User login
Lateral epicondylitis, also commonly referred to as tennis elbow, is a cumulative trauma disorder (CTD) that affects the extensor tendons of the forearm. Its causative mechanism is repetitive tension and movement of the extensor tendons of the wrist. Characteristic associated movements include supination and pronation of the forearm; these occur frequently during the performance of tasks that require repeated gripping and twisting.1
Among the extensor tendons affected by lateral epicondylitis, the extensor carpi radialis brevis is most commonly identified as the injured tendon.2 While the term epicondylitis implies inflammation as the pathological phenomenon behind this disorder, histologic evidence supports a degenerative process in which a noninflammatory angiofibroblastic tendinosis develops, one that is characterized by degenerative processes, including neovascularization and a disordered collagen matrix.3 In this discussion, therefore, while the disorder will be referred to as lateral epicondylitis (the more common nomenclature), lateral epicondylosis may be a more accurate term.
Pain symptoms described by patients with lateral epicondylitis are thought to be attributable to increasing numbers of free nerve endings in the newly developed granulomatous tissue, in addition to associated synovitis.4 The presence of microvascular damage, a histologic finding in lateral epicondylitis, has also led investigators to suggest several contributing risk factors for tennis elbow, including diabetes and smoking.5
More obscure contributing factors, including psychosocial and socioeconomic concerns, have also been suggested.6
EPIDEMIOLOGY
Though not uncommon in the general population, lateral epicondylitis has a peak incidence in the occupational setting, where its prevalence ranges from 4% to 30%.7 Lateral epicondylitis and other upper-extremity CTD account for 56% of all occupational injuries,8 making them a paramount source of concern for employers and employees alike. In a study of workers’ compensation claims in the United States, van Tulder et al6 found that the mean cost per repetitive strain injury ranged from $5,000 to $8,000. The medical costs and lost work time associated with lateral and medial epicondylitis have been estimated to total more than $22 billion per year in the US alone.7
DIAGNOSIS
Making a diagnosis of lateral epicondylitis is usually straightforward, requiring very little in the way of ancillary testing, such as x-rays or MRI.9
Patient History
A thorough patient history will typically reveal complaints of occupation- or activity-related pain in the lateral elbow, possibly affecting the muscle mass of the forearm.9 Often, the patient will report that symptoms are aggravated by repetitive movements that require strenuous use of the hand, wrist, and/or forearm.10 Examples may include using a screwdriver, grasping a lever, or lifting a heavy load. Occupations associated with risk for lateral epicondylitis include those in the construction industry (eg, plumbers, carpenters) and in manufacturing.
Because a positive association has been established between lateral epicondylitis and ipsilateral rotator cuff tears, carpal tunnel syndrome, and De Quervain’s syndrome, it is important to inquire about any prior history of musculoskeletal injury and coexisting musculoskeletal symptoms. Previous use of oral corticosteroids and a history of smoking are also considered risk factors for lateral epicondylitis.5
Physical Examination
Physical exam findings include reproducible pain at the lateral elbow with resisted supination or wrist dorsiflexion when the forearm is fully extended.9 The examiner may also elicit pain by palpating just distal to the lateral epicondyle over the extensor tendon mass (see Figure 1). Range of motion in the wrist may be diminished due to pain, as when the patient is asked to extend the wrist against resistance. As the condition progresses, the patient may also experience pain and weakness of the forearm with resisted finger motion.
TREATMENT
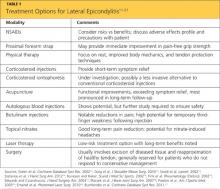
A number of researchers have investigated the most efficacious therapies for lateral epicondylitis (see Table 111-21); as in the case of other musculoskeletal injuries, rest is a cornerstone of treatment. NSAIDs, too, are often indicated, but the clinician must thoroughly evaluate risk versus benefit before initiating NSAID use.11 Additionally, the patient should be educated regarding NSAIDs’ potential side effects and recommended safety precautions.
Two bracing interventions commonly used to treat lateral epicondylitis are the wrist extension splint and the counterforce forearm strap (see Figure 2). In one small prospective, randomized trial (n = 44) in which these devices were compared, no significant between-group differences were found in terms of Mayo Elbow Performance scores, but according to scores derived from American Shoulder and Elbow Society assessments, pain relief was significantly better in patients who wore the wrist extension splint.12 In another study of orthotic management of lateral epicondylosis, immediate improvement in pain-free grip strength was reported in subjects wearing either an elbow strap or an elbow sleeve, but wearers of a wrist splint experienced no immediate change, making it inadvisable as a first-choice orthotic modality.22
Other treatment modalities to be considered include corticosteroid injections, acupuncture, autologous blood and other injection therapies, botulinum injection, topical nitrates, laser therapy, and surgery.
Corticosteroid Injections Versus Physical Therapy
In a randomized controlled trial contrasting the use of corticosteroid injections, physical therapy, and a wait-and-see approach for patients with lateral epicondylitis, corticosteroid injections were found superior in the short term (defined as six weeks after treatment initiation). In the long term, however (ie, at 52 weeks), physical therapy was found more effective than either of the alternative approaches. Outcome measures included general improvement, reduction in severity of the main complaint, alleviation of pain, improved elbow function, and patient satisfaction.13
A less invasive alternative to steroid injections for patients with lateral epicondylitis, though not yet FDA approved, has yielded promising results: administration of transdermal dexamethasone by way of iontophoresis.14,15 This delivery method (in which administration of ionic, water-soluble agents is facilitated using a weak electric current23) was recently studied by Stefanou et al14 in the form of a transdermal patch, activated by a 24-hour battery.
In the short term (ie, upon completion of therapy), patients who received iontophoretic dexamethasone had significantly better grip strength and were better able to return to work than those treated with injections of dexamethasone or triamcinolone. By six months, outcome measures were comparable among the three groups.14 However, possible advantages to iontophoresis are that it is painless, noninvasive, and less likely to cause adverse effects.15,23
Acupuncture
While few sources support the use of complementary modalities to treat lateral epicondylitis,24 findings from one randomized controlled trial offered modest support for acupuncture use. Compared with a sham procedure (in which nonspecific points were targeted), “real” acupuncture—selection and stimulation of specific acupuncture points—provided reductions in pain intensity and improvements in function and strength. Evidence of these improvements became even more robust at two-week follow-up. At two months, however, only improvements in function remained significant.16
Four Injection Therapies
Injections of autologous whole blood or platelet-rich plasma, prolotherapy (injections with hyperosmolar dextrose and sodium morrhuate25), and polidocanol injections were examined in a systematic literature review of treatment strategies for lateral epicondylosis published in 2009 by Rabago et al.3
Although most of the study cohorts involved were small, significant improvements were reported for all modalities and outcome measures, particularly pain: reduction in pain scores by as much as 88% among patients injected with autologous whole blood17; a 55% improvement at eight months in patients treated with the sclerosing agent polidocanol26; improvement as great as 90%, 16 weeks after treatment with prolotherapy (compared with 22% in controls)25; and, in a nonrandomized trial, pain reduction of 93% in patients who had received platelet-rich plasma injections about 26 months earlier.27 Nevertheless, the researchers note, further study is required in larger trials examining specified biomarkers in addition to clinical, biomechanical, and radiologic means of measurement to assure the long-term safety and effectiveness of each of these modalities.3
Botulinum Toxin
Injecting botulinum toxin is another treatment strategy that may be considered when results of more traditional approaches are unsatisfactory. In two double-blind, placebo-controlled, randomized studies, patients injected once with botulinum toxin A experienced significant reductions in pain within four to six weeks, compared with those given placebo.18,28 A notable but expected complication of this treatment reported by Placzek et al18 was weakness of the third finger of the treated hand, two weeks after treatment. However, normal strength was regained in all affected patients by week 18 of follow-up.
