeterminate because of inconsistent measurements of this variable. Importantly, a simulated shift work study found no phase-shifting advantages of melatonin in those who concomitantly used bright light during their work shift with or without morning protective eyewear.48
Hypnotic drugs. In simulation studies and field studies, people taking benzodiazepine receptor agonists have consistently said they sleep better.53–58 A simulation study noted additional benefit in the ability to stay alert during the night shift (assessed by maintenance of wakefulness testing),55 but two other studies saw no changes in manifest sleepiness (assessed with multiple sleep latency tests).53,54 These divergent findings may represent different effects on these two dimensions of sleepiness.
The only field study to assess post-sleep psychomotor performance found no impairments after taking 7.5 mg of zopiclone, a relatively long-acting nonbenzodiazepine hypnotic.57
Stimulants. In the largest trial to date of shift work sleep disorder, modafinil 200 mg (the only drug currently FDA-approved for shift work sleep disorder) had significant benefits compared with placebo with respect to objective measurements of workplace sleepiness, reaction time performance testing, and self-rated improvement of symptoms.59 Perhaps because of the low dose studied, both treated and untreated patients continued to manifest sleepiness within the pathologic range on objective testing.
Although the efficacy of caffeine is well documented as a countermeasure for sleepiness during experimentally induced sleep deprivation,20 very few field trials have specifically addressed impairments associated with shift work sleep disorder. In one study, caffeine at a dose of 4 mg/kg taken 30 minutes before starting a night shift provided objective improvement in both performance and alertness.60
Strategic napping is an additional practical intervention to promote alertness during night shifts, and cumulative data indicate that it provides objective and subjective improvements in alertness and performance.61,62 Earlier timed naps (ie, before or during the early portion of a shift) of short duration (ie, 20 minutes or less) are likely to produce maximal benefit, because they avoid sleep inertia (the grogginess or sleepiness that may follow a long nap), and also because they have no effect on the subsequent daytime sleep bout.61,63
Interventions may also be used in combination. For example, napping in conjunction with caffeine results in a greater degree of increased objective alertness than either intervention alone.60
How about days off?
The recommendations described here presume that shift workers maintain the workday sleep-wake schedule continuously, including when they are not at work. This is likely not a real-world scenario.
Smith et al64 developed a “compromise” phase position, whereby internal rhythms are optimized to facilitate alertness during work and sleepiness during the day, while allowing one to adopt a non-workday sleep schedule that maintains accessibility to family and social activities. In brief, non-workday sleep starts about 5.5 hours earlier than workday sleep; all sleep bouts are followed by brief exposure to bright light (to avoid excessive phase delay); and, as described previously, both workplace bright light and protection from morning light are implemented.
Although further studies are needed to determine whether this regimen is practical in real life, study participants who achieved desired partial phase shifts had performance ratings on a par with baseline levels, and comparable to those in a group that achieved complete re-entrainment.64
Finally, all shift workers need to be encouraged to protect the daytime bedroom environment just as daytime workers protect their nighttime environment. Sleep should be sought in an appropriately darkened and quiet environment, phones and doorbells silenced, and appointments scheduled accordingly.
For people who must travel long distances east or west by air or who must work the night shift, some relief is possible for the grogginess and disorientation that often ensue. The problems arise from the body’s internal clock being out of sync with the sun. Part of the solution involves helping reset the internal clock, or sometimes, preventing it from resetting itself.
This review will focus on jet lag sleep disorder and shift work sleep disorder, with an emphasis on the causes, the clinical assessment, and evidence-based treatment options.
WHEN THE INTERNAL CLOCK IS OUT OF SYNC WITH THE SUN
Circadian rhythm sleep disorders are the result of dyssynchrony between the body’s internal clock and the external 24-hour light-dark cycle. Patients typically present with insomnia or excessive somnolence. These disorders may represent an intrinsic disorder, such as delayed or advanced sleep-phase disorder, or may be the result of transmeridian air travel or working nonstandard shifts.1
The intrinsic human circadian period is typically slightly longer than 24 hours,9 but it is synchronized (“entrained”) to the 24-hour day by various environmental inputs, or zeitgebers (German for “time-givers”), the most important of which is light exposure.10
When the internal clock is out of sync with the sun, the misalignment can result in daytime anergia, alternating complaints of insomnia and hypersomnia, and various other symptoms, including emotional disturbances and gastrointestinal distress. In particular, long-distance air travel or a nocturnal work schedule overwhelms the ability of the intrinsic clock to adjust rapidly enough, and the result is jet lag sleep disorder or shift work sleep disorder.1
TOOLS TO EVALUATE CIRCADIAN RHYTHM DISTURBANCES
A thorough history is the cornerstone of the evaluation for all sleep disorders, and if a circadian rhythm disturbance is suspected, the sleep history is supplemented with specific questions to establish a clear diagnosis.
When assessing for jet lag disorder, ask about:
- The patient’s degree of sleep deprivation before and during travel
- His or her innate circadian preference (ie, whether he or she is a “night owl” or “early bird”)
- Patterns of alcohol and caffeine consumption.
When assessing for shift work disorder, include the above questions and also look for differences in the sleep-wake schedule on working days vs nonworking days, as well as external contributors to poor sleep quality (eg, the degree to which daytime sleep is not “protected”).
The following tools help in acquiring this information.
Sleep diary
In a sleep diary or log, patients record the times that they take naps, maintain consolidated sleep, and subsequently arise. The diary also prompts the patient for information about sleep latency, wakefulness after sleep onset, time in bed, medication and caffeine intake, and the restorative quality of sleep.
While the sleep diary by itself may provide insight into counteractive sleep-related behaviors and misperceptions the patient may have, compliance is often limited. Therefore, the sleep diary is best used in conjunction with actigraphy.
