User login
Improving the appearance of port wine stains usually requires multiple laser treatments, and research is ongoing to improve results, according to Dr. Kristen Kelly.
Port wine stains (PWS) are the most common vascular malformations treated by dermatologists. About 0.3% of newborns have a PWS birthmark, which does not proliferate rapidly, but "may thicken, darken and develop nodules over time," Dr. Kelly said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif.
Historically, treatments for PWS have included tattoos or radiation, but for almost 30 years laser therapy has been the mainstay of treatment. Although these devices have improved, 2-15 or more laser applications are needed at approximately 4-week intervals for successful treatment of these lesions, said Dr. Kelly of the University of California, Irvine, and the Beckman Laser Institute and Medical Clinic.
The pulsed dye laser is the standard of care for PWS treatment and is the laser that she and her associates use most often. However, "we use different lasers and settings over a course of treatment to try to improve our results," Dr. Kelly said in an interview. The other lasers they use include the 755-nm alexandrite laser and combined 1,064:595-nm laser system, as well as intense pulsed light.
For some patients undergoing treatment of a PWS, preparation may include use of a bleaching cream for several weeks before treatment. Sun protection of the area to be treated is recommended for all patients. She and her associates use general anesthesia for patients with large lesions and for children and infants, although this is not a universal practice among dermatologists, she pointed out.
Eye protection with a corneal shield is very important for patients if treatment involves the periorbital or eyelid area, Dr. Kelly said, noting that proper eye protection is also important for those treating the patient.
During treatment, she recommends using a 585-nm or 595-nm wavelength and 0.45-3 millisecond pulse duration--varying pulse duration and wavelength over time to achieve optimal results. Placing patients in the Trendelenburg position can increase blood flow to the area of the PWS, according to Dr. Kelly, who is also with the university's Vascular Birthmarks and Malformations Diagnostic Treatment Center.
Postoperatively, ice should be applied to the treated area, which should be elevated for the first 1-2 postoperative days. A mild analgesic like acetaminophen should be used for discomfort, she said. An emollient should be applied to the treated area, and patients should protect the treated area from sun exposure. A bleaching cream such as hydroquinone may be started 2-3 weeks after treatment for some patients.
Dr. Kelly said that most PWS birthmarks get lighter but require multiple treatments. Some lesions, however, are resistant to treatment, and complete removal is uncommon.
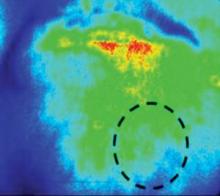
Research on improving results of PWS - to achieve more complete clearance over a shorter period of time - includes studies of imaging methods like laser speckle imaging (LSI), which is used intraoperatively to evaluate the impact of laser treatment on blood flow to determine if flow to the lesional blood vessel is decreased dramatically or shut down.
"Presumably, a greater reduction in flow is associated with greater damage to the blood vessels," said Dr. Kelly, who, with her associates, is studying whether a greater reduction in blood flow during treatment ultimately leads to better results. "We think it does, but we don't know that for sure yet," she said.
They also are studying whether the use of adjunctive agents after laser treatment improves results. These agents include antiangiogenic agents applied topically or administered orally or intravenously. An early study of imiquimod, an immune modulator with antiangiogenic effects, is underway, she noted.
Dr. Kelly disclosed that she has received research grants from Candela Corp. and Graceway Pharmaceuticals, and has served as a consultant to Lumenis. In addition, Graceway and Genentech have donated products for studies she is conducting.
SDEF and this news organization are both owned by Elsevier.
Improving the appearance of port wine stains usually requires multiple laser treatments, and research is ongoing to improve results, according to Dr. Kristen Kelly.
Port wine stains (PWS) are the most common vascular malformations treated by dermatologists. About 0.3% of newborns have a PWS birthmark, which does not proliferate rapidly, but "may thicken, darken and develop nodules over time," Dr. Kelly said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif.
Historically, treatments for PWS have included tattoos or radiation, but for almost 30 years laser therapy has been the mainstay of treatment. Although these devices have improved, 2-15 or more laser applications are needed at approximately 4-week intervals for successful treatment of these lesions, said Dr. Kelly of the University of California, Irvine, and the Beckman Laser Institute and Medical Clinic.
The pulsed dye laser is the standard of care for PWS treatment and is the laser that she and her associates use most often. However, "we use different lasers and settings over a course of treatment to try to improve our results," Dr. Kelly said in an interview. The other lasers they use include the 755-nm alexandrite laser and combined 1,064:595-nm laser system, as well as intense pulsed light.
For some patients undergoing treatment of a PWS, preparation may include use of a bleaching cream for several weeks before treatment. Sun protection of the area to be treated is recommended for all patients. She and her associates use general anesthesia for patients with large lesions and for children and infants, although this is not a universal practice among dermatologists, she pointed out.
Eye protection with a corneal shield is very important for patients if treatment involves the periorbital or eyelid area, Dr. Kelly said, noting that proper eye protection is also important for those treating the patient.