Nitrates
Use of topical nitric oxide showed promising results in a 2003 study by Australian researchers.19 Eighty-six patients with chronic extensor tendinosis, all of whom underwent a standard tendon rehabilitation program (ie, rest and stretching and strengthening exercises) and used a forearm counterforce brace, were randomized to receive glyceryl trinitrate transdermal patches or sham patches. One-quarter of a patch was applied just distal to the lateral epicondyle of the humerus for 24 hours, then replaced by another in a rotating fashion around the target spot.
Treated patients reported significant reduction in elbow pain within two weeks. At six months, 81% of patients with active patches were able to perform activities of daily living with no symptoms (versus 60% of controls, with the rehabilitation program and brace use alone).19
Laser Therapy
After completing a 2010 study of low-energy gallium-arsenide (GaAs) laser therapy for the treatment of lateral epicondylitis, researchers found no short-term advantages of laser therapy, compared with a sham procedure—but long-term results were more promising.20 Study participants underwent 15 sessions of treatment (application of a laser probe to the two most sensitive points, with a specified dose given) over a three-week period. Shortly after the treatment period ended, patients in both groups had significant improvements.
At 12 weeks’ follow-up, however, patients in the active treatment group had significantly better long-term results than did controls (about 60% vs 40% improvement from baseline, respectively), especially in functional outcome measures. As the study authors noted, low-energy laser therapy carries a low risk for adverse effects, making it a long-term treatment strategy to be considered for patients with intractable lateral epicondylitis.20
Surgery
When conservative strategies implemented for several months do not resolve symptoms of lateral epicondylitis, surgical intervention may be required.2,21 Whether in open, percutaneous, or arthroscopic procedures, tendinopathic tissue is excised at the origin of the extensor carpi radialis brevis tendon in an effort to re-approximate the healthy tendon.21
Another less frequently used surgical procedure for lateral epicondylitis is extensor tendon release. In one long-term study investigating outpatient open extensor tendon release in 77 affected patients, researchers noted predominately good to excellent outcomes (ie, symptom relief, functional improvement), coupled with a low perioperative complication rate.29
PREVENTION
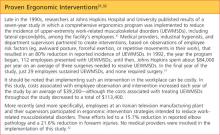
Prevention strategies are designed to mitigate the risk factors and minimize behaviors associated with each CTD. The science of ergonomics has produced numerous strategies intended to reduce the incidence of CTD through proper body mechanics, work habits, and equipment. In the workplace, CTD-specific ergonomic guidelines include posture training, reduction of excessive force and unnecessary repetition, and provision of adequate rest intervals. In addition to improving symptoms and possibly resolving some cases of lateral epicondylitis, ergonomic interventions may even reduce the incidence of new CTD in similarly exposed, asymptomatic workers30 (see “Proven Ergonomic Interventions”31,32).
Regarding specific prevention guidelines for lateral epicondylitis, several ergonomic recommendations can be offered to the patient and the patient’s employer. Consultation with a physical therapist may be helpful in developing specific recommendations focused on prevention of workplace injuries. Regarding CTD, physical therapists may recommend several tendon protection techniques that the clinician can then provide to the patient and his/her employer.33,34
Tendon protection techniques encourage proper body mechanics, avoidance of excessive force and repetition, as well as proper tool selection. Patients should be advised to avoid tasks that require unnecessary repetitive wrist flexion and extension, forearm pronation and supination, and strong, forceful gripping of objects. They should also avoid lifting objects with forearms pronated and wrists extended, as this will place increased tension and stress on the extensor tendon. Rather, patients should be advised to lift objects with their forearm supinated in a scooping motion (see Table 233).
Force is considered a significant contributor to the development of lateral epicondylitis. Thus, patients should be instructed to minimize forceful gestures at work, particularly with the forearm in full extension.34 Patients and employers should be advised to encourage use of proper tools for the tasks performed. Use of hand tools with lighter handles and larger grips requires less force than do tools with heavier, smaller grips, and are more likely to protect the upper-extremity tendons.
Finally, the worker who is required to perform a repetitive task for a sustained amount of time (eg, certain tasks performed by an electrical contractor; steady use of a computer workstation) is likely to benefit from small “micro-breaks” of a few minutes each hour. This habit may reduce cumulative stress, and possibly the incidence of CTD, including lateral epicondylitis.32,34
CONCLUSION
Primary care and occupational medicine clinicians, as well as providers in other frontline specialties, have a great deal to offer in regard to stemming the disabling symptoms and fiscal strain associated with lateral epicondylitis. While early recognition and intervention for patients with symptoms of lateral epicondylitis are essential to the clinician’s role, providers must also focus on key preventive measures. Involving key stakeholders, including patients and their employers and managers, in establishing appropriate safety measures in the workplace is an optimal strategy. The formation of a multidisciplinary health care team that includes ergonomists, physical therapists, and orthopedic specialists may also prove beneficial in both treatment and prevention.
REFERENCES
1. Noteboom T, Cruver R, Keller J, et al. Tennis elbow: a review. J Orthop Sports Phys Ther. 1994;19(6):357-366.
2. Cohen MS, Romeo AA. Lateral epicondylitis: open and arthroscopic treatment. J Am Soc Surg Hand. 2001;1(3):172-176.
3. Rabago D, Best TM, Zgierska AE, et al. A systematic review of four injection therapies for lateral epicondylosis: prolotherapy, polidocanol, whole blood and platelet-rich plasma. Br J Sports Med. 2009;43(7):471-481.
4. Calfee RP, Patel A, DaSilva MF, Akelman E. Management of lateral epicondylitis: current concepts. J Am Acad Orthop Surg. 2008;16(1):19-29.
5. Titchener AG, Fakis A, Tambe AA, et al. Risk factors in lateral epicondylitis (tennis elbow): a case-control study. J Hand Surg Eur Vol. 2012 Apr 4. [Epub ahead of print]
6. van Tulder M, Malmivaara A, Koes B. Repetitive strain injury. Lancet. 2007;369(9575):1815-1822.
7. Werner RA, Franzblau A, Gell N, et al. Predictors of persistent elbow tendonitis among auto assembly workers. J Occup Rehabil. 2005; 15(3):393-400.
8. Melhorn MJ. A prospective study for upper-extremity cumulative trauma disorders of workers in aircraft manufacturing. J Occup Environ Med. 1996;38(12):1264-1271.
9. Johnson GW, Cadwallader K, Scheffel SB, Epperly TD. Treatment of lateral epicondylitis. Am Fam Physician. 2007;76(6):843-848.