Actigraphy
An actigraph is a wristwatch-size motion detector, typically worn continuously for 7 days or longer. The data it gathers and stores serve as a surrogate measure of various sleep-wake variables.11
Either a sleep diary or actigraphy is required to demonstrate the stability of sleep patterns and circadian preference, but the actigraph typically generates more reliable data.11,12 It is also valuable in assessing the response to treatment of circadian rhythm sleep disorders.13
Are you an early bird or a night owl?
The Morningness-Eveningness questionnaire contains 19 items. Night owls tend to score lower on it than early birds do.14 This information may help some people avoid situations in which they may not do well, such as an early bird going on a permanent night-shift schedule.
Other assessment tools
Polysomnography is used primarily to rule out sleep-disordered breathing; it is not indicated for routine evaluation of circadian rhythm sleep disorders.
The minimum core body temperature and the peak melatonin secretion follow a 24-hour cycle. Although these measures are often used in research, they are not routinely used in clinical practice. (The minimum core body temperature is discussed further below.)
JET LAG SLEEP DISORDER
Jet lag results from air travel across multiple time zones, with a resultant discordance between the internal circadian clock and the destination’s light-dark cycle. Most sufferers report sleeping poorly at night and feeling groggy during the day, and some also experience general malaise and gastrointestinal distress.1
The severity depends on a number of variables.
Going west is easier than going east
Westward travel is normally less taxing than eastward travel, as it requires setting one’s internal clock later rather than earlier. Presumably, because the circadian period tends to exceed 24 hours, we can move our internal clock later by about 2 hours per day, but we can move it earlier by only 1 to 1.5 hours.15,16
The more time zones crossed, the longer it takes the circadian pacemaker to re-entrain and the longer-lasting and more severe are the symptoms of jet lag. Travel across one or two time zones is only transiently troublesome.
Does age affect jet lag?
Whether age affects the severity of jet lag is not yet known.
In a study of simulated jet lag (requiring a 6-hour advance), middle-aged people (ages 37 to 52) experienced a greater degree of fragmented sleep on polysomnography than younger ones (ages 18 to 25). The older group also had greater impairment in daytime alertness, suggesting that phase tolerance—ie, the ability to sleep at an abnormal time in the circadian cycle17—decreases with age. However, two field studies involving both eastward and westward travel yielded the opposite results, suggesting that older age may actually protect against jet lag.18–20
Methodologic differences preclude direct comparisons of the studies, as do differences in the age groups studied.
Light exposure can help or hurt, depending on the timing
Our core body temperature dips to its lowest point about 2 to 3 hours before we habitually awake. Exposure to bright light in the hours leading up to this minimum (the inverted triangle in Figure 2) sets our internal clock later (a phase delay)—desirable, say, for someone travelling from New York City to Los Angeles. Conversely, exposure to bright light after this temperature minimum sets the clock earlier.
Inadvertent shifting of circadian phase in the wrong direction (“antidromic re-entrainment”) is common and delays circadian reacclimation and the dissipation of jet lag symptoms.
We discuss ways to reduce antidromic reentrainment in more detail further below.
Other factors
Other factors that contribute to travel fatigue include sleep deprivation (before the flight or en route), acute discomfort as the plane ascends to its cruising altitude,25 and excessive alcohol or caffeine intake during the flight. Although the effects of these factors rapidly diminish once one reaches the travel destination, jet lag will persist until circadian re-entrainment occurs.15
NONDRUG THERAPIES FOR JET LAG SLEEP DISORDER
The goal of treatment is to realign the circadian rhythm in the most rapid and efficient way and to minimize symptoms in the meantime. Frequent shifts to different time zones, often required in business travel, are very difficult to accommodate, and business travelers actually may do better if they remain on their home-based schedule.
One study compared keeping home-based sleep hours as opposed to adopting local sleep hours during a 2-day stay after a 9-hour westward flight.26 Travelers who remained on home-based hours were less sleepy and had lower (ie, better) global jet lag ratings than those who adopted local sleep hours, in part because of better sleep quality and duration. Nevertheless, about one-third of the participants said they preferred to adhere to the local schedule.
Strategic avoidance of, and exposure to, light
If the traveler intends to remain at the destination long enough, he or she can adjust better (and avoid an antidromic process) via strategic avoidance of and exposure to light.24
People travelling east, who want to set their clocks ahead (a phase advance), need to keep to the dark in the 3 hours leading up to the time they reach their minimum core body temperature (depicted as “D” in Figure 3), and then expose themselves to light in the 3 hours immediately after (“L” in Figure 3). Thus, the traveler from Chicago to Paris would do better by avoiding light exposure on arrival, either by remaining in darkness in his or her hotel room, or by wearing dark sunglasses when outdoors. Wearing sunglasses during transit to the hotel would also help avoid light exposure.
When attempting to delay circadian rhythms, the opposite light-dark patterns are sought, as depicted in Figure 4. As flight and layover patterns often do not permit strict adherence to these measures, they represent idealized scenarios.
The first step is to make a grid with a concurrent listing of home and destination times. In the example in Figure 3, the person is traveling seven time zones east. On day 0, a rectangle is drawn around the times representing home-based sleep hours.
Next, we mark the time at which we expect the traveler’s core body temperature to reach its minimum (inverted triangle). If the person habitually sleeps no more than 7 hours per night, then we mark this point as 2 hours before his or her habitual wake-up time; if the person sleeps more than 7 hours, then we place it 3 hours before wake-up time.23,29 This process is repeated at the bottom of the grid to represent the desired sleep schedule at the traveler’s destination. The distance between the home and the destination-based minimum core body temperature symbols represents the required degree of circadian realignment.
