User login
according to researchers who conducted a recent multi-institutional analysis.
The proportion of margin-negative resections was 92% in a series of 59 patients who underwent resection at one of three tertiary hospitals, the study authors reported.
The 3-year disease-free survival and overall survival rates were 41.9% and 66%, respectively, in the 44 patients for whom longer-term follow-up was available, according to the investigators, led by Francesco Guerra, MD, of Ospedali Riuniti Marche Nord Hospital in Pesaro, Italy.
“These findings are consistent with those of patients resected via conventional laparoscopy or open surgery in contemporary series,” Dr. Guerra and his coauthors wrote in a report published in Surgical Oncology.
It’s still a matter of debate, however, whether robotic surgery has clear advantages over conventional laparoscopy for liver surgery, according to the investigators. Direct comparisons of robotic versus conventional laparoscopic liver resection are scarce, with most available data stemming from often heterogeneous case-control series with no long-term oncologic outcome data.
“Most centers have consolidated experience either in laparoscopic or in robotic liver resection,” the authors wrote. “Hence, reliable comparative analyses are likely difficult to carry out.”
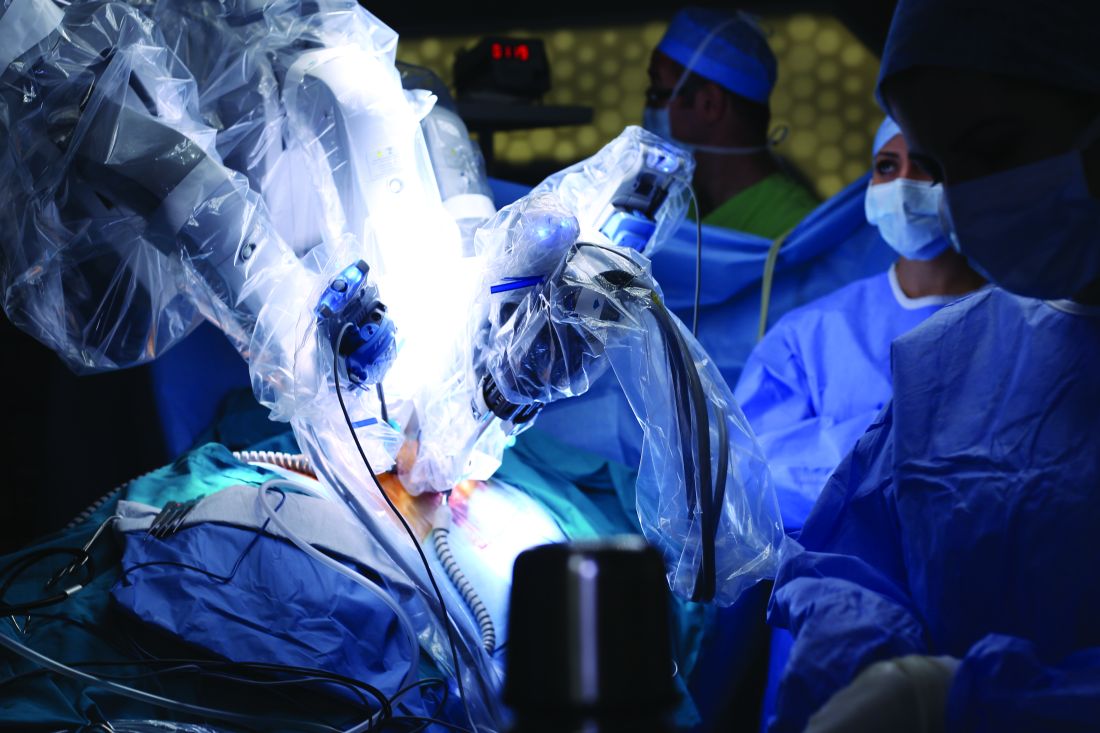
Because of the scarcity of results, Dr. Guerra and his colleagues sought to investigate short- and long-term outcomes for a consecutive series of 59 patients who underwent minimally invasive, ultrasound-guided robotic surgery between 2008 and 2018 at one of three tertiary facilities. Each procedure had been performed by surgeons experienced in both liver surgery and robotics. The median age of patients undergoing the procedure was 64 years, 63% were male, and the median body mass index was 26 kg/m2.
Almost half the patients (46%) had multiple lesions removed, while about one-quarter had concomitant procedures, mainly cholecystectomy, according to the report.
Robotic surgeries were converted to open procedures in seven patients, or about 12%, a statistic comparable with other reports of laparoscopic or robotic surgery, the investigators noted.
Postoperative complications were seen in 16 patients, or 27%. That included 13 patients with class I-II complications and 3 patients with class III-IV complications, including 2 cases of heart failure and 1 case of postoperative bile leak requiring radiologic and endoscopic therapy.
The reported 3-year disease-free and overall survival of 41.9% and 66.1% was based on a mean follow-up of 19.5 months in 44 patients for whom longer-term data were available. There were 16 cases of recurrent disease, including 10 patients with evidence of liver recurrence.
“Taken together, our data show that robotics is an effective option to resect colorectal liver metastases, providing an oncological outcome similar to that of laparoscopy and open surgery,” the investigators wrote.
Dr. Guerra and colleagues reported no disclosures related to their research.
SOURCE: Guerra F et al. Surg Oncol. 2018 Nov 1. doi: 10.1016/j.suronc.2018.10.011.
according to researchers who conducted a recent multi-institutional analysis.
The proportion of margin-negative resections was 92% in a series of 59 patients who underwent resection at one of three tertiary hospitals, the study authors reported.