10. Haahr JP, Andersen JH. Physical and psychosocial risk factors for lateral epicondylitis: a population based case-referent study. Occup Environ Med. 2003;60(5):322-329.
11. Green S, Buchbinder R, Barnsley L, et al. Non-steroidal anti-inflammatory drugs (NSAIDs) for treating lateral elbow pain in adults. Cochrane Database Syst Rev. 2002;(2):CD003686.
12. Garg R, Adamson GJ, Dawson PA, et al. A prospective randomized study comparing a forearm strap brace versus a wrist splint for the treatment of lateral epicondylitis. J Shoulder Elbow Surg. 2010;19(4):508-512.
13. Smidt N, van der Windt DA, Assendelft WJ, et al. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial. Lancet. 2002;359 (9307):657-662.
14. Stefanou A, Marshall N, Holdan W, Siddiqui A. A randomized study comparing corticosteroid injection to corticosteroid iontophoresis for lateral epicondylitis. J Hand Surg Am. 2012;37(1):104-109.
15. Runeson L, Haker E. Iontophoresis with cortisone in the treatment of lateral epicondylalgia (tennis elbow): a double-blind study. Scand J Med Sci Sports. 2002;12(3):136-142.
16. Fink M, Wolkenstein E, Krst M, Gehrke A. Acupuncture in chronic epicondylitis: a randomized controlled trial. Rheumatology (Oxford). 2002;41(2):205-209.
17. Edwards SG, Calandruccio JH. Autologous blood injections for refractory lateral epicondylitis. J Hand Surgery Am. 2003;28(2):272-278.
18. Placzek R, Drescher W, Deuretzbacher G. Treatment of chronic radial epicondylitis with botulinum toxin A: a double-blind, placebo-controlled, randomized multicenter study. J Bone Joint Surg Am. 2007;89(2):255-260.
19. Paoloni JA, Appleyard RC, Nelson J, Murrell GA. Topical nitric oxide application in the treatment of chronic extensor tendinosis at the elbow: a randomized, double-blinded, placebo-controlled clinical trial. Am J Sports Med. 2003;31(6):915-920.
20. Emanet SK, Altan LI, Yurtkuran M. Investigation of the effect of GaAs laser therapy on lateral epicondylitis. Photomed Laser Surg. 2010;28(3):397-403.
21. Buchbinder R, Johnston RV, Barnsley L, et al. Surgery for lateral elbow pain. Cochrane Database Syst Rev. 2011;(3):CD003525.
22. Jafarian FS, Demneh ES, Tyson SF. The immediate effect of orthotic management on grip strength of patients with lateral epicondylosis.
J Orthop Sports Phys Ther. 2009;39(6):484-489.
23. Grewal R, King GJW. Commentary on “Iontophoresis for the Treatment of Lateral Epicondylitis of the Elbow.” J Hand Surg Am. 2012;37(1):110-111.
24. Green S, Buchbinder R, Barnsley L, et al. Acupuncture for lateral elbow pain. Cochrane Database Syst Rev. 2002;(1):CD003527.
25. Scarpone M, Rabago DP, Zgierska A, et al. The efficacy of prolotherapy for lateral epicondylosis: a pilot study. Clin J Sport Med. 2008;18(3):248-254.
26. Zeisig E, Ohberg L, Alfredson H. Sclerosing polidocanol injections in chronic painful tennis elbow: promising results in a pilot study. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1218-1224.
27. Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med. 2006;34(11):1774-1778.
28. Wong SM, Hui AC, Tong PY, et al. Treatment of lateral epicondylitis with botulinum toxin: a randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2005;143(11):793-797.
29. Solheim E, Hegna J, Øyen J. Extensor tendon release in tennis elbow: results and prognostic factors in 80 elbows. Knee Surg Sports Traumatol Arthrosc. 2011;19(6):1023-1027.
30. Piligian G, Herbert R, Hearns M, et al. Evaluation and management of chronic work-related musculoskeletal disorders of the distal upper extremity. Am J Ind Med. 2000;37(1):75-93.
31. Bernacki EJ, Guidera JA, Schaefer JA, et al. An ergonomics program designed to reduce the incidence of upper extremity work related musculoskeletal disorders. J Occup Environ Med. 1999;41(12):1032-1040.
32. Motamedzade M, Mohseni M, Golmohammadi R, Mahjoob H. Ergonomics intervention in an Iranian television manufacturing industry. Work. 2011;38(3):257-263.
33. Fallon Clinic, Rehabilitation and Sports Medicine. Lateral epicondylitis: protection techniques. http://www.fallonclinic.org/internet/medical/rehab/exercisesheets/lateral_epicondylitis.pdf. Accessed November 27, 2012.
34. Occupational Safety and Health Administration, US Department of Labor. Computer workstations, additional information: awkward postures, contact stress, force, general controls, repetition. www.osha.gov/SLTC/etools/computer workstations/more.html. Accessed November 29, 2012.
Lateral epicondylitis, also commonly referred to as tennis elbow, is a cumulative trauma disorder (CTD) that affects the extensor tendons of the forearm. Its causative mechanism is repetitive tension and movement of the extensor tendons of the wrist. Characteristic associated movements include supination and pronation of the forearm; these occur frequently during the performance of tasks that require repeated gripping and twisting.1
Among the extensor tendons affected by lateral epicondylitis, the extensor carpi radialis brevis is most commonly identified as the injured tendon.2 While the term epicondylitis implies inflammation as the pathological phenomenon behind this disorder, histologic evidence supports a degenerative process in which a noninflammatory angiofibroblastic tendinosis develops, one that is characterized by degenerative processes, including neovascularization and a disordered collagen matrix.3 In this discussion, therefore, while the disorder will be referred to as lateral epicondylitis (the more common nomenclature), lateral epicondylosis may be a more accurate term.
Pain symptoms described by patients with lateral epicondylitis are thought to be attributable to increasing numbers of free nerve endings in the newly developed granulomatous tissue, in addition to associated synovitis.4 The presence of microvascular damage, a histologic finding in lateral epicondylitis, has also led investigators to suggest several contributing risk factors for tennis elbow, including diabetes and smoking.5
More obscure contributing factors, including psychosocial and socioeconomic concerns, have also been suggested.6
EPIDEMIOLOGY
Though not uncommon in the general population, lateral epicondylitis has a peak incidence in the occupational setting, where its prevalence ranges from 4% to 30%.7 Lateral epicondylitis and other upper-extremity CTD account for 56% of all occupational injuries,8 making them a paramount source of concern for employers and employees alike. In a study of workers’ compensation claims in the United States, van Tulder et al6 found that the mean cost per repetitive strain injury ranged from $5,000 to $8,000. The medical costs and lost work time associated with lateral and medial epicondylitis have been estimated to total more than $22 billion per year in the US alone.7
DIAGNOSIS
Making a diagnosis of lateral epicondylitis is usually straightforward, requiring very little in the way of ancillary testing, such as x-rays or MRI.9
Patient History
A thorough patient history will typically reveal complaints of occupation- or activity-related pain in the lateral elbow, possibly affecting the muscle mass of the forearm.9 Often, the patient will report that symptoms are aggravated by repetitive movements that require strenuous use of the hand, wrist, and/or forearm.10 Examples may include using a screwdriver, grasping a lever, or lifting a heavy load. Occupations associated with risk for lateral epicondylitis include those in the construction industry (eg, plumbers, carpenters) and in manufacturing.