If a phase advance is required (eg, if travelling from Chicago to Paris), the core body temperature symbol is drawn on day 1 in the same location as day 0. For each subsequent day, the symbol is moved 1 hour earlier (which is about how fast the internal clock can advance),15,27 until a clock time within 1 hour of the desired destination core body temperature time is reached or satisfactory sleep and daytime functioning are achieved (Figure 3). If a phase delay is required (eg, if travelling from New York City to Los Angeles), the symbol is drawn 2 hours later on day 1 than on day 0 (reflecting the greater ease at which delays are achieved),15,27 with subsequent daily shifts in 2-hour increments, again until a clock time within 1 hour of the desired destination minimum core body temperature time is reached or satisfactory sleep and daytime functioning are achieved.
Requirements for darkness can be met with protective eyewear (ie, dark sunglasses), or by remaining in a dark room. Light requirements can be met with outdoor exposure, with a commercial light box, or with a separate apparatus (eg, goggles, visors) portable enough for travel.
DRUGS TO TREAT JET LAG SLEEP DISORDER
Melatonin appears safe
Most field studies have found that nightly doses of melatonin (2–8 mg) improve the quality of sleep30–32 or alleviate daytime symptoms of jet lag, or both.20,30,31,33–36 Immediate-release preparations appear to be more effective than slow-release ones.31 Although most studies looked exclusively at adaptation to eastward travel,30–32,35,36 one studied westward travel,33 and another assessed melatonin’s effects during both departure and return trips that traversed 11 time zones.34
In studies of preflight dosing, melatonin was scheduled for up to 3 days before departure (and en route in two instances),30,34 at clock hours corresponding to the nocturnal sleep period at the travel destination (consistent times daily), and then for a subsequent 3 to 4 days between a destination time of 22:00 and 00:00 hours (ie, at bedtime).30,31,34–36 Several other studies further simplified this regimen, with participants taking nocturnal melatonin only on arrival at the destination, either for eastward31,32 or for westward travel.33
The study involving solely westward travel (Los Angeles to New Zealand) was the only one of the studies with positive findings that allowed for comparisons between participants who received melatonin before departure (3 days at 5-mg doses, taken between 07:00 and 08:00 Los Angeles time) and continuing for 5 days after arrival at 22:00 to 00:00 New Zealand time, and those who received melatonin beginning only on arrival.33 Significantly better jet lag outcomes were found in the latter group.
An important caveat is that melatonin is sold over the counter as a nutritional supplement and is not regulated by the United States Food and Drug Administration (FDA), so verification of purity of the product is difficult.
A comprehensive review by the National Academy of Sciences stated that, given the available data, short-term use of melatonin in total daily doses of 10 mg or less in healthy adults appears to be safe.37
Benzodiazepine receptor agonists improve sleep, but maybe not sleepiness
The use of standard hypnotics during periods of circadian realignment appears to be commonplace but has not been well studied.20 Trials of the newer benzodiazepine receptor agonists—three studies of zolpidem (Ambien) 10 mg30,38,39 and two of zopiclone 5 to 7.5 mg32,40—found consistently favorable subjective30,38 and objective32,39,40 outcomes in counteracting jet-lag-induced insomnia (for both eastward and westward travel). (Note: Zopiclone is not available in the United States, but its enantiomer eszopiclone [Lunesta] is.) However, the evidence is less clear for daytime symptoms of jet lag, with outcomes reported as favorable,30 equivocal,40 or inaccessible.32,38,39
The discrepancy between studies incorporating systematic daytime assessments may be due to differential medication effects (zolpidem vs zopiclone).
In two studies that compared these standard hypnotics to oral melatonin, one found that zopiclone 5 mg and melatonin 2 mg were equally beneficial with respect to sleep variables (other jet lag symptoms were not assessed).32 In another study, zolpidem 10 mg was superior to melatonin 5 mg for sleep and other jet lag symptoms, and the combination of zolpidem and melatonin was no better than zolpidem alone.30
Importantly, however, adverse effects were more frequent in those taking zolpidem and included nausea, vomiting, and confusion.30 Although these effects were not deemed serious, 14 participants (10%) withdrew from the study.
Stimulants
Caffeine is commonly used to combat the sleepiness of jet lag, but only two controlled field studies have assessed its efficacy.41,42 Both used slow-release preparations at a daily dosage of 300 mg.
In one study, after an eastward flight traversing seven time zones, participants took the pill at 08:00 destination time every day for 5 days.41 Curiously, alertness and other jet lag symptoms were not assessed, but circadian rhythms (determined by levels of cortisol in saliva) were re-entrained at a more rapid rate with caffeine than with placebo, and to a degree comparable with that achieved by exogenous melatonin.
In a follow-up study by the same group, those receiving caffeine were objectively less sleepy (as assessed by multiple sleep latency tests) than those taking melatonin or placebo, but subjective differences between groups were not identified.42 Furthermore, those taking caffeine had significantly more nocturnal sleep complaints, as assessed both objectively and subjectively.
A recent randomized, double-blind, placebo-controlled trial of the stimulant armodafinil (Nuvigil) found less sleepiness on multiple sleep latency testing and a decrease in jet leg symptoms with a dosage of 150 mg than with placebo.43
SHIFT WORK SLEEP DISORDER: DEFINITION, PREDISPOSING FACTORS
Shift work refers to nonstandard work schedules, including on-call duty, rotating shifts, and permanent night work. In the United States, one in five workers works a nonstandard shift.20
While shift work presents obvious difficulties, the diagnosis of shift work sleep disorder is reserved for those who have chronic insomnia or sleepiness at times that are not conducive to the externally demanded sleep-wake schedule, despite having the opportunity for sufficient daytime sleep.1 When defined in such a fashion, this disorder may afflict nearly a third of workers,44 with potential adverse effects on safety, health, and quality of life.