During treatment, she recommends using a 585-nm or 595-nm wavelength and 0.45-3 millisecond pulse duration--varying pulse duration and wavelength over time to achieve optimal results. Placing patients in the Trendelenburg position can increase blood flow to the area of the PWS, according to Dr. Kelly, who is also with the university's Vascular Birthmarks and Malformations Diagnostic Treatment Center.
Postoperatively, ice should be applied to the treated area, which should be elevated for the first 1-2 postoperative days. A mild analgesic like acetaminophen should be used for discomfort, she said. An emollient should be applied to the treated area, and patients should protect the treated area from sun exposure. A bleaching cream such as hydroquinone may be started 2-3 weeks after treatment for some patients.
Dr. Kelly said that most PWS birthmarks get lighter but require multiple treatments. Some lesions, however, are resistant to treatment, and complete removal is uncommon.
Research on improving results of PWS - to achieve more complete clearance over a shorter period of time - includes studies of imaging methods like laser speckle imaging (LSI), which is used intraoperatively to evaluate the impact of laser treatment on blood flow to determine if flow to the lesional blood vessel is decreased dramatically or shut down.
"Presumably, a greater reduction in flow is associated with greater damage to the blood vessels," said Dr. Kelly, who, with her associates, is studying whether a greater reduction in blood flow during treatment ultimately leads to better results. "We think it does, but we don't know that for sure yet," she said.
They also are studying whether the use of adjunctive agents after laser treatment improves results. These agents include antiangiogenic agents applied topically or administered orally or intravenously. An early study of imiquimod, an immune modulator with antiangiogenic effects, is underway, she noted.
Dr. Kelly disclosed that she has received research grants from Candela Corp. and Graceway Pharmaceuticals, and has served as a consultant to Lumenis. In addition, Graceway and Genentech have donated products for studies she is conducting.
SDEF and this news organization are both owned by Elsevier.
Improving the appearance of port wine stains usually requires multiple laser treatments, and research is ongoing to improve results, according to Dr. Kristen Kelly.
Port wine stains (PWS) are the most common vascular malformations treated by dermatologists. About 0.3% of newborns have a PWS birthmark, which does not proliferate rapidly, but "may thicken, darken and develop nodules over time," Dr. Kelly said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif.
Historically, treatments for PWS have included tattoos or radiation, but for almost 30 years laser therapy has been the mainstay of treatment. Although these devices have improved, 2-15 or more laser applications are needed at approximately 4-week intervals for successful treatment of these lesions, said Dr. Kelly of the University of California, Irvine, and the Beckman Laser Institute and Medical Clinic.
The pulsed dye laser is the standard of care for PWS treatment and is the laser that she and her associates use most often. However, "we use different lasers and settings over a course of treatment to try to improve our results," Dr. Kelly said in an interview. The other lasers they use include the 755-nm alexandrite laser and combined 1,064:595-nm laser system, as well as intense pulsed light.
For some patients undergoing treatment of a PWS, preparation may include use of a bleaching cream for several weeks before treatment. Sun protection of the area to be treated is recommended for all patients. She and her associates use general anesthesia for patients with large lesions and for children and infants, although this is not a universal practice among dermatologists, she pointed out.
Eye protection with a corneal shield is very important for patients if treatment involves the periorbital or eyelid area, Dr. Kelly said, noting that proper eye protection is also important for those treating the patient.
During treatment, she recommends using a 585-nm or 595-nm wavelength and 0.45-3 millisecond pulse duration--varying pulse duration and wavelength over time to achieve optimal results. Placing patients in the Trendelenburg position can increase blood flow to the area of the PWS, according to Dr. Kelly, who is also with the university's Vascular Birthmarks and Malformations Diagnostic Treatment Center.
Postoperatively, ice should be applied to the treated area, which should be elevated for the first 1-2 postoperative days. A mild analgesic like acetaminophen should be used for discomfort, she said. An emollient should be applied to the treated area, and patients should protect the treated area from sun exposure. A bleaching cream such as hydroquinone may be started 2-3 weeks after treatment for some patients.
Dr. Kelly said that most PWS birthmarks get lighter but require multiple treatments. Some lesions, however, are resistant to treatment, and complete removal is uncommon.
Research on improving results of PWS - to achieve more complete clearance over a shorter period of time - includes studies of imaging methods like laser speckle imaging (LSI), which is used intraoperatively to evaluate the impact of laser treatment on blood flow to determine if flow to the lesional blood vessel is decreased dramatically or shut down.
"Presumably, a greater reduction in flow is associated with greater damage to the blood vessels," said Dr. Kelly, who, with her associates, is studying whether a greater reduction in blood flow during treatment ultimately leads to better results. "We think it does, but we don't know that for sure yet," she said.
They also are studying whether the use of adjunctive agents after laser treatment improves results. These agents include antiangiogenic agents applied topically or administered orally or intravenously. An early study of imiquimod, an immune modulator with antiangiogenic effects, is underway, she noted.
Dr. Kelly disclosed that she has received research grants from Candela Corp. and Graceway Pharmaceuticals, and has served as a consultant to Lumenis. In addition, Graceway and Genentech have donated products for studies she is conducting.
SDEF and this news organization are both owned by Elsevier.