Because a positive association has been established between lateral epicondylitis and ipsilateral rotator cuff tears, carpal tunnel syndrome, and De Quervain’s syndrome, it is important to inquire about any prior history of musculoskeletal injury and coexisting musculoskeletal symptoms. Previous use of oral corticosteroids and a history of smoking are also considered risk factors for lateral epicondylitis.5
Physical Examination
Physical exam findings include reproducible pain at the lateral elbow with resisted supination or wrist dorsiflexion when the forearm is fully extended.9 The examiner may also elicit pain by palpating just distal to the lateral epicondyle over the extensor tendon mass (see Figure 1). Range of motion in the wrist may be diminished due to pain, as when the patient is asked to extend the wrist against resistance. As the condition progresses, the patient may also experience pain and weakness of the forearm with resisted finger motion.
TREATMENT
A number of researchers have investigated the most efficacious therapies for lateral epicondylitis (see Table 111-21); as in the case of other musculoskeletal injuries, rest is a cornerstone of treatment. NSAIDs, too, are often indicated, but the clinician must thoroughly evaluate risk versus benefit before initiating NSAID use.11 Additionally, the patient should be educated regarding NSAIDs’ potential side effects and recommended safety precautions.
Two bracing interventions commonly used to treat lateral epicondylitis are the wrist extension splint and the counterforce forearm strap (see Figure 2). In one small prospective, randomized trial (n = 44) in which these devices were compared, no significant between-group differences were found in terms of Mayo Elbow Performance scores, but according to scores derived from American Shoulder and Elbow Society assessments, pain relief was significantly better in patients who wore the wrist extension splint.12 In another study of orthotic management of lateral epicondylosis, immediate improvement in pain-free grip strength was reported in subjects wearing either an elbow strap or an elbow sleeve, but wearers of a wrist splint experienced no immediate change, making it inadvisable as a first-choice orthotic modality.22
Other treatment modalities to be considered include corticosteroid injections, acupuncture, autologous blood and other injection therapies, botulinum injection, topical nitrates, laser therapy, and surgery.
Corticosteroid Injections Versus Physical Therapy
In a randomized controlled trial contrasting the use of corticosteroid injections, physical therapy, and a wait-and-see approach for patients with lateral epicondylitis, corticosteroid injections were found superior in the short term (defined as six weeks after treatment initiation). In the long term, however (ie, at 52 weeks), physical therapy was found more effective than either of the alternative approaches. Outcome measures included general improvement, reduction in severity of the main complaint, alleviation of pain, improved elbow function, and patient satisfaction.13
A less invasive alternative to steroid injections for patients with lateral epicondylitis, though not yet FDA approved, has yielded promising results: administration of transdermal dexamethasone by way of iontophoresis.14,15 This delivery method (in which administration of ionic, water-soluble agents is facilitated using a weak electric current23) was recently studied by Stefanou et al14 in the form of a transdermal patch, activated by a 24-hour battery.
In the short term (ie, upon completion of therapy), patients who received iontophoretic dexamethasone had significantly better grip strength and were better able to return to work than those treated with injections of dexamethasone or triamcinolone. By six months, outcome measures were comparable among the three groups.14 However, possible advantages to iontophoresis are that it is painless, noninvasive, and less likely to cause adverse effects.15,23
Acupuncture
While few sources support the use of complementary modalities to treat lateral epicondylitis,24 findings from one randomized controlled trial offered modest support for acupuncture use. Compared with a sham procedure (in which nonspecific points were targeted), “real” acupuncture—selection and stimulation of specific acupuncture points—provided reductions in pain intensity and improvements in function and strength. Evidence of these improvements became even more robust at two-week follow-up. At two months, however, only improvements in function remained significant.16
Four Injection Therapies
Injections of autologous whole blood or platelet-rich plasma, prolotherapy (injections with hyperosmolar dextrose and sodium morrhuate25), and polidocanol injections were examined in a systematic literature review of treatment strategies for lateral epicondylosis published in 2009 by Rabago et al.3
Although most of the study cohorts involved were small, significant improvements were reported for all modalities and outcome measures, particularly pain: reduction in pain scores by as much as 88% among patients injected with autologous whole blood17; a 55% improvement at eight months in patients treated with the sclerosing agent polidocanol26; improvement as great as 90%, 16 weeks after treatment with prolotherapy (compared with 22% in controls)25; and, in a nonrandomized trial, pain reduction of 93% in patients who had received platelet-rich plasma injections about 26 months earlier.27 Nevertheless, the researchers note, further study is required in larger trials examining specified biomarkers in addition to clinical, biomechanical, and radiologic means of measurement to assure the long-term safety and effectiveness of each of these modalities.3
Botulinum Toxin
Injecting botulinum toxin is another treatment strategy that may be considered when results of more traditional approaches are unsatisfactory. In two double-blind, placebo-controlled, randomized studies, patients injected once with botulinum toxin A experienced significant reductions in pain within four to six weeks, compared with those given placebo.18,28 A notable but expected complication of this treatment reported by Placzek et al18 was weakness of the third finger of the treated hand, two weeks after treatment. However, normal strength was regained in all affected patients by week 18 of follow-up.
Nitrates
Use of topical nitric oxide showed promising results in a 2003 study by Australian researchers.19 Eighty-six patients with chronic extensor tendinosis, all of whom underwent a standard tendon rehabilitation program (ie, rest and stretching and strengthening exercises) and used a forearm counterforce brace, were randomized to receive glyceryl trinitrate transdermal patches or sham patches. One-quarter of a patch was applied just distal to the lateral epicondyle of the humerus for 24 hours, then replaced by another in a rotating fashion around the target spot.
Treated patients reported significant reduction in elbow pain within two weeks. At six months, 81% of patients with active patches were able to perform activities of daily living with no symptoms (versus 60% of controls, with the rehabilitation program and brace use alone).19
Laser Therapy
After completing a 2010 study of low-energy gallium-arsenide (GaAs) laser therapy for the treatment of lateral epicondylitis, researchers found no short-term advantages of laser therapy, compared with a sham procedure—but long-term results were more promising.20 Study participants underwent 15 sessions of treatment (application of a laser probe to the two most sensitive points, with a specified dose given) over a three-week period. Shortly after the treatment period ended, patients in both groups had significant improvements.