Older age is considered a risk factor for intolerance to shift work.20 In a study of physiologic phase shifts in response to night work, older workers were less able to recover after several night shifts.45 A large survey of police officers working the night shift supported the finding of more sleep disruption and on-duty sleepiness in older people.46
TREATMENT OF SHIFT WORK SLEEP DISORDER
Bright light at work, sunglasses on the way home
Various field studies have described hastening of circadian adaptation (and immediate alerting effects) during night shifts with the use of bright light.20
Boivin and James47 found that workers who received 6 hours of intermittent bright light during their shifts experienced significantly greater phase delays than those who received no such intervention. Those receiving bright light also wore sunglasses during the commute home (to protect from an undesired phase advance), and this has demonstrated favorable effects as an independent intervention.48
Drug treatment of shift work sleep disorder
Melatonin: Mixed results. Two field studies found that taking melatonin (5–6 mg) before the daytime sleep period had a favorable impact on subjective sleep quality.49,50 However, two other studies found no such benefit with doses ranging from 6 to 10 mg.51,52 Differences between these studies—eg, shift schedules, dosages, and the time the melatonin was taken—preclude definitive comparisons.
Effects of melatonin on workplace alertness are indeterminate because of inconsistent measurements of this variable. Importantly, a simulated shift work study found no phase-shifting advantages of melatonin in those who concomitantly used bright light during their work shift with or without morning protective eyewear.48
Hypnotic drugs. In simulation studies and field studies, people taking benzodiazepine receptor agonists have consistently said they sleep better.53–58 A simulation study noted additional benefit in the ability to stay alert during the night shift (assessed by maintenance of wakefulness testing),55 but two other studies saw no changes in manifest sleepiness (assessed with multiple sleep latency tests).53,54 These divergent findings may represent different effects on these two dimensions of sleepiness.
The only field study to assess post-sleep psychomotor performance found no impairments after taking 7.5 mg of zopiclone, a relatively long-acting nonbenzodiazepine hypnotic.57
Stimulants. In the largest trial to date of shift work sleep disorder, modafinil 200 mg (the only drug currently FDA-approved for shift work sleep disorder) had significant benefits compared with placebo with respect to objective measurements of workplace sleepiness, reaction time performance testing, and self-rated improvement of symptoms.59 Perhaps because of the low dose studied, both treated and untreated patients continued to manifest sleepiness within the pathologic range on objective testing.
Although the efficacy of caffeine is well documented as a countermeasure for sleepiness during experimentally induced sleep deprivation,20 very few field trials have specifically addressed impairments associated with shift work sleep disorder. In one study, caffeine at a dose of 4 mg/kg taken 30 minutes before starting a night shift provided objective improvement in both performance and alertness.60
Strategic napping is an additional practical intervention to promote alertness during night shifts, and cumulative data indicate that it provides objective and subjective improvements in alertness and performance.61,62 Earlier timed naps (ie, before or during the early portion of a shift) of short duration (ie, 20 minutes or less) are likely to produce maximal benefit, because they avoid sleep inertia (the grogginess or sleepiness that may follow a long nap), and also because they have no effect on the subsequent daytime sleep bout.61,63
Interventions may also be used in combination. For example, napping in conjunction with caffeine results in a greater degree of increased objective alertness than either intervention alone.60
How about days off?
The recommendations described here presume that shift workers maintain the workday sleep-wake schedule continuously, including when they are not at work. This is likely not a real-world scenario.
Smith et al64 developed a “compromise” phase position, whereby internal rhythms are optimized to facilitate alertness during work and sleepiness during the day, while allowing one to adopt a non-workday sleep schedule that maintains accessibility to family and social activities. In brief, non-workday sleep starts about 5.5 hours earlier than workday sleep; all sleep bouts are followed by brief exposure to bright light (to avoid excessive phase delay); and, as described previously, both workplace bright light and protection from morning light are implemented.
Although further studies are needed to determine whether this regimen is practical in real life, study participants who achieved desired partial phase shifts had performance ratings on a par with baseline levels, and comparable to those in a group that achieved complete re-entrainment.64
Finally, all shift workers need to be encouraged to protect the daytime bedroom environment just as daytime workers protect their nighttime environment. Sleep should be sought in an appropriately darkened and quiet environment, phones and doorbells silenced, and appointments scheduled accordingly.
- International Classification of Sleep Disorders: Diagnostic and Coding Manual/American Academy of Sleep Medicine. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005.
- Borbély AA, Achermann P. Concepts and models of sleep regulation: an overview. J Sleep Res 1992; 1:63–79.
- Carskadon MA, Dement WC. Effects of total sleep loss on sleep tendency. Percept Mot Skills 1979; 48:495–506.
- Beersma DG, Gordijn MC. Circadian control of the sleep-wake cycle. Physiol Behav 2007; 90:190–195.
- Moore RY, Eichler VB. Loss of a circadian adrenal corticosterone rhythm following suprachiasmatic lesions in the rat. Brain Res 1972; 42:201–206.
- Stephan FK, Zucker I. Circadian rhythms in drinking behavior and locomotor activity of rats are eliminated by hypothalamic lesions. Proc Natl Acad Sci U S A 1972; 69:1583–1586.
- Welsh DK, Logothetis DE, Meister M, Reppert SM. Individual neurons dissociated from rat suprachiasmatic nucleus express independently phased circadian firing rhythms. Neuron 1995; 14:697–706.
- Ralph MR, Foster RG, Davis FC, Menaker M. Transplanted suprachiasmatic nucleus determines circadian period. Science 1990; 247:975–978.
- Czeisler CA, Duffy JF, Shanahan TL, et al. Stability, precision, and near-24-hour period of the human circadian pacemaker. Science 1999; 284:2177–2181.
- Waterhouse JM, DeCoursey PJ. Human circadian organization. In:Dunlap JC, Loros JJ, DeCoursey PJ, editors. Chronobiology: Biological Timekeeping. Sunderland, MA: Sinauer Associates; 2004:291–324.