The 3-year disease-free survival and overall survival rates were 41.9% and 66%, respectively, in the 44 patients for whom longer-term follow-up was available, according to the investigators, led by Francesco Guerra, MD, of Ospedali Riuniti Marche Nord Hospital in Pesaro, Italy.
“These findings are consistent with those of patients resected via conventional laparoscopy or open surgery in contemporary series,” Dr. Guerra and his coauthors wrote in a report published in Surgical Oncology.
It’s still a matter of debate, however, whether robotic surgery has clear advantages over conventional laparoscopy for liver surgery, according to the investigators. Direct comparisons of robotic versus conventional laparoscopic liver resection are scarce, with most available data stemming from often heterogeneous case-control series with no long-term oncologic outcome data.
“Most centers have consolidated experience either in laparoscopic or in robotic liver resection,” the authors wrote. “Hence, reliable comparative analyses are likely difficult to carry out.”
Because of the scarcity of results, Dr. Guerra and his colleagues sought to investigate short- and long-term outcomes for a consecutive series of 59 patients who underwent minimally invasive, ultrasound-guided robotic surgery between 2008 and 2018 at one of three tertiary facilities. Each procedure had been performed by surgeons experienced in both liver surgery and robotics. The median age of patients undergoing the procedure was 64 years, 63% were male, and the median body mass index was 26 kg/m2.
Almost half the patients (46%) had multiple lesions removed, while about one-quarter had concomitant procedures, mainly cholecystectomy, according to the report.
Robotic surgeries were converted to open procedures in seven patients, or about 12%, a statistic comparable with other reports of laparoscopic or robotic surgery, the investigators noted.
Postoperative complications were seen in 16 patients, or 27%. That included 13 patients with class I-II complications and 3 patients with class III-IV complications, including 2 cases of heart failure and 1 case of postoperative bile leak requiring radiologic and endoscopic therapy.
The reported 3-year disease-free and overall survival of 41.9% and 66.1% was based on a mean follow-up of 19.5 months in 44 patients for whom longer-term data were available. There were 16 cases of recurrent disease, including 10 patients with evidence of liver recurrence.
“Taken together, our data show that robotics is an effective option to resect colorectal liver metastases, providing an oncological outcome similar to that of laparoscopy and open surgery,” the investigators wrote.
Dr. Guerra and colleagues reported no disclosures related to their research.
SOURCE: Guerra F et al. Surg Oncol. 2018 Nov 1. doi: 10.1016/j.suronc.2018.10.011.
according to researchers who conducted a recent multi-institutional analysis.
The proportion of margin-negative resections was 92% in a series of 59 patients who underwent resection at one of three tertiary hospitals, the study authors reported.
The 3-year disease-free survival and overall survival rates were 41.9% and 66%, respectively, in the 44 patients for whom longer-term follow-up was available, according to the investigators, led by Francesco Guerra, MD, of Ospedali Riuniti Marche Nord Hospital in Pesaro, Italy.
“These findings are consistent with those of patients resected via conventional laparoscopy or open surgery in contemporary series,” Dr. Guerra and his coauthors wrote in a report published in Surgical Oncology.
It’s still a matter of debate, however, whether robotic surgery has clear advantages over conventional laparoscopy for liver surgery, according to the investigators. Direct comparisons of robotic versus conventional laparoscopic liver resection are scarce, with most available data stemming from often heterogeneous case-control series with no long-term oncologic outcome data.
“Most centers have consolidated experience either in laparoscopic or in robotic liver resection,” the authors wrote. “Hence, reliable comparative analyses are likely difficult to carry out.”
Because of the scarcity of results, Dr. Guerra and his colleagues sought to investigate short- and long-term outcomes for a consecutive series of 59 patients who underwent minimally invasive, ultrasound-guided robotic surgery between 2008 and 2018 at one of three tertiary facilities. Each procedure had been performed by surgeons experienced in both liver surgery and robotics. The median age of patients undergoing the procedure was 64 years, 63% were male, and the median body mass index was 26 kg/m2.
Almost half the patients (46%) had multiple lesions removed, while about one-quarter had concomitant procedures, mainly cholecystectomy, according to the report.
Robotic surgeries were converted to open procedures in seven patients, or about 12%, a statistic comparable with other reports of laparoscopic or robotic surgery, the investigators noted.
Postoperative complications were seen in 16 patients, or 27%. That included 13 patients with class I-II complications and 3 patients with class III-IV complications, including 2 cases of heart failure and 1 case of postoperative bile leak requiring radiologic and endoscopic therapy.
The reported 3-year disease-free and overall survival of 41.9% and 66.1% was based on a mean follow-up of 19.5 months in 44 patients for whom longer-term data were available. There were 16 cases of recurrent disease, including 10 patients with evidence of liver recurrence.
“Taken together, our data show that robotics is an effective option to resect colorectal liver metastases, providing an oncological outcome similar to that of laparoscopy and open surgery,” the investigators wrote.
Dr. Guerra and colleagues reported no disclosures related to their research.
SOURCE: Guerra F et al. Surg Oncol. 2018 Nov 1. doi: 10.1016/j.suronc.2018.10.011.
FROM SURGICAL ONCOLOGY
Key clinical point: Outcomes for robotic surgery for colorectal liver metastases are not inferior to laparoscopic and open surgical approaches.
Major finding: Negative margins were achieved in 92% of lesions, while 3-year disease-free and overall survival were 41.9% and 66.1%, respectively.
Study details: An analysis of 59 patients undergoing robotic surgery for colorectal liver metastases at one of three institutions between 2008 and 2018.
Disclosures: The study authors reported no disclosures.
Source: Guerra F et al. Surg Oncol. 2018 Nov 1. doi: 10.1016/j.suronc.2018.10.011.