At 12 weeks’ follow-up, however, patients in the active treatment group had significantly better long-term results than did controls (about 60% vs 40% improvement from baseline, respectively), especially in functional outcome measures. As the study authors noted, low-energy laser therapy carries a low risk for adverse effects, making it a long-term treatment strategy to be considered for patients with intractable lateral epicondylitis.20
Surgery
When conservative strategies implemented for several months do not resolve symptoms of lateral epicondylitis, surgical intervention may be required.2,21 Whether in open, percutaneous, or arthroscopic procedures, tendinopathic tissue is excised at the origin of the extensor carpi radialis brevis tendon in an effort to re-approximate the healthy tendon.21
Another less frequently used surgical procedure for lateral epicondylitis is extensor tendon release. In one long-term study investigating outpatient open extensor tendon release in 77 affected patients, researchers noted predominately good to excellent outcomes (ie, symptom relief, functional improvement), coupled with a low perioperative complication rate.29
PREVENTION
Prevention strategies are designed to mitigate the risk factors and minimize behaviors associated with each CTD. The science of ergonomics has produced numerous strategies intended to reduce the incidence of CTD through proper body mechanics, work habits, and equipment. In the workplace, CTD-specific ergonomic guidelines include posture training, reduction of excessive force and unnecessary repetition, and provision of adequate rest intervals. In addition to improving symptoms and possibly resolving some cases of lateral epicondylitis, ergonomic interventions may even reduce the incidence of new CTD in similarly exposed, asymptomatic workers30 (see “Proven Ergonomic Interventions”31,32).
Regarding specific prevention guidelines for lateral epicondylitis, several ergonomic recommendations can be offered to the patient and the patient’s employer. Consultation with a physical therapist may be helpful in developing specific recommendations focused on prevention of workplace injuries. Regarding CTD, physical therapists may recommend several tendon protection techniques that the clinician can then provide to the patient and his/her employer.33,34
Tendon protection techniques encourage proper body mechanics, avoidance of excessive force and repetition, as well as proper tool selection. Patients should be advised to avoid tasks that require unnecessary repetitive wrist flexion and extension, forearm pronation and supination, and strong, forceful gripping of objects. They should also avoid lifting objects with forearms pronated and wrists extended, as this will place increased tension and stress on the extensor tendon. Rather, patients should be advised to lift objects with their forearm supinated in a scooping motion (see Table 233).
Force is considered a significant contributor to the development of lateral epicondylitis. Thus, patients should be instructed to minimize forceful gestures at work, particularly with the forearm in full extension.34 Patients and employers should be advised to encourage use of proper tools for the tasks performed. Use of hand tools with lighter handles and larger grips requires less force than do tools with heavier, smaller grips, and are more likely to protect the upper-extremity tendons.
Finally, the worker who is required to perform a repetitive task for a sustained amount of time (eg, certain tasks performed by an electrical contractor; steady use of a computer workstation) is likely to benefit from small “micro-breaks” of a few minutes each hour. This habit may reduce cumulative stress, and possibly the incidence of CTD, including lateral epicondylitis.32,34
CONCLUSION
Primary care and occupational medicine clinicians, as well as providers in other frontline specialties, have a great deal to offer in regard to stemming the disabling symptoms and fiscal strain associated with lateral epicondylitis. While early recognition and intervention for patients with symptoms of lateral epicondylitis are essential to the clinician’s role, providers must also focus on key preventive measures. Involving key stakeholders, including patients and their employers and managers, in establishing appropriate safety measures in the workplace is an optimal strategy. The formation of a multidisciplinary health care team that includes ergonomists, physical therapists, and orthopedic specialists may also prove beneficial in both treatment and prevention.
REFERENCES
1. Noteboom T, Cruver R, Keller J, et al. Tennis elbow: a review. J Orthop Sports Phys Ther. 1994;19(6):357-366.
2. Cohen MS, Romeo AA. Lateral epicondylitis: open and arthroscopic treatment. J Am Soc Surg Hand. 2001;1(3):172-176.
3. Rabago D, Best TM, Zgierska AE, et al. A systematic review of four injection therapies for lateral epicondylosis: prolotherapy, polidocanol, whole blood and platelet-rich plasma. Br J Sports Med. 2009;43(7):471-481.
4. Calfee RP, Patel A, DaSilva MF, Akelman E. Management of lateral epicondylitis: current concepts. J Am Acad Orthop Surg. 2008;16(1):19-29.
5. Titchener AG, Fakis A, Tambe AA, et al. Risk factors in lateral epicondylitis (tennis elbow): a case-control study. J Hand Surg Eur Vol. 2012 Apr 4. [Epub ahead of print]
6. van Tulder M, Malmivaara A, Koes B. Repetitive strain injury. Lancet. 2007;369(9575):1815-1822.
7. Werner RA, Franzblau A, Gell N, et al. Predictors of persistent elbow tendonitis among auto assembly workers. J Occup Rehabil. 2005; 15(3):393-400.
8. Melhorn MJ. A prospective study for upper-extremity cumulative trauma disorders of workers in aircraft manufacturing. J Occup Environ Med. 1996;38(12):1264-1271.
9. Johnson GW, Cadwallader K, Scheffel SB, Epperly TD. Treatment of lateral epicondylitis. Am Fam Physician. 2007;76(6):843-848.
10. Haahr JP, Andersen JH. Physical and psychosocial risk factors for lateral epicondylitis: a population based case-referent study. Occup Environ Med. 2003;60(5):322-329.
11. Green S, Buchbinder R, Barnsley L, et al. Non-steroidal anti-inflammatory drugs (NSAIDs) for treating lateral elbow pain in adults. Cochrane Database Syst Rev. 2002;(2):CD003686.
12. Garg R, Adamson GJ, Dawson PA, et al. A prospective randomized study comparing a forearm strap brace versus a wrist splint for the treatment of lateral epicondylitis. J Shoulder Elbow Surg. 2010;19(4):508-512.
13. Smidt N, van der Windt DA, Assendelft WJ, et al. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial. Lancet. 2002;359 (9307):657-662.
14. Stefanou A, Marshall N, Holdan W, Siddiqui A. A randomized study comparing corticosteroid injection to corticosteroid iontophoresis for lateral epicondylitis. J Hand Surg Am. 2012;37(1):104-109.
15. Runeson L, Haker E. Iontophoresis with cortisone in the treatment of lateral epicondylalgia (tennis elbow): a double-blind study. Scand J Med Sci Sports. 2002;12(3):136-142.
16. Fink M, Wolkenstein E, Krst M, Gehrke A. Acupuncture in chronic epicondylitis: a randomized controlled trial. Rheumatology (Oxford). 2002;41(2):205-209.
17. Edwards SG, Calandruccio JH. Autologous blood injections for refractory lateral epicondylitis. J Hand Surgery Am. 2003;28(2):272-278.
18. Placzek R, Drescher W, Deuretzbacher G. Treatment of chronic radial epicondylitis with botulinum toxin A: a double-blind, placebo-controlled, randomized multicenter study. J Bone Joint Surg Am. 2007;89(2):255-260.
19. Paoloni JA, Appleyard RC, Nelson J, Murrell GA. Topical nitric oxide application in the treatment of chronic extensor tendinosis at the elbow: a randomized, double-blinded, placebo-controlled clinical trial. Am J Sports Med. 2003;31(6):915-920.
20. Emanet SK, Altan LI, Yurtkuran M. Investigation of the effect of GaAs laser therapy on lateral epicondylitis. Photomed Laser Surg. 2010;28(3):397-403.
21. Buchbinder R, Johnston RV, Barnsley L, et al. Surgery for lateral elbow pain. Cochrane Database Syst Rev. 2011;(3):CD003525.