- Morgenthaler T, Alessi C, Friedman L, et al; Standards of Practice Committee; American Academy of Sleep Medicine. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007. Sleep 2007; 30:519–529.
- Bradshaw DA, Yanagi MA, Pak ES, Peery TS, Ruff GA. Nightly sleep duration in the 2-week period preceding multiple sleep latency testing. J Clin Sleep Med 2007; 3:613–619.
- Morgenthaler TI, Lee-Chiong T, Alessi C, et al; Standards of Practice Committee of the American Academy of Sleep Medicine. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report. Sleep 2007; 30:1445–1459.
- Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol 1976; 4:97–110.
- Waterhouse J, Reilly T, Atkinson G, Edwards B. Jet lag: trends and coping strategies. Lancet 2007; 369:1117–1129.
- Eastman CI, Gazda CJ, Burgess HJ, Crowley SJ, Fogg LF. Advancing circadian rhythms before eastward flight: a strategy to prevent or reduce jet lag. Sleep 2005; 28:33–44.
- Moline ML, Pollak CP, Monk TH, et al. Age-related differences in recovery from simulated jet lag. Sleep 1992; 15:28–40.
- Waterhouse J, Edwards B, Nevill A, et al. Identifying some determinants of “jet lag” and its symptoms: a study of athletes and other travellers. Br J Sports Med 2002; 36:54–60.
- Tresguerres JA, Ariznavarreta C, Granados B, et al. Circadian urinary 6-sulphatoxymelatonin, cortisol excretion and locomotor activity in airline pilots during transmeridian flights. J Pineal Res 2001; 31:16–22.
- Sack RL, Auckley D, Auger RR, et al; American Academy of Sleep Medicine. Circadian rhythm sleep disorders: part I, basic principles, shift work and jet lag disorders. An American Academy of Sleep Medicine review. Sleep 2007; 30:1460–1483.
- Burgess HJ, Sharkey KM, Eastman CI. Bright light, dark and melatonin can promote circadian adaptation in night shift workers. Sleep Med Rev 2002; 6:407–420.
- Lewy AJ, Bauer VK, Saeeduddin A, et al. The human phase response curve (PRC) to melatonin is about 12 hours out of phase with the PRC to light. Chronobiol Int 1998; 15:71–83.
- Burgess HJ, Eastman CT. Prevention of Jet Lag. 2010. http://pier.acponline.org/physicians/screening/prev1015/prev1015.html. Accessed June 25, 2010.
- Daan S, Lewy AJ. Scheduled exposure to daylight: a potential strategy to reduce “jet lag” following transmeridian flight. Psychopharmacol Bull 1984; 20:566–568.
- Muhm JM, Rock PB, McMullin DL, et al. Effect of aircraft-cabin altitude on passenger discomfort. N Engl J Med 2007; 357:18–27.
- Lowden A, Akerstedt T. Retaining home-base sleep hours to prevent jet lag in connection with a westward flight across nine time zones. Chronobiol Int 1998; 15:365–376.
- Eastman CI, Burgess HJ. How to travel the world without jet lag. Sleep Med Clin 2009; 4:241–255.
- Revell VL, Eastman CI. How to trick mother nature into letting you fly around or stay up all night. J Biol Rhythms 2005; 20:353–365.
- Cagnacci A, Elliott JA, Yen SS. Melatonin: a major regulator of the circadian rhythm of core temperature in humans. J Clin Endocrinol Metab 1992; 75:447–452.
- Suhner A, Schlagenhauf P, Höfer I, Johnson R, Tschopp A, Steffen R. Effectiveness and tolerability of melatonin and zolpidem for the alleviation of jet lag. Aviat Space Environ Med 2001; 72:638–646.
- Suhner A, Schlagenhauf P, Johnson R, Tschopp A, Steffen R. Comparative study to determine the optimal melatonin dosage form for the alleviation of jet lag. Chronobiol Int 1998; 15:655–666.
- Paul MA, Gray G, Sardana TM, Pigeau RA. Melatonin and zopiclone as facilitators of early circadian sleep in operational air transport crews. Aviat Space Environ Med 2004; 75:439–443.
- Petrie K, Dawson AG, Thompson L, Brook R. A double-blind trial of melatonin as a treatment for jet lag in international cabin crew. Biol Psychiatry 1993; 33:526–530.
- Petrie K, Conaglen JV, Thompson L, Chamberlain K. Effect of melatonin on jet lag after long haul flights. BMJ 1989; 298:705–707.
- Arendt J, Aldhous M, Marks V. Alleviation of jet lag by melatonin: preliminary results of controlled double blind trial. Br Med J (Clin Res Ed) 1986; 292:1170.
- Claustrat B, Brun J, David M, Sassolas G, Chazot G. Melatonin and jet lag: confirmatory result using a simplified protocol. Biol Psychiatry 1992; 32:705–711.
- Committee on the Framework for Evaluating the Safety of Dietary Supplements, Food and Nutrition Board, Board on Life Sciences, Institute of Medicine and National Research Council of the National Academies. Dietary supplements: a framework for evaluating safety. Washington, DC: The National Academies Press; 2005.
- Jamieson AO, Zammit GK, Rosenberg RS, Davis JR, Walsh JK. Zolpidem reduces the sleep disturbance of jet lag. Sleep Med 2001; 2:423–430.
- Hirschfeld U, Moreno-Reyes R, Akseki E, et al. Progressive elevation of plasma thyrotropin during adaptation to simulated jet lag: effects of treatment with bright light or zolpidem. J Clin Endocrinol Metab 1996; 81:3270–3277.
- Daurat A, Benoit O, Buguet A. Effects of zopiclone on the rest/activity rhythm after a westward flight across five time zones. Psychopharmacology (Berl) 2000; 149:241–245.