22. Jafarian FS, Demneh ES, Tyson SF. The immediate effect of orthotic management on grip strength of patients with lateral epicondylosis.
J Orthop Sports Phys Ther. 2009;39(6):484-489.
23. Grewal R, King GJW. Commentary on “Iontophoresis for the Treatment of Lateral Epicondylitis of the Elbow.” J Hand Surg Am. 2012;37(1):110-111.
24. Green S, Buchbinder R, Barnsley L, et al. Acupuncture for lateral elbow pain. Cochrane Database Syst Rev. 2002;(1):CD003527.
25. Scarpone M, Rabago DP, Zgierska A, et al. The efficacy of prolotherapy for lateral epicondylosis: a pilot study. Clin J Sport Med. 2008;18(3):248-254.
26. Zeisig E, Ohberg L, Alfredson H. Sclerosing polidocanol injections in chronic painful tennis elbow: promising results in a pilot study. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1218-1224.
27. Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med. 2006;34(11):1774-1778.
28. Wong SM, Hui AC, Tong PY, et al. Treatment of lateral epicondylitis with botulinum toxin: a randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2005;143(11):793-797.
29. Solheim E, Hegna J, Øyen J. Extensor tendon release in tennis elbow: results and prognostic factors in 80 elbows. Knee Surg Sports Traumatol Arthrosc. 2011;19(6):1023-1027.
30. Piligian G, Herbert R, Hearns M, et al. Evaluation and management of chronic work-related musculoskeletal disorders of the distal upper extremity. Am J Ind Med. 2000;37(1):75-93.
31. Bernacki EJ, Guidera JA, Schaefer JA, et al. An ergonomics program designed to reduce the incidence of upper extremity work related musculoskeletal disorders. J Occup Environ Med. 1999;41(12):1032-1040.
32. Motamedzade M, Mohseni M, Golmohammadi R, Mahjoob H. Ergonomics intervention in an Iranian television manufacturing industry. Work. 2011;38(3):257-263.
33. Fallon Clinic, Rehabilitation and Sports Medicine. Lateral epicondylitis: protection techniques. http://www.fallonclinic.org/internet/medical/rehab/exercisesheets/lateral_epicondylitis.pdf. Accessed November 27, 2012.
34. Occupational Safety and Health Administration, US Department of Labor. Computer workstations, additional information: awkward postures, contact stress, force, general controls, repetition. www.osha.gov/SLTC/etools/computer workstations/more.html. Accessed November 29, 2012.
Lateral epicondylitis, also commonly referred to as tennis elbow, is a cumulative trauma disorder (CTD) that affects the extensor tendons of the forearm. Its causative mechanism is repetitive tension and movement of the extensor tendons of the wrist. Characteristic associated movements include supination and pronation of the forearm; these occur frequently during the performance of tasks that require repeated gripping and twisting.1
Among the extensor tendons affected by lateral epicondylitis, the extensor carpi radialis brevis is most commonly identified as the injured tendon.2 While the term epicondylitis implies inflammation as the pathological phenomenon behind this disorder, histologic evidence supports a degenerative process in which a noninflammatory angiofibroblastic tendinosis develops, one that is characterized by degenerative processes, including neovascularization and a disordered collagen matrix.3 In this discussion, therefore, while the disorder will be referred to as lateral epicondylitis (the more common nomenclature), lateral epicondylosis may be a more accurate term.
Pain symptoms described by patients with lateral epicondylitis are thought to be attributable to increasing numbers of free nerve endings in the newly developed granulomatous tissue, in addition to associated synovitis.4 The presence of microvascular damage, a histologic finding in lateral epicondylitis, has also led investigators to suggest several contributing risk factors for tennis elbow, including diabetes and smoking.5
More obscure contributing factors, including psychosocial and socioeconomic concerns, have also been suggested.6
EPIDEMIOLOGY
Though not uncommon in the general population, lateral epicondylitis has a peak incidence in the occupational setting, where its prevalence ranges from 4% to 30%.7 Lateral epicondylitis and other upper-extremity CTD account for 56% of all occupational injuries,8 making them a paramount source of concern for employers and employees alike. In a study of workers’ compensation claims in the United States, van Tulder et al6 found that the mean cost per repetitive strain injury ranged from $5,000 to $8,000. The medical costs and lost work time associated with lateral and medial epicondylitis have been estimated to total more than $22 billion per year in the US alone.7
DIAGNOSIS
Making a diagnosis of lateral epicondylitis is usually straightforward, requiring very little in the way of ancillary testing, such as x-rays or MRI.9
Patient History
A thorough patient history will typically reveal complaints of occupation- or activity-related pain in the lateral elbow, possibly affecting the muscle mass of the forearm.9 Often, the patient will report that symptoms are aggravated by repetitive movements that require strenuous use of the hand, wrist, and/or forearm.10 Examples may include using a screwdriver, grasping a lever, or lifting a heavy load. Occupations associated with risk for lateral epicondylitis include those in the construction industry (eg, plumbers, carpenters) and in manufacturing.
Because a positive association has been established between lateral epicondylitis and ipsilateral rotator cuff tears, carpal tunnel syndrome, and De Quervain’s syndrome, it is important to inquire about any prior history of musculoskeletal injury and coexisting musculoskeletal symptoms. Previous use of oral corticosteroids and a history of smoking are also considered risk factors for lateral epicondylitis.5
Physical Examination
Physical exam findings include reproducible pain at the lateral elbow with resisted supination or wrist dorsiflexion when the forearm is fully extended.9 The examiner may also elicit pain by palpating just distal to the lateral epicondyle over the extensor tendon mass (see Figure 1). Range of motion in the wrist may be diminished due to pain, as when the patient is asked to extend the wrist against resistance. As the condition progresses, the patient may also experience pain and weakness of the forearm with resisted finger motion.
TREATMENT
A number of researchers have investigated the most efficacious therapies for lateral epicondylitis (see Table 111-21); as in the case of other musculoskeletal injuries, rest is a cornerstone of treatment. NSAIDs, too, are often indicated, but the clinician must thoroughly evaluate risk versus benefit before initiating NSAID use.11 Additionally, the patient should be educated regarding NSAIDs’ potential side effects and recommended safety precautions.
Two bracing interventions commonly used to treat lateral epicondylitis are the wrist extension splint and the counterforce forearm strap (see Figure 2). In one small prospective, randomized trial (n = 44) in which these devices were compared, no significant between-group differences were found in terms of Mayo Elbow Performance scores, but according to scores derived from American Shoulder and Elbow Society assessments, pain relief was significantly better in patients who wore the wrist extension splint.12 In another study of orthotic management of lateral epicondylosis, immediate improvement in pain-free grip strength was reported in subjects wearing either an elbow strap or an elbow sleeve, but wearers of a wrist splint experienced no immediate change, making it inadvisable as a first-choice orthotic modality.22
Other treatment modalities to be considered include corticosteroid injections, acupuncture, autologous blood and other injection therapies, botulinum injection, topical nitrates, laser therapy, and surgery.