- Piérard C, Beaumont M, Enslen M, et al. Resynchronization of hormonal rhythms after an eastbound flight in humans: effects of slow-release caffeine and melatonin. Eur J Appl Physiol 2001; 85:144–150.
- Beaumont M, Batéjat D, Piérard C, et al. Caffeine or melatonin effects on sleep and sleepiness after rapid eastward transmeridian travel. J Appl Physiol 2004; 96:50–58.
- Rosenberg RP, Bogan RK, Tiller JM, et al. A phase 3, double-blind, randomized, placebo-controlled study of armodafinil for excessive sleepiness associated with jet lag disorder. Mayo Clin Proc 2010; 85:630–638.
- Drake CL, Roehrs T, Richardson G, Walsh JK, Roth T. Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep 2004; 27:1453–1462.
- Härmä MI, Hakola T, Akerstedt T, Laitinen JT. Age and adjustment to night work. Occup Environ Med 1994; 51:568–573.
- Smith L, Mason C. Reducing night shift exposure: a pilot study of rota, night shift and age effects on sleepiness and fatigue. J Hum Ergol (Tokyo) 2001; 30:83–87.
- Boivin DB, James FO. Circadian adaptation to night-shift work by judicious light and darkness exposure. J Biol Rhythms 2002; 17:556–567.
- Crowley SJ, Lee C, Tseng CY, Fogg LF, Eastman CI. Combinations of bright light, scheduled dark, sunglasses, and melatonin to facilitate circadian entrainment to night shift work. J Biol Rhythms 2003; 18:513–523.
- Folkard S, Arendt J, Clark M. Can melatonin improve shift workers’ tolerance of the night shift? Some preliminary findings. Chronobiol Int 1993; 10:315–320.
- Yoon IY, Song BG. Role of morning melatonin administration and attenuation of sunlight exposure in improving adaptation of nightshift workers. Chronobiol Int 2002; 19:903–913.
- James M, Tremea MO, Jones JS, Krohmer JR. Can melatonin improve adaptation to night shift? Am J Emerg Med 1998; 16:367–370.
- Jorgensen KM, Witting MD. Does exogenous melatonin improve day sleep or night alertness in emergency physicians working night shifts? Ann Emerg Med 1998; 31:699–704.
- Walsh JK, Schweitzer PK, Anch AM, Muehlbach MJ, Jenkins NA, Dickins QS. Sleepiness/alertness on a simulated night shift following sleep at home with triazolam. Sleep 1991; 14:140–146.
- Walsh JK, Sugerman JL, Muehlbach MJ, Schweitzer PK. Physiological sleep tendency on a simulated night shift: adaptation and effects of triazolam. Sleep 1988; 11:251–264.
- Porcù S, Bellatreccia A, Ferrara M, Casagrande M. Performance, ability to stay awake, and tendency to fall asleep during the night after a diurnal sleep with temazepam or placebo. Sleep 1997; 20:535–541.
- Monchesky TC, Billings BJ, Phillips R, Bourgouin J. Zopiclone in insomniac shiftworkers. Evaluation of its hypnotic properties and its effects on mood and work performance. Int Arch Occup Environ Health 1989; 61:255–259.
- Moon CA, Hindmarch I, Holland RL. The effect of zopiclone 7.5 mg on the sleep, mood and performance of shift workers. Int Clin Psychopharmacol 1990; 5(suppl 2):79–83.
- Puca FM, Perrucci S, Prudenzano MP, et al. Quality of life in shift work syndrome. Funct Neurol 1996; 11:261–268.
- Czeisler CA, Walsh JK, Roth T, et al; US Modafinil in Shift Work Sleep Disorder Study Group. Modafinil for excessive sleepiness associated with shift-work sleep disorder. N Engl J Med 2005; 353:476–486.
- Schweitzer PK, Randazzo AC, Stone K, Erman M, Walsh JK. Laboratory and field studies of naps and caffeine as practical countermeasures for sleep-wake problems associated with night work. Sleep 2006; 29:39–50.
- Sallinen M, Härmä M, Akerstedt T, Rosa R, Lillqvist O. Promoting alertness with a short nap during a night shift. J Sleep Res 1998; 7:240–247.
- Garbarino S, Mascialino B, Penco MA, et al. Professional shift-work drivers who adopt prophylactic naps can reduce the risk of car accidents during night work. Sleep 2004; 27:1295–1302.
- Purnell MT, Feyer AM, Herbison GP. The impact of a nap opportunity during the night shift on the performance and alertness of 12-h shift workers. J Sleep Res 2002; 11:219–227.
- Smith MR, Fogg LF, Eastman CI. A compromise circadian phase position for permanent night work improves mood, fatigue, and performance. Sleep 2009; 32:1481–1489.
- International Classification of Sleep Disorders: Diagnostic and Coding Manual/American Academy of Sleep Medicine. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005.
- Borbély AA, Achermann P. Concepts and models of sleep regulation: an overview. J Sleep Res 1992; 1:63–79.
- Carskadon MA, Dement WC. Effects of total sleep loss on sleep tendency. Percept Mot Skills 1979; 48:495–506.
- Beersma DG, Gordijn MC. Circadian control of the sleep-wake cycle. Physiol Behav 2007; 90:190–195.
- Moore RY, Eichler VB. Loss of a circadian adrenal corticosterone rhythm following suprachiasmatic lesions in the rat. Brain Res 1972; 42:201–206.
- Stephan FK, Zucker I. Circadian rhythms in drinking behavior and locomotor activity of rats are eliminated by hypothalamic lesions. Proc Natl Acad Sci U S A 1972; 69:1583–1586.
- Welsh DK, Logothetis DE, Meister M, Reppert SM. Individual neurons dissociated from rat suprachiasmatic nucleus express independently phased circadian firing rhythms. Neuron 1995; 14:697–706.