Corticosteroid Injections Versus Physical Therapy
In a randomized controlled trial contrasting the use of corticosteroid injections, physical therapy, and a wait-and-see approach for patients with lateral epicondylitis, corticosteroid injections were found superior in the short term (defined as six weeks after treatment initiation). In the long term, however (ie, at 52 weeks), physical therapy was found more effective than either of the alternative approaches. Outcome measures included general improvement, reduction in severity of the main complaint, alleviation of pain, improved elbow function, and patient satisfaction.13
A less invasive alternative to steroid injections for patients with lateral epicondylitis, though not yet FDA approved, has yielded promising results: administration of transdermal dexamethasone by way of iontophoresis.14,15 This delivery method (in which administration of ionic, water-soluble agents is facilitated using a weak electric current23) was recently studied by Stefanou et al14 in the form of a transdermal patch, activated by a 24-hour battery.
In the short term (ie, upon completion of therapy), patients who received iontophoretic dexamethasone had significantly better grip strength and were better able to return to work than those treated with injections of dexamethasone or triamcinolone. By six months, outcome measures were comparable among the three groups.14 However, possible advantages to iontophoresis are that it is painless, noninvasive, and less likely to cause adverse effects.15,23
Acupuncture
While few sources support the use of complementary modalities to treat lateral epicondylitis,24 findings from one randomized controlled trial offered modest support for acupuncture use. Compared with a sham procedure (in which nonspecific points were targeted), “real” acupuncture—selection and stimulation of specific acupuncture points—provided reductions in pain intensity and improvements in function and strength. Evidence of these improvements became even more robust at two-week follow-up. At two months, however, only improvements in function remained significant.16
Four Injection Therapies
Injections of autologous whole blood or platelet-rich plasma, prolotherapy (injections with hyperosmolar dextrose and sodium morrhuate25), and polidocanol injections were examined in a systematic literature review of treatment strategies for lateral epicondylosis published in 2009 by Rabago et al.3
Although most of the study cohorts involved were small, significant improvements were reported for all modalities and outcome measures, particularly pain: reduction in pain scores by as much as 88% among patients injected with autologous whole blood17; a 55% improvement at eight months in patients treated with the sclerosing agent polidocanol26; improvement as great as 90%, 16 weeks after treatment with prolotherapy (compared with 22% in controls)25; and, in a nonrandomized trial, pain reduction of 93% in patients who had received platelet-rich plasma injections about 26 months earlier.27 Nevertheless, the researchers note, further study is required in larger trials examining specified biomarkers in addition to clinical, biomechanical, and radiologic means of measurement to assure the long-term safety and effectiveness of each of these modalities.3
Botulinum Toxin
Injecting botulinum toxin is another treatment strategy that may be considered when results of more traditional approaches are unsatisfactory. In two double-blind, placebo-controlled, randomized studies, patients injected once with botulinum toxin A experienced significant reductions in pain within four to six weeks, compared with those given placebo.18,28 A notable but expected complication of this treatment reported by Placzek et al18 was weakness of the third finger of the treated hand, two weeks after treatment. However, normal strength was regained in all affected patients by week 18 of follow-up.
Nitrates
Use of topical nitric oxide showed promising results in a 2003 study by Australian researchers.19 Eighty-six patients with chronic extensor tendinosis, all of whom underwent a standard tendon rehabilitation program (ie, rest and stretching and strengthening exercises) and used a forearm counterforce brace, were randomized to receive glyceryl trinitrate transdermal patches or sham patches. One-quarter of a patch was applied just distal to the lateral epicondyle of the humerus for 24 hours, then replaced by another in a rotating fashion around the target spot.
Treated patients reported significant reduction in elbow pain within two weeks. At six months, 81% of patients with active patches were able to perform activities of daily living with no symptoms (versus 60% of controls, with the rehabilitation program and brace use alone).19
Laser Therapy
After completing a 2010 study of low-energy gallium-arsenide (GaAs) laser therapy for the treatment of lateral epicondylitis, researchers found no short-term advantages of laser therapy, compared with a sham procedure—but long-term results were more promising.20 Study participants underwent 15 sessions of treatment (application of a laser probe to the two most sensitive points, with a specified dose given) over a three-week period. Shortly after the treatment period ended, patients in both groups had significant improvements.
At 12 weeks’ follow-up, however, patients in the active treatment group had significantly better long-term results than did controls (about 60% vs 40% improvement from baseline, respectively), especially in functional outcome measures. As the study authors noted, low-energy laser therapy carries a low risk for adverse effects, making it a long-term treatment strategy to be considered for patients with intractable lateral epicondylitis.20
Surgery
When conservative strategies implemented for several months do not resolve symptoms of lateral epicondylitis, surgical intervention may be required.2,21 Whether in open, percutaneous, or arthroscopic procedures, tendinopathic tissue is excised at the origin of the extensor carpi radialis brevis tendon in an effort to re-approximate the healthy tendon.21
Another less frequently used surgical procedure for lateral epicondylitis is extensor tendon release. In one long-term study investigating outpatient open extensor tendon release in 77 affected patients, researchers noted predominately good to excellent outcomes (ie, symptom relief, functional improvement), coupled with a low perioperative complication rate.29
PREVENTION
Prevention strategies are designed to mitigate the risk factors and minimize behaviors associated with each CTD. The science of ergonomics has produced numerous strategies intended to reduce the incidence of CTD through proper body mechanics, work habits, and equipment. In the workplace, CTD-specific ergonomic guidelines include posture training, reduction of excessive force and unnecessary repetition, and provision of adequate rest intervals. In addition to improving symptoms and possibly resolving some cases of lateral epicondylitis, ergonomic interventions may even reduce the incidence of new CTD in similarly exposed, asymptomatic workers30 (see “Proven Ergonomic Interventions”31,32).
Regarding specific prevention guidelines for lateral epicondylitis, several ergonomic recommendations can be offered to the patient and the patient’s employer. Consultation with a physical therapist may be helpful in developing specific recommendations focused on prevention of workplace injuries. Regarding CTD, physical therapists may recommend several tendon protection techniques that the clinician can then provide to the patient and his/her employer.33,34
Tendon protection techniques encourage proper body mechanics, avoidance of excessive force and repetition, as well as proper tool selection. Patients should be advised to avoid tasks that require unnecessary repetitive wrist flexion and extension, forearm pronation and supination, and strong, forceful gripping of objects. They should also avoid lifting objects with forearms pronated and wrists extended, as this will place increased tension and stress on the extensor tendon. Rather, patients should be advised to lift objects with their forearm supinated in a scooping motion (see Table 233).
Force is considered a significant contributor to the development of lateral epicondylitis. Thus, patients should be instructed to minimize forceful gestures at work, particularly with the forearm in full extension.34 Patients and employers should be advised to encourage use of proper tools for the tasks performed. Use of hand tools with lighter handles and larger grips requires less force than do tools with heavier, smaller grips, and are more likely to protect the upper-extremity tendons.