- Ralph MR, Foster RG, Davis FC, Menaker M. Transplanted suprachiasmatic nucleus determines circadian period. Science 1990; 247:975–978.
- Czeisler CA, Duffy JF, Shanahan TL, et al. Stability, precision, and near-24-hour period of the human circadian pacemaker. Science 1999; 284:2177–2181.
- Waterhouse JM, DeCoursey PJ. Human circadian organization. In:Dunlap JC, Loros JJ, DeCoursey PJ, editors. Chronobiology: Biological Timekeeping. Sunderland, MA: Sinauer Associates; 2004:291–324.
- Morgenthaler T, Alessi C, Friedman L, et al; Standards of Practice Committee; American Academy of Sleep Medicine. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007. Sleep 2007; 30:519–529.
- Bradshaw DA, Yanagi MA, Pak ES, Peery TS, Ruff GA. Nightly sleep duration in the 2-week period preceding multiple sleep latency testing. J Clin Sleep Med 2007; 3:613–619.
- Morgenthaler TI, Lee-Chiong T, Alessi C, et al; Standards of Practice Committee of the American Academy of Sleep Medicine. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report. Sleep 2007; 30:1445–1459.
- Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol 1976; 4:97–110.
- Waterhouse J, Reilly T, Atkinson G, Edwards B. Jet lag: trends and coping strategies. Lancet 2007; 369:1117–1129.
- Eastman CI, Gazda CJ, Burgess HJ, Crowley SJ, Fogg LF. Advancing circadian rhythms before eastward flight: a strategy to prevent or reduce jet lag. Sleep 2005; 28:33–44.
- Moline ML, Pollak CP, Monk TH, et al. Age-related differences in recovery from simulated jet lag. Sleep 1992; 15:28–40.
- Waterhouse J, Edwards B, Nevill A, et al. Identifying some determinants of “jet lag” and its symptoms: a study of athletes and other travellers. Br J Sports Med 2002; 36:54–60.
- Tresguerres JA, Ariznavarreta C, Granados B, et al. Circadian urinary 6-sulphatoxymelatonin, cortisol excretion and locomotor activity in airline pilots during transmeridian flights. J Pineal Res 2001; 31:16–22.
- Sack RL, Auckley D, Auger RR, et al; American Academy of Sleep Medicine. Circadian rhythm sleep disorders: part I, basic principles, shift work and jet lag disorders. An American Academy of Sleep Medicine review. Sleep 2007; 30:1460–1483.
- Burgess HJ, Sharkey KM, Eastman CI. Bright light, dark and melatonin can promote circadian adaptation in night shift workers. Sleep Med Rev 2002; 6:407–420.
- Lewy AJ, Bauer VK, Saeeduddin A, et al. The human phase response curve (PRC) to melatonin is about 12 hours out of phase with the PRC to light. Chronobiol Int 1998; 15:71–83.
- Burgess HJ, Eastman CT. Prevention of Jet Lag. 2010. http://pier.acponline.org/physicians/screening/prev1015/prev1015.html. Accessed June 25, 2010.
- Daan S, Lewy AJ. Scheduled exposure to daylight: a potential strategy to reduce “jet lag” following transmeridian flight. Psychopharmacol Bull 1984; 20:566–568.
- Muhm JM, Rock PB, McMullin DL, et al. Effect of aircraft-cabin altitude on passenger discomfort. N Engl J Med 2007; 357:18–27.
- Lowden A, Akerstedt T. Retaining home-base sleep hours to prevent jet lag in connection with a westward flight across nine time zones. Chronobiol Int 1998; 15:365–376.
- Eastman CI, Burgess HJ. How to travel the world without jet lag. Sleep Med Clin 2009; 4:241–255.
- Revell VL, Eastman CI. How to trick mother nature into letting you fly around or stay up all night. J Biol Rhythms 2005; 20:353–365.
- Cagnacci A, Elliott JA, Yen SS. Melatonin: a major regulator of the circadian rhythm of core temperature in humans. J Clin Endocrinol Metab 1992; 75:447–452.
- Suhner A, Schlagenhauf P, Höfer I, Johnson R, Tschopp A, Steffen R. Effectiveness and tolerability of melatonin and zolpidem for the alleviation of jet lag. Aviat Space Environ Med 2001; 72:638–646.
- Suhner A, Schlagenhauf P, Johnson R, Tschopp A, Steffen R. Comparative study to determine the optimal melatonin dosage form for the alleviation of jet lag. Chronobiol Int 1998; 15:655–666.
- Paul MA, Gray G, Sardana TM, Pigeau RA. Melatonin and zopiclone as facilitators of early circadian sleep in operational air transport crews. Aviat Space Environ Med 2004; 75:439–443.
- Petrie K, Dawson AG, Thompson L, Brook R. A double-blind trial of melatonin as a treatment for jet lag in international cabin crew. Biol Psychiatry 1993; 33:526–530.
- Petrie K, Conaglen JV, Thompson L, Chamberlain K. Effect of melatonin on jet lag after long haul flights. BMJ 1989; 298:705–707.
- Arendt J, Aldhous M, Marks V. Alleviation of jet lag by melatonin: preliminary results of controlled double blind trial. Br Med J (Clin Res Ed) 1986; 292:1170.
- Claustrat B, Brun J, David M, Sassolas G, Chazot G. Melatonin and jet lag: confirmatory result using a simplified protocol. Biol Psychiatry 1992; 32:705–711.
- Committee on the Framework for Evaluating the Safety of Dietary Supplements, Food and Nutrition Board, Board on Life Sciences, Institute of Medicine and National Research Council of the National Academies. Dietary supplements: a framework for evaluating safety. Washington, DC: The National Academies Press; 2005.
- Jamieson AO, Zammit GK, Rosenberg RS, Davis JR, Walsh JK. Zolpidem reduces the sleep disturbance of jet lag. Sleep Med 2001; 2:423–430.