Finally, the worker who is required to perform a repetitive task for a sustained amount of time (eg, certain tasks performed by an electrical contractor; steady use of a computer workstation) is likely to benefit from small “micro-breaks” of a few minutes each hour. This habit may reduce cumulative stress, and possibly the incidence of CTD, including lateral epicondylitis.32,34
CONCLUSION
Primary care and occupational medicine clinicians, as well as providers in other frontline specialties, have a great deal to offer in regard to stemming the disabling symptoms and fiscal strain associated with lateral epicondylitis. While early recognition and intervention for patients with symptoms of lateral epicondylitis are essential to the clinician’s role, providers must also focus on key preventive measures. Involving key stakeholders, including patients and their employers and managers, in establishing appropriate safety measures in the workplace is an optimal strategy. The formation of a multidisciplinary health care team that includes ergonomists, physical therapists, and orthopedic specialists may also prove beneficial in both treatment and prevention.
REFERENCES
1. Noteboom T, Cruver R, Keller J, et al. Tennis elbow: a review. J Orthop Sports Phys Ther. 1994;19(6):357-366.
2. Cohen MS, Romeo AA. Lateral epicondylitis: open and arthroscopic treatment. J Am Soc Surg Hand. 2001;1(3):172-176.
3. Rabago D, Best TM, Zgierska AE, et al. A systematic review of four injection therapies for lateral epicondylosis: prolotherapy, polidocanol, whole blood and platelet-rich plasma. Br J Sports Med. 2009;43(7):471-481.
4. Calfee RP, Patel A, DaSilva MF, Akelman E. Management of lateral epicondylitis: current concepts. J Am Acad Orthop Surg. 2008;16(1):19-29.
5. Titchener AG, Fakis A, Tambe AA, et al. Risk factors in lateral epicondylitis (tennis elbow): a case-control study. J Hand Surg Eur Vol. 2012 Apr 4. [Epub ahead of print]
6. van Tulder M, Malmivaara A, Koes B. Repetitive strain injury. Lancet. 2007;369(9575):1815-1822.
7. Werner RA, Franzblau A, Gell N, et al. Predictors of persistent elbow tendonitis among auto assembly workers. J Occup Rehabil. 2005; 15(3):393-400.
8. Melhorn MJ. A prospective study for upper-extremity cumulative trauma disorders of workers in aircraft manufacturing. J Occup Environ Med. 1996;38(12):1264-1271.
9. Johnson GW, Cadwallader K, Scheffel SB, Epperly TD. Treatment of lateral epicondylitis. Am Fam Physician. 2007;76(6):843-848.
10. Haahr JP, Andersen JH. Physical and psychosocial risk factors for lateral epicondylitis: a population based case-referent study. Occup Environ Med. 2003;60(5):322-329.
11. Green S, Buchbinder R, Barnsley L, et al. Non-steroidal anti-inflammatory drugs (NSAIDs) for treating lateral elbow pain in adults. Cochrane Database Syst Rev. 2002;(2):CD003686.
12. Garg R, Adamson GJ, Dawson PA, et al. A prospective randomized study comparing a forearm strap brace versus a wrist splint for the treatment of lateral epicondylitis. J Shoulder Elbow Surg. 2010;19(4):508-512.
13. Smidt N, van der Windt DA, Assendelft WJ, et al. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial. Lancet. 2002;359 (9307):657-662.
14. Stefanou A, Marshall N, Holdan W, Siddiqui A. A randomized study comparing corticosteroid injection to corticosteroid iontophoresis for lateral epicondylitis. J Hand Surg Am. 2012;37(1):104-109.
15. Runeson L, Haker E. Iontophoresis with cortisone in the treatment of lateral epicondylalgia (tennis elbow): a double-blind study. Scand J Med Sci Sports. 2002;12(3):136-142.
16. Fink M, Wolkenstein E, Krst M, Gehrke A. Acupuncture in chronic epicondylitis: a randomized controlled trial. Rheumatology (Oxford). 2002;41(2):205-209.
17. Edwards SG, Calandruccio JH. Autologous blood injections for refractory lateral epicondylitis. J Hand Surgery Am. 2003;28(2):272-278.
18. Placzek R, Drescher W, Deuretzbacher G. Treatment of chronic radial epicondylitis with botulinum toxin A: a double-blind, placebo-controlled, randomized multicenter study. J Bone Joint Surg Am. 2007;89(2):255-260.
19. Paoloni JA, Appleyard RC, Nelson J, Murrell GA. Topical nitric oxide application in the treatment of chronic extensor tendinosis at the elbow: a randomized, double-blinded, placebo-controlled clinical trial. Am J Sports Med. 2003;31(6):915-920.
20. Emanet SK, Altan LI, Yurtkuran M. Investigation of the effect of GaAs laser therapy on lateral epicondylitis. Photomed Laser Surg. 2010;28(3):397-403.
21. Buchbinder R, Johnston RV, Barnsley L, et al. Surgery for lateral elbow pain. Cochrane Database Syst Rev. 2011;(3):CD003525.
22. Jafarian FS, Demneh ES, Tyson SF. The immediate effect of orthotic management on grip strength of patients with lateral epicondylosis.
J Orthop Sports Phys Ther. 2009;39(6):484-489.
23. Grewal R, King GJW. Commentary on “Iontophoresis for the Treatment of Lateral Epicondylitis of the Elbow.” J Hand Surg Am. 2012;37(1):110-111.
24. Green S, Buchbinder R, Barnsley L, et al. Acupuncture for lateral elbow pain. Cochrane Database Syst Rev. 2002;(1):CD003527.
25. Scarpone M, Rabago DP, Zgierska A, et al. The efficacy of prolotherapy for lateral epicondylosis: a pilot study. Clin J Sport Med. 2008;18(3):248-254.
26. Zeisig E, Ohberg L, Alfredson H. Sclerosing polidocanol injections in chronic painful tennis elbow: promising results in a pilot study. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1218-1224.
27. Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med. 2006;34(11):1774-1778.
28. Wong SM, Hui AC, Tong PY, et al. Treatment of lateral epicondylitis with botulinum toxin: a randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2005;143(11):793-797.
29. Solheim E, Hegna J, Øyen J. Extensor tendon release in tennis elbow: results and prognostic factors in 80 elbows. Knee Surg Sports Traumatol Arthrosc. 2011;19(6):1023-1027.
30. Piligian G, Herbert R, Hearns M, et al. Evaluation and management of chronic work-related musculoskeletal disorders of the distal upper extremity. Am J Ind Med. 2000;37(1):75-93.
31. Bernacki EJ, Guidera JA, Schaefer JA, et al. An ergonomics program designed to reduce the incidence of upper extremity work related musculoskeletal disorders. J Occup Environ Med. 1999;41(12):1032-1040.
32. Motamedzade M, Mohseni M, Golmohammadi R, Mahjoob H. Ergonomics intervention in an Iranian television manufacturing industry. Work. 2011;38(3):257-263.
33. Fallon Clinic, Rehabilitation and Sports Medicine. Lateral epicondylitis: protection techniques. http://www.fallonclinic.org/internet/medical/rehab/exercisesheets/lateral_epicondylitis.pdf. Accessed November 27, 2012.
34. Occupational Safety and Health Administration, US Department of Labor. Computer workstations, additional information: awkward postures, contact stress, force, general controls, repetition. www.osha.gov/SLTC/etools/computer workstations/more.html. Accessed November 29, 2012.