- Hirschfeld U, Moreno-Reyes R, Akseki E, et al. Progressive elevation of plasma thyrotropin during adaptation to simulated jet lag: effects of treatment with bright light or zolpidem. J Clin Endocrinol Metab 1996; 81:3270–3277.
- Daurat A, Benoit O, Buguet A. Effects of zopiclone on the rest/activity rhythm after a westward flight across five time zones. Psychopharmacology (Berl) 2000; 149:241–245.
- Piérard C, Beaumont M, Enslen M, et al. Resynchronization of hormonal rhythms after an eastbound flight in humans: effects of slow-release caffeine and melatonin. Eur J Appl Physiol 2001; 85:144–150.
- Beaumont M, Batéjat D, Piérard C, et al. Caffeine or melatonin effects on sleep and sleepiness after rapid eastward transmeridian travel. J Appl Physiol 2004; 96:50–58.
- Rosenberg RP, Bogan RK, Tiller JM, et al. A phase 3, double-blind, randomized, placebo-controlled study of armodafinil for excessive sleepiness associated with jet lag disorder. Mayo Clin Proc 2010; 85:630–638.
- Drake CL, Roehrs T, Richardson G, Walsh JK, Roth T. Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep 2004; 27:1453–1462.
- Härmä MI, Hakola T, Akerstedt T, Laitinen JT. Age and adjustment to night work. Occup Environ Med 1994; 51:568–573.
- Smith L, Mason C. Reducing night shift exposure: a pilot study of rota, night shift and age effects on sleepiness and fatigue. J Hum Ergol (Tokyo) 2001; 30:83–87.
- Boivin DB, James FO. Circadian adaptation to night-shift work by judicious light and darkness exposure. J Biol Rhythms 2002; 17:556–567.
- Crowley SJ, Lee C, Tseng CY, Fogg LF, Eastman CI. Combinations of bright light, scheduled dark, sunglasses, and melatonin to facilitate circadian entrainment to night shift work. J Biol Rhythms 2003; 18:513–523.
- Folkard S, Arendt J, Clark M. Can melatonin improve shift workers’ tolerance of the night shift? Some preliminary findings. Chronobiol Int 1993; 10:315–320.
- Yoon IY, Song BG. Role of morning melatonin administration and attenuation of sunlight exposure in improving adaptation of nightshift workers. Chronobiol Int 2002; 19:903–913.
- James M, Tremea MO, Jones JS, Krohmer JR. Can melatonin improve adaptation to night shift? Am J Emerg Med 1998; 16:367–370.
- Jorgensen KM, Witting MD. Does exogenous melatonin improve day sleep or night alertness in emergency physicians working night shifts? Ann Emerg Med 1998; 31:699–704.
- Walsh JK, Schweitzer PK, Anch AM, Muehlbach MJ, Jenkins NA, Dickins QS. Sleepiness/alertness on a simulated night shift following sleep at home with triazolam. Sleep 1991; 14:140–146.
- Walsh JK, Sugerman JL, Muehlbach MJ, Schweitzer PK. Physiological sleep tendency on a simulated night shift: adaptation and effects of triazolam. Sleep 1988; 11:251–264.
- Porcù S, Bellatreccia A, Ferrara M, Casagrande M. Performance, ability to stay awake, and tendency to fall asleep during the night after a diurnal sleep with temazepam or placebo. Sleep 1997; 20:535–541.
- Monchesky TC, Billings BJ, Phillips R, Bourgouin J. Zopiclone in insomniac shiftworkers. Evaluation of its hypnotic properties and its effects on mood and work performance. Int Arch Occup Environ Health 1989; 61:255–259.
- Moon CA, Hindmarch I, Holland RL. The effect of zopiclone 7.5 mg on the sleep, mood and performance of shift workers. Int Clin Psychopharmacol 1990; 5(suppl 2):79–83.
- Puca FM, Perrucci S, Prudenzano MP, et al. Quality of life in shift work syndrome. Funct Neurol 1996; 11:261–268.
- Czeisler CA, Walsh JK, Roth T, et al; US Modafinil in Shift Work Sleep Disorder Study Group. Modafinil for excessive sleepiness associated with shift-work sleep disorder. N Engl J Med 2005; 353:476–486.
- Schweitzer PK, Randazzo AC, Stone K, Erman M, Walsh JK. Laboratory and field studies of naps and caffeine as practical countermeasures for sleep-wake problems associated with night work. Sleep 2006; 29:39–50.
- Sallinen M, Härmä M, Akerstedt T, Rosa R, Lillqvist O. Promoting alertness with a short nap during a night shift. J Sleep Res 1998; 7:240–247.
- Garbarino S, Mascialino B, Penco MA, et al. Professional shift-work drivers who adopt prophylactic naps can reduce the risk of car accidents during night work. Sleep 2004; 27:1295–1302.
- Purnell MT, Feyer AM, Herbison GP. The impact of a nap opportunity during the night shift on the performance and alertness of 12-h shift workers. J Sleep Res 2002; 11:219–227.
- Smith MR, Fogg LF, Eastman CI. A compromise circadian phase position for permanent night work improves mood, fatigue, and performance. Sleep 2009; 32:1481–1489.
KEY POINTS
- Symptoms include daytime anergia, alternating complaints of insomnia and hypersomnia, emotional disturbances, and gastrointestinal distress. The severity depends on the degree and the duration of dyssynchrony, as well as on innate factors such as age and whether the patient is an “early bird” or a “night owl.”
- Drug treatment addresses sleep-related symptoms (eg, somnolence, insomnia) and attempts to hasten circadian reacclimation.
- Exposure to bright light in the hours leading up to the patient’s minimum core body temperature tends to push the internal clock later in time, whereas bright light in the hours immediately afterward pushes the clock earlier in time.